Antegrade Femoral and Retrograde Popliteal Artery Access Aravinda

- Slides: 30
Antegrade Femoral and Retrograde Popliteal Artery Access Aravinda Nanjundappa, MD, FSCAI, FACC West Virginia University Charleston. WV
Disclosures • Paid consultant COOK medical • Speaker Bristol Mayer Squibb
Why access is important ? • No access no intervention • 2 important needs for intervention in vascular interventions: Ø Obtain a good access and closure at end of the case. Ø Ability to cross a CTO.
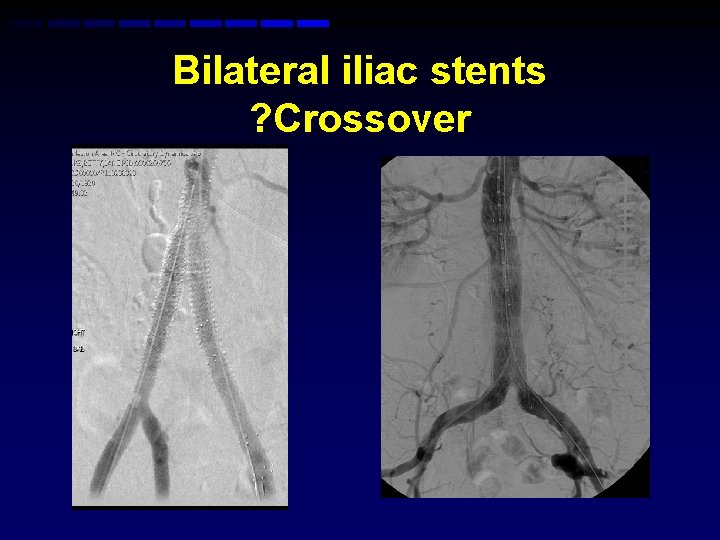
How to choose access? • Common femoral artery: Advantages Ø Retrograde: Most common to perform cross over, easy, familiar and convenient • CFA: Disadvantages Ø Sometimes not enough support to cross TASC D fem-pop and tibio Peroneal lesions Ø Limited catheters, wire and balloon length Ø Limited access in patients with steep iliac bifurcation, bilateral CIA stents, Aorto Bi fem grafts and AAA modular stent grafts
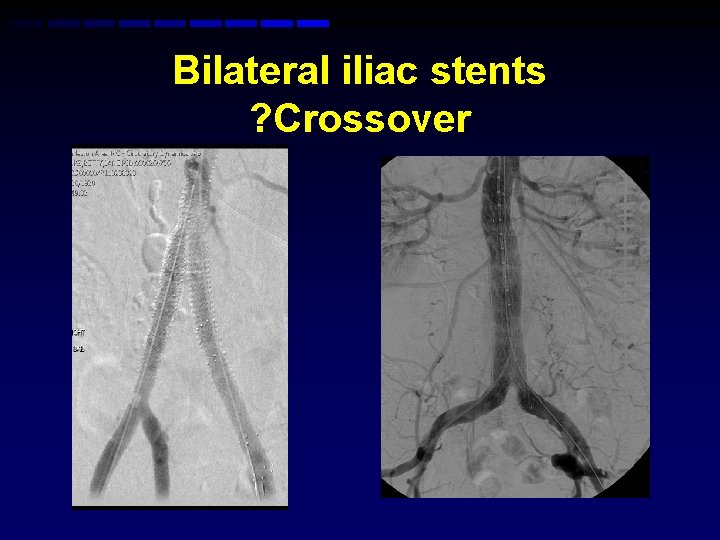
Bilateral iliac stents ? Crossover
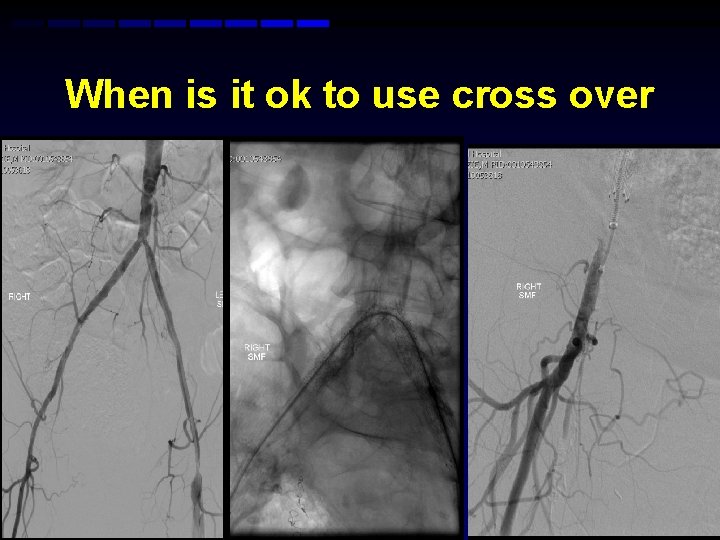
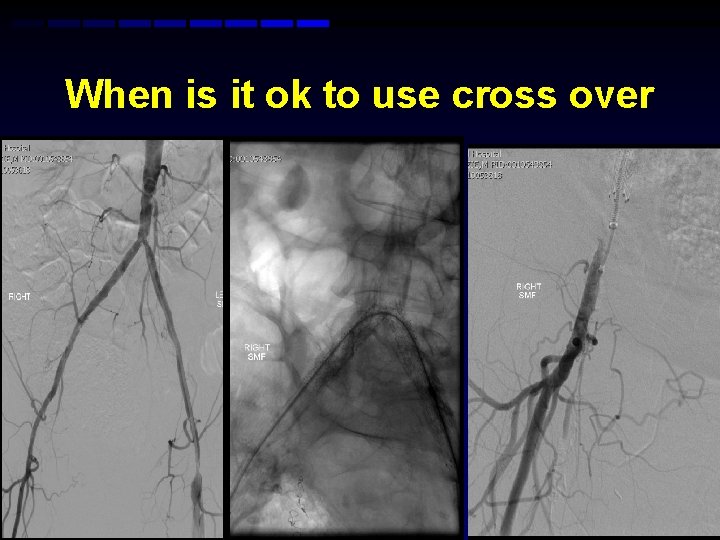
When is it ok to use cross over
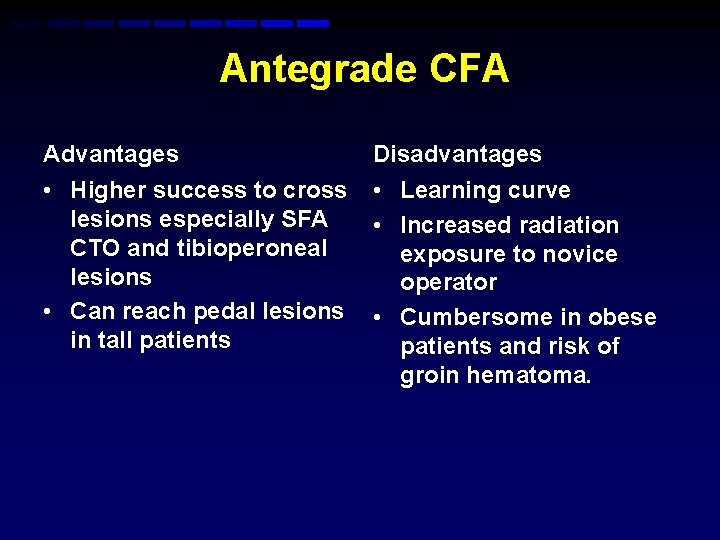
Antegrade CFA Advantages Disadvantages • Higher success to cross lesions especially SFA CTO and tibioperoneal lesions • Can reach pedal lesions in tall patients • Learning curve • Increased radiation exposure to novice operator • Cumbersome in obese patients and risk of groin hematoma.
