Anesthetic Implications for the Physiological Changes in Pregnancy

- Slides: 35
Anesthetic Implications for the Physiological Changes in Pregnancy & Basic FHR Monitoring J. E. Pellegrini, CRNA, Ph. D
Changes during the Puerperium z. Changes to anatomy & physiology y. Most changes to physiology occur during the 1 st trimester y. Most changes to anatomy occur during the 2 nd and 3 rd trimester y. Many of the changes are beneficial x. As an anesthetist you must have a good understanding of these changes and so that you can determine if they will have an impact on your anesthetic management
Physiological Changes of Pregnancy Primarily we’ll discuss: z Respiratory Changes z Cardiovascular Changes z GI/Hepatic/Renal Changes z Changes in Neural network (metabolism)
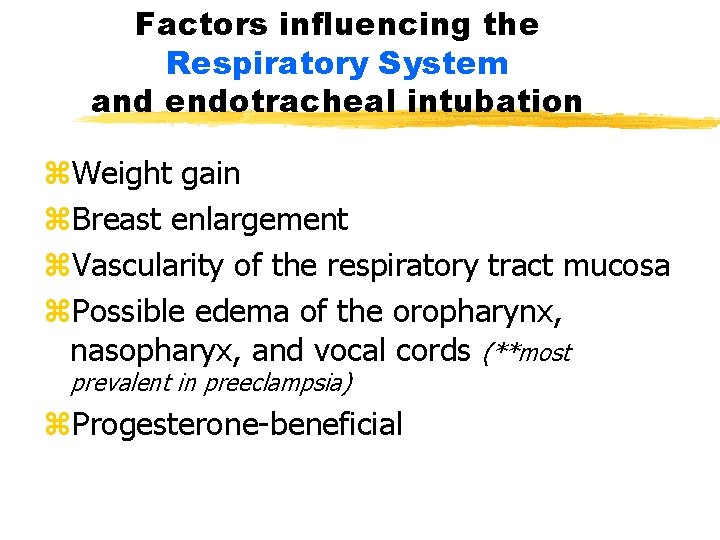
Factors influencing the Respiratory System and endotracheal intubation z. Weight gain z. Breast enlargement z. Vascularity of the respiratory tract mucosa z. Possible edema of the oropharynx, nasopharyx, and vocal cords (**most prevalent in preeclampsia) z. Progesterone-beneficial
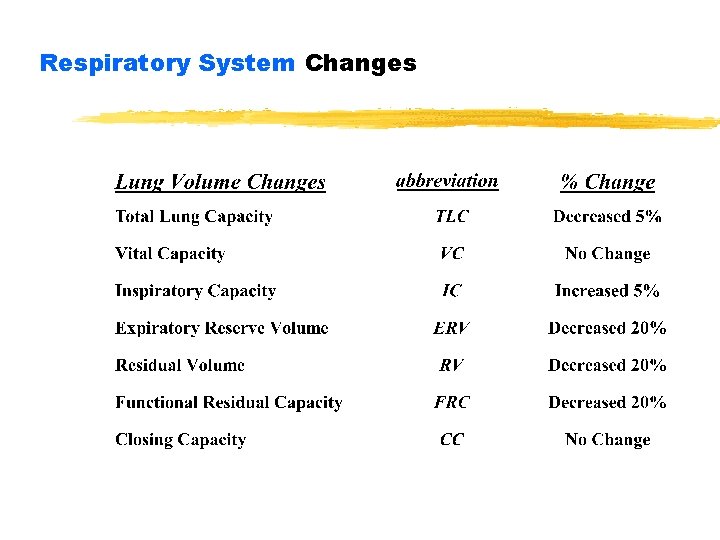
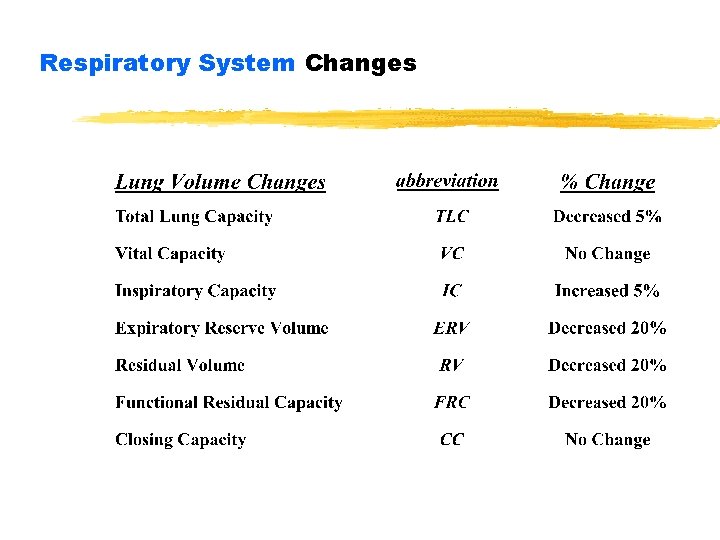
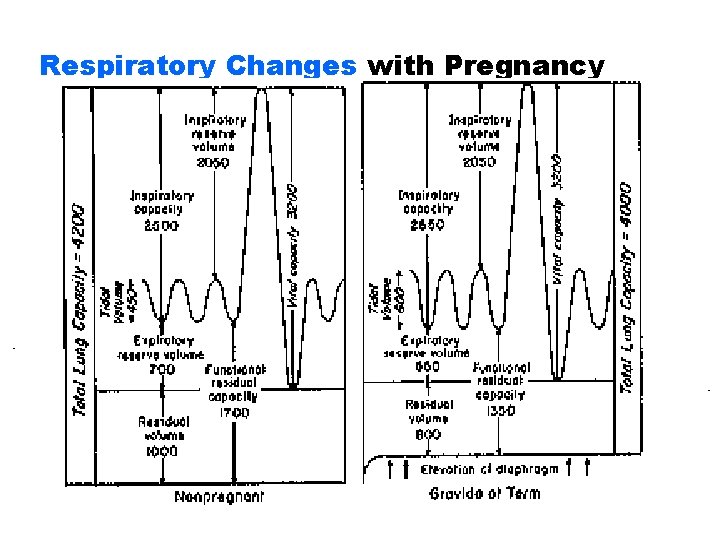
Respiratory System Changes
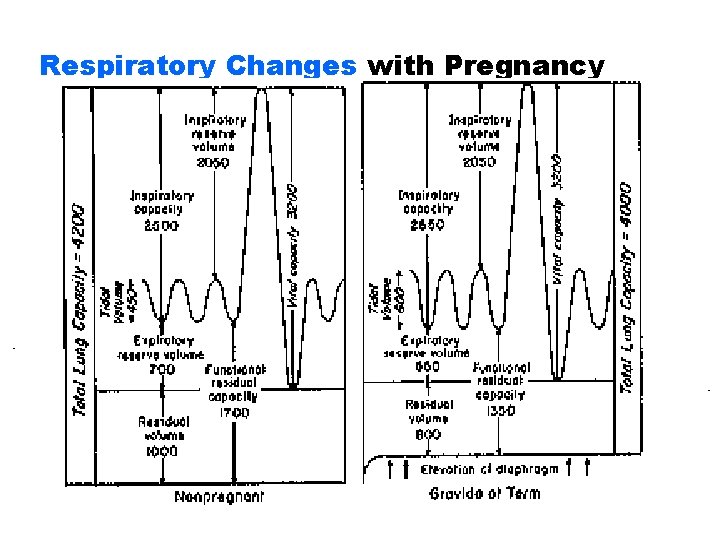
