Anemia in the newborn infants Hemoglobin increases with
Anemia in the newborn infants
Hemoglobin increases with advancing of gestational age, at term cord blood Hb is 16. 8 g/dl (range 14 -20 g/dl), Hb levels in very low birth weight infants (VLBW) are 1 -2 g/dl below those in term infants. Anemia: is defined when Hb level is less than the normal range for birth weight and post natal age. Physiological anemia: Its due to "physiologic" decrease in Hb levels in healthy neonate which is noted at 8 -12 wk in term infants (Hb 11 g/dl) and at about 6 wk in premature infants (Hb 7 -10 g/dl).
Etiology of neonatal anemia: Symptomatic anemia in neonatal period may be due to: I. Blood loss: 1. Fetal – maternal bleeding. ** 2. Placenta previa. ** 3. Abruptio placentae. ** 4. Twin – twin transfusion. ** 5. Rupture of umbilical cord. 6. Hepatic or splenic hematomas.
II. Decrease production: 1. Perinatal – congenital infections. ** 2. Anemia of prematurity. ** 3. Parvo virus infection. 4. Diamond – Blackfan syndrome. 5. Congenital leukemia. 6. Sideroblastic anemia.
III. Hemolysis: 1. Rh, ABO, or minor blood groups incompatibility ** enzymes defects (G 6 PD deficiency, pyruvate kinase deficiency). 3. Hemoglobinopathies (alpha thalasemia syndrome). 4. RBC membrane defects (spherocytosis). 5. DIC. 6. Maternal autoimmune disorders (SLE).
Clinical features: Its depend on the onset and the underlying cause of anemia. a due to acute blood loss at birth etomaternal hemorrhage, rupture of umbilical ord, placenta previa, and internal hemorrhage) st with pallor, diminished peripheral and shock, there are no signs of extramedullary hematopoisis and HSM. e Hb and S. iron levels initially are normal, t the Hb level decline during the subsequent 24 hr.
mia due to chronic blood loss (chronic al hemorrhage or twin-twin nsfusion) or due to hemolysis presents with pallor, heart failure, HSM with or drops, low Hb level at birth, romic microcytic blood smear, and decreased serum iron. mia due to decreased RBC production nts at birth with pallor, low reticulocyte nt and absence of erythroid precursors in the bone marrow.
Investigations of neonatal anemia: 1. CBC (low Hb concentration). Retic count: decrease in congenital hypoplastic anemia e. g. Diamond – Blackfan syndrome. ombs test: positive in ABO, Rh or minor blood groups incompatibility. CV: decrease in chronic intrauterine loss or alpha-thalassemia syndrome. Peripheral blood smear morphology: abnormal in hemolytic anemia or DIC.
Fetomaternal bleeding: Its occurs in more than 50% of all pregnancies, with fetal blood losses ranging between 1 -50 ml. The diagnosis of fetomaternal bleeding is confirm by acid elution test of Kleihauer and Betke in which the pink fetal RBCs are observed and counted in the mother peripheral blood smear because fetal Hb is resistant to acid elution, while adult Hb is eluted leaving discolored maternal cells.
Anemia of prematurity: Its occurs in LBW infants 1 -3 mo after birth, with Hb level bellow 7 -10 g/dl, presented with pallor, apnea, poor weight gain, decreased activity, tachypnea, tachycardia and feeding difficulties.
Causes: 1. Repeated blood sampling for laboratory tests. 2. Short RBCs survival. 3. Rapid growth. Physiological effects of transition from fetal life w Pa. O 2 and Hb saturation) to neonatal life (high Pa. O 2 and Hb saturation). uated erythropoietin response: The gen available to neonatal tissues is lower lts, but a neonatal ropoietin response is attenuated for the ee of anemia, resulting in low Hb levels with reticulocytopenia.
Treatment of neonatal anemia: I. Asymptomatic full-term infants with Hb levels of 10 g/dl required just observation. II. Blood transfusion: Packed RBCs transfusion (10 -15 ml/kg) is given at a rate of 2 -3 ml/kg/hr to raise the Hb level (2 ml/kg of packed RBCs raises b level 0. 5 -1 g/dl). Hemorrhaged should be treated by whole blood if available.
Indications: mptomatic neonates born after abruptio centae or with severe hemolytic disease of newborn. erm infants with repeated episodes of a and bradycardia despite theophylline and Hb level <10 g/d. 3. Infants with RDS or severe chronic lung disease. 4. Infants with reticulocytopenia and Hb levels< 6. 5 g/dl.
Recombinant human erythropoietin: given by. or S. C. routes and must bensupplemented h oral iron and vitamin E. s and regimens vary from 100 -200 se 5 days/wk to 400 U/kg/dose 3 days/wk. cation: for treatment or prevention of chronic anemia associated with: 1. Prematurity. 2. Chronic lung disease. 3. Hyporegenerative anemia of erythroblastosis fetalis.
Polycythemia (plethora) in the newborn infants
Polycythemia defined as central hematocrit of 65% or higher (peripheral e. g. heel stick hematocrit values are higher than central values). Plethora: is a deep red – purple appearance associated with high hematocrit, often due to polycythemia.
