Anesthesia in Electrophysiology 2016 Mark S Weiss MD







- Slides: 27

Anesthesia in Electrophysiology © 2016 Mark S Weiss, MD Department of Anesthesiology and Critical Care
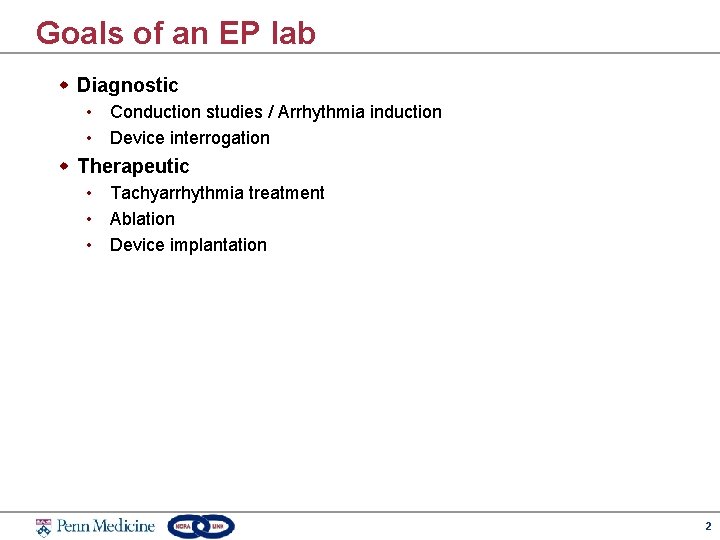
Goals of an EP lab w Diagnostic • Conduction studies / Arrhythmia induction • Device interrogation w Therapeutic • Tachyarrhythmia treatment • Ablation • Device implantation 2
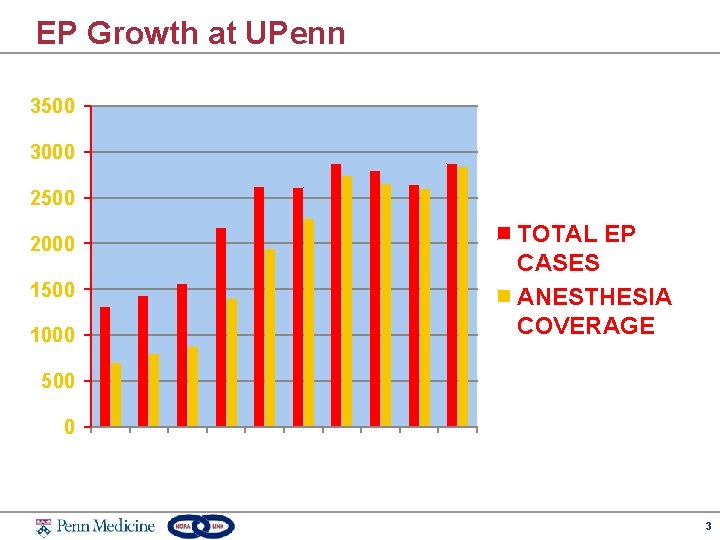
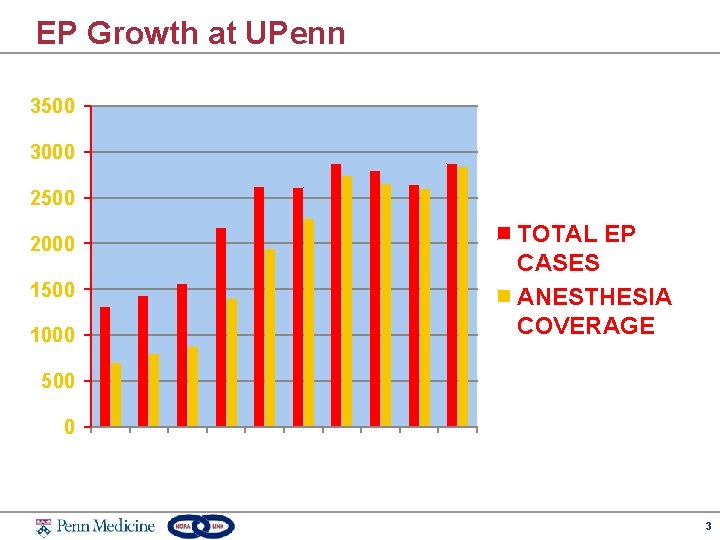
EP Growth at UPenn 3500 3000 2500 2000 1500 1000 TOTAL EP CASES ANESTHESIA COVERAGE 500 0 3
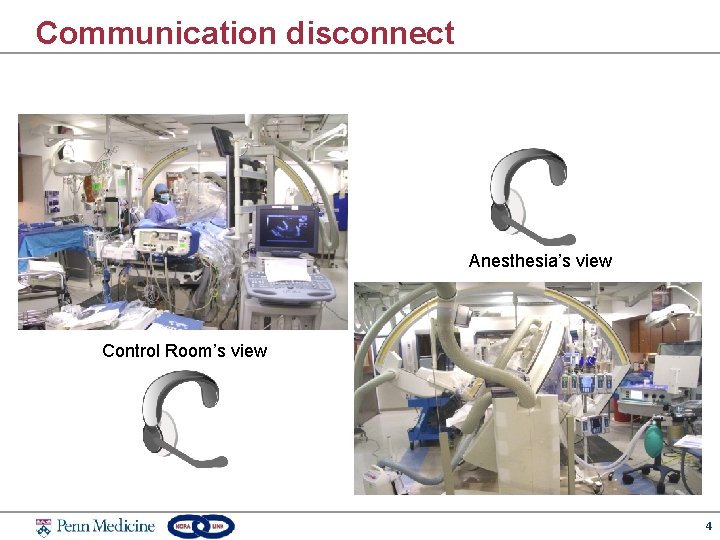
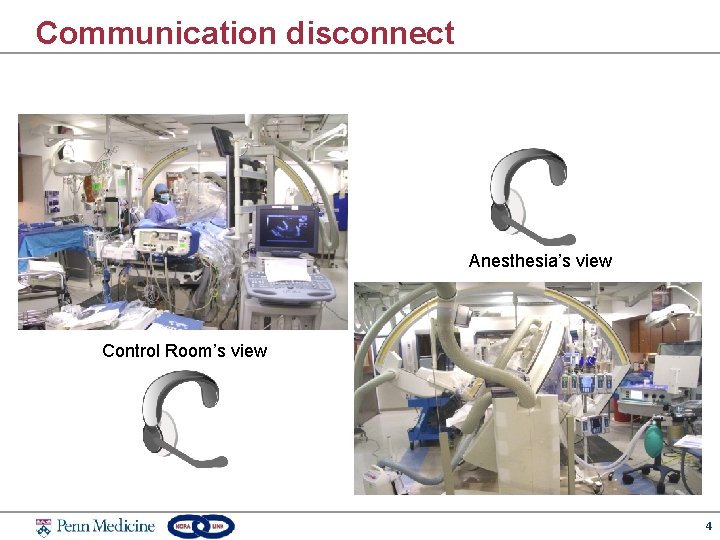
Communication disconnect Anesthesia’s view Control Room’s view 4
Preoperative Evaluation w Airway • challenges can be amplified in NORA environments w Allergies • Shellfish -> Contrast Dye • Fish -> Protamine • Antibiotics -> surgical site infection prevention protocols w Cardiac • Ejection Fraction – selecting pressor agents/anesthetic agents • Congestive heart failure – tolerance of supine position • Pulmonary HTN – sedation induced hypercarbia and hypoxia w Pulmonary • OSA/Morbid obesity - requirement for CPAP w Gastrointestinal • GERD – increased importance with sedation 5
