Anesthetic management of a patient requiring placement of

- Slides: 34
Anesthetic management of a patient requiring placement of a Y- stent Presented by 林起翎 蔡鵠遠 戴家煌

Brief History 呂xx, 61 y/o, male Persistent dry cough since 3 yrs ago. Dyspnea and wheezing on left side down. Tuberculosis was diagnosed at 署立新竹H. He started to receive regular medical therapy. CXR showed a granuloma at LUL on OPD follow-up in Aug. 2001.
He was transferred to Dr. 李元麒‘s OPD in Oct. 2001. Echo-guide biopsy was performed. Pathology report revealed tuberculosis. Sputum culture yielded “Mycobacterium gordonae” in March, 2002. Chest CT-scan showed persisted granuloma in May, 2002.
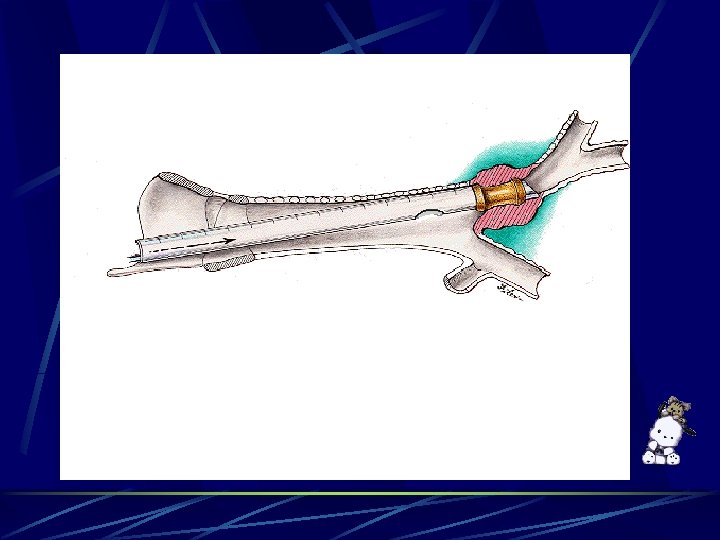
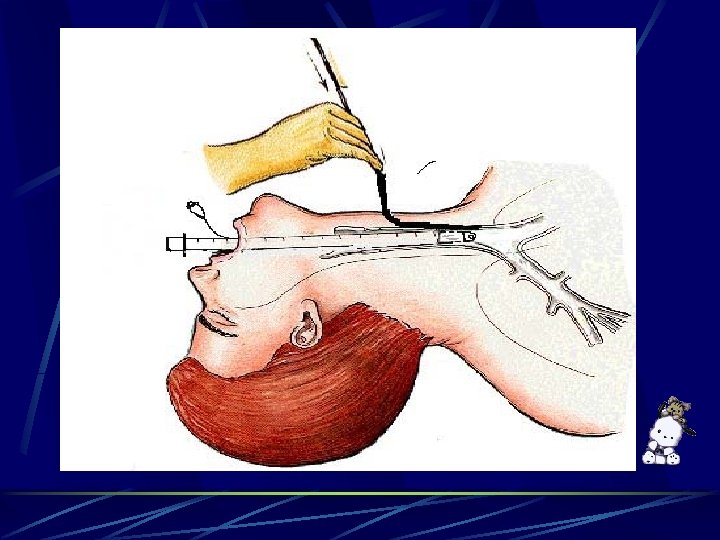
Left main bronchus stenosis was noted. Tracheostomy with left main bronchus dilation was done first on 10/3, 2002. Stenting for left main bronchus was inserted on 10/21, 2002. Productive cough with massive sputum was noted after he was discharged on 10/26. He was admitted again and bronchoscope revealed granulation tissue over distal end of the stent on 11/8. Arrange Y-stent on 11/11.
