Anesthetic management of foreign body bronchus in children
Anesthetic management of foreign body bronchus in children Dr. S. Parthasarathy MD. , DA. , DNB, MD (Acu), Dip. Diabetes, Diploma in Software based statistics, Ph. D ( physiology), IDRA , FICA , Certifícate in USGRA Associate editor - IJA
History • Gustav Killian was the first to use the rigid bronchoscopy method in 1897 to remove a foreign body from the right main bronchus. • flexible bronchoscope was started in the 1970 s, especially for the removal of aspirated foreign material localised in the distal airways
All contribute !! • • • 6 months to 5 years Propensity to play Incomplete chewing Putting everything in mouth Incomplete protective reflexes Airway anatomy
• History from parent • Something she was eating while playing or crying • Trying Fb removal by mother • Slowly moves from place to place and lands up after 12 hours sometimes • Means – not life threatening • Weeps or talks – chances of going in
Epidemiology • Exact data – in India not available !! • Many centers report 100 cases in four years • 25 cases / year – so many centres in India !! • Winter months ? • Eating peanuts and wall nuts in winter ?
Symptomatology • cough and noisy respiration • diminished air entry on examination is not always seen. • History of Fb ingestion ? Usually may be there • In cases with delayed diagnosis the unilateral subsidence of breath sounds, audible ronchi, persistent coughing and repetitive pneumonia may be observed • Suprasternal retraction respiratory distress and cyanosis
• Time • ( 12 hour to six months ) • 12 hours wait may get the patient sometimes unconscious • Situation • ( usually right main bronchus) • What is the type of FB ? • Organic (peanut ) and metals
Where is the FB ? • Subglottic area – narrowest portion ? • Stridor – inspiratory • Trachea – usually stridor with both inspiration and expiration • Carina - usually stridor with both inspiration and expiration
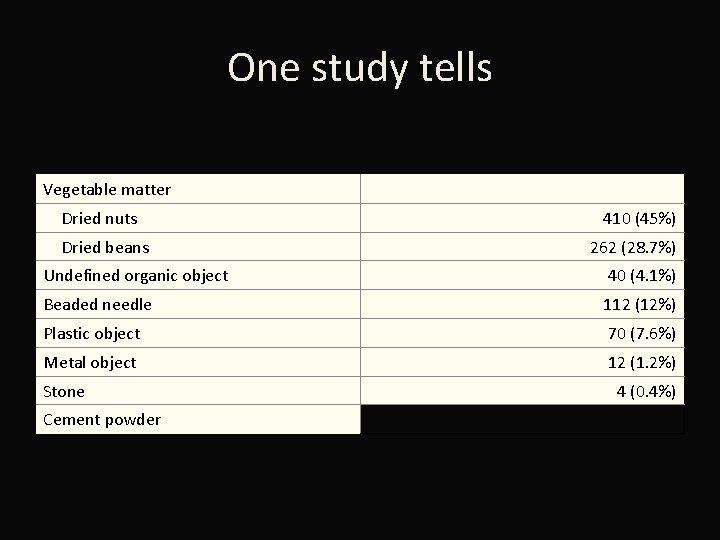
One study tells Vegetable matter Dried nuts Dried beans 410 (45%) 262 (28. 7%) Undefined organic object 40 (4. 1%) Beaded needle 112 (12%) Plastic object 70 (7. 6%) Metal object 12 (1. 2%) Stone Cement powder 4 (0. 4%)
• • Tamarind seed – thick – grasping easy Peanut – may come But groundnuts – difficult to grasp Sitaphal seed – vertical or horizontal – then grasping chances may change
Tricks of symptoms ! • organic foreign bodies are more inducive to inflammatory reactions and symptoms of fever and pneumonia are observed more frequently. • Some organic foreign materials may swell due to fluid absorption after aspiration and the partial blockage can become total in time.
