ANATOMY PHYSIOLOGY TISSUES TISSUES group of similar cells
- Slides: 68
ANATOMY & PHYSIOLOGY TISSUES
TISSUES �group of similar cells specialized to perform a specific function
Tissues: 4 Types 1. 2. 3. 4. Epithelial Connective Muscle Nervous
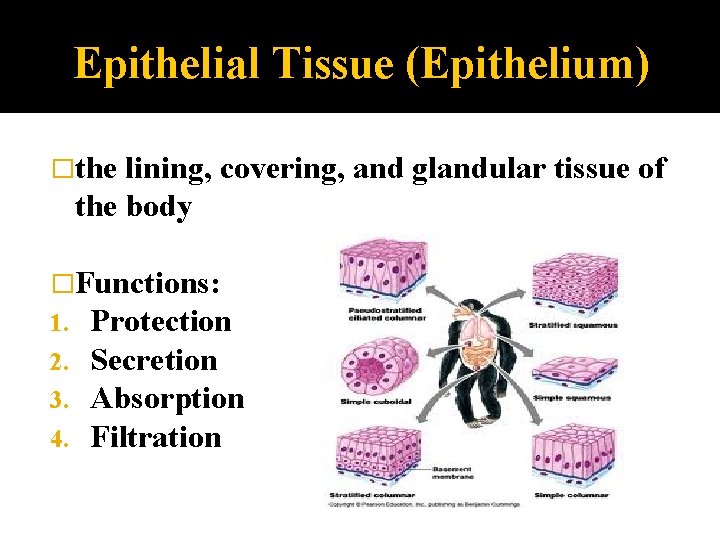
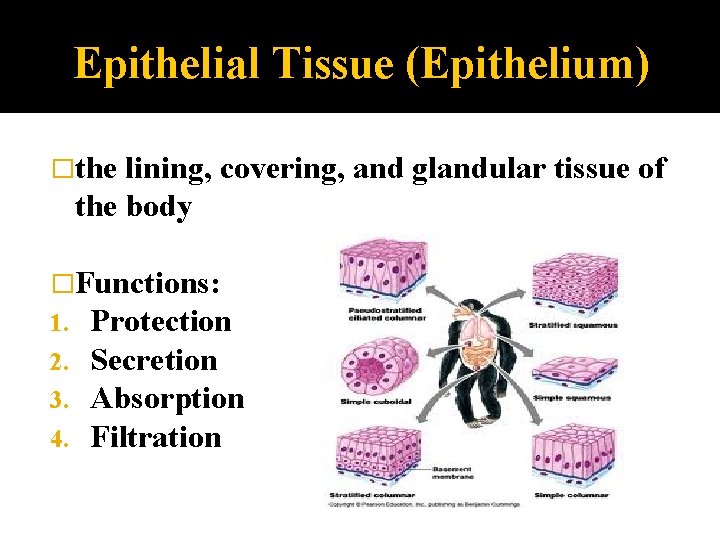
Epithelial Tissue (Epithelium) �the lining, covering, and glandular tissue of the body �Functions: 1. Protection 2. Secretion 3. Absorption 4. Filtration
Characteristic of Epithelium �cells close together, some connected by cell junctions �top layer exposed to exterior of body or inside of cavity (apical layer) �lower surface connected to a Basement Membrane (BM) �is avascular (no direct blood supply) �able to regenerate if well nourished
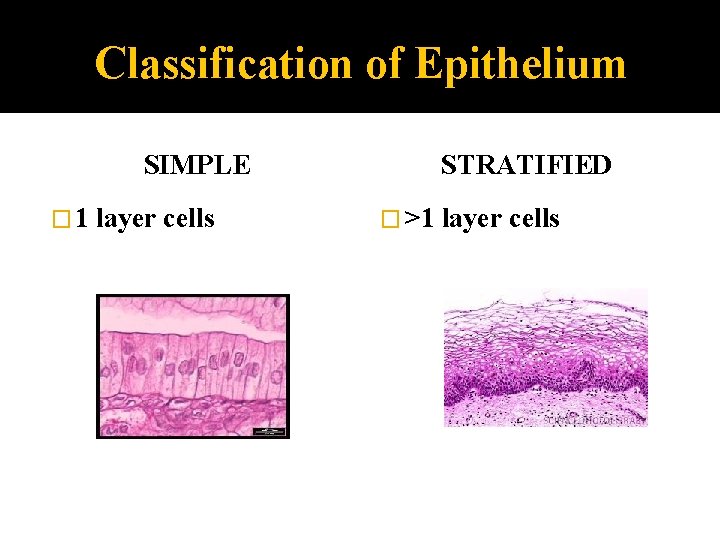
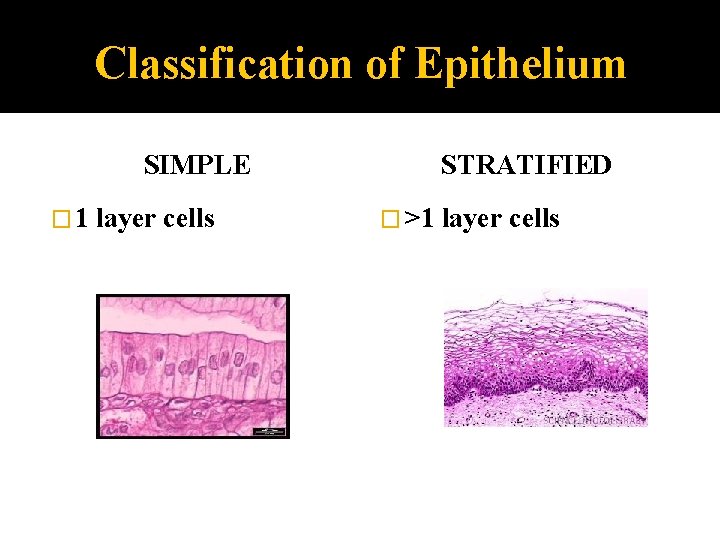
Classification of Epithelium SIMPLE � 1 layer cells STRATIFIED � >1 layer cells
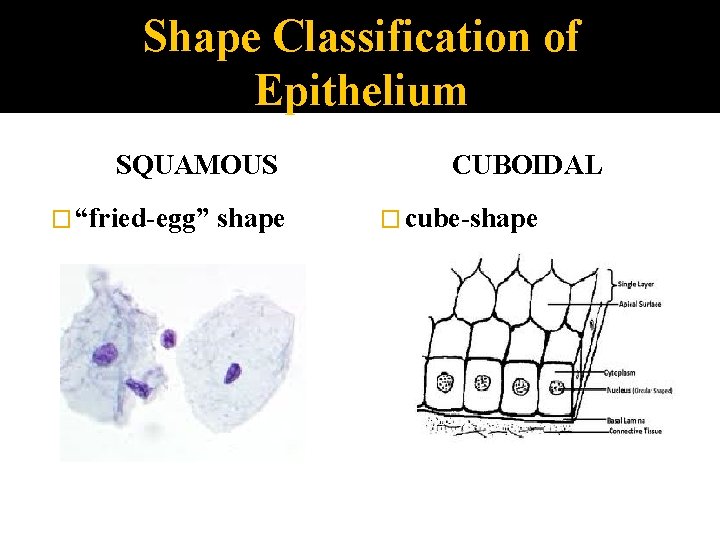
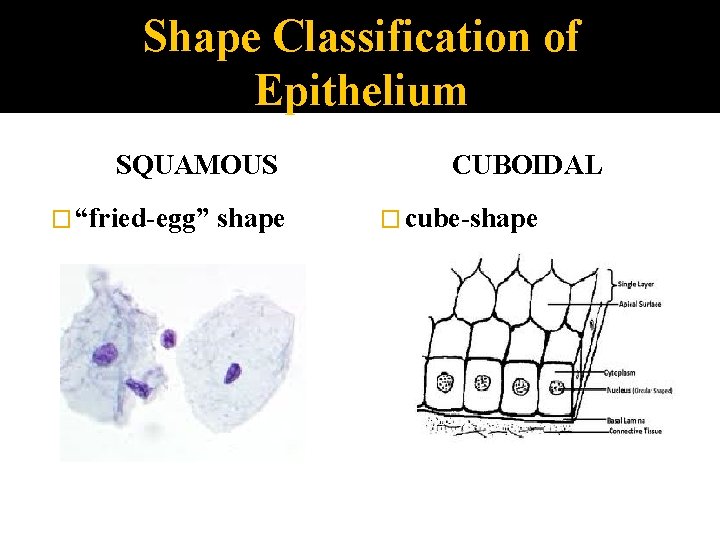
Shape Classification of Epithelium SQUAMOUS � “fried-egg” shape CUBOIDAL � cube-shape
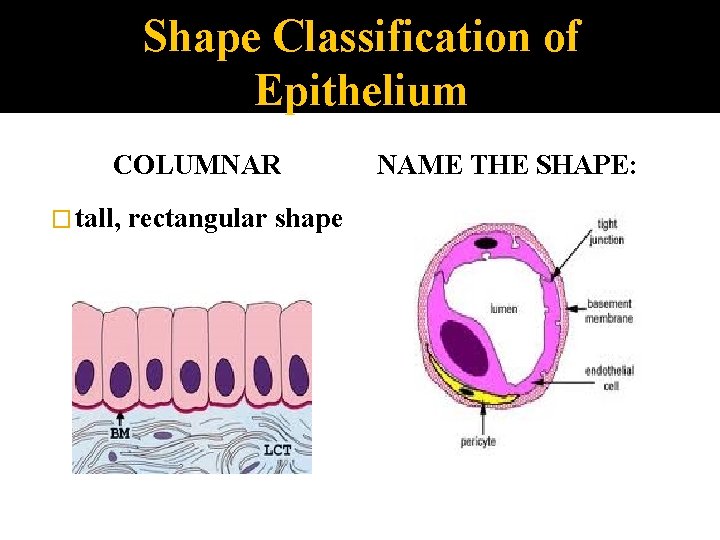
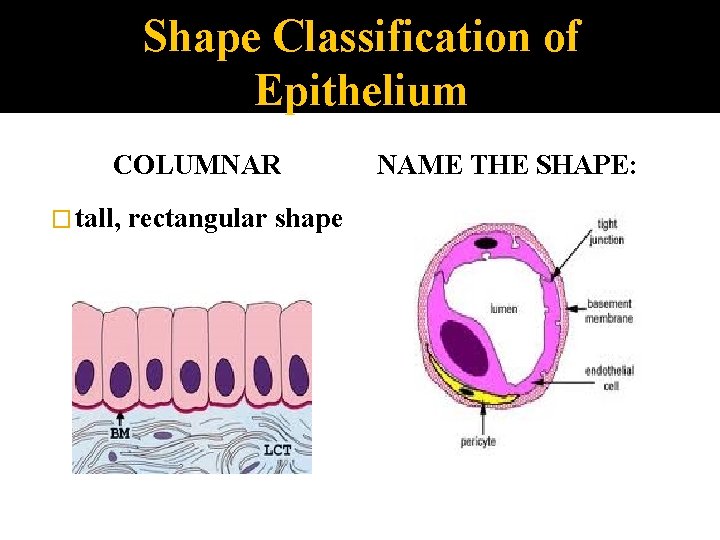
Shape Classification of Epithelium COLUMNAR � tall, rectangular shape NAME THE SHAPE:
Simple Epithelium � Functions: Absorption Secretion Filtration