Preanesthetic Preparation w w w w Machine –positive pressure ventilation Suction – sometimes shared with proceduralist Monitors – basic ASA and others as needed Airway IV –Sedation and TIVA common Drugs – resuscitation drugs Special equipment – jet ventilator, esophageal temperature probes, warming/cooling devices 6

Emergency Airway Equipment 7
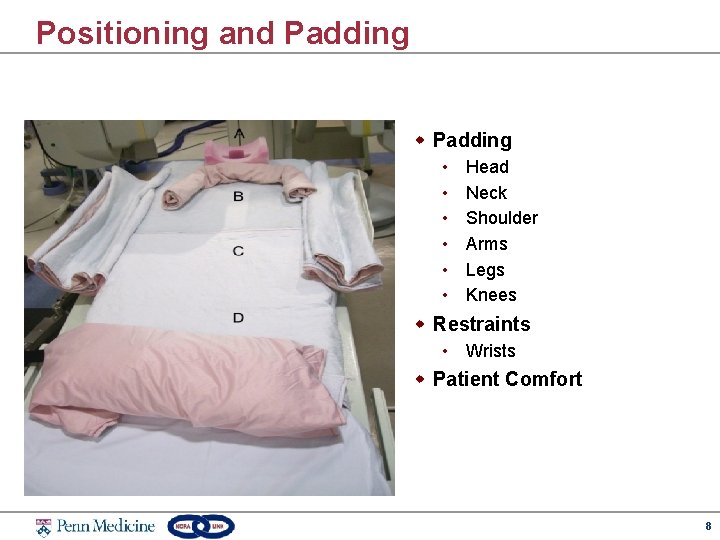
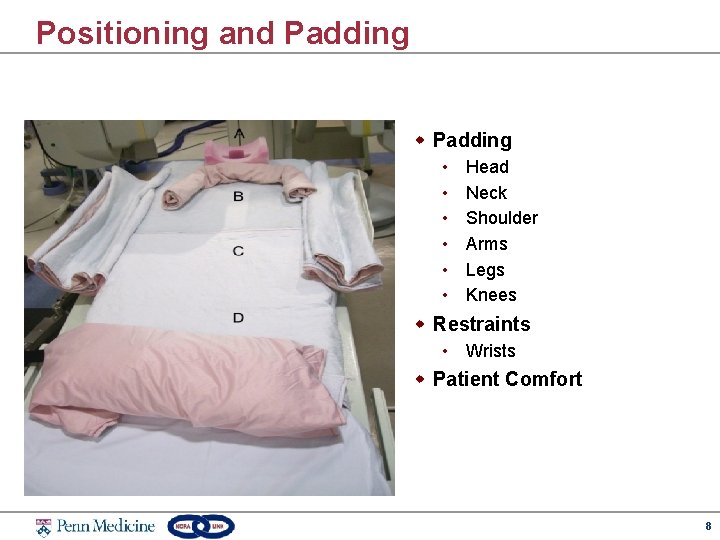
Positioning and Padding w Padding • • • Head Neck Shoulder Arms Legs Knees w Restraints • Wrists w Patient Comfort 8
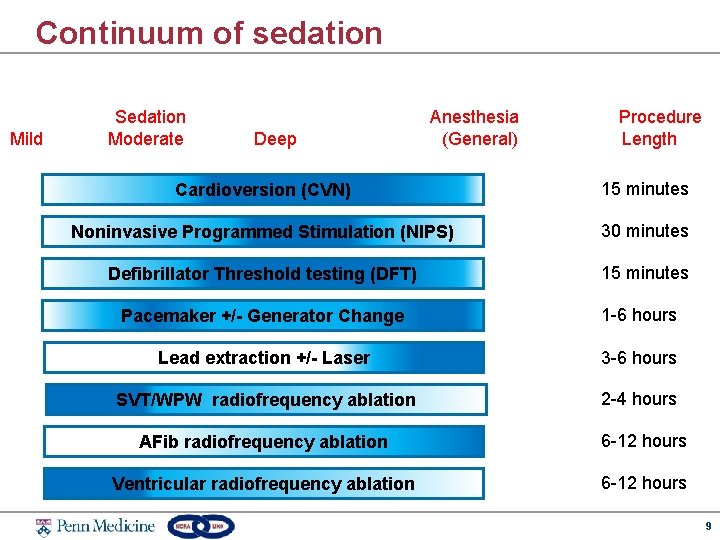
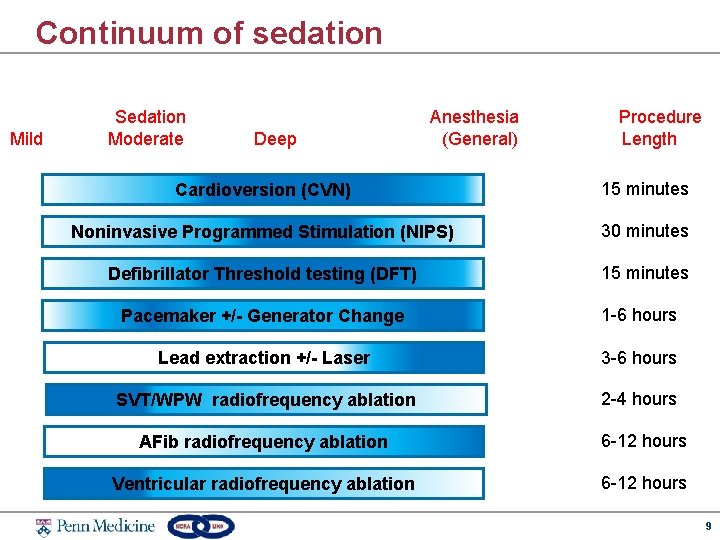
Continuum of sedation Mild Sedation Moderate Deep Anesthesia (General) Procedure Length Cardioversion (CVN) 15 minutes Noninvasive Programmed Stimulation (NIPS) 30 minutes Defibrillator Threshold testing (DFT) 15 minutes Pacemaker +/- Generator Change 1 -6 hours Lead extraction +/- Laser 3 -6 hours SVT/WPW radiofrequency ablation 2 -4 hours AFib radiofrequency ablation 6 -12 hours Ventricular radiofrequency ablation 6 -12 hours 9