How to confirm ? • Plain X‑ray of the chest can reveal • • • obstructive emphysema. Pneumonitis, collapse Pulmonary infections normal finding( radiolucent FBs )
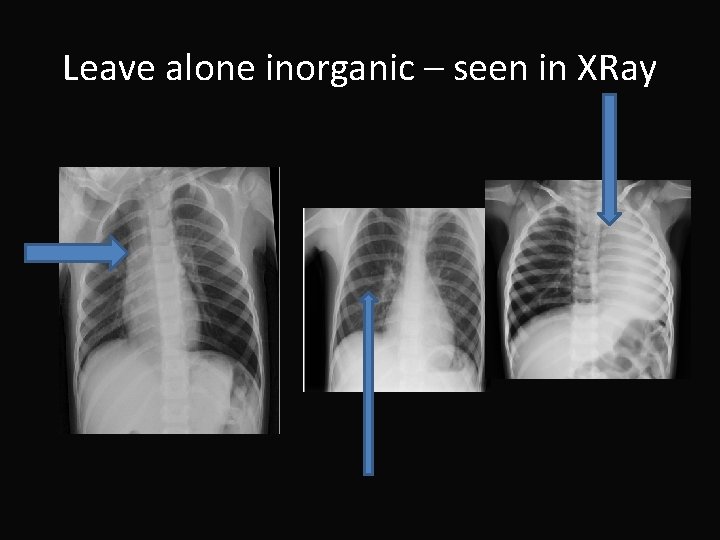
Leave alone inorganic – seen in XRay
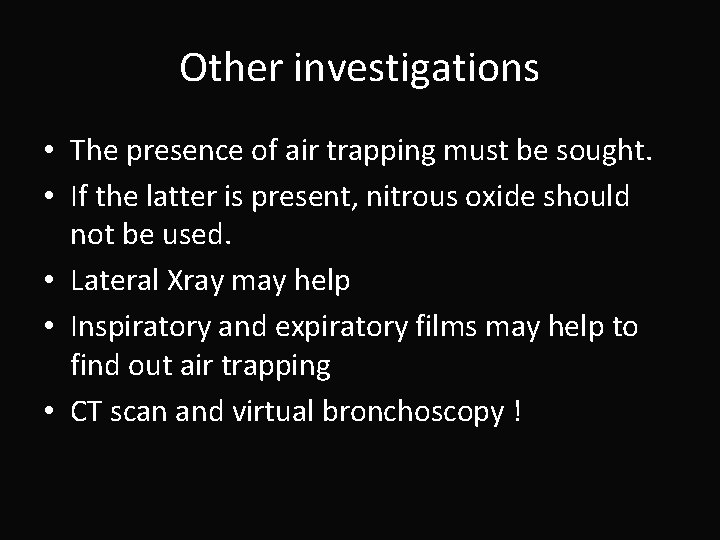
Other investigations • The presence of air trapping must be sought. • If the latter is present, nitrous oxide should not be used. • Lateral Xray may help • Inspiratory and expiratory films may help to find out air trapping • CT scan and virtual bronchoscopy !
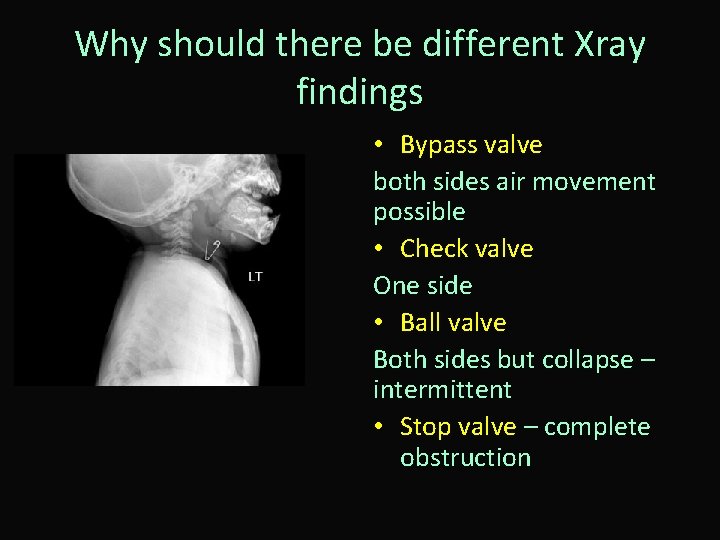
Why should there be different Xray findings • Bypass valve both sides air movement possible • Check valve One side • Ball valve Both sides but collapse – intermittent • Stop valve – complete obstruction
• Bronchoscopy • Rigid is the gold standard • Flexible scopes – less invasive – may not need GA – can go upto distal airways – • Skill necessary • Ideal size for bronchus and the larynx
• If bronchoscopy is not urgent, the patients should be fasted for at least 6 hours for solids and 2 hours for clear fluids to decrease the risk of aspiration during the procedure • Planning • Intercommunication between surgeon • Surgeon takes control of the airway – not us
Preop features • A stridor present only during inspiration suggests an extrathoracic obstruction; if the stridor is expiratory then an intrathoracic cause is likely. • • Investigations ? Think of the physical and chemical damage Antibiotics – must Steroids and humidified oxygen – preferred by many
As an emergency ? • The child should be allowed to clear the obstruction by coughing and observed for worsening of airway obstruction. If the airway obstruction is severe (the child is unable to make a sound), the child should receive sub diaphragmatic abdominal thrusts (Heimlich maneuver). • Infants should receive five back blows followed by five chest thrusts repeatedly until the object is expelled
