Ankle Joint Type Hinge synovial surface Articular surfaces














- Slides: 48
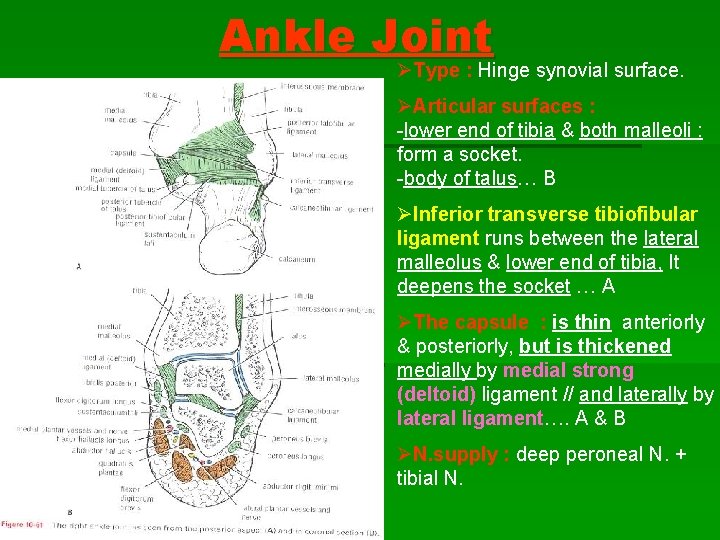
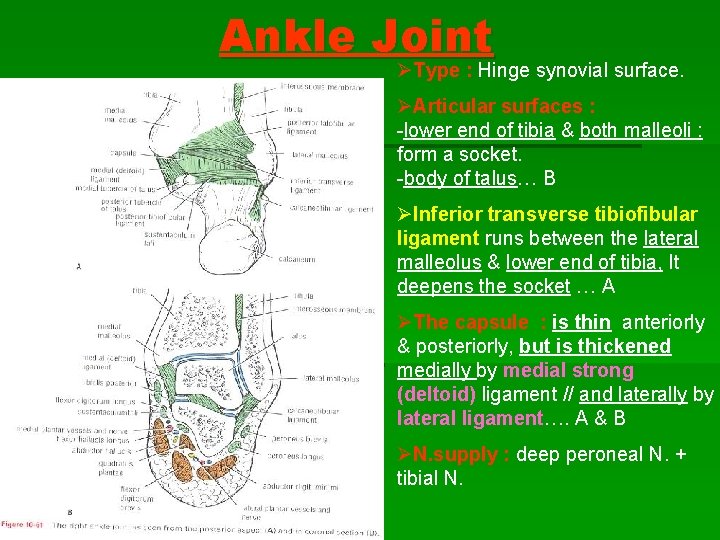
Ankle Joint ØType : Hinge synovial surface. ØArticular surfaces : -lower end of tibia & both malleoli : form a socket. -body of talus… B ØInferior transverse tibiofibular ligament runs between the lateral malleolus & lower end of tibia, It deepens the socket … A ØThe capsule : is thin anteriorly & posteriorly, but is thickened medially by medial strong (deltoid) ligament // and laterally by lateral ligament…. A & B ØN. supply : deep peroneal N. + tibial N.
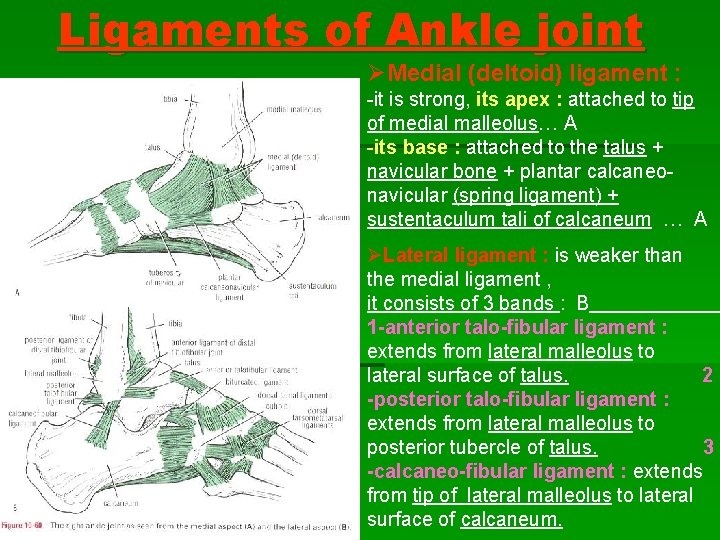
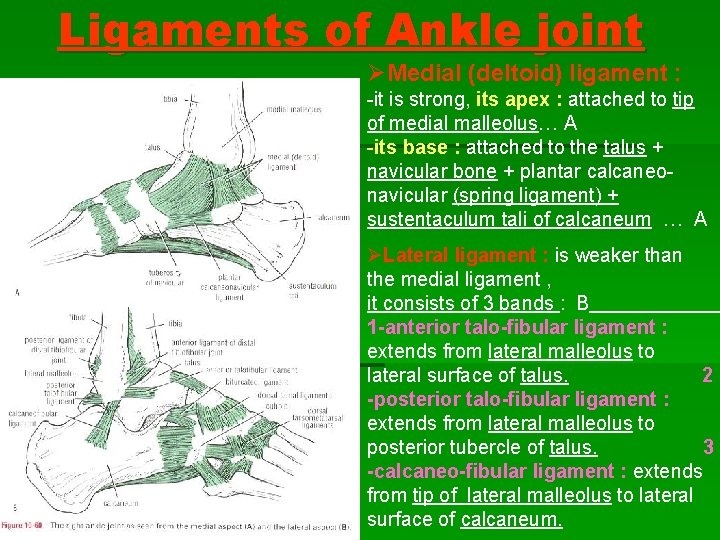
Ligaments of Ankle joint ØMedial (deltoid) ligament : -it is strong, its apex : attached to tip of medial malleolus… A -its base : attached to the talus + navicular bone + plantar calcaneonavicular (spring ligament) + sustentaculum tali of calcaneum … A ØLateral ligament : is weaker than the medial ligament , it consists of 3 bands : B 1 -anterior talo-fibular ligament : extends from lateral malleolus to lateral surface of talus. 2 -posterior talo-fibular ligament : extends from lateral malleolus to posterior tubercle of talus. 3 -calcaneo-fibular ligament : extends from tip of lateral malleolus to lateral surface of calcaneum.

