Anemia in pregnancy Definition Who has defined anemia

- Slides: 25
Anemia in pregnancy
Definition • Who has defined anemia as Hb level of <11 g/dl.
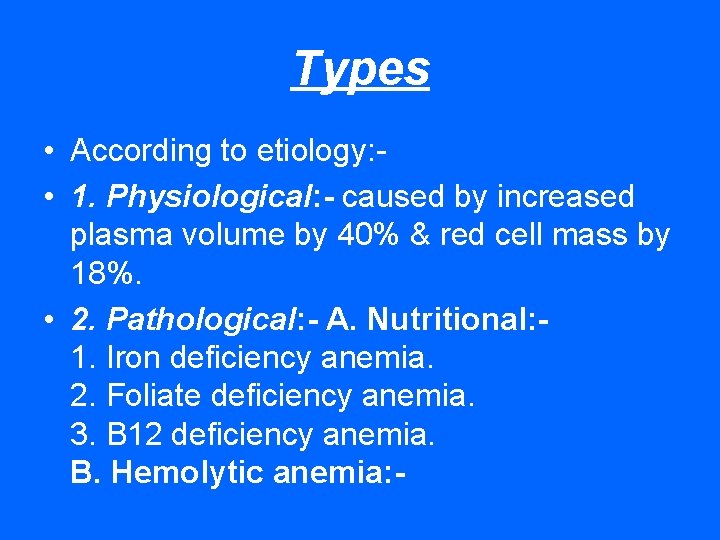
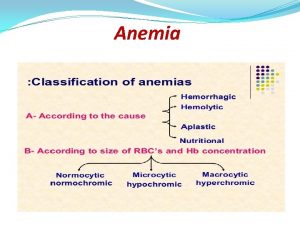
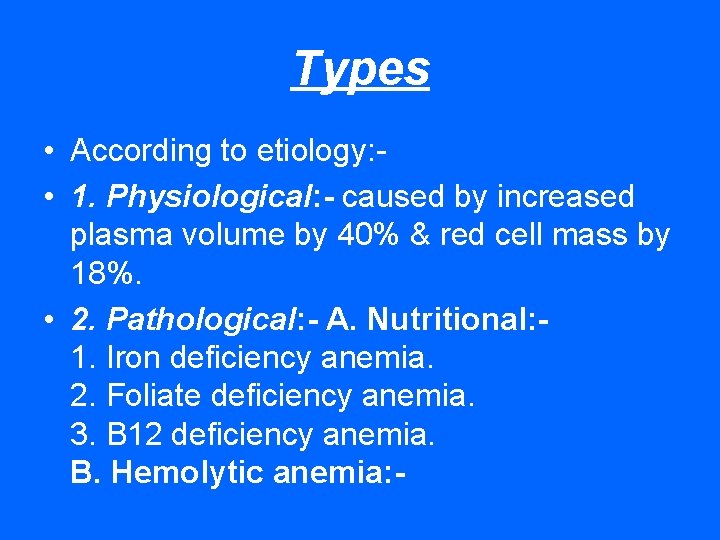
Types • According to etiology: • 1. Physiological: - caused by increased plasma volume by 40% & red cell mass by 18%. • 2. Pathological: - A. Nutritional: 1. Iron deficiency anemia. 2. Foliate deficiency anemia. 3. B 12 deficiency anemia. B. Hemolytic anemia: -
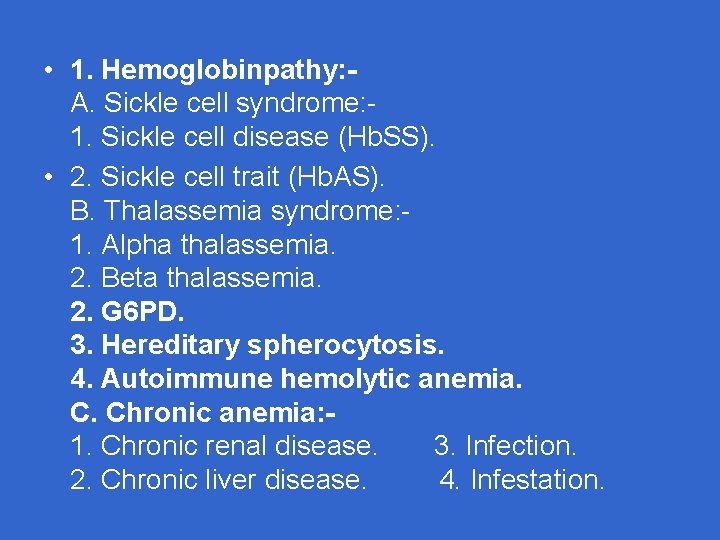