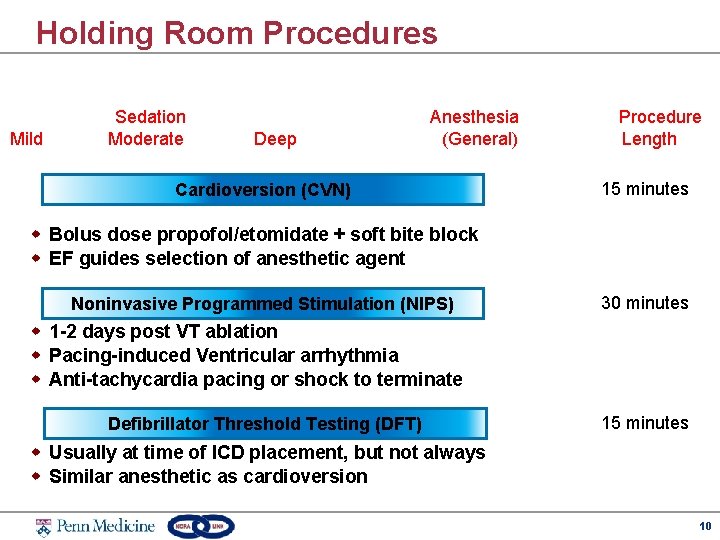
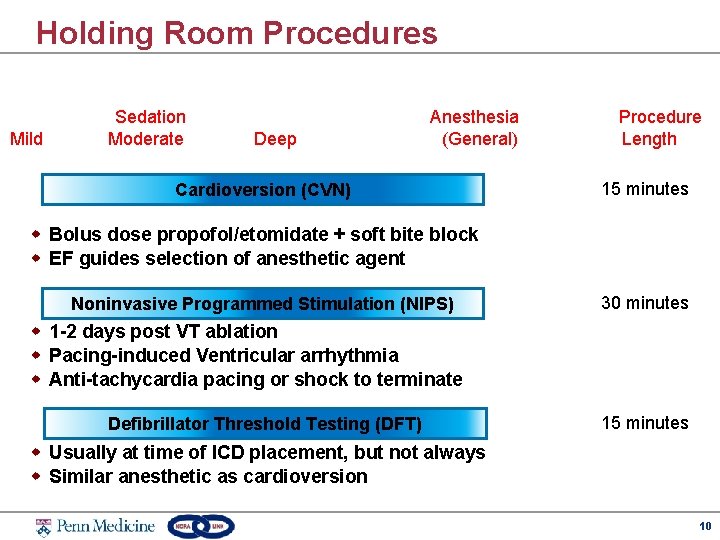
Holding Room Procedures Mild Sedation Moderate Deep Anesthesia (General) Cardioversion (CVN) Procedure Length 15 minutes w Bolus dose propofol/etomidate + soft bite block w EF guides selection of anesthetic agent Noninvasive Programmed Stimulation (NIPS) 30 minutes w 1 -2 days post VT ablation w Pacing-induced Ventricular arrhythmia w Anti-tachycardia pacing or shock to terminate Defibrillator Threshold Testing (DFT) 15 minutes w Usually at time of ICD placement, but not always w Similar anesthetic as cardioversion 10

Device Placement Mild Sedation Moderate Deep Anesthesia (General) Pacemaker +/- Generator Change Procedure Length 1 -6 hours w Device Placement – Pectoral vs. Subcutaneous • Symptomatic Bradycardia: Pacemaker • Tachyarrhythmia: ICD • Cardiac resynchronization therapy (CRT): Bi. V-ICD w Generator Change • Shorter procedure • May require DFT 11

Device Removal Mild Sedation Moderate Deep Anesthesia (General) Lead extraction +/- Laser Procedure Length 3 -6 hours w Indications • System infection • Lead malfunction (fracture/failure/erosion) w