Etiology of polycythemia: 1. High altitude. 2. Postmaturity. 3. IUGR. 4. Recipient infant of twin – twin transfusion. 5. Delayed clamping of umbilical cord. 6. Infants of diabetic mothers. 7. Trisomy – 13, 18, or 21. 8. Congenital adrenal hyperplasia. 9. Neonatal Graves disease. 10. Hypothyroidism. 11. Beckwith-Wiedeman syndrome.
Pathophysiology: Infants may exposed to chronic hypoxia (as in infants of diabetic mothers, high altitude, IUGR) which stimulate erythropoietin production and increases RBCs production. Polycythemia causing hyperviscosity with decreased perfusion of the capillary beds which causing ischemia of body organs, so clinical symptoms can affect several organ systems
Clinical features: Anorexia, lethargy, tachypnea, respiratory distress, cyanosis, feeding problems, hyperbilirubinemia, hypoglycemia, and thrombocytopenia. Complications: 1. Seizures. 2. Pulmonary hypertension. 3. Necrotizing enterocolitis 4. Renal failure.
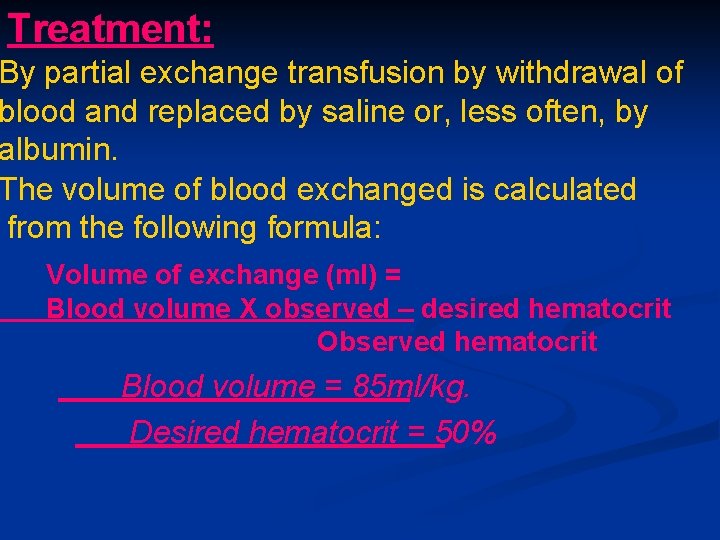
Treatment: By partial exchange transfusion by withdrawal of blood and replaced by saline or, less often, by albumin. The volume of blood exchanged is calculated from the following formula: Volume of exchange (ml) = Blood volume X observed – desired hematocrit Observed hematocrit Blood volume = 85 ml/kg. Desired hematocrit = 50%
Blood is withdrawn at a steady rate from an umbilical vein while the replacement solution is infused at the same rate through a peripheral vein over 15 -30 minutes. Prognosis: Reported adverse outcome of polycythemia include speech deficit, abnormal fine motor control, reduced I. Q. and other neurological abnormalities.
Hemorrhagic disease of newborn Is bleeding disorder of newborn infants due to deficiency of vitamin K dependent clotting factors. Its of 3 types assic hemorrhagic disease of born characterized by spontaneous rolonged bleeding in newborn infants, only between 2 -7 days of life, due to ent deficiency of vitamin K dependent factors (factors II, VII, IX, and X)
This transient deficiency of vitamin K dependent factors due to: 1. Lack of free vitamin K in the mother. bsence of bacterial intestinal flora normally responsible for synthesis of V. K. in newborn. milk is poor source of V. K. and hagic disease is more common in breast-feed than in formula-feed infants.
Normally, there's moderate decrease of V. K. dependent factors occurs in all newborn infants by 48 -72 hr after birth, with a gradual return to birth levels by 7 -10 days of age, but occasionally there's accentuation and prolongation of this deficiency between 2 -7 days of life resulting in spontaneous and prolonged bleeding especially in preterm infants.
t (birth-24 hr) morrhagic disease of newborn s if the mother treated with drugs that fere with V. K. function like Phenobarbital and phyntoin. e onset (>1 wk) hemorrhagic ease of newborn is often associated malabsorption as in neonatal hepatitis or biliary atrasia.
Clinical features: It's characterized by bleeding that maybe gastrointestinal, nasal, intracranial or after circumcision. Investigations: Prolonged prothrombin time (PT), coagulation time, and partial thromboplastin time (PTT). 2. Decreased levels of factors II, VII, IX and X. eeding time, fibrinogen, platelets, capillary fragility, factors V and VIII are normal.
Prevention: By I. M. injection of 1 mg of V. K. at the time of birth to all newborn infants (full term or preterm). Treatment: By slow I. V. infusion of 1 -5 mg of V. K. , with improvement of coagulation defects and cessation of bleeding within few hours. Serious bleeding, especially in preterm infants or those with liver disease, may require transfusion of fresh frozen plasma (10 ml/kg) or whole blood.
Differential diagnosis: 1. Congenital defects in blood coagulation. 2. Disseminated intravascular coagulopathy (DIC). Swallowed blood syndrome (blood swallowed ring delivery or from fissure in mother nipple ng bloody stools usually on 2 nd or 3 rd day of life). e superficial blood vessels causing bcutaneous ecchymosis in premature infants at or immediately after birth. 5. Nucal cord causing petechiae limited to face, head, and neck.
- Slides: 28