ANEMIAS Dr Aamer Aleem Consultant Hematologist Associate Prof




- Slides: 70
ANEMIAS Dr. Aamer Aleem Consultant Hematologist Associate Prof. of Medicine KKUH & College of Medicine Riyadh
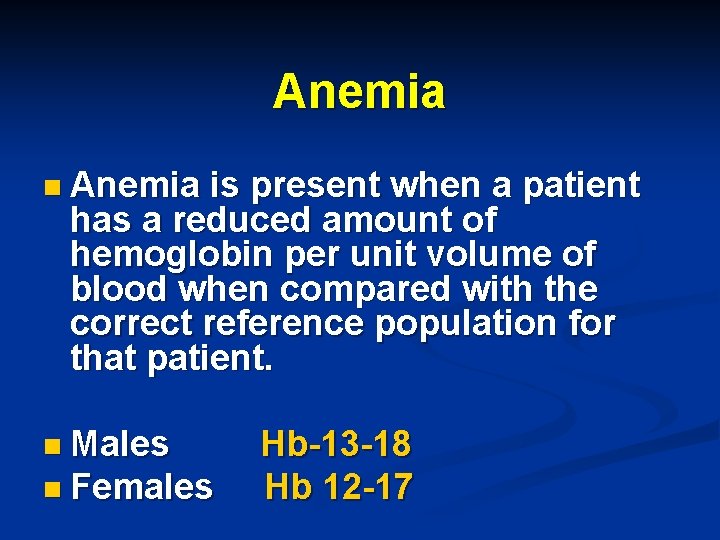
Anemia n Anemia is present when a patient has a reduced amount of hemoglobin per unit volume of blood when compared with the correct reference population for that patient. n Males n Females Hb-13 -18 Hb 12 -17
ANEMIA Single cell line(RBC) problem n Multiple cell line problem (RBC, WBC, Platelet) -Bone marrow suppression -immunologic disorders -peripheral destruction/sequestration n
Anemia n Anemia is generally defined as a hematocrit <40% (hemoglobin <13. 0 g/d. L) in men or <37% (hemoglobin <12. 0 g/d. L) in women. (WHO definition) Red blood cell (RBC) indices, which include the mean corpuscular volume (MCV), the mean corpuscular hemoglobin (MCH), the mean corpuscular hemoglobin content (MCHC), and the red-cell distribution width (RDW) index, are further used to define types of anemia.
Anemia Despite having a set of peculiar symptoms and signs, anemia is not a disease per se, but a syndrome, as it may arise from an extensive list of causes. n It is the chronic syndrome of highest prevalence in clinical medicine. n
Anemia Etiology Based on Hb, red cell indices, retic count and red cell morphology n (1) Inadequate response A. Hypochromic microcyctic B. Normochromic Normocytic C. Macrocytic n (2)Adequate response R/O blood loss---Includes Hemolytic disorders n
Anemia-symptoms n What are the symptoms of Anemia ? n General malaise, weakness, fatigue, breathlessness on exertion, palpitations, angina. n Desire to eat sand clay. n Menorrhagia common in women.
Symptoms of Anemia n n n The central nervous system, the heart and the muscle mass are the most affected organs, since they are the ones that most need oxygen for their functions. The symptoms increase with physical activity, as this consumes oxygen. With hemoglobin between 9 and 11 g/d. L there's irritability, headache and psychic asthenia; in the elder fatigability is observed, and angina may occur. With hemoglobin between 6 and 9 g/d. L there's tachycardia, dyspnea and fatigue upon the slightest effort. With hemoglobin below 6 g/d. L symptoms are
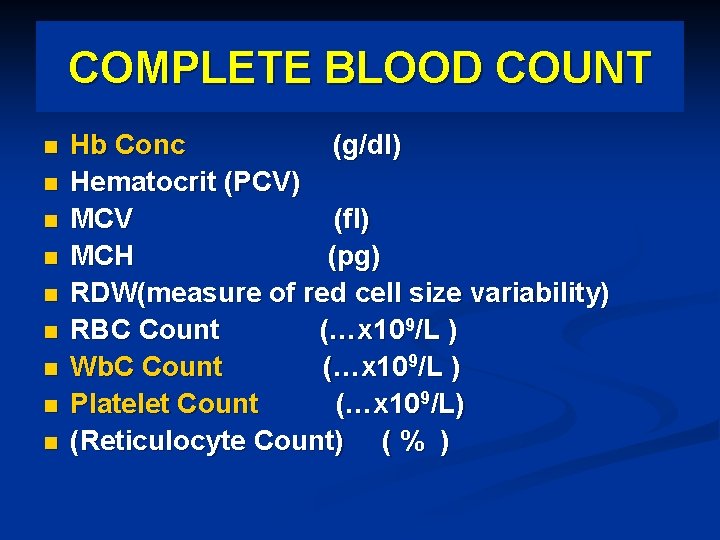
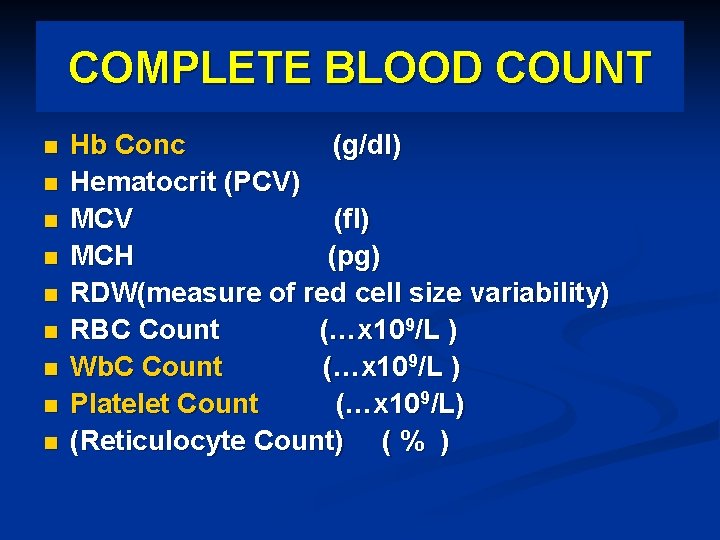
COMPLETE BLOOD COUNT n n n n n Hb Conc (g/dl) Hematocrit (PCV) MCV (fl) MCH (pg) RDW(measure of red cell size variability) RBC Count (…x 109/L ) Wb. C Count (…x 109/L ) Platelet Count (…x 109/L) (Reticulocyte Count) ( % )
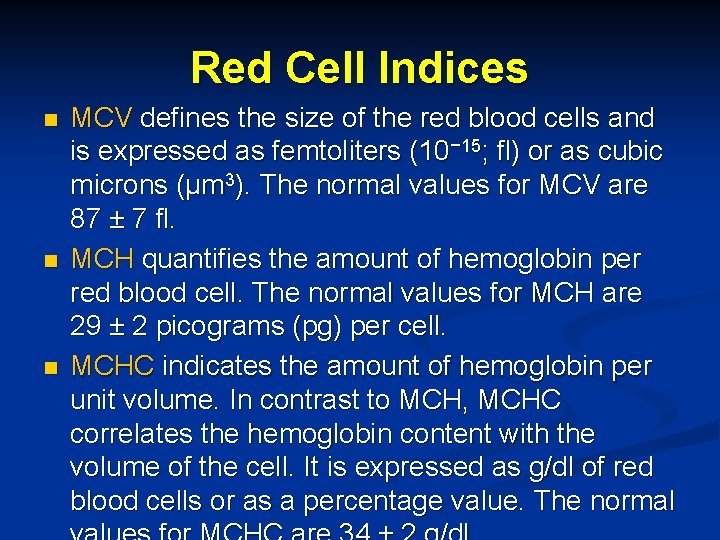
Red Cell Indices n n n MCV defines the size of the red blood cells and is expressed as femtoliters (10− 15; fl) or as cubic microns (μm 3). The normal values for MCV are 87 ± 7 fl. MCH quantifies the amount of hemoglobin per red blood cell. The normal values for MCH are 29 ± 2 picograms (pg) per cell. MCHC indicates the amount of hemoglobin per unit volume. In contrast to MCH, MCHC correlates the hemoglobin content with the volume of the cell. It is expressed as g/dl of red blood cells or as a percentage value. The normal
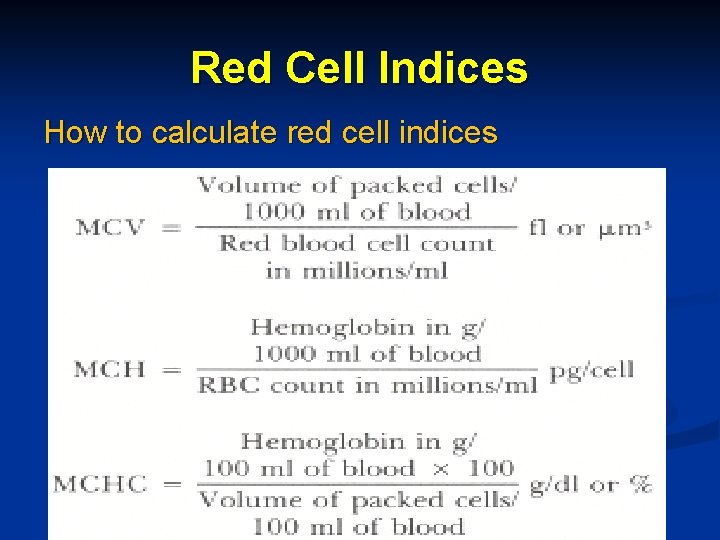
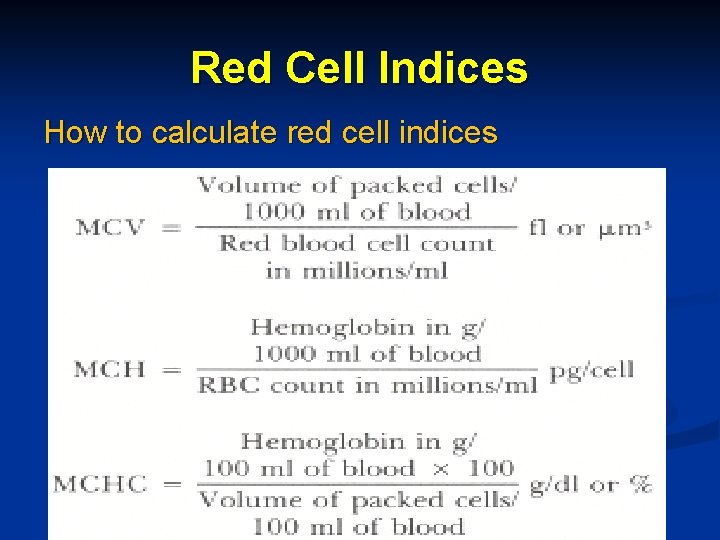
Red Cell Indices How to calculate red cell indices
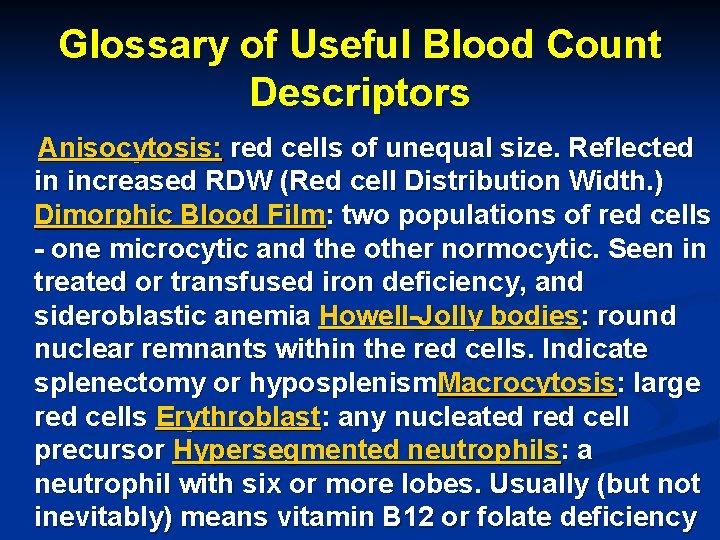
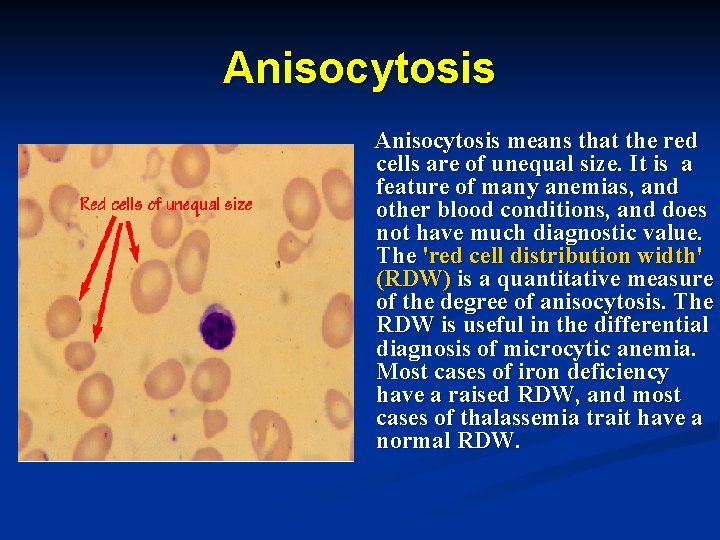