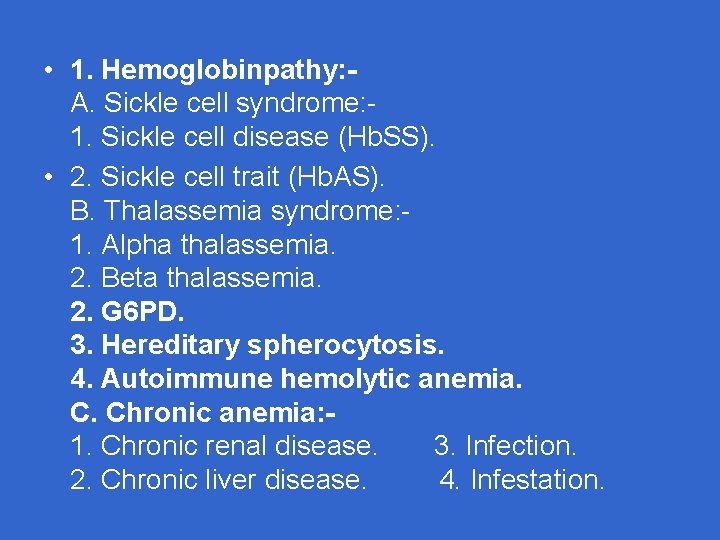
• 1. Hemoglobinpathy: A. Sickle cell syndrome: 1. Sickle cell disease (Hb. SS). • 2. Sickle cell trait (Hb. AS). B. Thalassemia syndrome: 1. Alpha thalassemia. 2. Beta thalassemia. 2. G 6 PD. 3. Hereditary spherocytosis. 4. Autoimmune hemolytic anemia. C. Chronic anemia: 1. Chronic renal disease. 3. Infection. 2. Chronic liver disease. 4. Infestation.
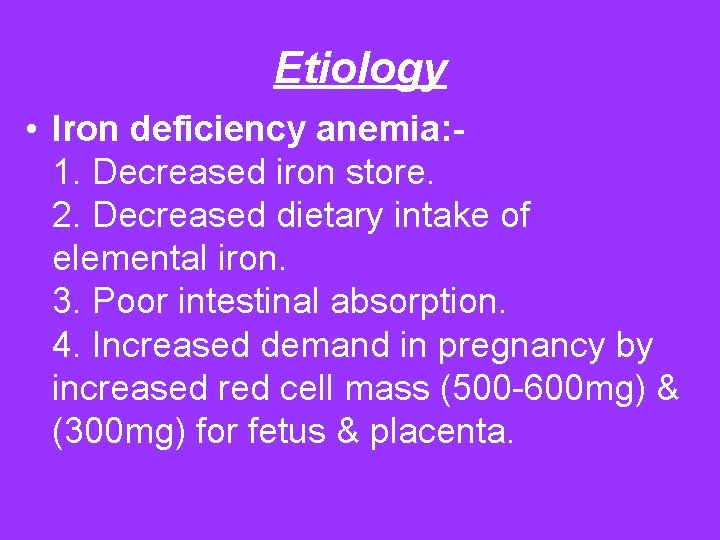
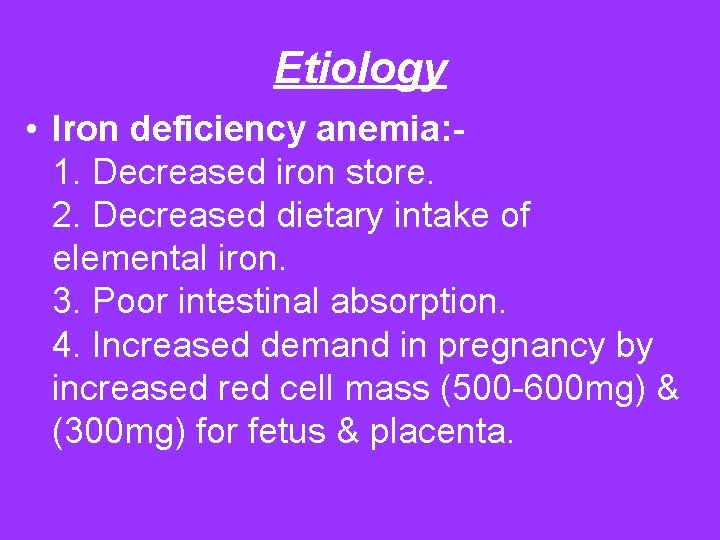
Etiology • Iron deficiency anemia: 1. Decreased iron store. 