Respiratory Changes with Pregnancy
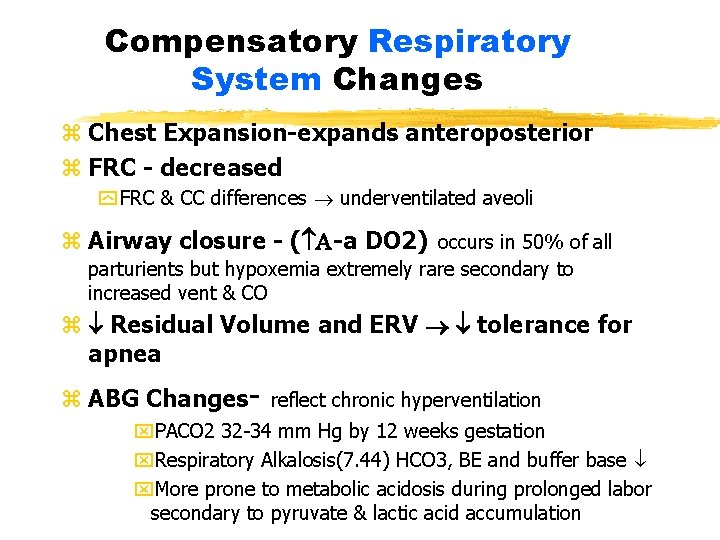
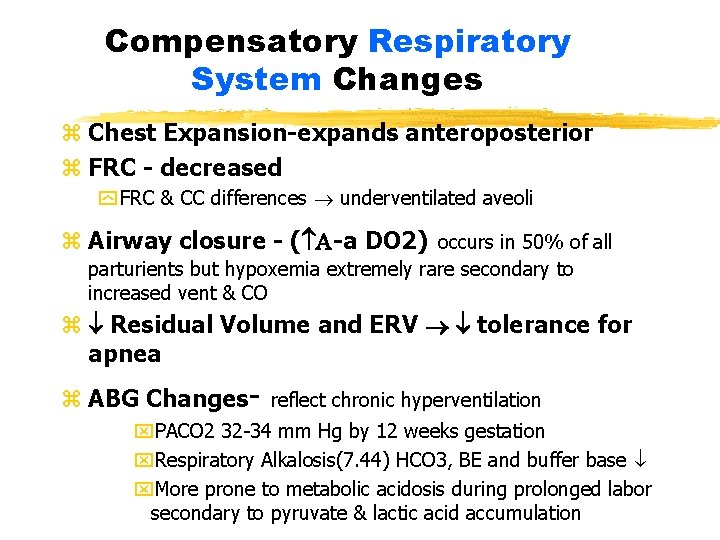
Compensatory Respiratory System Changes z Chest Expansion-expands anteroposterior z FRC - decreased y FRC & CC differences underventilated aveoli z Airway closure - ( -a DO 2) occurs in 50% of all parturients but hypoxemia extremely rare secondary to increased vent & CO z Residual Volume and ERV tolerance for apnea z ABG Changes- reflect chronic hyperventilation x. PACO 2 32 -34 mm Hg by 12 weeks gestation x. Respiratory Alkalosis(7. 44) HCO 3, BE and buffer base x. More prone to metabolic acidosis during prolonged labor secondary to pyruvate & lactic acid accumulation
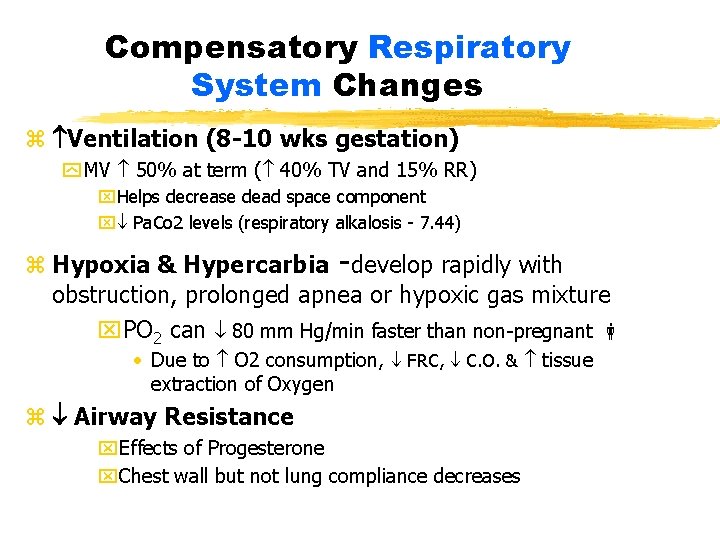
Compensatory Respiratory System Changes z Ventilation (8 -10 wks gestation) y MV 50% at term ( 40% TV and 15% RR) x. Helps decrease dead space component x Pa. Co 2 levels (respiratory alkalosis - 7. 44) z Hypoxia & Hypercarbia -develop rapidly with obstruction, prolonged apnea or hypoxic gas mixture x. PO 2 can 80 mm Hg/min faster than non-pregnant • Due to O 2 consumption, FRC, C. O. & tissue extraction of Oxygen z Airway Resistance x. Effects of Progesterone x. Chest wall but not lung compliance decreases
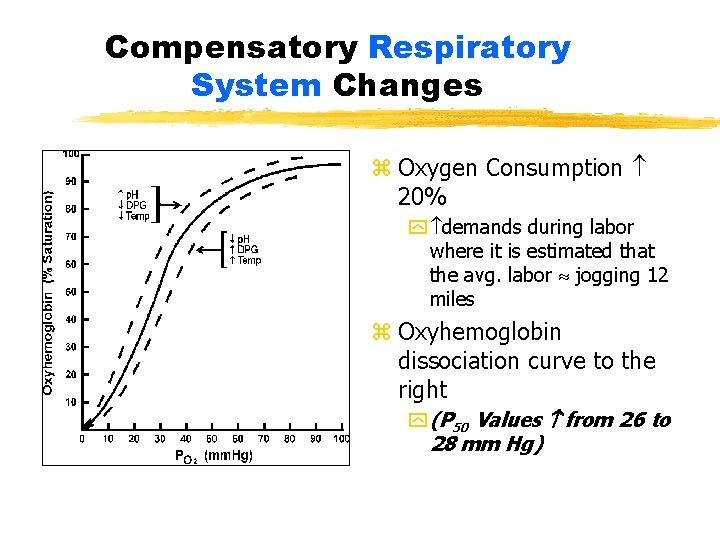