Past History Old MI at 4 years ago DM(-), HTN(-), other systemic dz. (-) No known food or drug allergy Smoking(+), quitted for 3 yrs Alcohol(-), betel nut(-) Family history:non-contributory Previous operation history:tracheostomy and stenting
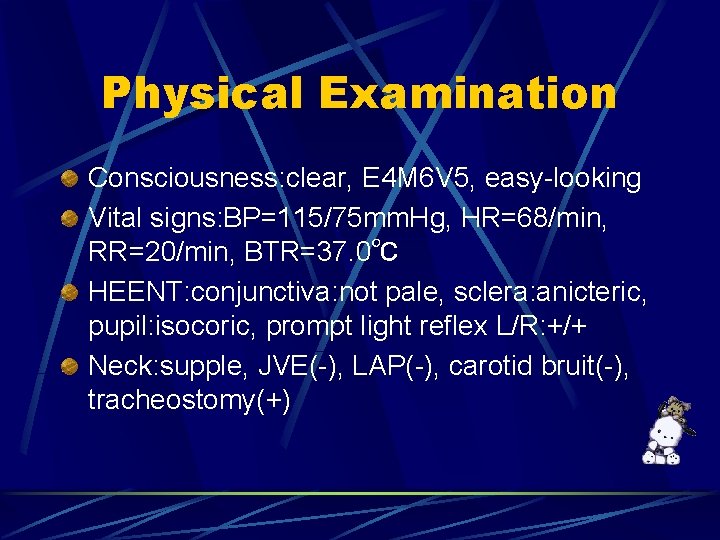
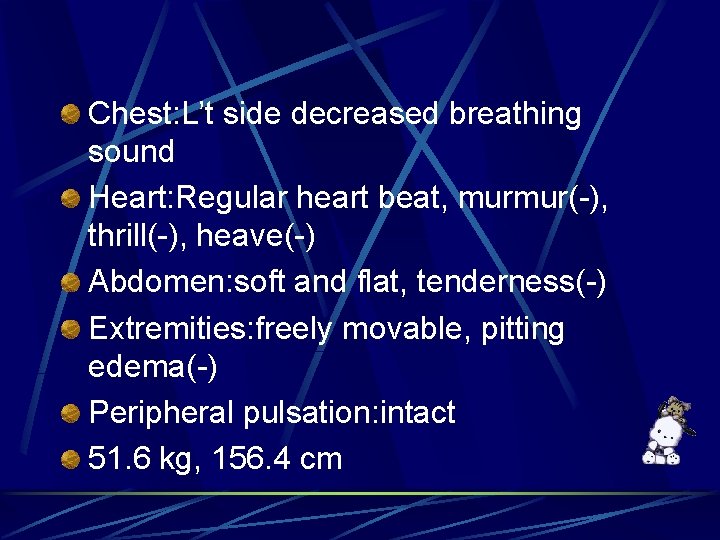
Physical Examination Consciousness: clear, E 4 M 6 V 5, easy-looking Vital signs: BP=115/75 mm. Hg, HR=68/min, RR=20/min, BTR=37. 0℃ HEENT: conjunctiva: not pale, sclera: anicteric, pupil: isocoric, prompt light reflex L/R: +/+ Neck: supple, JVE(-), LAP(-), carotid bruit(-), tracheostomy(+)
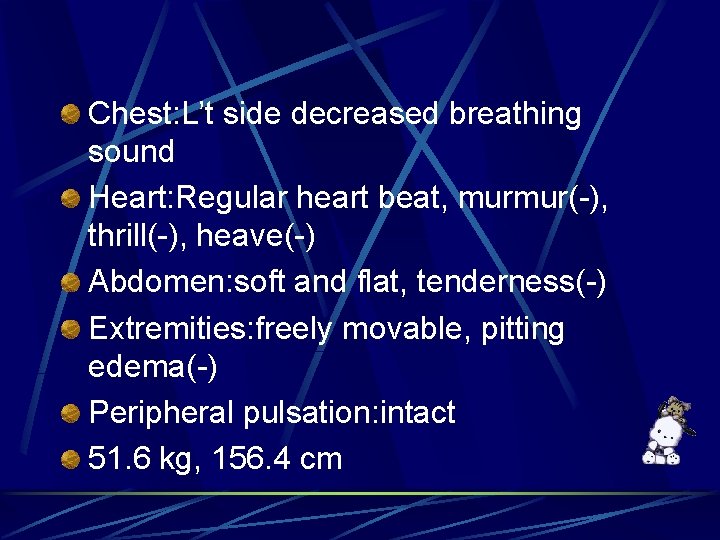
Chest: L’t side decreased breathing sound Heart: Regular heart beat, murmur(-), thrill(-), heave(-) Abdomen: soft and flat, tenderness(-) Extremities: freely movable, pitting edema(-) Peripheral pulsation: intact 51. 6 kg, 156. 4 cm
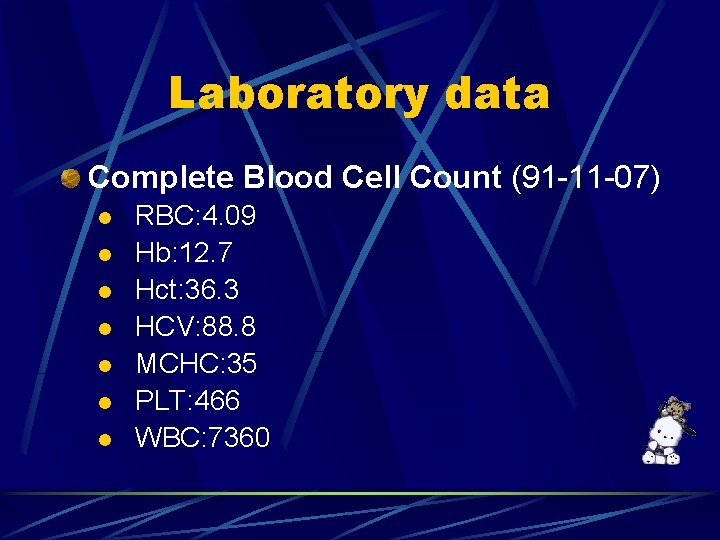