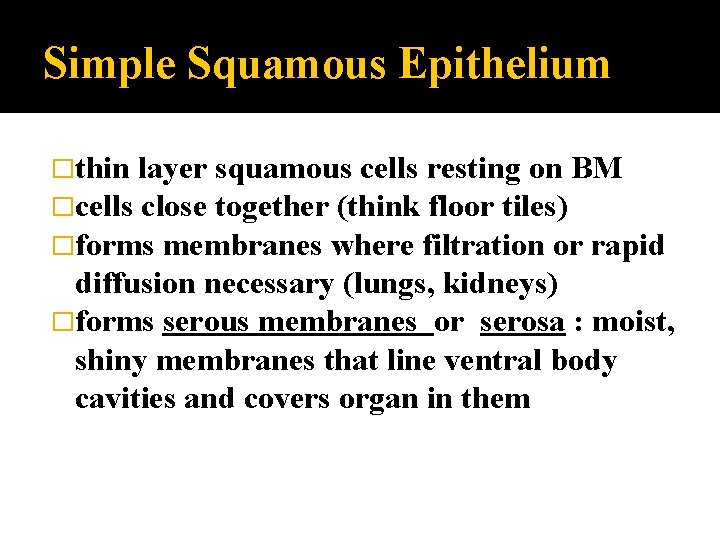
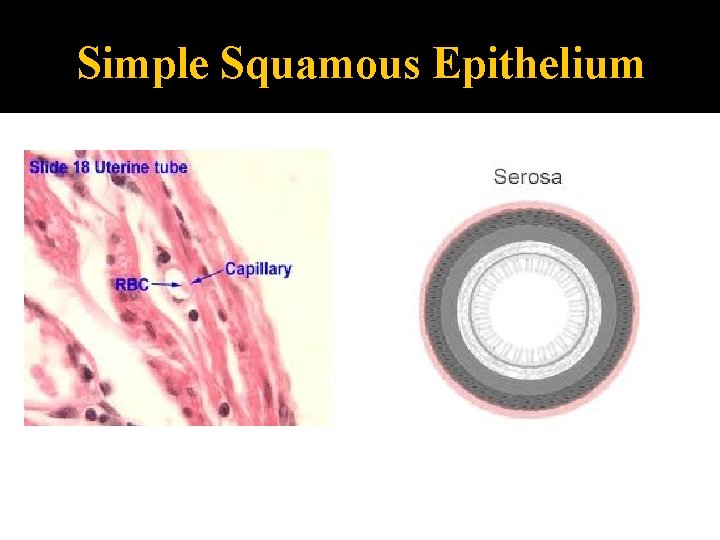
Simple Squamous Epithelium �thin layer squamous cells resting on BM �cells close together (think floor tiles) �forms membranes where filtration or rapid diffusion necessary (lungs, kidneys) �forms serous membranes or serosa : moist, shiny membranes that line ventral body cavities and covers organ in them
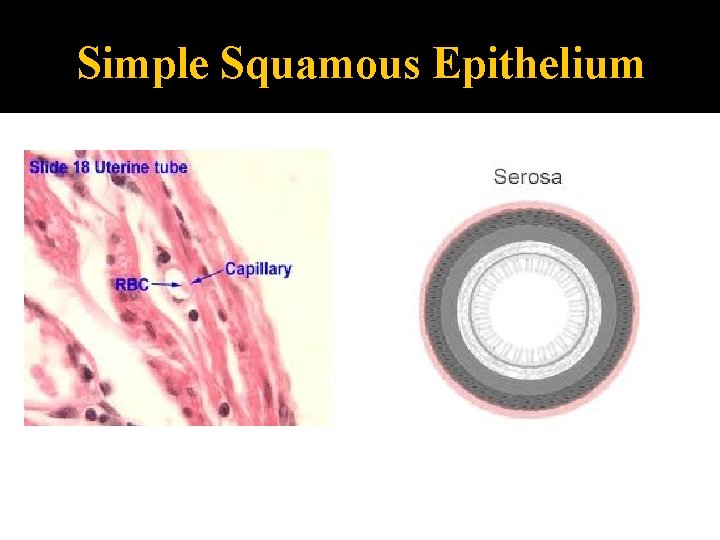
Simple Squamous Epithelium
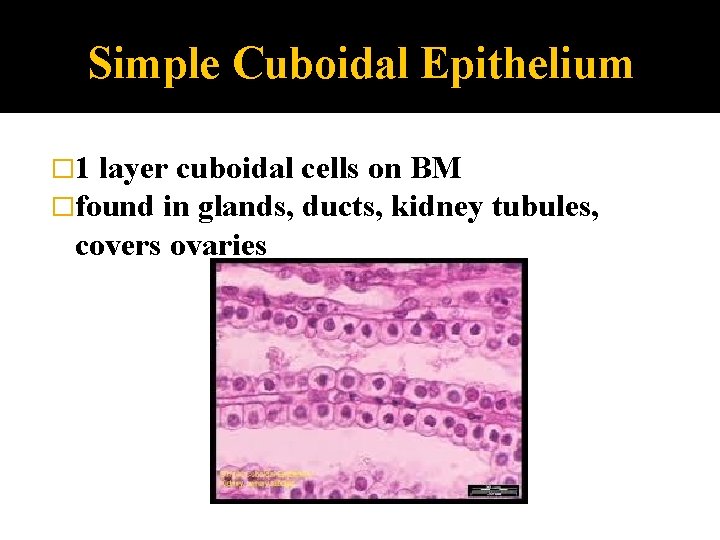
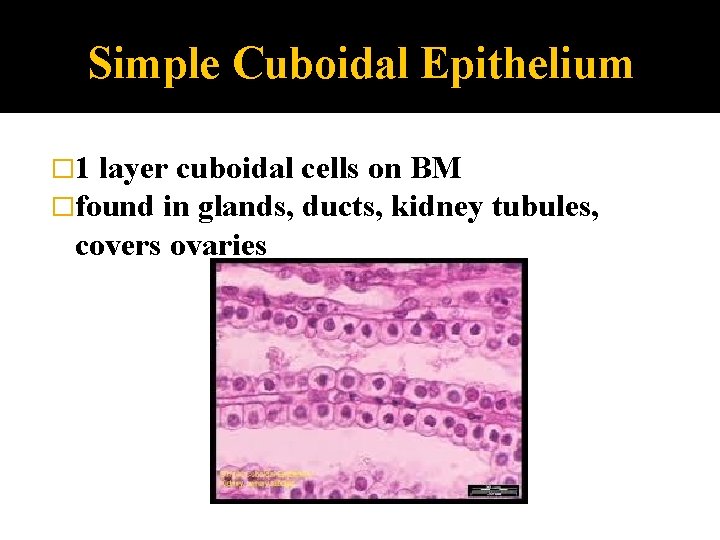
Simple Cuboidal Epithelium � 1 layer cuboidal cells on BM �found in glands, ducts, kidney covers ovaries tubules,
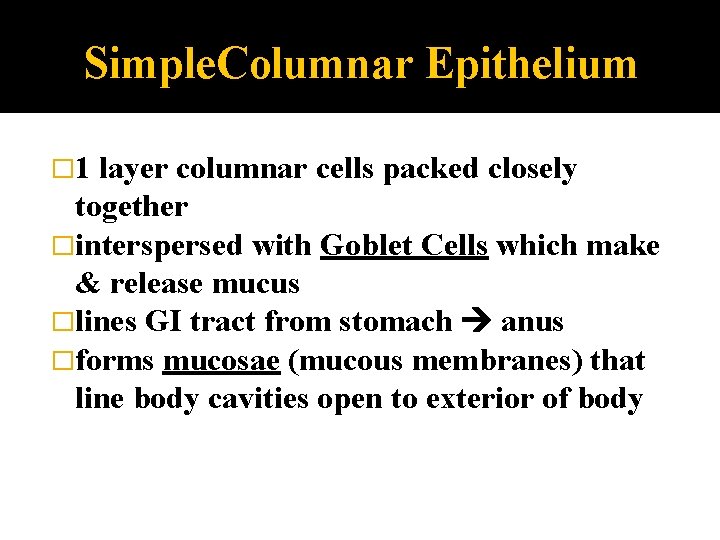
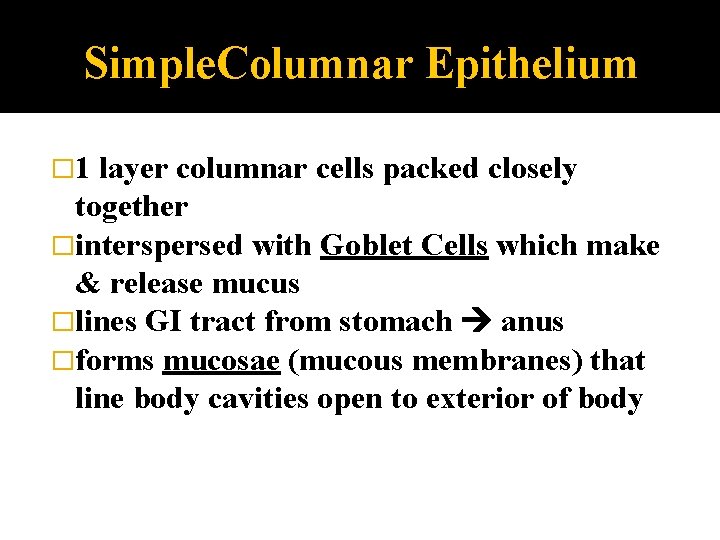
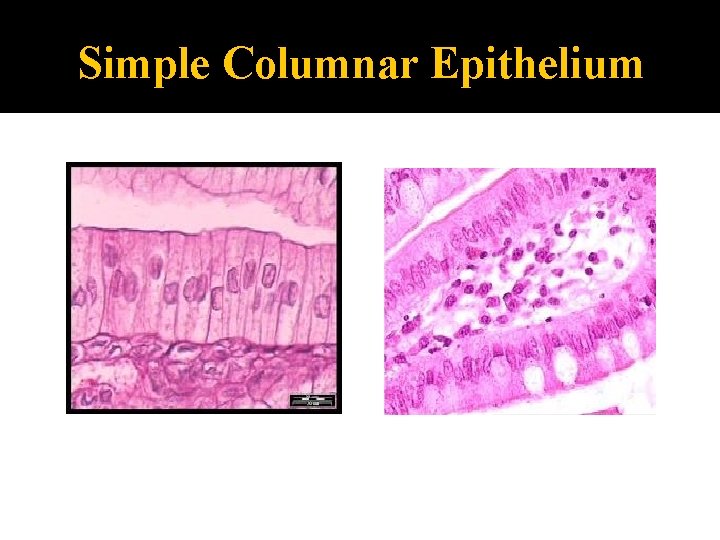
Simple. Columnar Epithelium � 1 layer columnar cells packed closely together �interspersed with Goblet Cells which make & release mucus �lines GI tract from stomach anus �forms mucosae (mucous membranes) that line body cavities open to exterior of body
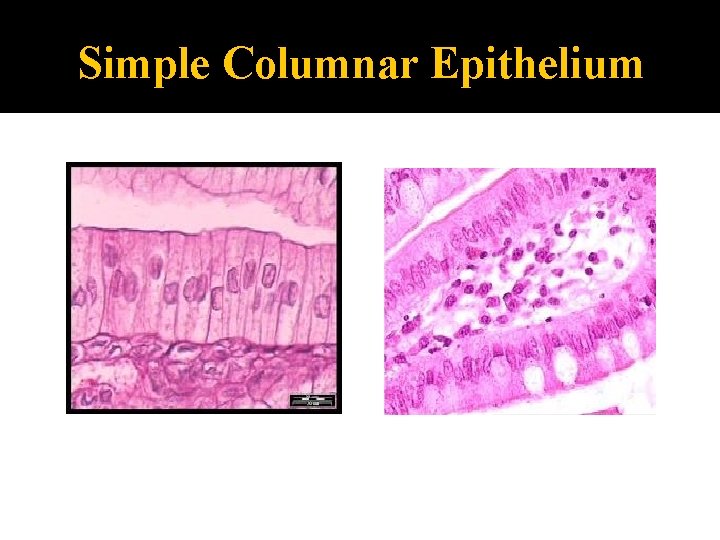
Simple Columnar Epithelium
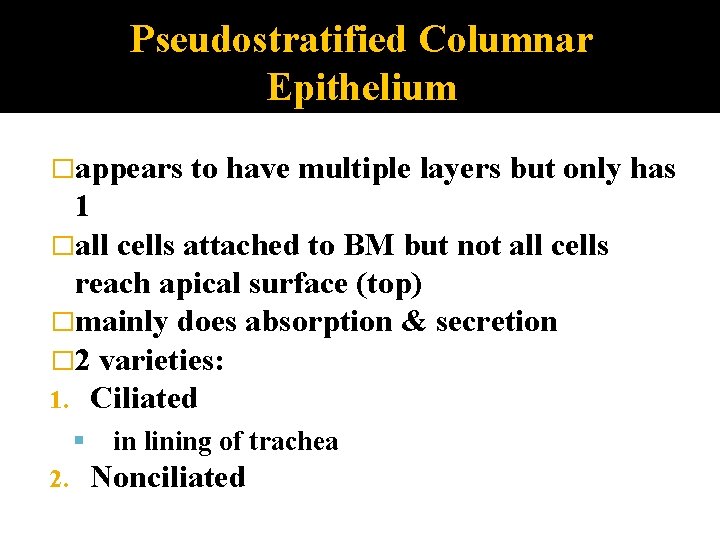
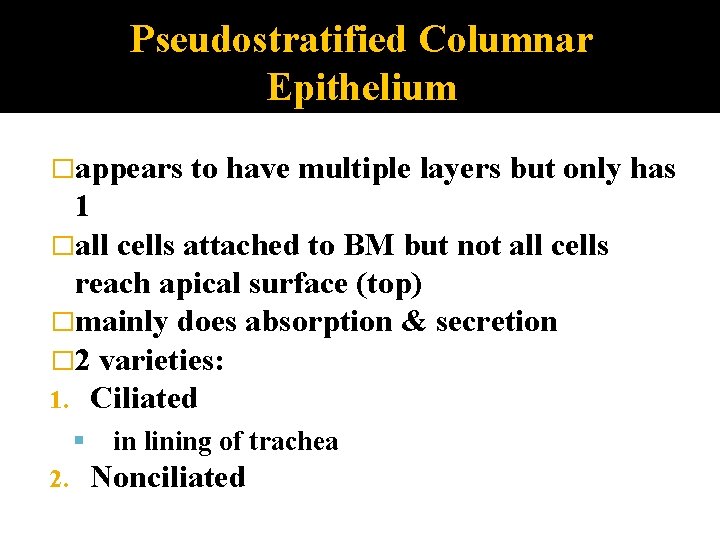
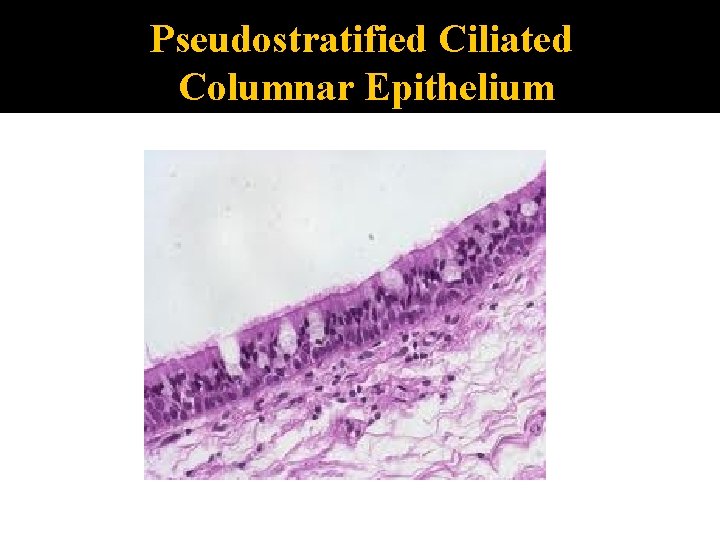
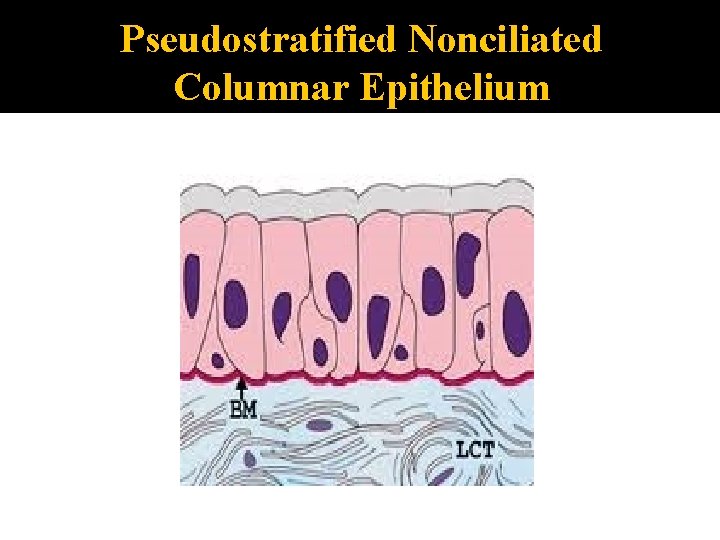