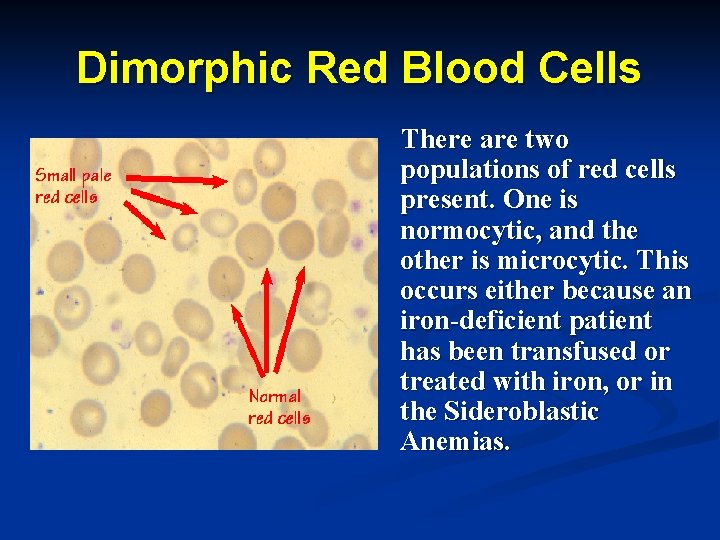
Glossary of Useful Blood Count Descriptors Anisocytosis: red cells of unequal size. Reflected in increased RDW (Red cell Distribution Width. ) Dimorphic Blood Film: two populations of red cells - one microcytic and the other normocytic. Seen in treated or transfused iron deficiency, and sideroblastic anemia Howell-Jolly bodies: round nuclear remnants within the red cells. Indicate splenectomy or hyposplenism. Macrocytosis: large red cells Erythroblast: any nucleated red cell precursor Hypersegmented neutrophils: a neutrophil with six or more lobes. Usually (but not inevitably) means vitamin B 12 or folate deficiency
Glossary of Useful Blood Count Descriptors Hypochromia: pale red cells. Always accompanied by microcytosis Leukoerythroblastic: the presence of erythroblasts and myelocytes (which are precursors of mature cells) in the blood. Often indicates marrow infiltration eg by secondary cancer or fibrosis Microangiopathy: indicates mechanical damage to red cells with red cell fragments on the blood film. Microcytosis: small red cells Poikilocytosis: a traditional term for red cells of unequal shape Polychromasia: grey coloured cells on film, indicating presence of increased reticulocytes Reticulocyte: an erythrocyte newly released from the bone marrow
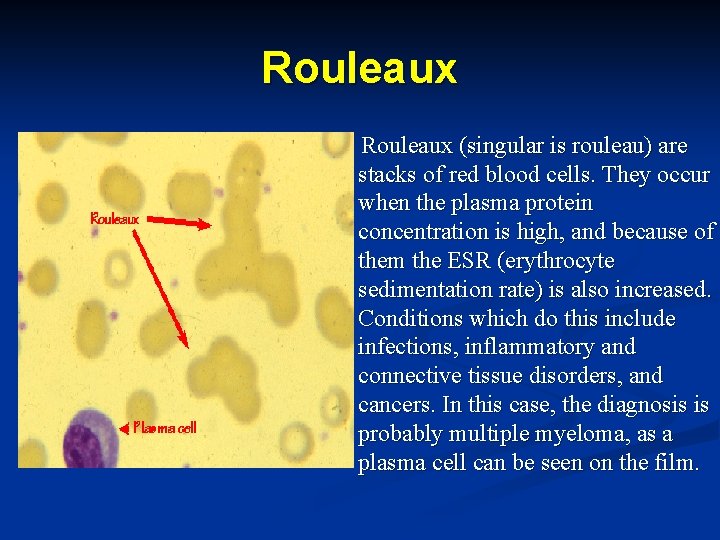
n n n Glossary of Useful Blood Count Descriptors Rouleaux: red cells in stacks, as coins. Indicates high ESR, eg infection, myeloma, cancer, collagen disease, TB etc. Schistocyte: a red cell which has undergone mechanical damage - synonymous with red cell fragment Spherocyte: a spherical red cell due to disproportionate membrane loss. Either inherited, or acquired from (usually) immune causes Sickle cell: a crescent-shaped red cell characteristic of Sickle Cell Anemia Target cell: red cell with central area of Hb giving the appearance of a target. Seen in many
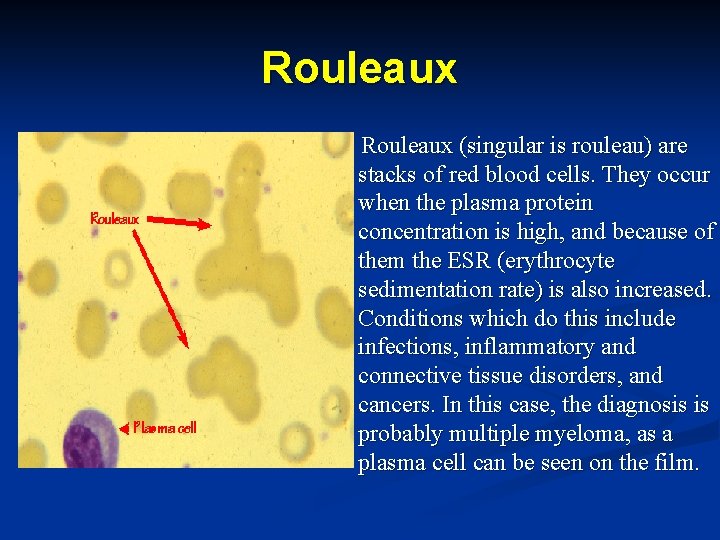
Rouleaux (singular is rouleau) are stacks of red blood cells. They occur when the plasma protein concentration is high, and because of them the ESR (erythrocyte sedimentation rate) is also increased. Conditions which do this include infections, inflammatory and connective tissue disorders, and cancers. In this case, the diagnosis is probably multiple myeloma, as a plasma cell can be seen on the film.
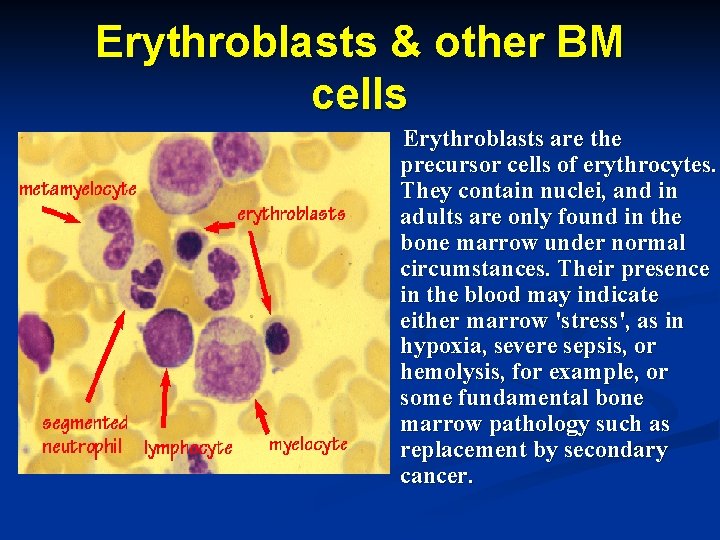
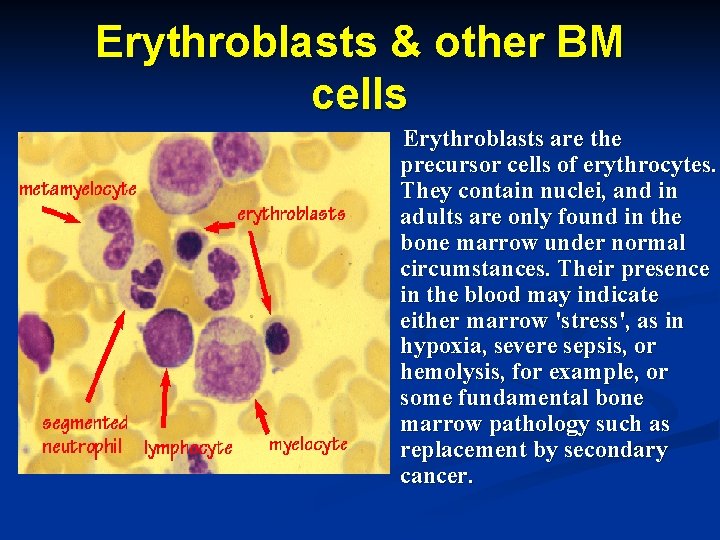
Erythroblasts & other BM cells Erythroblasts are the precursor cells of erythrocytes. They contain nuclei, and in adults are only found in the bone marrow under normal circumstances. Their presence in the blood may indicate either marrow 'stress', as in hypoxia, severe sepsis, or hemolysis, for example, or some fundamental bone marrow pathology such as replacement by secondary cancer.
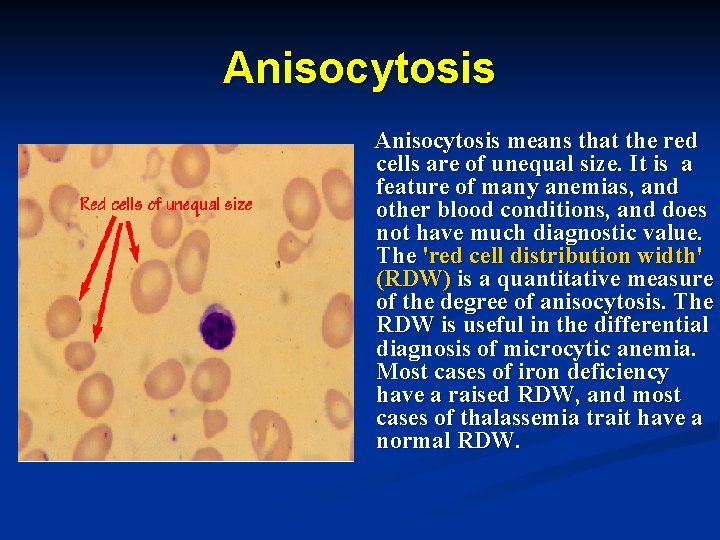
Anisocytosis means that the red cells are of unequal size. It is a feature of many anemias, and other blood conditions, and does not have much diagnostic value. The 'red cell distribution width' (RDW) is a quantitative measure of the degree of anisocytosis. The RDW is useful in the differential diagnosis of microcytic anemia. Most cases of iron deficiency have a raised RDW, and most cases of thalassemia trait have a normal RDW.