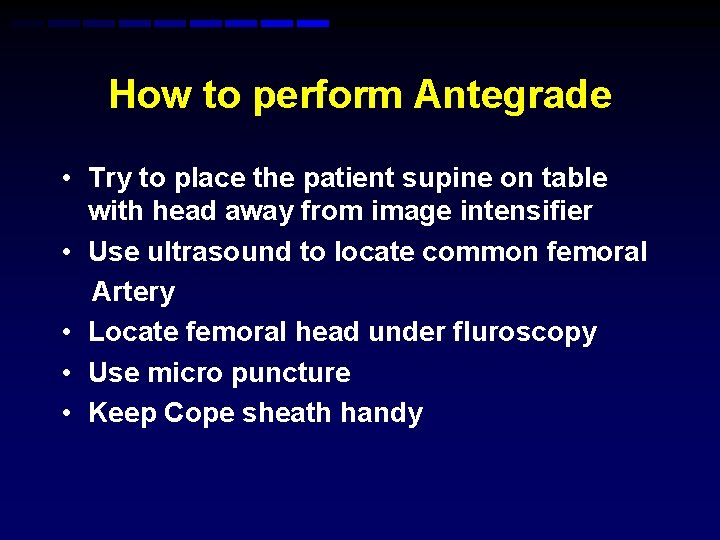
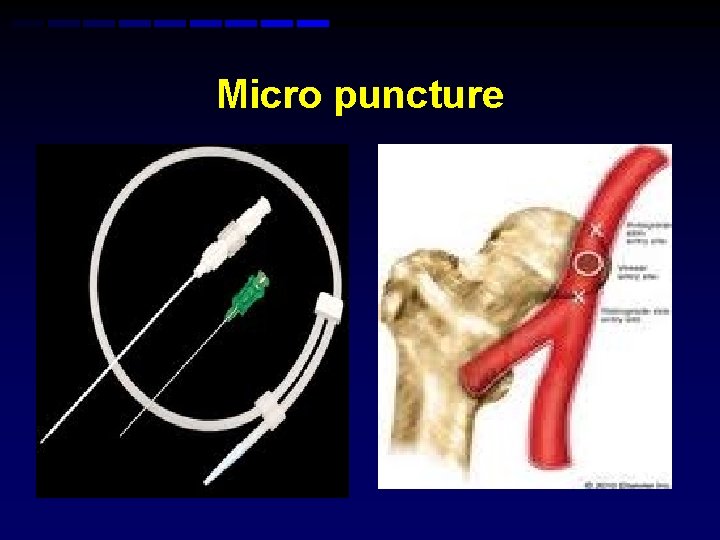
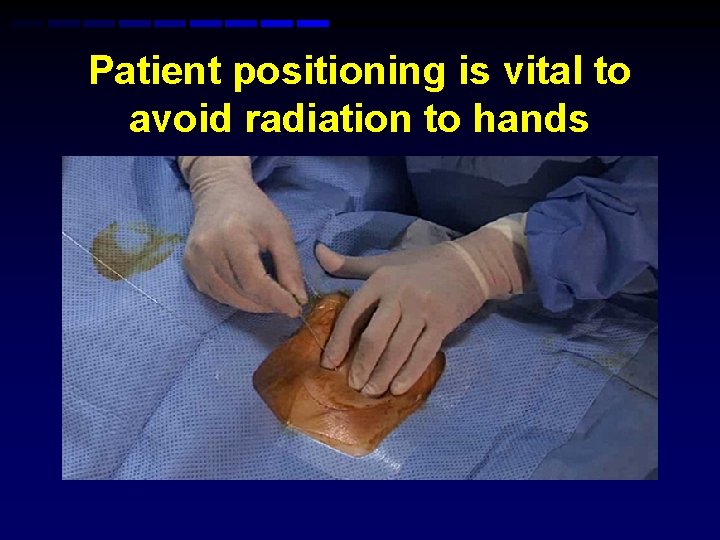
How to perform Antegrade • Try to place the patient supine on table with head away from image intensifier • Use ultrasound to locate common femoral Artery • Locate femoral head under fluroscopy • Use micro puncture • Keep Cope sheath handy
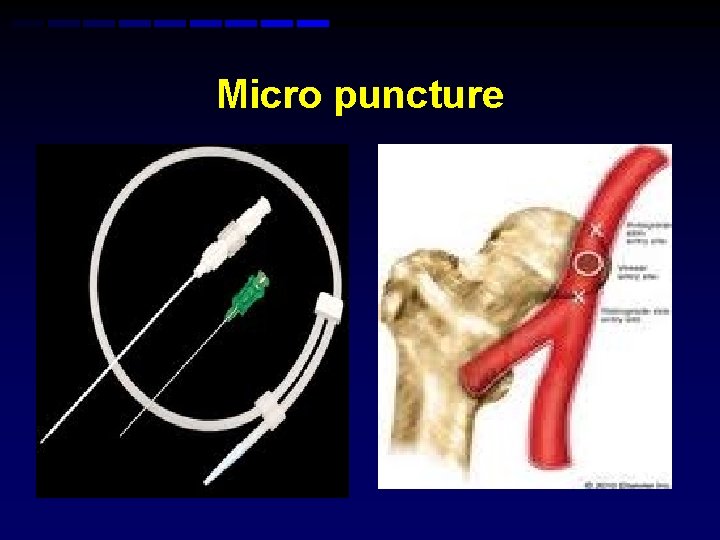
Micro puncture
Patient positioning is vital to avoid radiation to hands
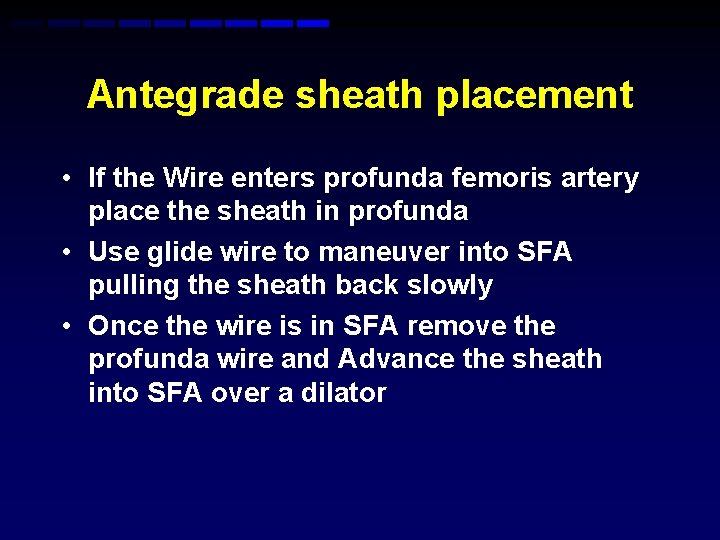
