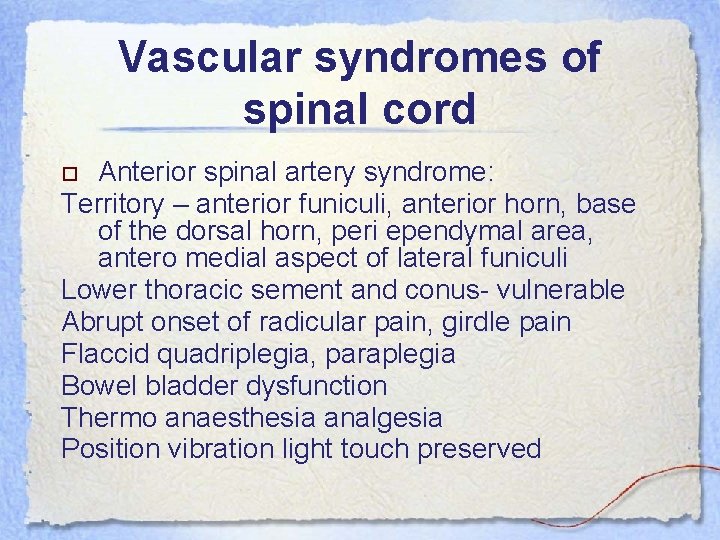
Anatomy Spinal cord ends as conus medullaris at

- Slides: 35
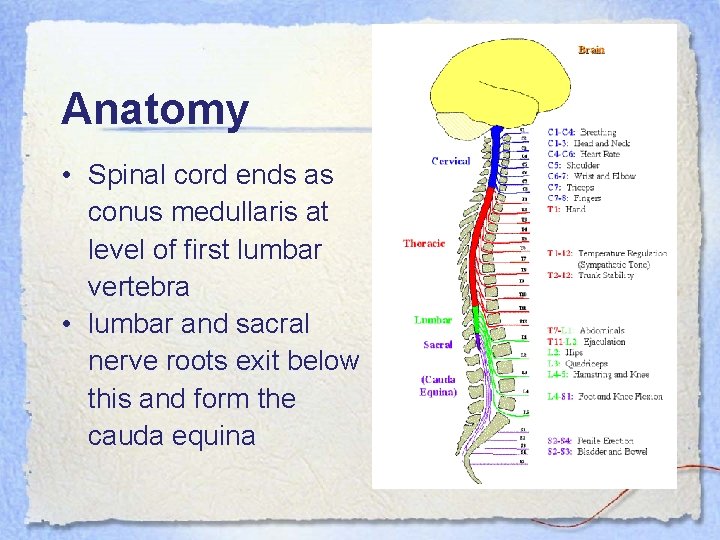
Anatomy • Spinal cord ends as conus medullaris at level of first lumbar vertebra • lumbar and sacral nerve roots exit below this and form the cauda equina
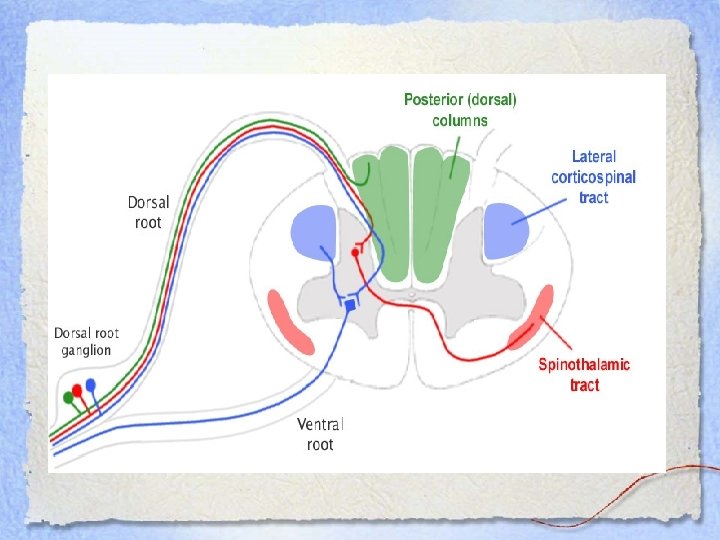
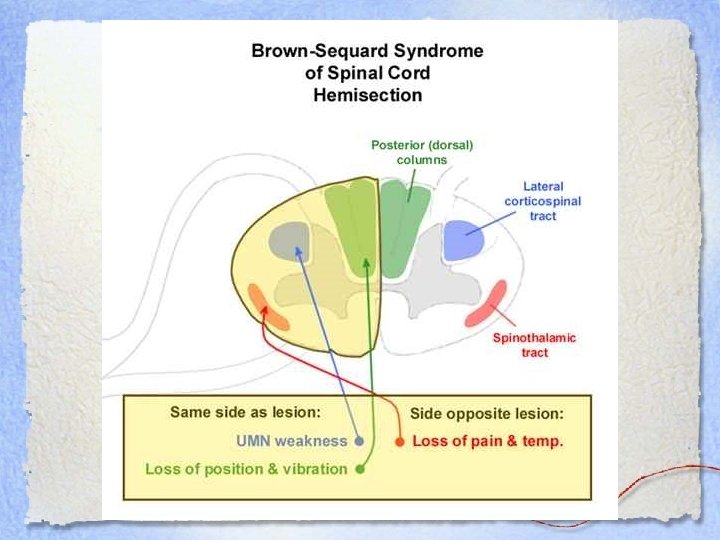
Neuroanatomy • Corticospinal tracts • Spinothalamic tracts • Dorsal (posterior) columns
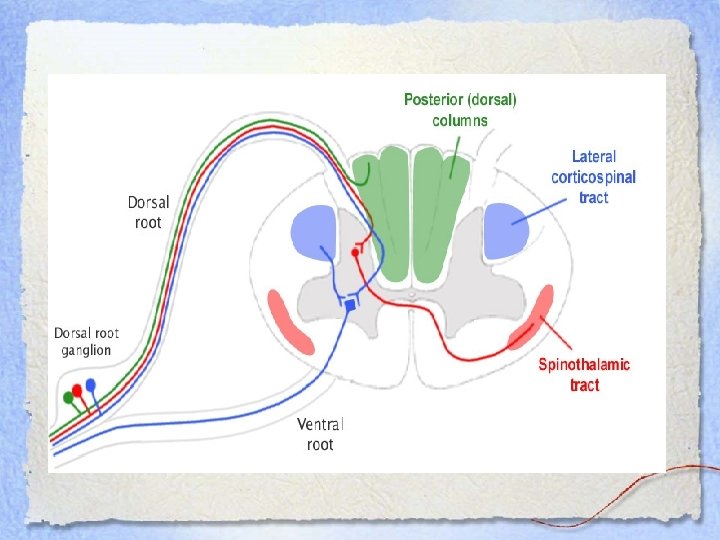
Corticospinal Tract • Descending motor pathway • Forms the pyramid of the medulla • In the lower medulla, 90% of fibers decussate and descend as the lateral corticospinal tract • Synapse on LMN in the spinal cord • 10% that do not cross descend as the ventral corticospinal tract • Damage to this part cause ipsilateral UMN findings