Considerations • Leads > 1 year old can have adhesions – May lead to cardiac/vascular avulsion or injury • Blood / Rapid infuser availability • Cardiac surgery backup • May have to be done in main OR 12
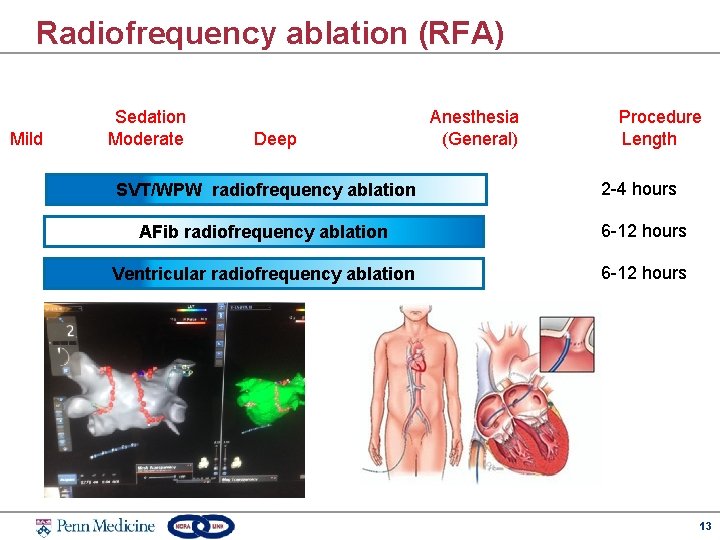
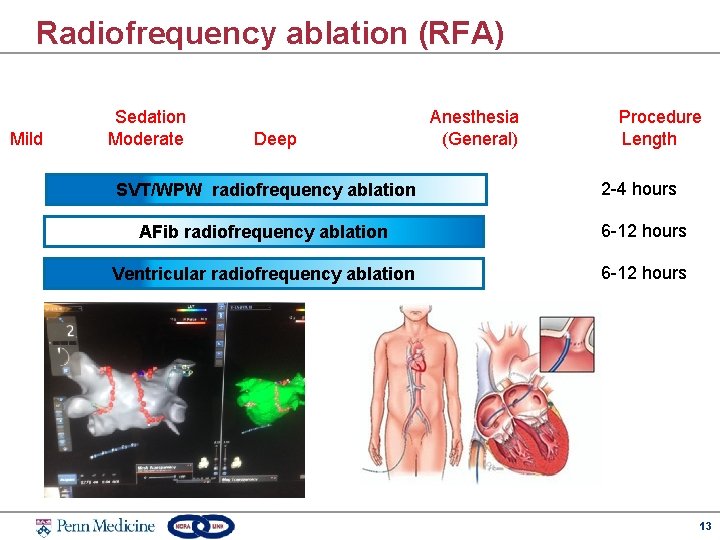
Radiofrequency ablation (RFA) Mild Sedation Moderate Deep Anesthesia (General) Procedure Length SVT/WPW radiofrequency ablation 2 -4 hours AFib radiofrequency ablation 6 -12 hours Ventricular radiofrequency ablation 6 -12 hours 13

Esophageal Temperature Probes w 26% of patients with esophageal injuries without luminal esophageal monitoring during RFA “ Preventions of Esophageal Injury during Radiofrequency Ablation for Atrial Fibrillation” Enzhao L, Shehata M, Liu T, et al - J Interv Card Electrophysiol 2012; 35: 35 -44. 14
High Frequency Jet Ventilation (HFJV) w Increases efficiency/efficacy by decreasing respiratory motion artifacts w Requires GA with ETT and TIVA 15
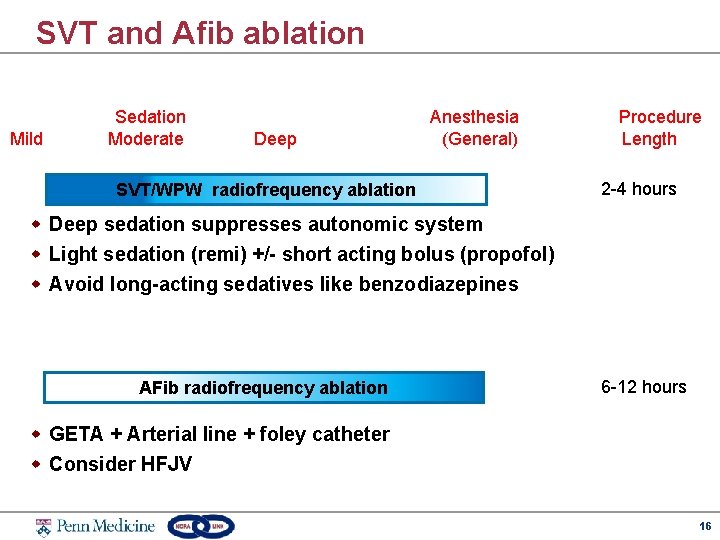
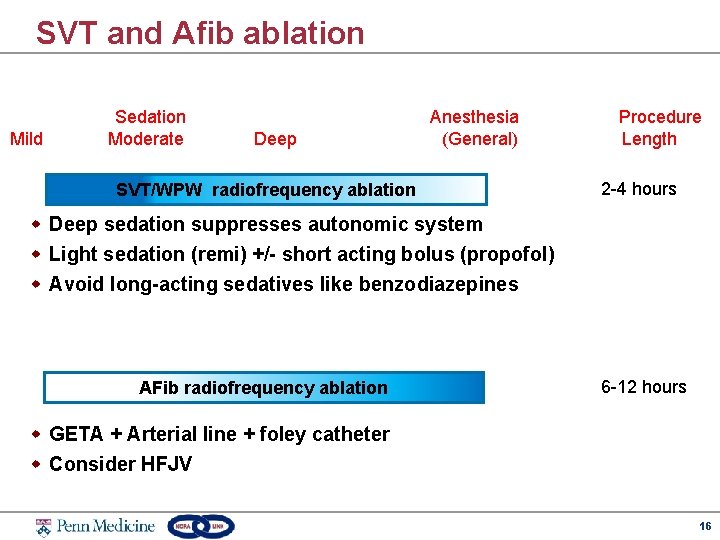
