Anesthesiology Conference Liver Transplantation for Urea Cycle Disorder
- Slides: 28
Anesthesiology Conference Liver Transplantation for Urea Cycle Disorder - A Case Study Sep. 26, 2003 Presented and Edited by Ri 吳智君, 楊翔惟 Directed by Vs 詹光政 , CR 郭書麟
Case Presentation (Liver transplantation) Ri 楊翔惟
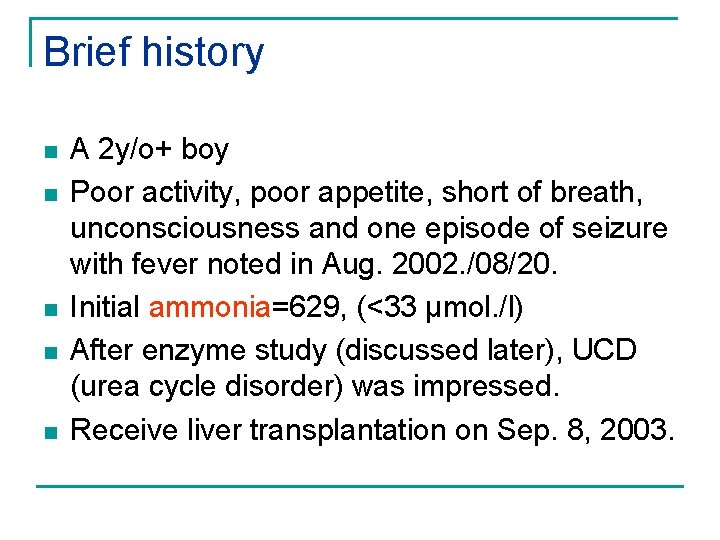
Brief history n n n A 2 y/o+ boy Poor activity, poor appetite, short of breath, unconsciousness and one episode of seizure with fever noted in Aug. 2002. /08/20. Initial ammonia=629, (<33 µmol. /l) After enzyme study (discussed later), UCD (urea cycle disorder) was impressed. Receive liver transplantation on Sep. 8, 2003.
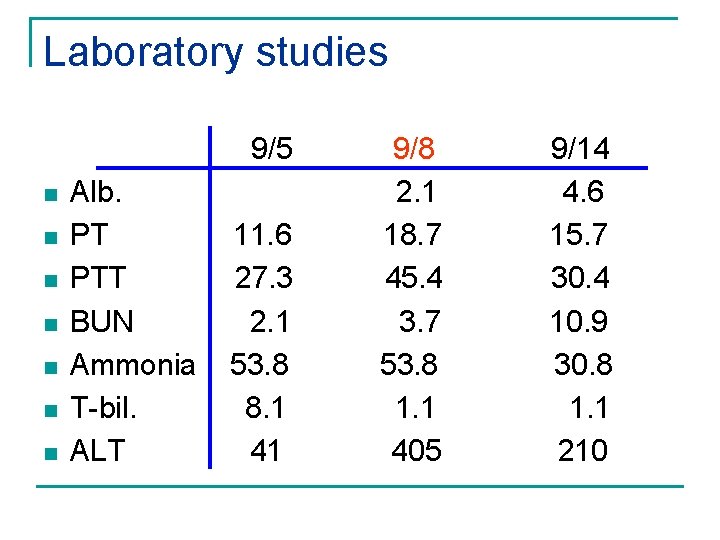
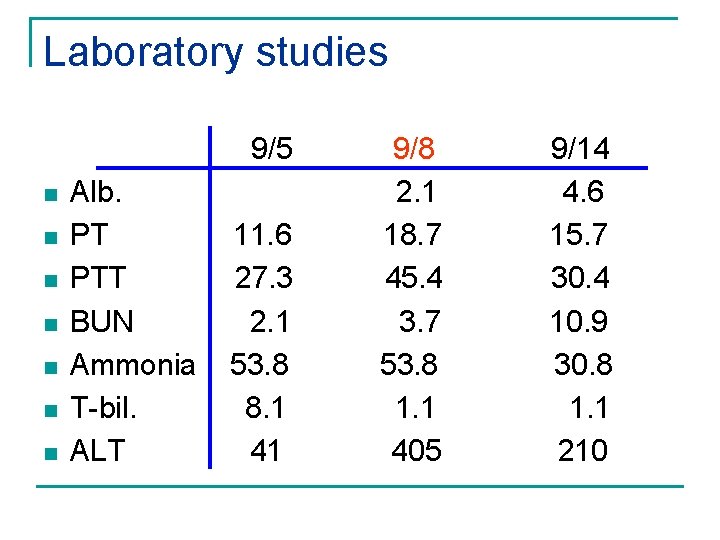