2. Decreased dietary intake of elemental iron. 3. Poor intestinal absorption. 4. Increased demand in pregnancy by increased red cell mass (500 -600 mg) & (300 mg) for fetus & placenta.
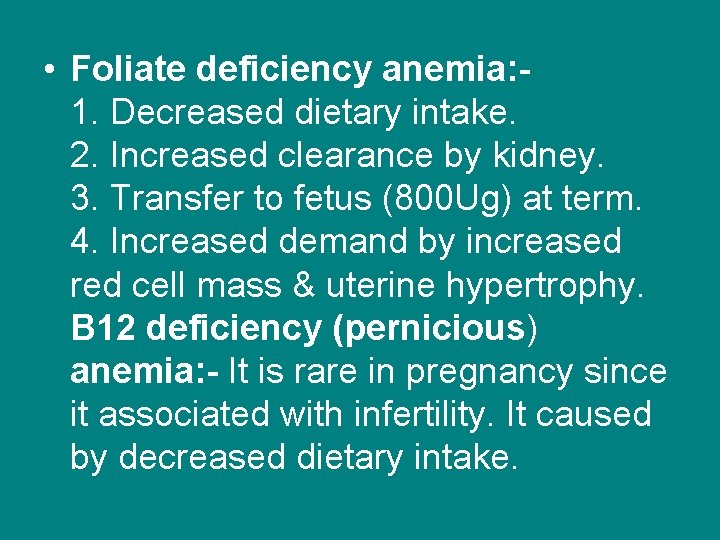
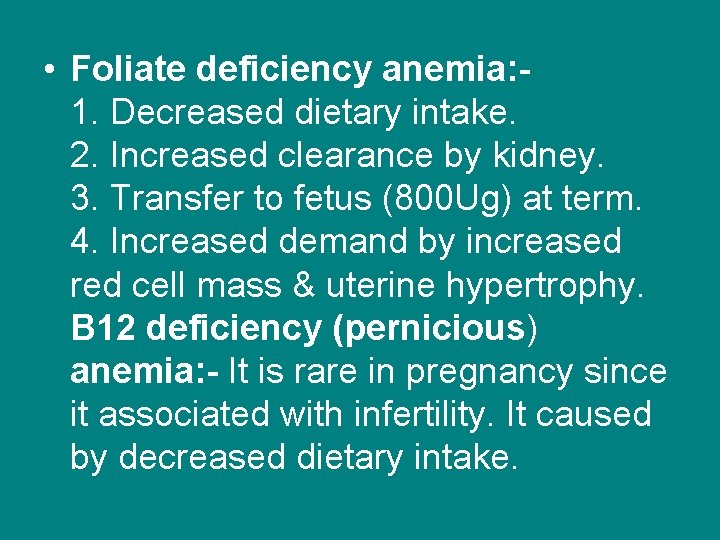
• Foliate deficiency anemia: 1. Decreased dietary intake. 2. Increased clearance by kidney. 3. Transfer to fetus (800 Ug) at term. 4. Increased demand by increased red cell mass & uterine hypertrophy. B 12 deficiency (pernicious) anemia: - It is rare in pregnancy since it associated with infertility. It caused by decreased dietary intake.