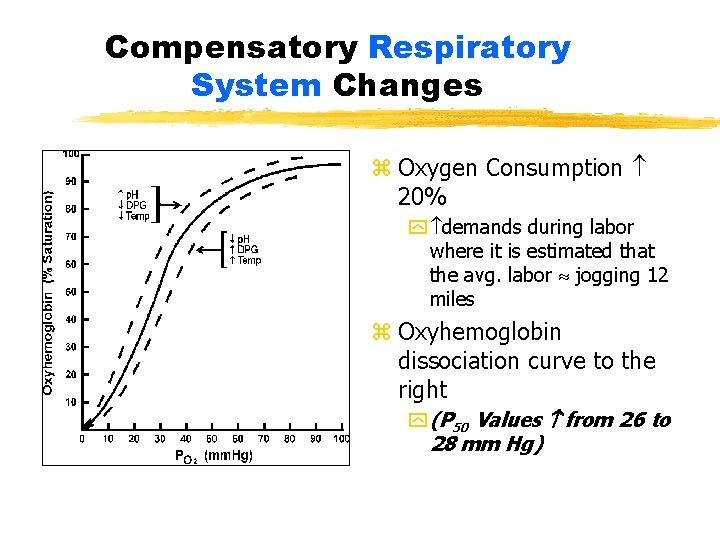
Compensatory Respiratory System Changes z z Oxygen Consumption 20% y demands during labor where it is estimated that the avg. labor jogging 12 miles z Oxyhemoglobin dissociation curve to the right y (P 50 Values from 26 to 28 mm Hg)
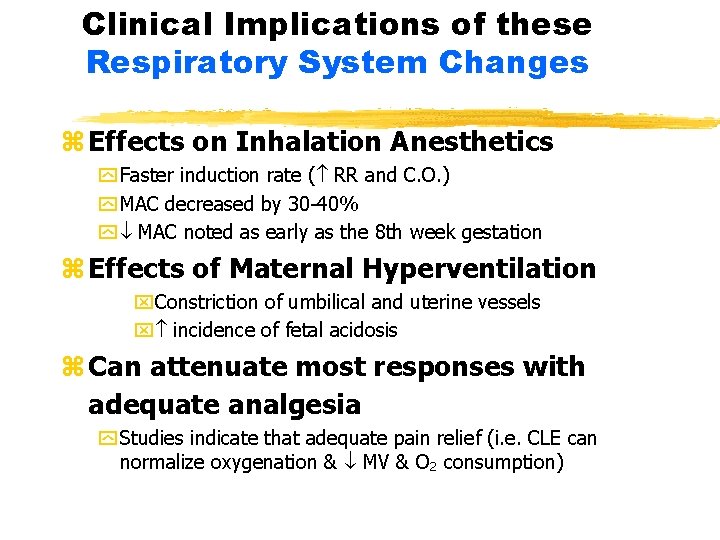
Clinical Implications of these Respiratory System Changes z Effects on Inhalation Anesthetics y Faster induction rate ( RR and C. O. ) y MAC decreased by 30 -40% y MAC noted as early as the 8 th week gestation z Effects of Maternal Hyperventilation x. Constriction of umbilical and uterine vessels x incidence of fetal acidosis z Can attenuate most responses with adequate analgesia y Studies indicate that adequate pain relief (i. e. CLE can normalize oxygenation & MV & O 2 consumption)
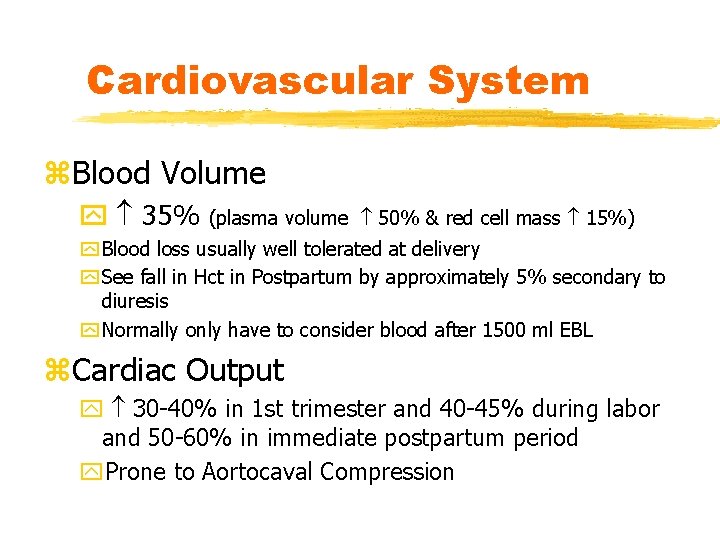
Cardiovascular System z. Blood Volume y 35% (plasma volume 50% & red cell mass 15%) y Blood loss usually well tolerated at delivery y See fall in Hct in Postpartum by approximately 5% secondary to diuresis y Normally only have to consider blood after 1500 ml EBL z. Cardiac Output y 30 -40% in 1 st trimester and 40 -45% during labor and 50 -60% in immediate postpartum period y. Prone to Aortocaval Compression