Spinothalmic Tract • Ascending sensory tract from skin and muscle via dorsal root ganglia to cerebral cortex • Temperature and pain sensation • Damage to this part of the spinal cord causes: – Loss of pain and temperature sensation in the contralateral side – Loss begins 1 -2 segments below the level of the lesion
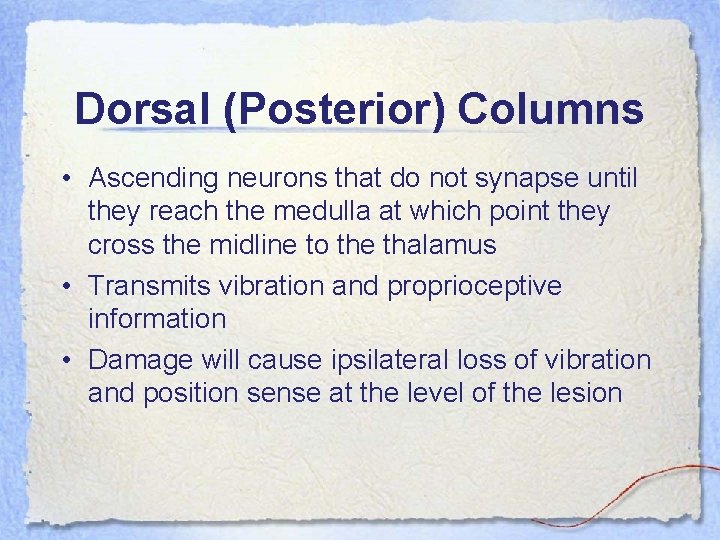
Dorsal (Posterior) Columns • Ascending neurons that do not synapse until they reach the medulla at which point they cross the midline to the thalamus • Transmits vibration and proprioceptive information • Damage will cause ipsilateral loss of vibration and position sense at the level of the lesion
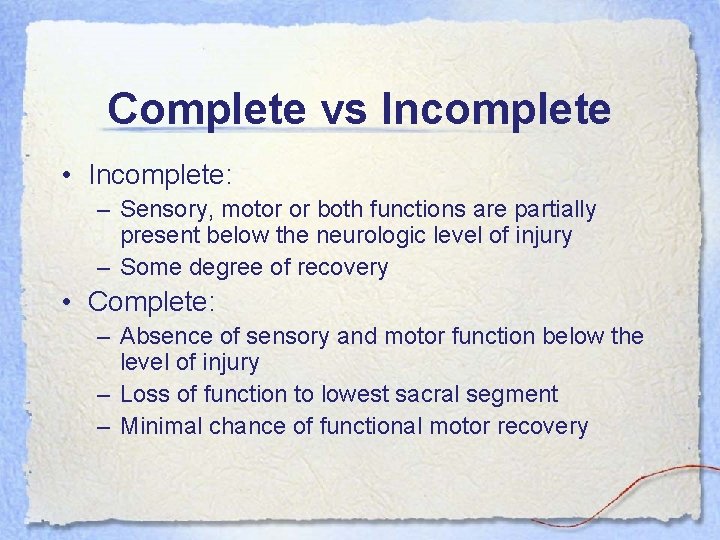
Complete vs Incomplete • Incomplete: – Sensory, motor or both functions are partially present below the neurologic level of injury – Some degree of recovery • Complete: – Absence of sensory and motor function below the level of injury – Loss of function to lowest sacral segment – Minimal chance of functional motor recovery
Light touch… • Transmitted through both the dorsal columns and the spinothalamic tracts • Lost entirely ONLY if both tracts are damaged