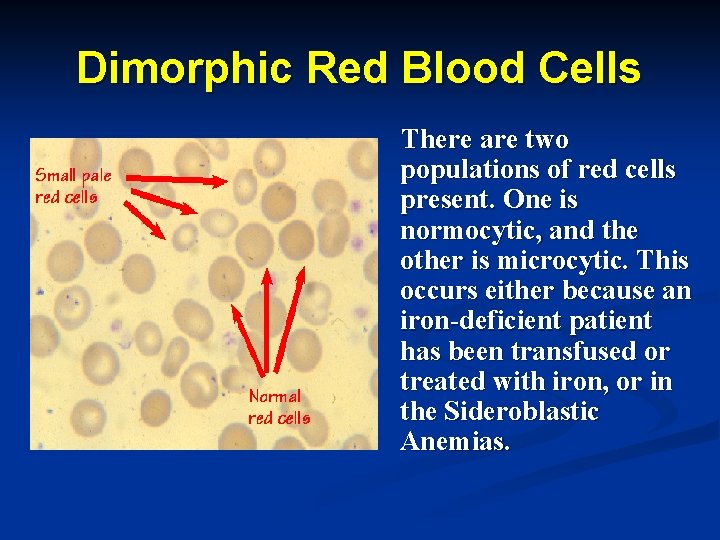
Dimorphic Red Blood Cells There are two populations of red cells present. One is normocytic, and the other is microcytic. This occurs either because an iron-deficient patient has been transfused or treated with iron, or in the Sideroblastic Anemias.
Anemia-diagnosis n How can we diagnose Anemia ? Blood tests to detect the various components of blood is carried out for proper diagnosis. Red blood cell count may be normal or decreased. Peripheral blood smear shows pale small cells. White blood cell count normal or decreased
Classification of anemia n n n Anemia can be either acute or chronic. In acute anemia (sudden loss of blood), the lack of blood volume in the circulatory system is more important than the deficiency of hemoglobin. A loss up to 10% of blood volume, as that taking place upon blood donation, is well tolerated. Losses between 10 and 20% cause postural hypotension, dizziness and faint. In losses above 20%, there's tachycardia, cold extremities, extreme paleness and hypotension, followed by shock; should the loss surmount 30%, without immediate replacement of intravenous fluids, the shock rapidly becomes irreversible and fatal. In chronic anemia, there's no decrease in blood
Classification of anemia Based on MCV n Microcytic anemia n Normocytic anemia n Macrocytic anemai
Classification of anemia Based on underlying process n Blood loss or def. of nutrients n Hemolysis n Failure of production
A diagnostic scheme for anemias Determine the MCV n The most useful initial approach to anemia is based on red cell size. The Mean Corpuscular Volume (MCV) represents a direct measurement of red cell size. When this is reduced, the anemia is referred to as microcytic. It is macrocytic when the MCV is increased, and normocytic when the MCV is normal.
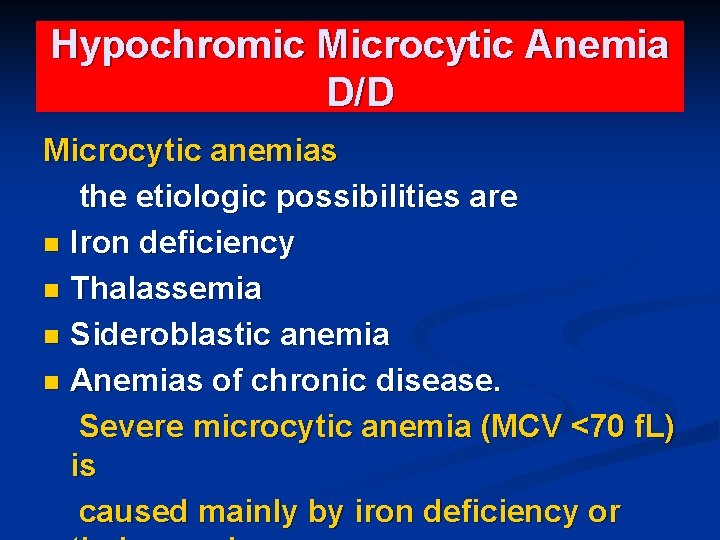
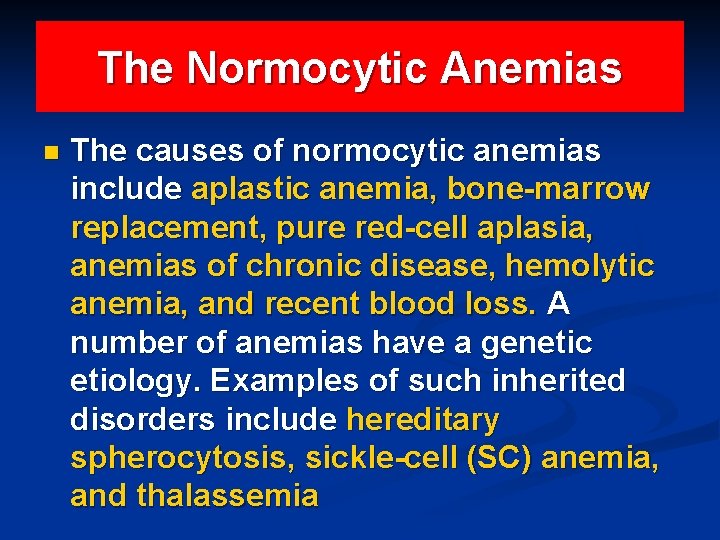
Anemia-classification n One way to classify anemia is by RBC size (i. e. , MCV), as microcytic, macrocytic, or normocytic. For the microcytic anemias, the etiologic possibilities are iron deficiency, thalassemia, sideroblastic anemia, and the anemias of chronic disease. Severe microcytic anemia (MCV <70 f. L) is caused mainly by iron deficiency or thalassemia. Macrocytic anemia may be the result of megaloblastic (folate or vitamin B 12 deficiency) or nonmegaloblastic causes. Folate deficiency can in turn be due to either reduced intake or diminished absorption. Severe macrocytic anemia (MCV >125 f. L) is almost always megaloblastic. In some rare cases, macrocytic anemia is related to the myelodysplastic syndromes prior to or after chemotherapy. n The causes of normocytic anemias include aplastic anemia, bone-marrow replacement, pure red-cell aplasia, anemias of chronic disease, hemolytic anemia, and recent blood loss. A number of anemias have a genetic etiology. Examples of such

Hypochromic Microcytic Anemia D/D Microcytic anemias the etiologic possibilities are n Iron deficiency n Thalassemia n Sideroblastic anemia n Anemias of chronic disease. Severe microcytic anemia (MCV <70 f. L) is caused mainly by iron deficiency or
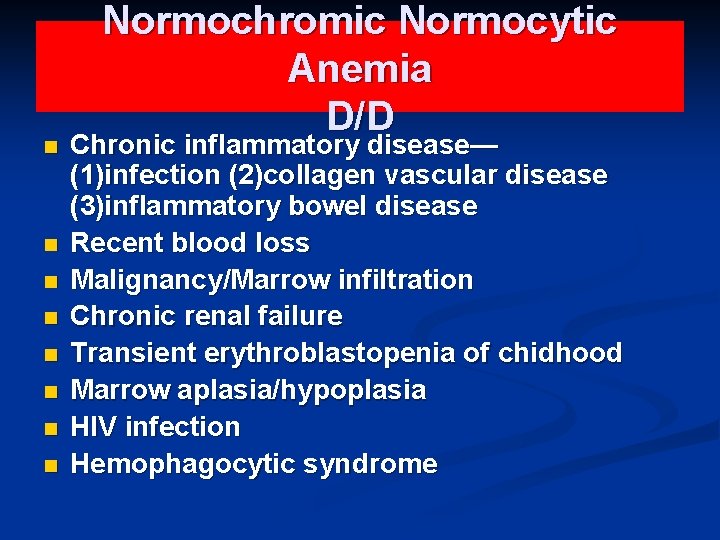
n n n n Normochromic Normocytic Anemia D/D Chronic inflammatory disease— (1)infection (2)collagen vascular disease (3)inflammatory bowel disease Recent blood loss Malignancy/Marrow infiltration Chronic renal failure Transient erythroblastopenia of chidhood Marrow aplasia/hypoplasia HIV infection Hemophagocytic syndrome
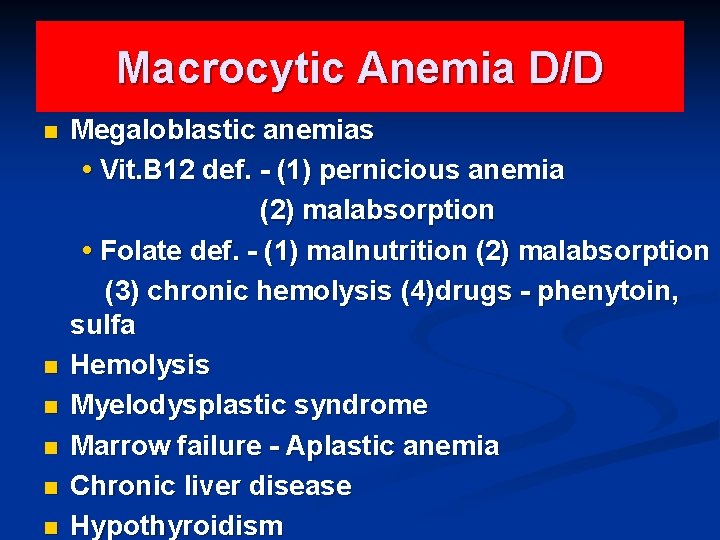
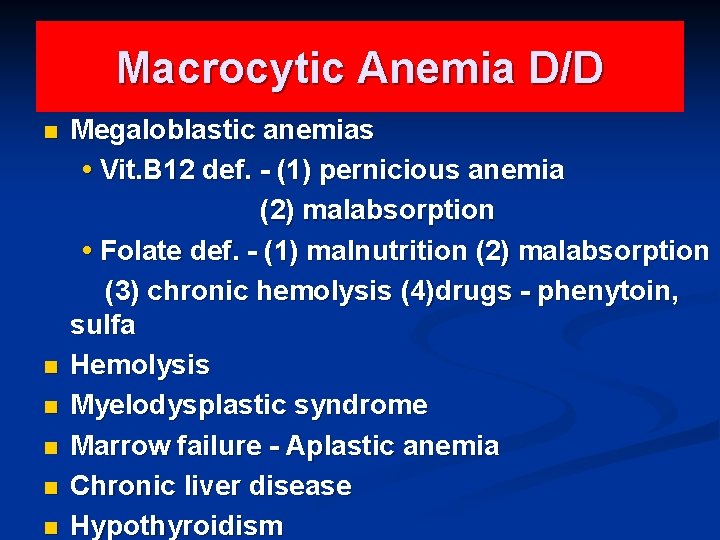
Macrocytic Anemia D/D n n n Megaloblastic anemias • Vit. B 12 def. - (1) pernicious anemia (2) malabsorption • Folate def. - (1) malnutrition (2) malabsorption (3) chronic hemolysis (4)drugs - phenytoin, sulfa Hemolysis Myelodysplastic syndrome Marrow failure - Aplastic anemia Chronic liver disease Hypothyroidism
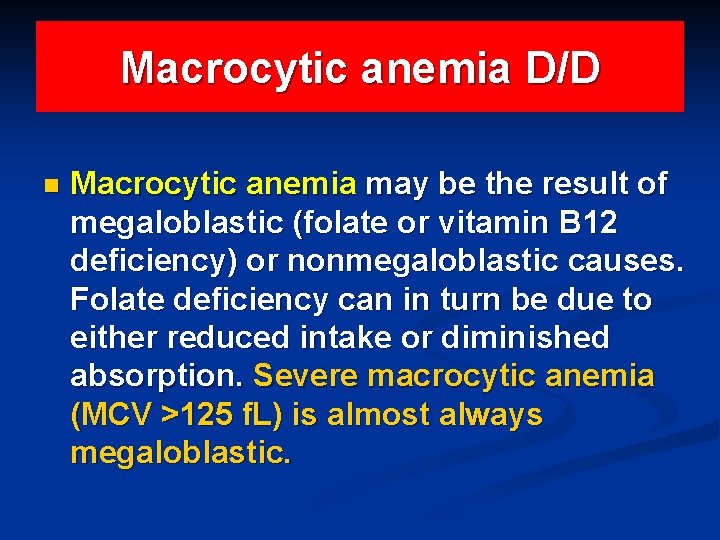
Macrocytic anemia D/D n Macrocytic anemia may be the result of megaloblastic (folate or vitamin B 12 deficiency) or nonmegaloblastic causes. Folate deficiency can in turn be due to either reduced intake or diminished absorption. Severe macrocytic anemia (MCV >125 f. L) is almost always megaloblastic.