SVT and Afib ablation Mild Sedation Moderate Deep Anesthesia (General) SVT/WPW radiofrequency ablation Procedure Length 2 -4 hours w Deep sedation suppresses autonomic system w Light sedation (remi) +/- short acting bolus (propofol) w Avoid long-acting sedatives like benzodiazepines AFib radiofrequency ablation 6 -12 hours w GETA + Arterial line + foley catheter w Consider HFJV 16

PVC and Vfib ablation Mild Sedation Moderate Deep Anesthesia (General) Ventricular radiofrequency ablation w w w Procedure Length 6 -12 hours Deep sedation suppresses autonomic system Usually have low EF ( < 10%) Light narcotic sedation used (remifentanil infusion) Mental status during V-tach assesses need for defibrillation If GETA, cerebral oximetry used to guide decision 17
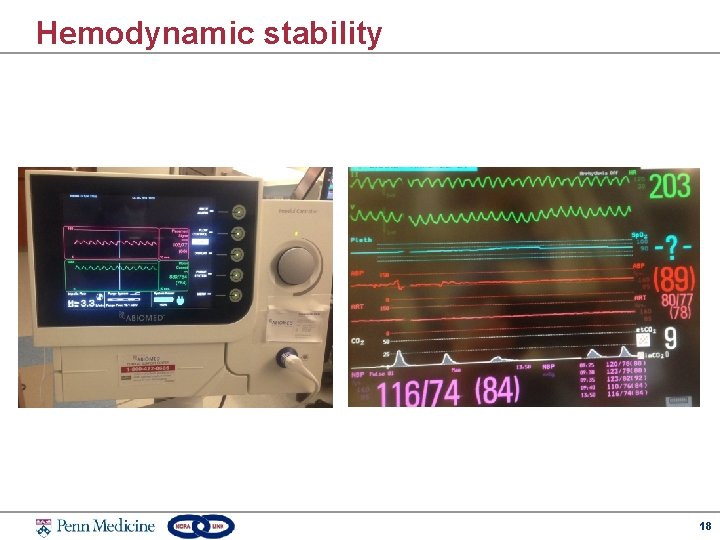
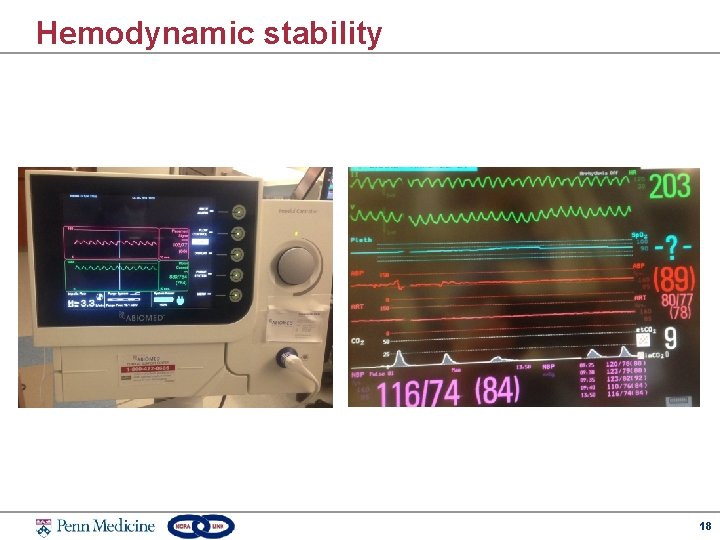
Hemodynamic stability 18
Isoproterenol (Isuprel) w Basic concepts • • • Nonspecific beta agonist Positive chronotropic, dromotropic, and inotropic effects Used to induce ventricular arrhythmias Beta 2 -mediated hypotension Can cause an increase in the MAC requirement 19
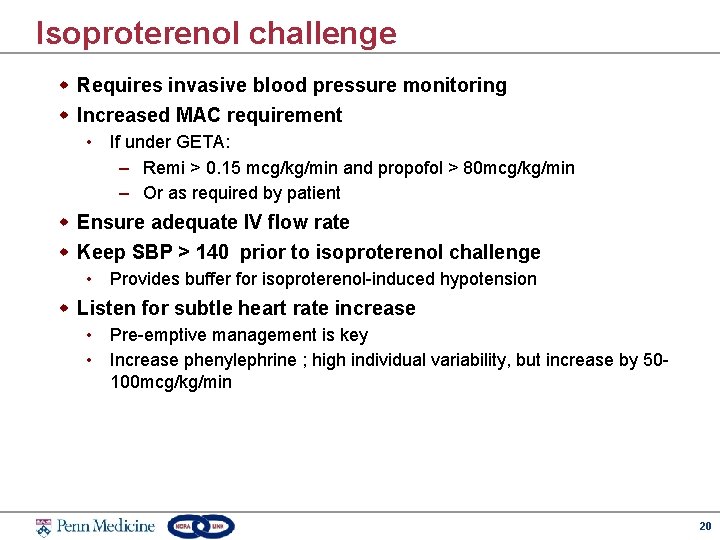
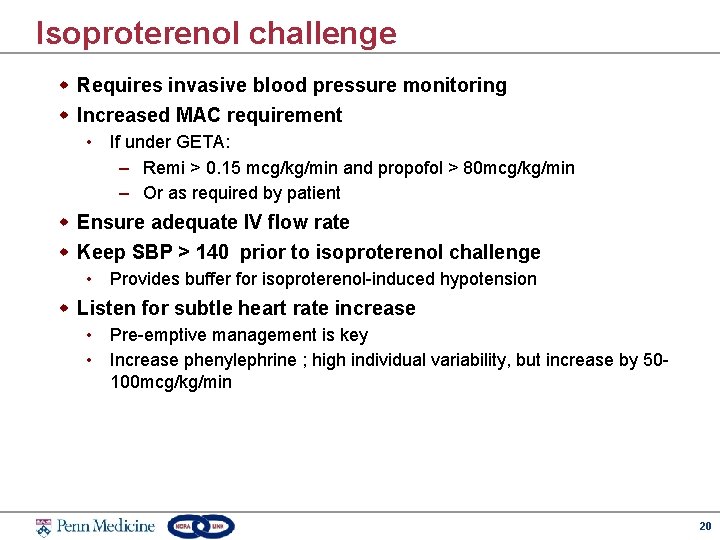