Upper vs. Lower Motor Neuron • Upper motor neuron lesion – Motor cortex brainstem spinal cord internal capsule • Lower motor neuron lesion – Anterior horn cell plexus peripheral nerve root
Basic Features of Spinal Cord Disease • UMN findings below the lesion – Hyperreflexia and Babinski’s • Sensory and motor involvement that localizes to a spinal cord level • Bowel and Bladder dysfunction common • Remember that the spinal cord ends at about T 12 -L 1
Motor Exam • Strength - helps to localize the lesion – Upper cervical • Quadriplegia with impaired respiration – Lower cervical • Proximal arm strength preserved • Hand weakness and leg weakness – Thoracic • Paraplegia – Can also see paraplegia with a midline lesion in the brain • Tone – Increased distal to the lesion
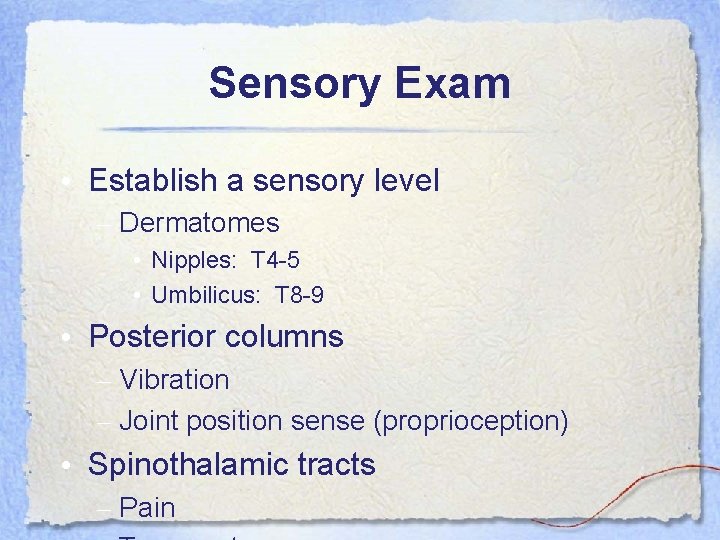
Sensory Exam • Establish a sensory level – Dermatomes • Nipples: T 4 -5 • Umbilicus: T 8 -9 • Posterior columns – Vibration – Joint position sense (proprioception) • Spinothalamic tracts – Pain