Laboratory studies 9/5 n n n n Alb. PT PTT BUN Ammonia T-bil. ALT 11. 6 27. 3 2. 1 53. 8 8. 1 41 9/8 2. 1 18. 7 45. 4 3. 7 53. 8 1. 1 405 9/14 4. 6 15. 7 30. 4 10. 9 30. 8 1. 1 210
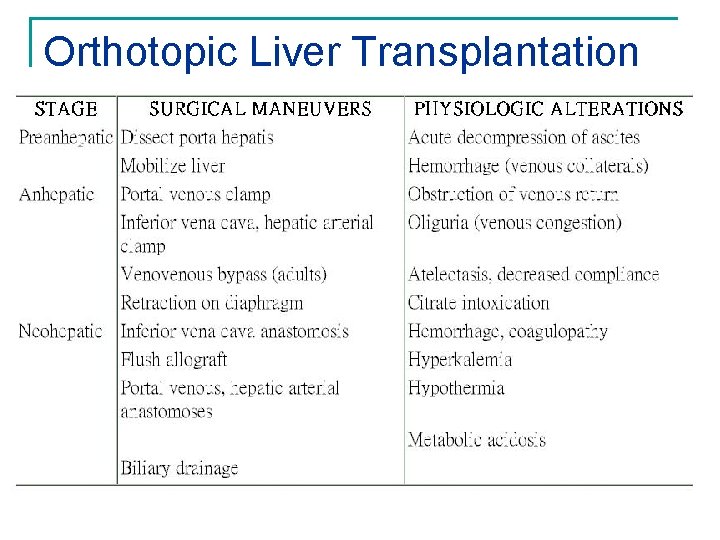
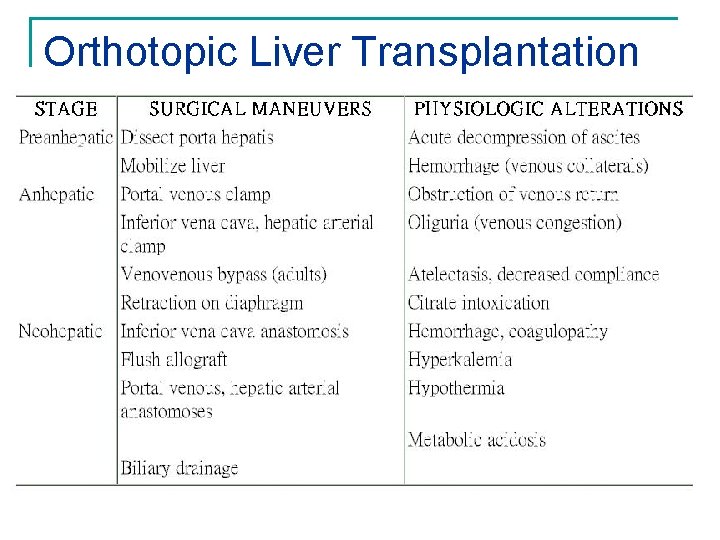
Orthotopic Liver Transplantation
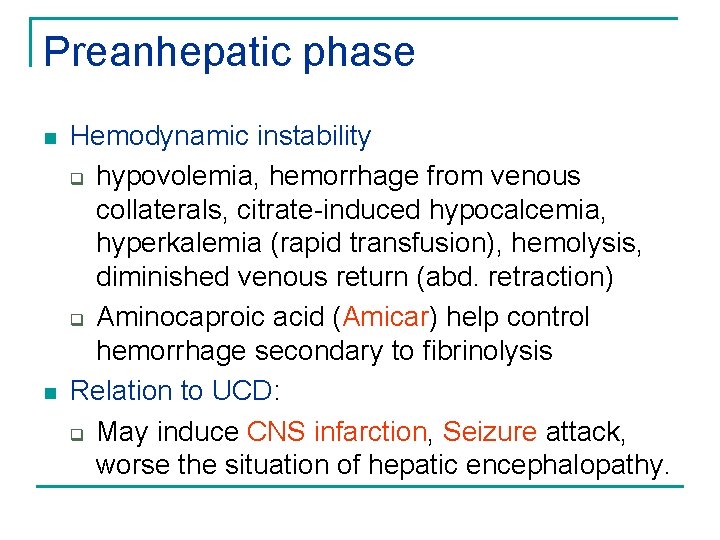
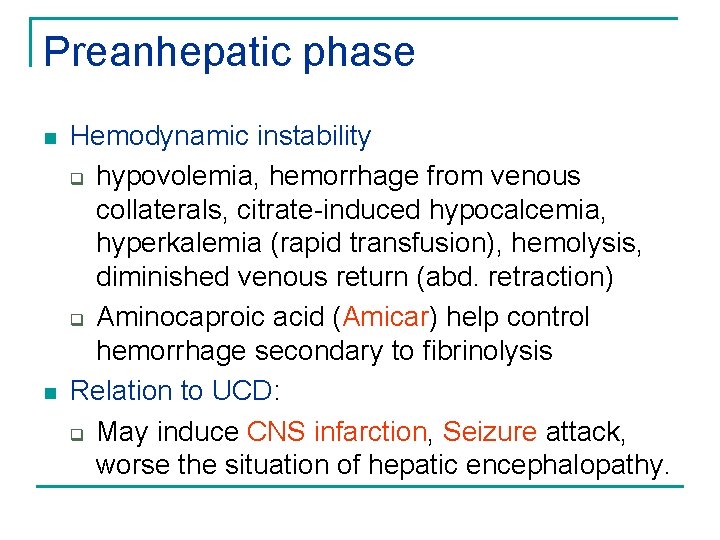
Preanhepatic phase n n Hemodynamic instability q hypovolemia, hemorrhage from venous collaterals, citrate-induced hypocalcemia, hyperkalemia (rapid transfusion), hemolysis, diminished venous return (abd. retraction) q Aminocaproic acid (Amicar) help control hemorrhage secondary to fibrinolysis Relation to UCD: q May induce CNS infarction, Seizure attack, worse the situation of hepatic encephalopathy.
