Anesthesia for Robotic Surgery May 12 th 2009
Anesthesia for Robotic Surgery May 12 th 2009 Department of Anesthesiology and Pain medicine Choi Sung Uk, MD, Ph. D
Contents u Introduction – History u Robotic System – da Vinci system – Advantages and Disadvantages – Current Applications u Anesthetic Concerns – General Surgery – Cardiac Surgery – Urologic Surgery u Summary
Introduction u Robotic device (technically) – “powered, computer controlled manipulator with artificial sensing that can be reprogrammed to move and position tools to carry out a wide range of tasks” – Autonomous device capable of various tasks
Introduction u Robots and Robotics – “Robot” • By the Czech brothers Karel and Josef Capek, in the play R. U. R (Rossum’s Universal Robots) in 1923 • The Czech word robota means drudgery – “Robotics” • By Isaac Asimov, in the short science fiction story "Runaround" in 1942
Introduction u In the future – Directed from vastly remote locations – Computer-controlled or autonomous function u Present-day – Mere instruments manipulated remotely by a surgeon using an electromechanical interface – Not autonomous
Introduction History u Surgical robotic systems grew out of the concept of telesurgery – First developed by the NASA for use in space exploration; Telemanipulators – Through virtual reality, the surgeon could be brought to the wounded soldiers’ side; Telepresence – Research in telemanipulation for remote mobile surgical units that would allow for telepresence by the Department of Defense
Introduction History u PUMA 560 – Neurosurgical biopsy by Kwoh et al. in 1988 u PROBOT – Robot-assisted TURP by Davies et al. in 1991
Introduction History u ROBODOC – First commercially available robotic system for orthopaedic hip surgery in 1992
Introduction History - ROBODOC
Introduction History u AESOP – Automated Endoscopic System for Optimal Positioning: voice-activated robotic arm for camera holder in 1994 (Computer Motion) – First approved surgical robotic system by FDA
Introduction History - AESOP
Introduction History u ZEUS – Marketed in 1998 (Computer Motion) – Transatlantic robot-assisted telesurgery between NY(USA) and Strasbourg(France) in 2001
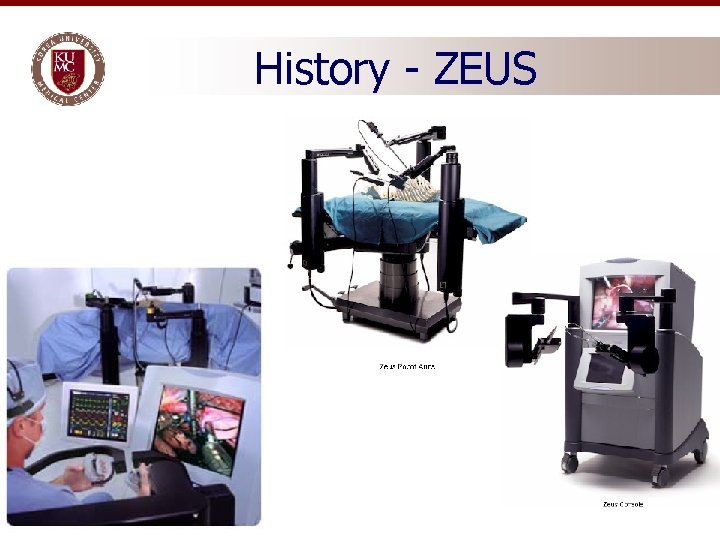
History - ZEUS
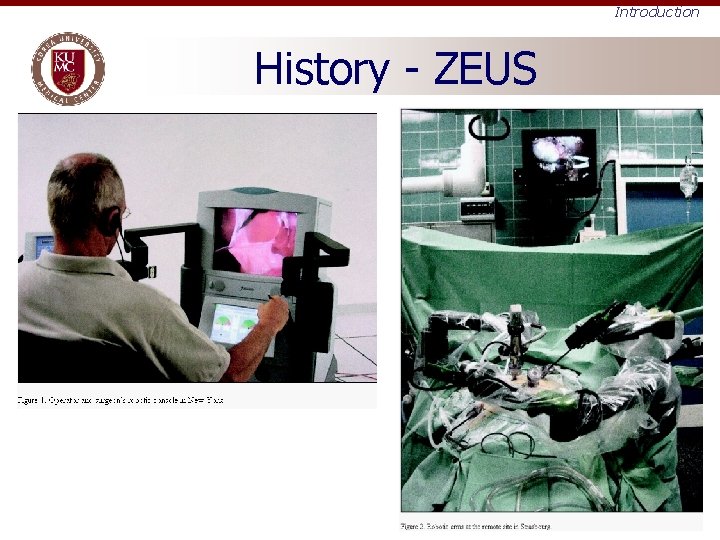
Introduction History - ZEUS
Introduction History u da Vinci – Initially developed by US Department of Defense in 1991 – Intuitive Surgical acquired the prototype and commercialized the system – Approved by FDA in July 2000