Movements of Ankle joint § Dorsiflexion & plantar flexion at ankle joint , but movements of inversion & eversion take place at tarsal joints and not at ankle joint. § Dorsiflexion : is performed by : tibialis anterior, extensor hallucis longus, extensor digitorum longus and peroneus tertius. -It is limited by the tension of tendo-calcaneus, medial ligament (posterior fibres) & lateral lig. (calcaneo-fibular ligament). -During dorsiflexion, the joint is locked and lateral movement is prevented.
Movements of Ankle joint § Plantar flexion : is performed by : gastrocnemius, soleus, plantaris, / peroneus longus & brevis, / tibialis posterior, flexor digitorum longus, and flexor hallucis longus. -It is limited by the tension of the opposing ms. , medial ligament (anterior fibres) & lateral ligament (anterior talo-fibular ligament). -During plantar flexion, the joint is loose and unlocked with possible some lateral movement.
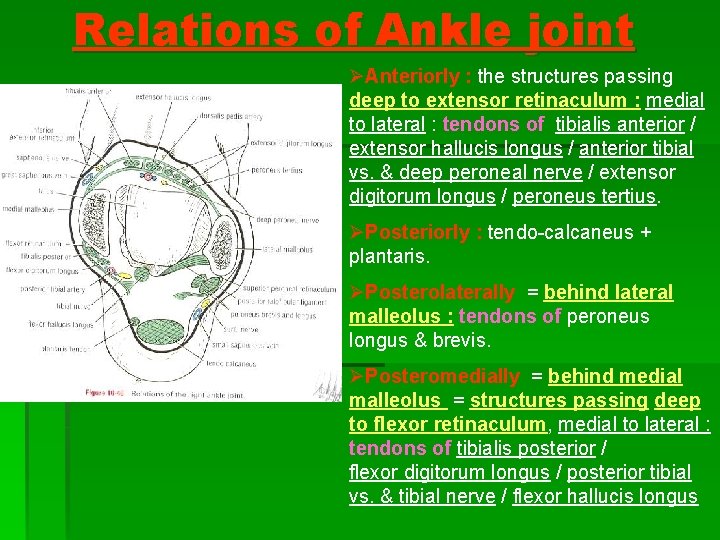
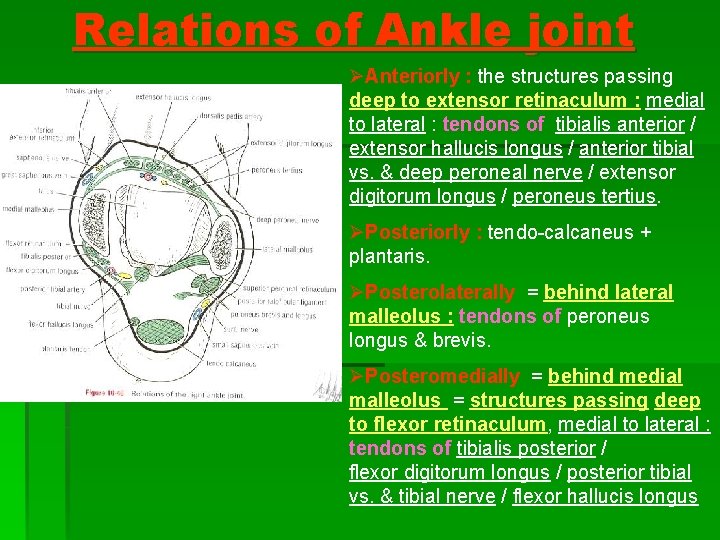
Relations of Ankle joint ØAnteriorly : the structures passing deep to extensor retinaculum : medial to lateral : tendons of tibialis anterior / extensor hallucis longus / anterior tibial vs. & deep peroneal nerve / extensor digitorum longus / peroneus tertius. ØPosteriorly : tendo-calcaneus + plantaris. ØPosterolaterally = behind lateral malleolus : tendons of peroneus longus & brevis. ØPosteromedially = behind medial malleolus = structures passing deep to flexor retinaculum, medial to lateral : tendons of tibialis posterior / flexor digitorum longus / posterior tibial vs. & tibial nerve / flexor hallucis longus
Function of Arches of the Foot : ØThey act as a weight bearing. ØThey act as a locomotive part of the body in walking & running. ØThey provide space in the sole of foot to contain and protect the muscles, nerves and blood vessels of the sole.
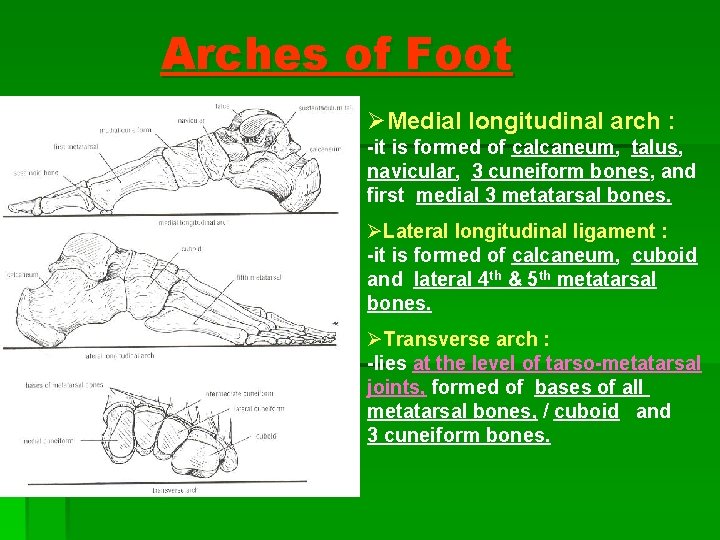
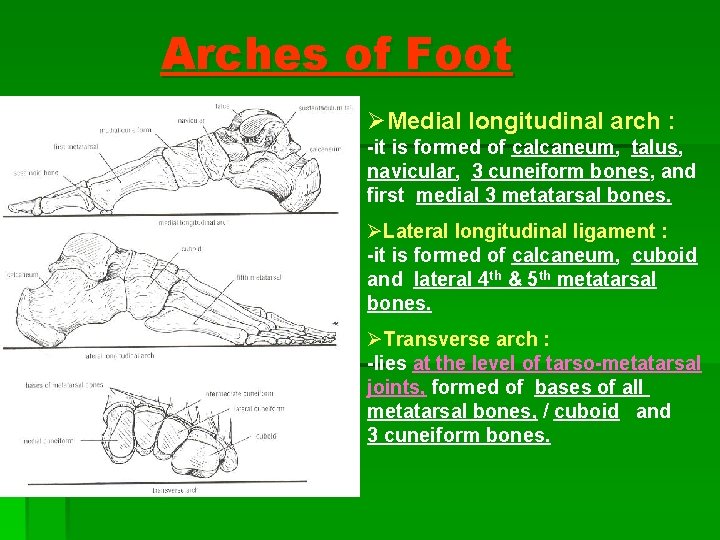
Arches of Foot ØMedial longitudinal arch : -it is formed of calcaneum, talus, navicular, 3 cuneiform bones, and first medial 3 metatarsal bones. ØLateral longitudinal ligament : -it is formed of calcaneum, cuboid and lateral 4 th & 5 th metatarsal bones. ØTransverse arch : -lies at the level of tarso-metatarsal joints, formed of bases of all metatarsal bones, / cuboid and 3 cuneiform bones.
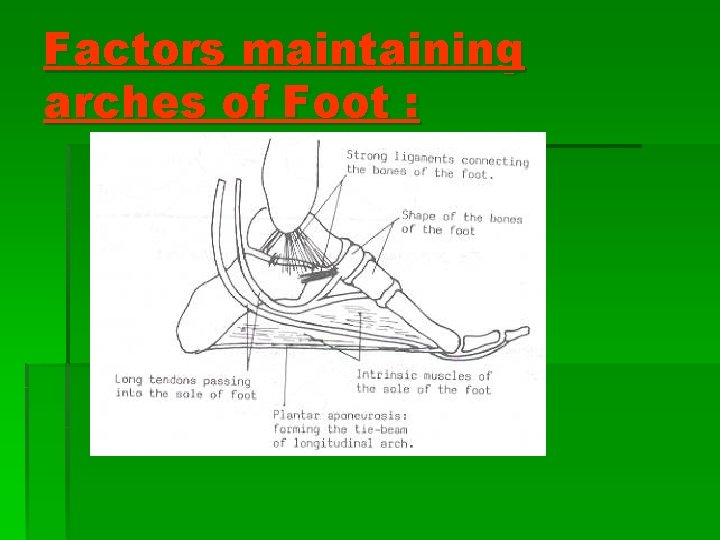
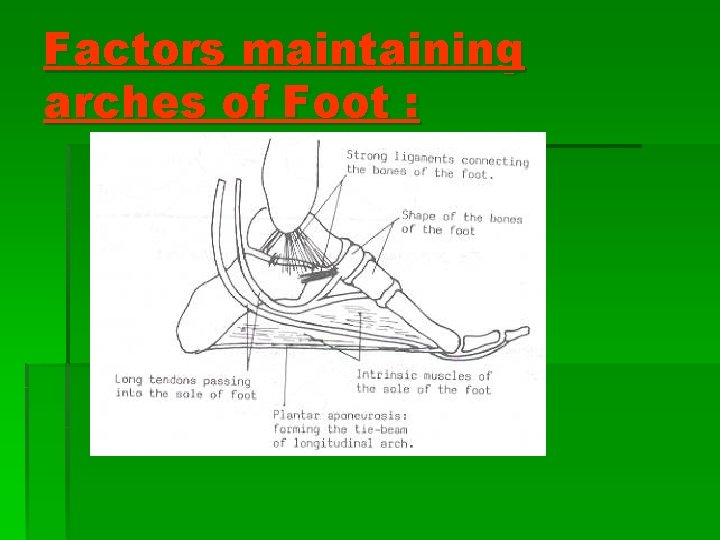
Factors maintaining arches of Foot :
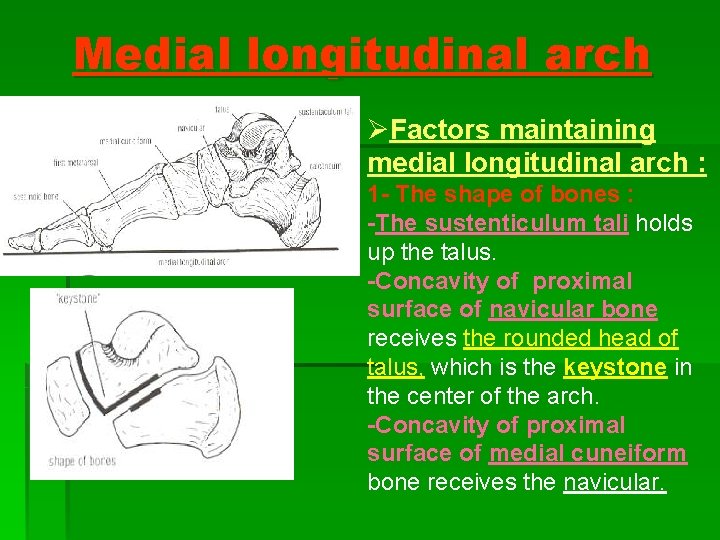
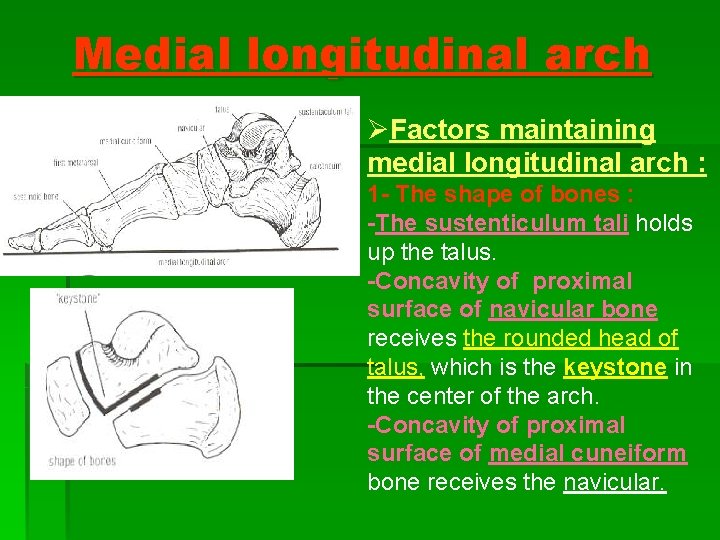
Medial longitudinal arch ØFactors maintaining medial longitudinal arch : 1 - The shape of bones : -The sustenticulum tali holds up the talus. -Concavity of proximal surface of navicular bone receives the rounded head of talus, which is the keystone in the center of the arch. -Concavity of proximal surface of medial cuneiform bone receives the navicular.
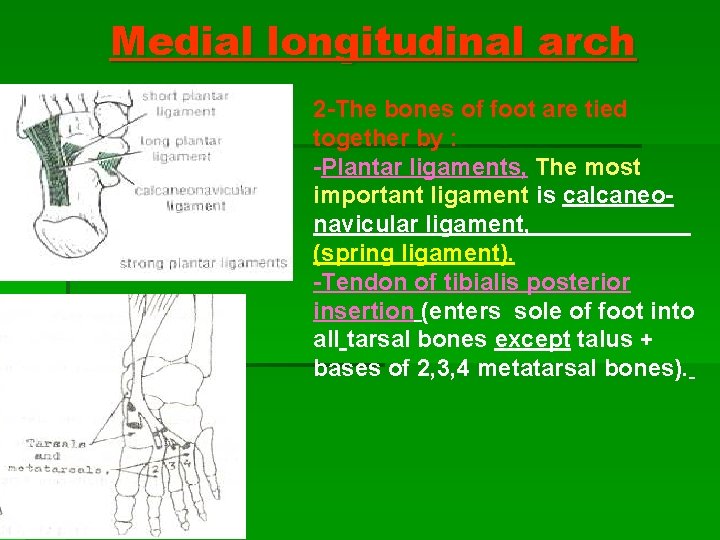
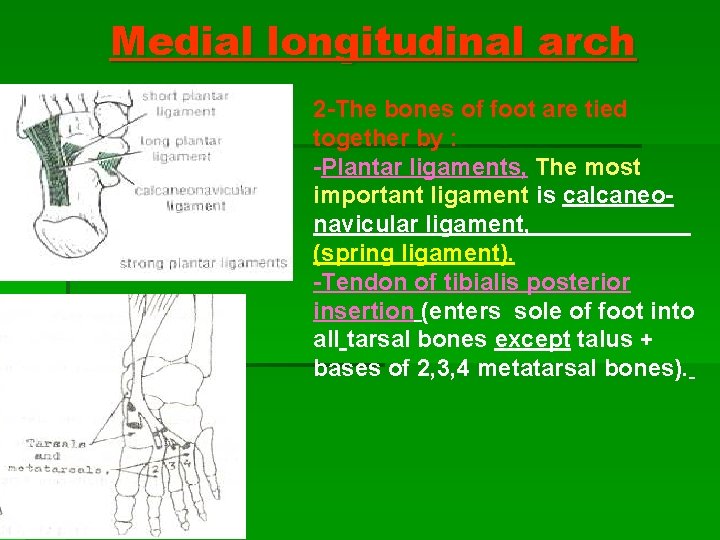
Medial longitudinal arch 2 -The bones of foot are tied together by : -Plantar ligaments, The most important ligament is calcaneonavicular ligament, (spring ligament). -Tendon of tibialis posterior insertion (enters sole of foot into all tarsal bones except talus + bases of 2, 3, 4 metatarsal bones).

Medial longitudinal arch 3 -tying the ends of the arch together by : -Plantar aponeurosis (extends from calcaneum to heads of metatarsal bones) -Medial parts of flexor digitorum longus + flexor digitorum brevis. -Abductor hallucis. -Tendons of Flexor hallucis longus +Flexor hallucis brevis. 4 -Suspending the arch from above by : Tibialis anterior -Tibialis anterior (descends in front of tibia to be inserted into medial sides of medial cuneiform bone + base of 1 st metatarsal bone) + tibialis posterior. -Medial ligament (deltoid lig. ) of ankle joint.

