Anatomy physiology of voiding URINARY BLADDER AND URETHRA
Anatomy & physiology of voiding
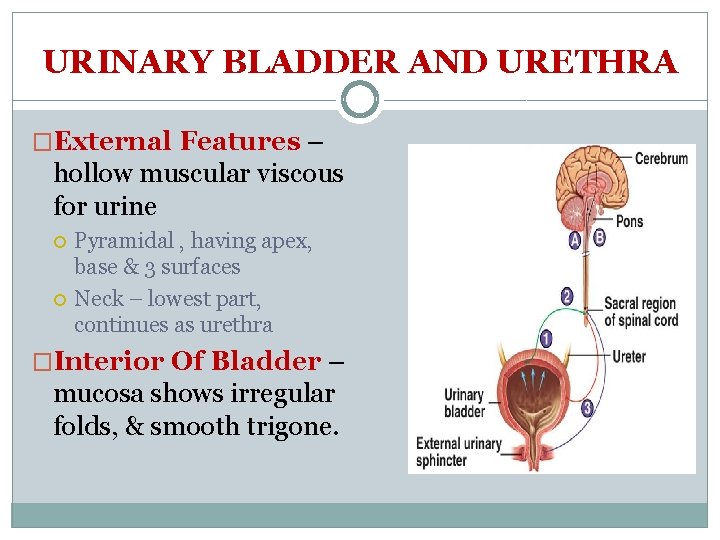
URINARY BLADDER AND URETHRA �External Features – hollow muscular viscous for urine Pyramidal , having apex, base & 3 surfaces Neck – lowest part, continues as urethra �Interior Of Bladder – mucosa shows irregular folds, & smooth trigone.
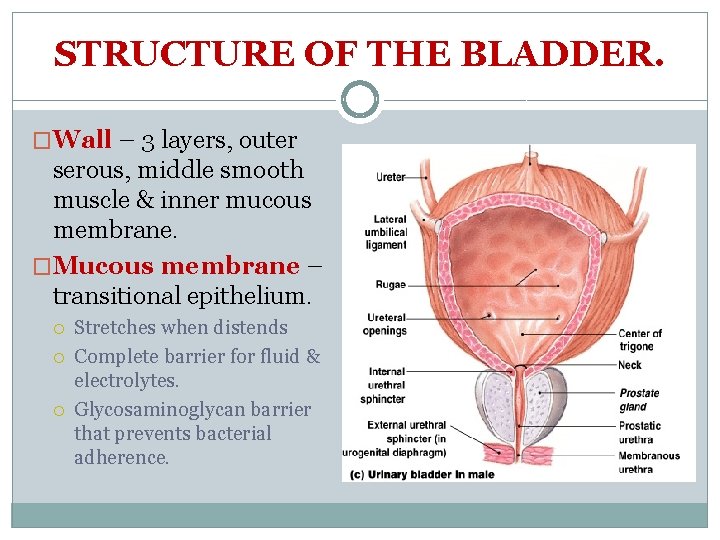
STRUCTURE OF THE BLADDER. �Wall – 3 layers, outer serous, middle smooth muscle & inner mucous membrane. �Mucous membrane – transitional epithelium. Stretches when distends Complete barrier for fluid & electrolytes. Glycosaminoglycan barrier that prevents bacterial adherence.
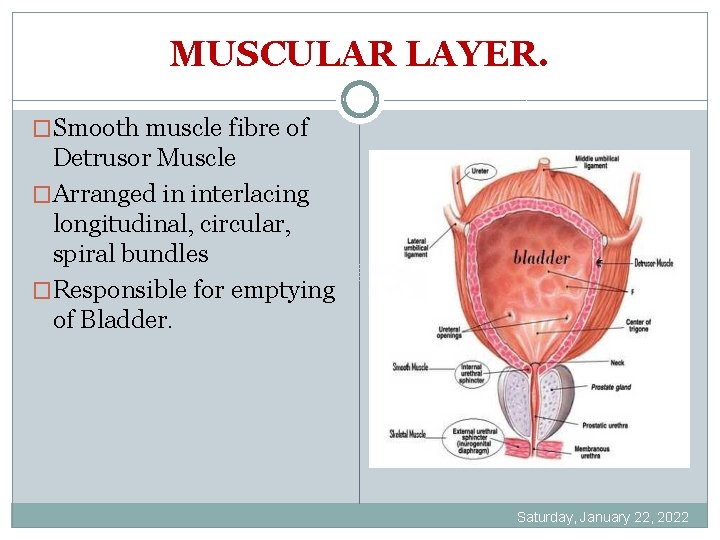
MUSCULAR LAYER. �Smooth muscle fibre of Detrusor Muscle �Arranged in interlacing longitudinal, circular, spiral bundles �Responsible for emptying of Bladder. Saturday, January 22, 2022
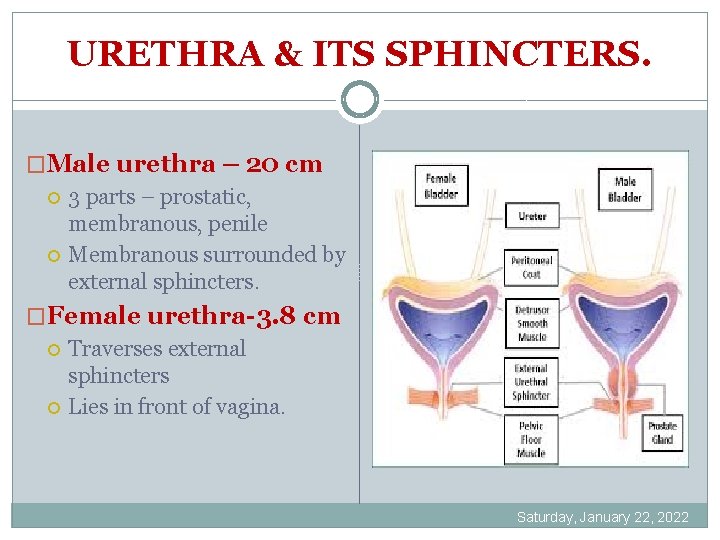
URETHRA & ITS SPHINCTERS. �Male urethra – 20 cm 3 parts – prostatic, membranous, penile Membranous surrounded by external sphincters. �Female urethra-3. 8 cm Traverses external sphincters Lies in front of vagina. Saturday, January 22, 2022