Antegrade sheath placement • If the Wire enters profunda femoris artery place the sheath in profunda • Use glide wire to maneuver into SFA pulling the sheath back slowly • Once the wire is in SFA remove the profunda wire and Advance the sheath into SFA over a dilator
Reality for ante grade puncture
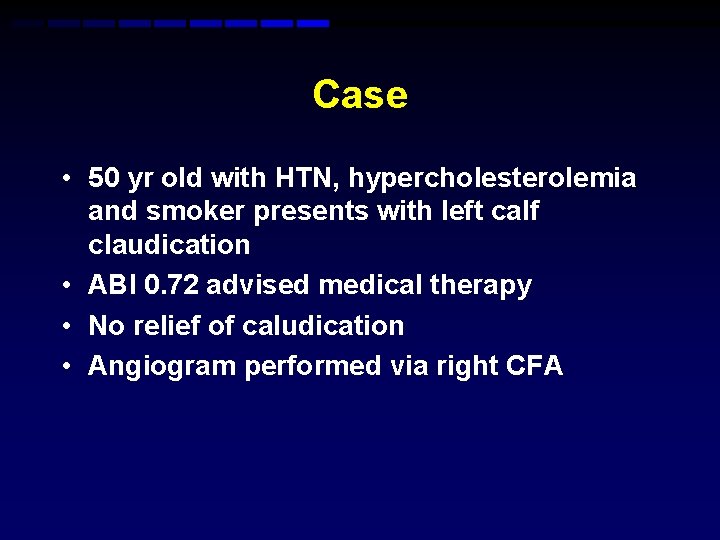
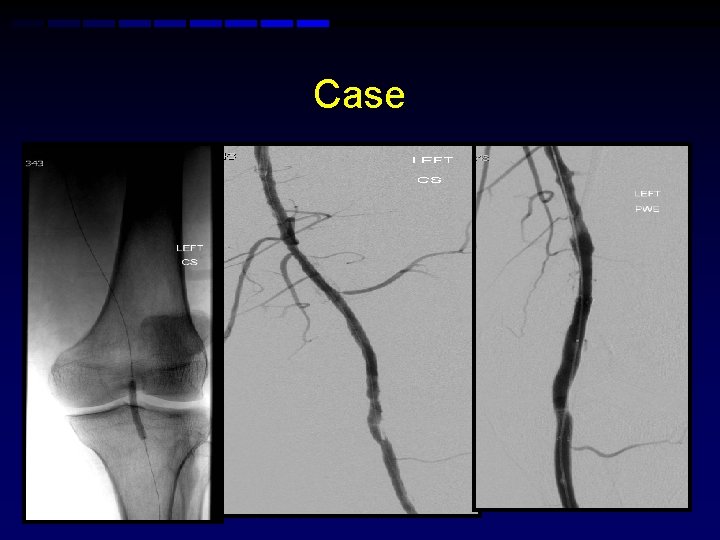
Case • 50 yr old with HTN, hypercholesterolemia and smoker presents with left calf claudication • ABI 0. 72 advised medical therapy • No relief of caludication • Angiogram performed via right CFA
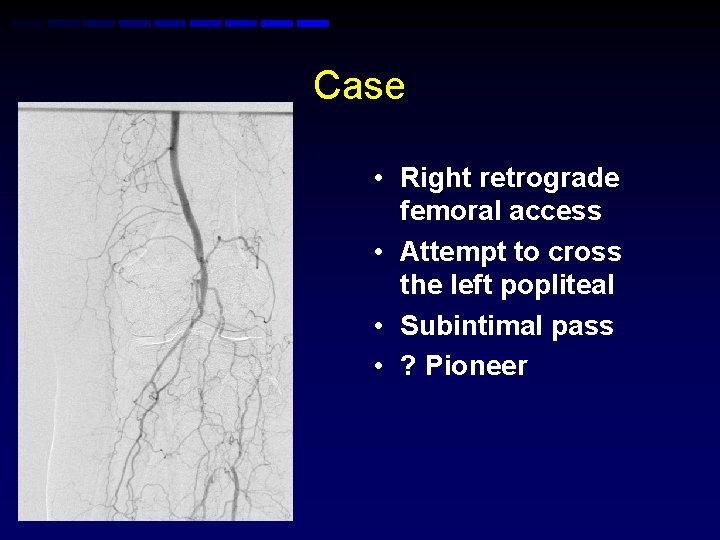
Case • Right retrograde femoral access • Attempt to cross the left popliteal • Subintimal pass • ? Pioneer