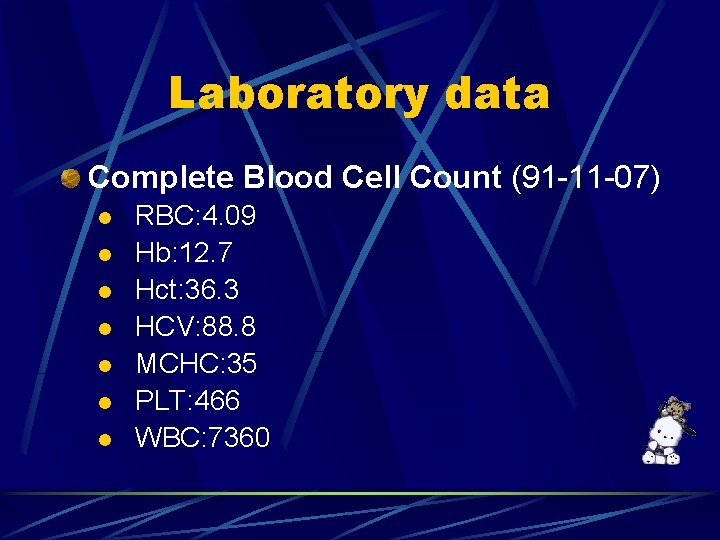
Laboratory data Complete Blood Cell Count (91 -11 -07) RBC: 4. 09 l Hb: 12. 7 l Hct: 36. 3 l HCV: 88. 8 l MCHC: 35 l PLT: 466 l WBC: 7360 l
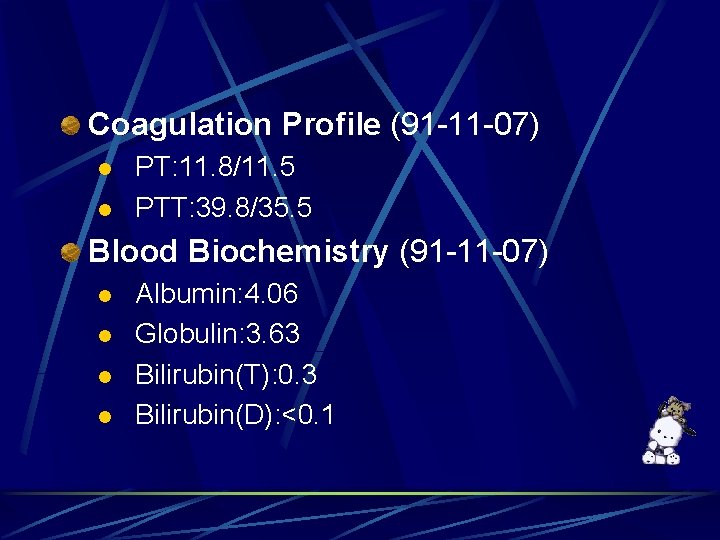
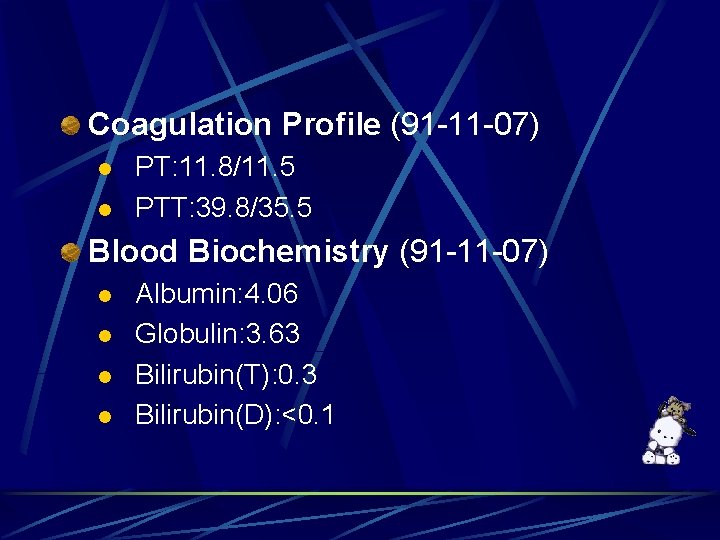
Coagulation Profile (91 -11 -07) PT: 11. 8/11. 5 l PTT: 39. 8/35. 5 l Blood Biochemistry (91 -11 -07) Albumin: 4. 06 l Globulin: 3. 63 l Bilirubin(T): 0. 3 l Bilirubin(D): <0. 1 l
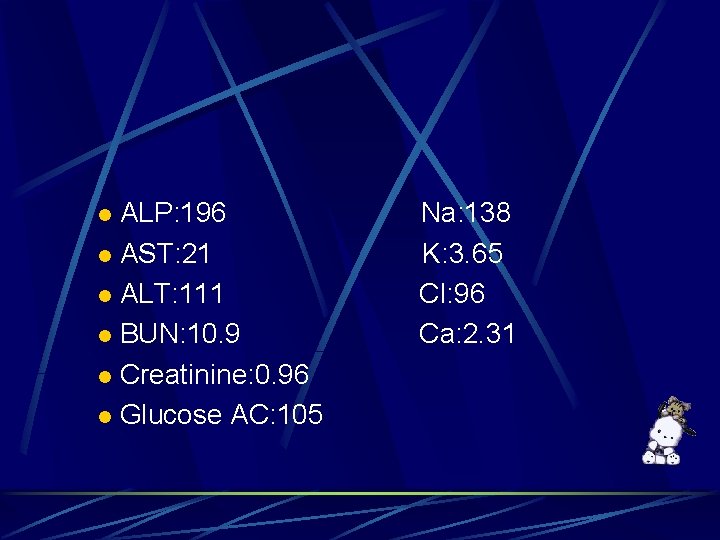
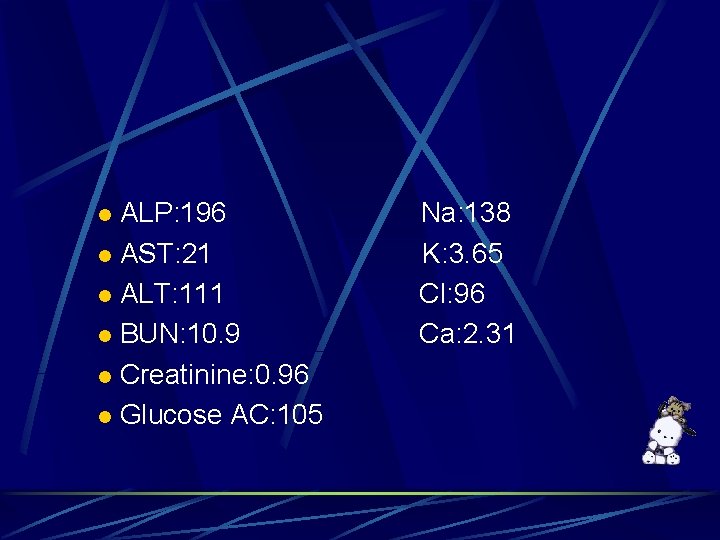
ALP: 196 Na: 138 l AST: 21 K: 3. 65 l ALT: 111 Cl: 96 l BUN: 10. 9 Ca: 2. 31 l Creatinine: 0. 96 l Glucose AC: 105 l
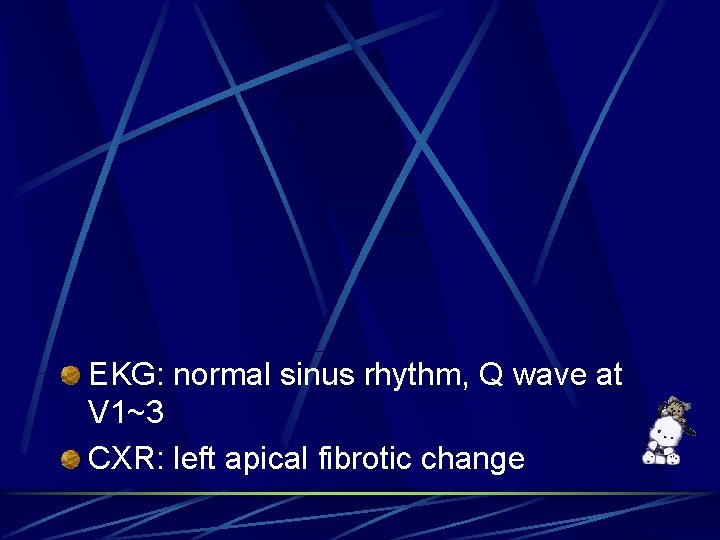
EKG: normal sinus rhythm, Q wave at V 1~3 CXR: left apical fibrotic change
Anesthesia IVA
Monitor EKG , BP , A line , 2 IV line end-tidal CO 2 , pulse oxymeter Urinary output
