Antenatal assessment of fetal wellbeing Professor Dr Parul
Antenatal assessment of fetal wellbeing Professor Dr. Parul Jahan Head of the Dept. of Obs & gynae MCW&H
Definition These are some tools for assessment of fetal condition in ante natal period.
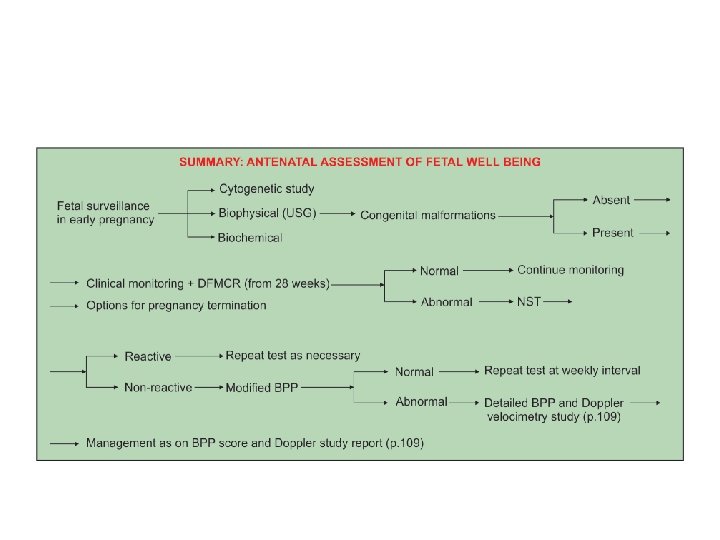
Antenatal Fetal Monitoring Aims : • Ensure growth & well being of fetus • Screen high risk factors that may affect fetal growth Primary objective : Avoid fetal death
Indications 1)Pregnancy with obstetric complications: IUGR Multiple pregnancy Polyhydramnios Oligohydramnios Rhesus alloimmunization
Indications 1)Pregnancy with obstetric complications: IUGR Multiple pregnancy Polyhydramnios Oligohydramnios Rhesus alloimmunization
Contd… 2) Pregnancy with medical complications: Diabetes mellitus Hypertension Epilepsy Renal or Cardiac disease Infection (Tuberculosis) SLE
Contd… 3)Others: Advanced maternal age (> 35 years) Previous still birth or recurrent abortion Structural (anencephaly, spina bifida) Chromosomal abnormalities 4)Routine antenatal testing
Rationality • Tests must provide superior information than clinical evaluation • Should be helpful in management • Benefits of tests must outweigh potential risks and costs.
Clinical Assessment • Maternal weight measurement in each F/U : 2 nd half of pregnancy - 1 kg a fortnight. • Blood pressure: Prior to 12 weeks helps to differentiate a pre-existing chronic HTN from PIH.