Pseudostratified Columnar Epithelium �appears to have multiple layers but only has 1 �all cells attached to BM but not all cells reach apical surface (top) �mainly does absorption & secretion � 2 varieties: 1. Ciliated 2. in lining of trachea Nonciliated
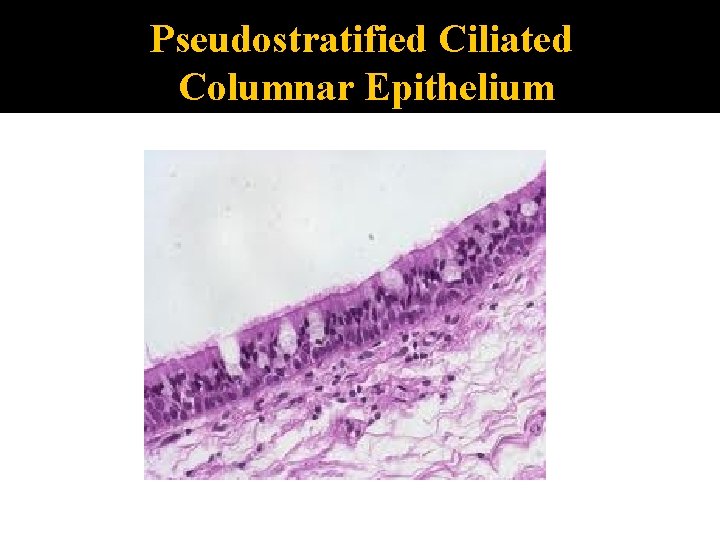
Pseudostratified Ciliated Columnar Epithelium
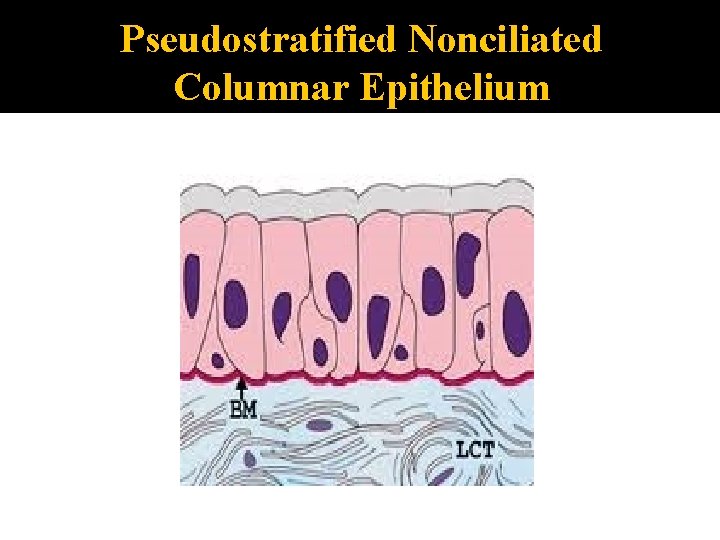
Pseudostratified Nonciliated Columnar Epithelium
Stratified Epithelium �>1 layer of cells, epithelium named for shape of top layer �more durable than simple epithelium �primary function is protection
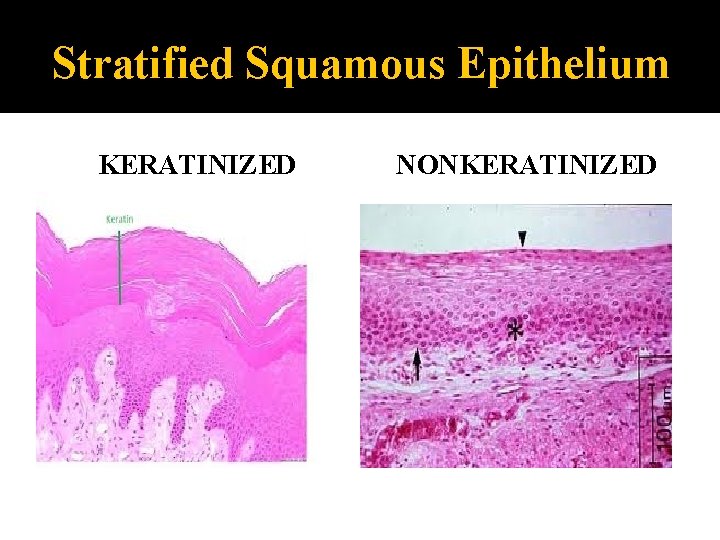
Stratified Squamous Epithelium �#1 stratified epithelium � 2 varieties: 1. keratinized 2. nonkeratinized in body Keratin: tough, insoluble protein found in hair, nails, & epidermis
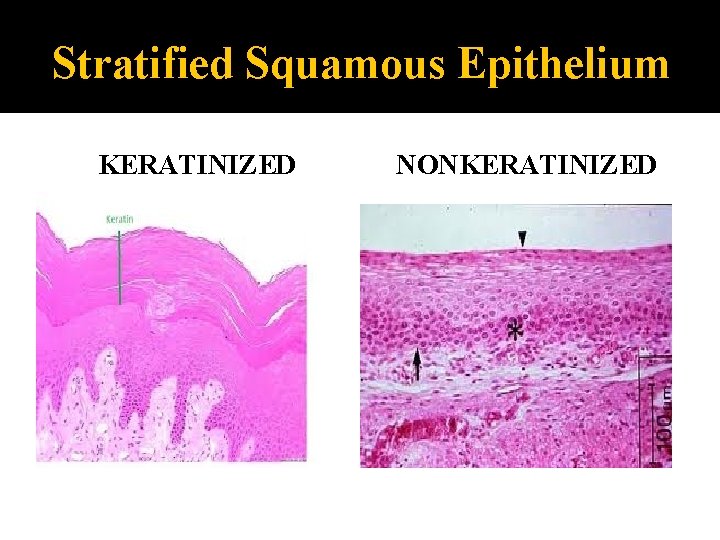
Stratified Squamous Epithelium KERATINIZED NONKERATINIZED
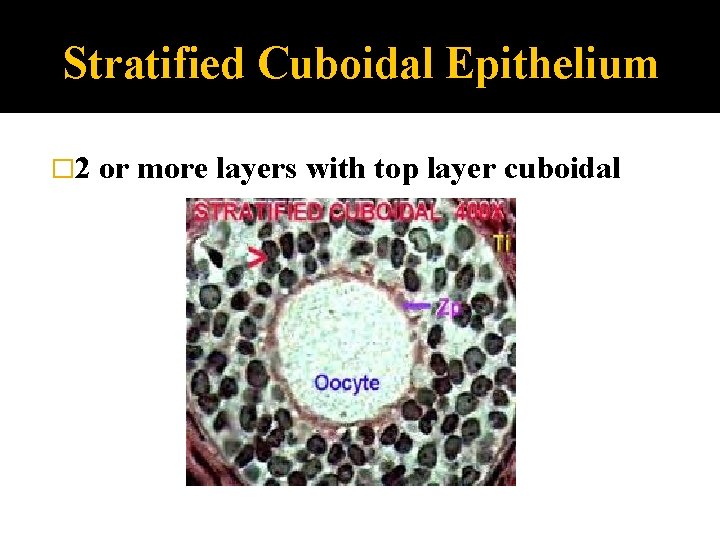
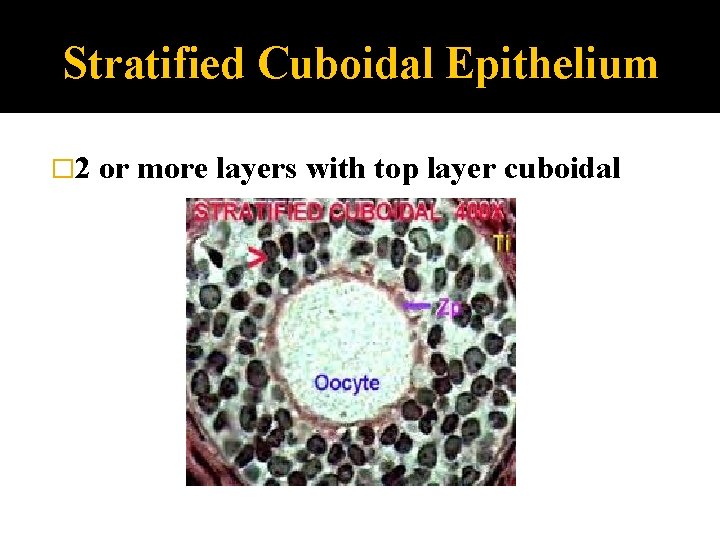
Stratified Cuboidal Epithelium � 2 or more layers with top layer cuboidal
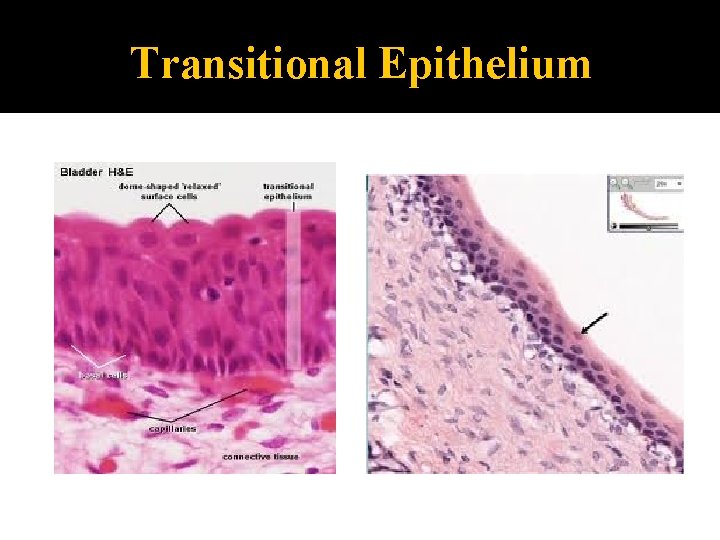
Transitional Epithelium �“transitions” from 1 shape to another �found in urinary bladder, ureters, urethra �when vol of urine high epitheliumis stretched and epithelium looks like squamous cells �when vol of urine low cells appear domeshaped, cuboidal
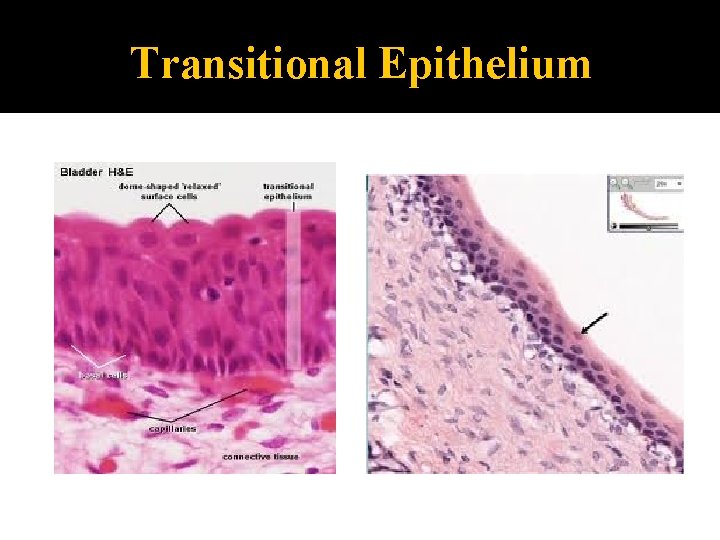
Transitional Epithelium