Induction: Fentanyl: 1 ml Pentothal: 250 mg Atracurium: 25 mg Xylocaine: 100 mg Robinul: 0. 2 mg Nitroderm: 1 TTS Vitacal: 1 amp Maintenance: IV propofol infusion: 50~100 mg/h
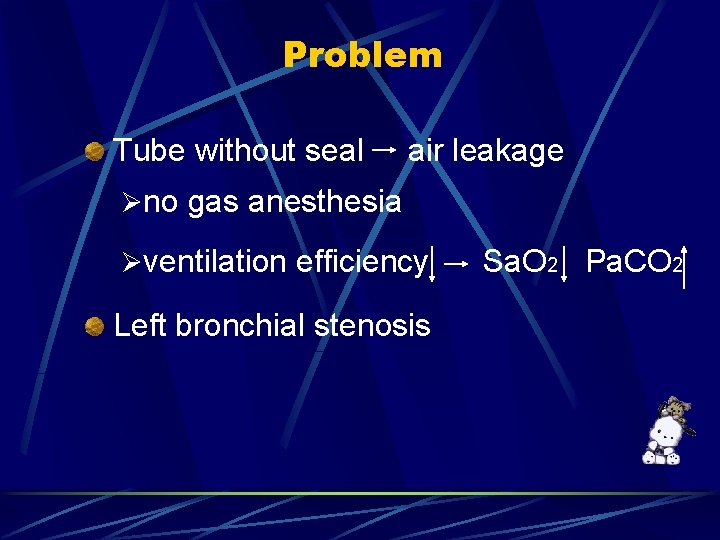
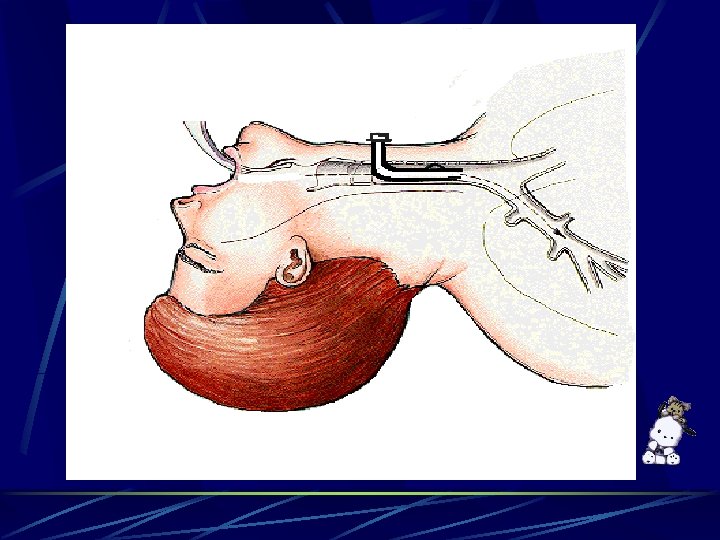
Problem Tube without seal air leakage Øno gas anesthesia Øventilation efficiency Sa. O 2 Pa. CO 2 Left bronchial stenosis
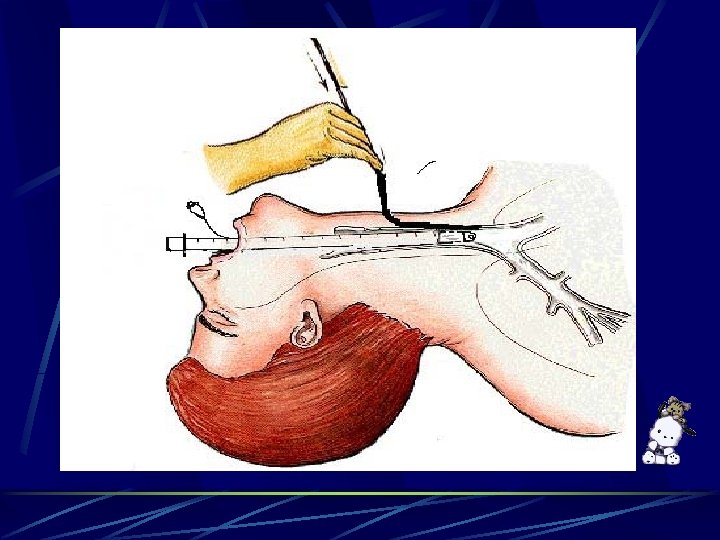
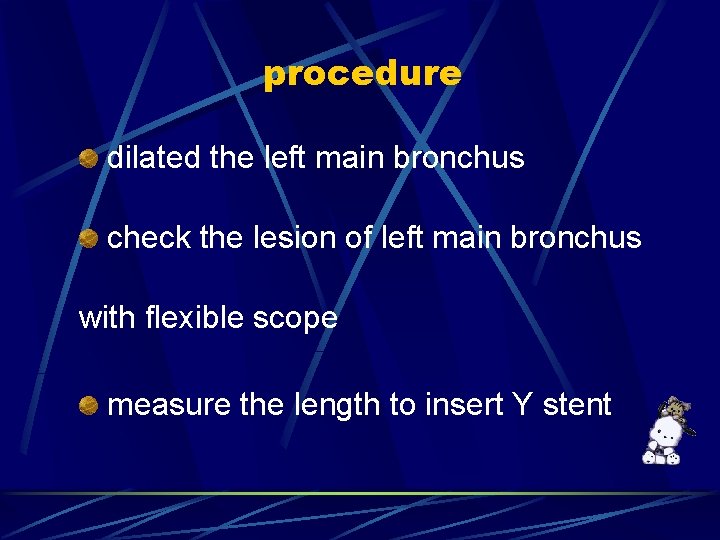
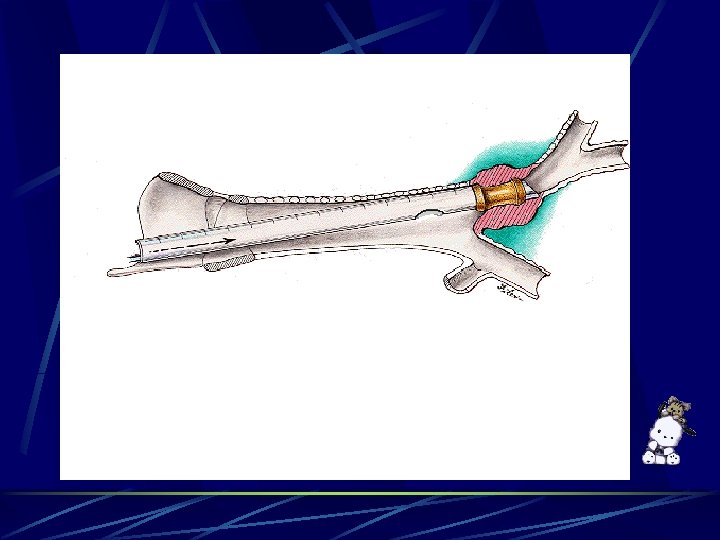
procedure dilated the left main bronchus check the lesion of left main bronchus with flexible scope measure the length to insert Y stent
Problem Tube without seal air leakage Øno gas anesthesia Øventilation efficiency Sa. O 2 Pa. CO 2 Irritation of airway Ølaryngospasm, bronchospasm ØHR BP
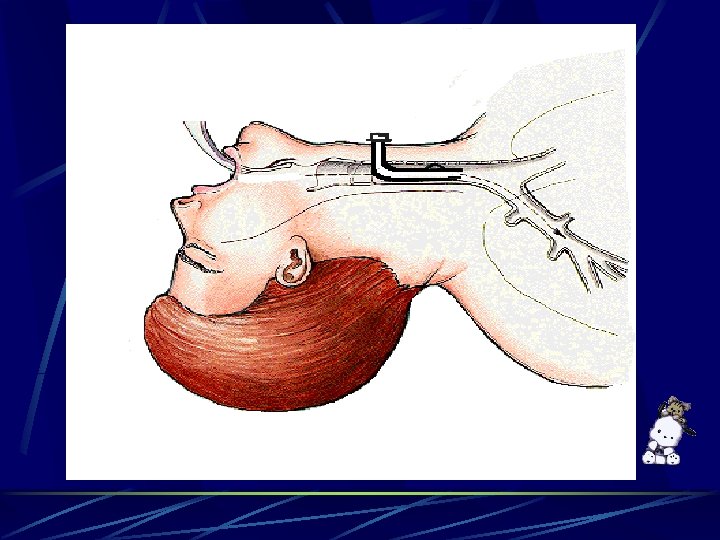
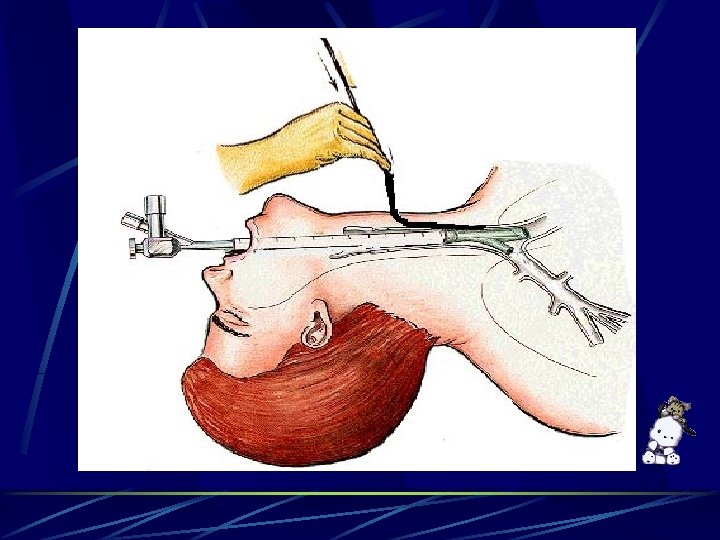
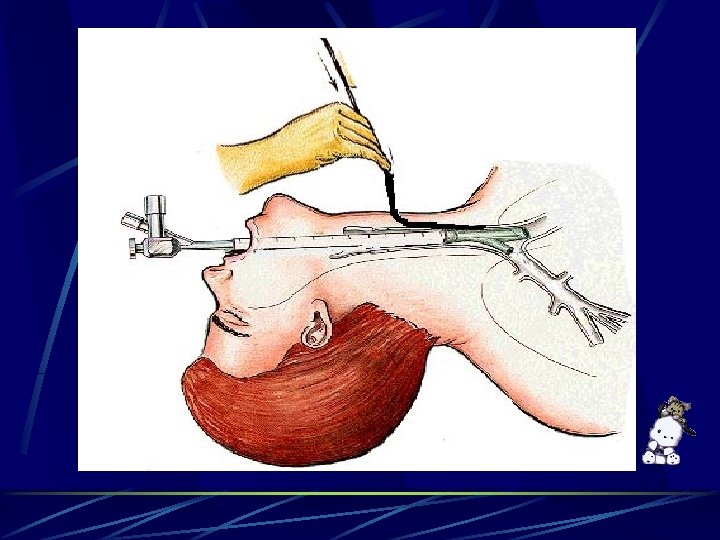
