Anesthetics Management for Neonates with Gastroschisis Repair Claire



























- Slides: 35
Anesthetics Management for Neonates with Gastroschisis Repair Claire Yang, SRNA Duke University Class of 2013
Objectives Differentiate between gastroschisis and omphalocele Temperature regulation of the neonate Identify correct strategies for fluid management List the preop considerations, possible intraop complications, and postop anesthetic care

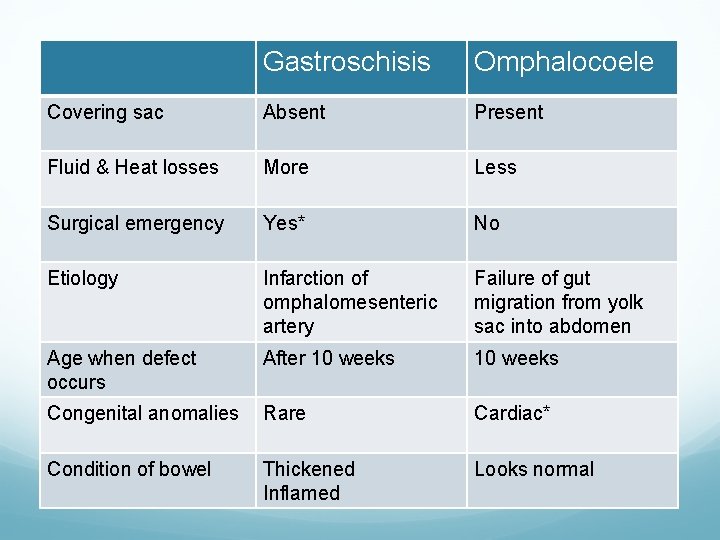
Gastroschisis & Omphalacoele
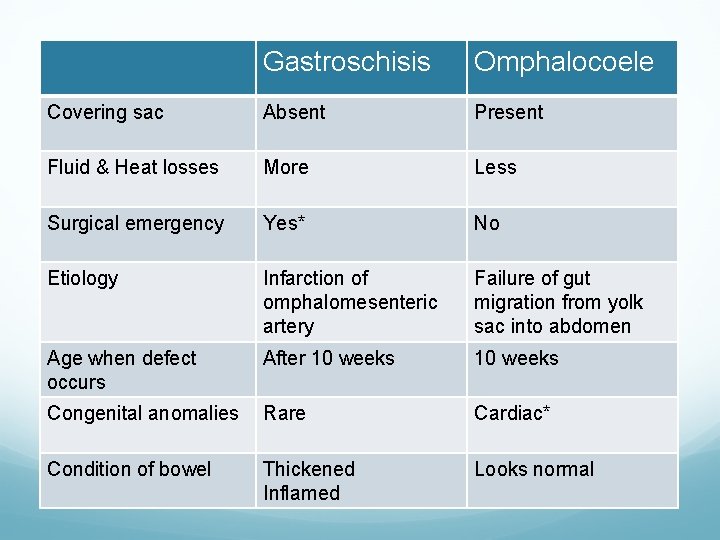
Gastroschisis Omphalocoele Covering sac Absent Present Fluid & Heat losses More Less Surgical emergency Yes* No Etiology Infarction of omphalomesenteric artery Failure of gut migration from yolk sac into abdomen Age when defect occurs After 10 weeks Congenital anomalies Rare Cardiac* Condition of bowel Thickened Inflamed Looks normal
Gastroshisis 1 birth per 10, 000, male > female Young maternal age <20, cigarette smoking, preterm, and low birth weight Often diagnosed with routine ultrasound When? Where? How to deliver?