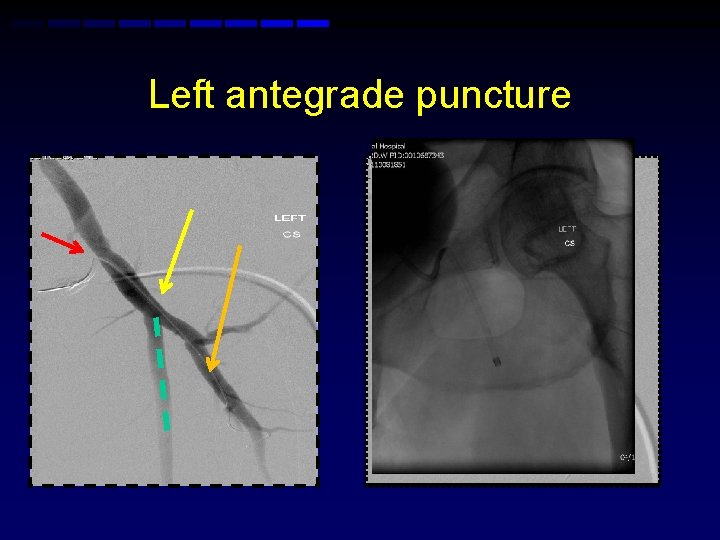
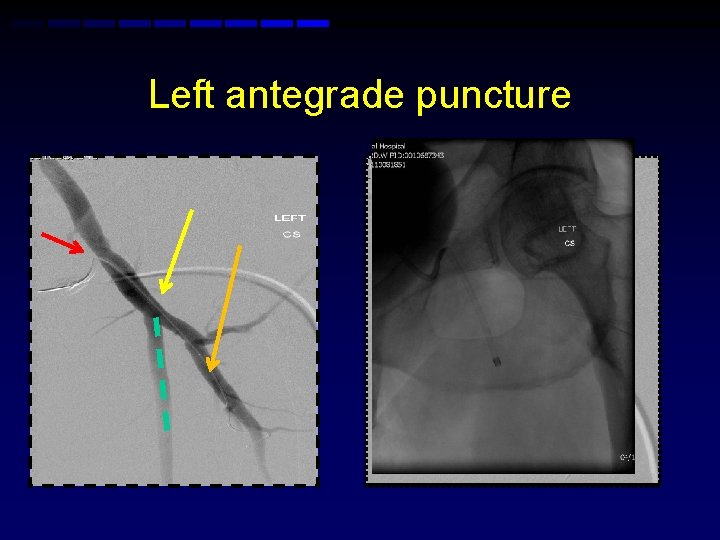
Left antegrade puncture
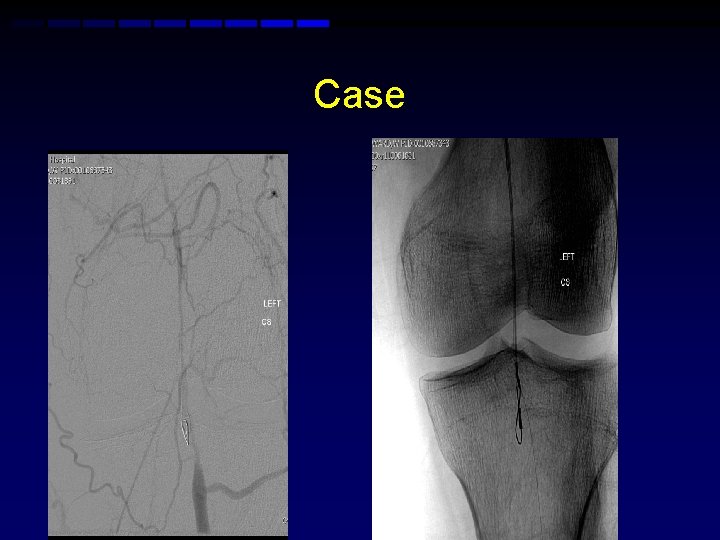
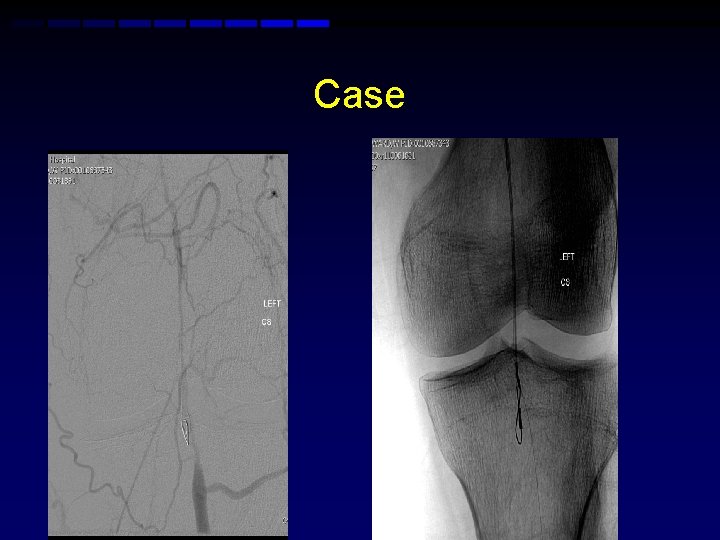
Case
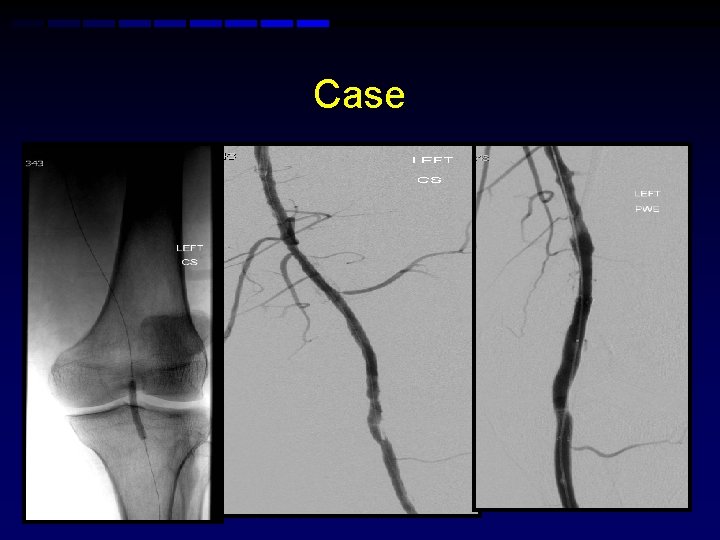
Case
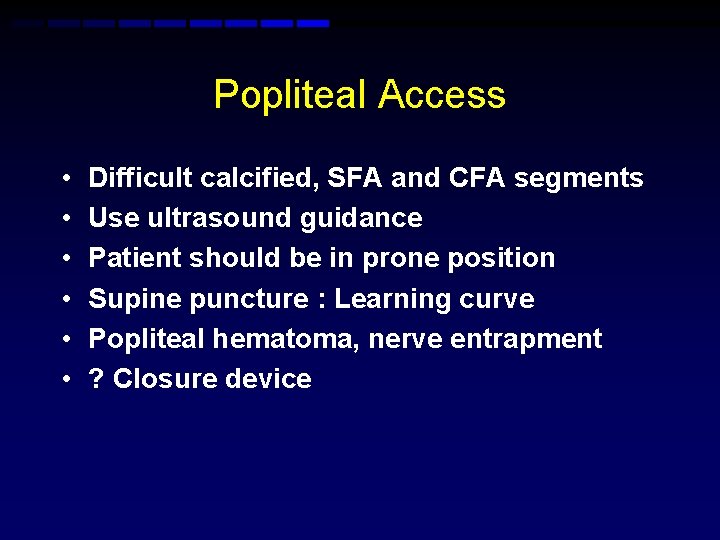
Popliteal Access • • • Difficult calcified, SFA and CFA segments Use ultrasound guidance Patient should be in prone position Supine puncture : Learning curve Popliteal hematoma, nerve entrapment ? Closure device
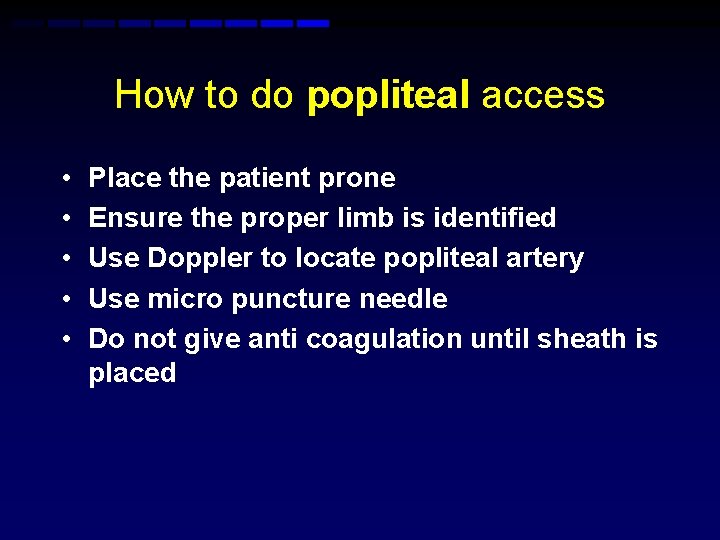