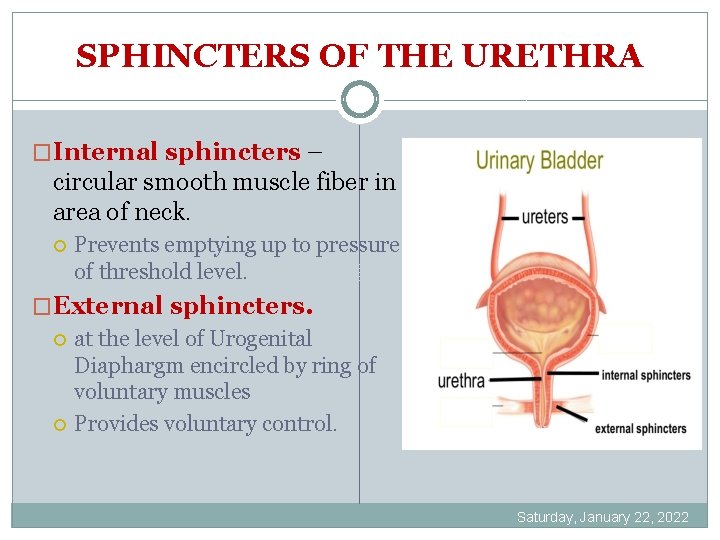
SPHINCTERS OF THE URETHRA �Internal sphincters – circular smooth muscle fiber in area of neck. Prevents emptying up to pressure of threshold level. �External sphincters. at the level of Urogenital Diaphargm encircled by ring of voluntary muscles Provides voluntary control. Saturday, January 22, 2022
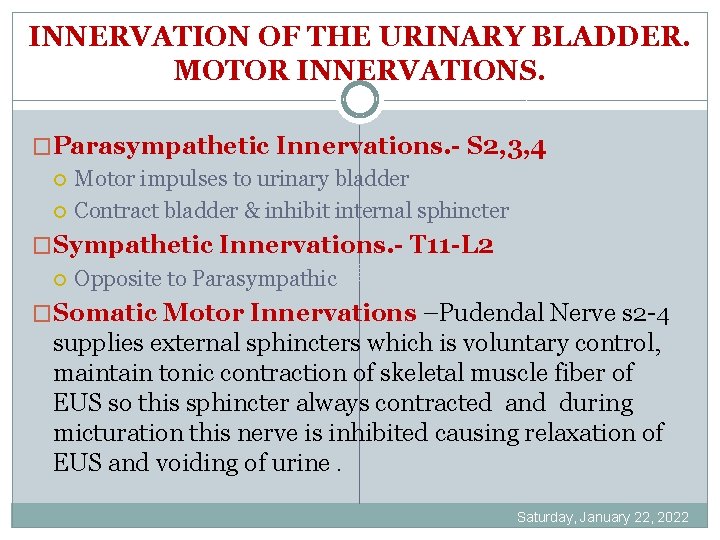
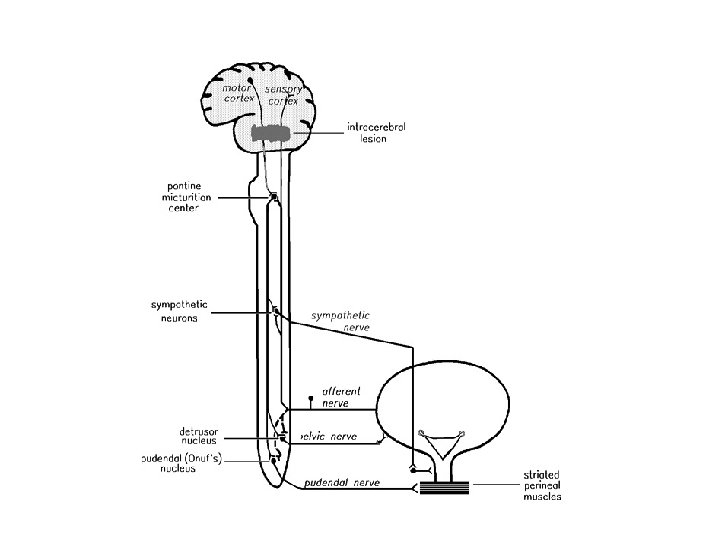
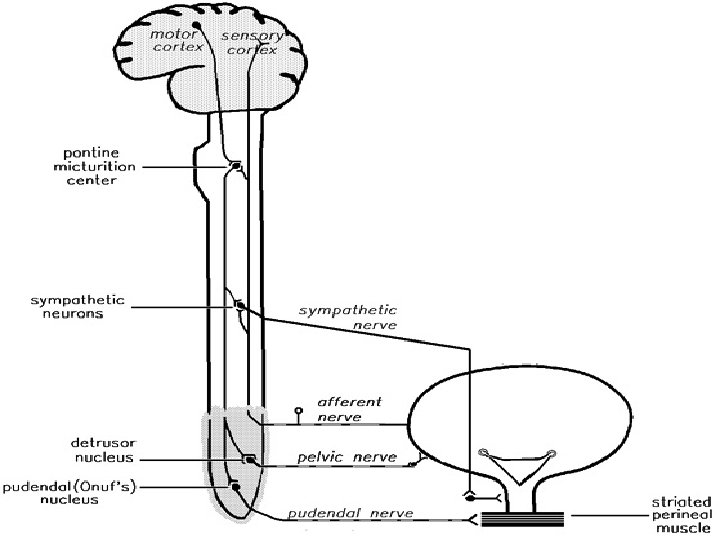
INNERVATION OF THE URINARY BLADDER. MOTOR INNERVATIONS. �Parasympathetic Innervations. - S 2, 3, 4 Motor impulses to urinary bladder Contract bladder & inhibit internal sphincter �Sympathetic Innervations. - T 11 -L 2 Opposite to Parasympathic �Somatic Motor Innervations –Pudendal Nerve s 2 -4 supplies external sphincters which is voluntary control, maintain tonic contraction of skeletal muscle fiber of EUS so this sphincter always contracted and during micturation this nerve is inhibited causing relaxation of EUS and voiding of urine. Saturday, January 22, 2022
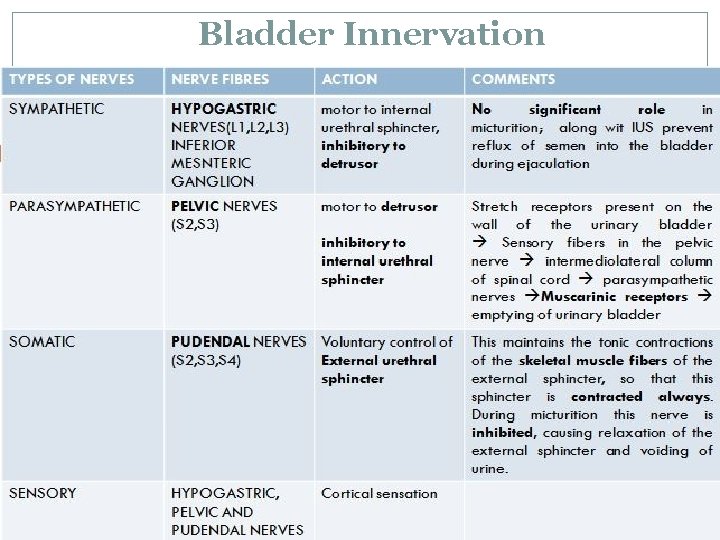