Contd… • Symphysio-fundal height : - After 24 weeks corresponds to period of gestation. - Variation of 1– 2 cm acceptable. • Clinical assessment of liquor • Girth of abdomen
Special investigations • Biochemical • Biophysical • Cytogenetic analysis
Biochemical Tests • Maternal serum alpha fetoprotein (MSAFP) • Triple test: MSAFP, h. CG and UE 3. • Quadruple test (MSAFP, UE 3, Total h. CG, Inhibin A) • Acetylcholine esterase - ↑in open neural tube defects. • Inhibin A - ↑ in Down’s syndrome
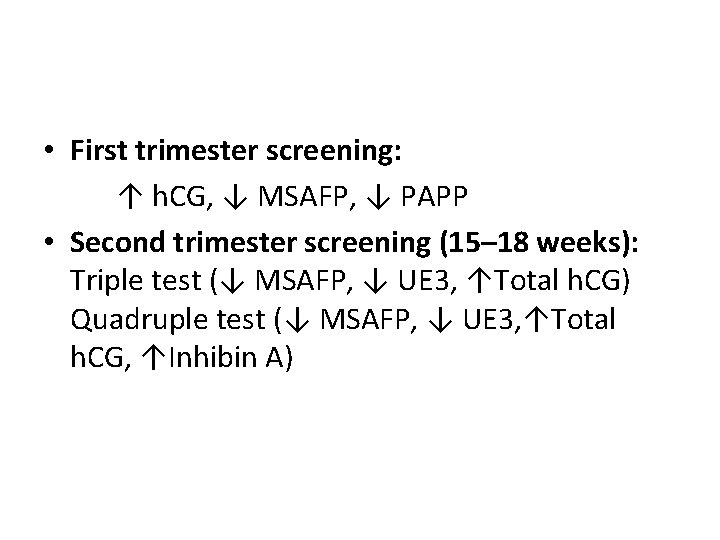
• First trimester screening: ↑ h. CG, ↓ MSAFP, ↓ PAPP • Second trimester screening (15– 18 weeks): Triple test (↓ MSAFP, ↓ UE 3, ↑Total h. CG) Quadruple test (↓ MSAFP, ↓ UE 3, ↑Total h. CG, ↑Inhibin A)
Cytogenetic Analysis : • Amniocentesis • Chorion villus sampling (CVS) • Cordocentesis • Fluorescence In Situ Hybridization
Biophysical Tests in late pregnancy (I) Fetal movement count (II) Cardiotocography (CTG) (III) Non-stress test (NST) (IV) USG (V) Fetal biophysical profile (BPP) (VI) Doppler ultrasound (VII) Vibro acoustic stimulation test (VIII) Contraction stress test (CST)
Fetal movement count Any of the two methods can be applied: • Cardif ‘count 10’ formula: The patient counts fetal movements starting at 9 am. The counting comes to an end as soon as 10 movements are perceived. She is instructed to report the physician if— (i) less than 10 movements occur during 12 hours on 2 successive days or (ii) no movement is perceived even after 12 hours in a single day.