Hypothermia Large surface area to body weight ratio Less SQ fat to insulate Infants less than 3 months cannot shiver Immature SNS, can’t control vasoconstriction Greater skin permeability to water Exaggerated by the exposed bowel
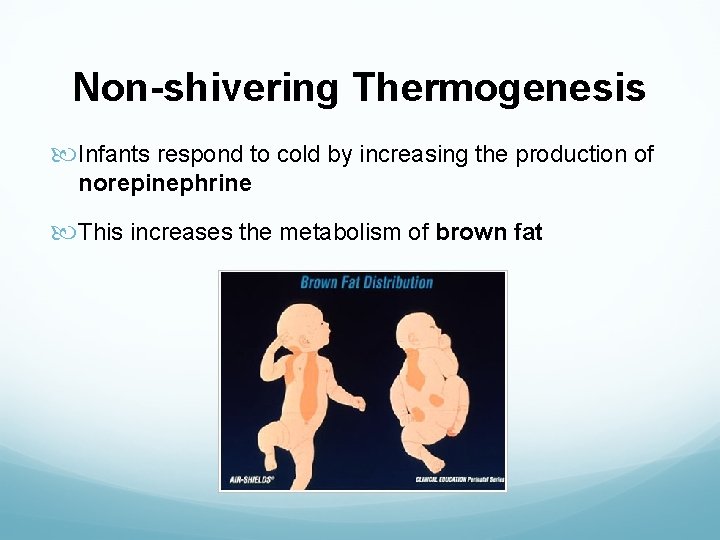
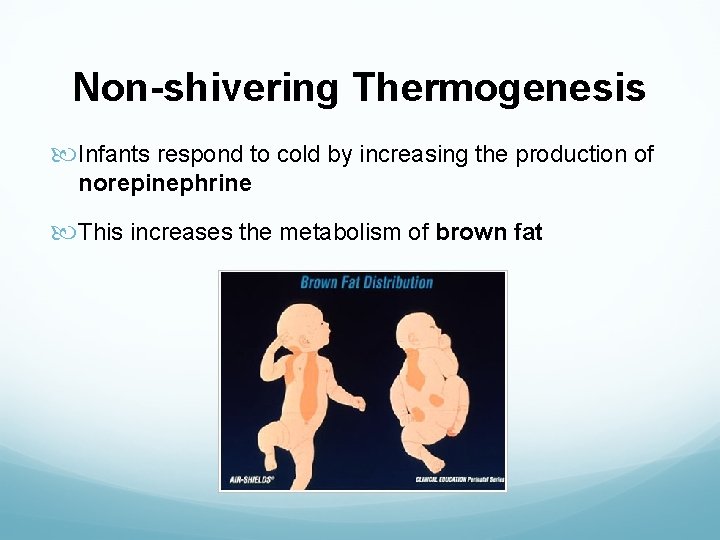
Non-shivering Thermogenesis Infants respond to cold by increasing the production of norepinephrine This increases the metabolism of brown fat

Thermoregulation Brown Adipose Tissue (Brown Fat) Found in newborn and hibernating mammals Develops at 26 to 30 weeks of gestation 5% of total weight Midscapular, back of the neck, clavicles, axillae, mediastinum, kidneys, and adrenal glands Abundance of mitochondria, glycogen stores, blood supply to generate body heat
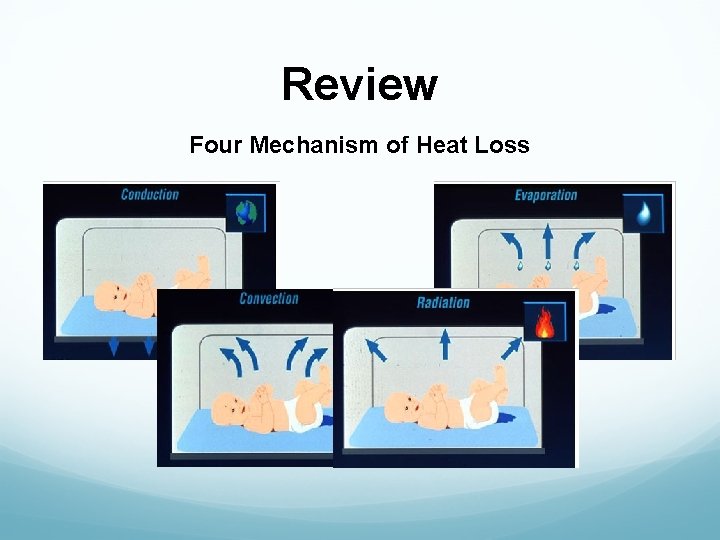
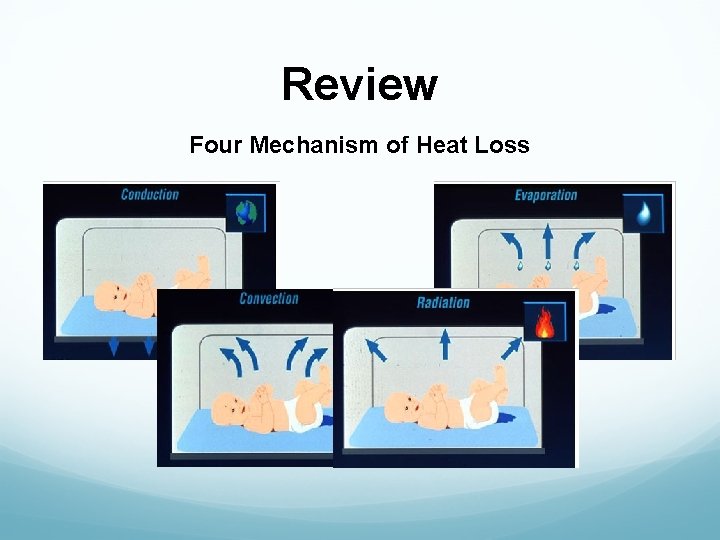
Review Four Mechanism of Heat Loss