Isoproterenol challenge w Requires invasive blood pressure monitoring w Increased MAC requirement • If under GETA: – Remi > 0. 15 mcg/kg/min and propofol > 80 mcg/kg/min – Or as required by patient w Ensure adequate IV flow rate w Keep SBP > 140 prior to isoproterenol challenge • Provides buffer for isoproterenol-induced hypotension w Listen for subtle heart rate increase • Pre-emptive management is key • Increase phenylephrine ; high individual variability, but increase by 50100 mcg/kg/min 20
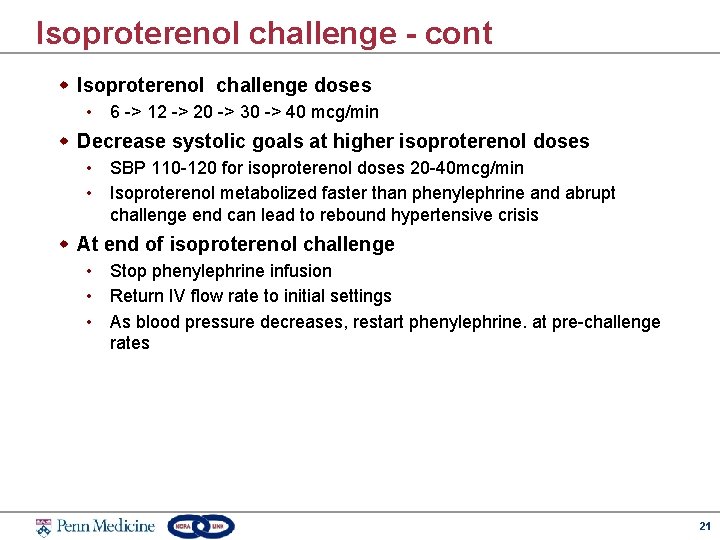
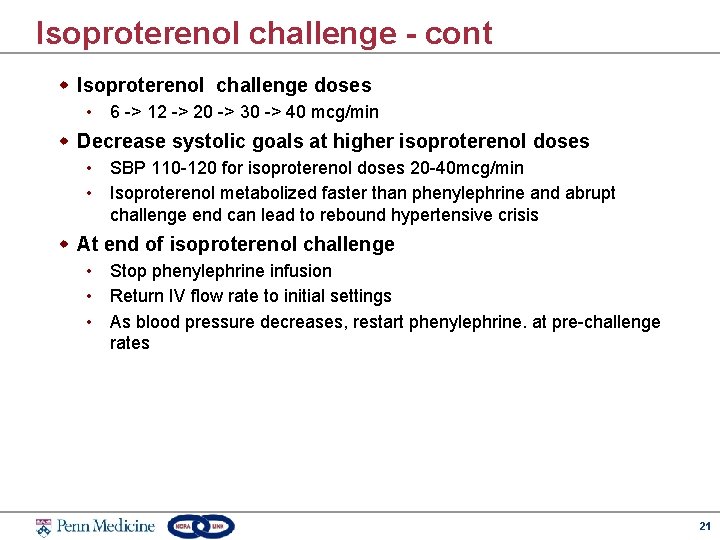
Isoproterenol challenge - cont w Isoproterenol challenge doses • 6 -> 12 -> 20 -> 30 -> 40 mcg/min w Decrease systolic goals at higher isoproterenol doses • SBP 110 -120 for isoproterenol doses 20 -40 mcg/min • Isoproterenol metabolized faster than phenylephrine and abrupt challenge end can lead to rebound hypertensive crisis w At end of isoproterenol challenge • Stop phenylephrine infusion • Return IV flow rate to initial settings • As blood pressure decreases, restart phenylephrine. at pre-challenge rates 21
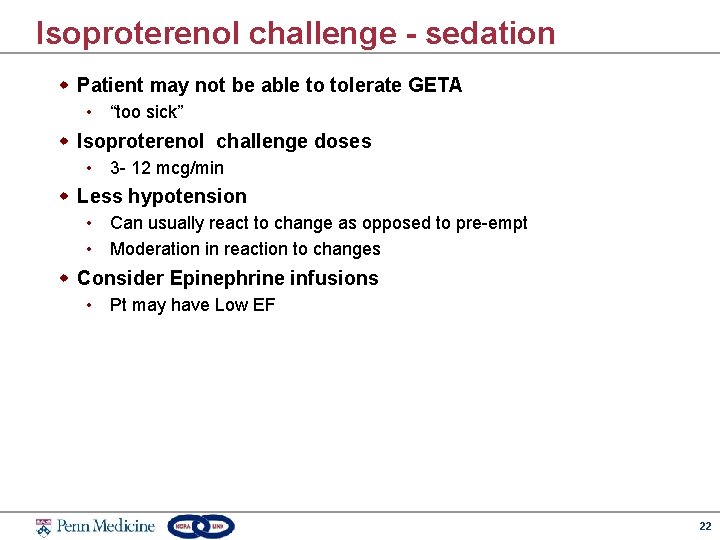
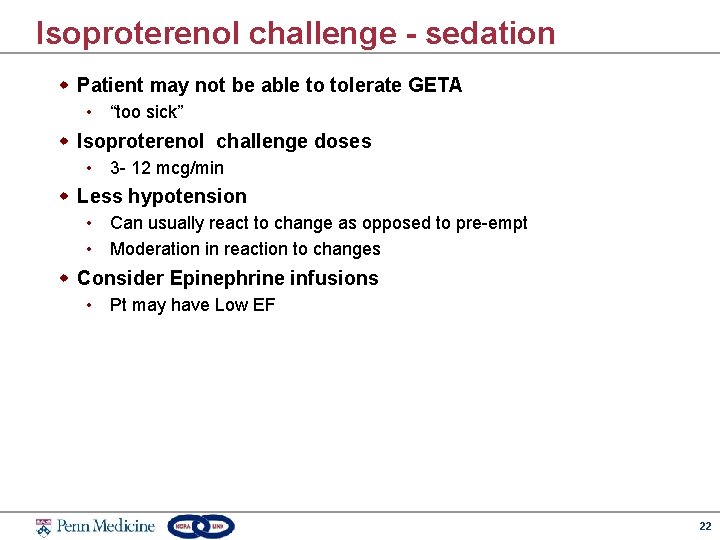