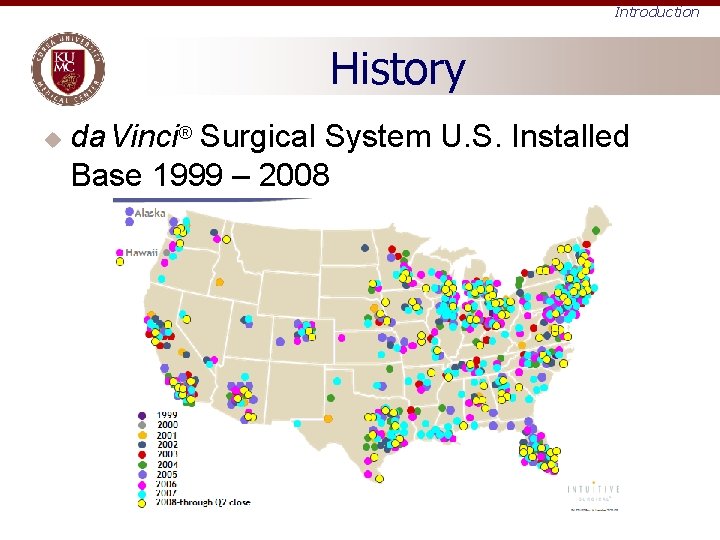
Introduction History u da Vinci® Surgical System U. S. Installed Base 1999 – 2008
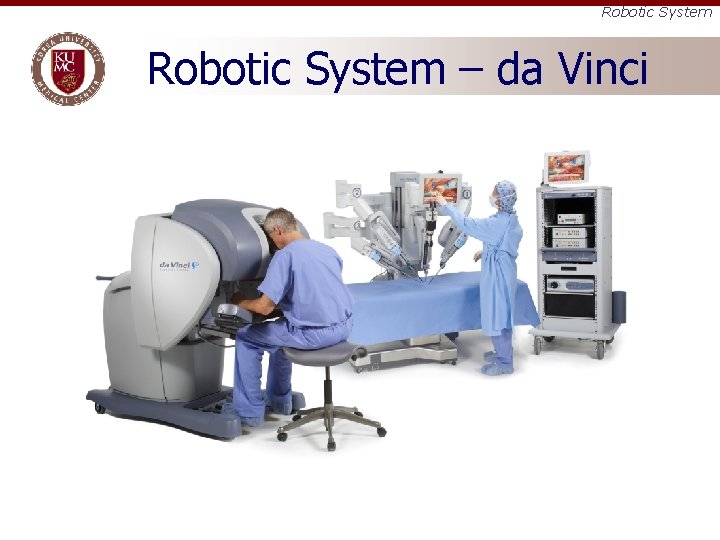
Robotic System – da Vinci
Robotic System – da Vinci
Robotic System Advantages over Laparoscopic Surgery 6 degrees of freedom compared to 4 degrees of freedom of laparoscopy u Magnification (10 -fold) u 3 -D view (=Depth perception) u Tremor filtration & Motion scaling u Better hand-eye coordination u Comfortable seat posture – ergonomic u Shorter learning curve u
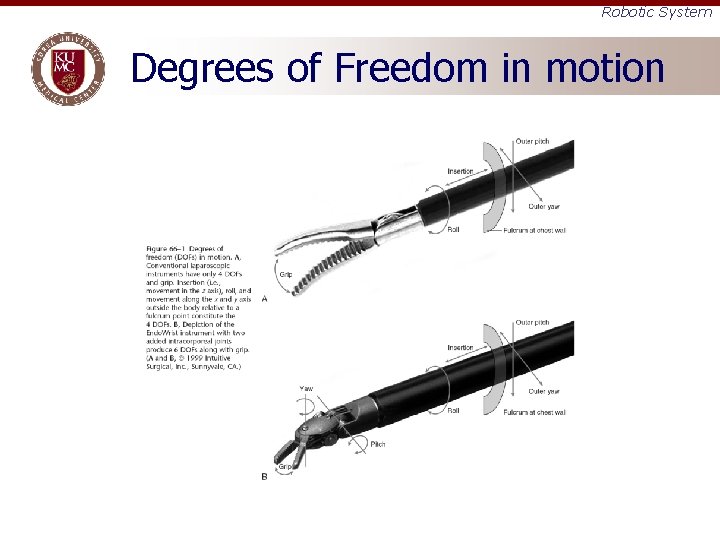
Robotic System Degrees of Freedom in motion
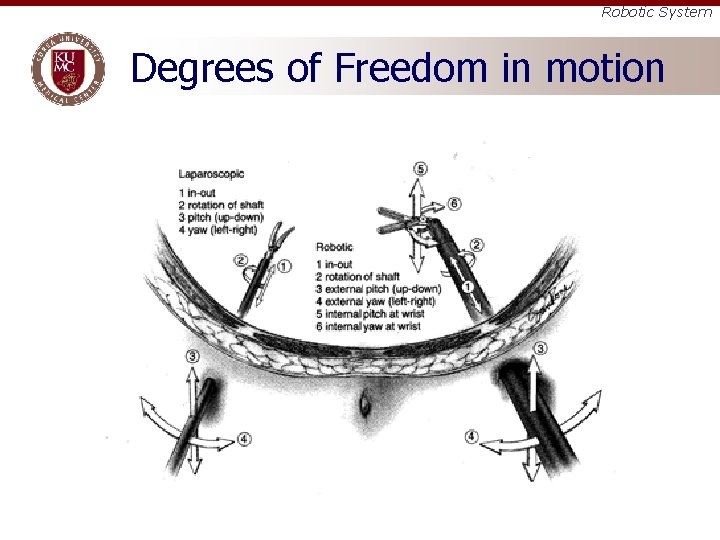
Robotic System Degrees of Freedom in motion
Robotic System Advantages over Laparoscopic Surgery More precision u Fewer traumas to the tissues u Less blood loss u Lesser adhesion u Less postoperative pain u Early ambulation u Lesser postoperative complications u
Robotic System Disadvantages or Limitation Lack of tactile sensation u Risk of break down u Surgical skills required u Prolonged operating times u Significant surgeon fatigue u Anesthetic complications u Cost-effectiveness of Robotic surgery – high installation and maintenance costs u
