ANNUAL HEALTH CHECK FOR PEOPLE WITH LEARNING DISABILITY
ANNUAL HEALTH CHECK FOR PEOPLE WITH LEARNING DISABILITY Tower Hamlets Community Learning Disability Service

INTRODUCTION

What is your experience of working with people with intellectual disability? What issues have you faced?

Learning outcomes • • Promoting Access to Health Optimising Communication Effective working with families and carers Services for people with intellectual disability – and what you might ask from them

CEG TH LD DES Activity Dr A Jabin

LD patients aged 18 Y and over 116 168 121 104 122 113 171 86 1, 001 LD Health Check done 26 12 6 10 18 5 36 23 136 LD Health Check done but Health Action Plan neither done nor declined 3 1 0 1 1 0 8 1 15

LD Health Checks Uptake Incentive • In 2017/18 GP practices will be entitled to a quarterly health check completion payment of £ 140. 00 for each patient aged 14 or over in the financial year on the practices agreed learning disabilities register who received a compliant health check in that quarter. Only one payment may be made as regards to any patient in any one financial year. • There is also further £ 37, 500 CQUIN pot of money available for practices to share for any further work in improving this service or for any training when we hit the target of 75% as borough. • These funds are available for GPCG to reinvest in services to support practices to fund activities such as the flu clinics in Hubs we are planning for this year. • These funds would not come directly to practices but are held in a shared pot and is really important not to let our THT partners as more funding will be at stake in the future.
The CEG Template The CEG Learning Disability Health Check clinical template is available for GP Practices through EMIS. The template offers GPs a systematic approach to the health Check which is code based drawing on the existing patient record. This means that the structure of the template can adjust according to the individual patient.

COMMUNICATION Lead Speech & Language Therapist & group of Service Users

Effective Communication http: //www. gmc-uk. org/learningdisabilities/35. aspx What do you think are the principles of good communication?


What are the challenges of working with families and carers?

Working with families and support networks • • • Address language barriers Understanding of cultural practice and religious beliefs Role of a person with intellectual disability in the family Hierarchical structures in some cultures Financial impacts Burden of care • http: //www. gmc-uk. org/learningdisabilities/351. aspx
Case Scenarios

Case Scenario 1 - Jay • • • Moved out of the family home about 5 years ago, lives alone Signed off sick for three years, had worked for 20 yrs previously Brittle asthma poorly managed by patient – several inpatient admissions Invertebral disc prolapse – managed with daily analgesics Lack of engagement with services due to poor literacy Forgetful, poor communication What can we do to support this man to improve his quality of life?
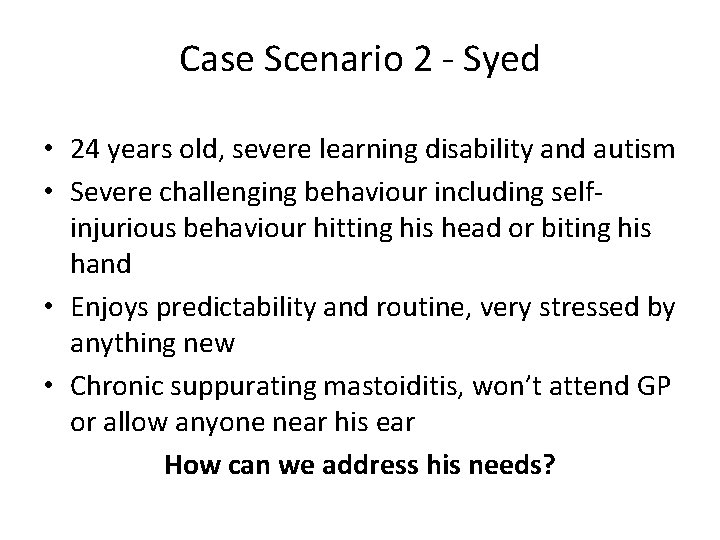
Case Scenario 2 - Syed • 24 years old, severe learning disability and autism • Severe challenging behaviour including selfinjurious behaviour hitting his head or biting his hand • Enjoys predictability and routine, very stressed by anything new • Chronic suppurating mastoiditis, won’t attend GP or allow anyone near his ear How can we address his needs?
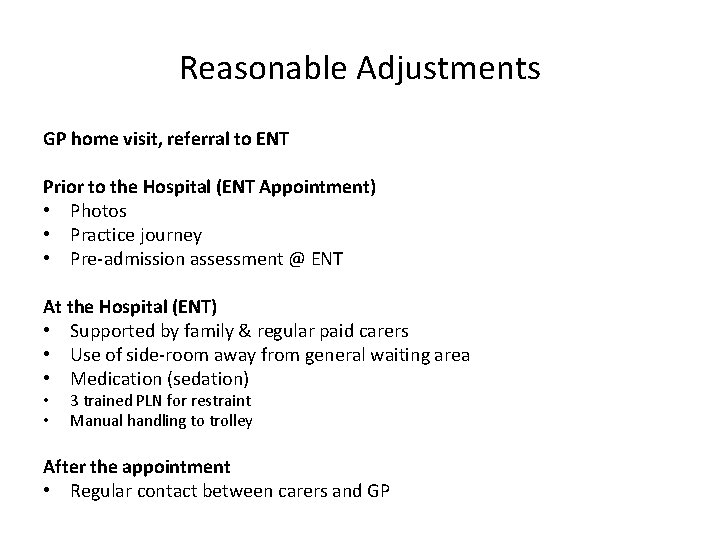
Reasonable Adjustments GP home visit, referral to ENT Prior to the Hospital (ENT Appointment) • Photos • Practice journey • Pre-admission assessment @ ENT At the Hospital (ENT) • Supported by family & regular paid carers • Use of side-room away from general waiting area • Medication (sedation) • • 3 trained PLN for restraint Manual handling to trolley After the appointment • Regular contact between carers and GP
Support Network • • • Families Supported Living and Residential Care Day services; Schools and Colleges Outreach support; Respite Care Employment support Primary care Mental Health services Acute Hospitals Community LD teams