Lateral longitudinal arch ØFactors maintaining lateral longitudinal arch : 1 -shape of bones : minimal shaping of distal end of calcaneum & proximal end of cuboid. The cuboid is the keystone. 2 -The bones are tied together by : -long plantar ligament + short plantar ligament (plantar calcaneo-cuboid) + -short muscles of foot. 3 -Tying the ends of the arch together : by plantar aponeurosis + abductor digiti minimi + lateral part of flexor digitorum longus & brevis. 4 -Suspending the arch from above : peroneus longus & brevis.
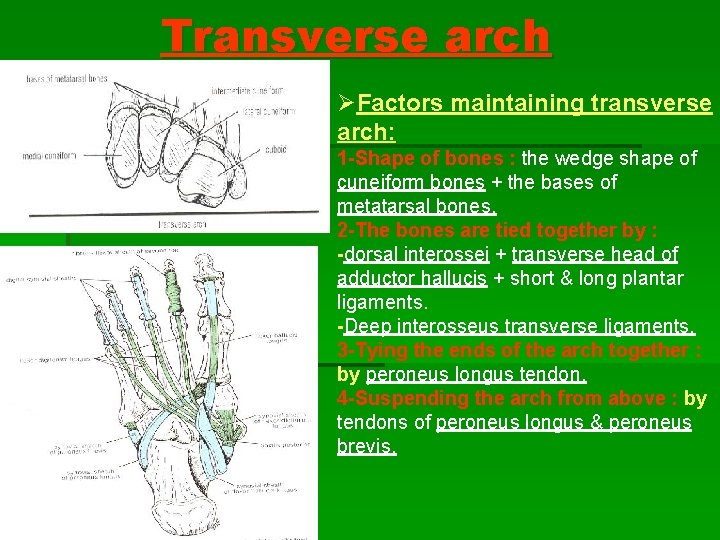
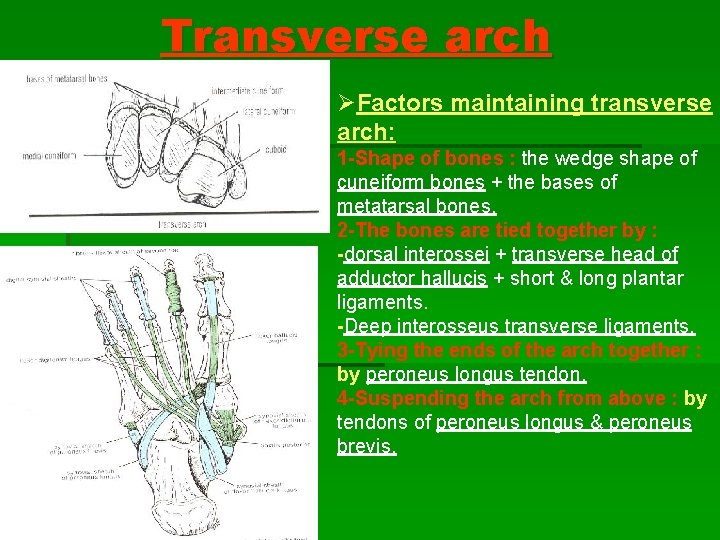
Transverse arch ØFactors maintaining transverse arch: 1 -Shape of bones : the wedge shape of cuneiform bones + the bases of metatarsal bones. 2 -The bones are tied together by : -dorsal interossei + transverse head of adductor hallucis + short & long plantar ligaments. -Deep interosseus transverse ligaments. 3 -Tying the ends of the arch together : by peroneus longus tendon. 4 -Suspending the arch from above : by tendons of peroneus longus & peroneus brevis.
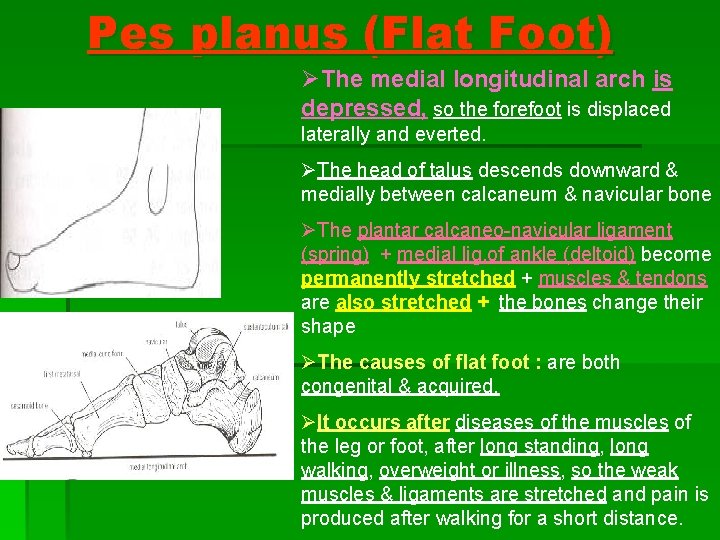
Pes planus (Flat Foot) ØThe medial longitudinal arch is depressed, so the forefoot is displaced laterally and everted. ØThe head of talus descends downward & medially between calcaneum & navicular bone ØThe plantar calcaneo-navicular ligament (spring) + medial lig. of ankle (deltoid) become permanently stretched + muscles & tendons are also stretched + the bones change their shape ØThe causes of flat foot : are both congenital & acquired. ØIt occurs after diseases of the muscles of the leg or foot, after long standing, long walking, overweight or illness, so the weak muscles & ligaments are stretched and pain is produced after walking for a short distance.

Pes Cavus (Clawfoot) ØThe medial longitudinal arch becomes too high. ØIt is produced by muscle imbalance, (shortening of muscles or tendons of leg or sole), in most cases due to poliomyelitis.

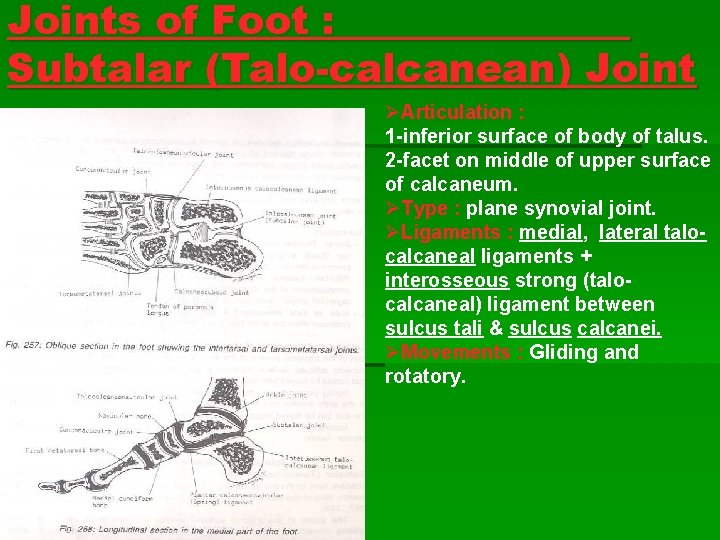
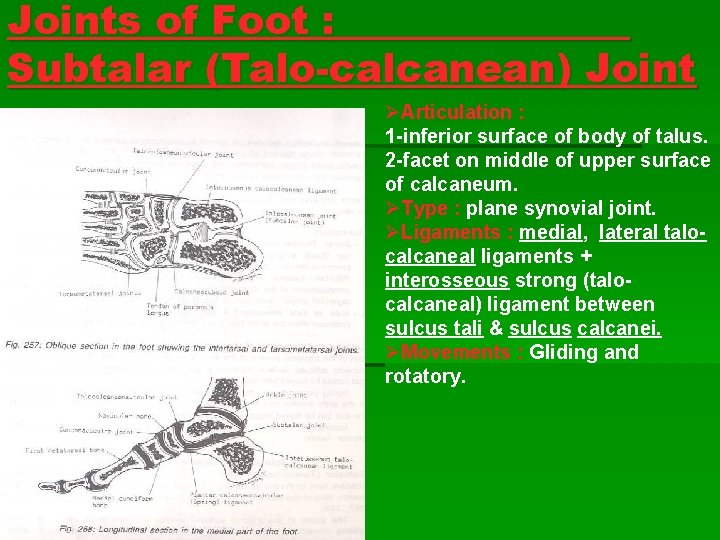
Joints of Foot : Subtalar (Talo-calcanean) Joint ØArticulation : : 1 -inferior surface of body of talus. 2 -facet on middle of upper surface of calcaneum. ØType : plane synovial joint. ØLigaments : medial, lateral talocalcaneal ligaments + interosseous strong (talocalcaneal) ligament between sulcus tali & sulcus calcanei. ØMovements : Gliding and rotatory.
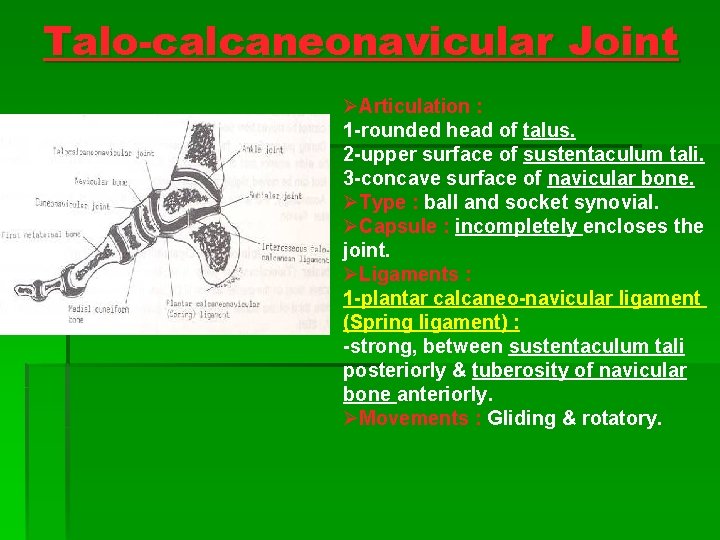
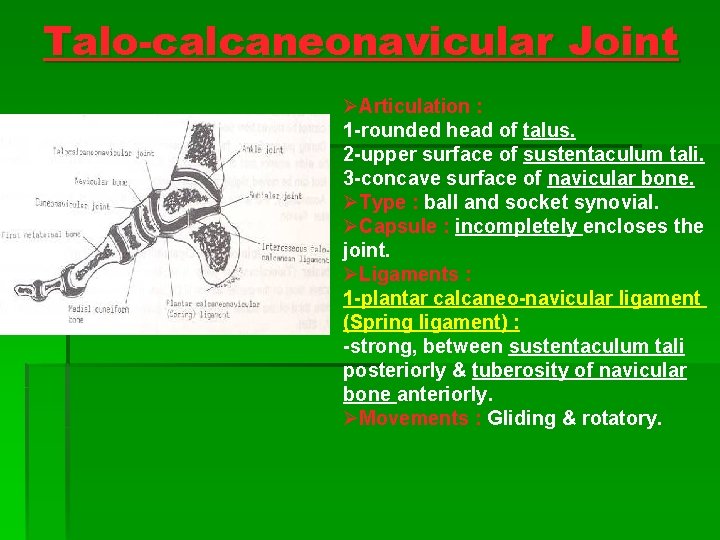
Talo-calcaneonavicular Joint ØArticulation : 1 -rounded head of talus. 2 -upper surface of sustentaculum tali. 3 -concave surface of navicular bone. ØType : ball and socket synovial. ØCapsule : incompletely encloses the joint. ØLigaments : 1 -plantar calcaneo-navicular ligament (Spring ligament) : -strong, between sustentaculum tali posteriorly & tuberosity of navicular bone anteriorly. ØMovements : Gliding & rotatory.
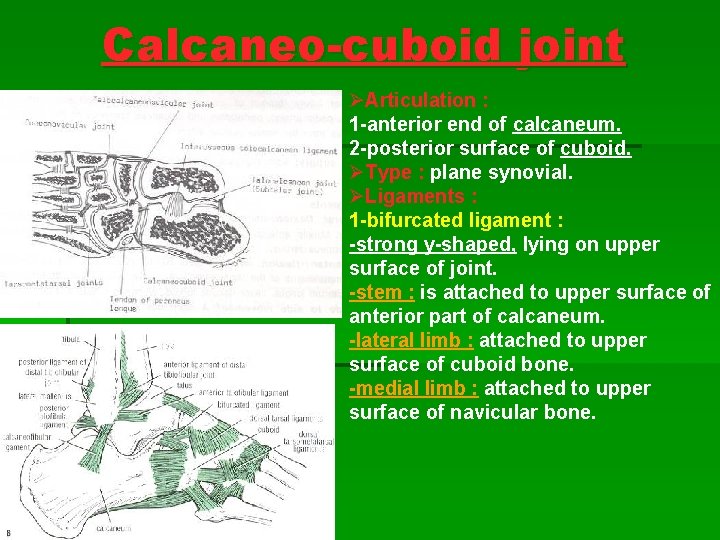
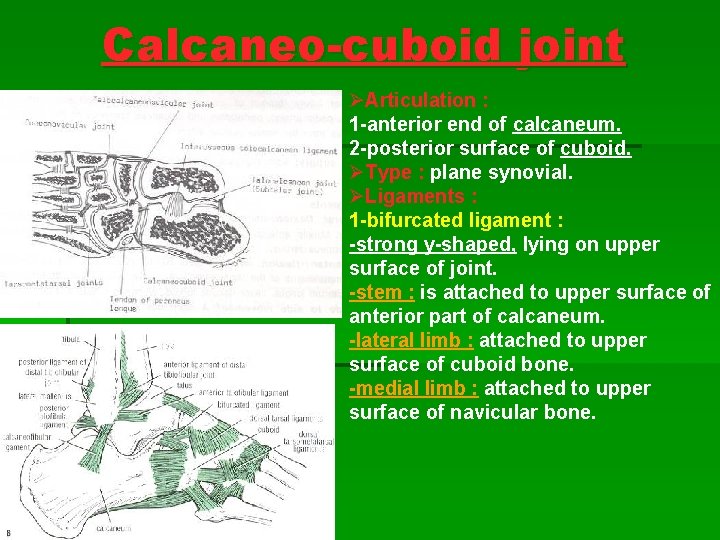
Calcaneo-cuboid joint ØArticulation : 1 -anterior end of calcaneum. 2 -posterior surface of cuboid. ØType : plane synovial. ØLigaments : 1 -bifurcated ligament : -strong y-shaped, lying on upper surface of joint. -stem : is attached to upper surface of anterior part of calcaneum. -lateral limb : attached to upper surface of cuboid bone. -medial limb : attached to upper surface of navicular bone.
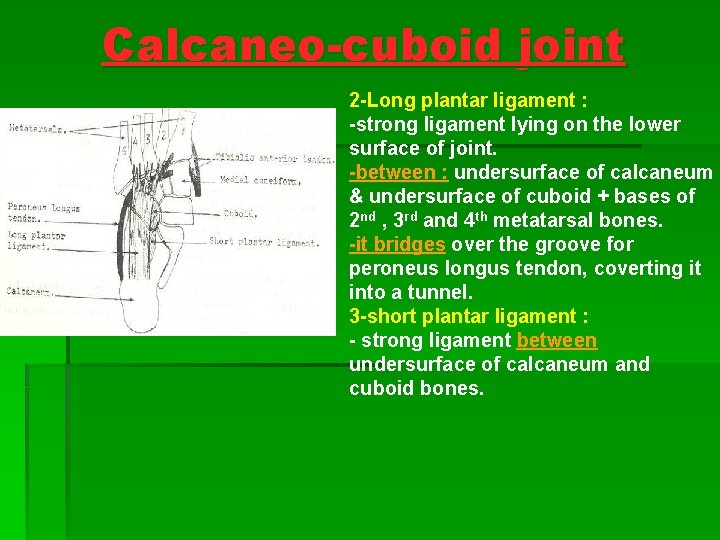
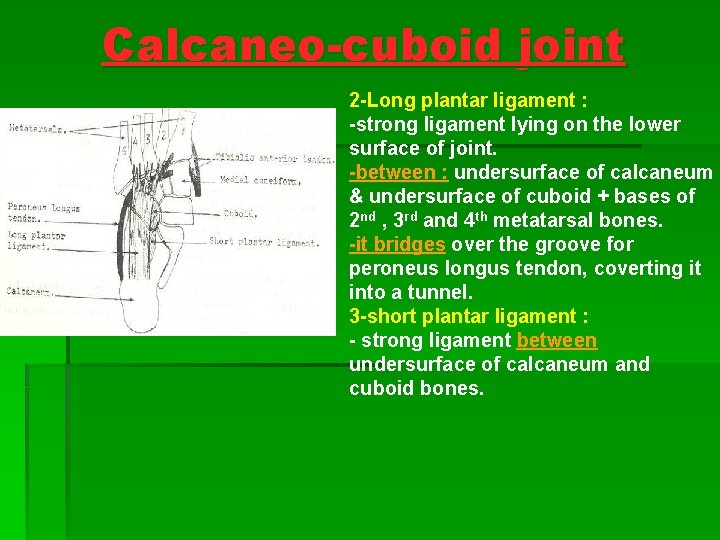
Calcaneo-cuboid joint 2 -Long plantar ligament : -strong ligament lying on the lower surface of joint. -between : undersurface of calcaneum & undersurface of cuboid + bases of 2 nd , 3 rd and 4 th metatarsal bones. -it bridges over the groove for peroneus longus tendon, coverting it into a tunnel. 3 -short plantar ligament : - strong ligament between undersurface of calcaneum and cuboid bones.