Danger of heimlich • Use of the Heimlich maneuver has improved the mortality rate of patients with complete airway obstruction, • but use of it in patients with partial obstruction may produce complete obstruction • Subglottic Fbs – ideal for Heimlich
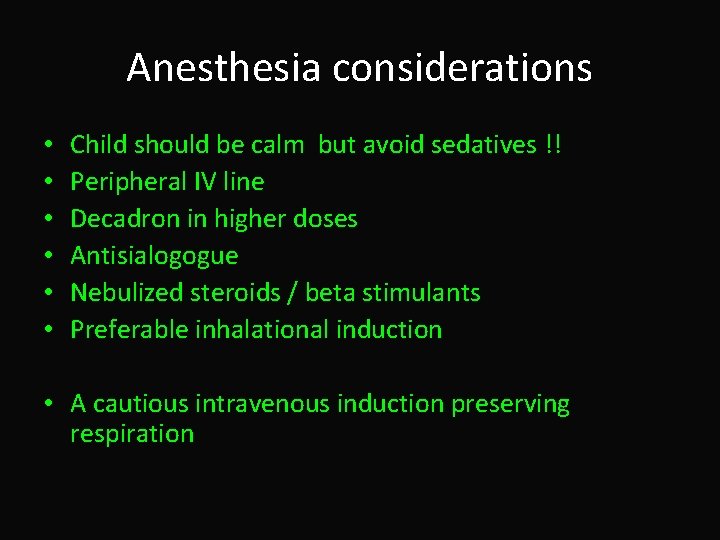
Anesthesia considerations • • • Child should be calm but avoid sedatives !! Peripheral IV line Decadron in higher doses Antisialogogue Nebulized steroids / beta stimulants Preferable inhalational induction • A cautious intravenous induction preserving respiration
• Superficial foreign bodies • Upper airway • Short procedures • Need not paralyse
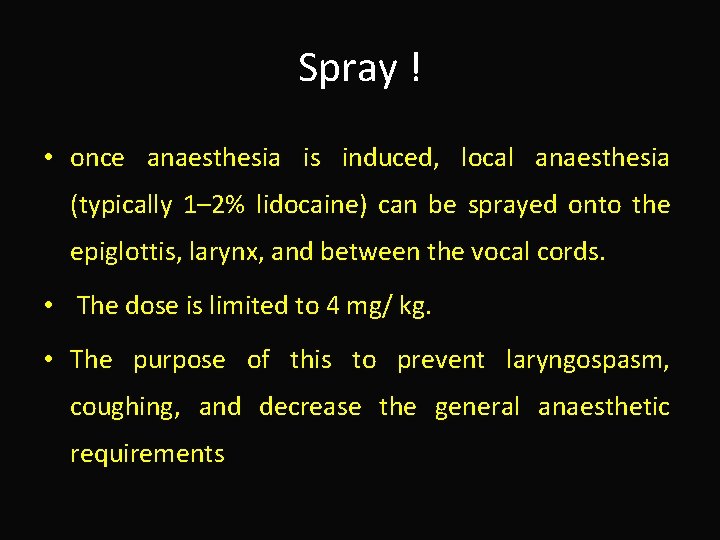
Spray ! • once anaesthesia is induced, local anaesthesia (typically 1– 2% lidocaine) can be sprayed onto the epiglottis, larynx, and between the vocal cords. • The dose is limited to 4 mg/ kg. • The purpose of this to prevent laryngospasm, coughing, and decrease the general anaesthetic requirements
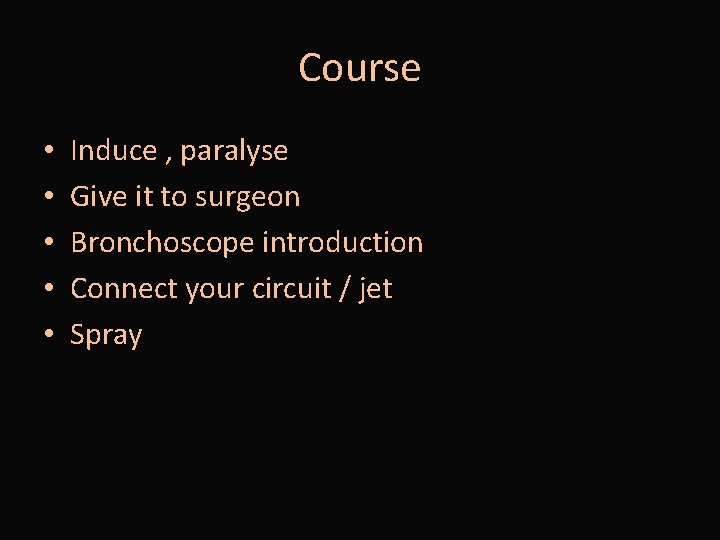
Course • • • Induce , paralyse Give it to surgeon Bronchoscope introduction Connect your circuit / jet Spray
Essentials • • • Pulse oximeter ECG Precordial steth Capnography Symmetrical expansion
• Deeper foreign bodies • Cant locate FBs • More time consuming • May go for paralysis
If we start paralysis – three things to come to our mind !! • Oxygenation • Ventilation • Anaesthesia • Surgical exposure
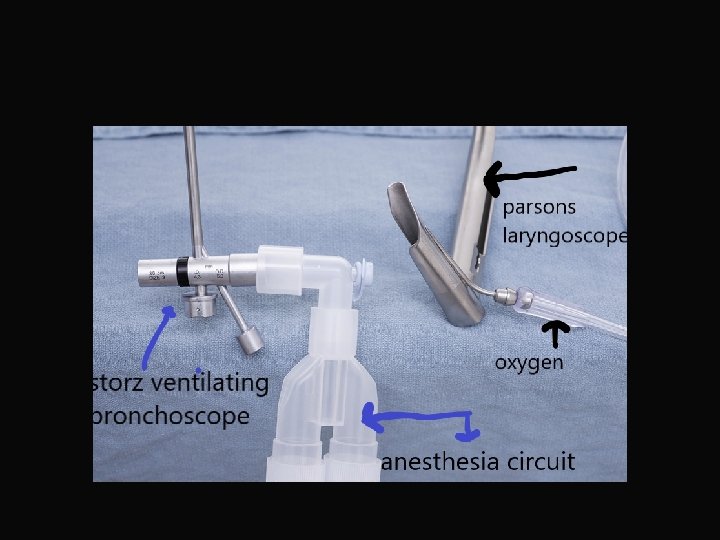
Options • Controlled GA with muscle paralyses • With ventilating bronchoscope • • Leaks Will we able to do in certain FBs Will we be pushing distal ? Waste and pollution – gases