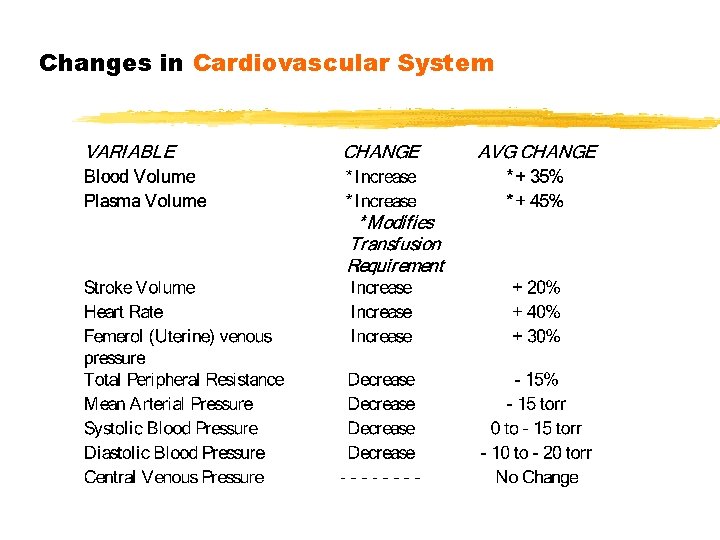
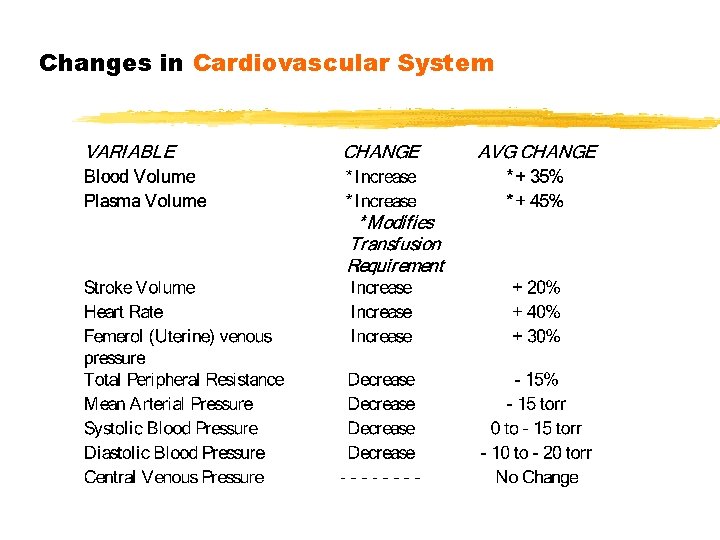
Changes in Cardiovascular System
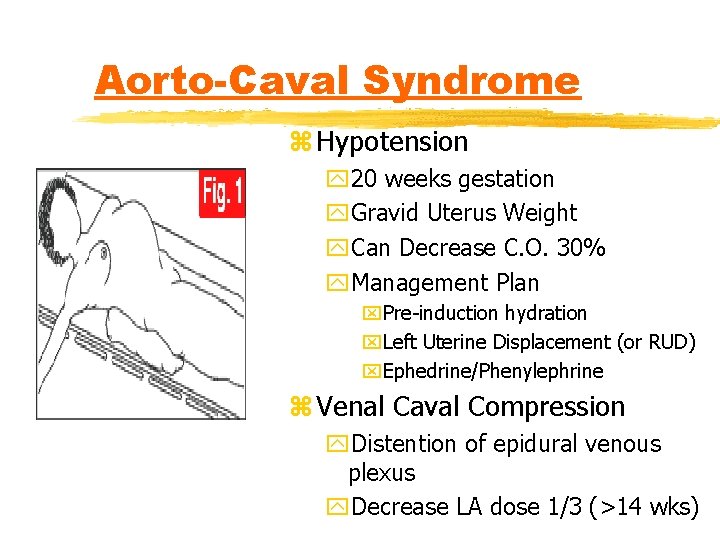
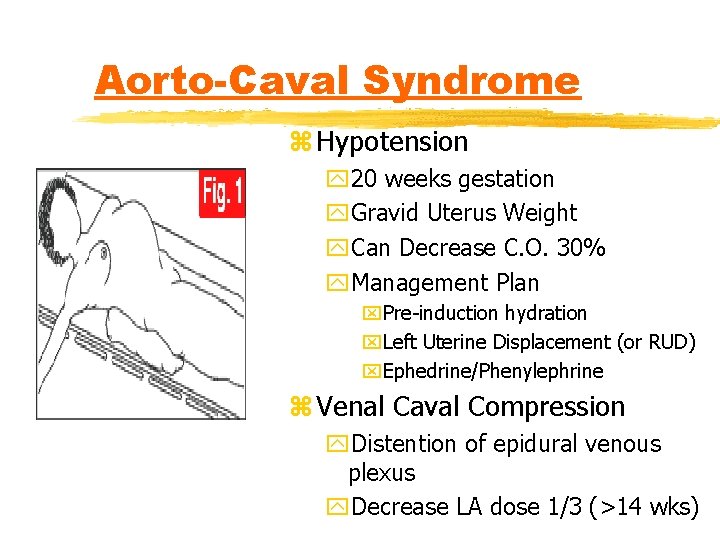
Aorto-Caval Syndrome z Hypotension y 20 weeks gestation y. Gravid Uterus Weight y. Can Decrease C. O. 30% y. Management Plan x. Pre-induction hydration x. Left Uterine Displacement (or RUD) x. Ephedrine/Phenylephrine z Venal Caval Compression y. Distention of epidural venous plexus y. Decrease LA dose 1/3 (>14 wks)
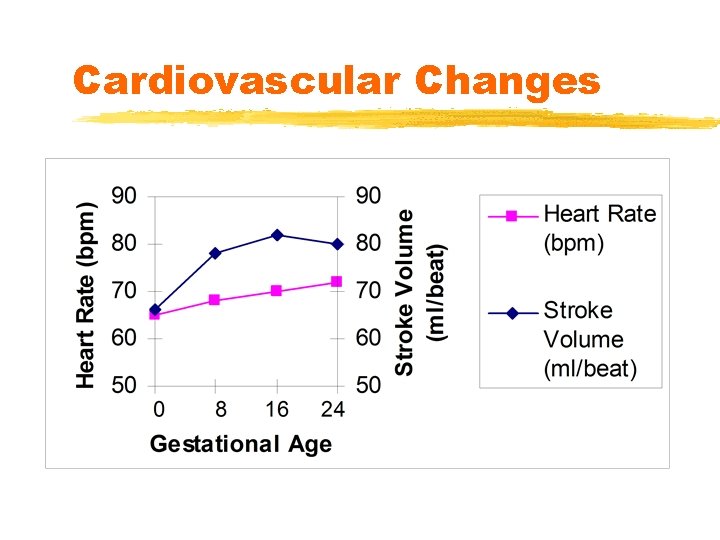
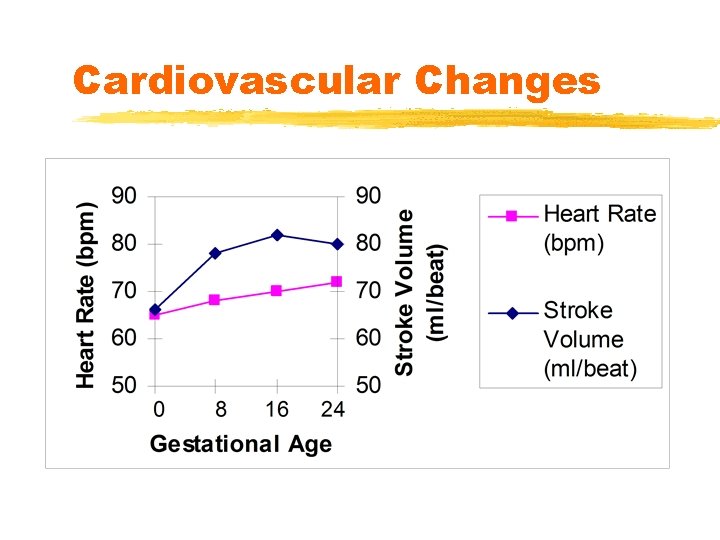
Cardiovascular Changes
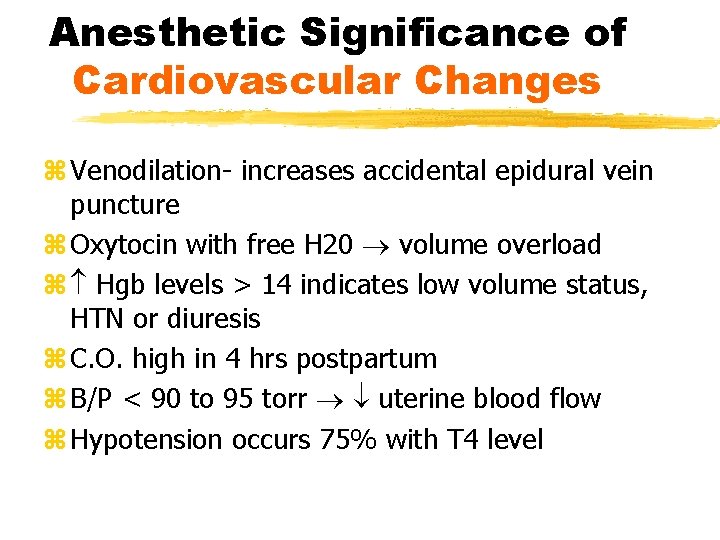
Anesthetic Significance of Cardiovascular Changes z Venodilation- increases accidental epidural vein puncture z Oxytocin with free H 20 volume overload z Hgb levels > 14 indicates low volume status, HTN or diuresis z C. O. high in 4 hrs postpartum z B/P < 90 to 95 torr uterine blood flow z Hypotension occurs 75% with T 4 level
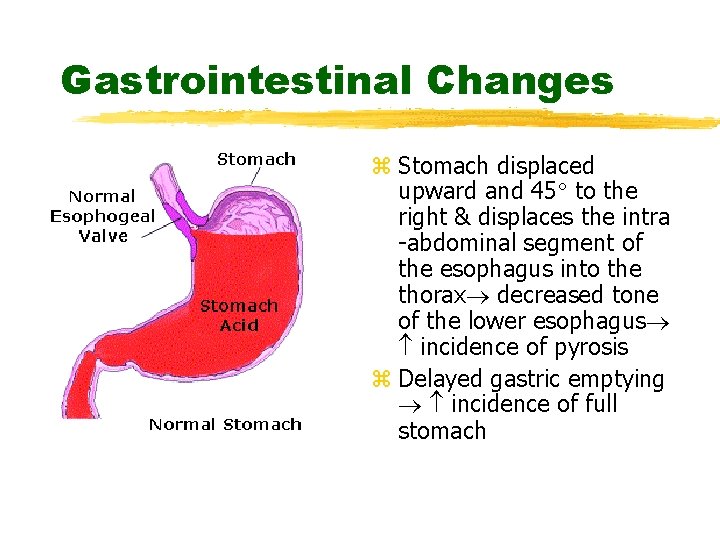
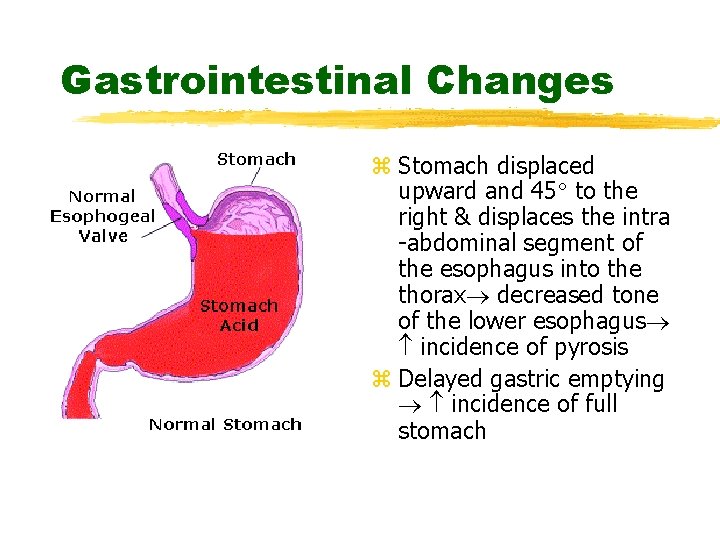
Gastrointestinal Changes z Stomach displaced upward and 45 to the right & displaces the intra -abdominal segment of the esophagus into the thorax decreased tone of the lower esophagus incidence of pyrosis z Delayed gastric emptying incidence of full stomach