Movements in Subtalar, Talo-calcaneonavicular, and Calcaneo-cuboid Joints : § Talo-calcaneonavicular + calcaneo-cuboid joints are referred to as midtarsal or transverse tarsal joints. § Inversion + eversion of foot take place in subtalar + transverse tarsal joints. § Inversion is performed by : tibialis anterior, tibialis posterior, extensor H. L + medial tendons of extensor D. L. § Eversion is performed by : peroneus longus, peroneus brevis, and peroneus tertius. Lateral tendons of extensor digitorum longus assist.

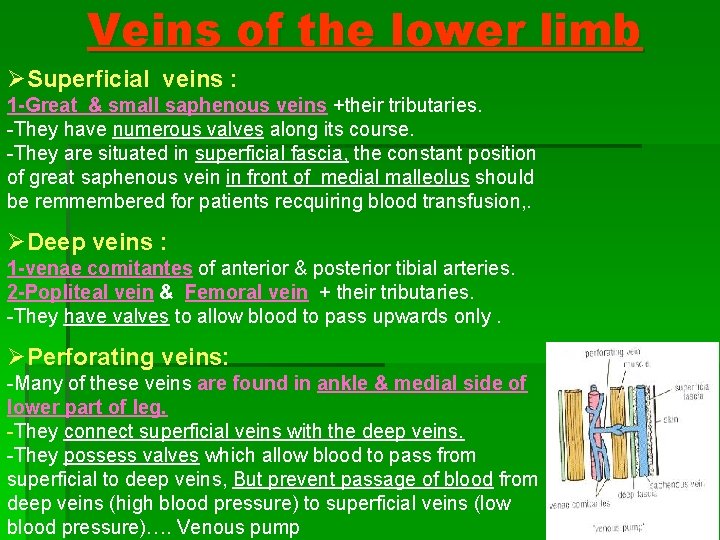
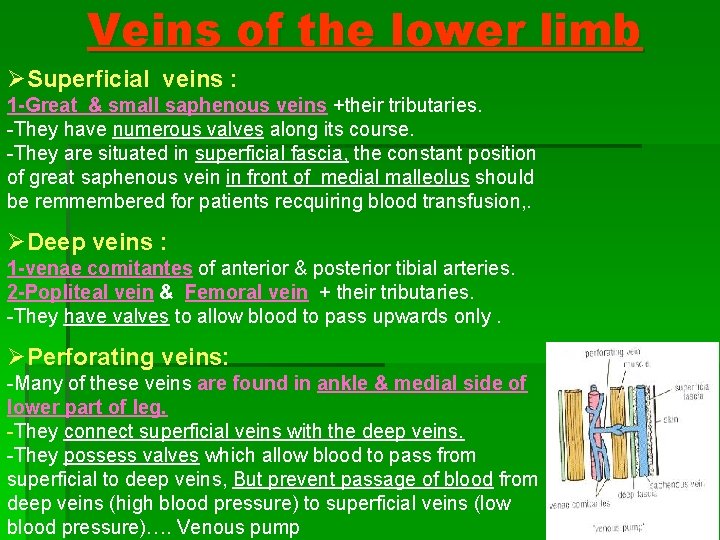
Veins of the lower limb ØSuperficial veins : 1 -Great & small saphenous veins +their tributaries. -They have numerous valves along its course. -They are situated in superficial fascia, the constant position of great saphenous vein in front of medial malleolus should be remmembered for patients recquiring blood transfusion, . ØDeep veins : 1 -venae comitantes of anterior & posterior tibial arteries. 2 -Popliteal vein & Femoral vein + their tributaries. -They have valves to allow blood to pass upwards only. ØPerforating veins: -Many of these veins are found in ankle & medial side of lower part of leg. -They connect superficial veins with the deep veins. -They possess valves which allow blood to pass from superficial to deep veins, But prevent passage of blood from deep veins (high blood pressure) to superficial veins (low blood pressure)…. Venous pump
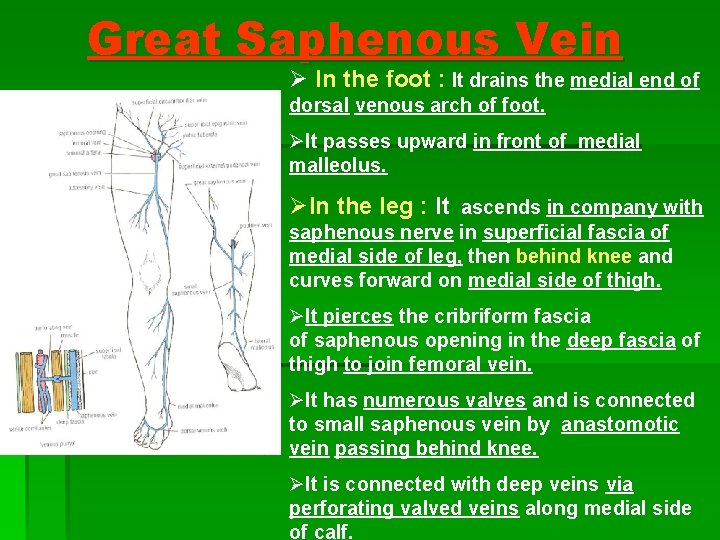
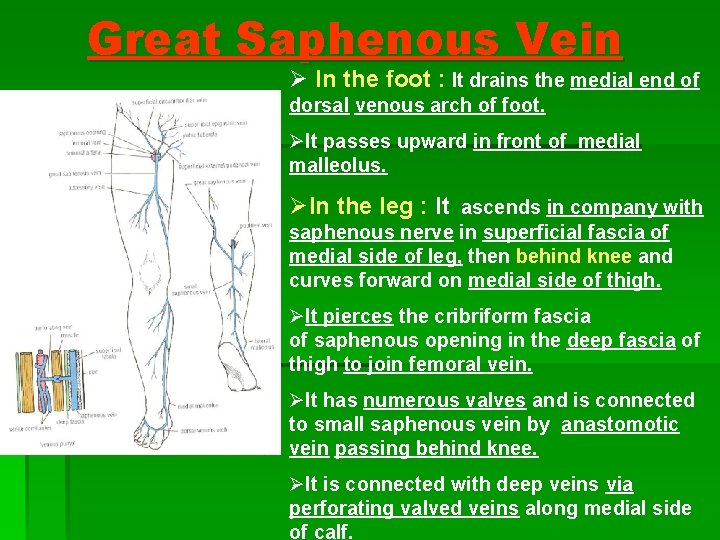
Great Saphenous Vein Ø In the foot : It drains the medial end of dorsal venous arch of foot. ØIt passes upward in front of medial malleolus. ØIn the leg : It ascends in company with saphenous nerve in superficial fascia of medial side of leg, then behind knee and curves forward on medial side of thigh. ØIt pierces the cribriform fascia of saphenous opening in the deep fascia of thigh to join femoral vein. ØIt has numerous valves and is connected to small saphenous vein by anastomotic vein passing behind knee. ØIt is connected with deep veins via perforating valved veins along medial side of calf.
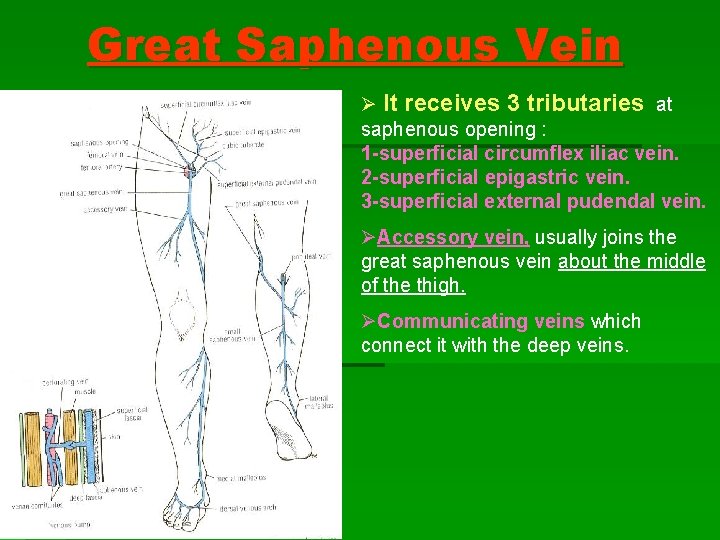
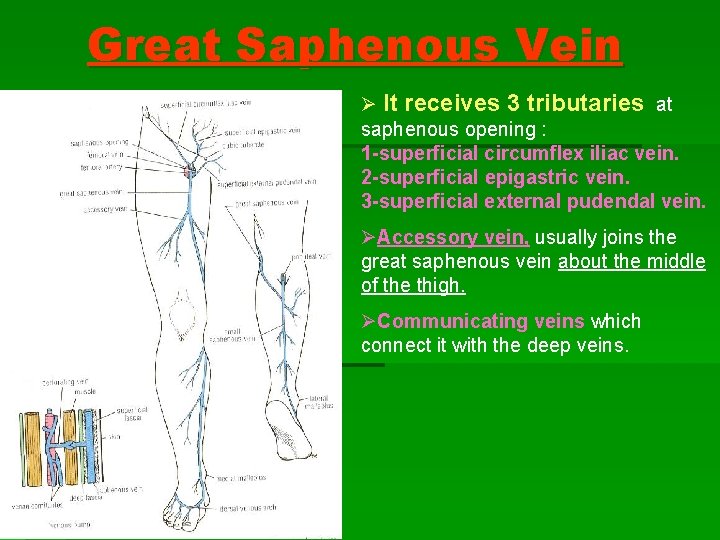
Great Saphenous Vein Ø It receives 3 tributaries at saphenous opening : 1 -superficial circumflex iliac vein. 2 -superficial epigastric vein. 3 -superficial external pudendal vein. ØAccessory vein, usually joins the great saphenous vein about the middle of the thigh. ØCommunicating veins which connect it with the deep veins.