• Hemoglobinpathy: - Normal Hb molecule consist of two alpha chains & two Beta chains. Each chain consist of series of amino acids so hemoglobinpathy arise if there is qualitative or quantitative defect. Sickle cell syndrome: - There is qualitative defect caused by substitution of valine to glutamic acid at position 6 of Beta chain producing Hb. S. Thalassemia syndrome: - There is quantitative defect in production of Alpha chain or Beta chain.
• 1. Alpha- thalassemia: a. Minor: - deficient of one or two genes in Alpha chain. b. H: - Deficient three genes. c. Major: - No Alpha chain & replaced by four Gamma chain. 2. Beta- thalassemia: - a. Major. b. intermediate. c. Minor. G 6 PD: - Deficient glucose 6 - pyruvate dehydrogenase enzyme involved in metabolism of red cell. Hereditary spherocytosis: - abnormal red cell membrane. Autoimmune hemolytic anemia: - autoimmune antibody against red cell wall.
• Chronic anemia: 1. Chronic renal disease: - decrease in erythropoietin production. 2. Infection: - Malaria, HIV. 3. Infestation: - Hook warm. Risk factors: - 1. Malnutrition. 2. Multiparty. 3. Low social class. 4. Poor education. 5. Short interval between pregnancies. 6. Prolong lactation. 7. Teenage female.
Maternal Risk • 1. Difficult to perform usual work. 2. Easy to get infection. 3. APH especially accidental hemorrhage in foliate deficiency. 4. PET mainly in hemoglobinpathy. 5. P. P. H. 6. Recurrent U. T. I. 7. Delay recovery from anesthesia & wound healing after C/S.
Fetal risk • 1. Congenital defect as N. T. D. , cleft lip, cleft palate mainly in foliate deficiency. 2. Preterm delivery. 3. I. U. G. R. 4. I. U. D. 5. High prenatal mortality mainly due to preterm labor. 6. Neonatal anemia which result behavioral changes in first year of life.
Clinical features • 1. Symptoms: - 1. Headache & blurred vision. 2. Palpitation & S. O. B. 3. Easy fatigue & intolerance to exercise. 4. Generalized bone pain. 5. Nausea & vomiting. 6. Fainting attacks in sever anemia. 7. Numbness & parasthesia in B 12 deficiency anemia.

• 2. Signs: 1. Pallor discoloration of skin & mucous membrane. 2. Rapid pulse rate & decreased in blood pressure. 3. Ejection systolic murmur. 4. Angular stomatitis, loss of tongue papillae & tongue ulcer in foliate deficiency. 5. Jaundice , hepato-splenomegaly in hemoglobinpathies. 6. Koilonychias of fingers in chronic anemia.
Clinical features of sickle cell crisis • 1. Sudden sever bone pain mainly in upper & lower limbs. 2. Chest pain. 3. Hematuria. 4. Sever pallor & jaundice. 5. Rapid pulse & low blood pressure.
Investigations • A. Iron deficiency anemia: 1. Decreased serum ferritin level. 2. Decreased serum iron level. 3. Increased total iron binding capacity evel. 4. Blood film show microcytic (decreased MCV) & hypo chromic (decreased MCHC). 5. Bone marrow shows absence of stainable iron.