Gastrointestinal Changes z Obesity - associated 2 -20 fold in mortality (PIH, IDDM) z Progesterone y Gastrointestinal motility & esophageal sphincter tone z Parturients beyond 18 th week of gestation more prone to vomiting and regurgitation y. Treat as full stomach at 12 th week *put it all together and this spells trouble
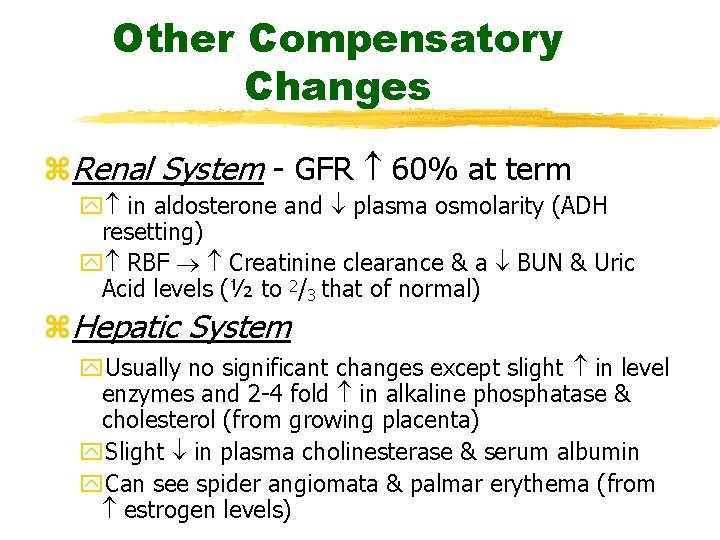
Other Compensatory Changes z. Renal System - GFR 60% at term y in aldosterone and plasma osmolarity (ADH resetting) y RBF Creatinine clearance & a BUN & Uric Acid levels (½ to 2/3 that of normal) z. Hepatic System y. Usually no significant changes except slight in level enzymes and 2 -4 fold in alkaline phosphatase & cholesterol (from growing placenta) y. Slight in plasma cholinesterase & serum albumin y. Can see spider angiomata & palmar erythema (from estrogen levels)
Neuromuscular Changes z. Endorphins z. MAC by 40% z Sedative Effect from Progesterone z Changes in SNS y. See down-regulation y. Altered Response to Catecholamines
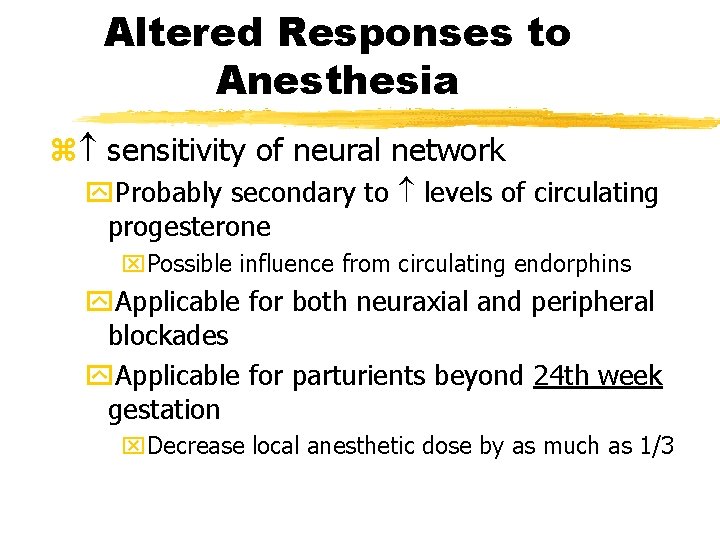
Altered Responses to Anesthesia z sensitivity of neural network y. Probably secondary to levels of circulating progesterone x. Possible influence from circulating endorphins y. Applicable for both neuraxial and peripheral blockades y. Applicable for parturients beyond 24 th week gestation x. Decrease local anesthetic dose by as much as 1/3