Varicose Veins § A varicose vein is a vein which becomes dilated, elongated and tortuous. § It affects the superficial veins of the lower limb. § It is produced when the valves of the perforating veins become incompetent (so, allow blood to pass from deep veins to superficial veins). § As a result, the blood passes from deep veins (high pressure) to superficial veins (low pressure), so the superficial veins become dilated, elongated and tortuous.
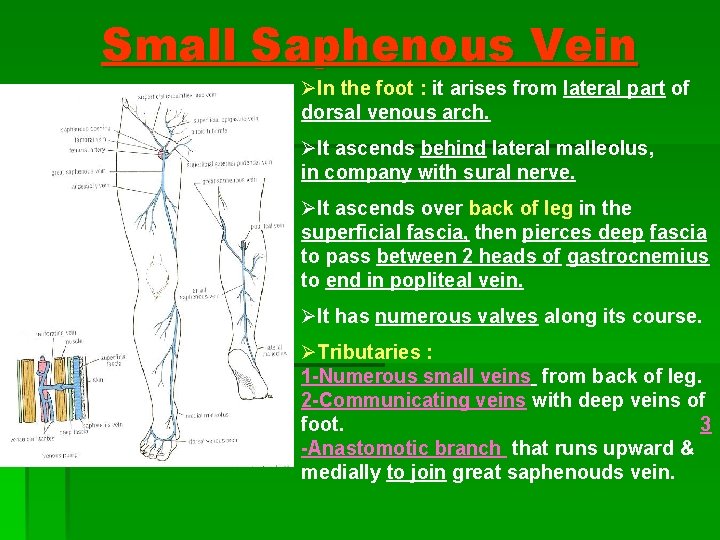
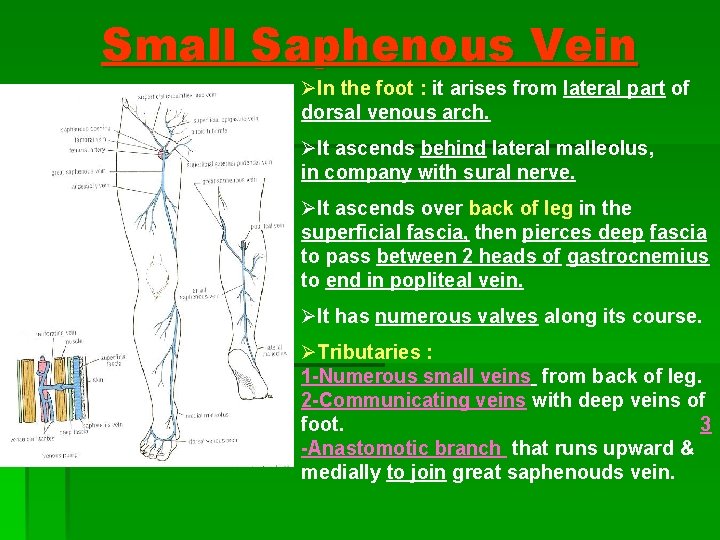
Small Saphenous Vein ØIn the foot : it arises from lateral part of dorsal venous arch. ØIt ascends behind lateral malleolus, in company with sural nerve. ØIt ascends over back of leg in the superficial fascia, then pierces deep fascia to pass between 2 heads of gastrocnemius to end in popliteal vein. ØIt has numerous valves along its course. ØTributaries : 1 -Numerous small veins from back of leg. 2 -Communicating veins with deep veins of foot. 3 -Anastomotic branch that runs upward & medially to join great saphenouds vein.
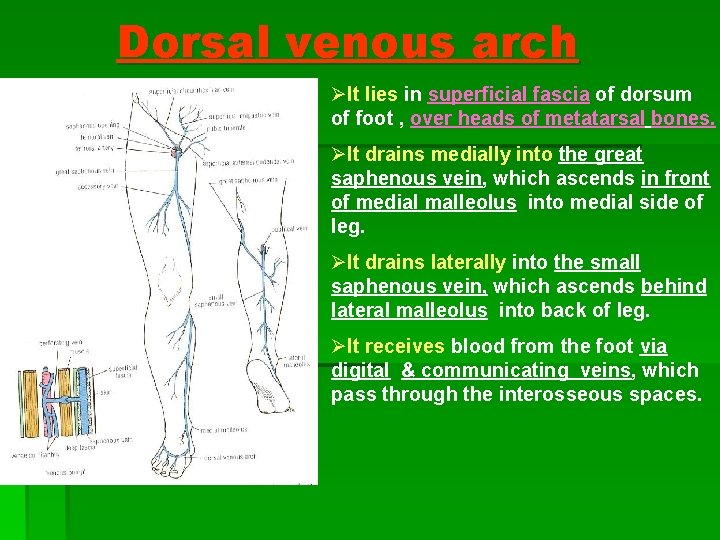
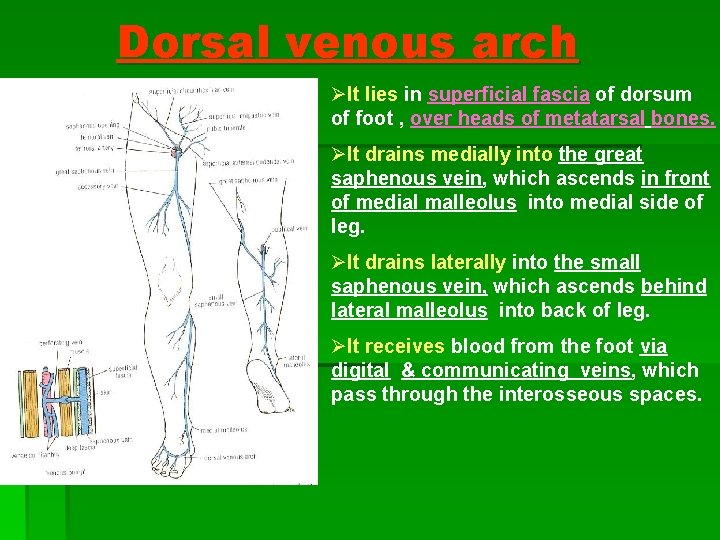
Dorsal venous arch ØIt lies in superficial fascia of dorsum of foot , over heads of metatarsal bones. ØIt drains medially into the great saphenous vein, which ascends in front of medial malleolus into medial side of leg. ØIt drains laterally into the small saphenous vein, which ascends behind lateral malleolus into back of leg. ØIt receives blood from the foot via digital & communicating veins, which pass through the interosseous spaces.
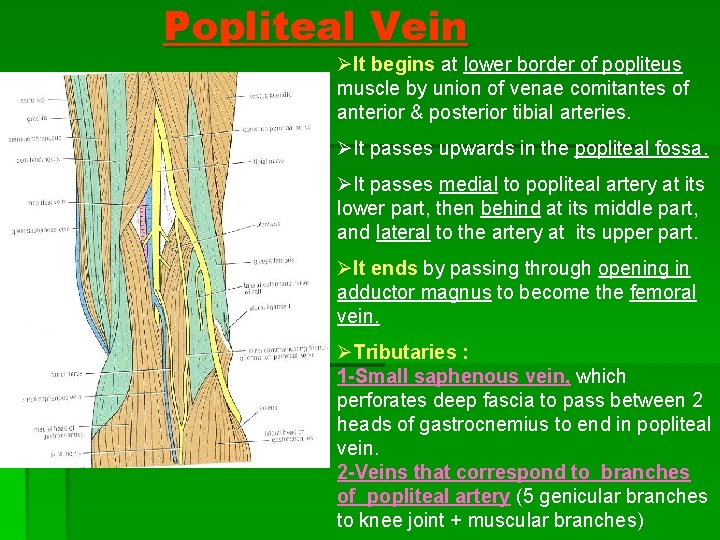
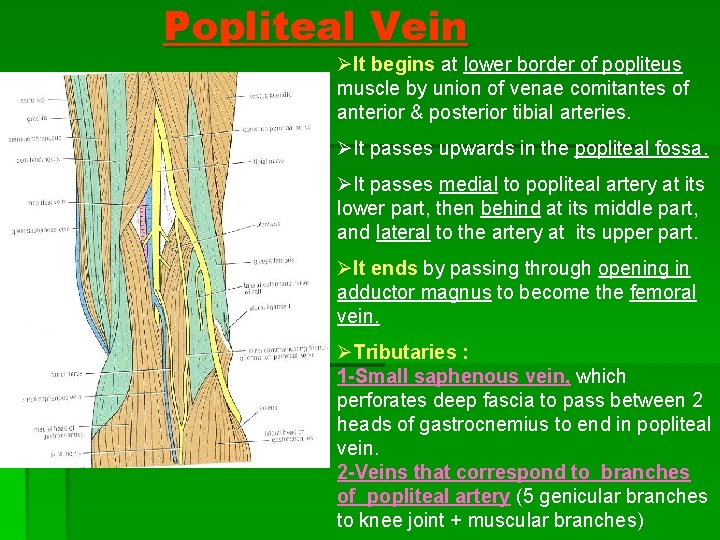
Popliteal Vein ØIt begins at lower border of popliteus muscle by union of venae comitantes of anterior & posterior tibial arteries. ØIt passes upwards in the popliteal fossa. ØIt passes medial to popliteal artery at its lower part, then behind at its middle part, and lateral to the artery at its upper part. ØIt ends by passing through opening in adductor magnus to become the femoral vein. ØTributaries : 1 -Small saphenous vein, which perforates deep fascia to pass between 2 heads of gastrocnemius to end in popliteal vein. 2 -Veins that correspond to branches of popliteal artery (5 genicular branches to knee joint + muscular branches)
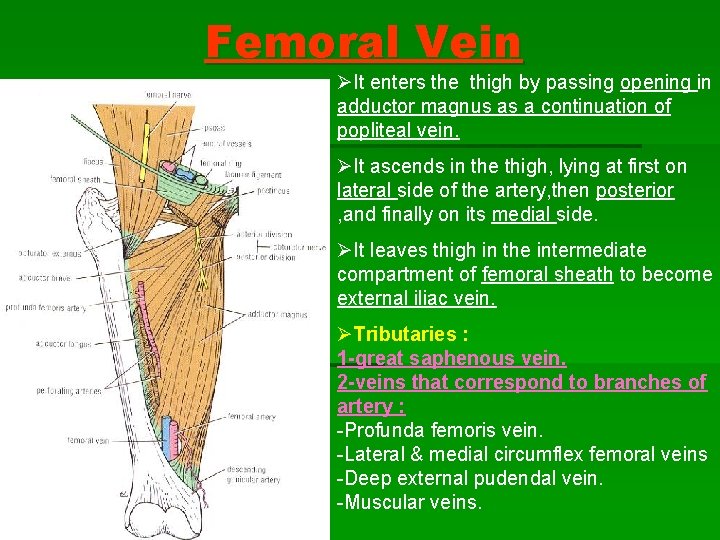
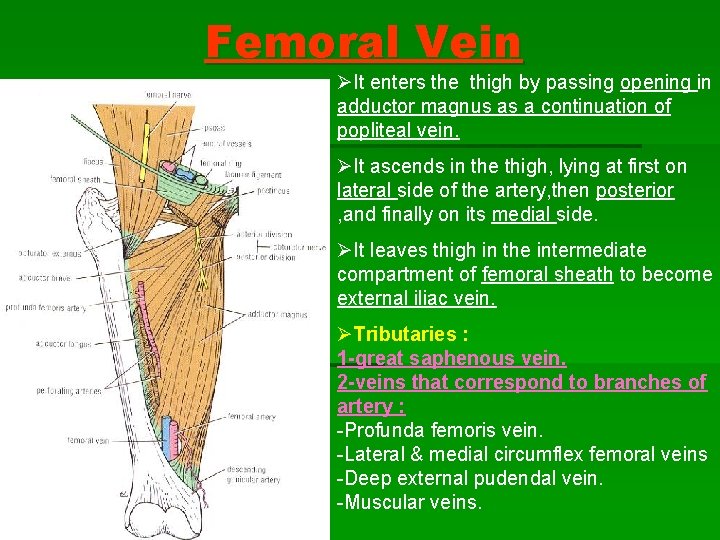
Femoral Vein ØIt enters the thigh by passing opening in adductor magnus as a continuation of popliteal vein. ØIt ascends in the thigh, lying at first on lateral side of the artery, then posterior , and finally on its medial side. ØIt leaves thigh in the intermediate compartment of femoral sheath to become external iliac vein. ØTributaries : 1 -great saphenous vein. 2 -veins that correspond to branches of artery : -Profunda femoris vein. -Lateral & medial circumflex femoral veins -Deep external pudendal vein. -Muscular veins.