How to do popliteal access • • • Place the patient prone Ensure the proper limb is identified Use Doppler to locate popliteal artery Use micro puncture needle Do not give anti coagulation until sheath is placed
Steps for popliteal access
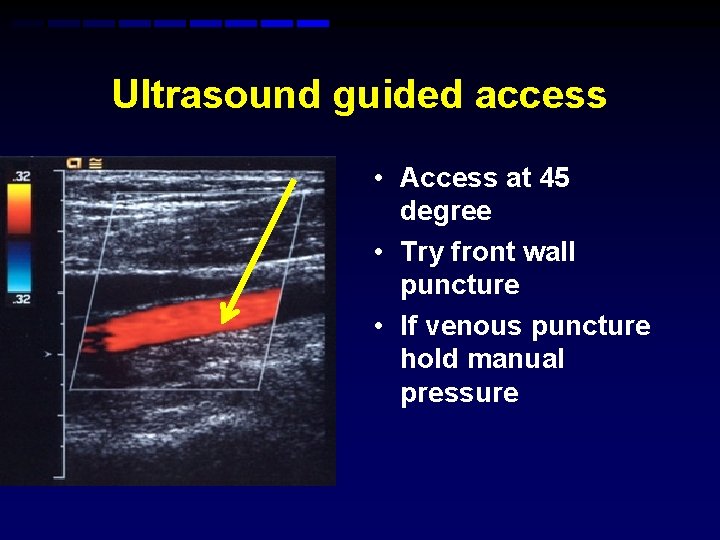
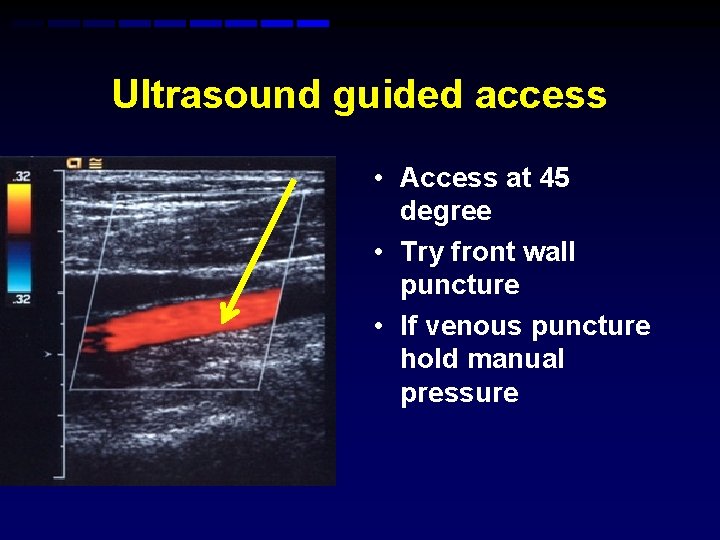
Ultrasound guided access • Access at 45 degree • Try front wall puncture • If venous puncture hold manual pressure
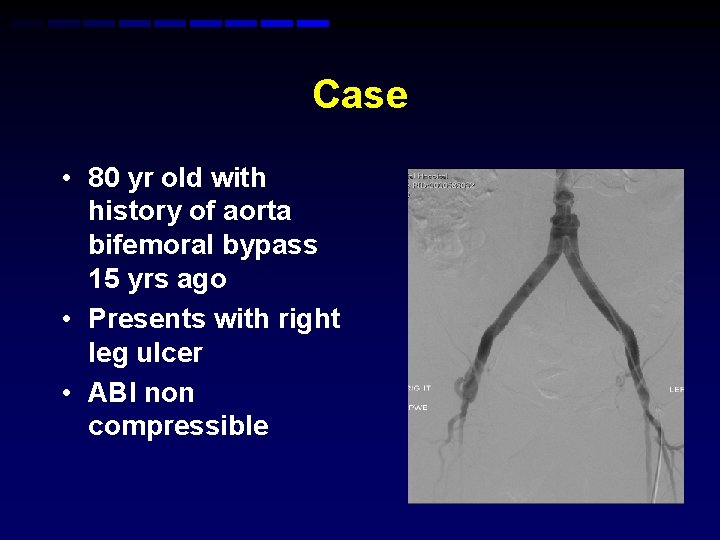
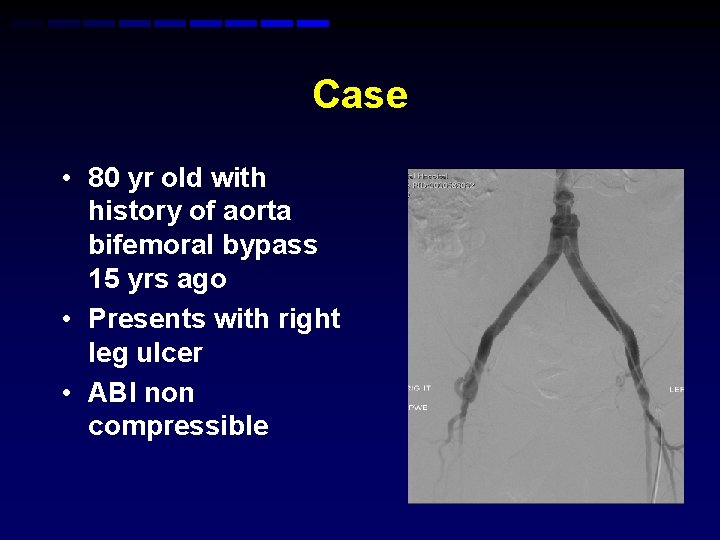
Case • 80 yr old with history of aorta bifemoral bypass 15 yrs ago • Presents with right leg ulcer • ABI non compressible