Isoproterenol challenge - sedation w Patient may not be able to tolerate GETA • “too sick” w Isoproterenol challenge doses • 3 - 12 mcg/min w Less hypotension • Can usually react to change as opposed to pre-empt • Moderation in reaction to changes w Consider Epinephrine infusions • Pt may have Low EF 22
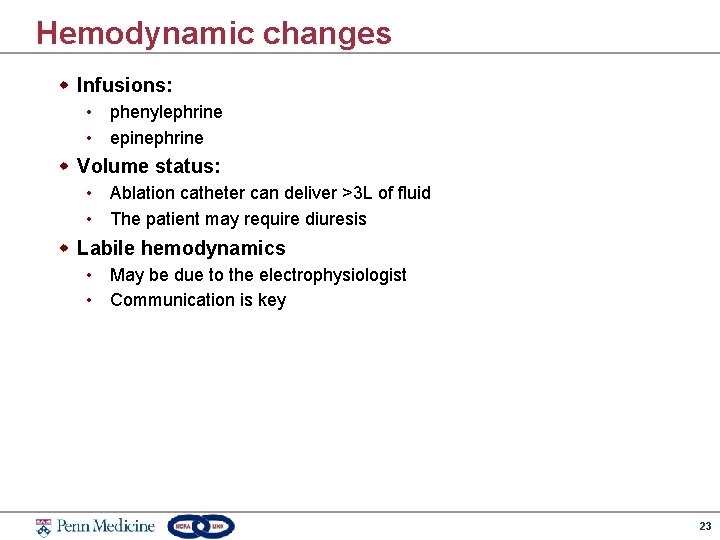
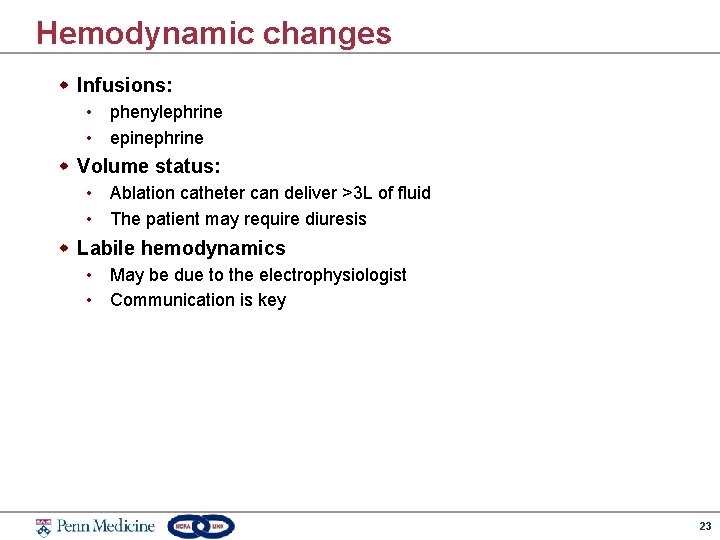
Hemodynamic changes w Infusions: • phenylephrine • epinephrine w Volume status: • Ablation catheter can deliver >3 L of fluid • The patient may require diuresis w Labile hemodynamics • May be due to the electrophysiologist • Communication is key 23
Tamponade 24
Postoperative Pain management w Pain generators • Back pain/Extremity pain for laying supine for prolonged period • Foley catheter • Intravascular Catheters in groin, need to hold pressure w Typical Pain medications: • Ketorolac typically given (avoid in renal impairment) • Morphine/Dilaudid to be considered w Ondansetron for PONV 25
Tips for success w Communication w Understanding procedures and their effects on hemodynamics as much as possible w Preparation and ensuring proper positioning, line set up w Comfort in a NORA setting 26