Bladder Innervation
Voiding � is a process by which urinary bladder empties when it becomes filled � Begins in 5 th month of intrauterine life 1. Filling phase - progressively till the tension of the wall rise above threshold 2. Voiding phase - Nervous reflex – micturition reflex that emptied the bladder or at least causes conscious desire of urination
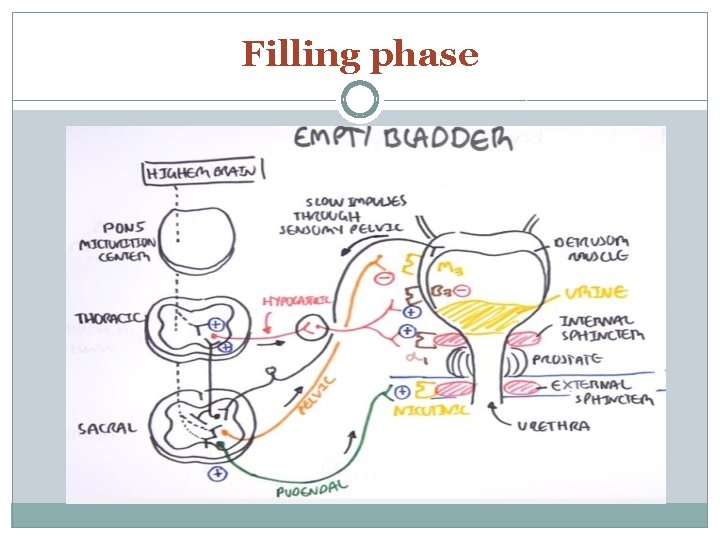
Filling phase
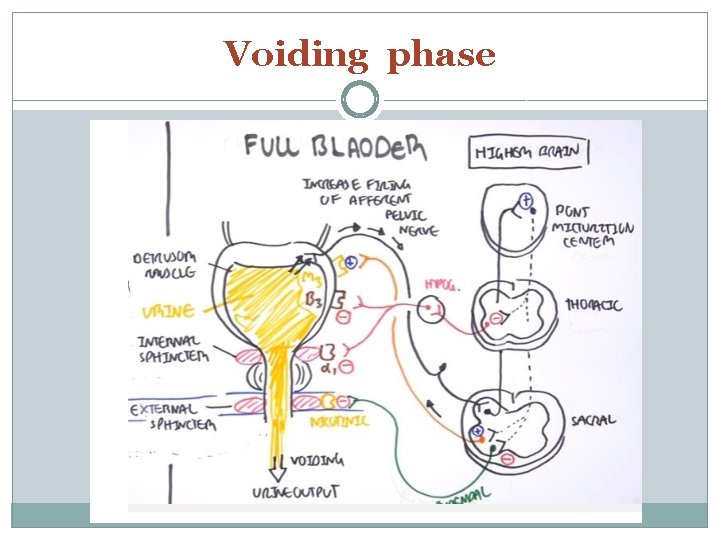
Voiding phase
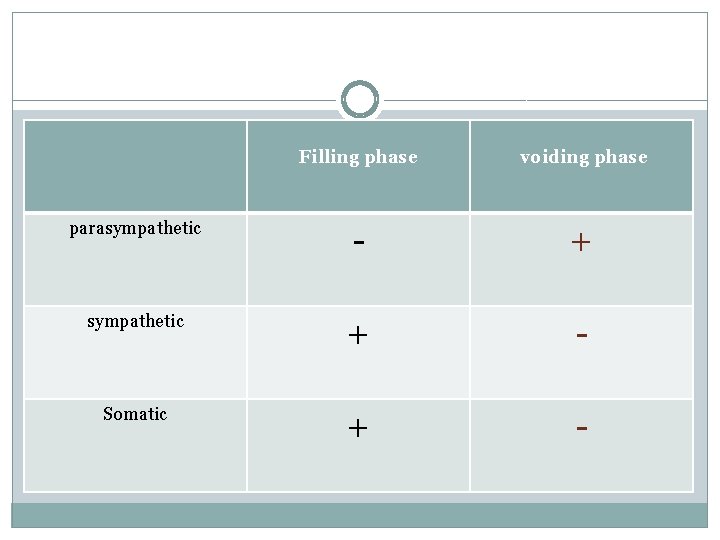
Filling phase voiding phase parasympathetic - + sympathetic + - Somatic + -
urinate phase: (Micturition Reflex) � micturition contractions are the result of a stretch reflex initiated by sensory stretch receptors in the bladder wall, � 250 -350 ml urine in bladder � Especially by the receptors in the posterior urethra when this area begins to fill with urine at the higher bladder pressures. � Sensory signals from the bladder stretch receptors are conducted to the sacral segments of the cord through the pelvic nerves � and then reflexively back again to the bladder through the parasympathetic nerve fibers by way of these same nerves.