Robotic System Current Applications u Approved by FDA – – – – – Apr 1997 : General surgical assistance Jul 2000 : General laparoscopic procedures Mar 2001 : Non-cardiac thoracoscopic procedures May 2001 : Prostatectomy procedures Nov 2002 : Cardiotomy procedures Jul 2004 : Cardiac revascularization procedures Mar 2005 : Urologic surgical procedures Apr 2005 : Gynecologic surgical procedures Jun 2005 : Pediatric surgical procedures
Robotic System Current Applications u Urology – Radical prostatectomy, pyeloplasty, cystectomy, nephrectomy, ureteral reimplantation u Cardiothoracic – Mitral valve repair, ASD closure, PDA ligation, IMA mobilization and totally endoscopic CABG u Gynecology – Hysterectomy and myomectomy u Pediatrics – Pyeloplasty for ureteropelvic junction obstruction, gastroesophageal repair GERD, ligation of PDA u General Surgery – Cholecystectomy, Nissen fundoplication, Heller myotomy, gastric bypass, donor nephrectomy, adrenalectomy, splenectomy, bowel resection and thyroidectomy
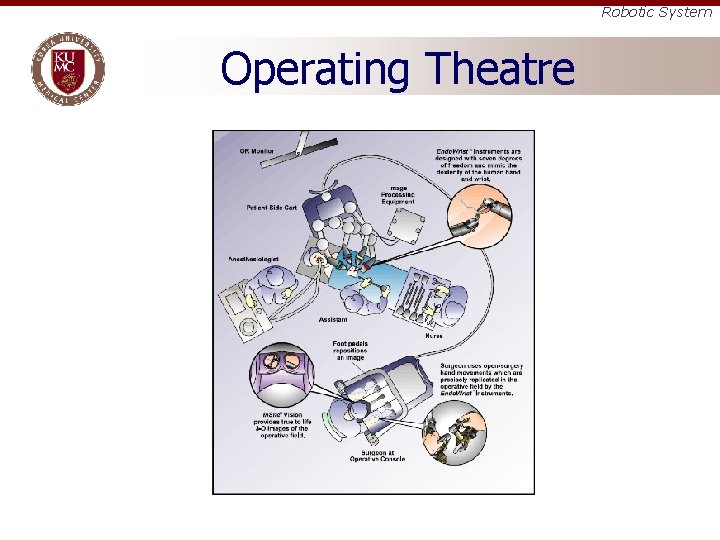
Robotic System Operating Theatre
Anesthetic Concerns u Several important issues related to and specific to robotic surgeries – Patient positioning – Duration of the procedure – Development of hypothermia – Hemodynamic and Respiratory effects of the pneumoperitoneum – Occult blood loss