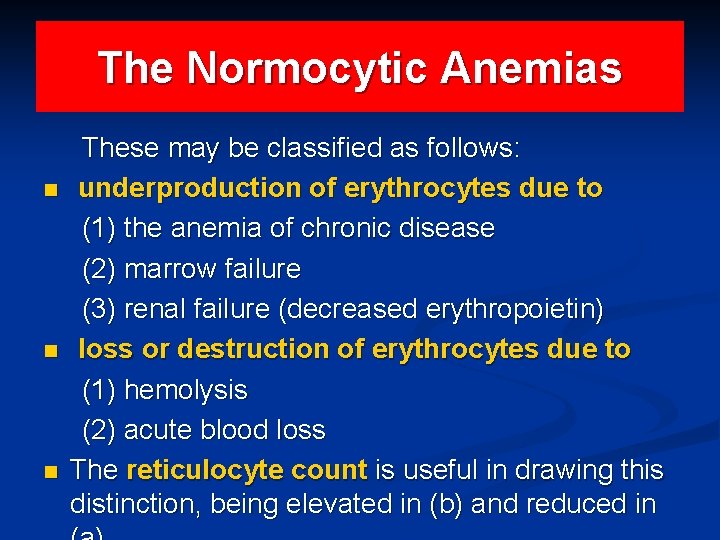
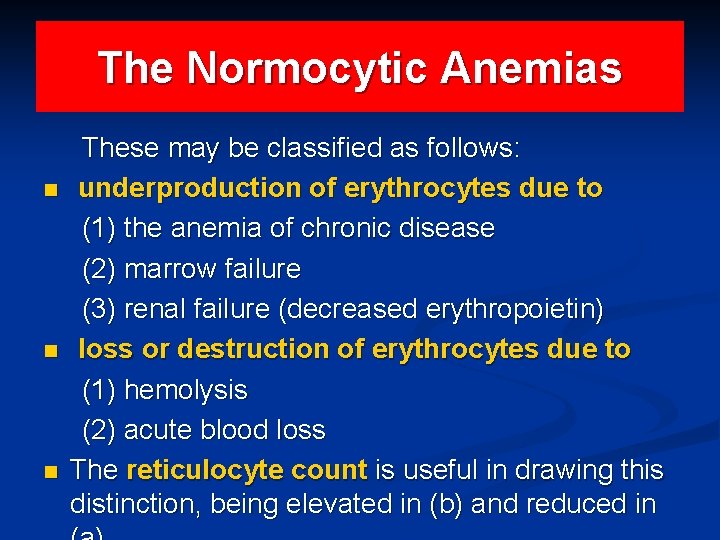
The Normocytic Anemias n n n These may be classified as follows: underproduction of erythrocytes due to (1) the anemia of chronic disease (2) marrow failure (3) renal failure (decreased erythropoietin) loss or destruction of erythrocytes due to (1) hemolysis (2) acute blood loss The reticulocyte count is useful in drawing this distinction, being elevated in (b) and reduced in
The Normocytic Anemias n The causes of normocytic anemias include aplastic anemia, bone-marrow replacement, pure red-cell aplasia, anemias of chronic disease, hemolytic anemia, and recent blood loss. A number of anemias have a genetic etiology. Examples of such inherited disorders include hereditary spherocytosis, sickle-cell (SC) anemia, and thalassemia
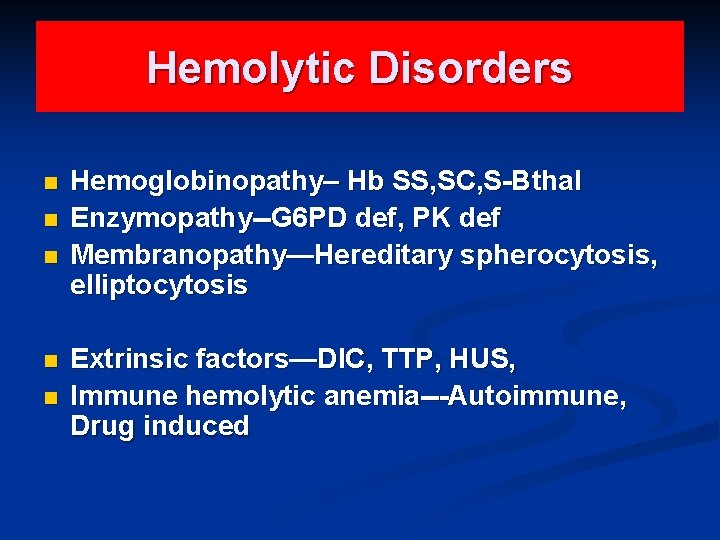
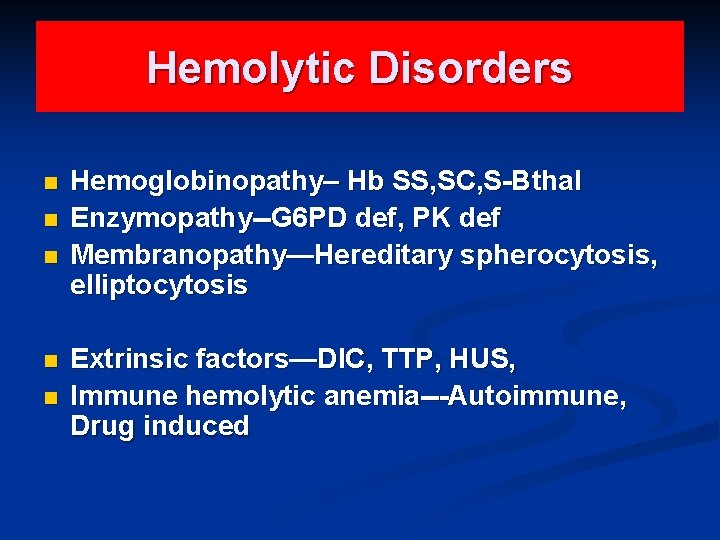
Hemolytic Disorders n n n Hemoglobinopathy– Hb SS, SC, S-Bthal Enzymopathy--G 6 PD def, PK def Membranopathy—Hereditary spherocytosis, elliptocytosis Extrinsic factors—DIC, TTP, HUS, Immune hemolytic anemia---Autoimmune, Drug induced

Diagnostic Approach-History n n Age : Iron def rare without blood loss before 6 months in term infants. Family Hist &Genetics: (1)X-linked: G 6 PD deficiency (2)Aut dominant: Spherocytosis (3)Aut recessive: Sickle cell, Fanconi anemia (4)Family member with early age of cholecystectomy/splenectomy (5)Ethnicity (Thalassemia: Mediterranean; G 6 PD def: (Greeks, Blacks, Middle eastern) (6)Race: Bthal: Mediterranean, African, Asian; A-thal: Blacks, Asians
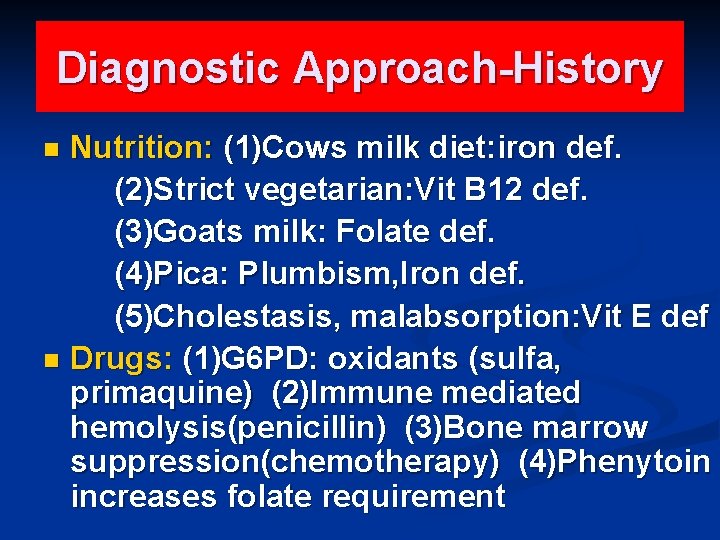
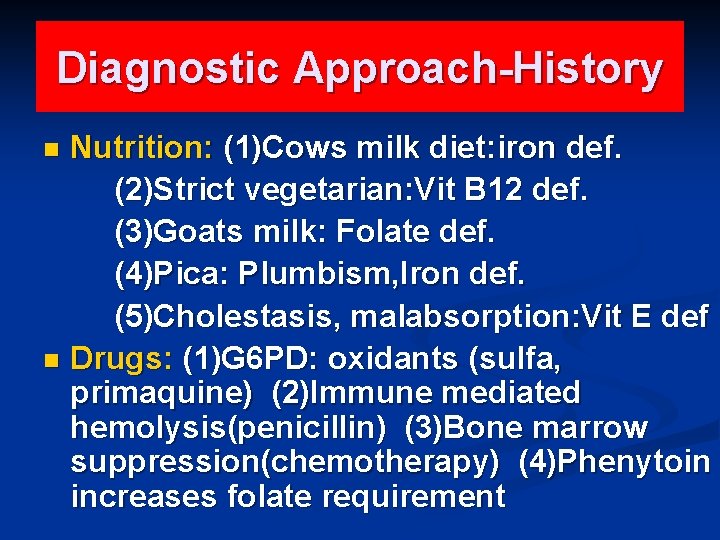
Diagnostic Approach-History Nutrition: (1)Cows milk diet: iron def. (2)Strict vegetarian: Vit B 12 def. (3)Goats milk: Folate def. (4)Pica: Plumbism, Iron def. (5)Cholestasis, malabsorption: Vit E def n Drugs: (1)G 6 PD: oxidants (sulfa, primaquine) (2)Immune mediated hemolysis(penicillin) (3)Bone marrow suppression(chemotherapy) (4)Phenytoin increases folate requirement n
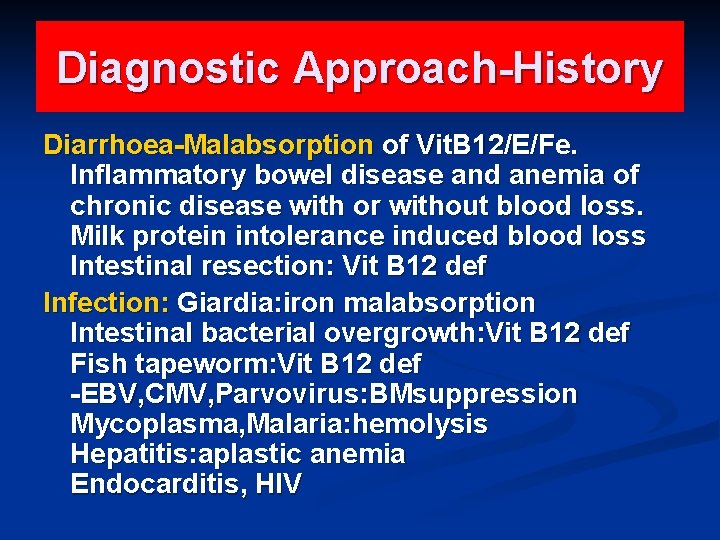
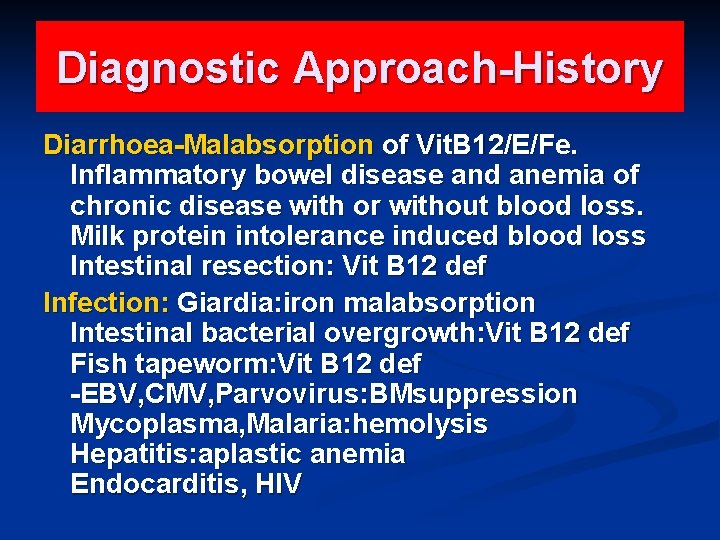
Diagnostic Approach-History Diarrhoea-Malabsorption of Vit. B 12/E/Fe. Inflammatory bowel disease and anemia of chronic disease with or without blood loss. Milk protein intolerance induced blood loss Intestinal resection: Vit B 12 def Infection: Giardia: iron malabsorption Intestinal bacterial overgrowth: Vit B 12 def Fish tapeworm: Vit B 12 def -EBV, CMV, Parvovirus: BMsuppression Mycoplasma, Malaria: hemolysis Hepatitis: aplastic anemia Endocarditis, HIV
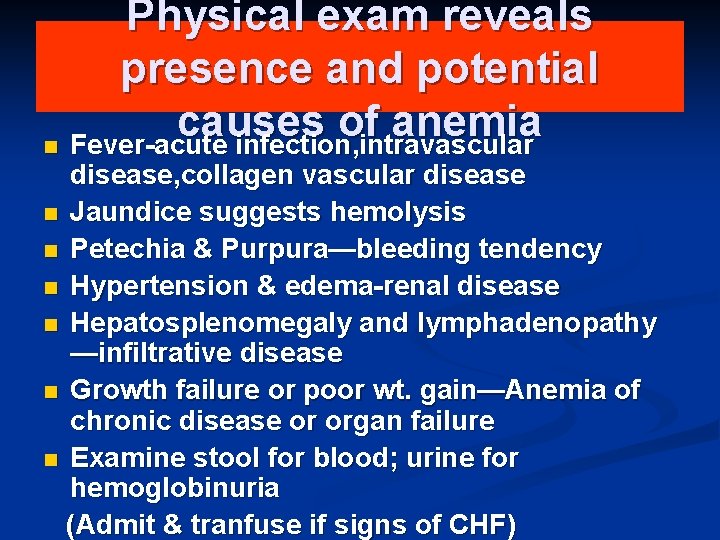
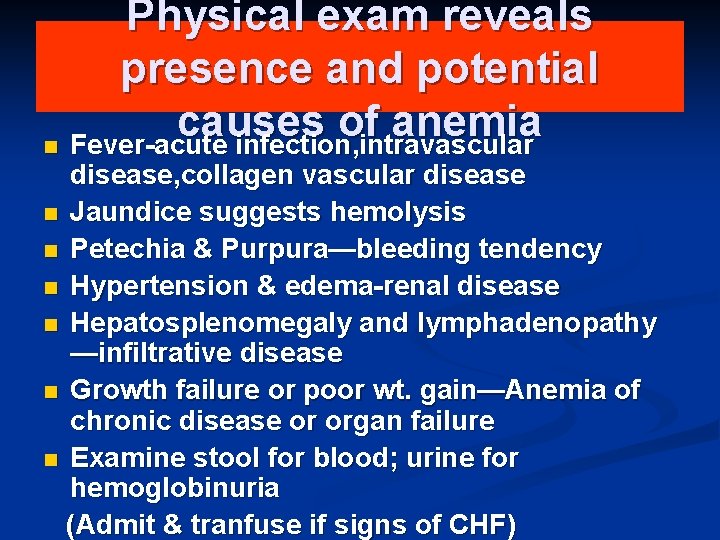
Physical exam reveals presence and potential causes of anemia n Fever-acute infection, intravascular disease, collagen vascular disease n Jaundice suggests hemolysis n Petechia & Purpura—bleeding tendency n Hypertension & edema-renal disease n Hepatosplenomegaly and lymphadenopathy —infiltrative disease n Growth failure or poor wt. gain—Anemia of chronic disease or organ failure n Examine stool for blood; urine for hemoglobinuria (Admit & tranfuse if signs of CHF)
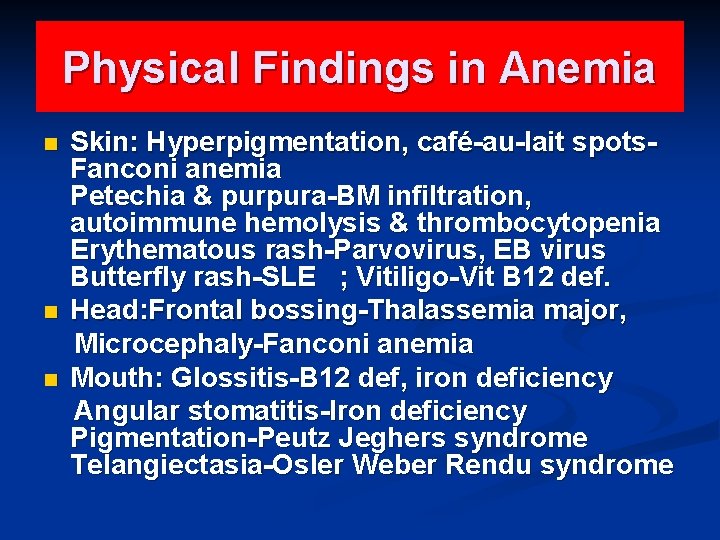
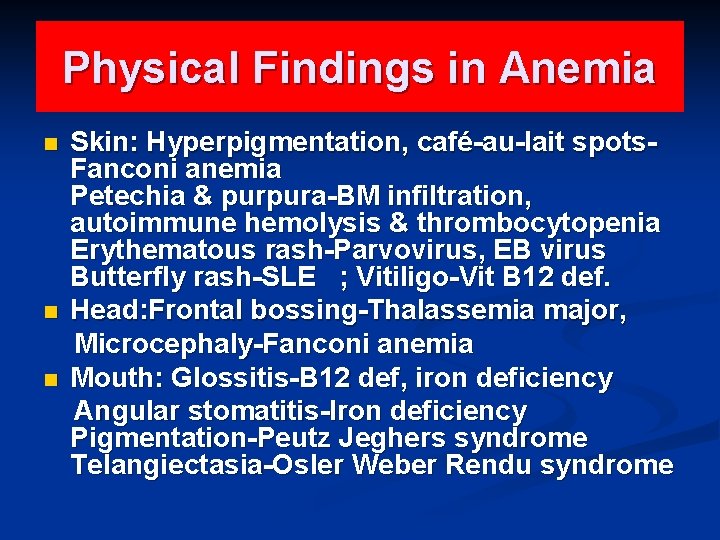
Physical Findings in Anemia n n n Skin: Hyperpigmentation, café-au-lait spots. Fanconi anemia Petechia & purpura-BM infiltration, autoimmune hemolysis & thrombocytopenia Erythematous rash-Parvovirus, EB virus Butterfly rash-SLE ; Vitiligo-Vit B 12 def. Head: Frontal bossing-Thalassemia major, Microcephaly-Fanconi anemia Mouth: Glossitis-B 12 def, iron deficiency Angular stomatitis-Iron deficiency Pigmentation-Peutz Jeghers syndrome Telangiectasia-Osler Weber Rendu syndrome