Preanhepatic phase
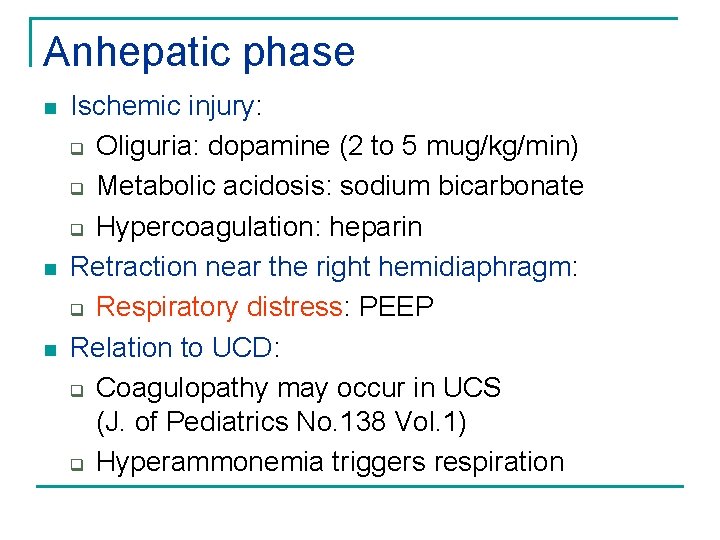
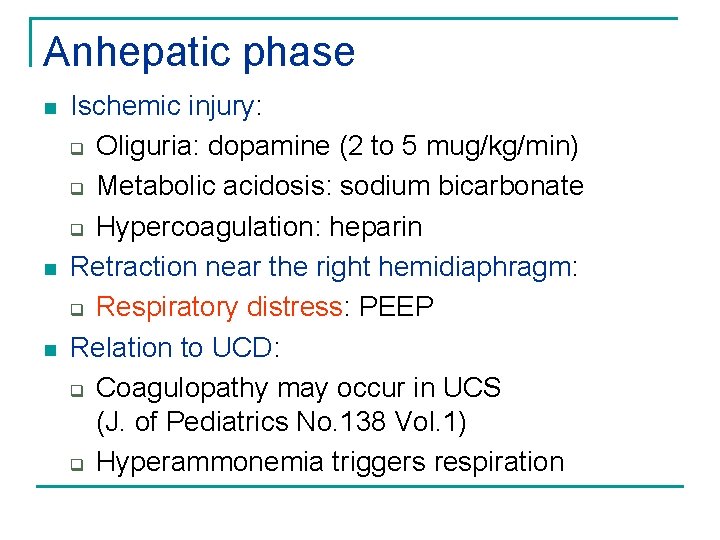
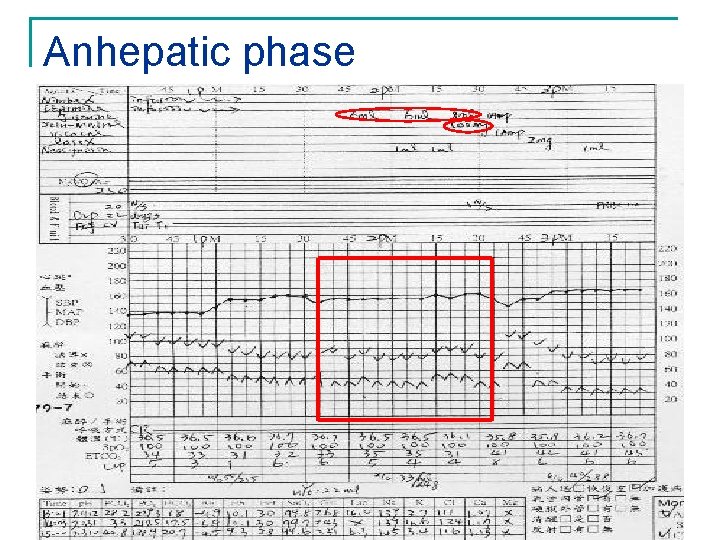
Anhepatic phase n n n Ischemic injury: q Oliguria: dopamine (2 to 5 mug/kg/min) q Metabolic acidosis: sodium bicarbonate q Hypercoagulation: heparin Retraction near the right hemidiaphragm: q Respiratory distress: PEEP Relation to UCD: q Coagulopathy may occur in UCS (J. of Pediatrics No. 138 Vol. 1) q Hyperammonemia triggers respiration