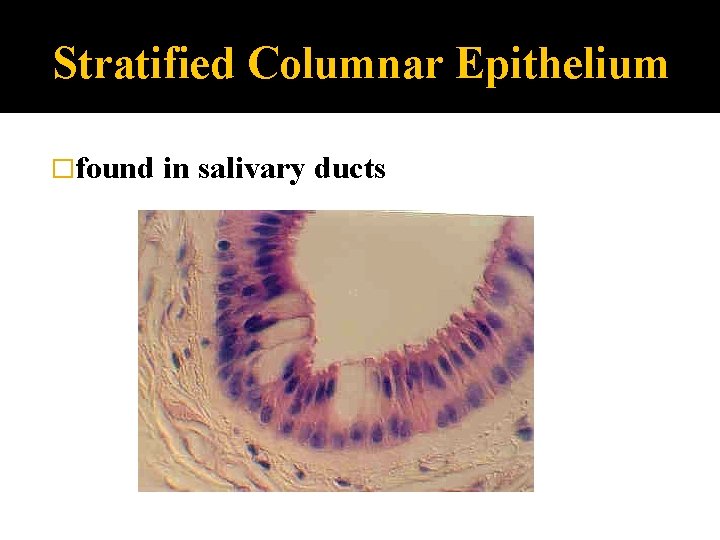
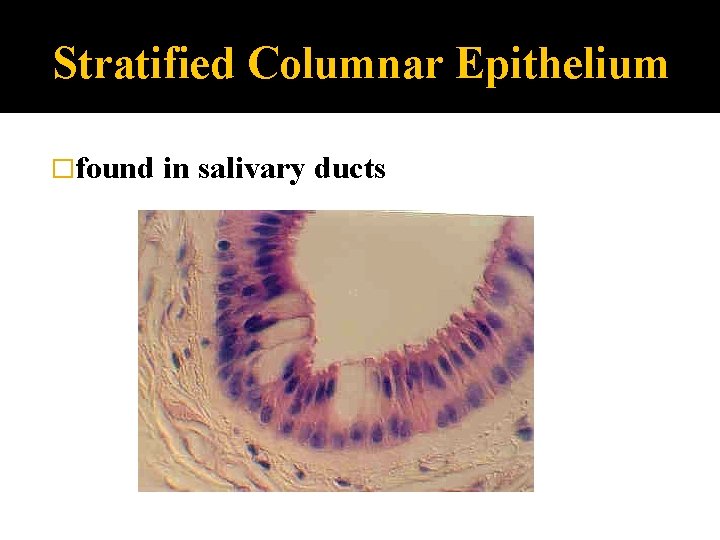
Stratified Columnar Epithelium �found in salivary ducts
Connective Tissue (CT) �connects things �is everywhere in body �#1 tissue type for amount and distribution
Connective Tissue Characteristics most CT well vascularized 1. 2. except: ▪ ligaments, tendons poor blood supply ▪ cartilage is avascular make extracellular matrix (in varying amounts)
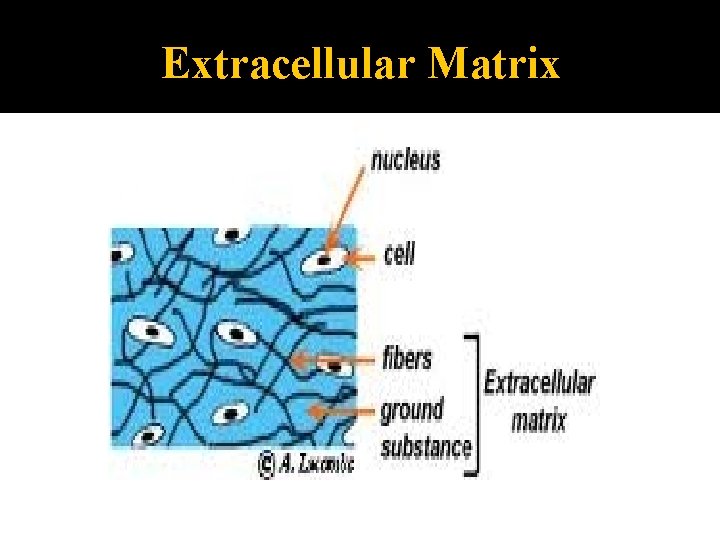
Extracellular Matrix � 2 main elements: 1. structureless ground substance water adhesive proteins (glues everything together) charged polysaccharides (trap water) control viscosity of the CT fibers 2. collagen: #1 protein in body elastic reticular
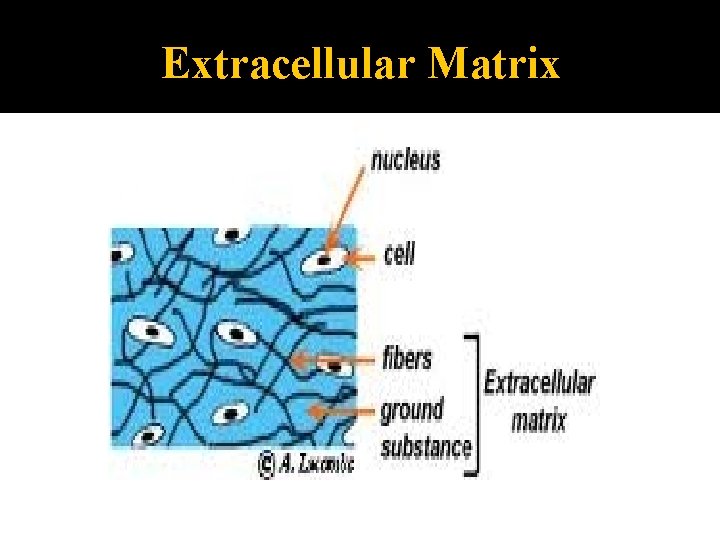
Extracellular Matrix
Connective Tissues Functions 1. 2. 3. 4. protection support binding substances together absorption of large amounts of water (ground substance)
Types of Connective Tissues 1. 2. 3. 4. 5. Bone Cartilage Dense CT Loose CT Blood
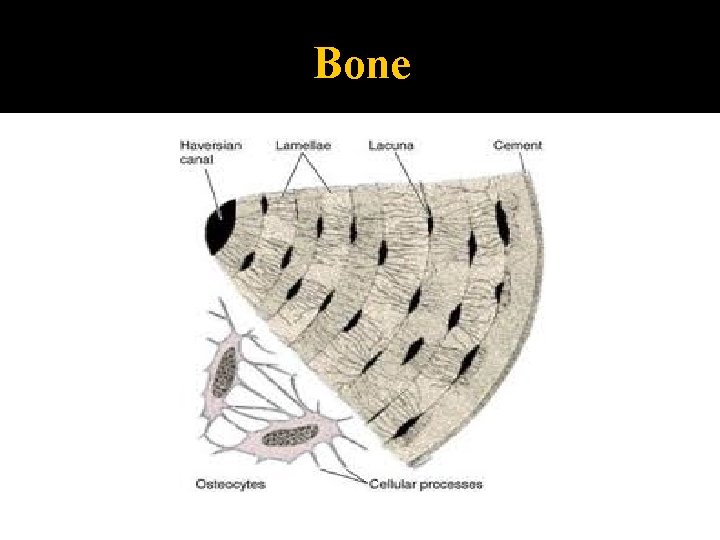
Bone �aka osseous tissue �few cells surrounded by hard matrix calcium salts �due to its hardness has exceptional ability to protect & support
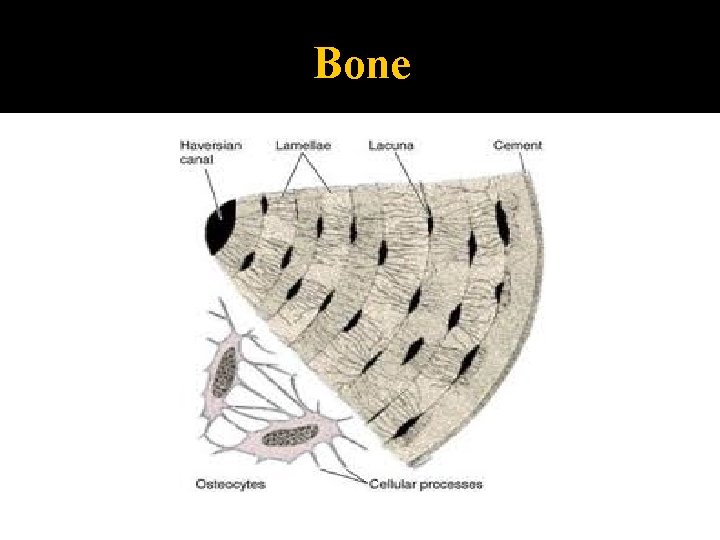
Bone
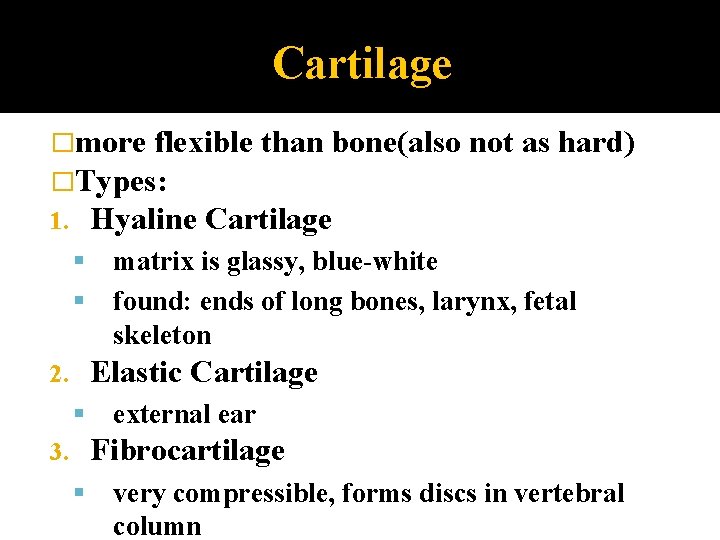
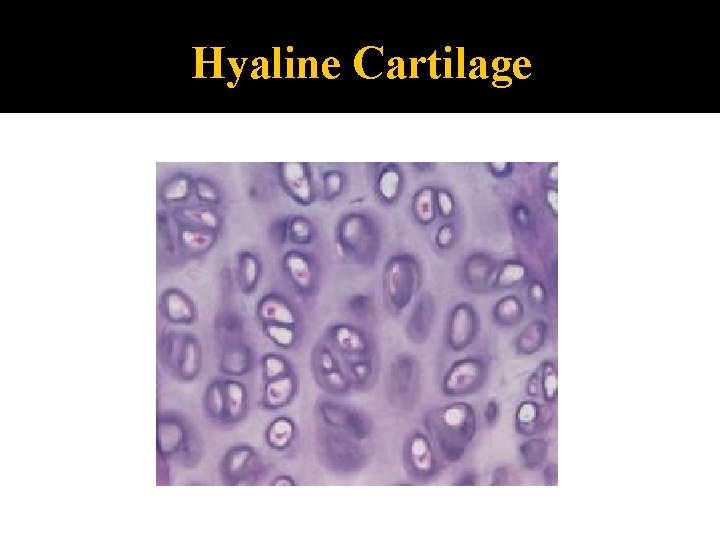