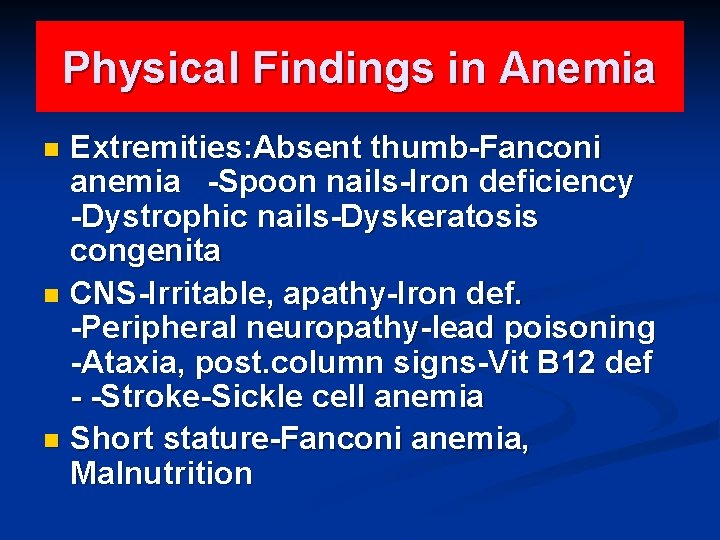
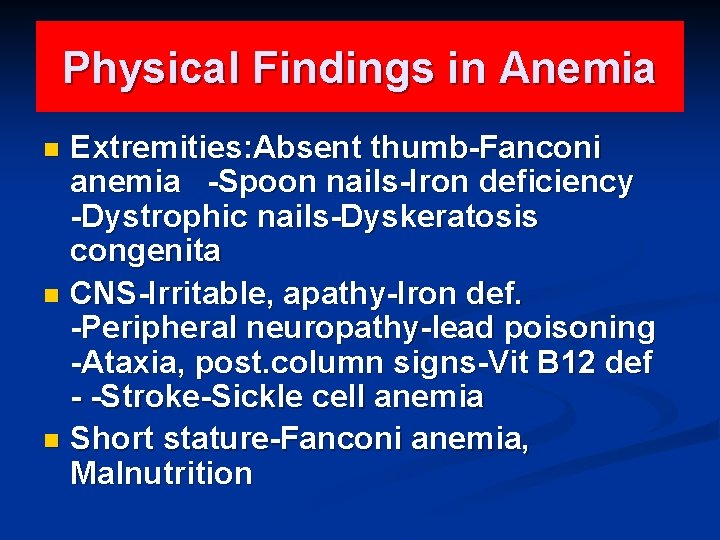
Physical Findings in Anemia Extremities: Absent thumb-Fanconi anemia -Spoon nails-Iron deficiency -Dystrophic nails-Dyskeratosis congenita n CNS-Irritable, apathy-Iron def. -Peripheral neuropathy-lead poisoning -Ataxia, post. column signs-Vit B 12 def - -Stroke-Sickle cell anemia n Short stature-Fanconi anemia, Malnutrition n

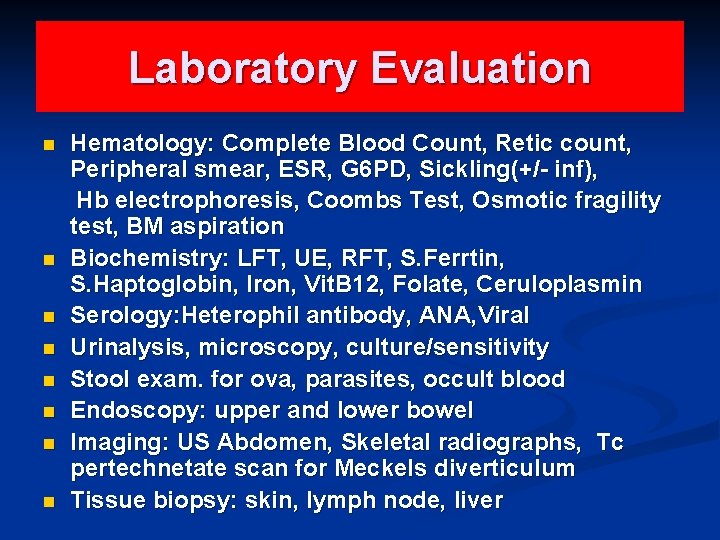
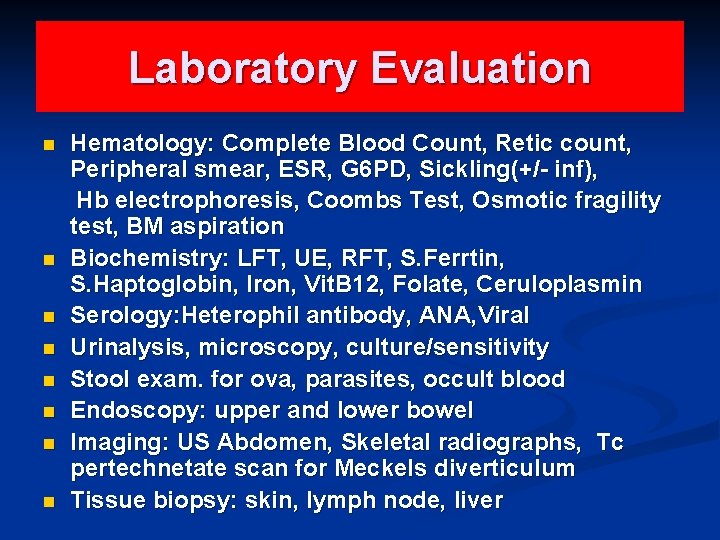
Laboratory Evaluation n n n n Hematology: Complete Blood Count, Retic count, Peripheral smear, ESR, G 6 PD, Sickling(+/- inf), Hb electrophoresis, Coombs Test, Osmotic fragility test, BM aspiration Biochemistry: LFT, UE, RFT, S. Ferrtin, S. Haptoglobin, Iron, Vit. B 12, Folate, Ceruloplasmin Serology: Heterophil antibody, ANA, Viral Urinalysis, microscopy, culture/sensitivity Stool exam. for ova, parasites, occult blood Endoscopy: upper and lower bowel Imaging: US Abdomen, Skeletal radiographs, Tc pertechnetate scan for Meckels diverticulum Tissue biopsy: skin, lymph node, liver
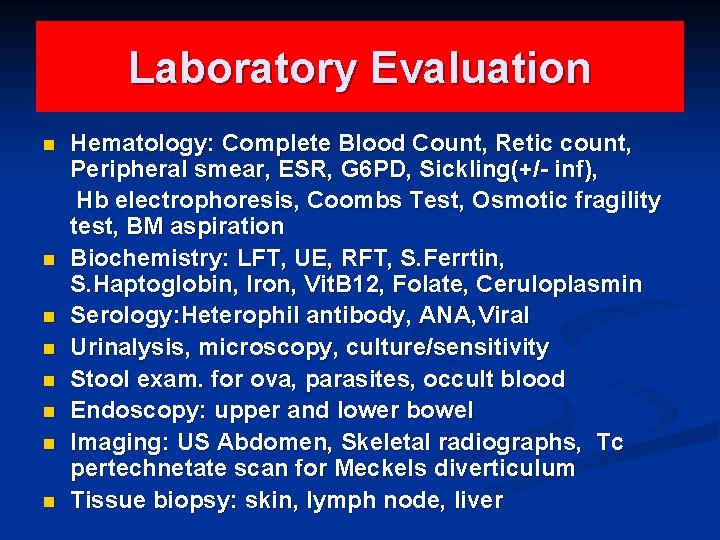
Laboratory Evaluation n n n n Hematology: Complete Blood Count, Retic count, Peripheral smear, ESR, G 6 PD, Sickling(+/- inf), Hb electrophoresis, Coombs Test, Osmotic fragility test, BM aspiration Biochemistry: LFT, UE, RFT, S. Ferrtin, S. Haptoglobin, Iron, Vit. B 12, Folate, Ceruloplasmin Serology: Heterophil antibody, ANA, Viral Urinalysis, microscopy, culture/sensitivity Stool exam. for ova, parasites, occult blood Endoscopy: upper and lower bowel Imaging: US Abdomen, Skeletal radiographs, Tc pertechnetate scan for Meckels diverticulum Tissue biopsy: skin, lymph node, liver
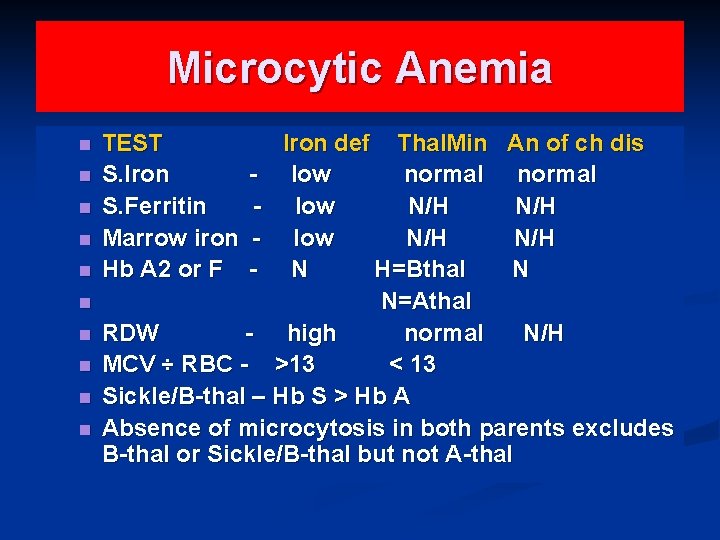
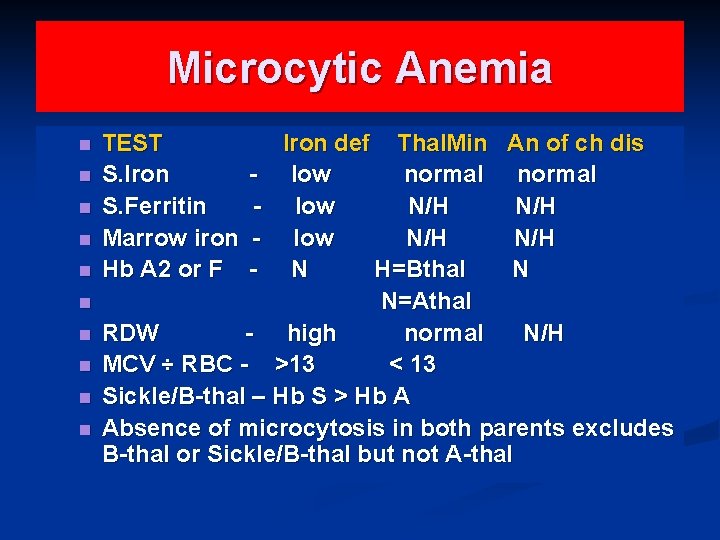
Microcytic Anemia n n n n n TEST S. Iron S. Ferritin Marrow iron Hb A 2 or F Iron def Thal. Min An of ch dis - low normal - low N/H N/H - N H=Bthal N N=Athal RDW - high normal N/H MCV ÷ RBC - >13 < 13 Sickle/B-thal – Hb S > Hb A Absence of microcytosis in both parents excludes B-thal or Sickle/B-thal but not A-thal
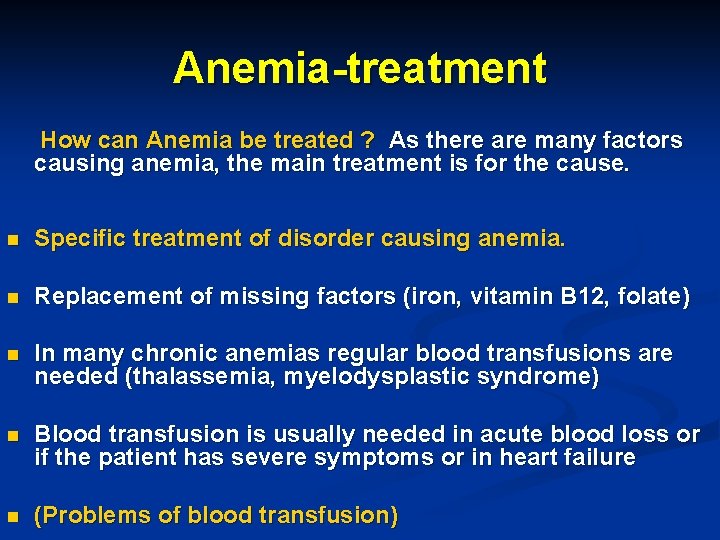
Anemia-treatment How can Anemia be treated ? As there are many factors causing anemia, the main treatment is for the cause. n Specific treatment of disorder causing anemia. n Replacement of missing factors (iron, vitamin B 12, folate) n In many chronic anemias regular blood transfusions are needed (thalassemia, myelodysplastic syndrome) n Blood transfusion is usually needed in acute blood loss or if the patient has severe symptoms or in heart failure n (Problems of blood transfusion)
Iron deficiency anemia (IDA) n It is a condition when supply of iron in the body to bone marrow falls short of that required for the production of red blood cells. It is the commonest cause of anemia throughout the world.
Iron Deficiency Anemia n The incidence of anemia in the general population is about 1. 5%. n Iron deficiency related to inadequate replacement of lost iron is the most frequent cause of asymptomatic anemia and has a variety of causes. n Iron deficiency is common among women of childbearing age; 10% to 20% of menstruating women have abnormally low concentrations of