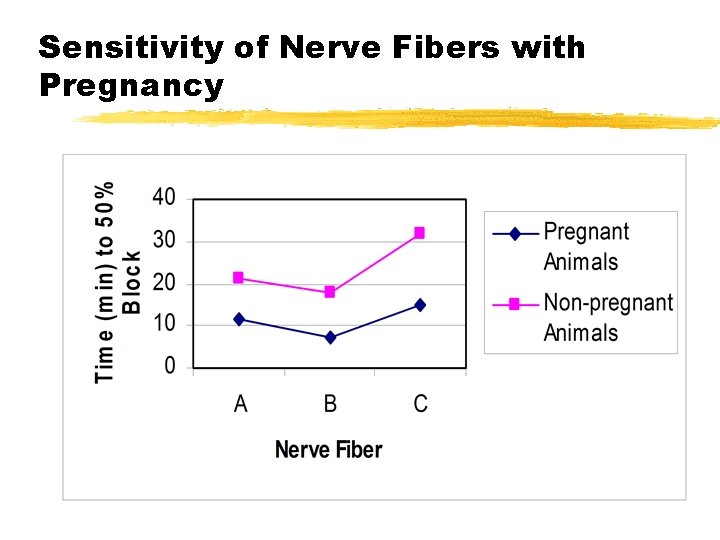
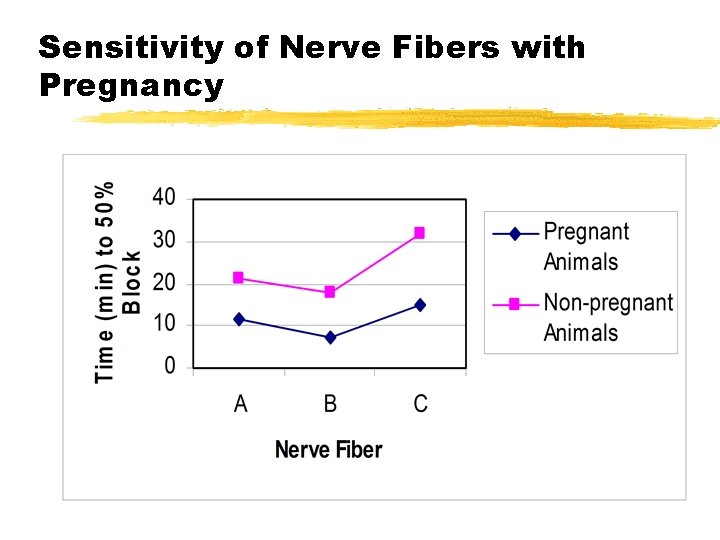
Sensitivity of Nerve Fibers with Pregnancy
Summary z. Multiple physiological changes in pregnancy have profound impact on your anesthetic management z. The conservative approach is the best approach when dealing with the OB patient z. Your principle patient is the parturient
Fetal Monitoring z. No ideal way to assess fetal well-being z. FHR one of the better methods y. FHR influenced by Para and sympathetic outflow y. FHR responds to Baro & Chemo receptors
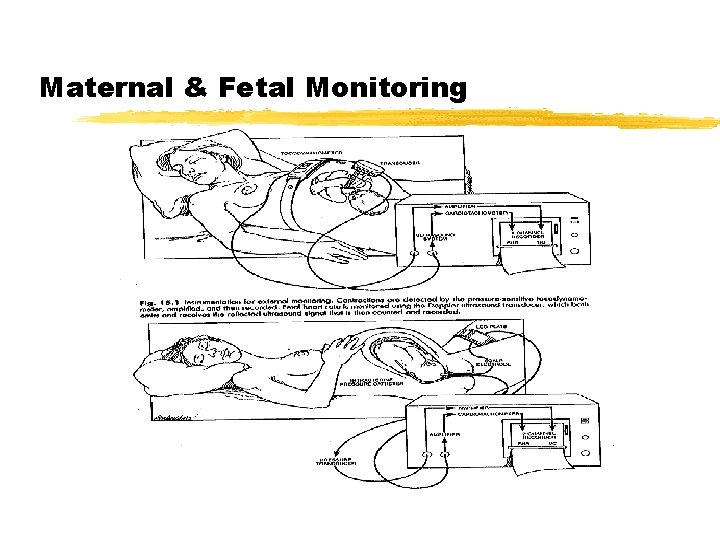
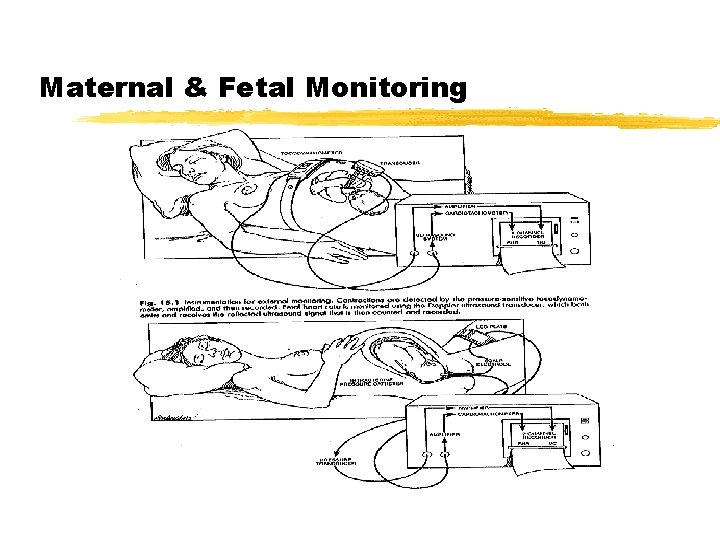
Maternal & Fetal Monitoring
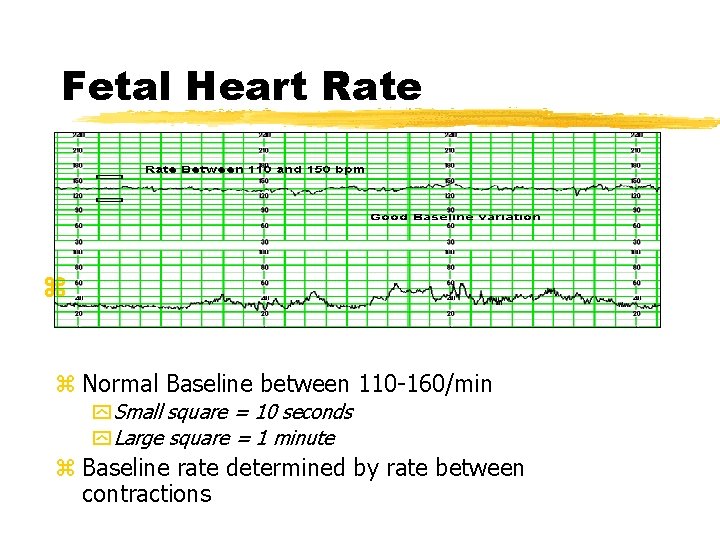
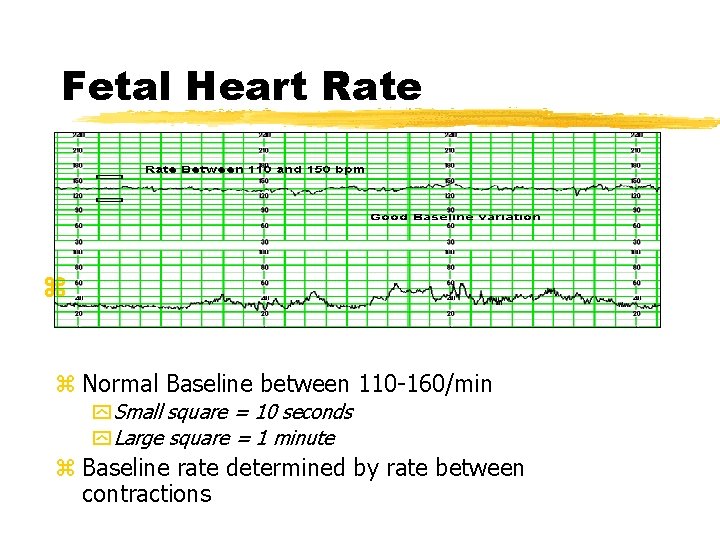
Fetal Heart Rate z z Normal Baseline between 110 -160/min y Small square = 10 seconds y Large square = 1 minute z Baseline rate determined by rate between contractions
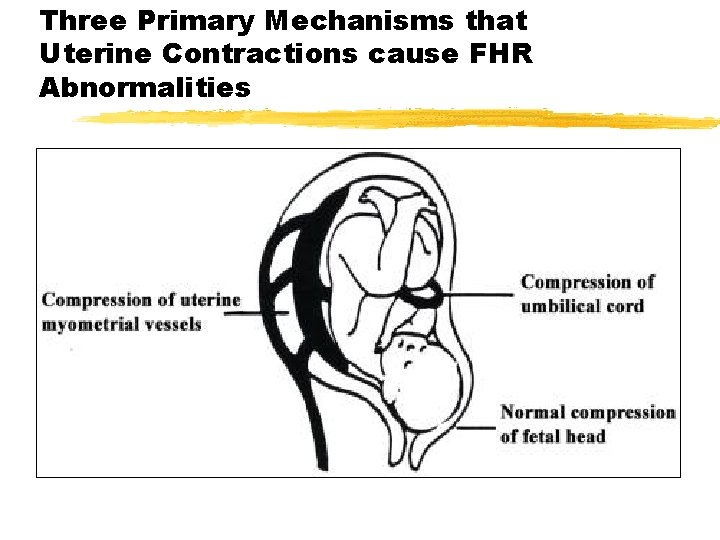
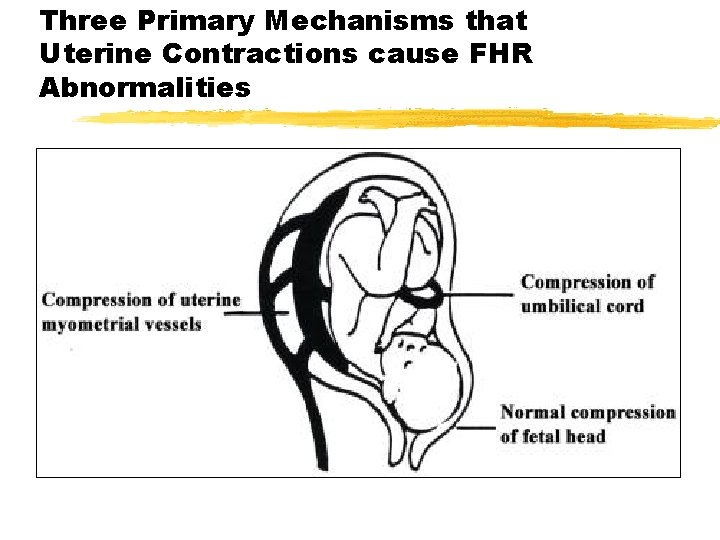
Three Primary Mechanisms that Uterine Contractions cause FHR Abnormalities
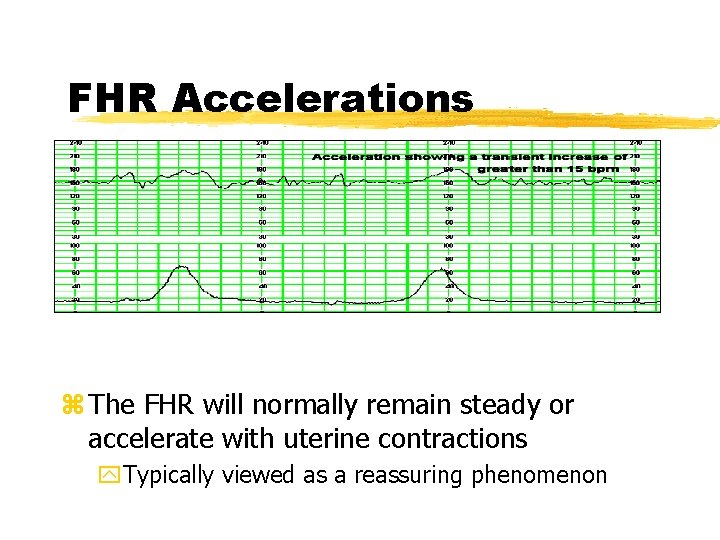