• Daily fetal movement count (DFMC): 3 counts each of one hour duration (morning, noon and evening) are recommended. Total counts multiplied by four gives daily (12 hour) fetal movement count (DFMC). If there is diminution of the number of ‘kicks’ to less than 10 in 12 hours (or less than 3 in each hour), it indicates fetal compromise.
Role of USG Late Pregnancy : Measurement of BPD, AC, HC, FL and AFI. IUGR can be diagnosed accurately with serial measurement of BPD, AC, HC, FL and amniotic fluid volume. AC is the single measurement which best reflects fetal nutrition. When the HC/AC ratio is elevated (> 1. 0) after 34 weeks, IUGR is suspected.
Non-stress test (NST) In non-stress test, a continuous electronic monitoring of the fetal heart rate along with recording of fetal movement is undertaken.
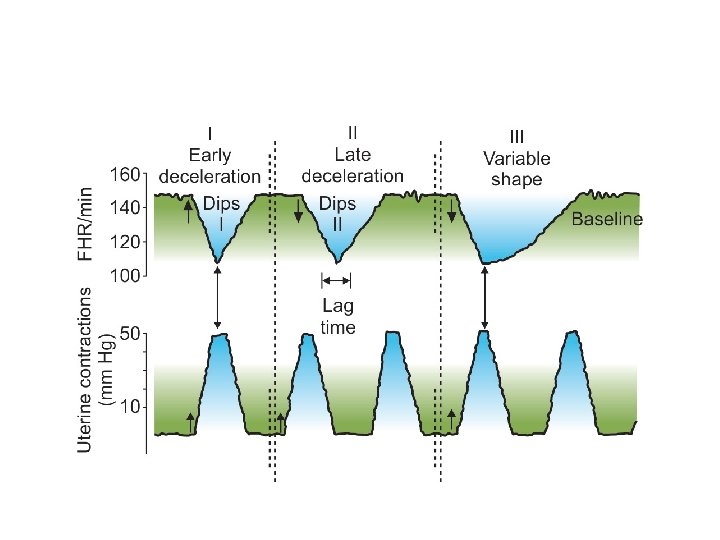
Fetal Cardiotocography (CTG): Defition : Is the graphical presentation of the foetal heart activity and the uterine contraction to detect the foetal hypoxia. A normal CTG tracing after 32 weeks, • Base line heart rate of 110– 150 b/m • Base line variability 5– 25 bpm. • No deceleration or early deceleration of very short duration. • 2 or more accelerations during a 20 minute period
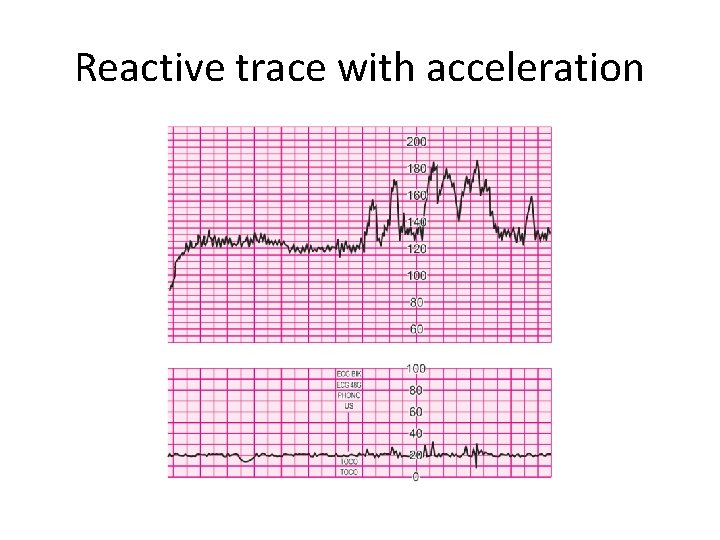
Reactive trace with acceleration
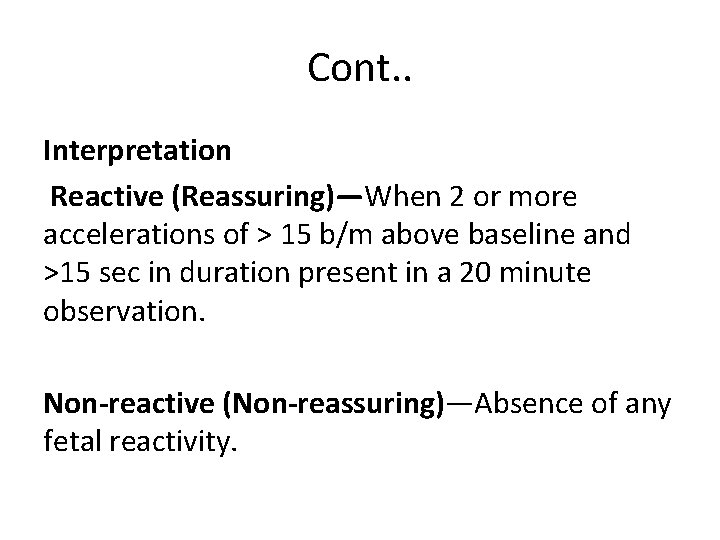
Cont. . Interpretation Reactive (Reassuring)—When 2 or more accelerations of > 15 b/m above baseline and >15 sec in duration present in a 20 minute observation. Non-reactive (Non-reassuring)—Absence of any fetal reactivity.