procedure Remove the granulation tissue and blood clot 13 mm Y stent insertion by rigid bronchoscope Adjust Y stent position via tracheostomy tube under flexible scope guide
Problem Apnea: O 2 supply via side hole of rigid bronchoscope ØSa. O 2: 99% 92% in about 5 mins Irritation of airway Ølaryngospasm, bronchospasm ØHR BP : BP up to 180/110
Problem Blood clot and debris: lower airway obstruction
Major Problems T. B. Poor ventilation efficiency upper airway leakage lower airway obstruction Apnea during procedure Surgical airway manipulation is a strong stimulus resulting in bronchospasm Blood clot and debris: lower airway obstruction
Discussion Airway management ventilation l laryngospasm and bronchospasm l bleeding due to surgical manipulation l Tuberculosis
Ventilation Intermittent ventilation Closely monitor Avoid continuous positive pressure ventilation l increased intrathoracic pressure
Laryngospasm Anesthetic depth should be adjusted If laryngospasm occurs Remove the offending stimulus l Give 100% oxygen l Increase anesthetic depth l Succinylcholine l
Bronchospasm Intravenous aminophylline or salbutamol Volatile anesthetic agents and ketamine are also effective bronchodilators Epinephrine is indicated in lifethreatening situations
Bleeding during surgery Suction One lung intubation
Anesthesia in patients with TB Delay elective surgical procedures until no longer considered infectious Perform tracheal intubation in a negative pressure environment Place a high efficiency particulate air filter between the Y-connector and mask or tracheal tube
Place bacterial filters on the exhalation limb of the anesthesia delivery circuit Use a dedicated mechanical ventilator Postoperative care in an isolation room
Conclusion O 2 saturation Anesthetic depth
Thank you for your attention!
 Anesthetic machine parts
Anesthetic machine parts Anesthetic, pungent, sweet
Anesthetic, pungent, sweet Virtual memory meaning