Iron Deficiency Anemia n n § What are the causes of IDA ? Increased physiological demand for more red blood cells eg: increased physical activity. In children, during spurts of growth. • In women during menstruation, pregnancy, parturition and lactation. • Inadequate dietary intake due to poor economic reasons or deficient foods. Decreased absorption due to disorders in the digestive system. GI blood loss Peptic ulcer, piles, hiatus hernia, carcinoma of stomach, carcinoma colon, chronic ingestion of a § §
Iron Deficiency Anemia Between 20% and 60% of pregnant women have hemoglobin levels <11 g per 100 m. L. Anemia was found in 6% of white women and 17% of black women during the first trimester and in 25% of white women and 46% of black women during the third trimester.
Iron Deficiency Anemia The high rates of anemia in pregnant women are not attributable to iron deficiency alone, however. In a large study of low-income, urban, mostly minority pregnant women, only 12. 5% were iron deficient. Women progressing through pregnancy develop a lowered hematocrit as a result of physiologic hydremia related to a disproportionate increase in plasma volume.
Iron Deficiency Anemia § § The daily oral iron requirement for men and postmenopausal women is 0. 5 and 1 mg Menstruating and pregnant women have higher requirements: 2 mg and 2. 5 mg, respectively. The replacement of lost iron is complicated by the fact that only 5% to 10% of the 10 to 20 mg of the iron in the average adult diet is absorbed. Anemia is less likely to occur in women taking birth control pills and more likely to occur in women with intrauterine devices.
Iron Deficiency Anemia Because men and postmenopausal women rarely develop iron deficiency that is not related to gastrointestinal blood loss (often occult), an evaluation of gastrointestinal tract must be performed when an iron deficiency is detected in these individuals
IDA-Practice Point Iron def. is common in children 9 mo-3 yr n Iron def. anemia in a child over 3 yr should prompt consideration of occult blood loss. n Infants less than 6 months generally do not develop iron def. ; the exception to this rule is premature infants, who are at risk of iron def. at 4 mo, if iron supplementation is not given. n
Iron Deficiency Anemia. Diagnosis n n n n Red blood cell count may be normal or decreased. Peripheral blood smear shows pale small cells. Aniso-poikilocytosis White blood cell count usually normal Serum iron is reduced Total iron binding capacity of blood shows an increase. Low serum ferritin
Iron Deficiency Anemia. Treatment Correction of iron deficiency - to restore hemoglobin level. n To replenish iron stores. n Oral iron administration is advised. (Side effects of oral iron) n Parenteral iron may be needed occasionally n Treat the underlying cause n
Anemia of Chronic Disease n Patients with cancer, infection, or inflammation, commonly have a mild-to -moderate anemia caused by red cell underproduction. This 'anemia of chronic disease' is very common, and is usually normocytic. Some cases develop abnormalities of iron metabolism, in which case there may be a microcytosis.
Hemolysis n n (a) (b) (c) (d) Hemolysis is defined as the premature destruction of red blood cells, from whatever cause. Recognising the presence of hemolysis The simplest tests are Raised reticulocyte count Raised indirect (unconjugated) bilirubin Raised serum LDH Diminished serum haptoglobin concentration. Further more sophisticated testing may be needed in some cases.