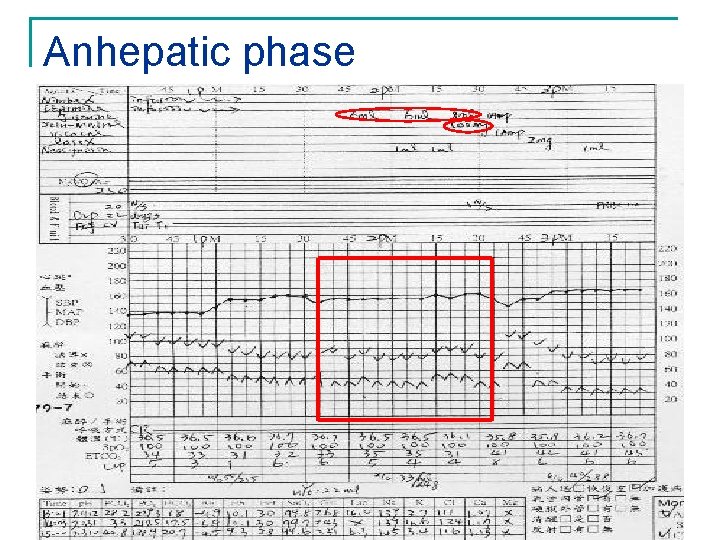
Anhepatic phase
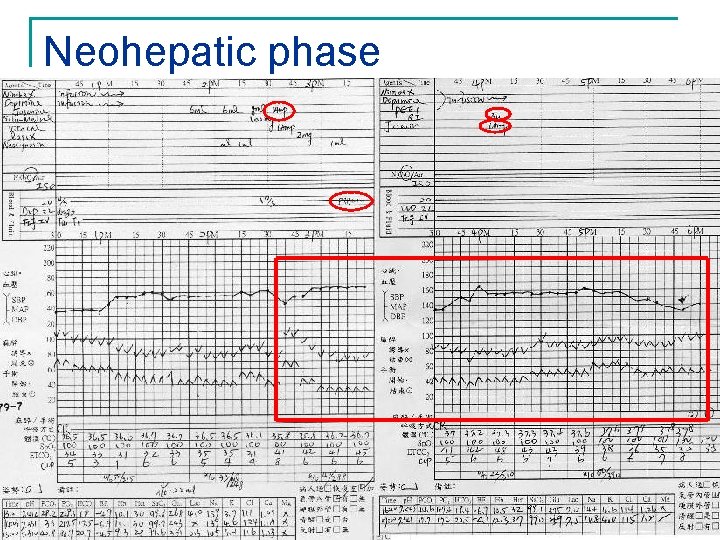
Neohepatic phase n Elevate O 2 consumption and CO 2 elimination: q Oxygen debt from graft tissue and GI systems n Hypotention, Arrhythmia, Thromboembolism q From ischemic metabolites (reperfusion injury), air embolism of reperfusion tissue q Avoid cardiovascular depressant anesthetics
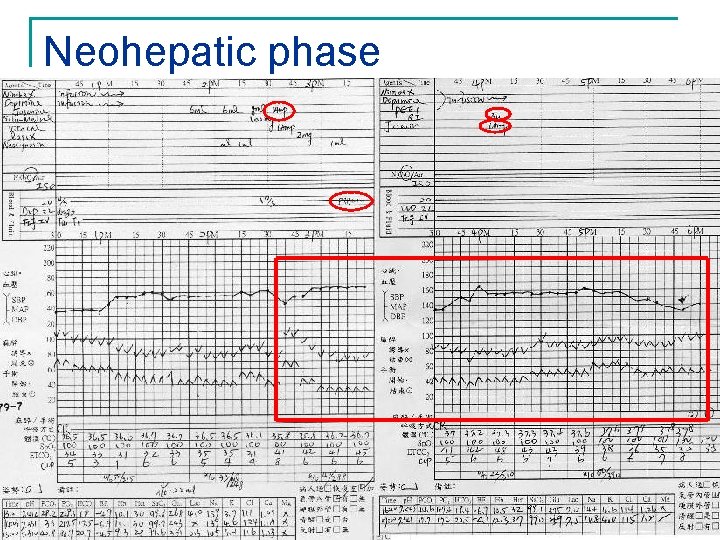
Neohepatic phase