Advantages • include the ability to provide optimal oxygenation and ventilation during the breathing phase • assurance of lack of patient movement to airway manipulation.
spontaneous ventilation • continuous ventilation is occurring, despite interruptions in the anesthesia breathing circuit. • For some obstructive lesions, negative-pressure breathing may provide better oxygenation and ventilation.
Disadvantages • Requirement to maintain a sufficient depth of anesthesia to obliterate airway reflexes and prevent patient movement • during instrumentation, yet maintain sufficient ventilatory function and hemodynamic stability. • Resistance of the system • Leaks and higher flows • Topical anesthesia to the airway is an important component of this technique
Spontaneous ? ? • The child develops a more negative pressure to overcome the resistance • It cant expel the exhaled gases in time as the elastic recoil may be insufficient • trapping and stacking will occur. • This is often confirmed by a tracheal “whoosh” as the bronchoscopist removes the telescope and the trapped gas in the overinflated lung escapes
See the next technique • Many a time • A Propofol infusion • Or • A Remifentanil infusion with or without agents may be needed to maintain anaesthesia
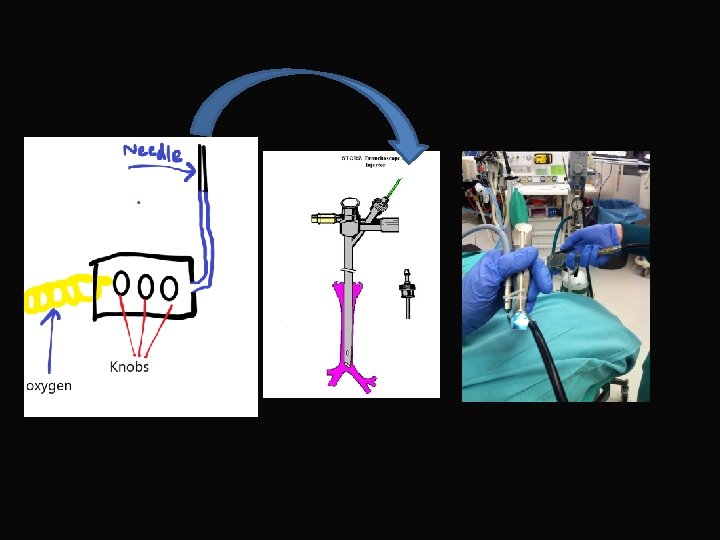
Jet ventilation through the bronchoscope • Only oxygenation is possible • We have to see that carbon-dioxide is getting excreted through the sides of the scope • As soon as the surgery begins with manipulation of the FB and swelling • Oxygenation • Symmetrical expansion
What to adjust in jet ventilator • There are three control knobs – • inspiratory pressure, • inspiratory time, • and expiratory time. • The flow is continuous and arbitrary adjustments were done with the three knobs so that chest expansion was satisfactory. The volume delivered and rate was monitored clinically by looking at the chest.