SFA occluded mid segment and reconstitutes distal
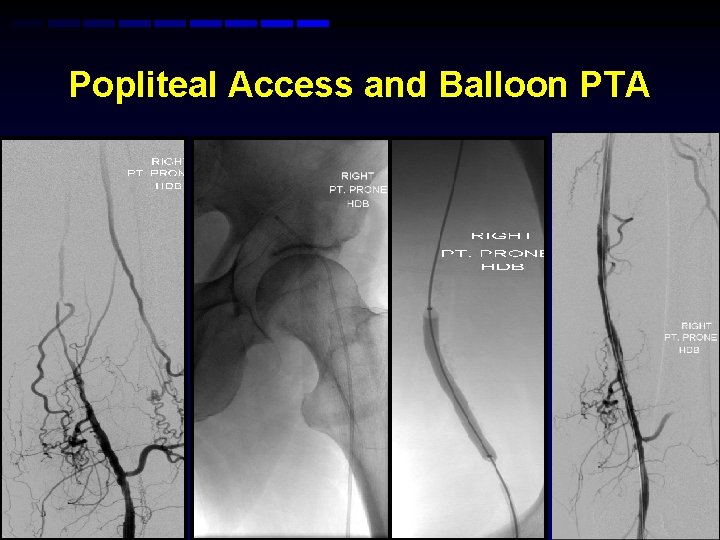
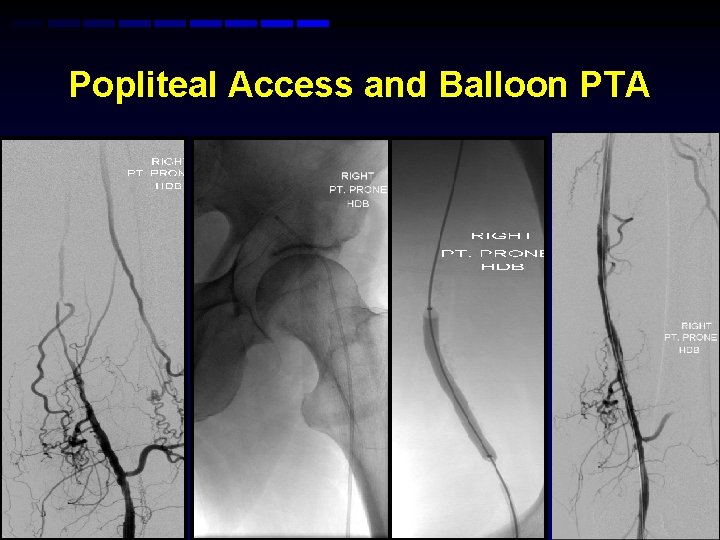
Popliteal Access and Balloon PTA
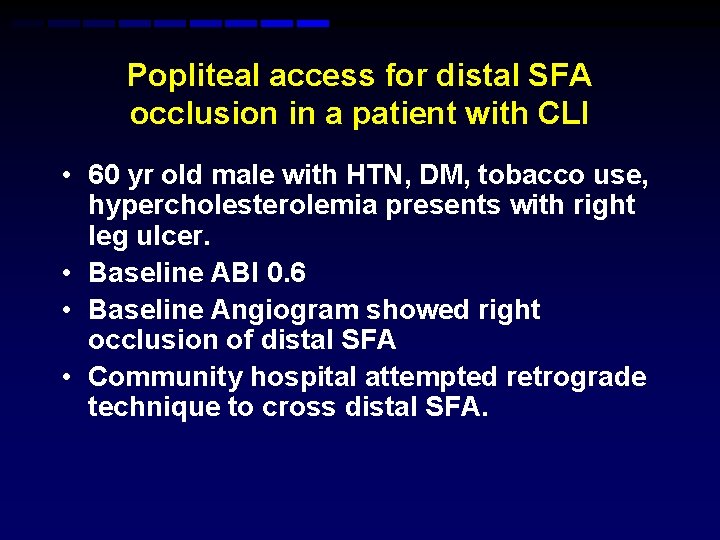
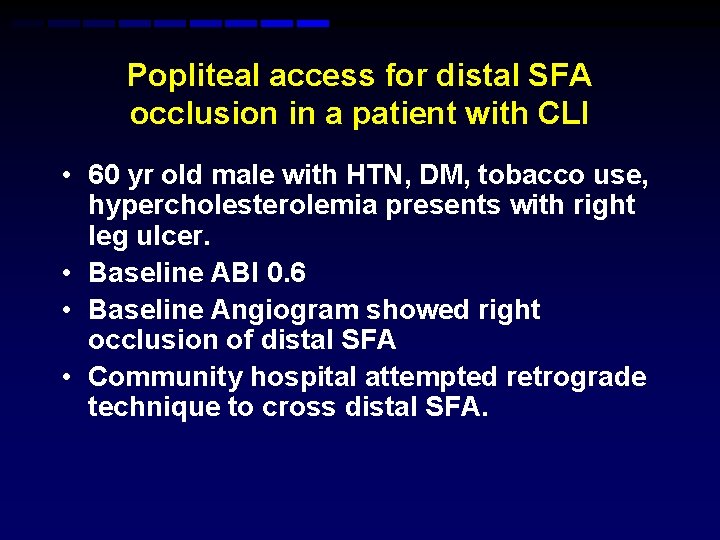
Popliteal access for distal SFA occlusion in a patient with CLI • 60 yr old male with HTN, DM, tobacco use, hypercholesterolemia presents with right leg ulcer. • Baseline ABI 0. 6 • Baseline Angiogram showed right occlusion of distal SFA • Community hospital attempted retrograde technique to cross distal SFA.