Cartilage �more flexible than bone(also �Types: 1. Hyaline Cartilage not as hard) matrix is glassy, blue-white found: ends of long bones, larynx, fetal skeleton Elastic Cartilage 2. external ear Fibrocartilage 3. very compressible, forms discs in vertebral column
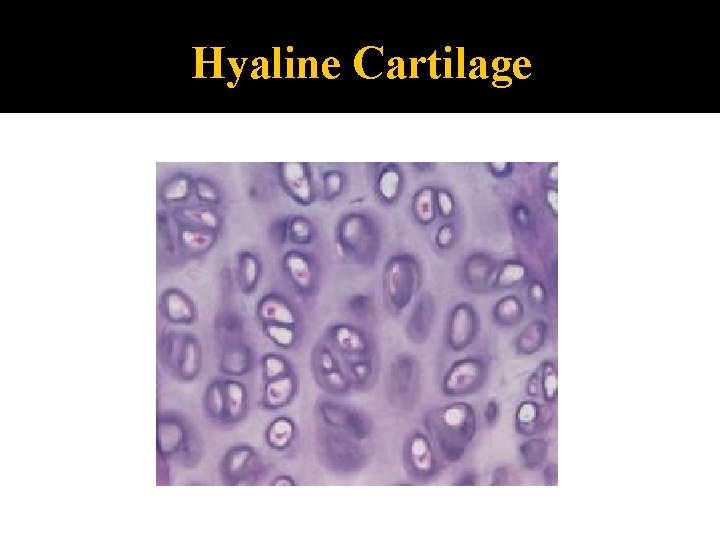
Hyaline Cartilage
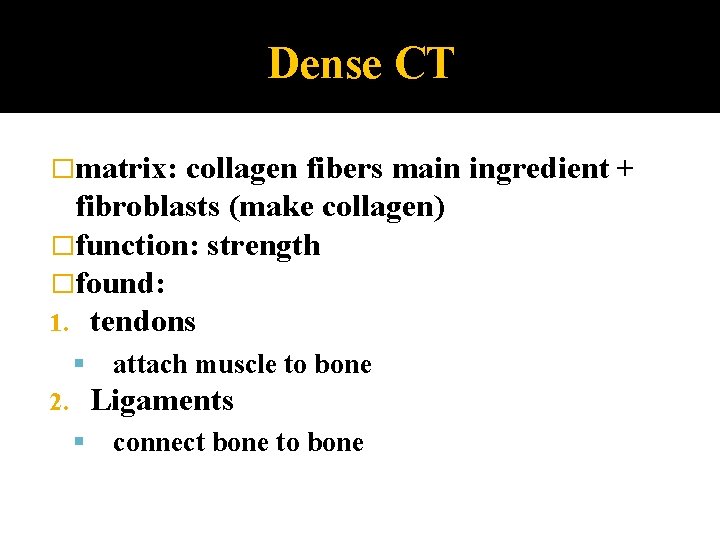
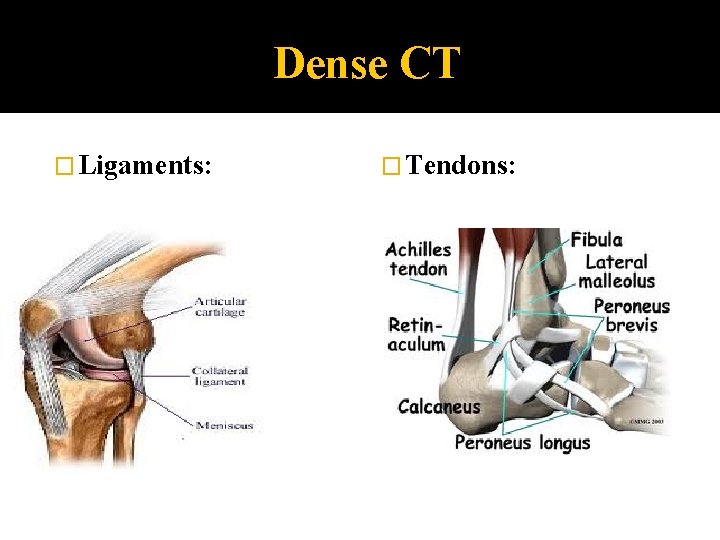
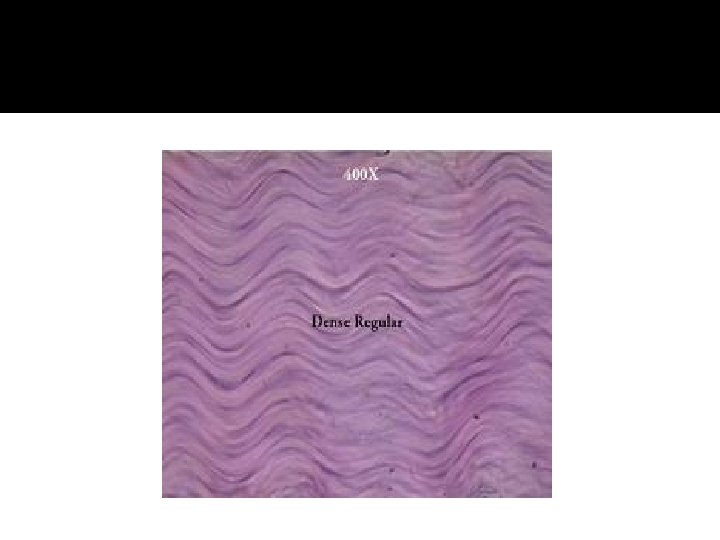
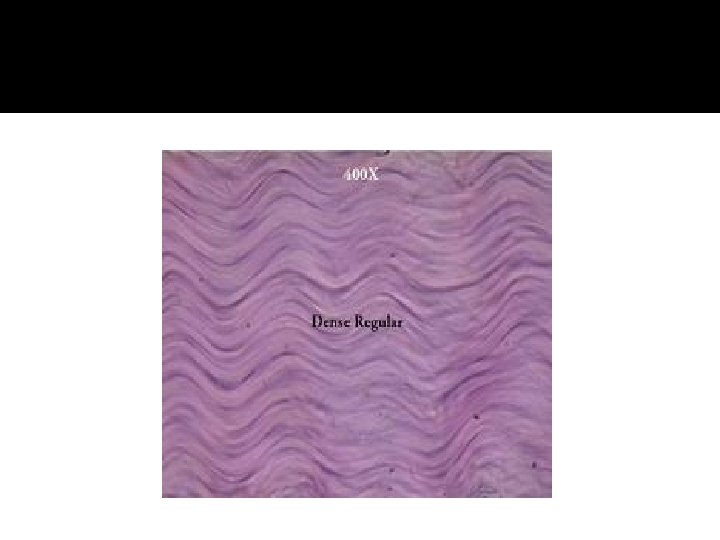
Dense CT �matrix: collagen fibers main ingredient + fibroblasts (make collagen) �function: strength �found: 1. tendons attach muscle to bone Ligaments 2. connect bone to bone
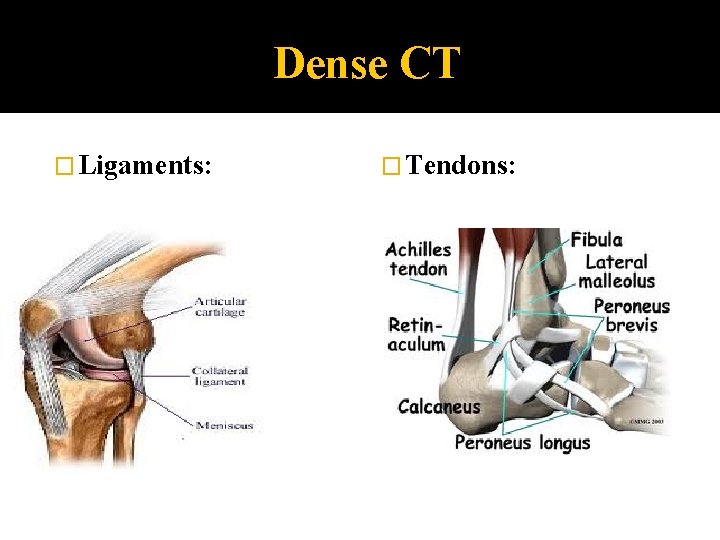
Dense CT � Ligaments: � Tendons:
Loose CT �softer, more cellular, fewer fibers than most other CT �Types: 1. Areolar CT 2. Adipose Tissue 3. Reticular CT
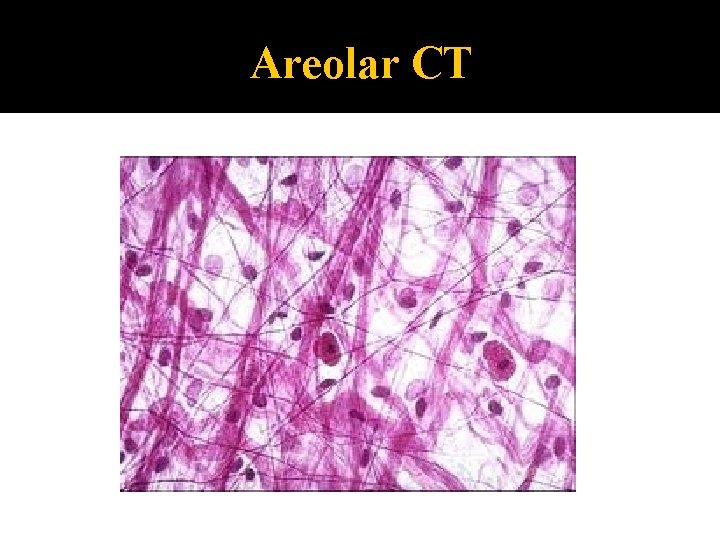
Areolar CT �“cobwebby” �diffusely distributed thru out body �layer under all mucous membranes (lamina propria) �Functions: 1. cushions & protects 2. holds things together 3. reservoir of water (where water held when injured area becomes edematous)
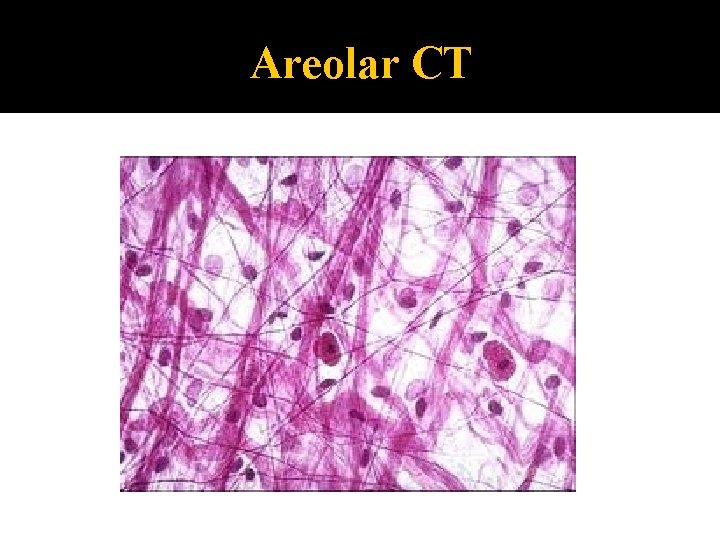
Areolar CT
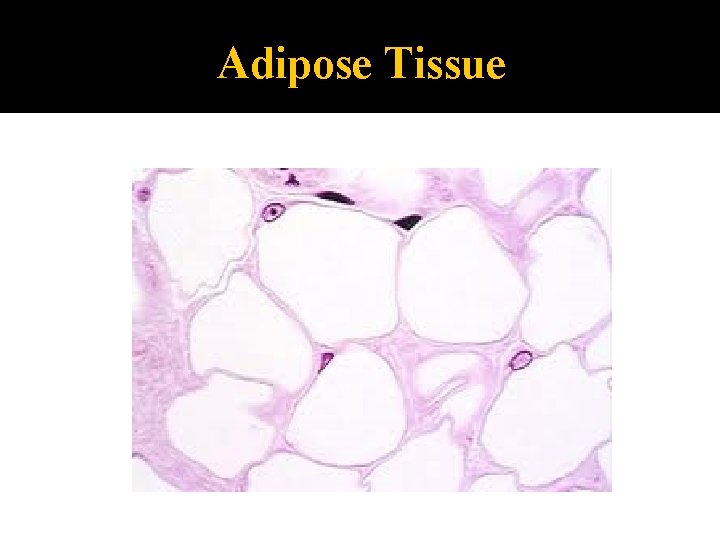
Adipose Tissue �aka fat �adipocytes =fat cells “signet ring” �found : subcutaneous layer beneath skin around kidneys, eyeballs