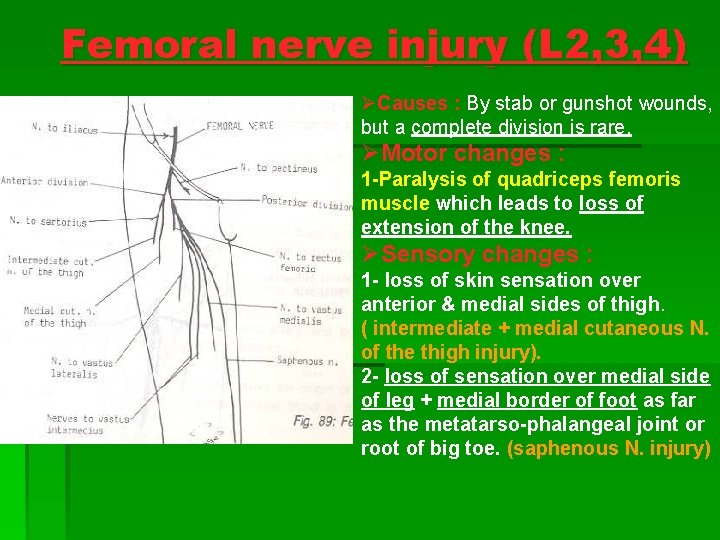
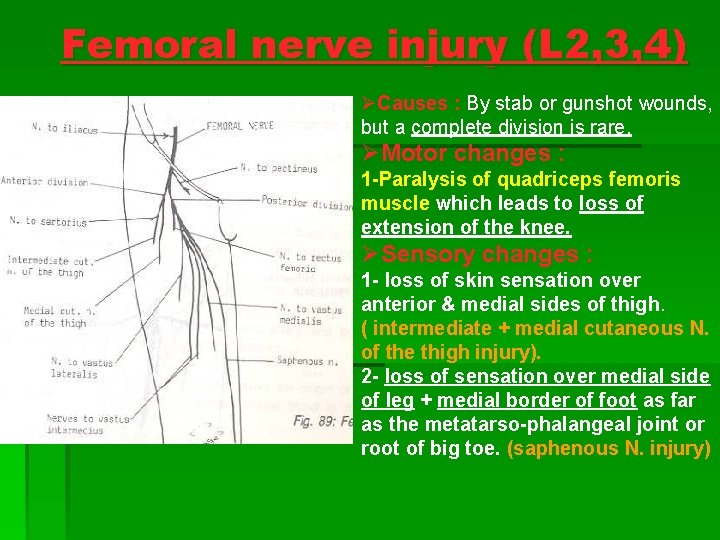
Femoral nerve injury (L 2, 3, 4) ØCauses : By stab or gunshot wounds, but a complete division is rare. ØMotor changes : 1 -Paralysis of quadriceps femoris muscle which leads to loss of extension of the knee. ØSensory changes : 1 - loss of skin sensation over anterior & medial sides of thigh. ( intermediate + medial cutaneous N. of the thigh injury). 2 - loss of sensation over medial side of leg + medial border of foot as far as the metatarso-phalangeal joint or root of big toe. (saphenous N. injury)
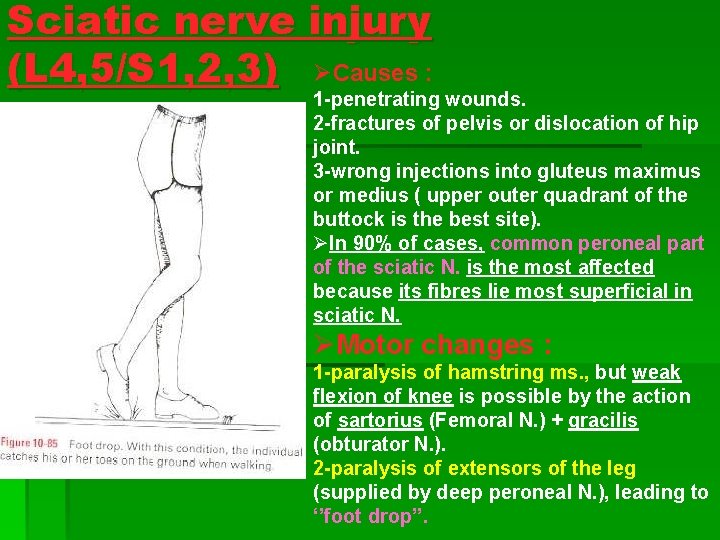
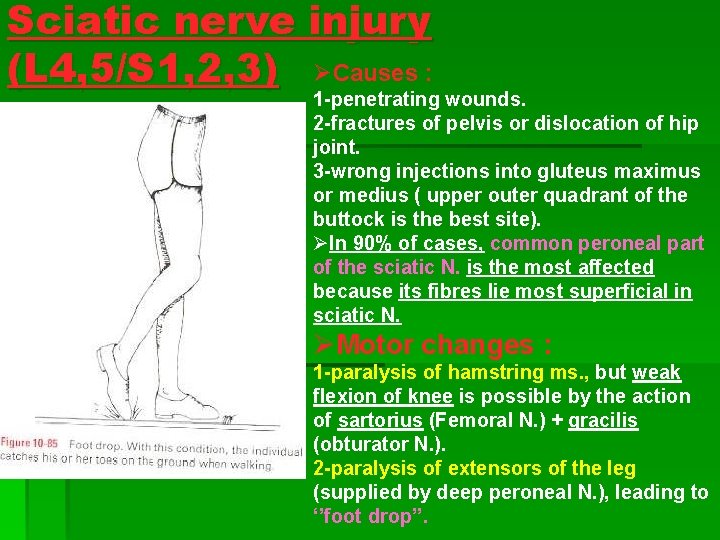
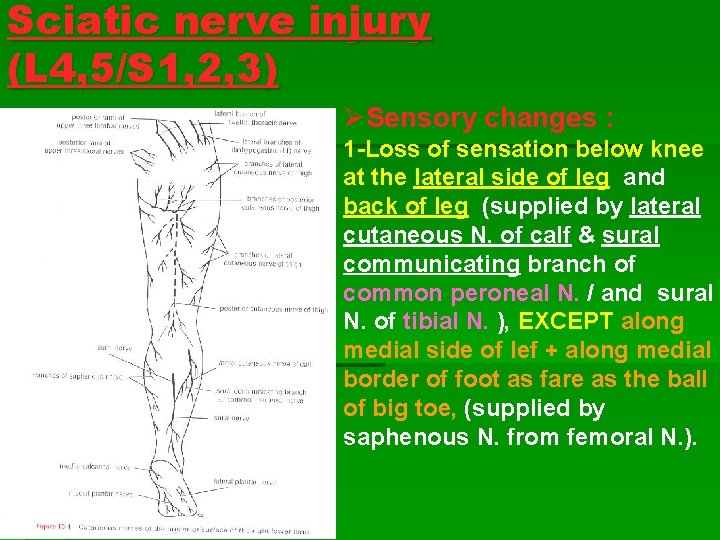
Sciatic nerve injury (L 4, 5/S 1, 2, 3) ØCauses : 1 -penetrating wounds. 2 -fractures of pelvis or dislocation of hip joint. 3 -wrong injections into gluteus maximus or medius ( upper outer quadrant of the buttock is the best site). ØIn 90% of cases, common peroneal part of the sciatic N. is the most affected because its fibres lie most superficial in sciatic N. ØMotor changes : 1 -paralysis of hamstring ms. , but weak flexion of knee is possible by the action of sartorius (Femoral N. ) + gracilis (obturator N. ). 2 -paralysis of extensors of the leg (supplied by deep peroneal N. ), leading to ‘’foot drop’’.
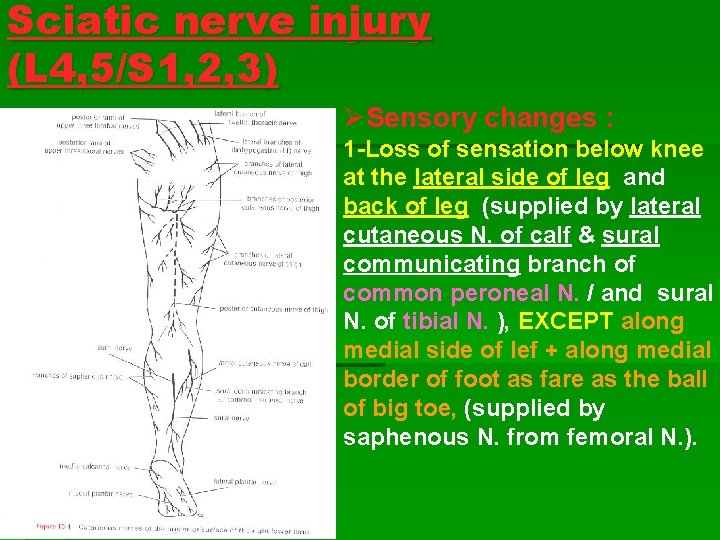
Sciatic nerve injury (L 4, 5/S 1, 2, 3) ØSensory changes : 1 -Loss of sensation below knee at the lateral side of leg and back of leg (supplied by lateral cutaneous N. of calf & sural communicating branch of common peroneal N. / and sural N. of tibial N. ), EXCEPT along medial side of lef + along medial border of foot as fare as the ball of big toe, (supplied by saphenous N. from femoral N. ).
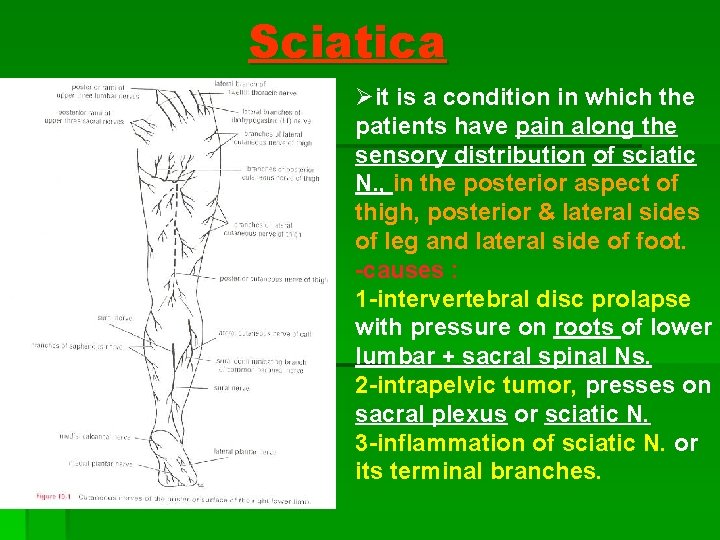
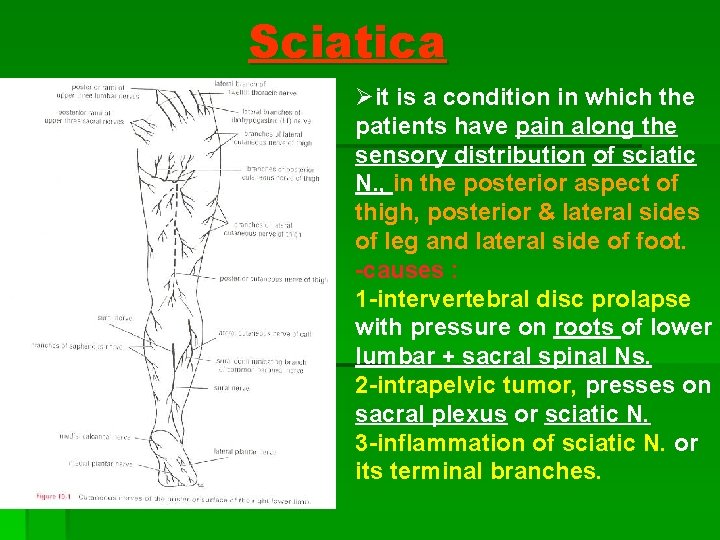
Sciatica Øit is a condition in which the patients have pain along the sensory distribution of sciatic N. , in the posterior aspect of thigh, posterior & lateral sides of leg and lateral side of foot. -causes : 1 -intervertebral disc prolapse with pressure on roots of lower lumbar + sacral spinal Ns. 2 -intrapelvic tumor, presses on sacral plexus or sciatic N. 3 -inflammation of sciatic N. or its terminal branches.
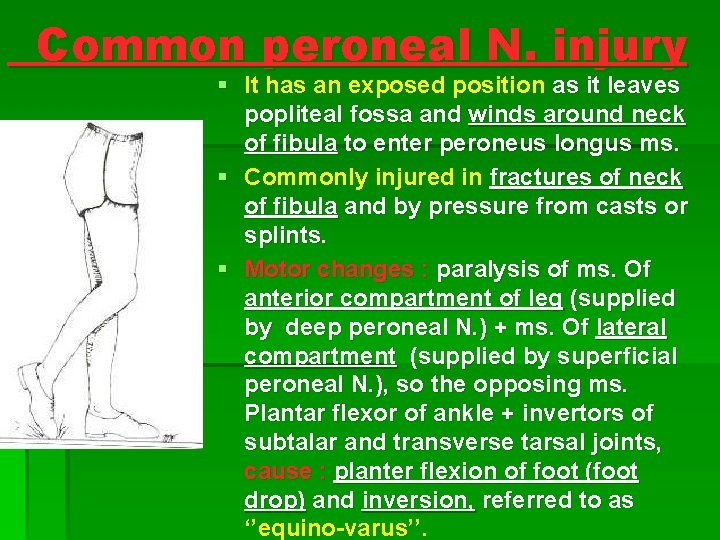
Common peroneal N. injury § It has an exposed position as it leaves popliteal fossa and winds around neck of fibula to enter peroneus longus ms. § Commonly injured in fractures of neck of fibula and by pressure from casts or splints. § Motor changes : paralysis of ms. Of anterior compartment of leg (supplied by deep peroneal N. ) + ms. Of lateral compartment (supplied by superficial peroneal N. ), so the opposing ms. Plantar flexor of ankle + invertors of subtalar and transverse tarsal joints, cause : planter flexion of foot (foot drop) and inversion, referred to as ‘’equino-varus’’.
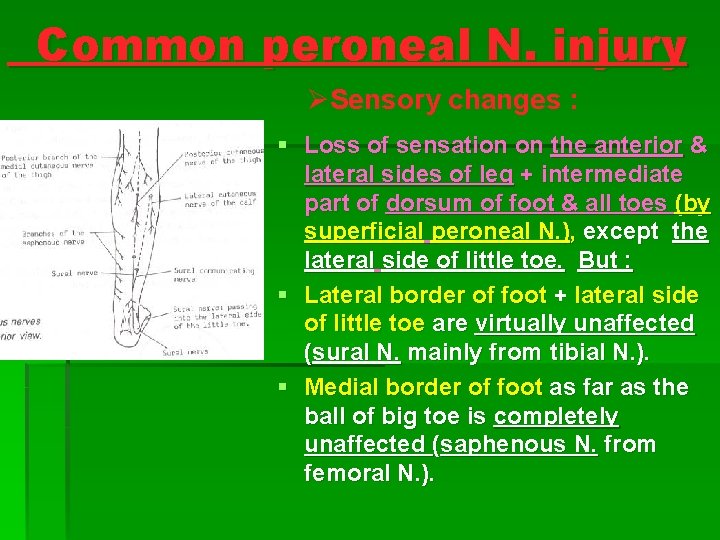
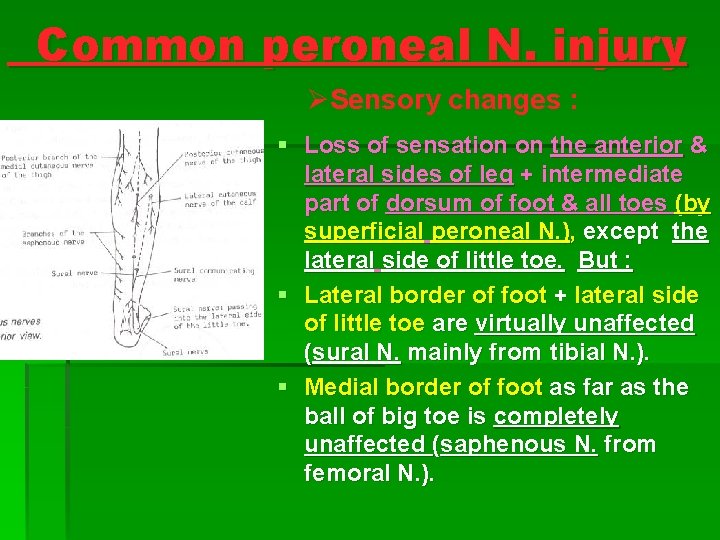
Common peroneal N. injury ØSensory changes : § Loss of sensation on the anterior & lateral sides of leg + intermediate part of dorsum of foot & all toes (by superficial peroneal N. ), except the lateral side of little toe. But : § Lateral border of foot + lateral side of little toe are virtually unaffected (sural N. mainly from tibial N. ). § Medial border of foot as far as the ball of big toe is completely unaffected (saphenous N. from femoral N. ).