Autonomic disturbances • Neurogenic bladder – Urgency, incontinence, retention • Bowel dysfunction – Constipation more frequent than incontinence • With a high cord lesion, loss of blood pressure control • Alteration in sweating
Total transsection - Injuries - Tumors - infection
Total transsection Below the lesion: first stage - Loss of motor function - Loss of sensory - Areflexion - Decreased tension of muscles
Total transsection Below the lesion: second stage - Normal reflexes increased - Normal tension increased spasticity
Total transsection Bladder: 1. Areflexion 2. Ischuria paradoxa 3. Automatic or autonomic
Spinal Shock • Loss of neurological function and autonomic tone below level of lesion • Loss of all reflexes • Resolves over 24 -48 h but may last for days
Spinal Shock • Symptoms: • • • Flaccid paralysis Loss of sensation Bladder incontinence Bradycardia Hypotension Hypothermia
Hypotension • Must determine cause: – – Spinal cord injury Blood loss Cardiac injury Combination of above
Neurogenic Shock • Neurogenic Shock: – Warm – Peripherally vasodilated – Bradycardic • Bradycardia may be caused by something other than neurogenic shock • Cervical spine injury may cause sympathetic denervation
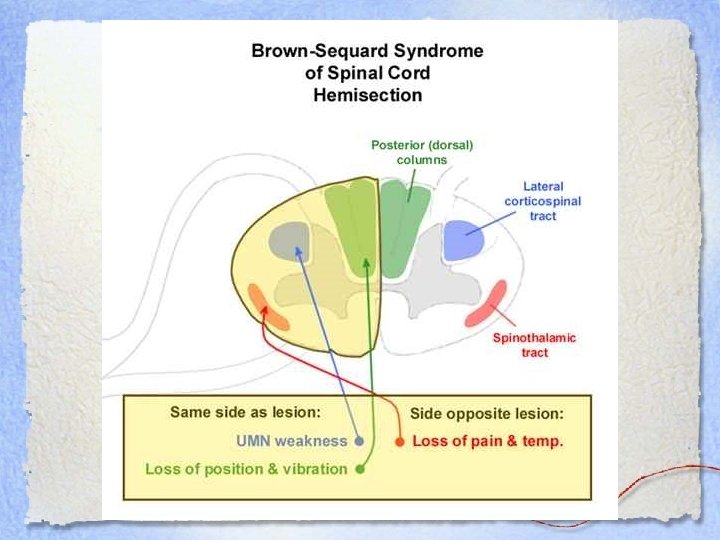
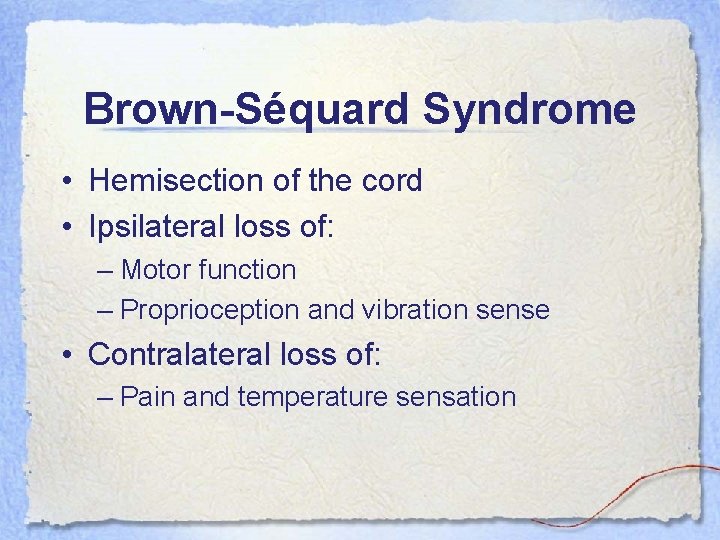
Brown-Séquard Syndrome • Hemisection of the cord • Ipsilateral loss of: – Motor function – Proprioception and vibration sense • Contralateral loss of: – Pain and temperature sensation
BSS • Caused by: – Penetrating injury – Lateral cord compression from: • • Disk protrusion Hematomas Bone injury Tumours • Prognosis: GOOD
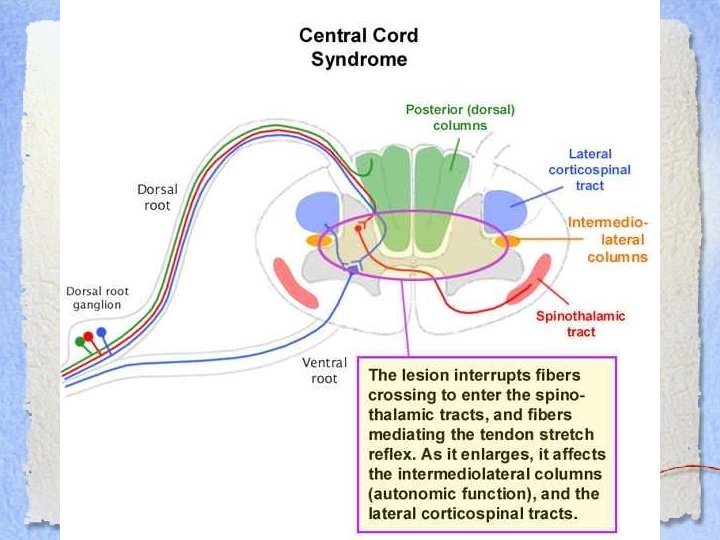
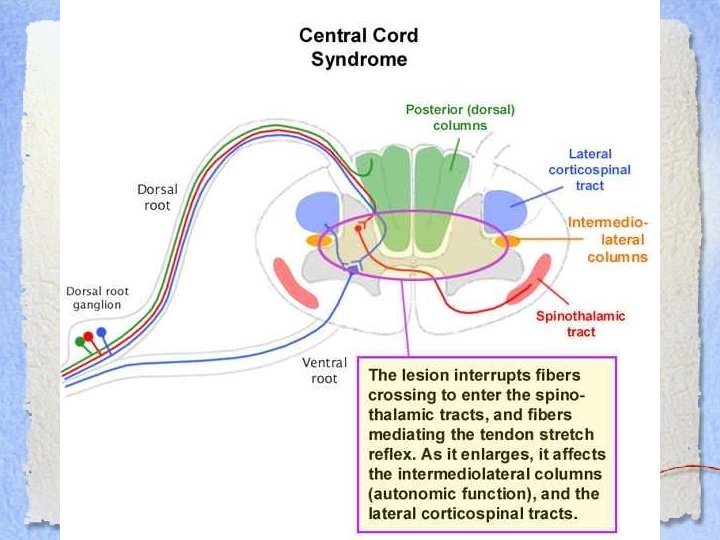
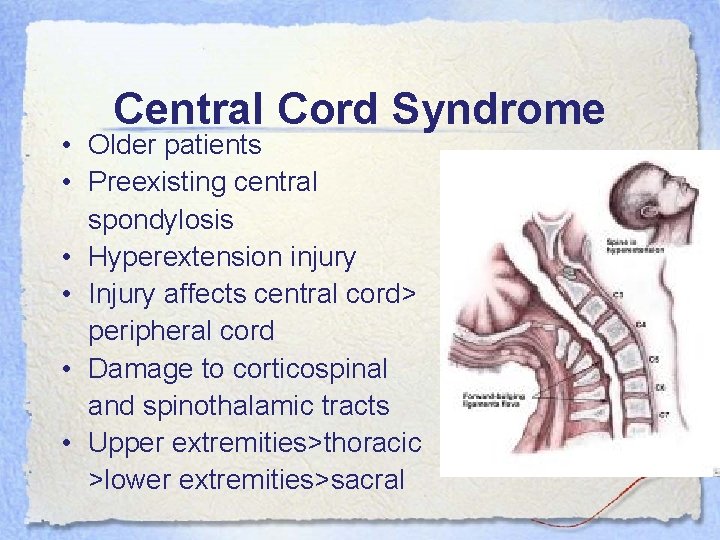
Central Cord Syndrome • Older patients • Preexisting central spondylosis • Hyperextension injury • Injury affects central cord> peripheral cord • Damage to corticospinal and spinothalamic tracts • Upper extremities>thoracic >lower extremities>sacral