Anesthetic Concerns Pathophysiological changes during laparoscopy u Cardiovascular effects – Depends on • Intra-abdominal pressure (IAP) • Patient position • Volume of CO 2 absorption • Patient’s intravascular volume • Ventilatory technique • Surgical condition • Anesthetic agents used
Anesthetic Concerns Pathophysiological changes during laparoscopy u Cardiovascular effects – IAP • Below 15 mm. Hg : increased C. O. – Blood from splanchnic venous bed is “squeezed” – Vasoconstriction due to sympathetic activation – > Increased venous return • Upper than 15 mm. Hg: decreased C. O. – Vena cava and other collateral vessel is compressed
Anesthetic Concerns Pathophysiological changes during laparoscopy u Cardiovascular effects – Bradyarrthymias • Includes bradycardia, AV dissociation, asystole • Due to vagal stimulation of trocar, peritoneal stretch, CO 2 embolization – Tacchyarrhythmias • Includes tachycardia, hypertension, VF • Due to increased CO 2 and catecholamines – Can be reduced when induction of pneumoperitoneum is done in supine position
Anesthetic Concerns Pathophysiological changes during laparoscopy u Respiratory effects – Compromises pulmonary function by • Diaphragmatic elevation • Early closure of small airways → atelectasis • Preferential ventilation of nondependent parts of the lung → V/Q mismatch • Risk of endobronchial intubation – In pulmonary compromised patients • Preoperative PFT and ABGA