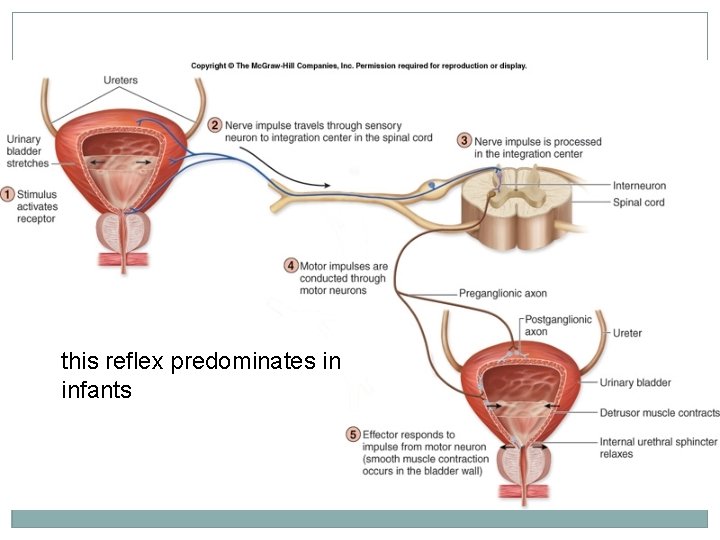
this reflex predominates in infants

Facilitation or inhibition of micturition by brain • Pons – Facilitatory and inhibitory centers • Cortex – Mainly inhibitory centers Voluntary Urination
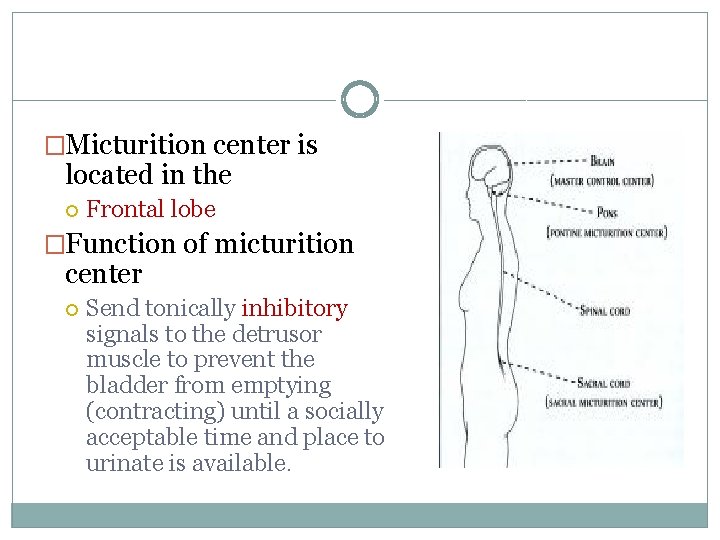
�Micturition center is located in the Frontal lobe �Function of micturition center Send tonically inhibitory signals to the detrusor muscle to prevent the bladder from emptying (contracting) until a socially acceptable time and place to urinate is available.
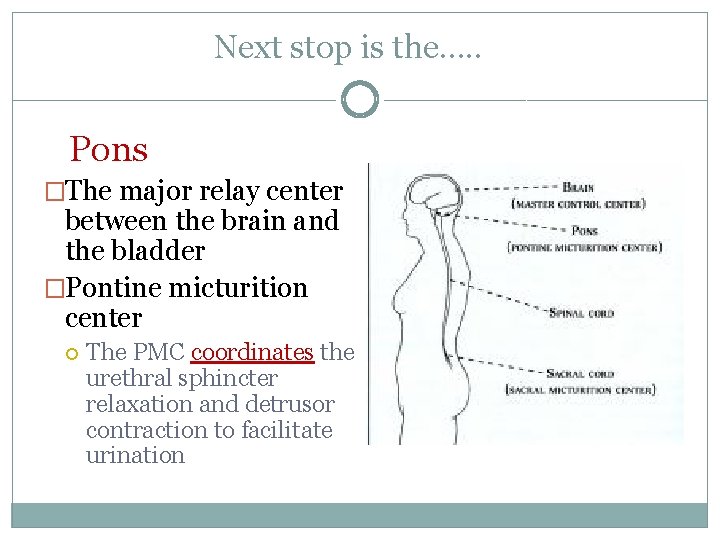
Next stop is the…. . Pons �The major relay center between the brain and the bladder �Pontine micturition center The PMC coordinates the urethral sphincter relaxation and detrusor contraction to facilitate urination
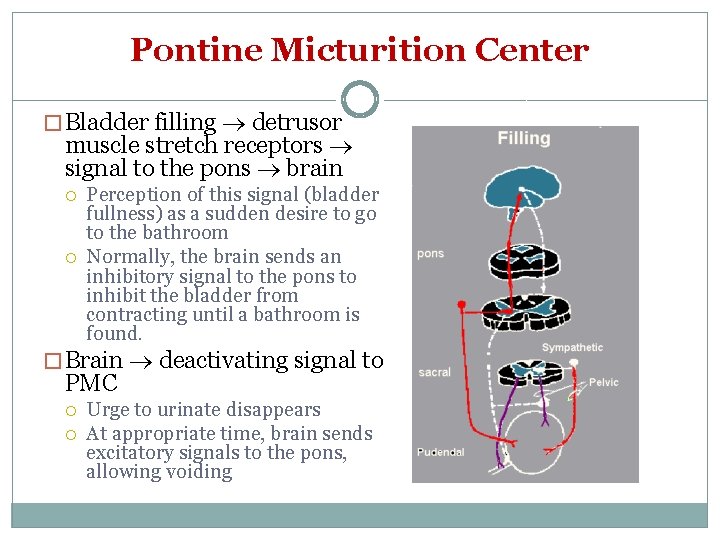
Pontine Micturition Center � Bladder filling detrusor muscle stretch receptors signal to the pons brain Perception of this signal (bladder fullness) as a sudden desire to go