• B. Foliate deficiency anemia: 1. Decreased serum foliate level. 2. Decreased red cell foliate level. 3. Decreased reticulocytes. 4. Blood film shows macrocytic (increased MCV) with hyper segmentation of nuclei of neutrophil. 5. Bone marrow shows large erythroblasts & giant metamylocyte. • C. B 12 deficiency anemia: Decreased serum B 12 level.
• D. Hemoglobinpathy: 1. Increased reticulocytes & decreased platelets & WBC count. 2. Blood film shows sickle shaped red cells when exposed to reducing agents or hypoxia (positive sickling test) & features of hyposplenism (Howell jolly bodies). 3. Normal MCV &MCHC; if these are low; think about associated iron deficiency or thalassemia trait. 4. Increased serum bilirubin level. 5. Hb electrophoresis to detect type of Hb, amount & character of Hb variant.
Treatment • Iron deficiency anemia: Iron therapy can be used as: 1. Prophylactic: - used in asymptomatic women to prevent development of anemia in pregnancy as iron demand increase. 2. Therapeutic: - used to treat symptomatic anemia in pregnancy. Iron therapy can be given as: A. Oral iron: - as Ferrous sulphate; each tablet contain (200 mg) which supply(67 mg)
• Of elemental iron. It is given thrice daily & it is cheap & best absorbed. Other oral types are ferrous fumerate & ferrous gluconate. These supply (37 mg) of elemental iron in (200 mg) tablet. G. I. side effects as nausea, vomiting & constipation are common. B. Parental iron: - It is given as iron dextran (Inferone) I. V. as infusion or bolus dose. Iron sorbitol (jectofer) is given as I. M. The total dose of iron required is calculated by 1. 3 x. B. W. x. Hb deficit.
• Oral iron is same in efficiency as parental therefore it is given to treat anemia early in pregnancy & parental can given if : 1. Poor compliance of patient. 2. Poor intestinal absorption. 3. Intolerance to side effects. Response to iron therapy is assessed by rise in Hb level by 1 -2 gm/dl after two weeks. • Blood transfusion can be used to correct anemia late in pregnancy as Hb level is 8 gm/dl or less.
• Foliate deficiency anemia: Folic acid is given as either prophylactic as (1 mg tab. ) or as therapeutic as (5 mgtab. ). It is mandatory in those with hemoglobinpathies as 5 mg tab. Pre-pregnancy use is helpful to prevent N. T. D. • B 12 deficiency anemia: Treated by 1000 Ug injection once weekly. • Hemoglobinpathy: 1. Oral folic acid tablet of 5 mg twice daily. 2. Iron therapy can be used in sickle cell trait & thalassemia minor but not in sickle cell disease as there is risk of hemosiderosis.
• 3. Screening for U. T. I. & chest infection & treatment. 4. Ante partum blood transfusion may required to maintain normal Hb A constitute 60% of whole Hb ; this given either as prophylactic or selective when Hb level <8 gm/dl. 5. Discontinue (hydroxyurea); a drug that increased Hb. F, improve red cell hydration, decrease polymerization of Hb. S since it is teratogenic.
Treatment of sickle cell crisis • • • Adequate hydration. Adequate oxygen supply. Adequate analgesia & pain killer. Treatment of infection any where. Blood transfusion.