How to Warm? Warm OR to 75 -80*F Heat lamps Bair Hugger blanket Plastic Fluid warmer

Post-Delivery Management Begin in delivery room before coming to the OR Assess V/S and early stabilization (oxygenation, intubation*, ventilation, IV access*) Place gastric tube to decompress the stomach Cover bowels with warm, moist, sterile dressing Cover the entire lower body with a sterile plastic bag Transfer to OR or other facilities in the incubator Avoid further trauma to bowel during transport (twisted bowel can result in ischemia)


Preop Assessment Gestational age? Term or preterm? Weight? Vitamin K? Surfactant? If intubated already, check the ETT size and position If not intubated, continue respiratory assessment ( Sa. O 2 on routine handling, tachypnea, tachycardia, nasal flaring) Signs of circulatory insufficiency: tachypnea, tachycardia, cold peripheries, pale or mottled skin, delayed capillary refill; low BP is a late sign. Continue fluid resuscitation, reassess and repeat

Intraop Monitoring Standard ASA Monitoring (EKG, BP, Sa. O 2, ETCO 2, Temp) If the neonate is able to maintain respiratory homeostasis and whose hernia size is < 4 cm Invasive Pressure Monitoring If the neonate is unstable, hypotensive, hypoxic, using accessory muscle to maintain saturation, and with hernia size > 4 cm Central venous line, arterial line

Anesthetic Technique Susceptible to aspiration Awake intubation or RSI with Propofol; +/- muscle relaxant Mask induction with Sevoflurane & oxygen Preemie: 2. 5 ETT Term: 3. 0 -3. 5 ETT A slight leak pressure of 20 -25 cm. H 2 O to prevent compression damage to the tracheal mucosa Bradycardia b/c PNS is dominant

Maintenance of Anesthesia requirement for maintenance in neonates (Sevo 2. 1%) is less than infants (3. 2%) Oxygen, air, and Sevoflurane Maintain O 2 saturation mid-90’s% to avoid the risk for retinopathy of prematurity No Nitrous oxide Keep them on muscle relaxant* Opioids*

Intraop Fluid Management Maintenance Third space losses Estimated blood volume Maximum allowable blood loss How to give blood and albumin

Maintenance Fluid D 5 0. 2%NS Via syringe pump or 250 ml bag on IV pump or buratrol drip chamber tubing No air bubbles May double the MIVF 0 -10 kg 11 -20 kg >20 kg 4 -8 ml/kg/hr 2 ml/kg/hr 1 ml/kg/hr

3 rd Space Losses LR is used Albumin 5% maybe used if rapid volume expansion is needed 6 -10 -15 ml/kg/hr

Estimated Blood Volume Preterm Full term 100 ml/kg 90 ml/kg

Allowable Blood Lost ABL = EBV x (starting Hct – allowable Hct) starting Hct

How to Give Blood and Albumin Warm blood with hotline Use a pediatric blood set + stopcock Push blood with a syringe for accurate measurement Give 10 -20 ml/kg at a time Watch BP!!!