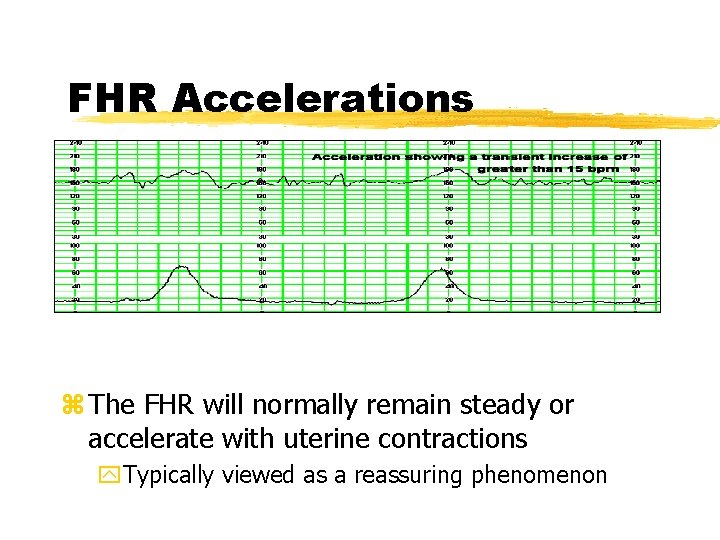
FHR Accelerations z The FHR will normally remain steady or accelerate with uterine contractions y. Typically viewed as a reassuring phenomenon
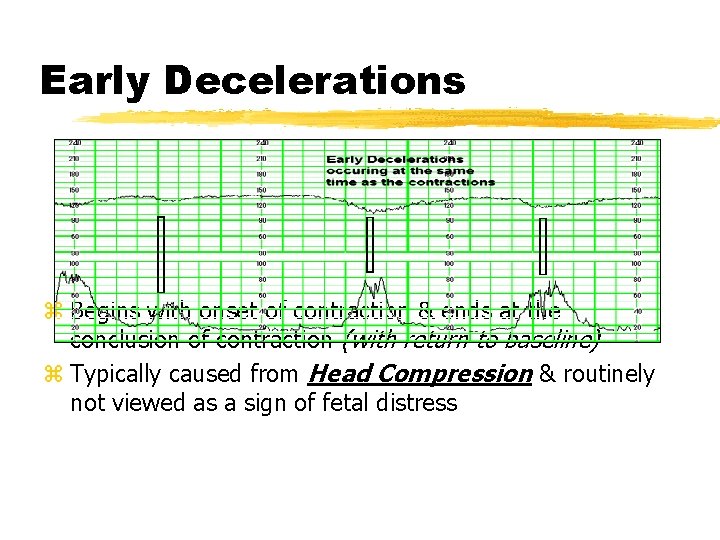
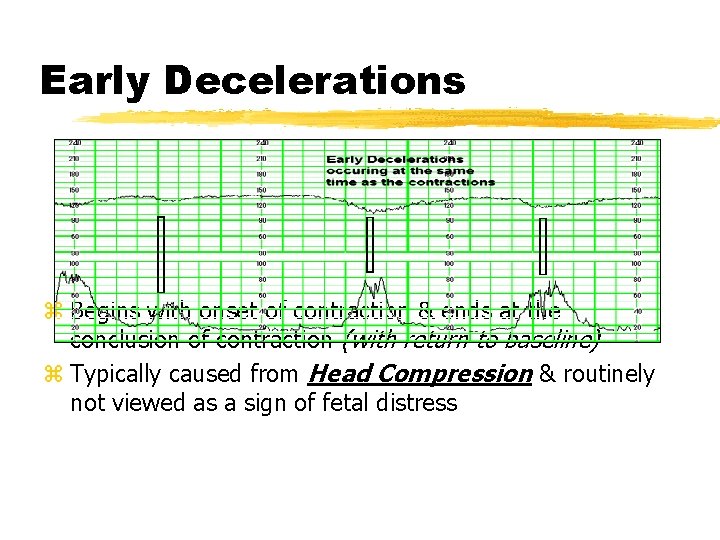
Early Decelerations z Begins with onset of contraction & ends at the conclusion of contraction (with return to baseline) z Typically caused from Head Compression & routinely not viewed as a sign of fetal distress
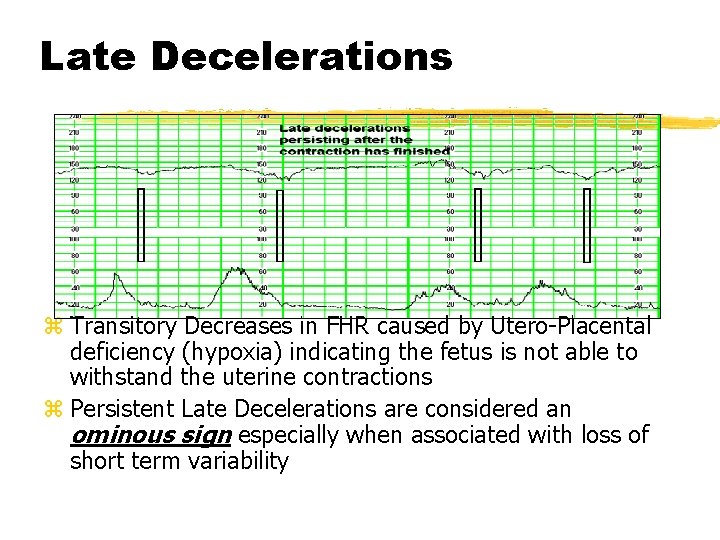
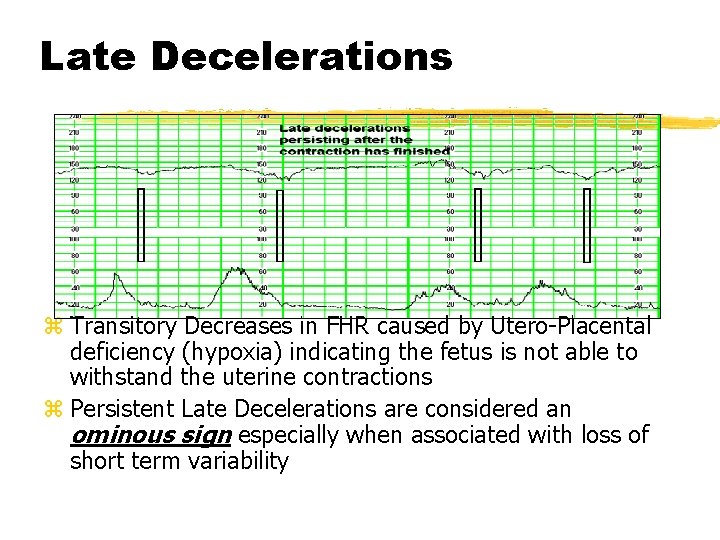
Late Decelerations z Transitory Decreases in FHR caused by Utero-Placental deficiency (hypoxia) indicating the fetus is not able to withstand the uterine contractions z Persistent Late Decelerations are considered an ominous sign especially when associated with loss of short term variability
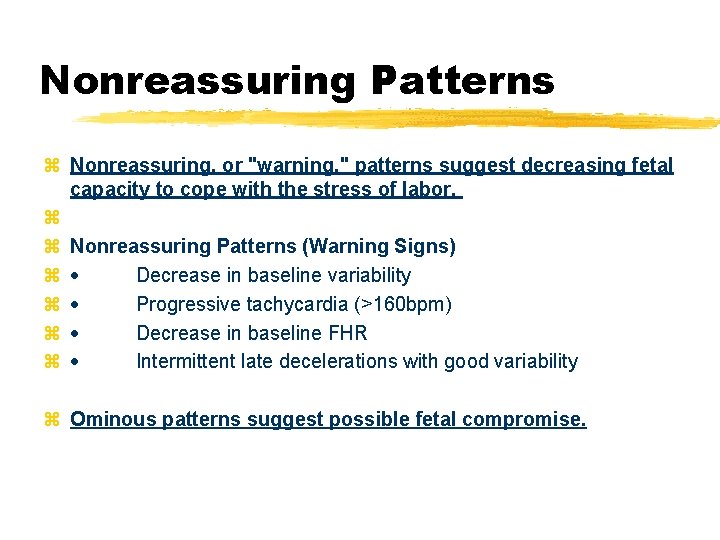
Nonreassuring Patterns z Nonreassuring, or "warning, " patterns suggest decreasing fetal capacity to cope with the stress of labor. z z Nonreassuring Patterns (Warning Signs) z · Decrease in baseline variability z · Progressive tachycardia (>160 bpm) z · Decrease in baseline FHR z · Intermittent late decelerations with good variability z Ominous patterns suggest possible fetal compromise.