Hemolysis A Direct Coombs' Test tells you whether the red blood cells are antibody-coated, and, in the presence of hemolysis, indicates an immunemediated process (Autoimmune hemolytic anemia). n Note that many patients with a positive Direct Coombs' test do not have hemolysis. n
Hemolysis Principal causes Inherited abnormalities * Membrane (Hereditary Spherocytosis) * Hemoglobin (Sickle Cell Anemia) * Enzymes (Glucose-6 -phosphate dehydrogenase (G 6 PD) deficiency)
Hemolysis Acquired causes n Immune Warm and Cold Autoimmune Hemolytic Anemia n Non-immune * Mechanical Damage from leaky heart valves * Microangiopathic hemolytic anemia (MAHA) like TTP, HUS & DIC
Lead Poisoning Hypochromic microcytic anemia n Associated iron deficiency n Child has pica and is exposed to lead paint or lead dust n Blood smear shows basophilic stipling and blood lead is elevated. n Removal from exposure, chelation therapy and correction of iron deficiency are important. n
THALASSEMIA Normal Hb is a tetramer of 2 alpha and 2 beta chains n Alpha-thalassemia: decrease or total lack of alpha globin synthesis n Beta-thalassemia: decrease or total lack of beta globin synthesis n
THALASSEMIA n n n n Clinical classification. Silent carrier(Aor. B): normal CBC Thal trait(Aor. B): mild anemia(HM) Hb. Hdisease(A-thal): moderately severe hemolytic anemia, icterus, splenomegaly Severe Beta-thal: severe anemia, growth retardation, hepatosplenomegaly, bony def. Thalassemia major: tranfusion dependent Thal-intermedia: no regular transfusions
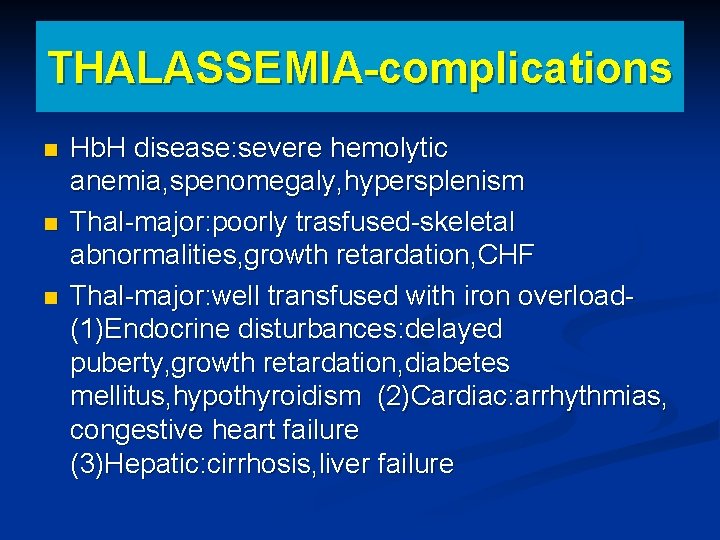
THALASSEMIA-complications n n n Hb. H disease: severe hemolytic anemia, spenomegaly, hypersplenism Thal-major: poorly trasfused-skeletal abnormalities, growth retardation, CHF Thal-major: well transfused with iron overload(1)Endocrine disturbances: delayed puberty, growth retardation, diabetes mellitus, hypothyroidism (2)Cardiac: arrhythmias, congestive heart failure (3)Hepatic: cirrhosis, liver failure
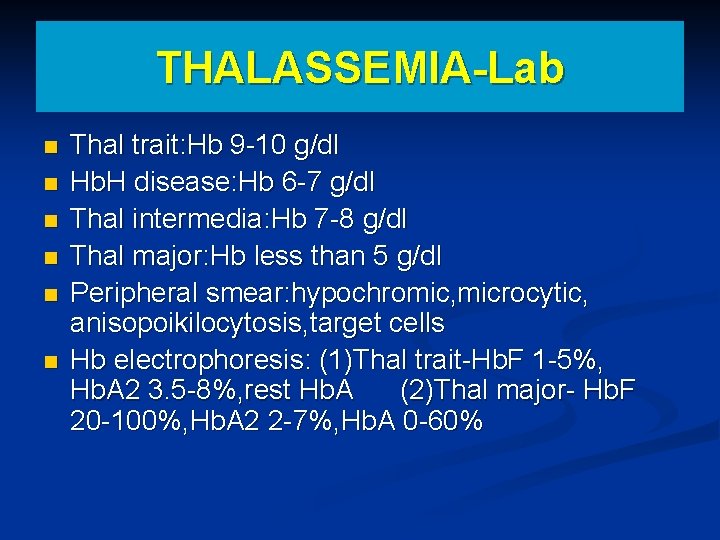
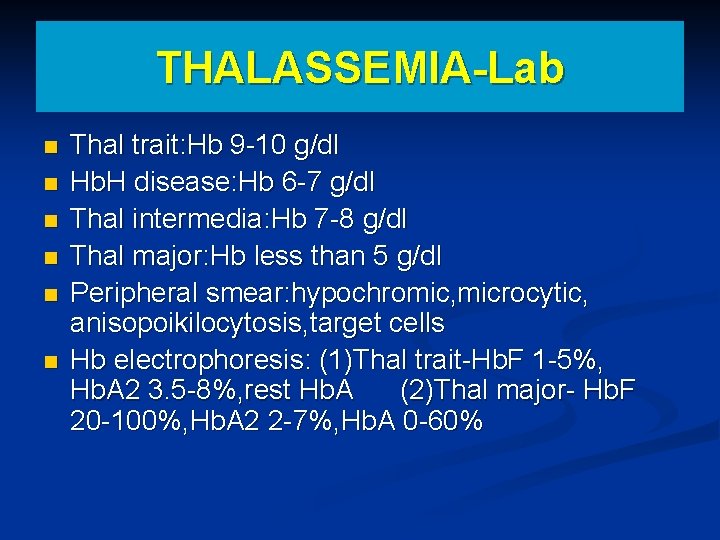
THALASSEMIA-Lab n n n Thal trait: Hb 9 -10 g/dl Hb. H disease: Hb 6 -7 g/dl Thal intermedia: Hb 7 -8 g/dl Thal major: Hb less than 5 g/dl Peripheral smear: hypochromic, microcytic, anisopoikilocytosis, target cells Hb electrophoresis: (1)Thal trait-Hb. F 1 -5%, Hb. A 2 3. 5 -8%, rest Hb. A (2)Thal major- Hb. F 20 -100%, Hb. A 2 2 -7%, Hb. A 0 -60%
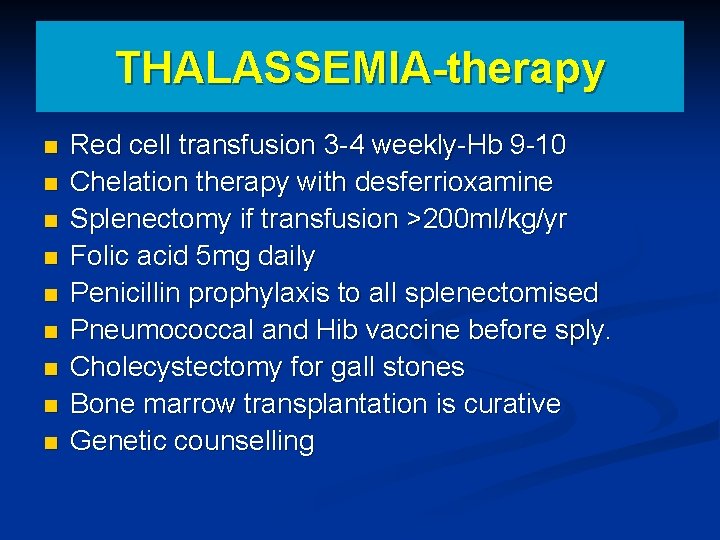
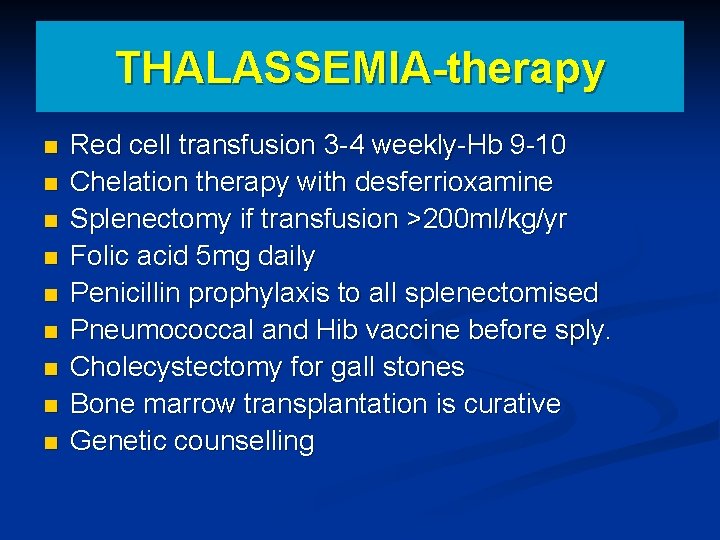