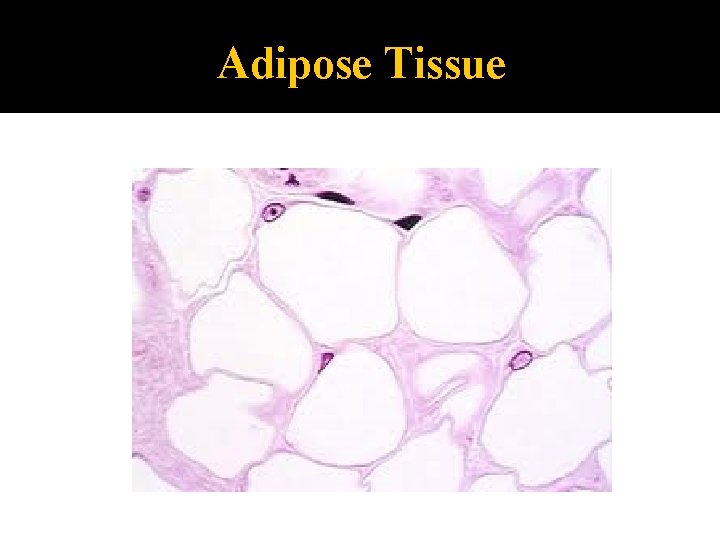
Adipose Tissue
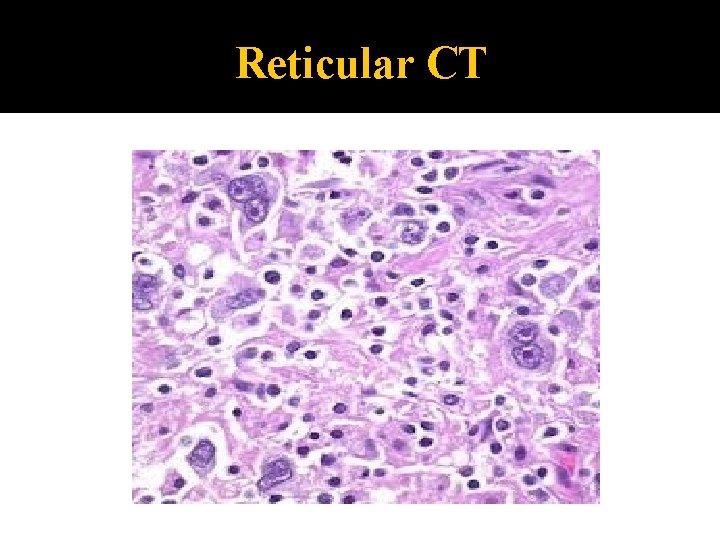
Reticular CT �reticular cells which make reticular fibers (finer than collagen) �forms: stroma: internal framework that supports ie. Stroma in lymph nodes support lymphocytes
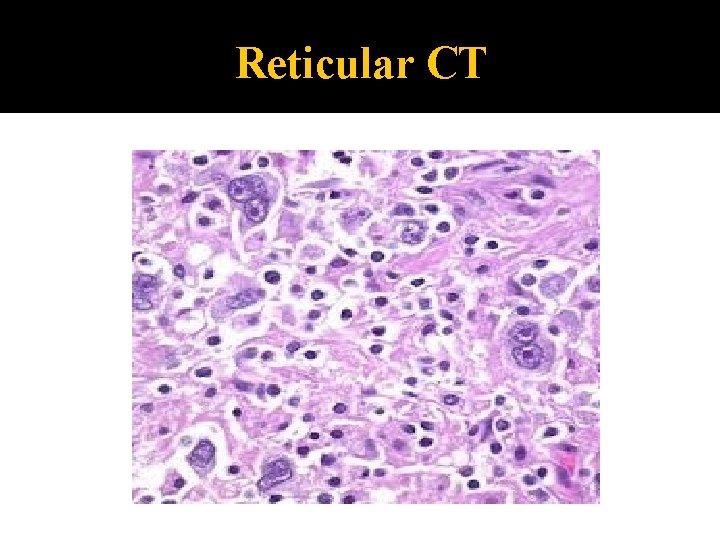
Reticular CT
Blood �blood cells �Function: in fluid matrix (plasma) carries nutrients, gases, wastes, hormones etc. to/from cells �Plasma: fibers: soluble proteins become visible during blood clotting
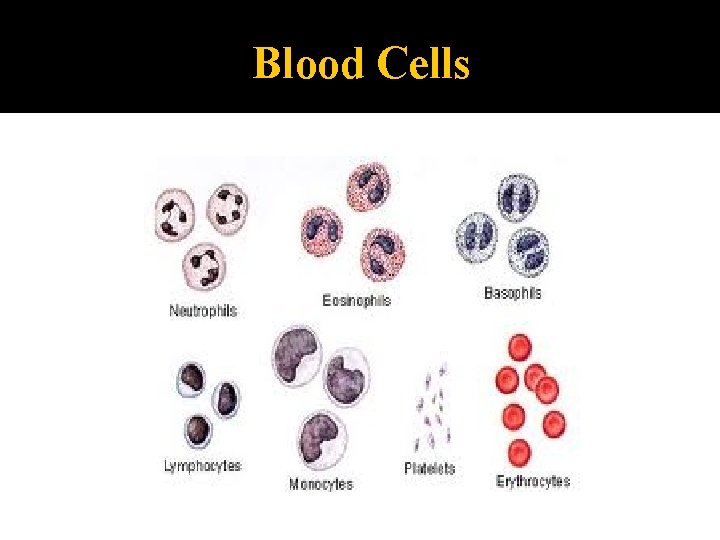
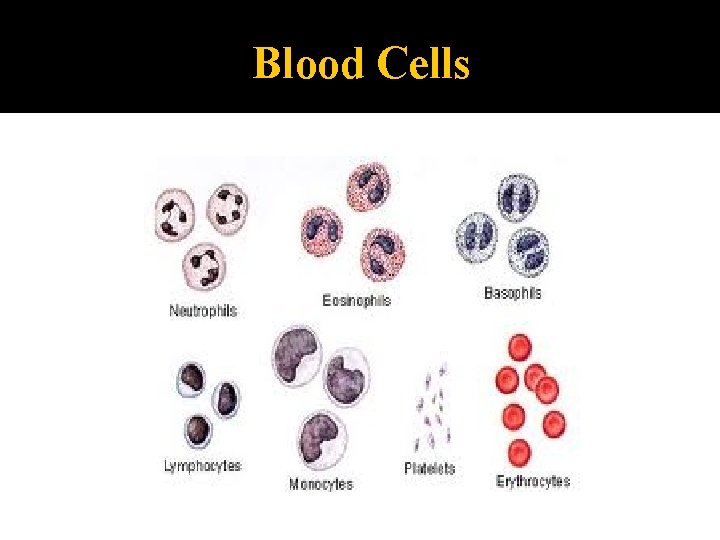
Blood Cells
Muscle Tissue �specialized to contract �cells called muscle fibers �Types: 1. Skeletal 2. Cardiac 3. Smooth produce motion
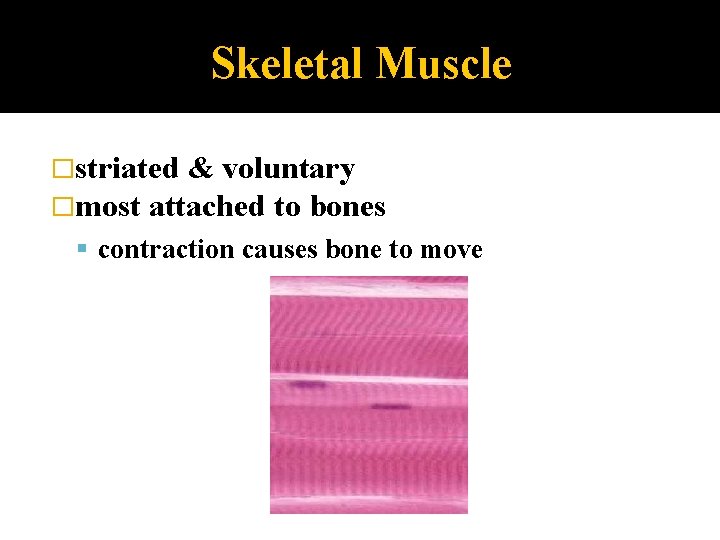
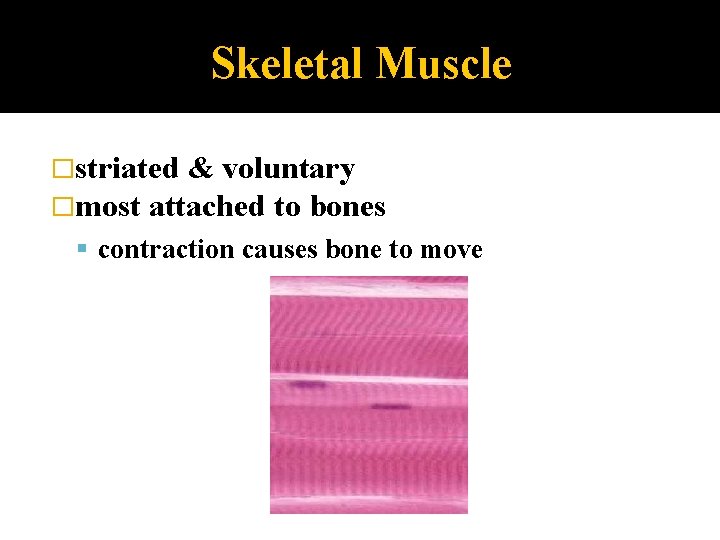
Skeletal Muscle �striated & voluntary �most attached to bones contraction causes bone to move
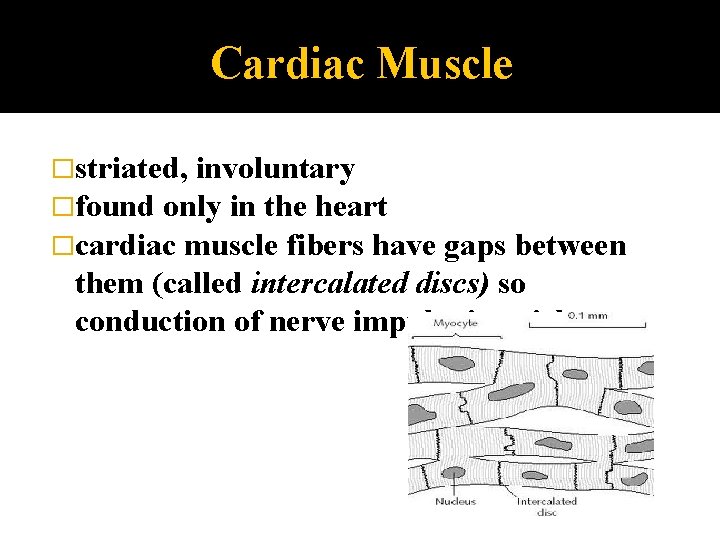
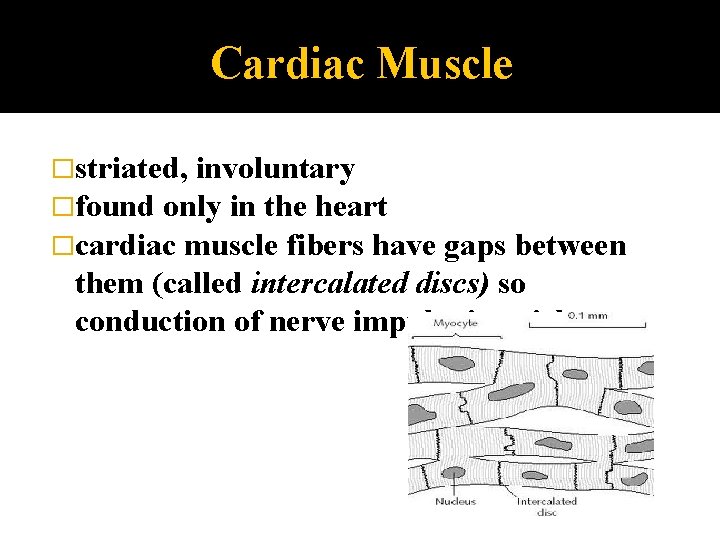
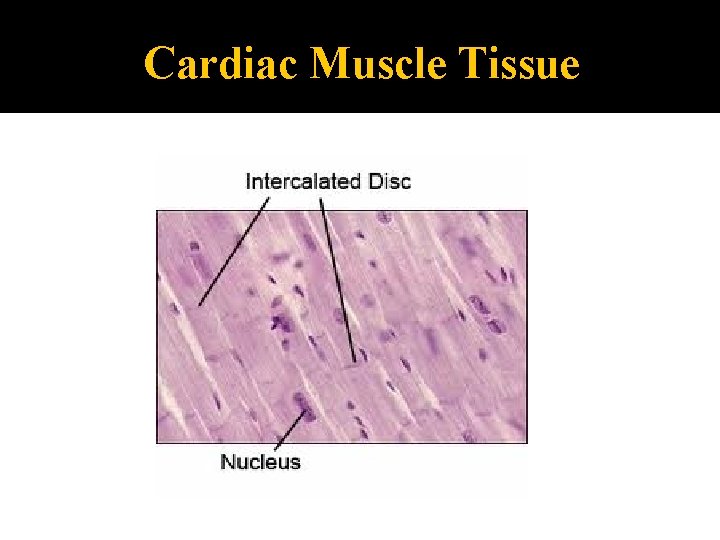
Cardiac Muscle �striated, involuntary �found only in the heart �cardiac muscle fibers have gaps between them (called intercalated discs) so conduction of nerve impulse is quicker
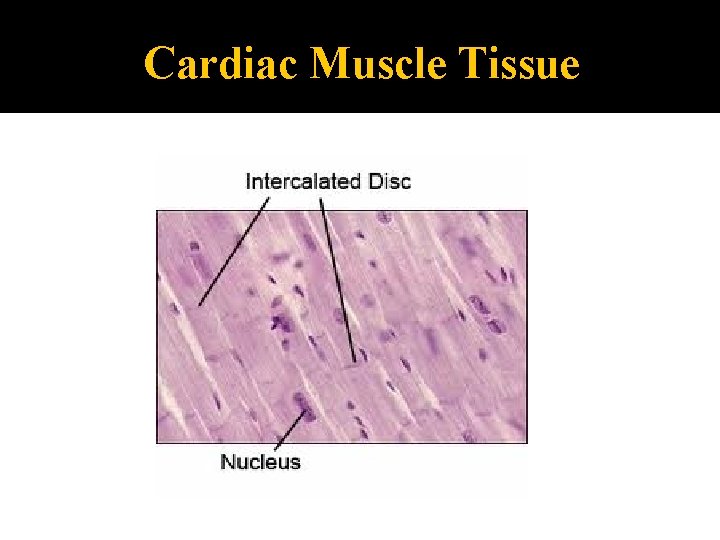
Cardiac Muscle Tissue
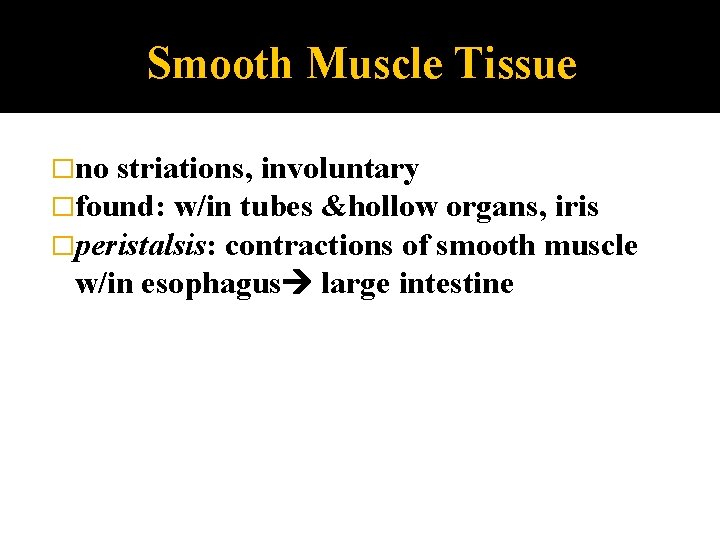
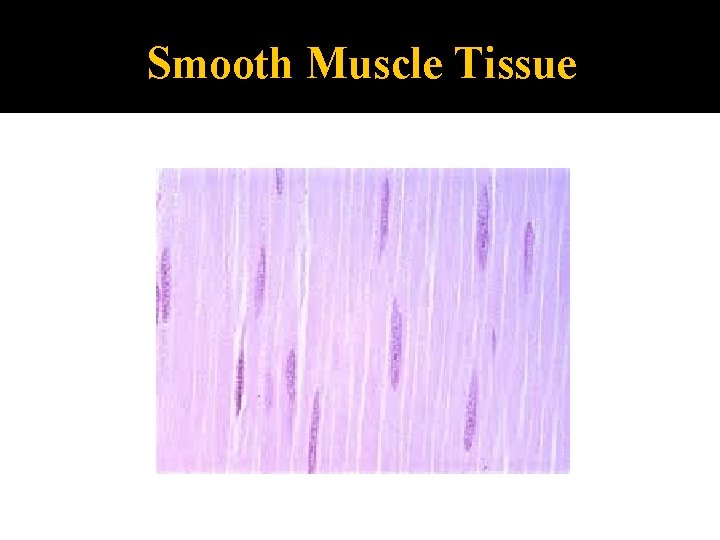