to the bathroom Normally, the brain sends an inhibitory signal to the pons to inhibit the bladder from contracting until a bathroom is found. � Brain deactivating signal to PMC Urge to urinate disappears At appropriate time, brain sends excitatory signals to the pons, allowing voiding
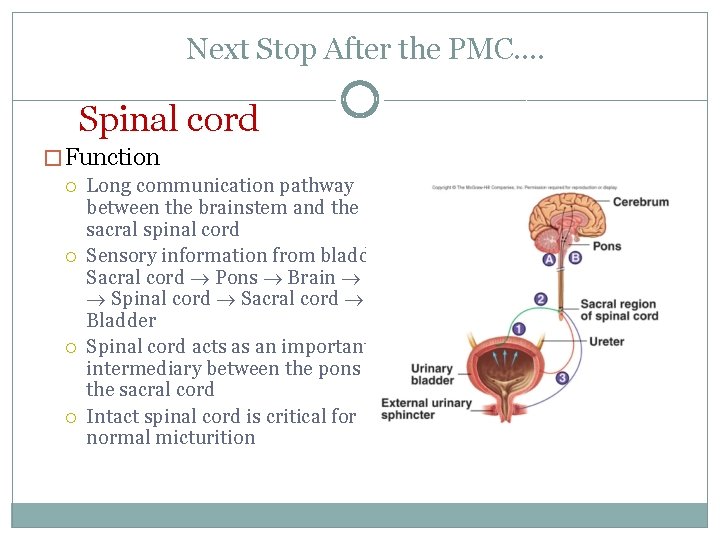
Next Stop After the PMC…. Spinal cord � Function Long communication pathway between the brainstem and the sacral spinal cord Sensory information from bladder Sacral cord Pons Brain Pons Spinal cord Sacral cord Bladder Spinal cord acts as an important intermediary between the pons and the sacral cord Intact spinal cord is critical for normal micturition
Neurogenuc bladder Joman Awwad
Diffenetion: • A malfunctioning urinary bladder due to neurologic dysfunction or insult emanating from internal or external trauma, disease, or injury.
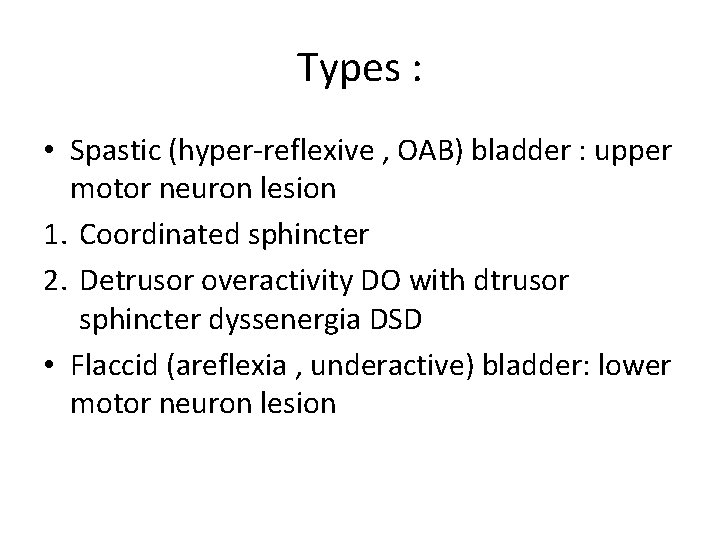