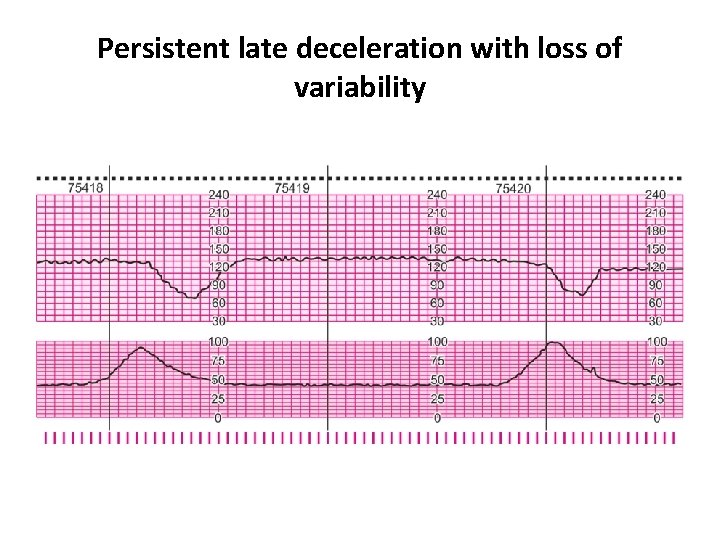
Persistent late deceleration with loss of variability
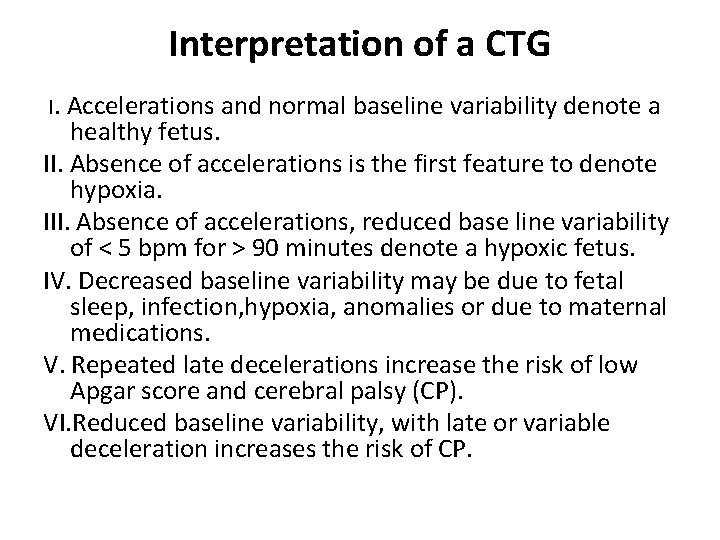
Interpretation of a CTG I. Accelerations and normal baseline variability denote a healthy fetus. II. Absence of accelerations is the first feature to denote hypoxia. III. Absence of accelerations, reduced base line variability of < 5 bpm for > 90 minutes denote a hypoxic fetus. IV. Decreased baseline variability may be due to fetal sleep, infection, hypoxia, anomalies or due to maternal medications. V. Repeated late decelerations increase the risk of low Apgar score and cerebral palsy (CP). VI. Reduced baseline variability, with late or variable deceleration increases the risk of CP.
Biophysical profile Definition : Screening test for utero-placental insufficiency. Pathophysiology : Fetal biophysical activities are initiated, modulated and regulated through fetal nervous system. Fetal CNS is very much sensitive to diminished oxygenation. Hypoxia → metabolic acidosis → CNS depression → changes in fetal biophysical activity.