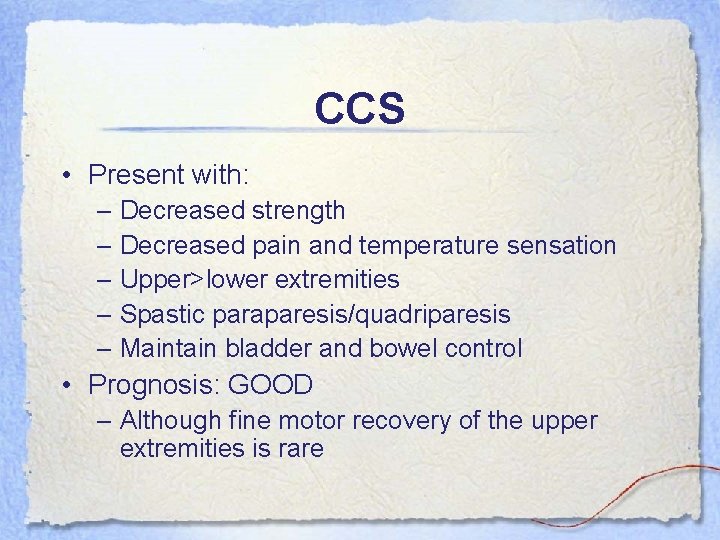
CCS • Present with: – Decreased strength – Decreased pain and temperature sensation – Upper>lower extremities – Spastic paraparesis/quadriparesis – Maintain bladder and bowel control • Prognosis: GOOD – Although fine motor recovery of the upper extremities is rare
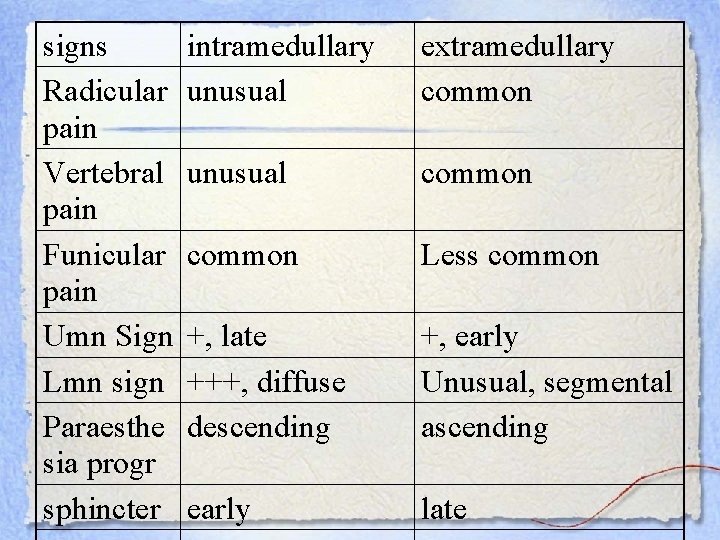
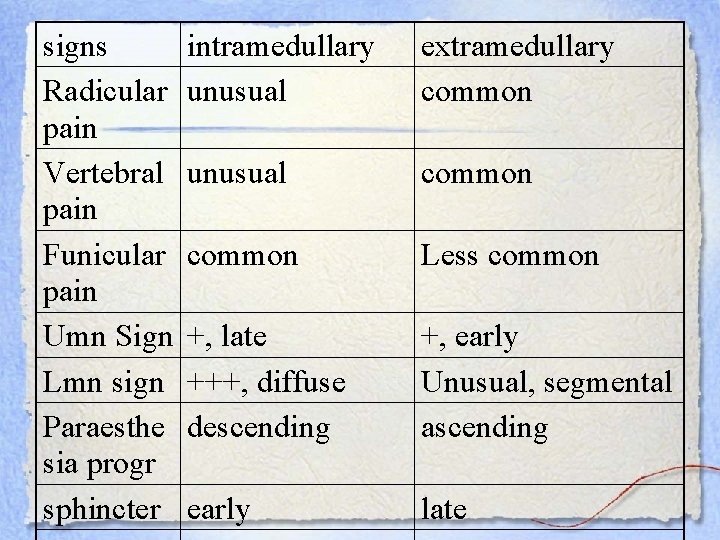
signs Radicular pain Vertebral pain Funicular pain Umn Sign Lmn sign Paraesthe sia progr sphincter intramedullary unusual extramedullary common unusual common Less common +, late +++, diffuse descending +, early Unusual, segmental ascending early late
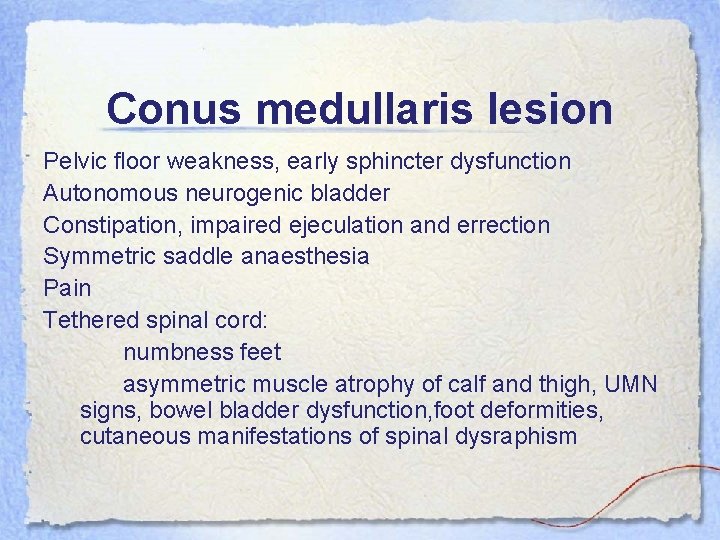
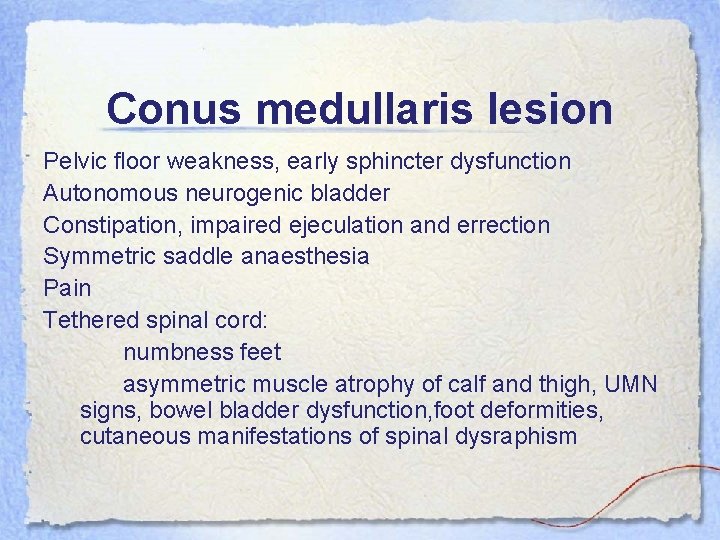
Conus medullaris lesion Pelvic floor weakness, early sphincter dysfunction Autonomous neurogenic bladder Constipation, impaired ejeculation and errection Symmetric saddle anaesthesia Pain Tethered spinal cord: numbness feet asymmetric muscle atrophy of calf and thigh, UMN signs, bowel bladder dysfunction, foot deformities, cutaneous manifestations of spinal dysraphism
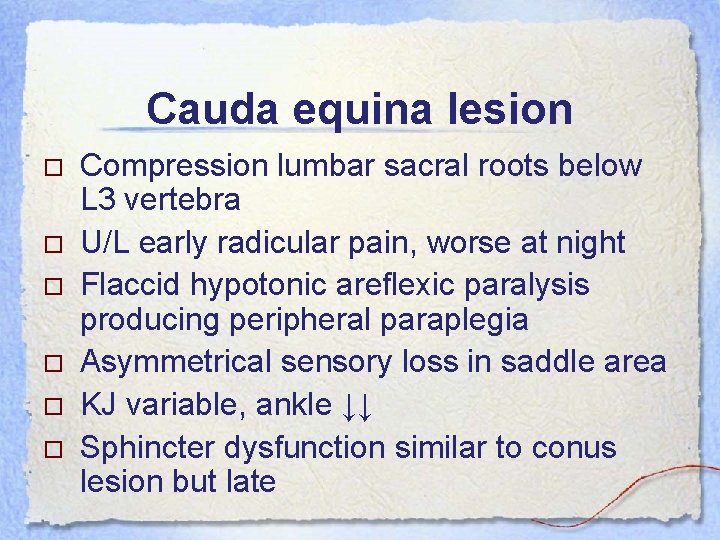
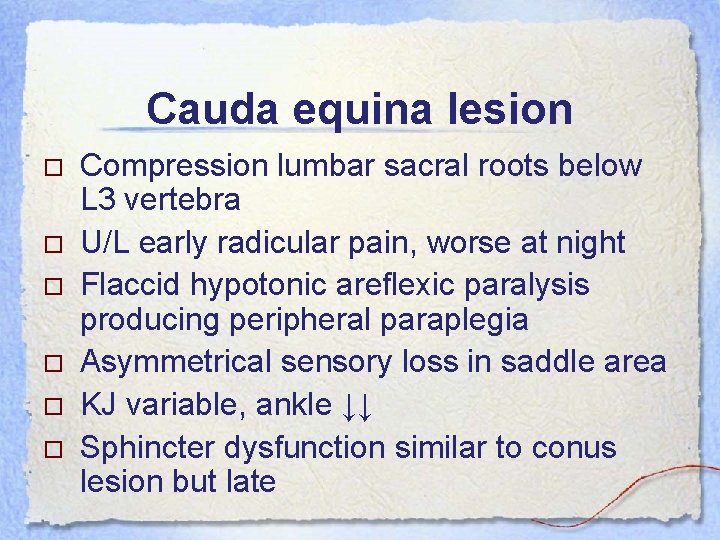
Cauda equina lesion Compression lumbar sacral roots below L 3 vertebra U/L early radicular pain, worse at night Flaccid hypotonic areflexic paralysis producing peripheral paraplegia Asymmetrical sensory loss in saddle area KJ variable, ankle ↓↓ Sphincter dysfunction similar to conus lesion but late
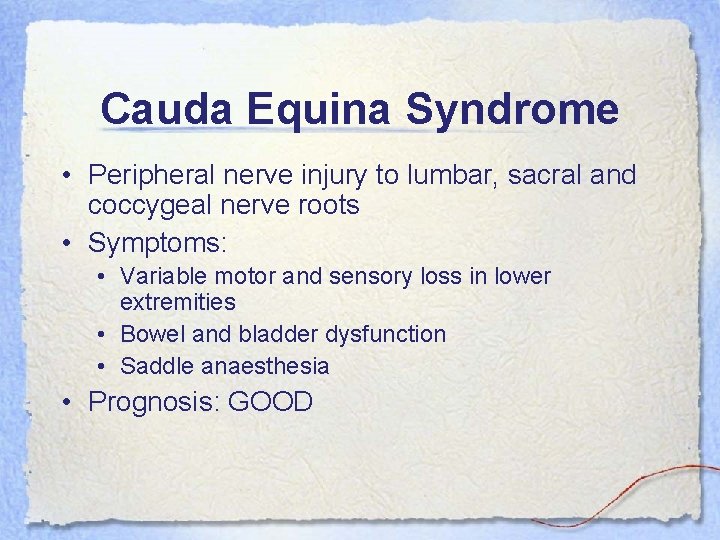
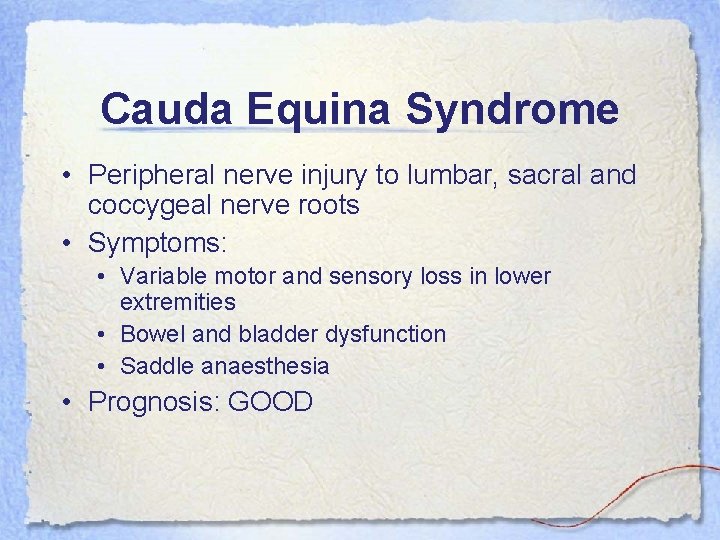
Cauda Equina Syndrome • Peripheral nerve injury to lumbar, sacral and coccygeal nerve roots • Symptoms: • Variable motor and sensory loss in lower extremities • Bowel and bladder dysfunction • Saddle anaesthesia • Prognosis: GOOD
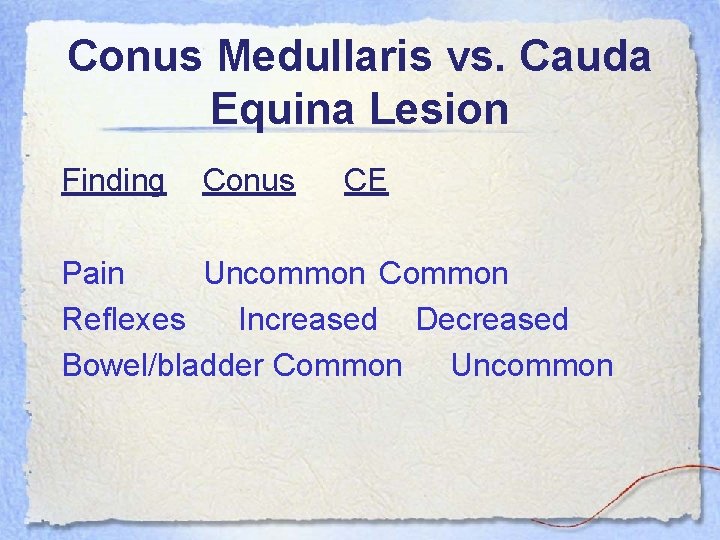
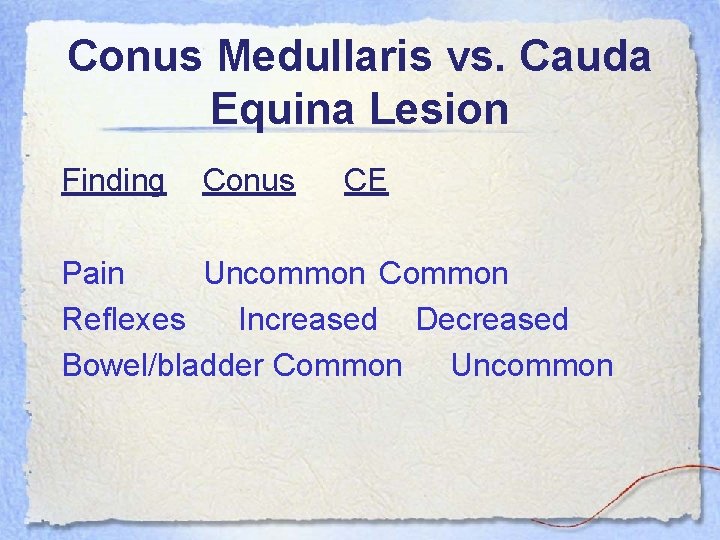