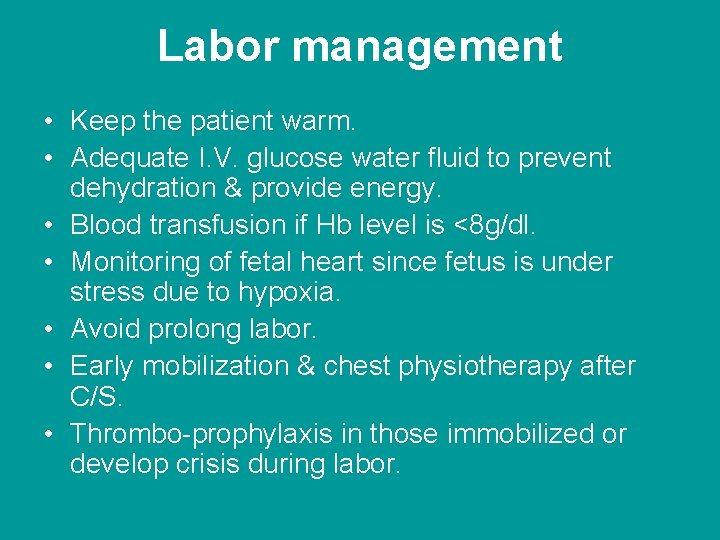
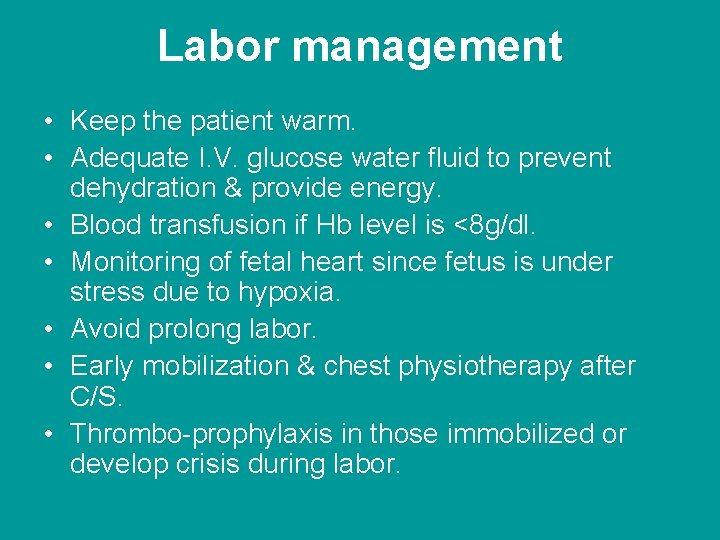
Labor management • Keep the patient warm. • Adequate I. V. glucose water fluid to prevent dehydration & provide energy. • Blood transfusion if Hb level is <8 g/dl. • Monitoring of fetal heart since fetus is under stress due to hypoxia. • Avoid prolong labor. • Early mobilization & chest physiotherapy after C/S. • Thrombo-prophylaxis in those immobilized or develop crisis during labor.
Thank you •
 Spotting in pregnancy
Spotting in pregnancy Anemia in pregnancy guideline
Anemia in pregnancy guideline Dashod dog
Dashod dog Anemia pregnancy
Anemia pregnancy Nursing care plan for anemia in pregnancy slideshare
Nursing care plan for anemia in pregnancy slideshare Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Causes of macrocytic anaemia
Causes of macrocytic anaemia Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia A collection of well defined objects
A collection of well defined objects Proper places
Proper places Normal pregnancy definition
Normal pregnancy definition Normal pregnancy definition
Normal pregnancy definition Malaria in pregnancy definition
Malaria in pregnancy definition Malaria in pregnancy definition
Malaria in pregnancy definition Piecewise defined function definition
Piecewise defined function definition Pregnancy declaration
Pregnancy declaration Dystocia
Dystocia Sola pith hymen
Sola pith hymen Pregnancy rhinitis treatment
Pregnancy rhinitis treatment Chapter 16 lesson 2 the male reproductive system
Chapter 16 lesson 2 the male reproductive system Hypothyroidism treatment in pregnancy
Hypothyroidism treatment in pregnancy Iat
Iat Nursing theories related to teenage pregnancy
Nursing theories related to teenage pregnancy For teen
For teen Folic acid dose in pregnancy
Folic acid dose in pregnancy Epilization
Epilization