Fetal Biophysical Profile (BPP) BPP using real time ultrasonography has a high predictive value for fetal assessment. Indication— Non-reactive NST High risk pregnancy Test frequency weekly - normal NST twice weekly - an abnormal test
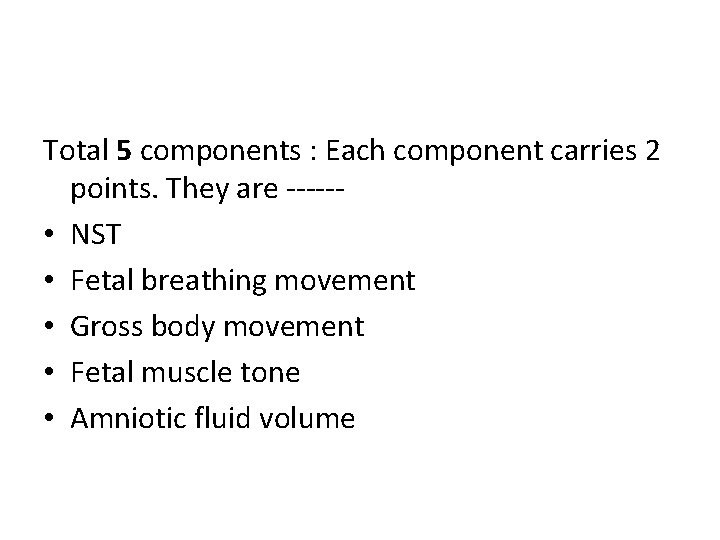
Total 5 components : Each component carries 2 points. They are ----- • NST • Fetal breathing movement • Gross body movement • Fetal muscle tone • Amniotic fluid volume
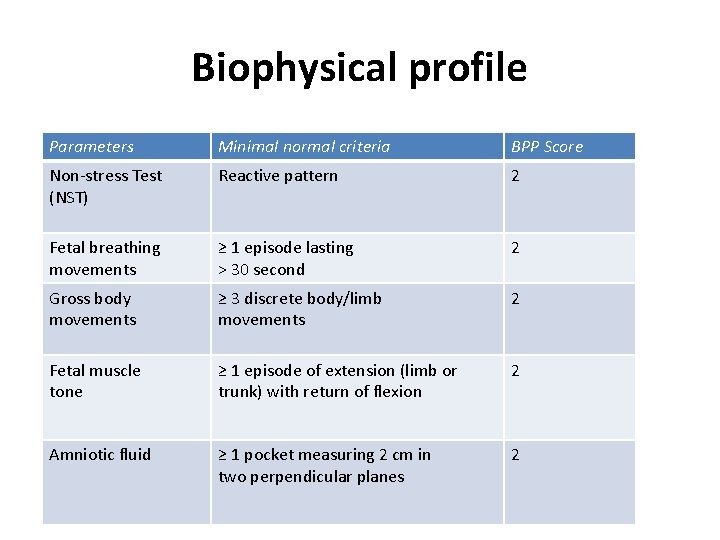
Biophysical profile Parameters Minimal normal criteria BPP Score Non-stress Test (NST) Reactive pattern 2 Fetal breathing movements ≥ 1 episode lasting > 30 second 2 Gross body movements ≥ 3 discrete body/limb movements 2 Fetal muscle tone ≥ 1 episode of extension (limb or trunk) with return of flexion 2 Amniotic fluid ≥ 1 pocket measuring 2 cm in two perpendicular planes 2
Modified Biophysical Profile Consists of NST Amniotic fluid index
Amniotic fluid volume (AFV) • Amniotic fluid volume is primarily dependent upon the fetal urine, pulmonary fluid production and fetal swallowing. • Decreasing AFV may be the result of fetal hypoxia and placental insufficiency. A vertical pocket of amniotic fluid > 2 cm is considered normal.
Amniotic fluid index (AFI) : is the sum of vertical pockets from 4 quadrants of uterine cavity. Norma value : 5 - 20 AFI < 5 is associated with increased risk of perinatal mortality and morbidity.
Contraction stress test (CST) Based on the response of the fetus at risk for utero placental insufficiency in relation to uterine contractions
Doppler Ultrasound Velocimetry Doppler flow velocity wave forms are obtained from arterial and venous beds in the fetus. Arterial Doppler : waveforms are helpful to assess the downstream vascular resistance. It is used to measure the peak systolic(s), peak diastolic (D) and mean (M) volumes. From these values S/D ratio, pulsatility index (PI), Resistance Index (RI) are calculated.
• In a normal pregnancy the S/D ratio, PI and RI decreases as the gestational age advances. Higher values greater than 2 SDs above the gestational age mean indicates reduced diastolic velocities and increased placental vascular resistance. These features are at increased risk for adverse pregnancy outcome.
Venous Doppler provide information about cardiac forward function (cardiac compliance, contractility and after load). Fetuses with abnormal cardiac function show pulsatile flow in the umbilical vein (UV) instead of monophasic flow.

THANK YOU
- Slides: 38