Types : • Spastic (hyper-reflexive , OAB) bladder : upper motor neuron lesion 1. Coordinated sphincter 2. Detrusor overactivity DO with dtrusor sphincter dyssenergia DSD • Flaccid (areflexia , underactive) bladder: lower motor neuron lesion
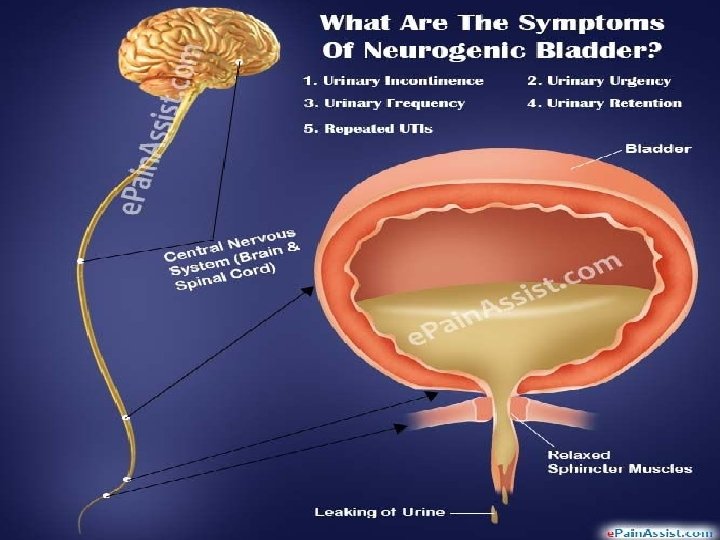
Symptoms:
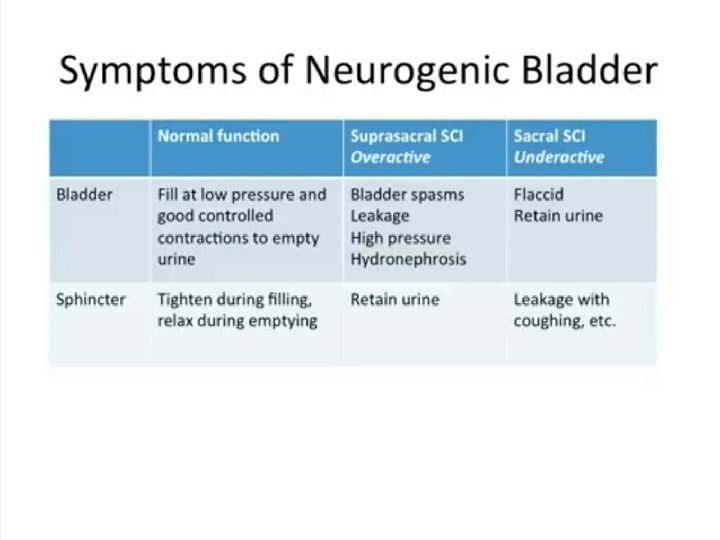
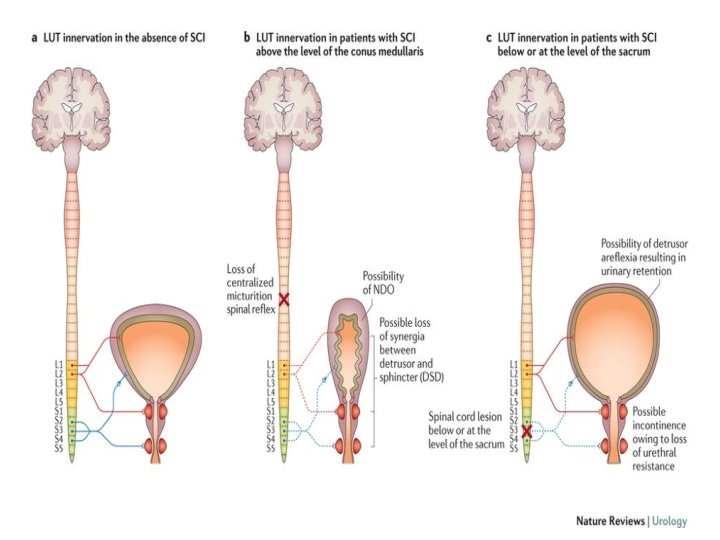
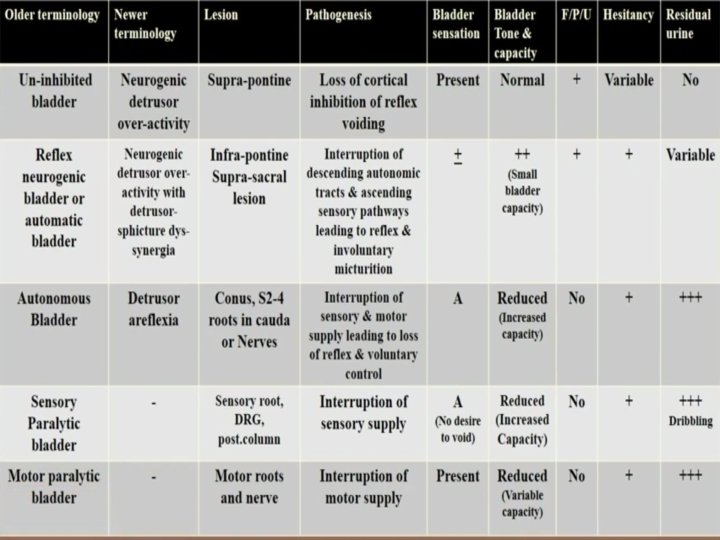
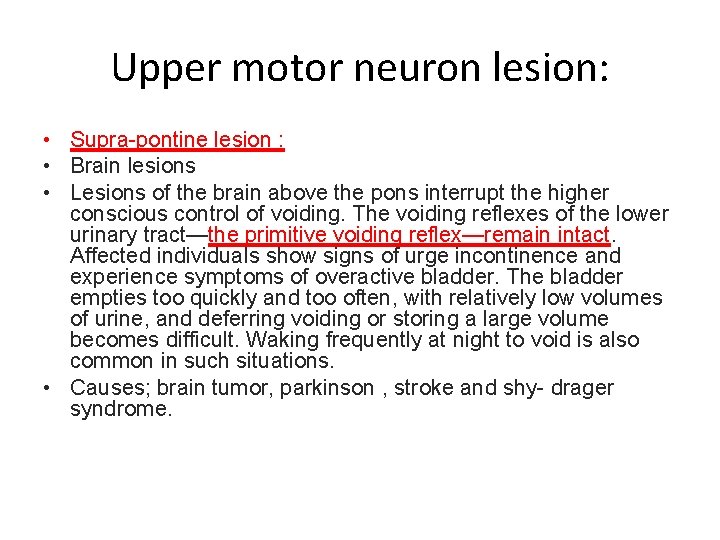
Upper motor neuron lesion: • Supra-pontine lesion : • Brain lesions • Lesions of the brain above the pons interrupt the higher conscious control of voiding. The voiding reflexes of the lower urinary tract—the primitive voiding reflex—remain intact. Affected individuals show signs of urge incontinence and experience symptoms of overactive bladder. The bladder empties too quickly and too often, with relatively low volumes of urine, and deferring voiding or storing a large volume becomes difficult. Waking frequently at night to void is also common in such situations. • Causes; brain tumor, parkinson , stroke and shy- drager syndrome.