Conus Medullaris vs. Cauda Equina Lesion Finding Conus CE Pain Uncommon Common Reflexes Increased Decreased Bowel/bladder Common Uncommon
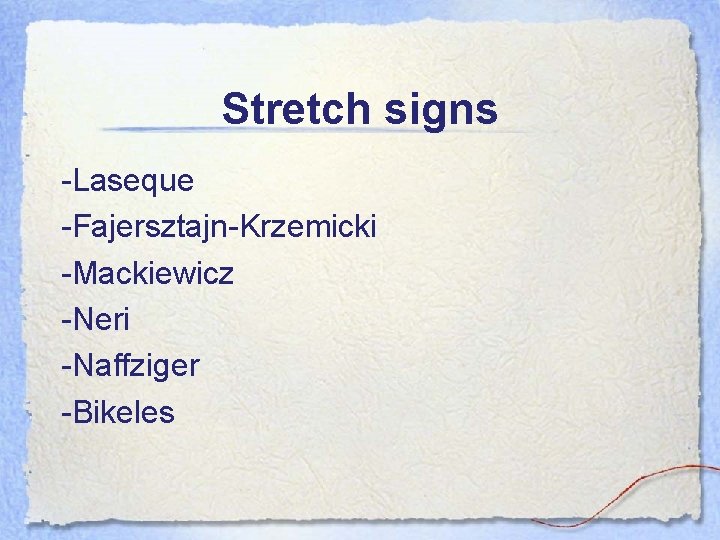
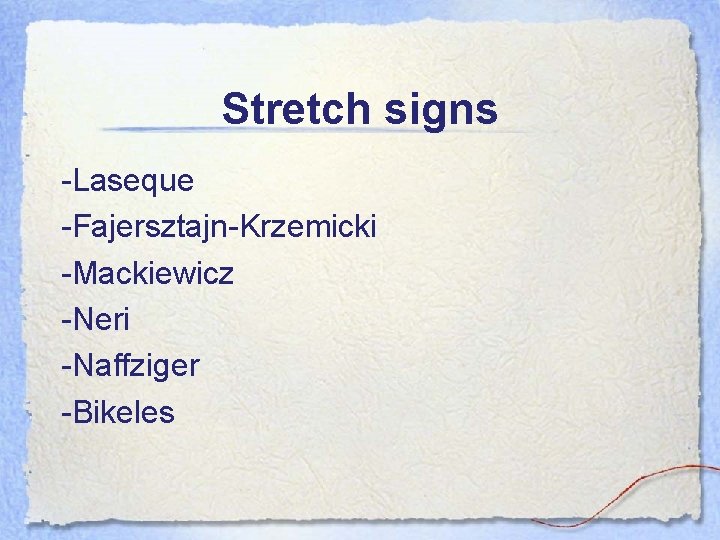
Stretch signs -Laseque -Fajersztajn-Krzemicki -Mackiewicz -Neri -Naffziger -Bikeles
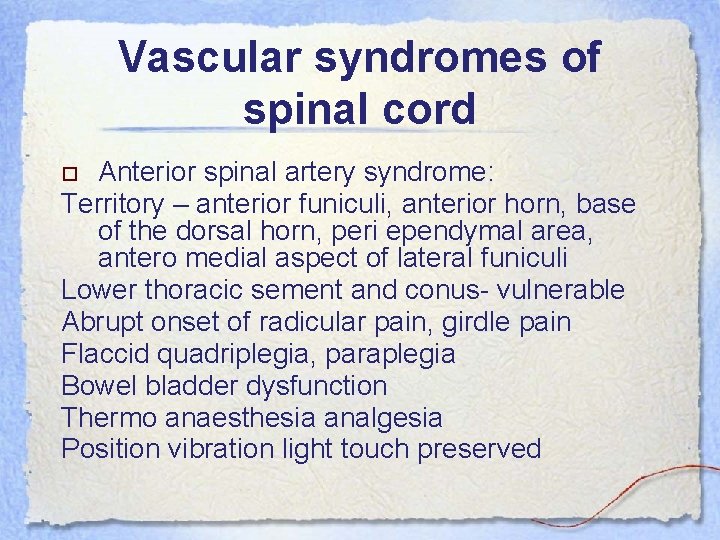
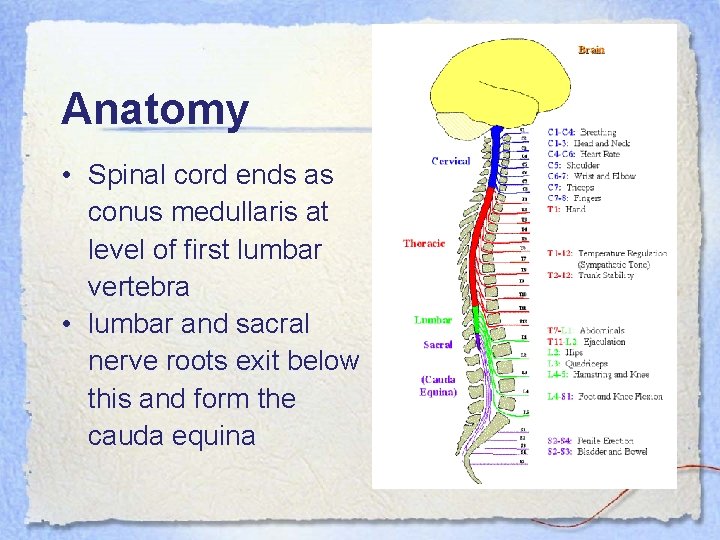
Vascular syndromes of spinal cord Anterior spinal artery syndrome: Territory – anterior funiculi, anterior horn, base of the dorsal horn, peri ependymal area, antero medial aspect of lateral funiculi Lower thoracic sement and conus- vulnerable Abrupt onset of radicular pain, girdle pain Flaccid quadriplegia, paraplegia Bowel bladder dysfunction Thermo anaesthesia analgesia Position vibration light touch preserved
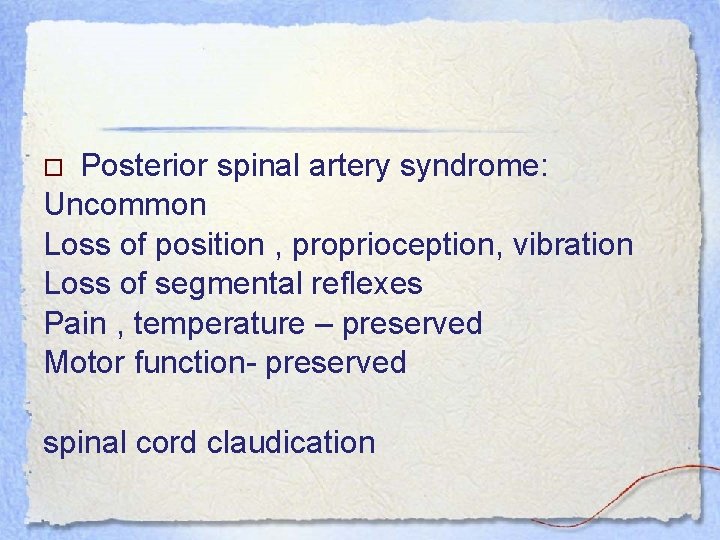
Posterior spinal artery syndrome: Uncommon Loss of position , proprioception, vibration Loss of segmental reflexes Pain , temperature – preserved Motor function- preserved spinal cord claudication