Anesthetic Concerns Pathophysiological changes during laparoscopy u Neurologic effects – Increased ICP and decreased CPP • Increased SVR • Head-down position • Elevation of IAP • Hypercapnia – Should be cautious when intracranial compliance is reduced
Anesthetic Concerns General Surgery u Gastrointestinal Surgery – Supine position with reverse Trendelenburg – Robot over the patient’s head or at a 45° angle from the bed – Robotic arms in very close proximity to the patient’s airway, face, and chest – Rapid sequence induction with cricoid pressure – Muscle relaxation is paramount
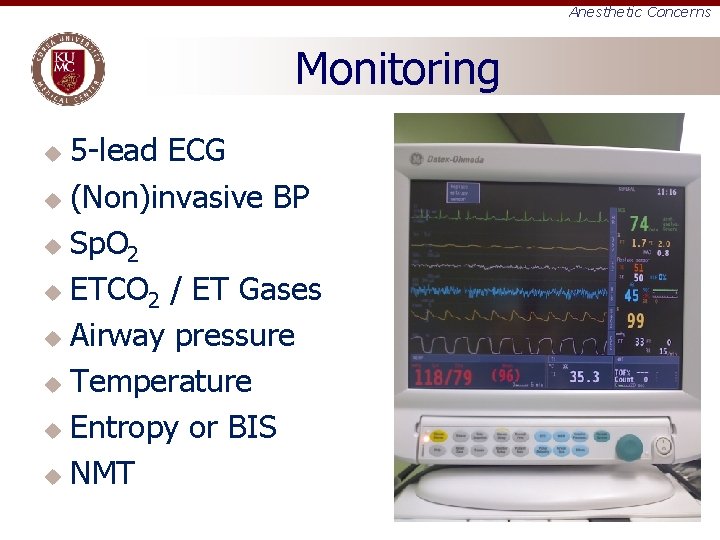
Anesthetic Concerns Monitoring 5 -lead ECG u (Non)invasive BP u Sp. O 2 u ETCO 2 / ET Gases u Airway pressure u Temperature u Entropy or BIS u NMT u
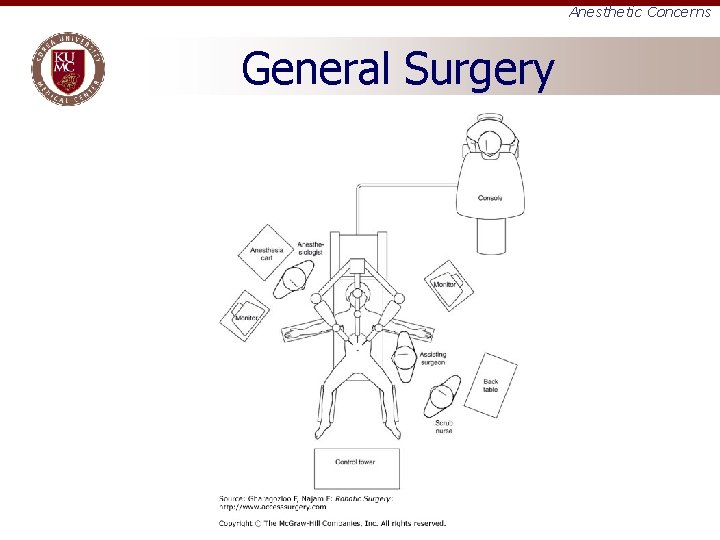
Anesthetic Concerns General Surgery
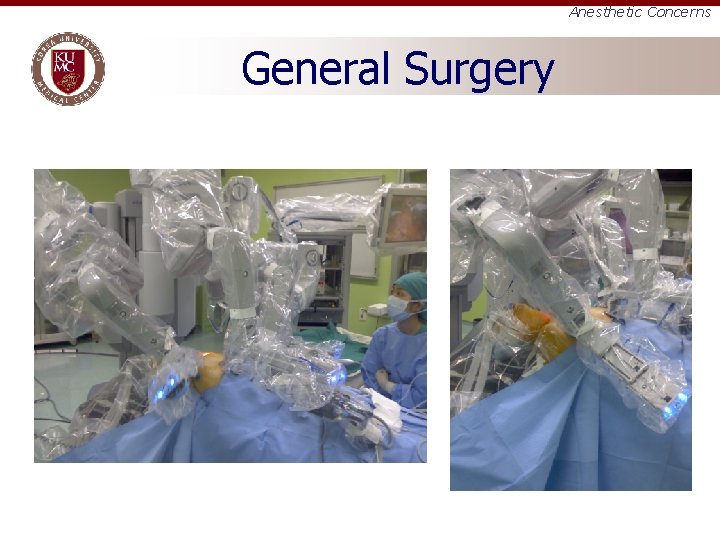
Anesthetic Concerns General Surgery
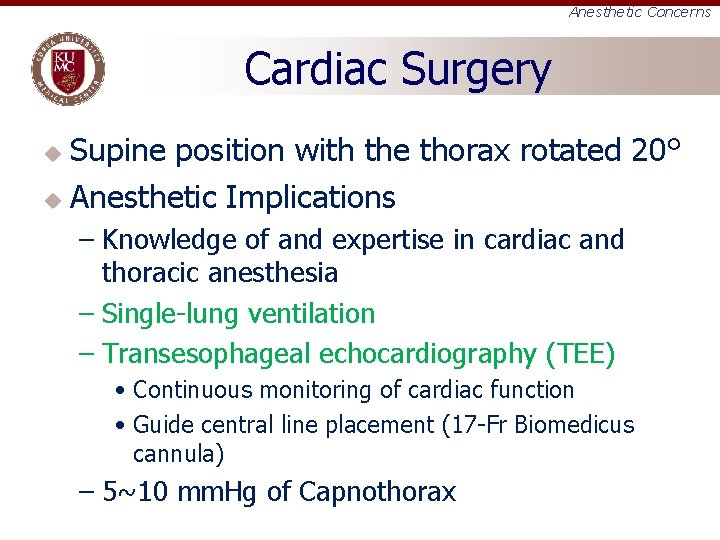