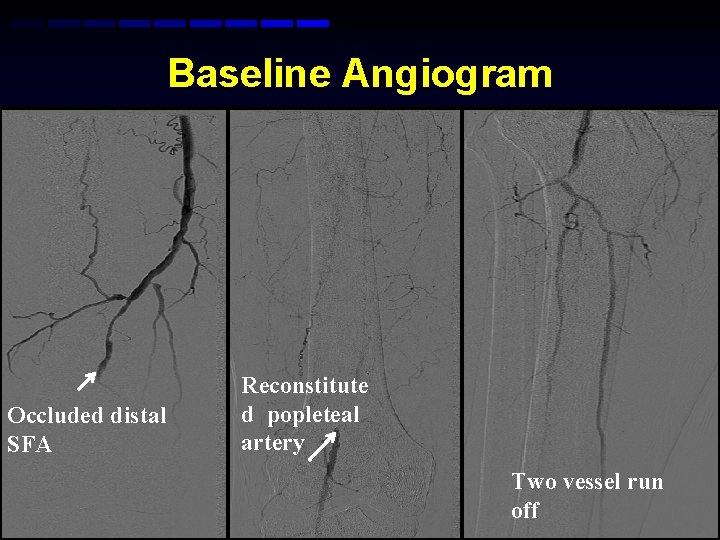
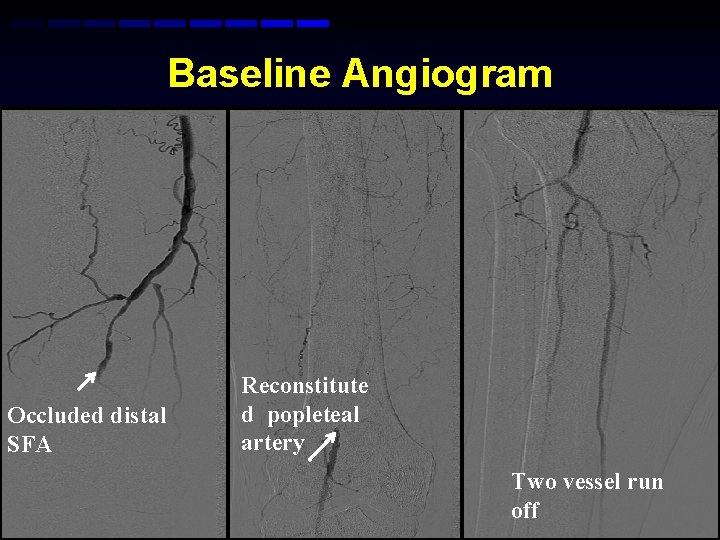
Baseline Angiogram Occluded distal SFA Reconstitute d popleteal artery Two vessel run off
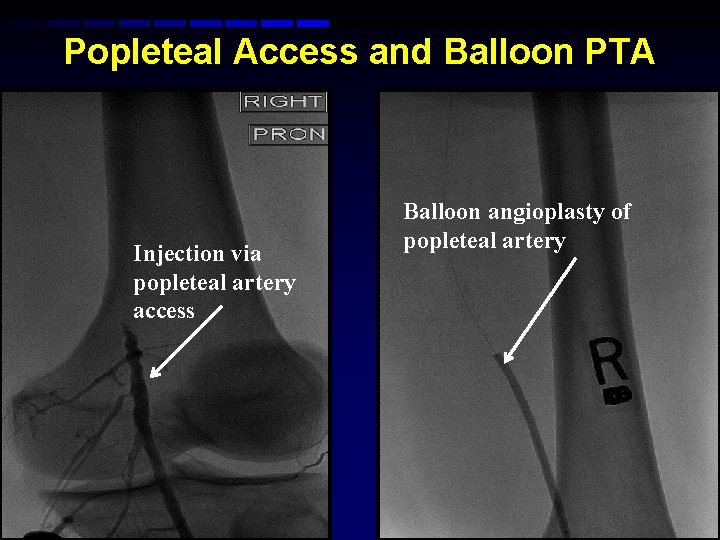
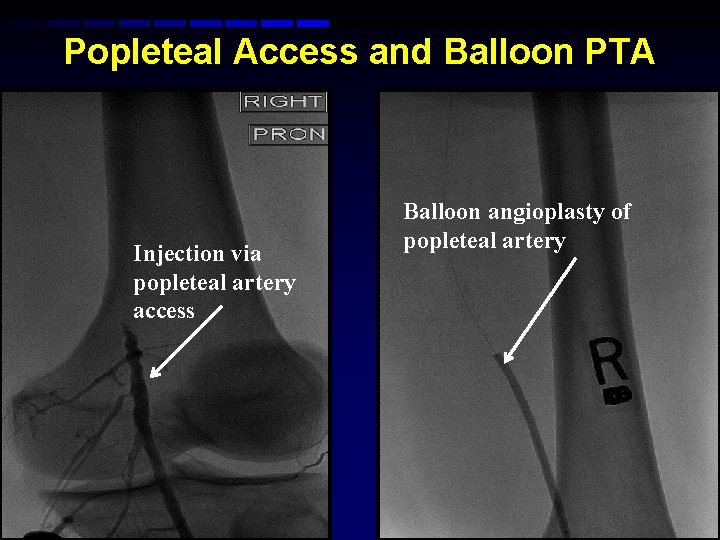
Popleteal Access and Balloon PTA Injection via popleteal artery access Balloon angioplasty of popleteal artery
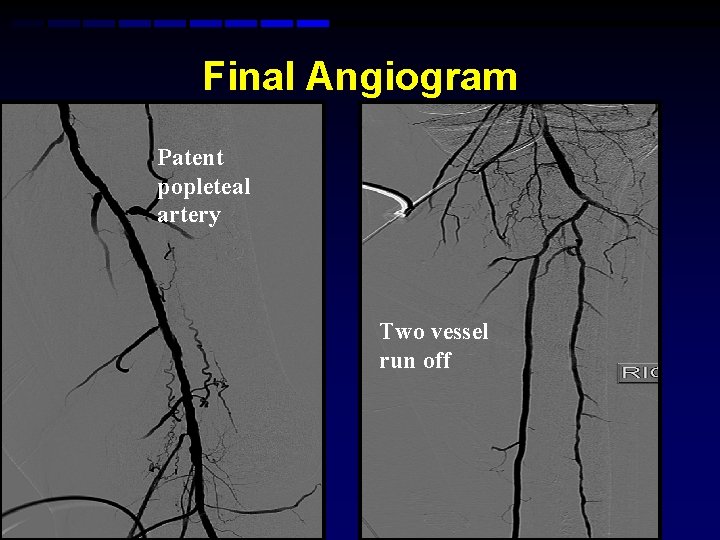
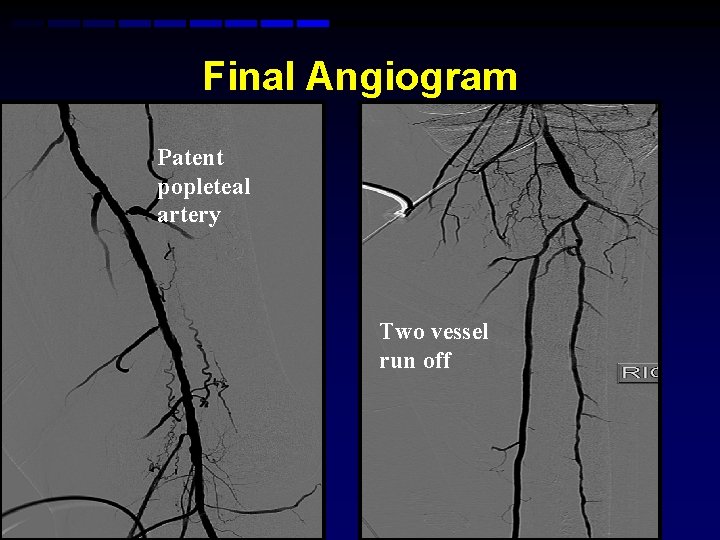
Final Angiogram Patent popleteal artery Two vessel run off
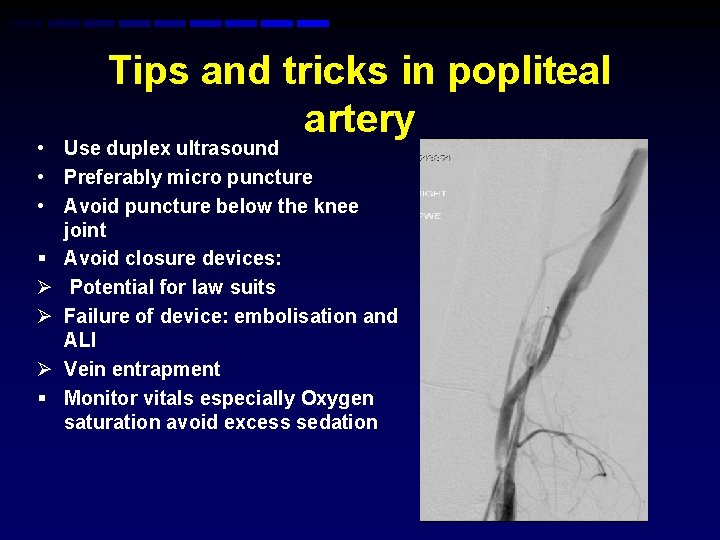
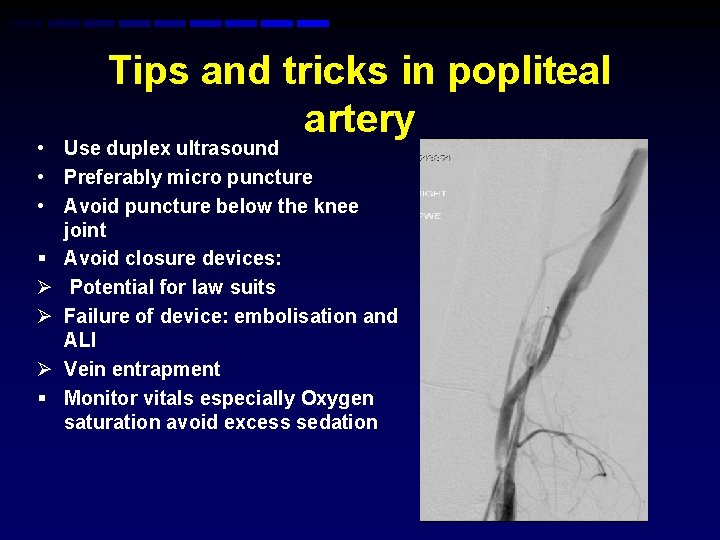
Tips and tricks in popliteal artery • Use duplex ultrasound • Preferably micro puncture • Avoid puncture below the knee joint § Avoid closure devices: Ø Potential for law suits Ø Failure of device: embolisation and ALI Ø Vein entrapment § Monitor vitals especially Oxygen saturation avoid excess sedation
Conclusion • Access is the key to a successful intervention • Choose your access carefully start with retrograde CFA, brachial, antegrade, popleteal and Pedal • Know your anatomy • Keep a alternative back up plan for additional access • Use of ultrasound to locate artery and micro puncture are essential