27
 Electrophysiology
Electrophysiology Cheryl weiss
Cheryl weiss Nathan weiss graduate college
Nathan weiss graduate college Daniel a weiss
Daniel a weiss Gary weiss fordham
Gary weiss fordham Richard weiss md
Richard weiss md Deanna weiss
Deanna weiss Optotipo pigassou
Optotipo pigassou Brian weiss quotes
Brian weiss quotes Weiss’ strategic framework for negotiating
Weiss’ strategic framework for negotiating You better wise up janet weiss
You better wise up janet weiss Haber weiss reaksiyonu
Haber weiss reaksiyonu Weiss reflex
Weiss reflex Ron weiss mit
Ron weiss mit Byron smith modified kuhnt szymanowski
Byron smith modified kuhnt szymanowski Paweł weiss usg
Paweł weiss usg Gorazd weiss
Gorazd weiss Michele weiss
Michele weiss Bernice weiss
Bernice weiss Miller indices (1-10)
Miller indices (1-10) Haber weiss
Haber weiss Hydrodynamics
Hydrodynamics Kierunki w sztuce 20 wieku
Kierunki w sztuce 20 wieku Peter weiss judr
Peter weiss judr Shifting dullness ascites
Shifting dullness ascites Dr noah weiss
Dr noah weiss Weiss wie kreide leicht wie flaum
Weiss wie kreide leicht wie flaum Dr. christoph weiss
Dr. christoph weiss