Anesthetic Concerns Cardiac Surgery Supine position with the thorax rotated 20° u Anesthetic Implications u – Knowledge of and expertise in cardiac and thoracic anesthesia – Single-lung ventilation – Transesophageal echocardiography (TEE) • Continuous monitoring of cardiac function • Guide central line placement (17 -Fr Biomedicus cannula) – 5~10 mm. Hg of Capnothorax
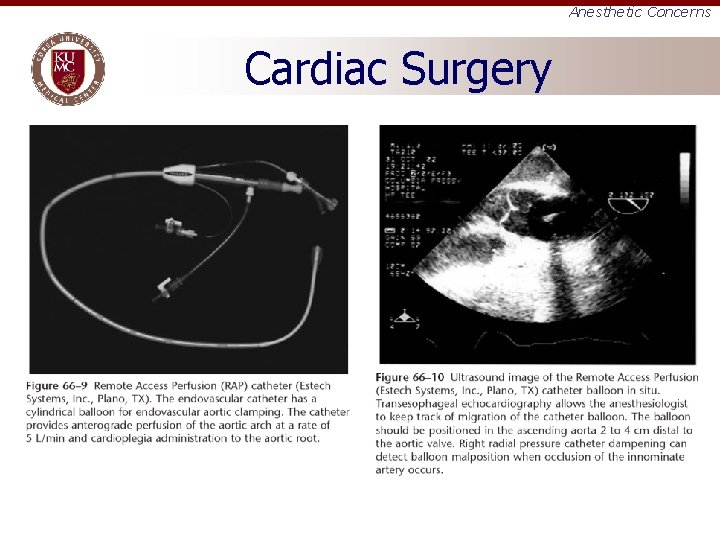
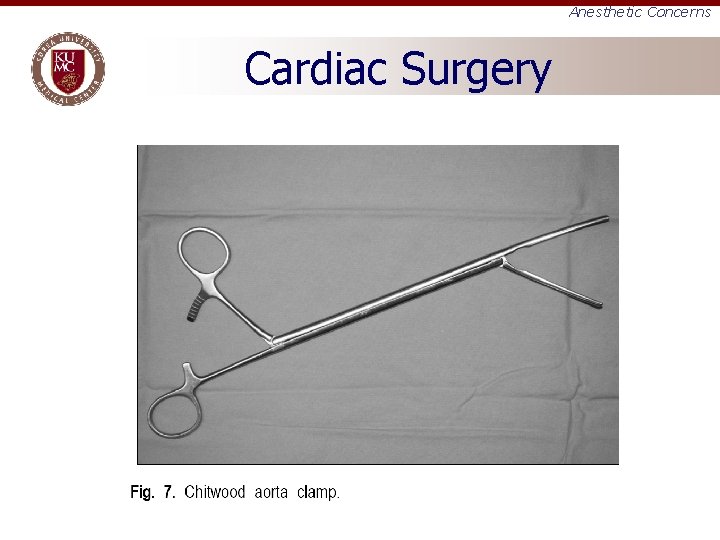
Anesthetic Concerns Cardiac Surgery
Anesthetic Concerns Cardiac Surgery
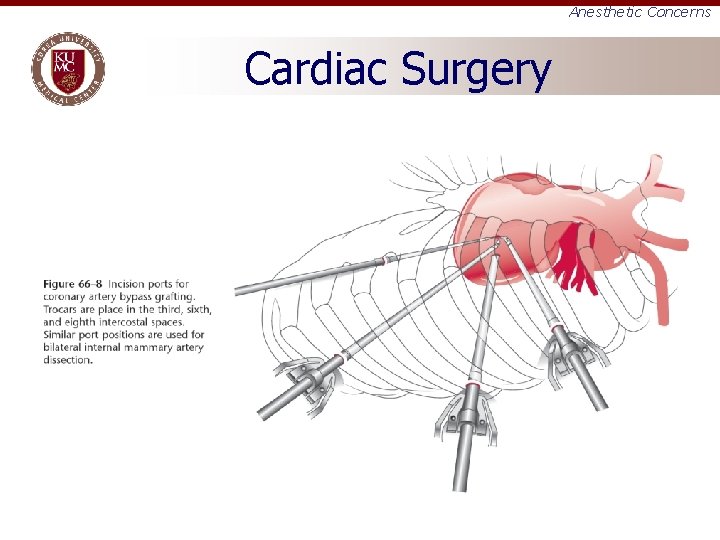
Anesthetic Concerns Cardiac Surgery
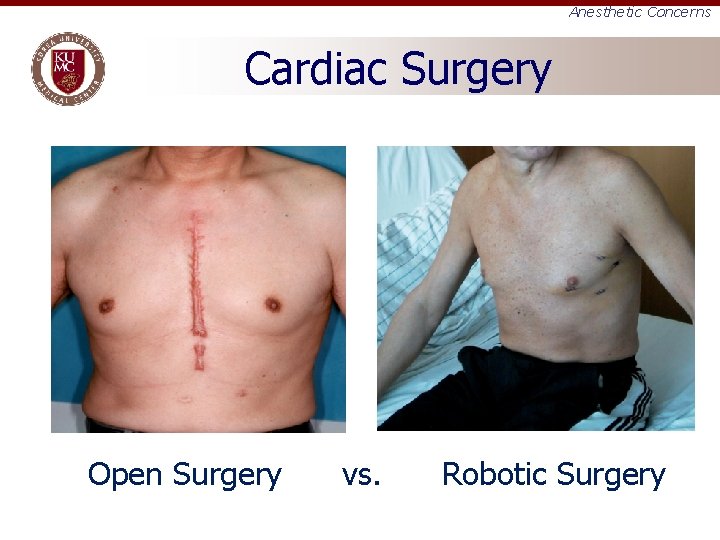
Anesthetic Concerns Cardiac Surgery Open Surgery vs. Robotic Surgery
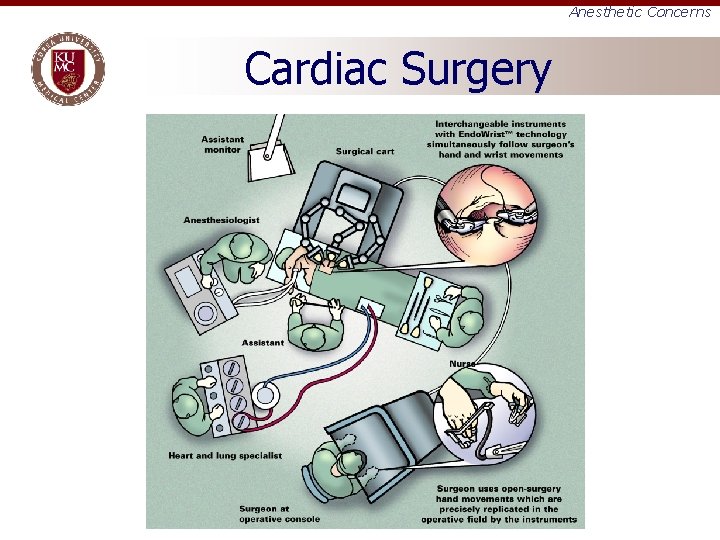
Anesthetic Concerns Cardiac Surgery
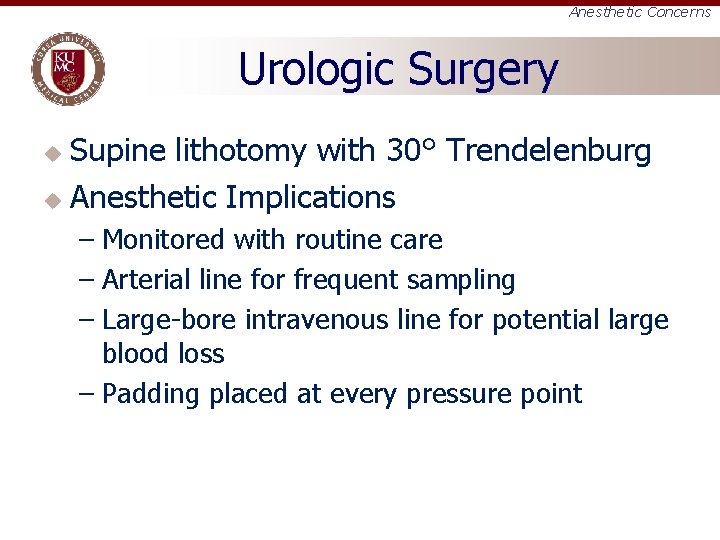
Anesthetic Concerns Urologic Surgery Supine lithotomy with 30° Trendelenburg u Anesthetic Implications u – Monitored with routine care – Arterial line for frequent sampling – Large-bore intravenous line for potential large blood loss – Padding placed at every pressure point
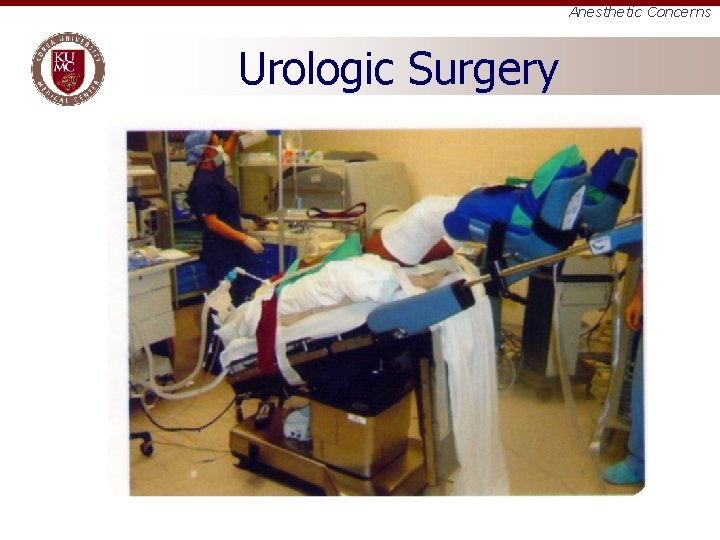
Anesthetic Concerns Urologic Surgery

Anesthetic Concerns Urologic Surgery
Anesthetic Concerns Urologic Surgery
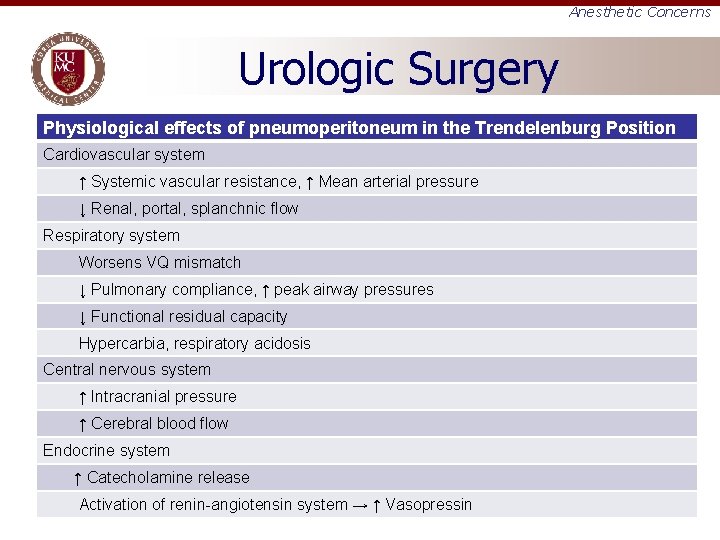