Discussion Ri 吳智君
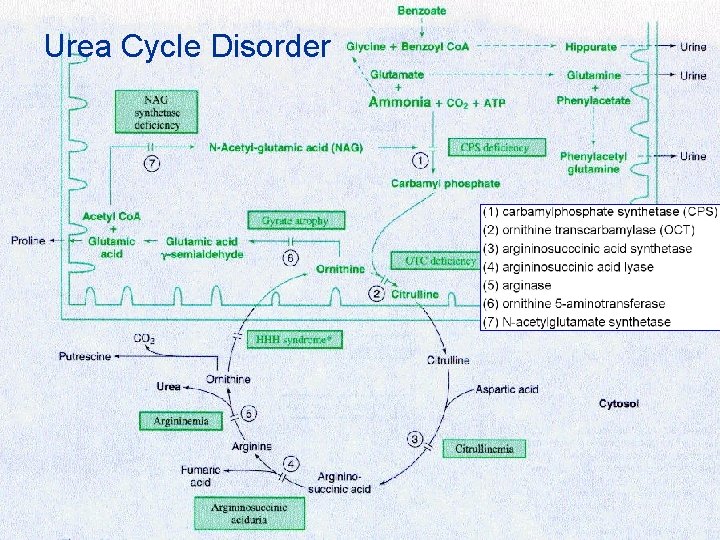
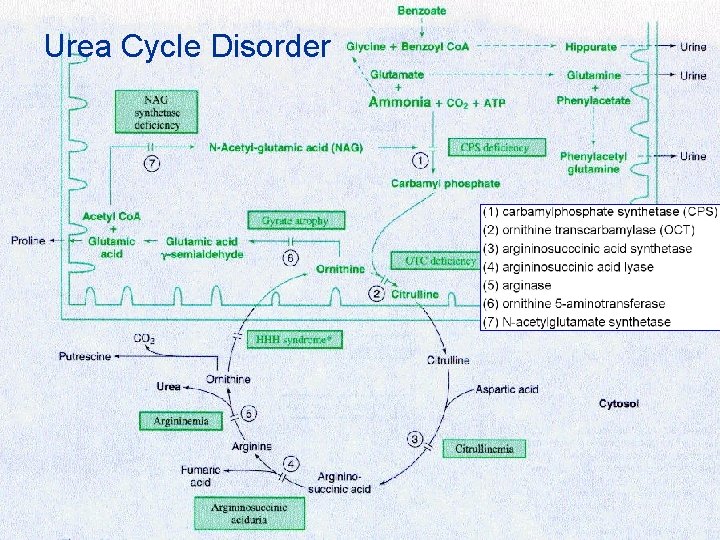
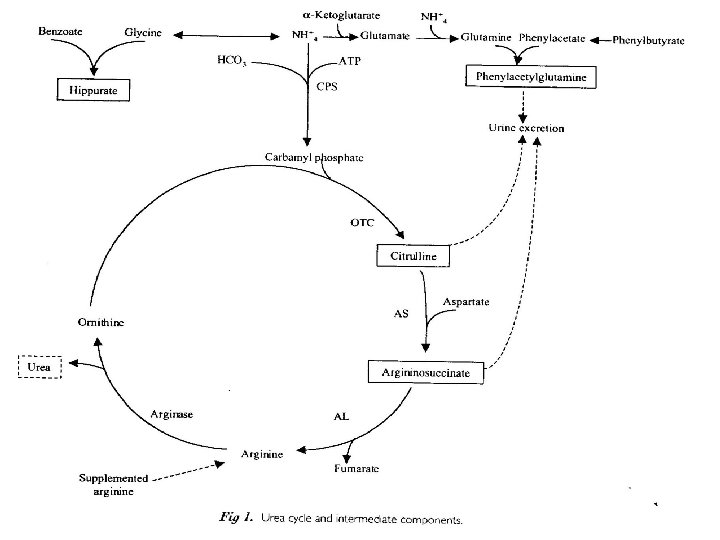
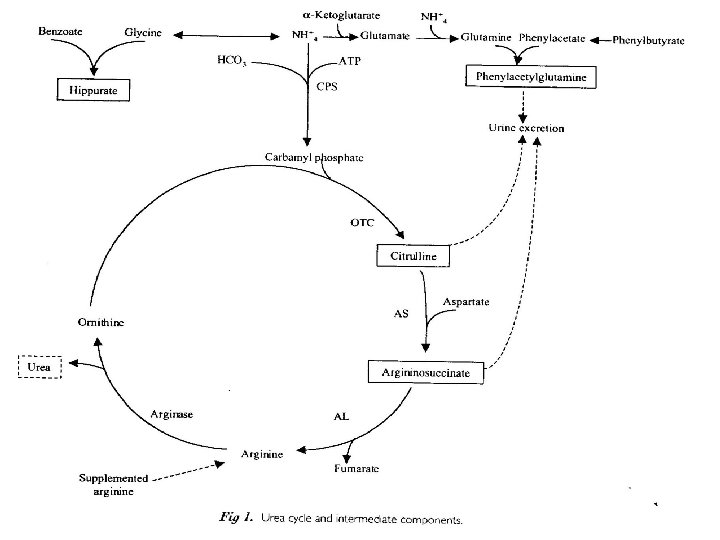
Urea Cycle Disorder n Enzymes: q q q q (1) carbamylphosphate synthetase (CPS) (2) ornithine transcarbamylase (OCT) (3) argininosucccinic acid synthetase (4) argininosuccinic acid lyase (5) arginase (6) ornithine 5 -aminotransferase (7) N-acetylglutamate synthetase