THALASSEMIA-therapy n n n n n Red cell transfusion 3 -4 weekly-Hb 9 -10 Chelation therapy with desferrioxamine Splenectomy if transfusion >200 ml/kg/yr Folic acid 5 mg daily Penicillin prophylaxis to all splenectomised Pneumococcal and Hib vaccine before sply. Cholecystectomy for gall stones Bone marrow transplantation is curative Genetic counselling
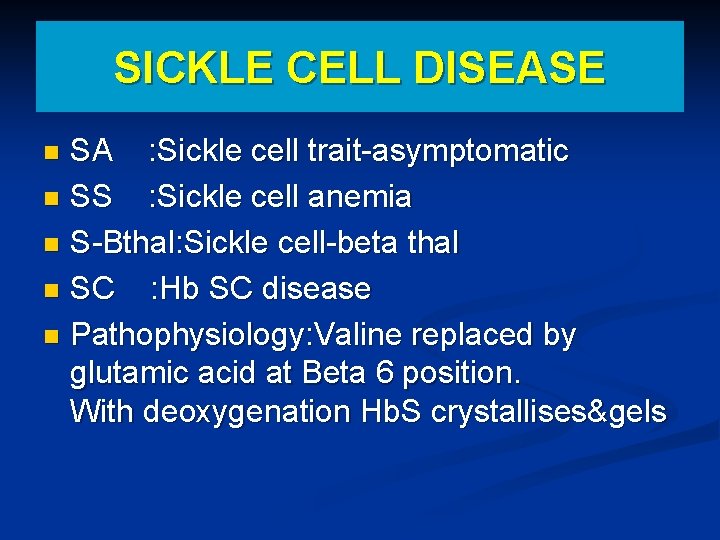
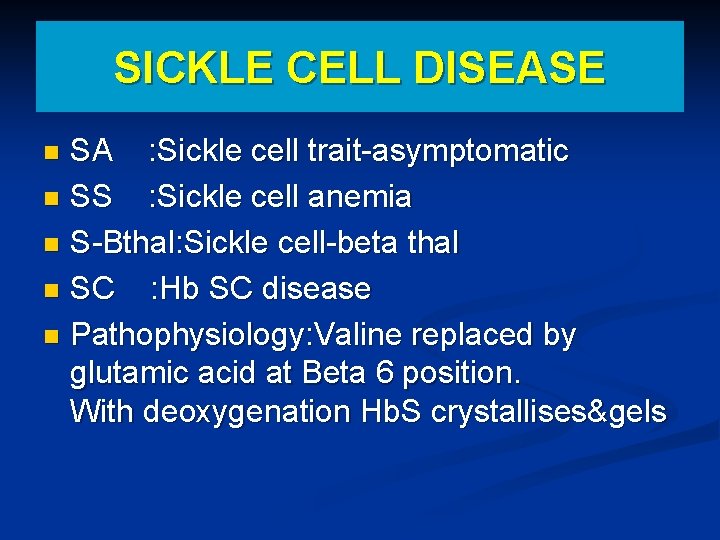
SICKLE CELL DISEASE SA : Sickle cell trait-asymptomatic n SS : Sickle cell anemia n S-Bthal: Sickle cell-beta thal n SC : Hb SC disease n Pathophysiology: Valine replaced by glutamic acid at Beta 6 position. With deoxygenation Hb. S crystallises&gels n
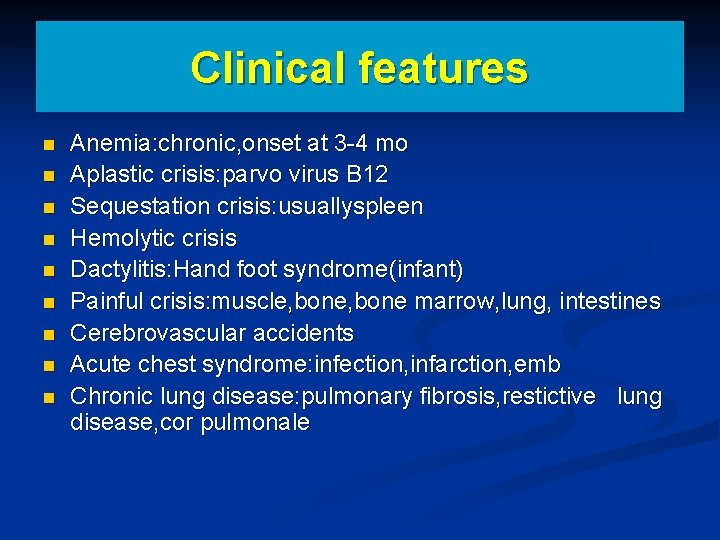
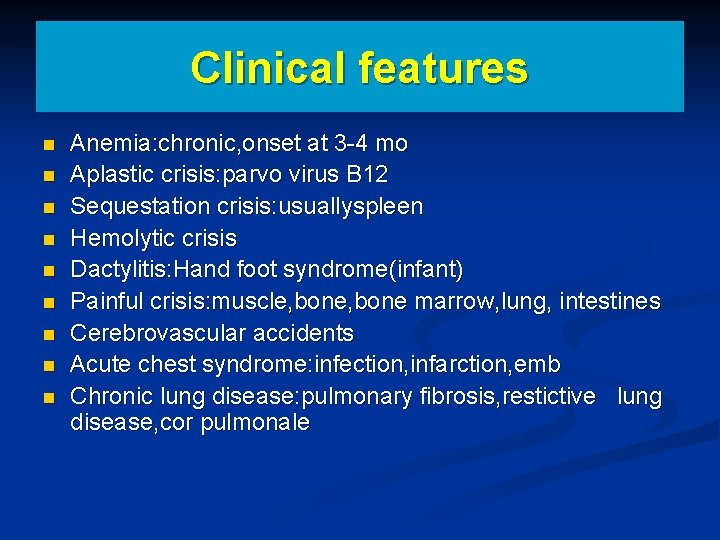
Clinical features n n n n n Anemia: chronic, onset at 3 -4 mo Aplastic crisis: parvo virus B 12 Sequestation crisis: usuallyspleen Hemolytic crisis Dactylitis: Hand foot syndrome(infant) Painful crisis: muscle, bone marrow, lung, intestines Cerebrovascular accidents Acute chest syndrome: infection, infarction, emb Chronic lung disease: pulmonary fibrosis, restictive lung disease, cor pulmonale
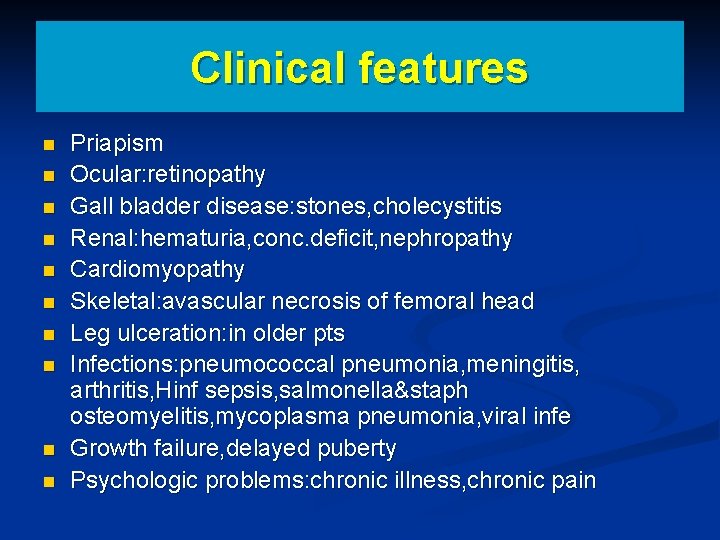
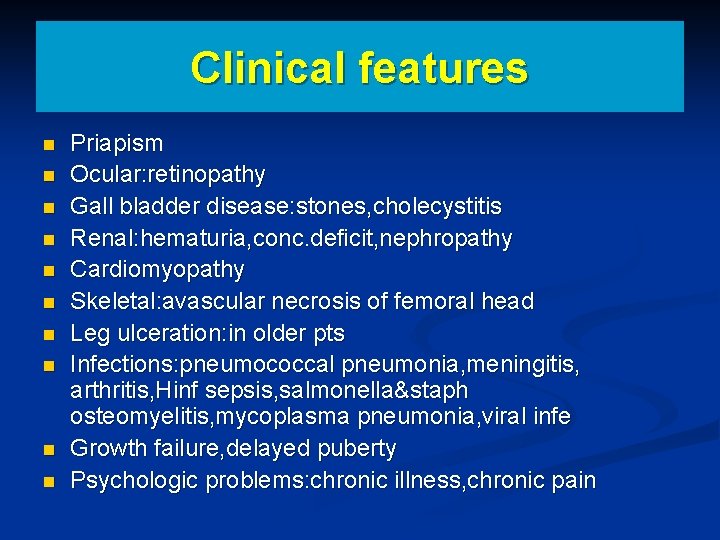
Clinical features n n n n n Priapism Ocular: retinopathy Gall bladder disease: stones, cholecystitis Renal: hematuria, conc. deficit, nephropathy Cardiomyopathy Skeletal: avascular necrosis of femoral head Leg ulceration: in older pts Infections: pneumococcal pneumonia, meningitis, arthritis, Hinf sepsis, salmonella&staph osteomyelitis, mycoplasma pneumonia, viral infe Growth failure, delayed puberty Psychologic problems: chronic illness, chronic pain
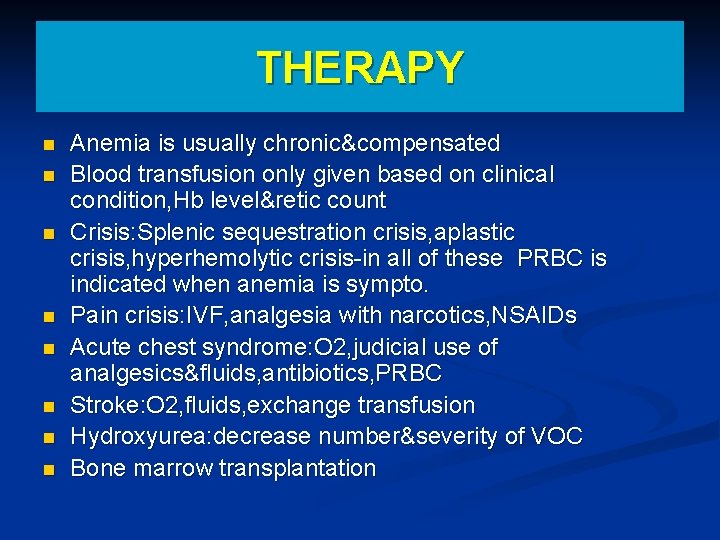
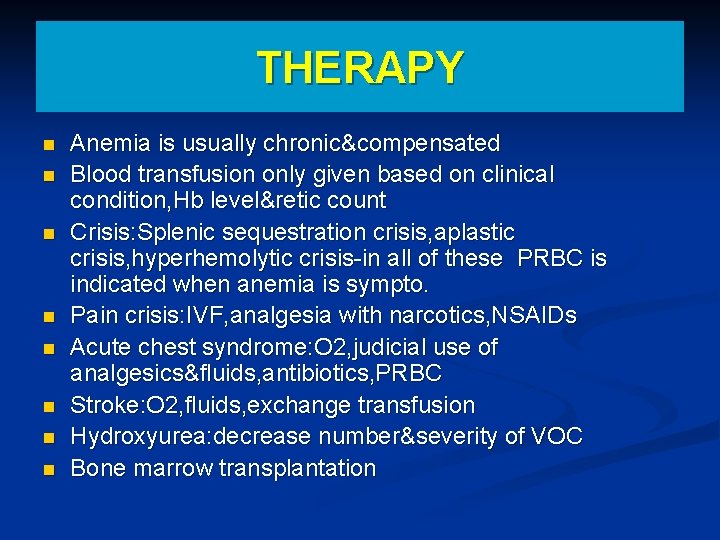
THERAPY n n n n Anemia is usually chronic&compensated Blood transfusion only given based on clinical condition, Hb level&retic count Crisis: Splenic sequestration crisis, aplastic crisis, hyperhemolytic crisis-in all of these PRBC is indicated when anemia is sympto. Pain crisis: IVF, analgesia with narcotics, NSAIDs Acute chest syndrome: O 2, judicial use of analgesics&fluids, antibiotics, PRBC Stroke: O 2, fluids, exchange transfusion Hydroxyurea: decrease number&severity of VOC Bone marrow transplantation
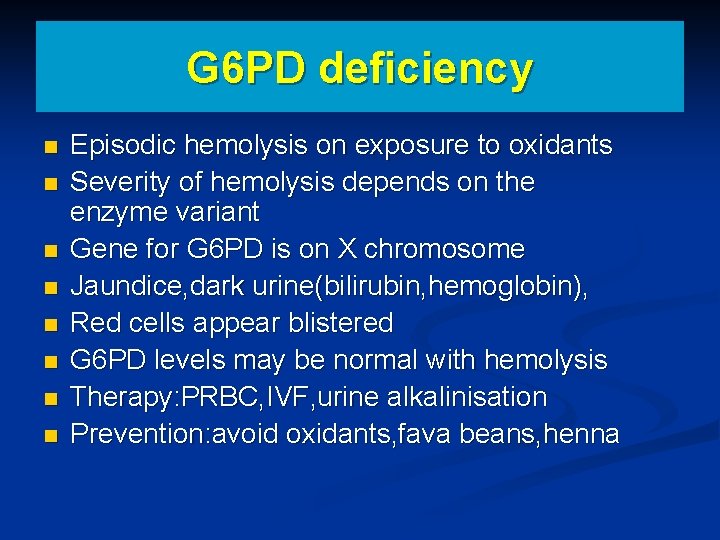
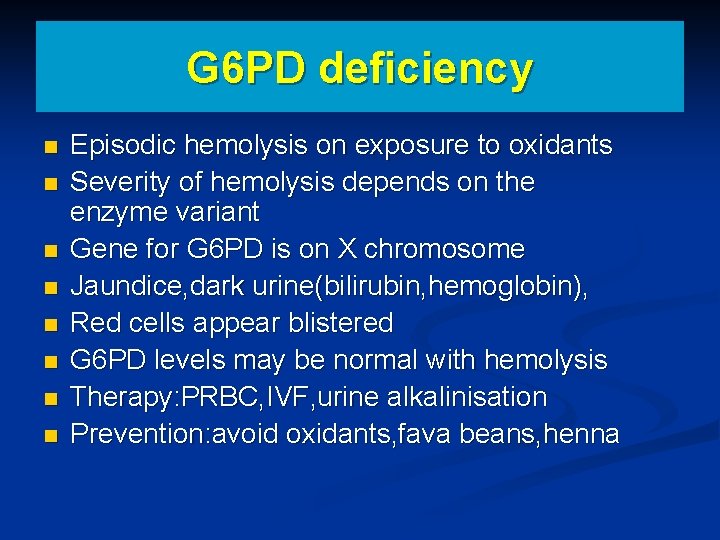
G 6 PD deficiency n n n n Episodic hemolysis on exposure to oxidants Severity of hemolysis depends on the enzyme variant Gene for G 6 PD is on X chromosome Jaundice, dark urine(bilirubin, hemoglobin), Red cells appear blistered G 6 PD levels may be normal with hemolysis Therapy: PRBC, IVF, urine alkalinisation Prevention: avoid oxidants, fava beans, henna