Community learning disabilities services Multi-Disciplinary Team - Social Workers - Speech and Language Therapists - Occupational Therapists - Physiotherapists - Psychologists and Behavioural Therapists - Community Learning Disability Nurses - Psychiatrists Working partnerships: - Families/ Carers - GPs - Mainstream mental health services/crisis teams - Voluntary sectors including respite/day services - Dental/ Hospital specialists/ Liaison
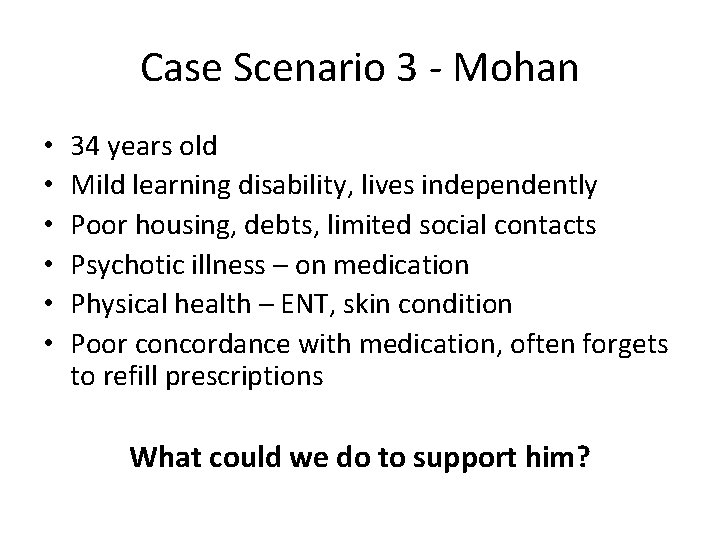
Case Scenario 3 - Mohan • • • 34 years old Mild learning disability, lives independently Poor housing, debts, limited social contacts Psychotic illness – on medication Physical health – ENT, skin condition Poor concordance with medication, often forgets to refill prescriptions What could we do to support him?

Diagnostic Overshadowing Symptoms of mental illness and physical illness may be mistakenly attributed to the learning disability
Access to Health • • Annual Health checks Health Action Plans Health facilitation Primary care liaison nurse Reasonable adjustments Assessment Delivering interventions
Maximising the health of people with intellectual disability • • • Poor access to Health has caused severe problems Reasonable adjustments Maximising communication Diagnostic overshadowing Plenty of specialist support is available – be sure to ask
Resources MENCAP – Don’t miss out https: //youtu. be/z 8407 Uzys 3 E RCGP guide (2010) http: //www. rcgp. org. uk/learningdisabilities/ Electronic clinical template https: //www. england. nhs. uk/publication/a-summary-andoverview-of-the-learning-disability-annual-health-checkelectronic-clinical-template-2017/ www. easyhealth. org. uk – lots of ‘easy read’ information
Desensitisation Having a blood test

Case Patient – Female 23 yrs of age Bengali Diagnosis: - Mild LD, Atypical Autism, Psychotic Illness Referred By Psychiatry to Nursing as GP requesting support for blood test. Required monitoring due to metabolic side effects of antipsychotic medication. Last bloods 2009. GP had made several attempts without success as patient refused.
Steps Met with Patient in familiar environment. Talk about blood test, did she know what a blood test was, had she had a blood test before, why she did not like blood tests, why blood tests were important. Use pictures of blood test to talk about the process. Agree for her to try to give blood. Appt made – refused. Plan made with staff member at GP surgery. EMLA cream prescription, tourniquet, no needle butterfly clip. Agreed to meet with patient a number of times at day centre to use equipment and to take photographs of her engagement in the process. Slight pressure applied when placing butterfly clip. Her to practice on me. Further appointment made in agreement with patient. Make patient a booklet.






Appointment Day Despite all – patient still refused. Gave blood in front of patient – still refused. While giving blood, patient stating “no don, t do it” and became anxious. Once completed, patient began praising me telling me I was “really brave”. Patient still refused. Outcome – clear that we were not going to be successful now, so urine sample collected in order for glucosuria to be measured. Psychiatry and Nursing monitoring MH and Day Centre monitoring weight and general well being. Further discussion – deep rooted fear, how best to support patient, what would help?
Now and Tomorrow Now – CLDS able to work with dental team for bloods to be taken under GA (two birds one stone). Sedation for patients who present with challenging behaviours. Lengthy desensitising work Tomorrow – example. Wigan & Leigh Trust LD Team have been working closely with Phlebotomy services for the completion of blood tests via the capillary blood collection procedure. Clinic set up for patients with moderate to complex LD, and who had fears associated with blood collection. Small lancet used to make small incision in side of finger and then squeezing the finger to obtain small samples via tubes or a collector device. Considered low impact invasive procedure and low risk of injury. Still requires a desensitising programme: Trips to clinic, accessible information, increased exposure to clinic and equipment, squeezing of finger. Would this method make home blood taking easier? Patients are unique and we should be trying to work out what works for the person. As clinicians we need to consider what we can test for from capillary testing alone. If a blood test can be completed – would it be useful to test for as much as possible especially for non verbal patients who cannot tell you what is wrong. ?
Maximising the health of people with intellectual disability • • • Poor access to Health has caused severe problems Reasonable adjustments Maximising communication Diagnostic overshadowing Plenty of specialist support is available – be sure to ask
- Slides: 36