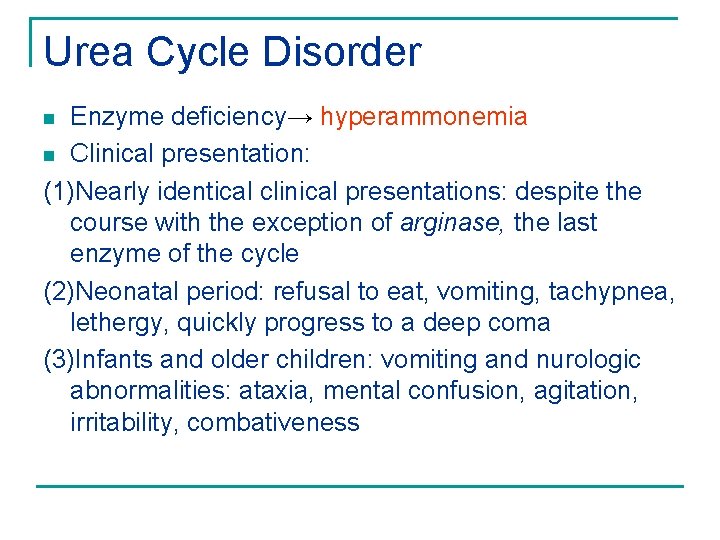
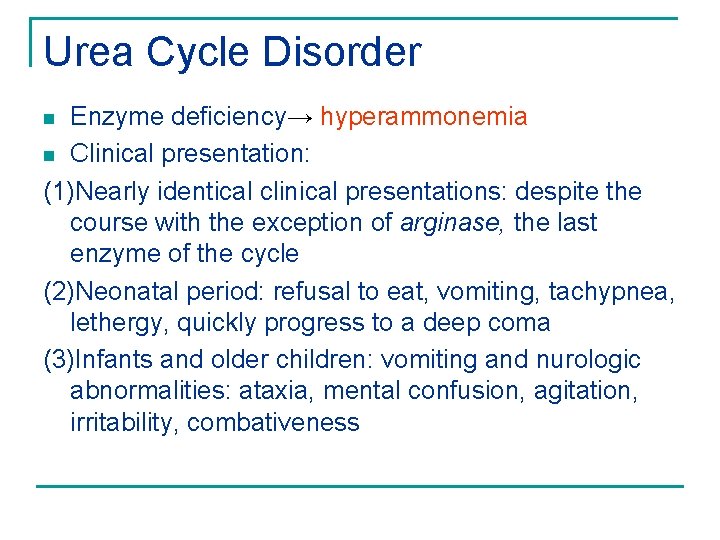
Urea Cycle Disorder Enzyme deficiency→ hyperammonemia n Clinical presentation: (1)Nearly identical clinical presentations: despite the course with the exception of arginase, the last enzyme of the cycle (2)Neonatal period: refusal to eat, vomiting, tachypnea, lethergy, quickly progress to a deep coma (3)Infants and older children: vomiting and nurologic abnormalities: ataxia, mental confusion, agitation, irritability, combativeness n