Tibial N. injury § It leaves popliteal fossa deep to gastrocnemius & soleus ms. § Because of its deep position, it is rarely injured. § Motor changes : -paralysis of plantar flexor ms. Of back of leg + of sole of foot, so the opposing ms. (extensors) dorsiflex the foot at ankle + evert foot at subtalar & transverse tarsal joints, it is reffered to as calcaneo-valgus. § Sensory changes : -loss of sensation on sole of foot, Later trophic ulcers develop.

Obturator N. injury ØIt enters thigh as anterior & posterior divisions through upper part of obturator foramen. / anterior division descends infront of adductor brevis, and posterior division descends behind adductor brevis and in front of adductor magnus. ØIt is rarely injured as in case of penetrating wounds. ØMotor changes : paralysis of all adductor ms. Except ischial (hamstring) part of adductor magnus (by sciatic N. ). ØSensory changes : is minimal on the medial aspect of the thigh.

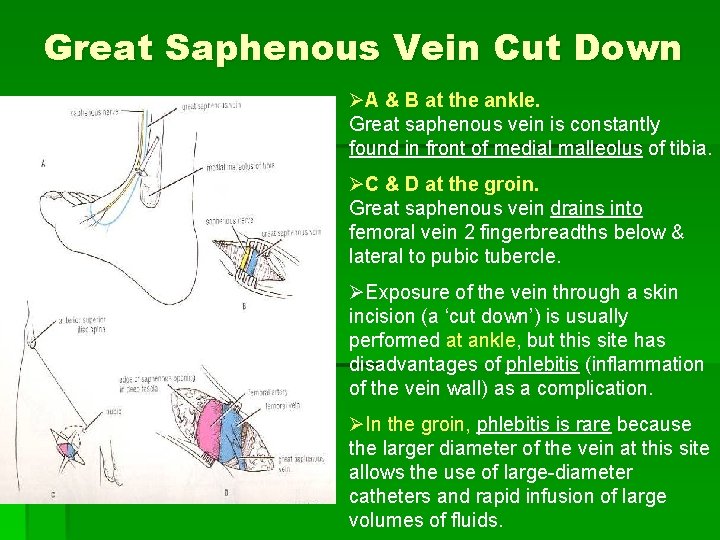
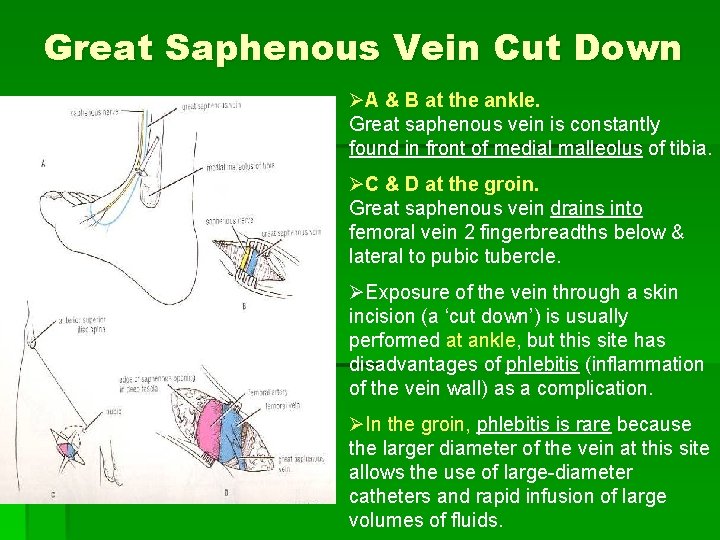
Great Saphenous Vein Cut Down ØA & B at the ankle. Great saphenous vein is constantly found in front of medial malleolus of tibia. ØC & D at the groin. Great saphenous vein drains into femoral vein 2 fingerbreadths below & lateral to pubic tubercle. ØExposure of the vein through a skin incision (a ‘cut down’) is usually performed at ankle, but this site has disadvantages of phlebitis (inflammation of the vein wall) as a complication. ØIn the groin, phlebitis is rare because the larger diameter of the vein at this site allows the use of large-diameter catheters and rapid infusion of large volumes of fluids.

Great Saphenous Vein in Coronary Bypass surgery § In occlusive coronary disease, the diseased arterial segment can be bypassed by inserting a graft from great saphenous vein. § At the donor sit, the superficial venous blood ascends the lower limb against gravity by passing through perforating veins into the deep veins. § Great saphenous vein can also be used to bypass obstructions of brachial or femoral arteries.
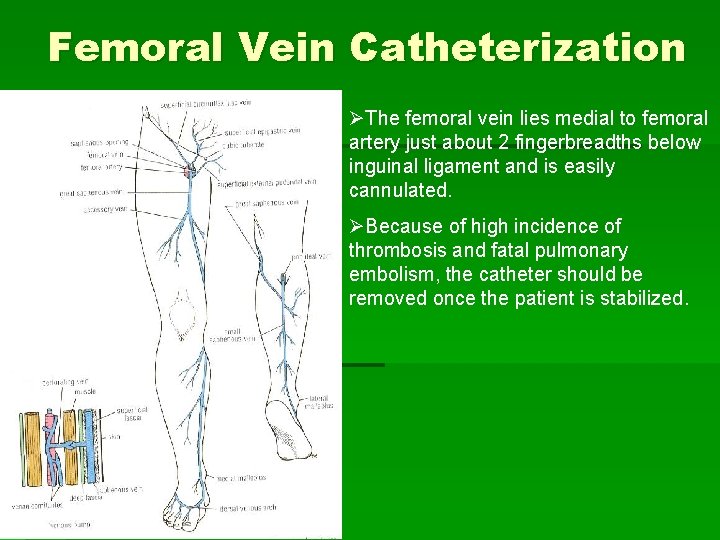
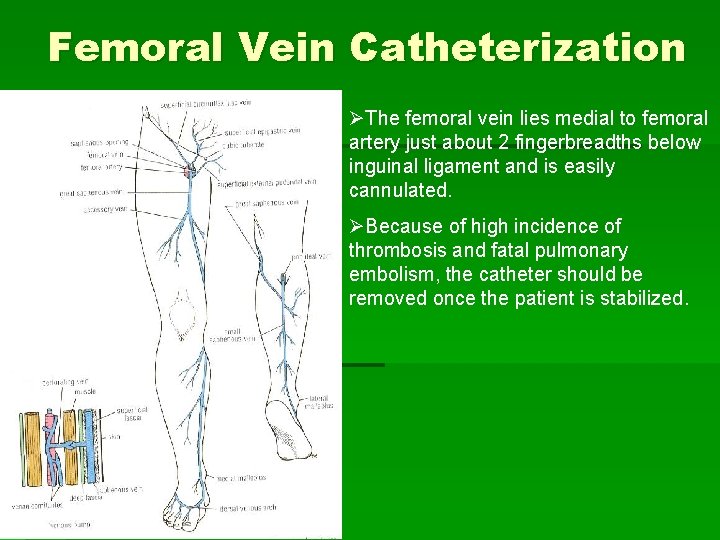
Femoral Vein Catheterization ØThe femoral vein lies medial to femoral artery just about 2 fingerbreadths below inguinal ligament and is easily cannulated. ØBecause of high incidence of thrombosis and fatal pulmonary embolism, the catheter should be removed once the patient is stabilized.