• Oxygen through the jet • Carbondioxide through the sides of the scope • TIVA

During recovery • Sometimes the surgeon will remove the FB • Entrainment will be big • Surgeon will remove the scope with FB • Put in the tube and ventilate with circuit • When the peanut is bigger, during picking and removal , it may drop down to complete obstruction. • Some use nebulized adrenaline immediate post op
Intraoperative complications • • • hypoxia, hypercarbia, hypotension Arrhythmias Cannot find FB Bleeding – rarely dangerous Awareness Injuries during extirpation of the FB
Worried about hypoxemia If the scope is placed in a bronchus, hypoxia may occur despite the presence of the side ports and the scope may need to be repeatedly withdrawn. • Excessive suctioning will remove gases including oxygen and cause increased atelectasis. • Bronchospasm – may be inadequate anesthesia (sometimes bucking) • Hypoxia due to improper jet • Bradycardia due to hypoxia or otherwise
Chen et al identified the following risk factors for hypoxemia: • • • Patient age (younger more likely), FB type (plant seed), surgical duration, preexisting pneumonia, spontaneous ventilation
Clinical tips • operating theater assistant as they have control over the forceps or the basket. • The mortality of TFBs ranged from 0. 21% to 3% in a few studies according to other studies which was 0. 13%. • children should be forbidden running or jumping ? Talking when eating nuts to avoid TFBs inhalation.
Intubation after FB removal in paralysed patients • Tracheal intubation allows tracheobronchial suction, • lung expansion, • and oxygenation and ventilation until adequate reversal of muscle relaxation and return to spontaneous breathing.
Other options • Life saving measure • Establishment of airway with either a surgical or a percutaneous cricothyrotomy • patients needed pulmonary resection because of irreversible pulmonary damage such as bronchiectasis and destroyed lung.
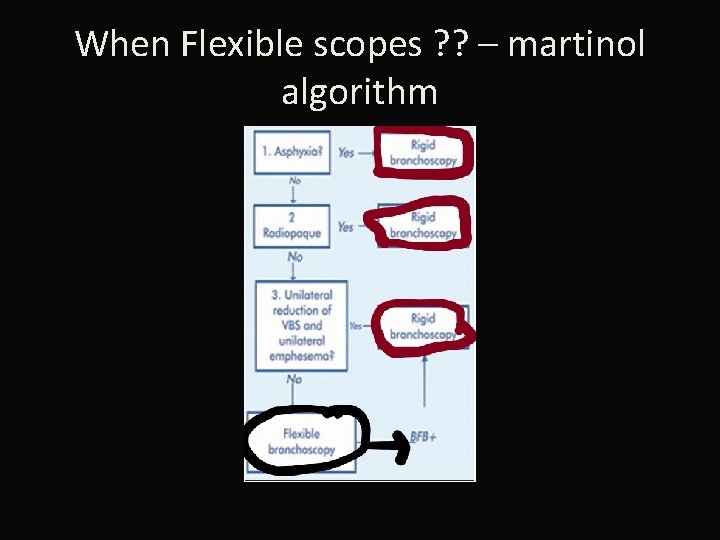
When Flexible scopes ? ? – martinol algorithm
In the post op • Check bronchoscopy after FB removal • Post operative antibiotics and steroids • A chest X-ray at 6 -8 hours postbronchoscopy to assess lung expansion and exclude a pneumothorax and residual foreign body
Summary • • Age and why Types of FB Symptoms and types of valve Investigations Algorithm Three types of anesthetic management Intra op problems Post op problems
Thank you all
- Slides: 50