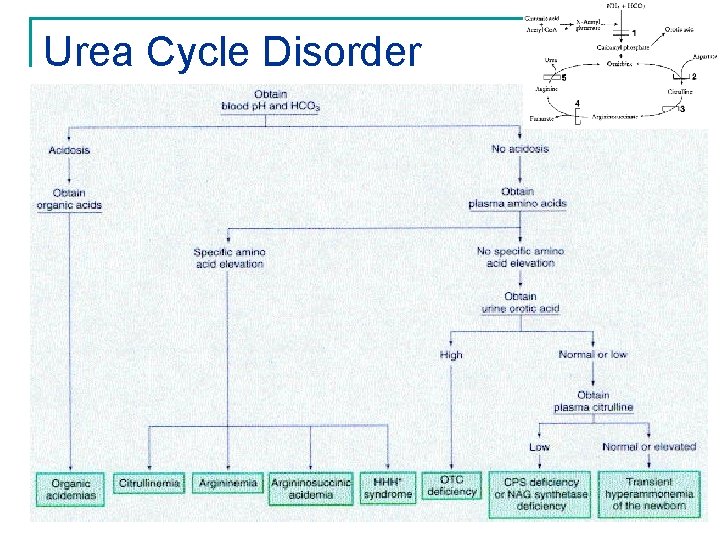
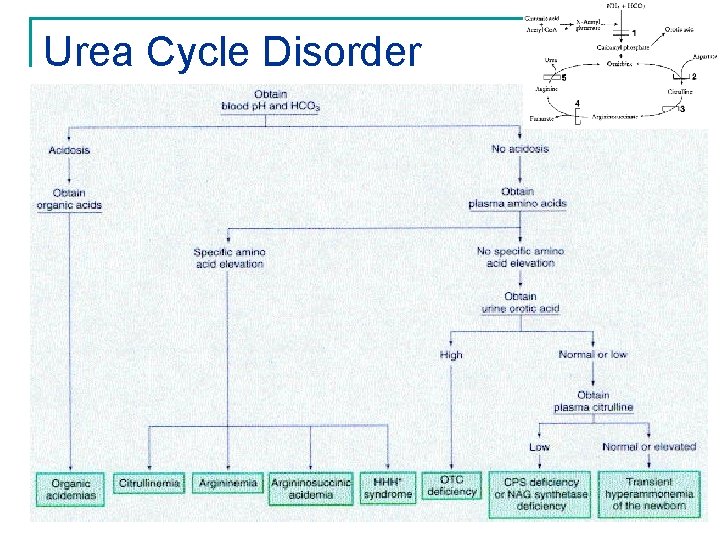
Urea Cycle Disorder
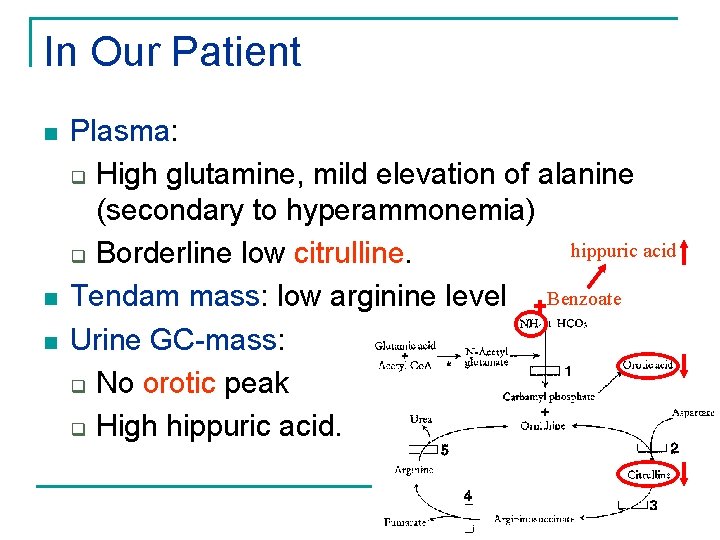
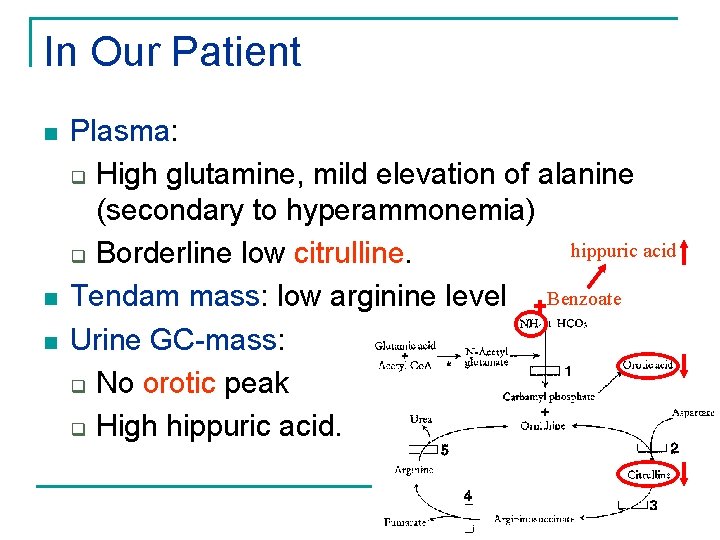
In Our Patient n n n Plasma: q High glutamine, mild elevation of alanine (secondary to hyperammonemia) hippuric acid q Borderline low citrulline. Tendam mass: low arginine level Benzoate Urine GC-mass: q No orotic peak q High hippuric acid.