Virtual memory meaning Industries requiring compulsory licensing *
Industries requiring compulsory licensing * Excellent choice for systems requiring high reliability
Excellent choice for systems requiring high reliability Sdlc vs slc
Sdlc vs slc Patient 2 patient
Patient 2 patient Types of contract in spm
Types of contract in spm Sap patient management
Sap patient management Treatment of ocd
Treatment of ocd Chapter 20 patient collections and financial management
Chapter 20 patient collections and financial management Resource patient management system
Resource patient management system Preoperative nursing care for cataract surgery
Preoperative nursing care for cataract surgery Patient management problem
Patient management problem Patient blood management definition
Patient blood management definition Nursing diagnosis of retinal detachment slideshare
Nursing diagnosis of retinal detachment slideshare Hospital management system web application
Hospital management system web application Patient safety incident management system
Patient safety incident management system Disuse syndrome
Disuse syndrome Top management and middle management
Top management and middle management Management pyramid
Management pyramid Top management and middle management
Top management and middle management Zoll e learning
Zoll e learning Math 155 wvu
Math 155 wvu Go2 work placement
Go2 work placement El sr. ortega / inteligente / es / profesor / un
El sr. ortega / inteligente / es / profesor / un Awana t&t badge placement
Awana t&t badge placement Gwar sdsu
Gwar sdsu Arterial line placement
Arterial line placement Uva calculus placement test
Uva calculus placement test Cadet badges placement
Cadet badges placement Tongue placement for r
Tongue placement for r Pept meaning
Pept meaning Erf placement test
Erf placement test Intraosseous meaning
Intraosseous meaning