Surgical Repair Goal: to return the bowel to the abdomen and close the fascia in one operation Primary closure Staged closure: silo pouch first complete closure Gastroschisis. net

Hemodynamic Effects of Primary Closure Intra-abdominal Pressure A NG/OG can be placed in the stomach with a column of saline; or bladder pressure Goal: < 20 mm. Hg when closing the defect Increased intra-abdominal pressure results in: preload: hypotension pulmonary compliance: PIP, Vt, ETCO 2, Sa. O 2 urine output

Yaster et al Intragastric pressure > 20 mm. Hg or CVP > 4 mm. Hg Higher mortality rate caused by ischemia of the bowel or the lower extremities Morgan & Mikhail Suggested criteria for a staged closure include: 1. Intragastric pressure >20 mm. Hg 2. PIP > 35 cm. H 2 O 3. ETCO 2 > 50 mm. Hg

Emergence If the neonate tolerated the primary closure or the defect is very small, may try extubate at the end of the surgery. In these patients, give reversal and extubate when fully awake, with regular spontaneous breathing, grimacing, moving all limbs vigorously However, the majority of babies will returned to NICU intubated b/c the increased intra-abd pressure with compromised respiratory function

The Sux Dart If laryngospasm does occur post extubation, remember to give atropine and succinycholine together If IV access is not present, atropine and succinycholine can be given IM or sublingually Atropine 0. 02 mg/kg IM Succ 4 mg/kg IM

Postop Management Neonatal ICU If remains intubated, continue sedation with morphine (10 -20 mcq/kg/hr) Some may require muscle relaxation for 24 hrs; cisatracurium (3 mcq/kg/min) The duration of sedation and paralysis is governed by the ease and speed of return of bowel to the abdominal cavity ~ 10 days

#1 Postop Complication Abdominal Compartment Syndrome Upward shift in the diaphragm interfering with ventilation Renal and hepatic perfusion Perfusion to lower limbs, ✓ Sa. O 2 on big toes Re-open the abdomen and place the silo pouch Reduce the tension on the pouch and allow a portion of the bowel to re-herniate

Other Postop Complications GI Non-GI Necrotizing enterocolitis Sepsis Renal insufficiency Ventilator-acquired Pneumonia Cellulitis of the abd wall UTI Abd wall breakdown Wound infection Gastroesophageal reflux Cholestasis

Prognosis In the 1960’s, up to 70% of these neonates failed to survive With improved preoperative and postop resuscitation, 90% survival rate Majority of the neonates have no associated cardiac or respiratory abnormalities, survive to normal adult lives

Summary Neonates with gastroschisis require emergent surgical repair Susceptible to heat/fluid loss, infection, electrolyte imbalance, and trauma Goals: secure the airway, obtain I. V. access, begin fluid resuscitation as early as possible, prevent hypothermia, continue ventilatory support intraop and postop Questions?
Reference Cauchi, J. , Parikh, D. H. , Samuel, M. , & Gornall, P. (2006). Does gastroschisis reduction require general anesthesia? A comparative analysis. Journal of Pediatric Surgery, 41, 1294 -1297 Hartley, L. , & Poddar, R. (2009). Exomphalos and gastroschisis. Continuing Education in Anaesthesia, Critical Care & Pain. doi: 10. 1093/bjaceaccp/mkp 001 Jaffe RA, Samuels SL. (2004). Anesthesiologist’s Manual of Surgical Procedures. 3 rd ed. Philadelphia PA: Lippincott Williams & Wilkins Leabetter, D. (2006). Gastroschisis and omphalocele. Surgical Clinics of North America, 86, 249 -260

Reference Macksey, L. F. (2009). Pediatric Anesthetics and Emergency Drug Guide. Sudbury, Massachusetts: Jones and Bartlett Publishers Morgan, G. E. , Mikhail, M. S. , & Murray, M. J. (2006). Clinical Anesthesiology. 4 th ed. New York, NY: Mc. Graw-Hill Myo, C. C. (2007). Preanesthetic assessment of the newborn with an abdominal wall defect. Retrieved from http: //www. amcresidents. com Wielar, A. (2011). Anesthetic Considerstions for Patients Smaller Than a Box. [Power. Point slides]. Retrieved from Duke University Advanced Principles of Anesthesia II Blackboard: http: //blackboard. duke. edu
Reference Wouters, K. , & Walker, I. (2007). Anaesthesia for neonates with abdominal wall defects. Retrieved from: http: //www. frca. co. uk/article. aspx? articleid=100983