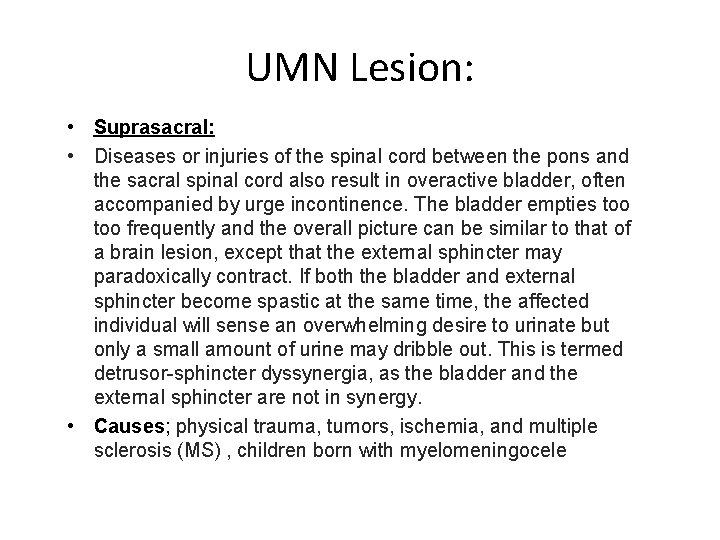
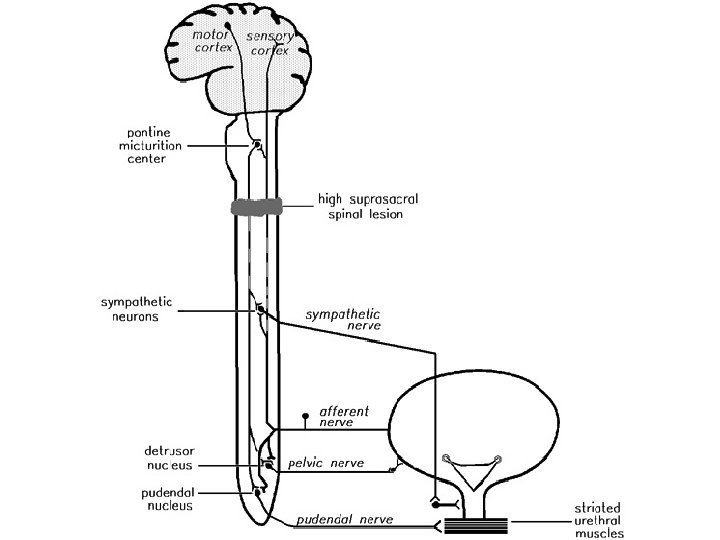
UMN Lesion: • Suprasacral: • Diseases or injuries of the spinal cord between the pons and the sacral spinal cord also result in overactive bladder, often accompanied by urge incontinence. The bladder empties too frequently and the overall picture can be similar to that of a brain lesion, except that the external sphincter may paradoxically contract. If both the bladder and external sphincter become spastic at the same time, the affected individual will sense an overwhelming desire to urinate but only a small amount of urine may dribble out. This is termed detrusor-sphincter dyssynergia, as the bladder and the external sphincter are not in synergy. • Causes; physical trauma, tumors, ischemia, and multiple sclerosis (MS) , children born with myelomeningocele
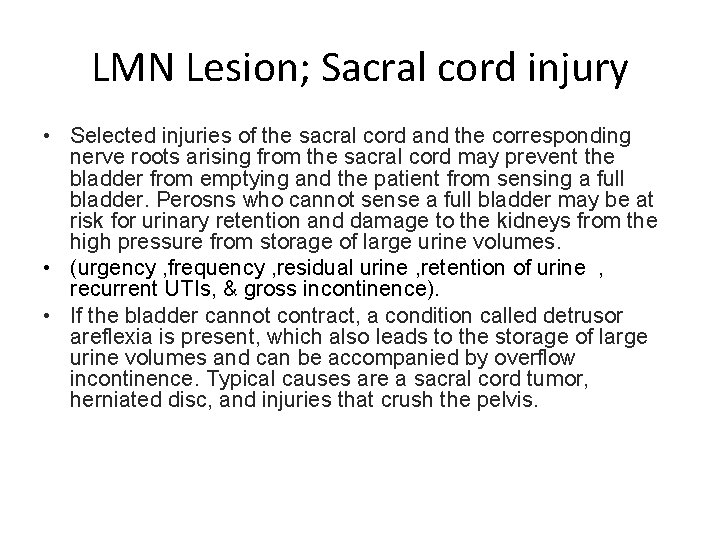
LMN Lesion; Sacral cord injury • Selected injuries of the sacral cord and the corresponding nerve roots arising from the sacral cord may prevent the bladder from emptying and the patient from sensing a full bladder. Perosns who cannot sense a full bladder may be at risk for urinary retention and damage to the kidneys from the high pressure from storage of large urine volumes. • (urgency , frequency , residual urine , retention of urine , recurrent UTIs, & gross incontinence). • If the bladder cannot contract, a condition called detrusor areflexia is present, which also leads to the storage of large urine volumes and can be accompanied by overflow incontinence. Typical causes are a sacral cord tumor, herniated disc, and injuries that crush the pelvis.