Anesthetic Concerns Urologic Surgery Physiological effects of pneumoperitoneum in the Trendelenburg Position Cardiovascular system ↑ Systemic vascular resistance, ↑ Mean arterial pressure ↓ Renal, portal, splanchnic flow Respiratory system Worsens VQ mismatch ↓ Pulmonary compliance, ↑ peak airway pressures ↓ Functional residual capacity Hypercarbia, respiratory acidosis Central nervous system ↑ Intracranial pressure ↑ Cerebral blood flow Endocrine system ↑ Catecholamine release Activation of renin-angiotensin system → ↑ Vasopressin
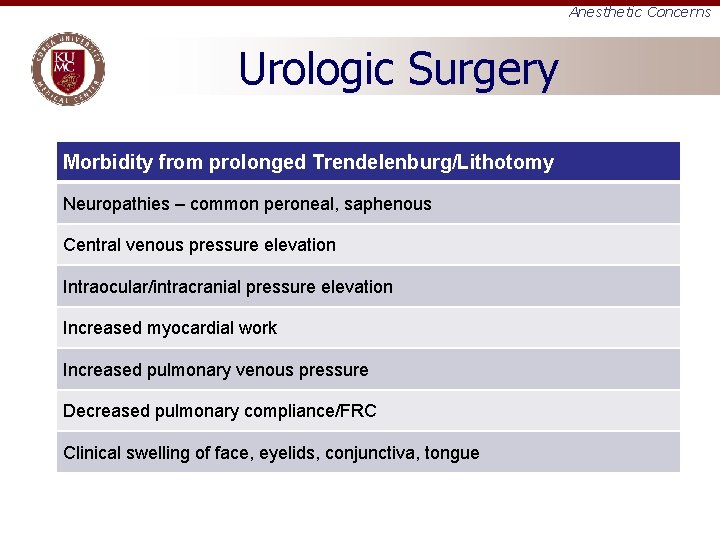
Anesthetic Concerns Urologic Surgery Morbidity from prolonged Trendelenburg/Lithotomy Neuropathies – common peroneal, saphenous Central venous pressure elevation Intraocular/intracranial pressure elevation Increased myocardial work Increased pulmonary venous pressure Decreased pulmonary compliance/FRC Clinical swelling of face, eyelids, conjunctiva, tongue
Summary u Future use of robotic technology in surgery is likely to increase at a rapid rate – – u Improved surgical precision Better visualization More intuitive/ergonomic instrument control Faster surgical learning curves for surgeons Anesthesiologists must be aware of these changes and adjust their practice in order to provide safe patient care
Questions and answers
- Slides: 53