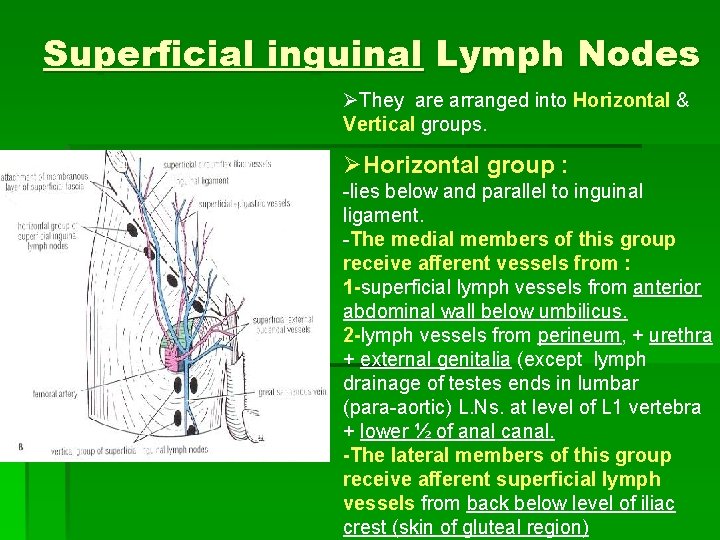
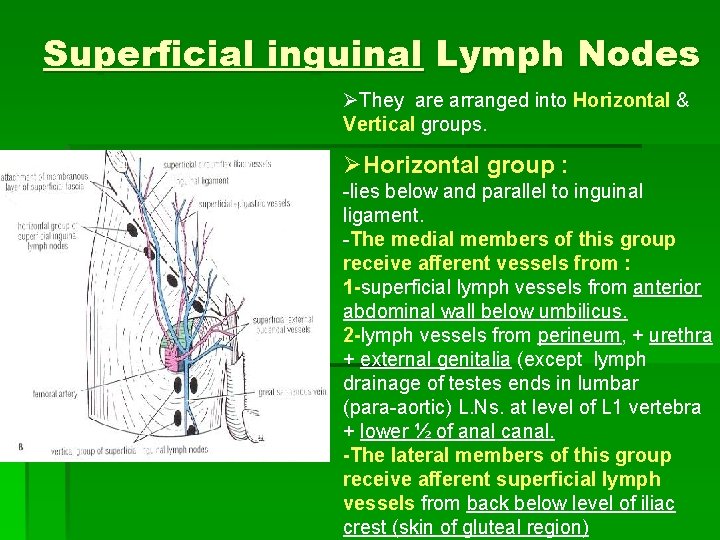
Superficial inguinal Lymph Nodes ØThey are arranged into Horizontal & Vertical groups. ØHorizontal group : -lies below and parallel to inguinal ligament. -The medial members of this group receive afferent vessels from : 1 -superficial lymph vessels from anterior abdominal wall below umbilicus. 2 -lymph vessels from perineum, + urethra + external genitalia (except lymph drainage of testes ends in lumbar (para-aortic) L. Ns. at level of L 1 vertebra + lower ½ of anal canal. -The lateral members of this group receive afferent superficial lymph vessels from back below level of iliac crest (skin of gluteal region)
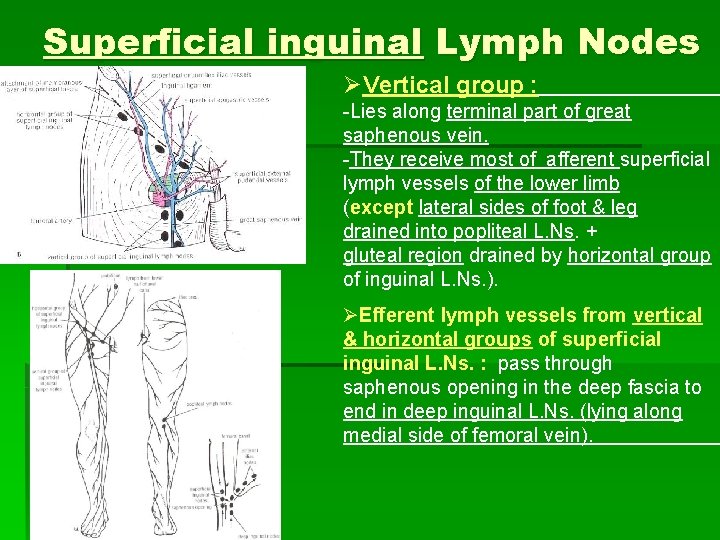
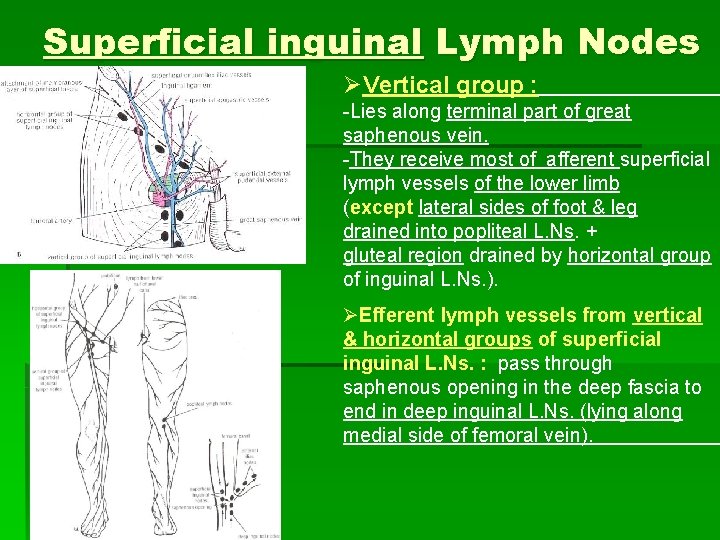
Superficial inguinal Lymph Nodes ØVertical group : -Lies along terminal part of great saphenous vein. -They receive most of afferent superficial lymph vessels of the lower limb (except lateral sides of foot & leg drained into popliteal L. Ns. + gluteal region drained by horizontal group of inguinal L. Ns. ). ØEfferent lymph vessels from vertical & horizontal groups of superficial inguinal L. Ns. : pass through saphenous opening in the deep fascia to end in deep inguinal L. Ns. (lying along medial side of femoral vein).
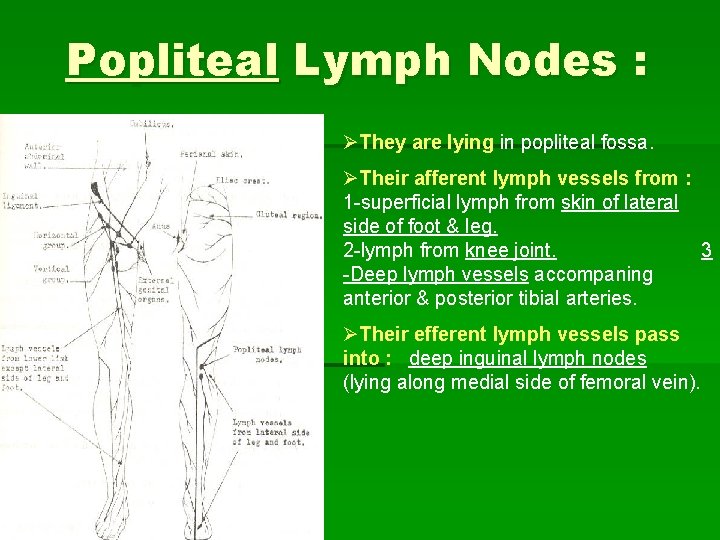
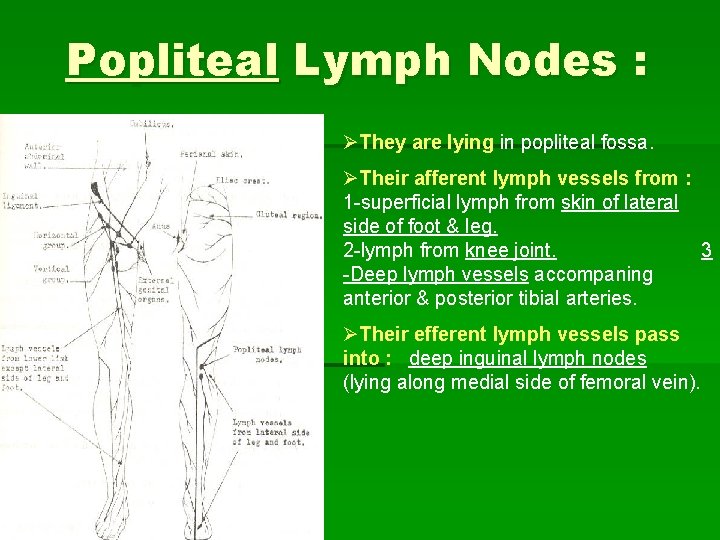
Popliteal Lymph Nodes : ØThey are lying in popliteal fossa. ØTheir afferent lymph vessels from : 1 -superficial lymph from skin of lateral side of foot & leg. 2 -lymph from knee joint. 3 -Deep lymph vessels accompaning anterior & posterior tibial arteries. ØTheir efferent lymph vessels pass into : deep inguinal lymph nodes (lying along medial side of femoral vein).
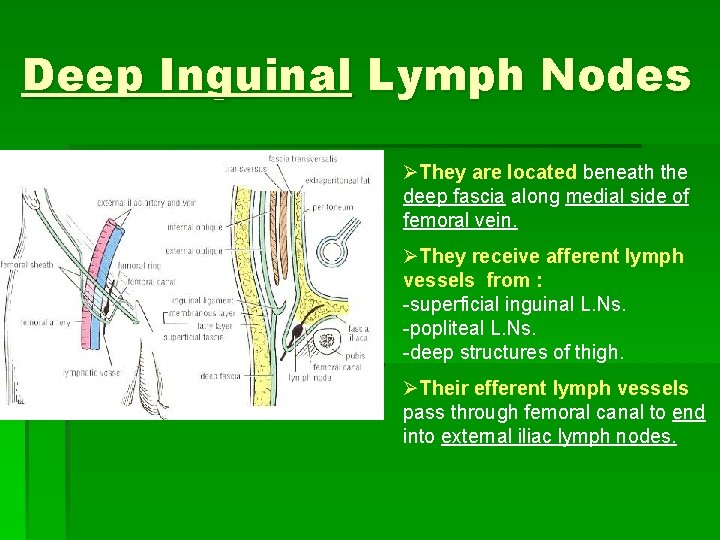
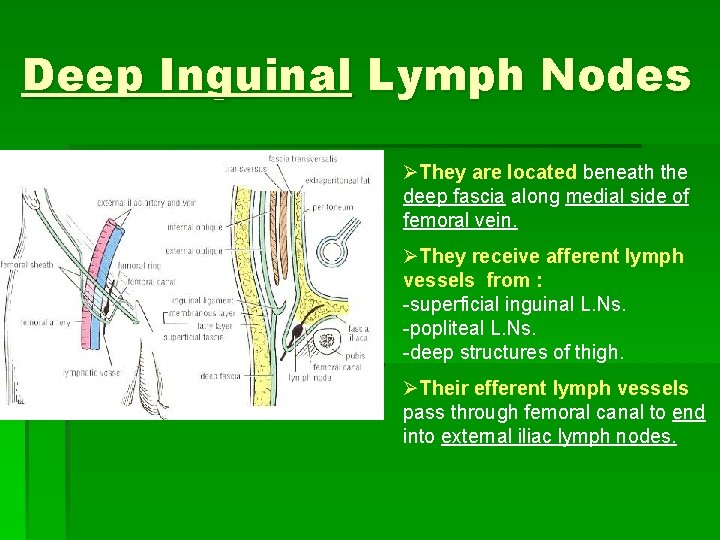
Deep Inguinal Lymph Nodes ØThey are located beneath the deep fascia along medial side of femoral vein. ØThey receive afferent lymph vessels from : -superficial inguinal L. Ns. -popliteal L. Ns. -deep structures of thigh. ØTheir efferent lymph vessels pass through femoral canal to end into external iliac lymph nodes.