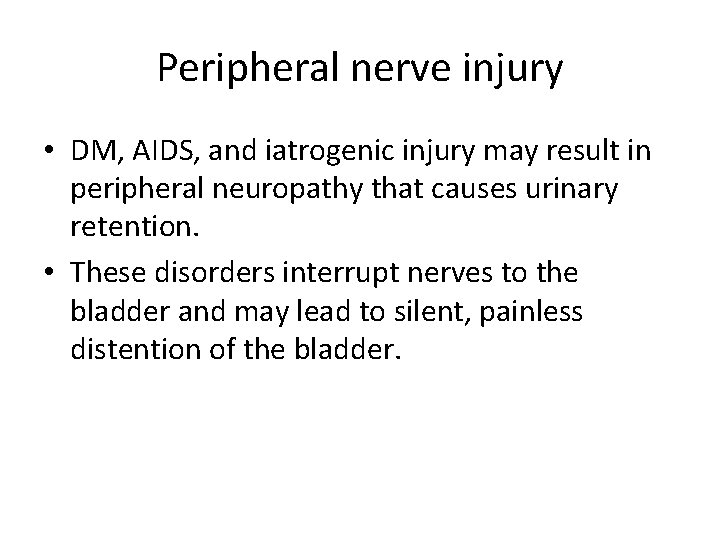
Peripheral nerve injury • DM, AIDS, and iatrogenic injury may result in peripheral neuropathy that causes urinary retention. • These disorders interrupt nerves to the bladder and may lead to silent, painless distention of the bladder.

SPINAL SHOCK • Immediately following severe injury to the spinal cord or conus medullaris, regardless of level, there is a stage of flaccid paralysis, with numbness below the level of the injury and the anal and bulbocavernous reflex is absent. • During this time the urinary bladder will be in retention- detrusor areflexia. • The smooth muscle of the detrusor and rectum is affected. The result is detrusor overfilling to the point of overflow incontinence and rectal impaction. • Spinal shock may last from 6 -12 weeks • Management: - Indwelling foley catheter or clean intermittent catheterization. Dr
How to differentiate between UMN vs LMN? • History. • Bulbocavernous reflex : The test involves monitoring anal sphincter contraction in response to squeezing the glans penis or tugging on an indwelling Foley catheter. The reflex is spinal mediated and involves S 2 -S 4.
Diagnosis • History • Physical examination 1. Flank tenderness: pyelonehritis 2. Abdominal mass: distended bladder, urinary retention 3. Innervation of external urethral sphincter which shares the same sacral root as anal sphincter can be tested by assesing: perineal sensation The anal wink reflex s 4 -s 5 Bulbocavernous reflex. • Lab investigations; 1. Urinalysis and urine culture 2. Urine cytology 3. Renal function test • Urodynamic studies
Urodynamic studies �Urodynamics; is a study that assesses how the bladder and urethra are performing their job of storing and releasing urine. �Used to asses the following conditions: �Incontinence �Urgency �Frequency �Dysurea �Recurrent urinary tract infection �Hesitancy �Incomplete evacuation
Urodynamic tests include: • • uroflowmetry postvoid residual measurement cystometric test leak point pressure measurement pressure flow study electromyography video urodynamic tests Dr
Management • When to refer to urologist? 1. Current bladder management is not effective 2. >3 UTIs per year 3. Kidney or bladder stone 4. Urethral complication 5. Worsening symptoms 6. Hydronephrosis on US
Goals of bladder management • Achieve regular bladder empyting • Avoid high filling and voiding pressure and preserve kidney function • Maintain continence and avoid symptoms of frequency and urgency • Prevent and treat complications like UTIs.
Spastic bladder management: • • • Bladder training : Kegel exercise Delayed urination Scheduled bathroom trip Anti-chloinergics Botulinum toxin injection Neuromodulation Surgery : to increase bladder capacity. Dr
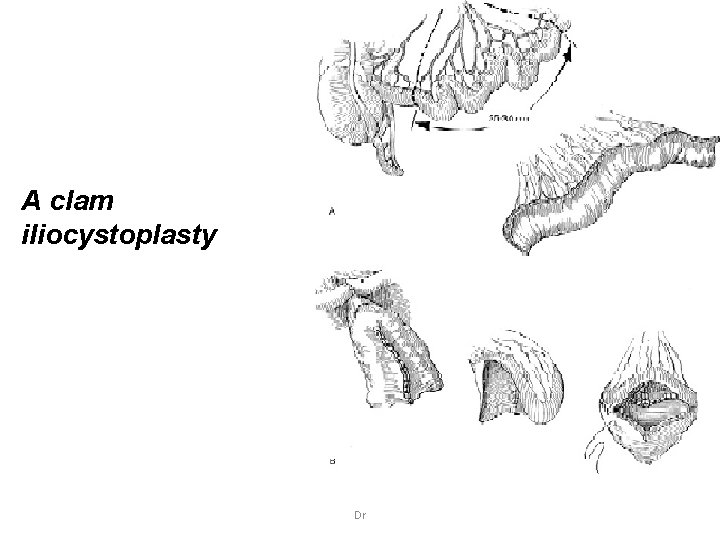
A clam iliocystoplasty Dr
Flaccid Neuropathic Bladder: 1)Valsalva and Crede maneuver(suprapubic pressure). 2)Intermittent catheterization: This technique eliminates residual urine, helps prevent infection, avoids incontinence, and protects against damage to the upper urinary tract. 3)Surgery: Transurethral resection is indicated for hypertrophy of the bladder neck or an enlarged prostate, either of which may cause obstruction of the bladder outlet and retention of residual urine. 4)Parasympathomimetic. Dr
• Treatment of overactive sphincter(to insure adequate drainage): 1)CISC→ Usually done 3 -4 hourly. Problems: -recurrent UTIs. -recurrent incontinence. 2) Supravesical urinary diversion. 3)sphincterotomy. Dr
COMPLICATIONS OF NEUROPATHIC BLADDER • Stasis of urine lead to: 1. Acute or chronic infection: UTIs is the most common complication. (also repeated catheterization to empty a flaccid bladder increases infection risk). 2. Reflux: backflow of urine from a full bladder hydronehrosis pyelonephritis and renal damage ESRD. 3. Renal stone. Dr
Thank you
- Slides: 46