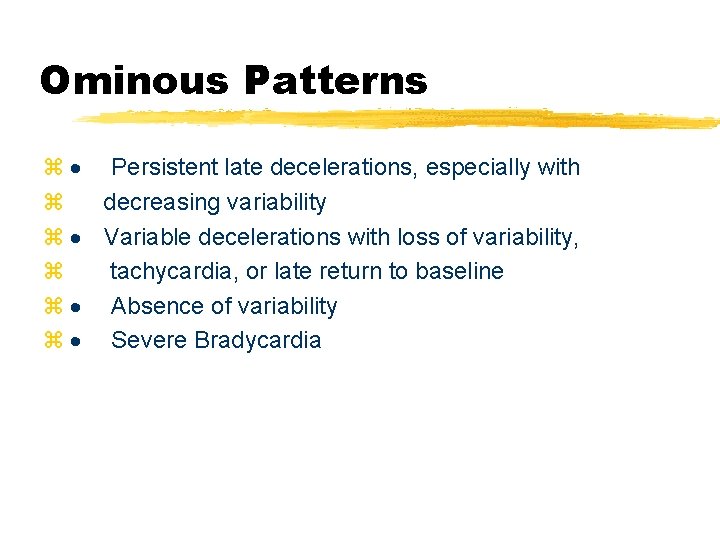
Ominous Patterns z · Persistent late decelerations, especially with z decreasing variability z · Variable decelerations with loss of variability, z tachycardia, or late return to baseline z · Absence of variability z · Severe Bradycardia
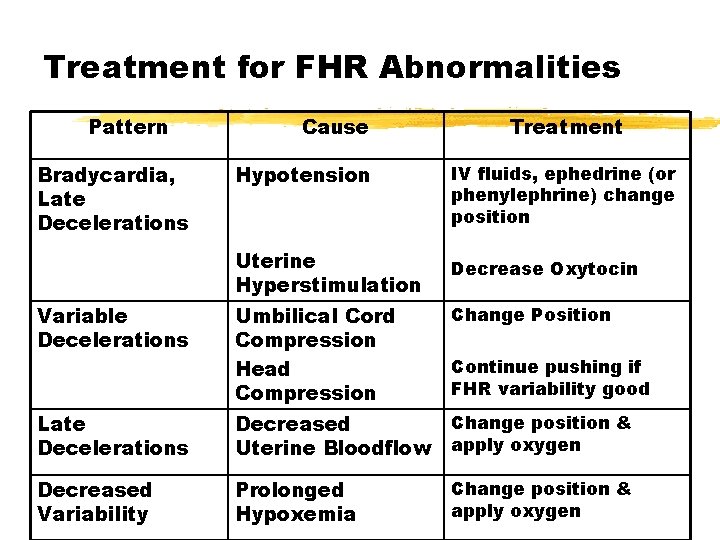
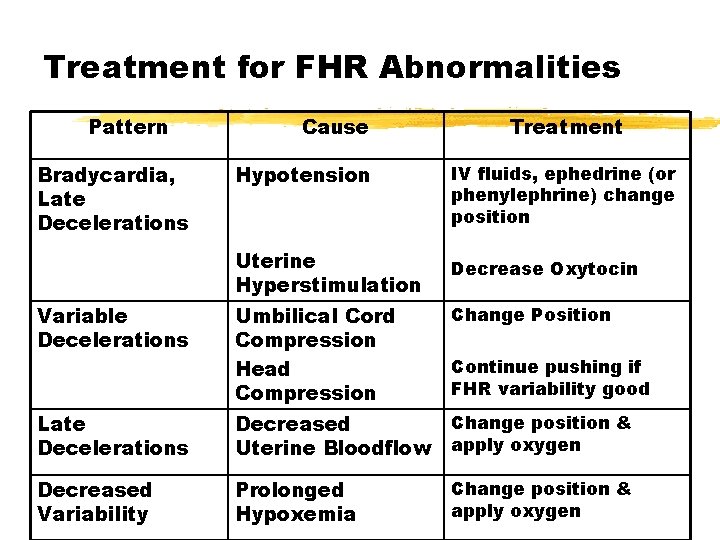
Treatment for FHR Abnormalities Pattern Bradycardia, Late Decelerations Cause Treatment Hypotension IV fluids, ephedrine (or phenylephrine) change position Uterine Hyperstimulation Decrease Oxytocin Variable Decelerations Umbilical Cord Compression Head Compression Change Position Late Decelerations Change position & Decreased Uterine Bloodflow apply oxygen Decreased Variability Prolonged Hypoxemia Continue pushing if FHR variability good Change position & apply oxygen
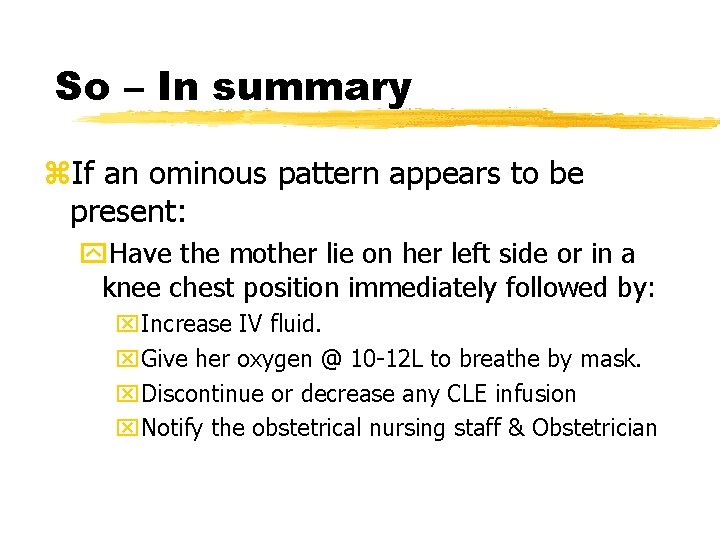
So – In summary z. If an ominous pattern appears to be present: y. Have the mother lie on her left side or in a knee chest position immediately followed by: x. Increase IV fluid. x. Give her oxygen @ 10 -12 L to breathe by mask. x. Discontinue or decrease any CLE infusion x. Notify the obstetrical nursing staff & Obstetrician

Pellegrini@son. umaryland. edu