Smooth Muscle Tissue �no striations, involuntary �found: w/in tubes &hollow organs, iris �peristalsis: contractions of smooth muscle w/in esophagus large intestine
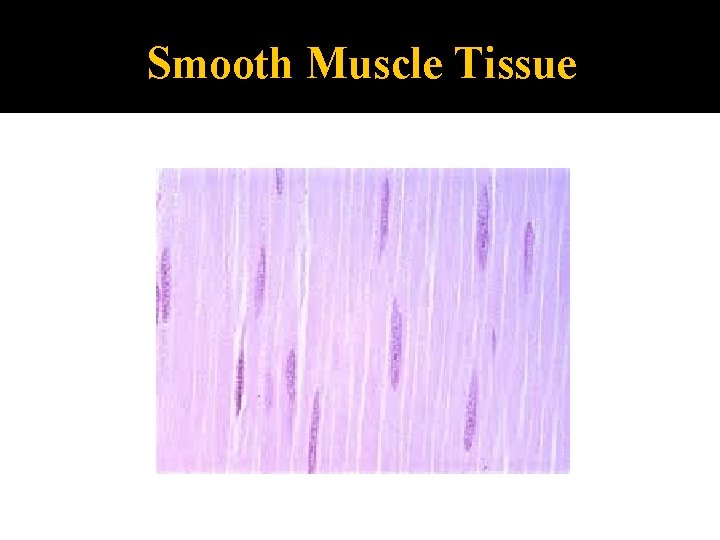
Smooth Muscle Tissue
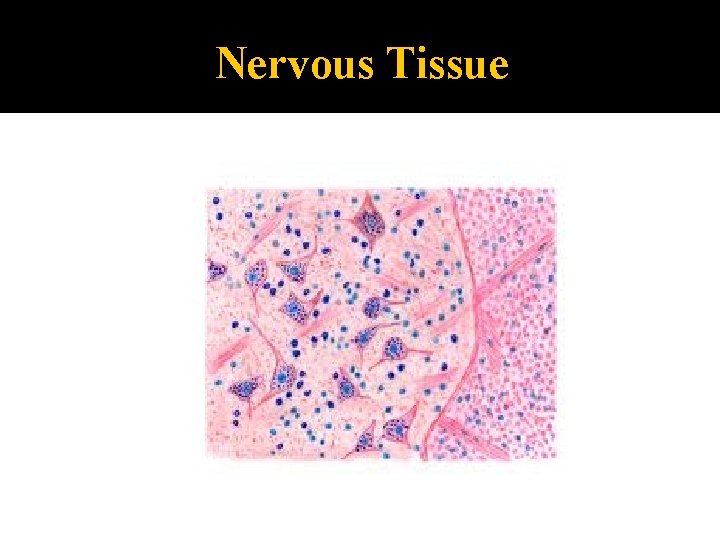
Nervous Tissue �found in brain, spinal cord, �nerve cells called neurons �irritability & conductivity nerves neurons receive & conduct nerve impulses
Neuroglia �cells that support neurons astrocytes oligodendrocytes ependymal cells microglia Schwann cells satellite cells
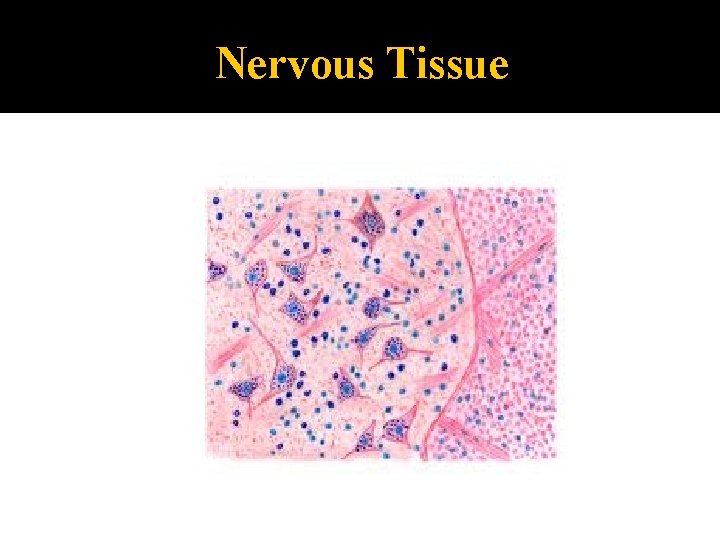
Nervous Tissue
Wound Healing �Inflammation: �nonspecific, generalized response aimed at preventing further injury �Immune Response: �specific response aimed at specific invader
Wound Healing Regeneration 1. replacement of destroyed tissue by same cells repair appears like normal tissue Fibrosis 2. repair by dense, fibrous CT ? Regeneration or Fibrosis? ▪ type of tissue ▪ severity of injury
3 Stages of Tissue Injury Leaky Capillaries clotting proteins enter injured area & form clot � bleeding stops & clot holds edges of wound together � clot protects injured area from contamination(infection, dirt) � clot dries scab 1. �
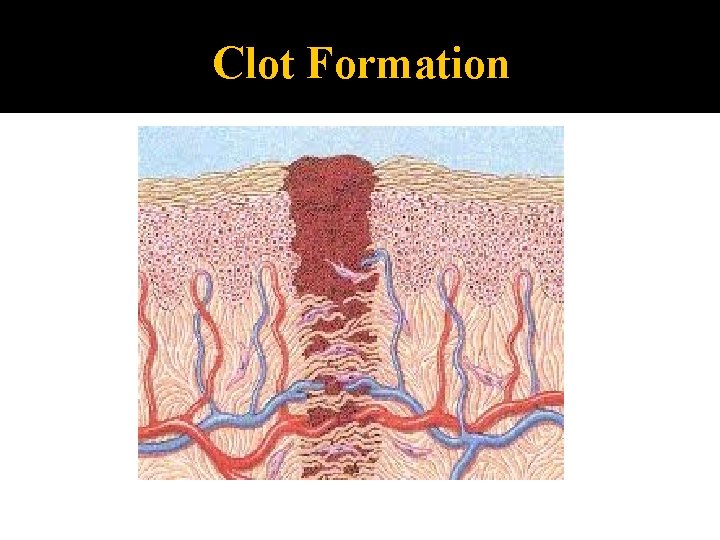
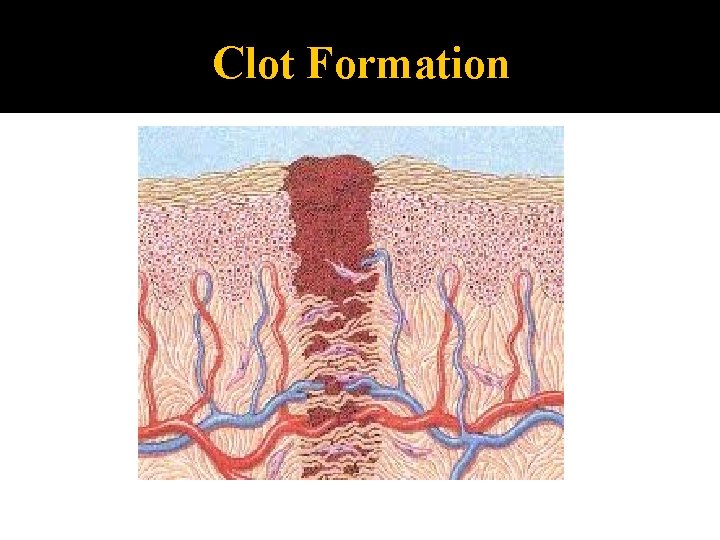
Clot Formation
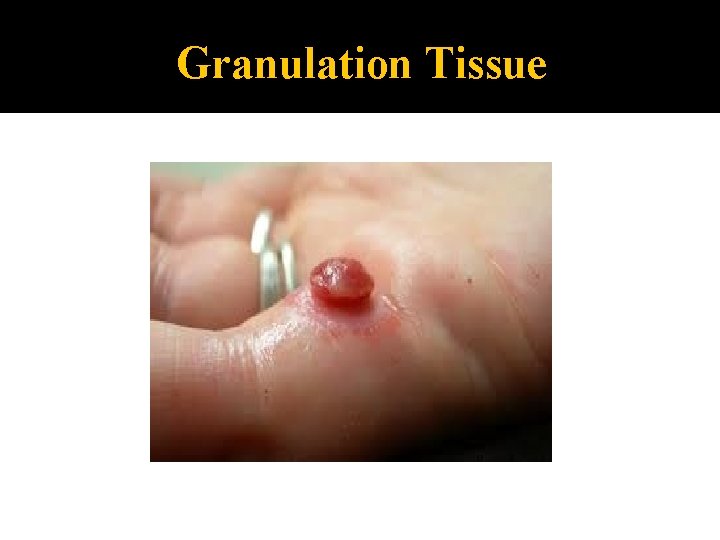