The Natural History of CPS (Carbamylphosphate synthetase) deficiency n n n A wide variation in severity of symptoms and the age presentation Most commonly symptoms occur during the first few days: early-onset lethargy and seizures often are the first sign of abnormality Coma and death may occur during these hyperammonic episodes
Current strategies for the management of neonatal urea cycle disorders Early supportive treatment n Bulk ammonia removal—dialysis n Pharmacologic management --Phenylacetate --Benzoate --Arginine supplement n Long term correction --orthotopic liver transplantation n go to --gene therapy Indications ~The journal of pediatrics vol 138, no 1, s 30~38
Indications for Liver Transplantation for urea cycle disorder n n Who cannot follow the necessary dietary restrictions Who has recurrent episodes of hyperammonemia despite optimal medical management Patients with CPS and OTC deficiency need early transplantation due to more difficult control of the natural history Rigid dietary and pharmacotherapy regimen vs immunosuppression regimen
Contraindications to Liver Transplantation n Positive immunodeficiency virus culture n Severe irreversible neurologic injury
Indications for liver transplantation n Urea cycle disorder, r/o CPS deficiency, r/o N-acetylglutamate synthetase deficiency difficult control of the natural course n Delayed growth of motor function, but no irreversible neurologic injury
Donor options n n Donor allograft size reduction Living-donor liver transplantation Split-liver transplantation The mortality of potential recipients<20 kg await for OLT have reduced from 25%~50% to 2~5%
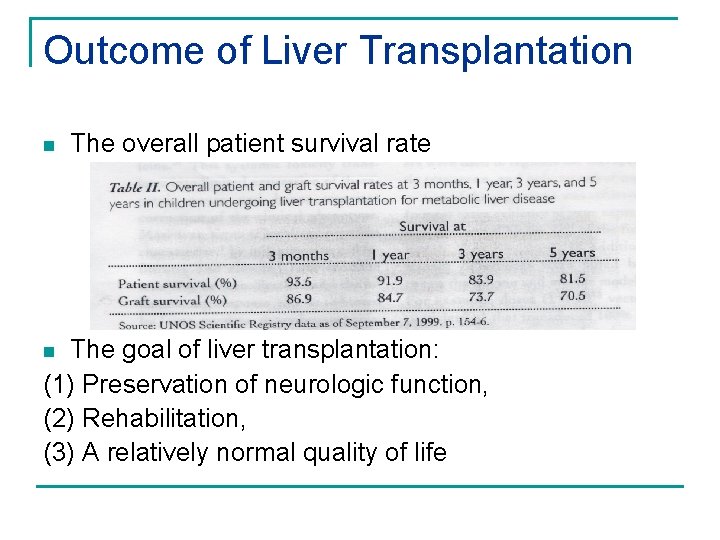
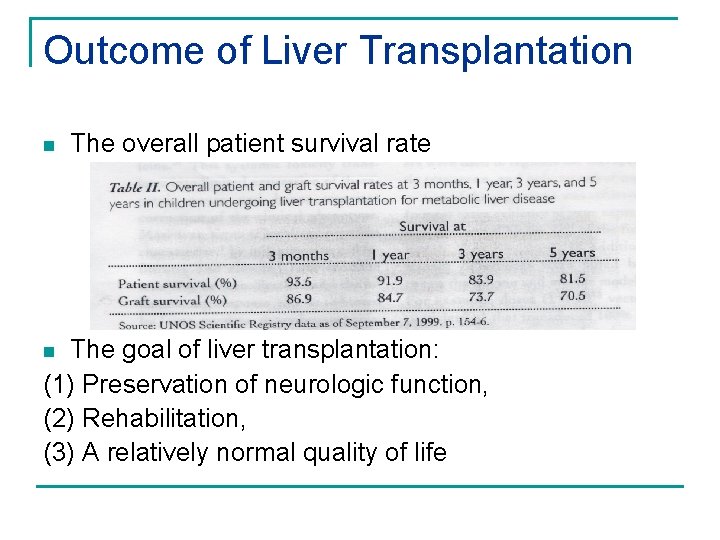
Outcome of Liver Transplantation n The overall patient survival rate The goal of liver transplantation: (1) Preservation of neurologic function, (2) Rehabilitation, (3) A relatively normal quality of life n
Outcome of Liver Transplantation n n resulted in correction of hyperammonaemia in all patients. The neurological outcome after transplantation correlated closely with the condition prior to transplantation. relatively few problems in the long term related to the liver transplant itself. The quality of life seems to be much improved ~Journal of Inherited Metabolic Disease. 21 Suppl 1: 112 -8, 1998. , Acta Gastroenterologica Belgica. 62(3): 300 -5, 1999 Jul-Sep. ,
Comparison of outcome after pediatric liver transplantation for metabolic diseases and biliary natresia. Pediatric OLT: cholestatic liver disorders n n ranking first, followed by hepatic based metabolic disorders The mean infection, complication, intervention, and retransplantation rate was equal in both groups. Mortality and morbidity are not different despite the better starting point for children with MD. ~European Journal of Pediatric Surgery. 11(1): 28 -35, 2001 Feb.
Donation from a donor with ornithine transcarbamylase deficiency. n n The donor's OTC deficiency was diagnosed retrospectively since the liver graft recipient developed cerebral edema postoperatively due to extremely hyperammonemia(3793 micromol/l), but was not accompanied by general liver dysfunction In contrast to the fatal course of the liver graft recipient, the kidney, lung, and heart transplantations were successful. ~. Transplant International. 14(3): 196 -201, 2001 Jun.
Thank you~