2. Granulation Tissue Forms �is a delicate pink tissue �mostly capillaries (friable) �contains phagocytes (eat up clot & fibroblasts that synthesize collagen which forms scar)
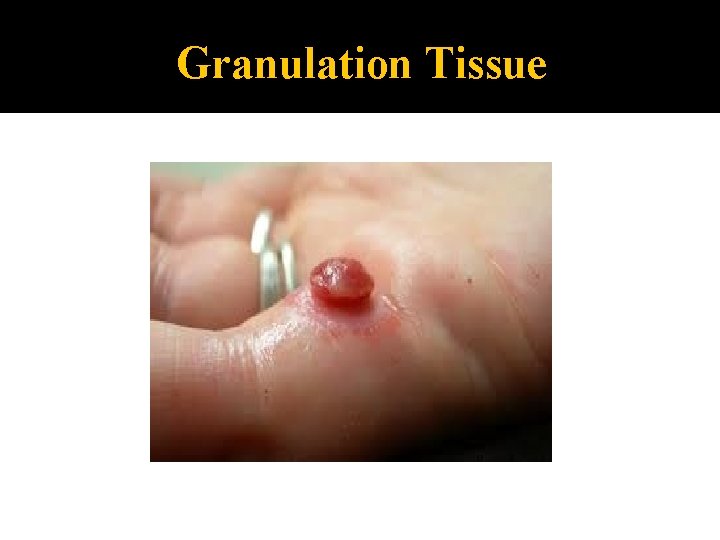
Granulation Tissue
3. Surface epithelium regenerates � grows from edges center �scar depends on depth & severity of wound
Regeneration varies by tissue type �Regeneration goes well in epithelial tissues and fibrous CT & bone �Muscle regenerates poorly �Nervous tissue replaced by scar tissue
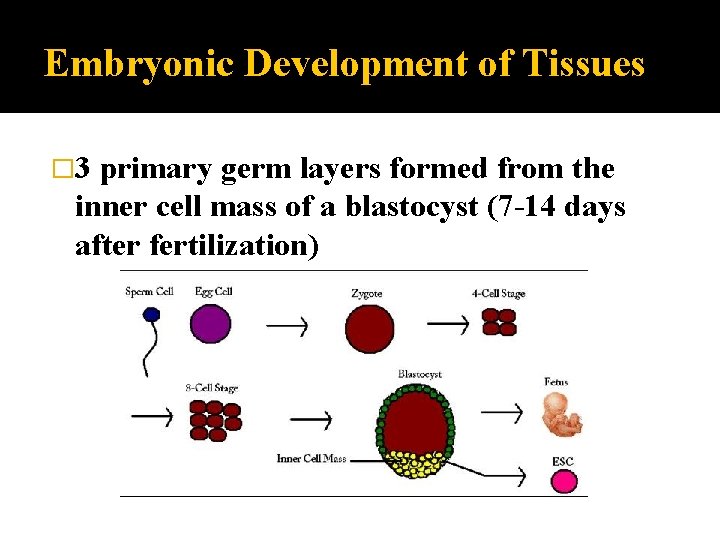
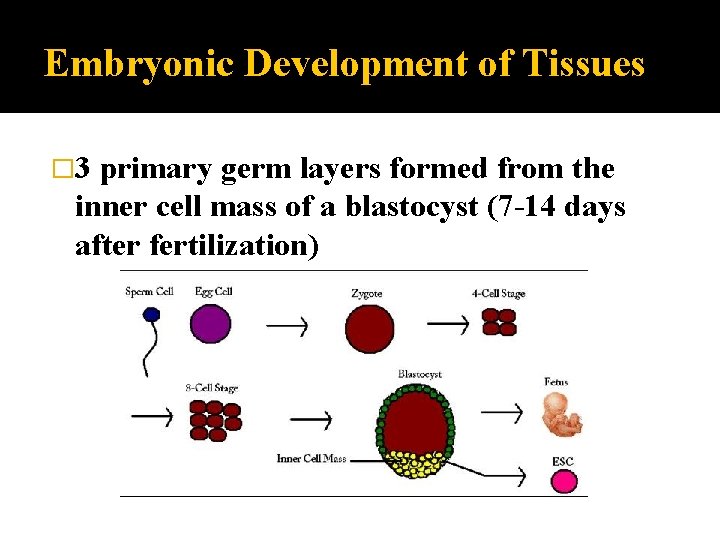
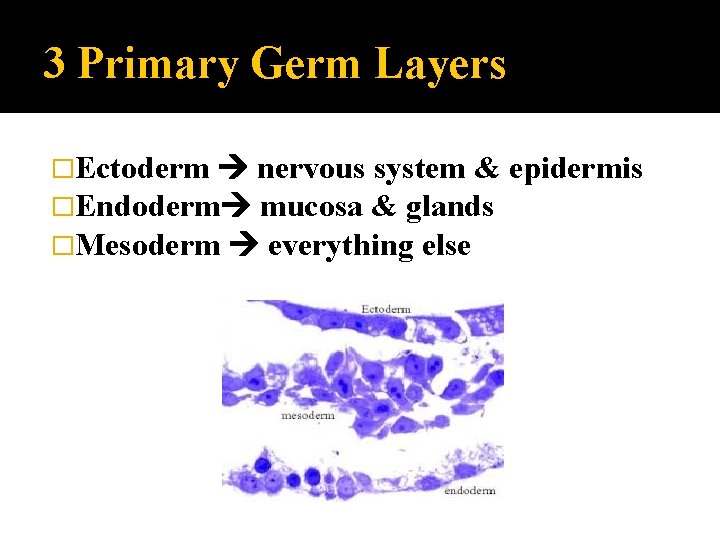
Embryonic Development of Tissues � 3 primary germ layers formed from the inner cell mass of a blastocyst (7 -14 days after fertilization)
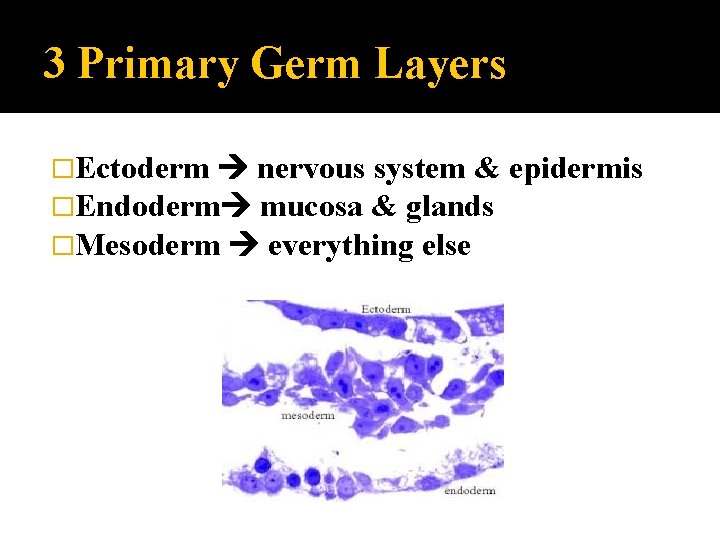
3 Primary Germ Layers �Ectoderm nervous system & �Endoderm mucosa & glands �Mesoderm everything else epidermis
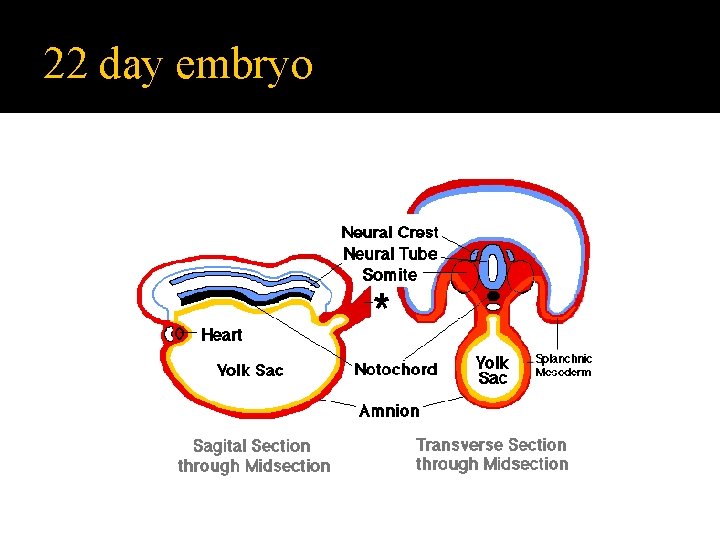
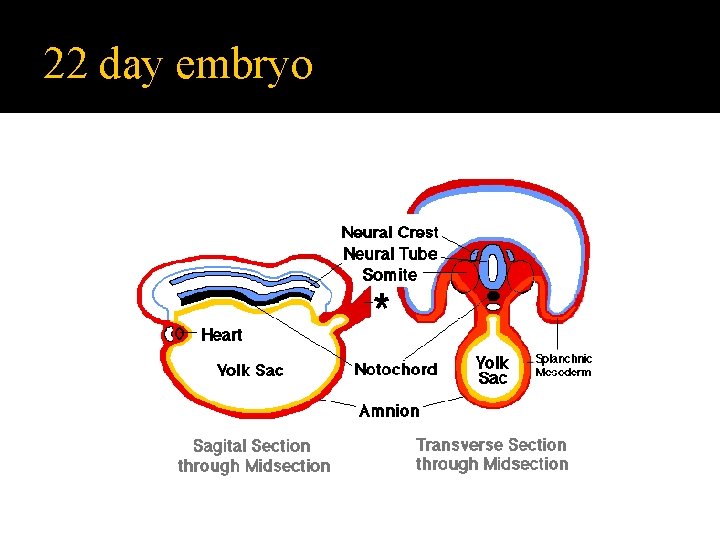
22 day embryo
Normal Aging Process �uncertain what causes aging process to start chemical or environmental insults aging “clock”
Tissue Changes with Aging �Epithelial: membranes thin, skin less elastic, glands secrete less �CT: bones porous, tissue repair slower �Muscle Tissue: muscles atrophy �Nervous Tissue: nervous tissue atrophies