Anatomy Pertinent to Mitral Intervention for MR Mechanisms





- Slides: 65

Anatomy Pertinent to Mitral Intervention for MR: Mechanisms and Severity Steven A. Goldstein MD FACC, FASE Professor of Medicine Georgetown University Medical School Washington Hospital Center Saturday, March 3, 2018
DISCLOSURE I have N O relevant financial relationships
3 D-TEE in Mitral Interventions • Surgical mitral valve repair (Operating Rm) • Edge-to-edge repair of mitral regurgitation • Transcatheter MV insertion (TMVI) (e. g. , Tendyne) • Closure of paravalvular mitral regurgitation • Valve-in-valve implantation • Balloon mitral valvuloplasty (mitral stenosis)
Echo for MV Disease • Mitral valve anatomy/pathology Mechanism(s) of MV disease • Quantitation of MR • Procedural guidance
Unlike AS singular pathology MR highly variable etiologies
MV anatomy/pathology
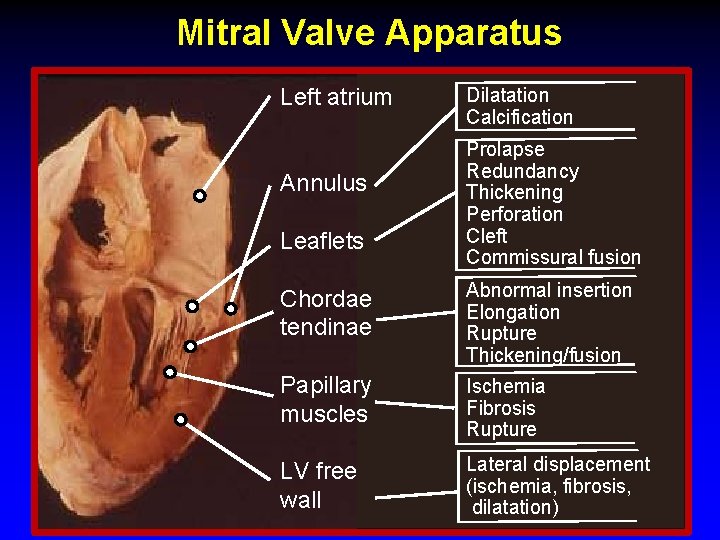
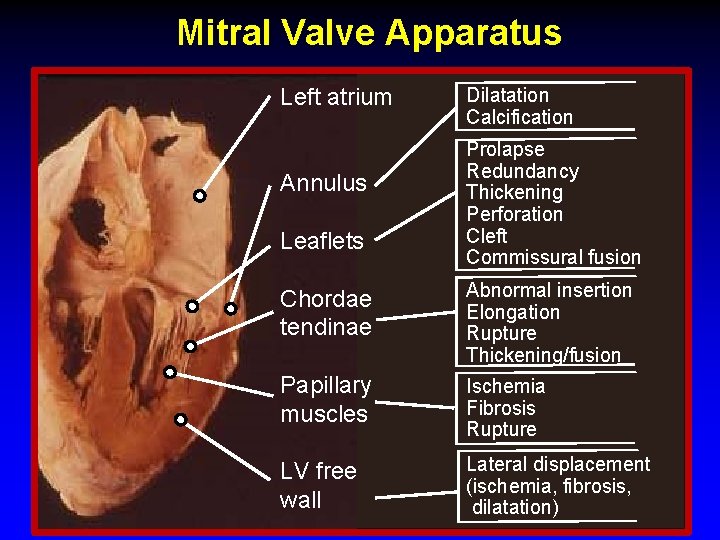
Mitral Valve Apparatus Dilatation Left atrium Annulus Leaflets Dilatation Calcification Prolapse Redundancy Thickening Perforation Cleft Commissural fusion Chordae tendinae Abnormal insertion Elongation Rupture Thickening/fusion Papillary muscles Ischemia Fibrosis Rupture LV free wall Lateral displacement (ischemia, fibrosis, dilatation)
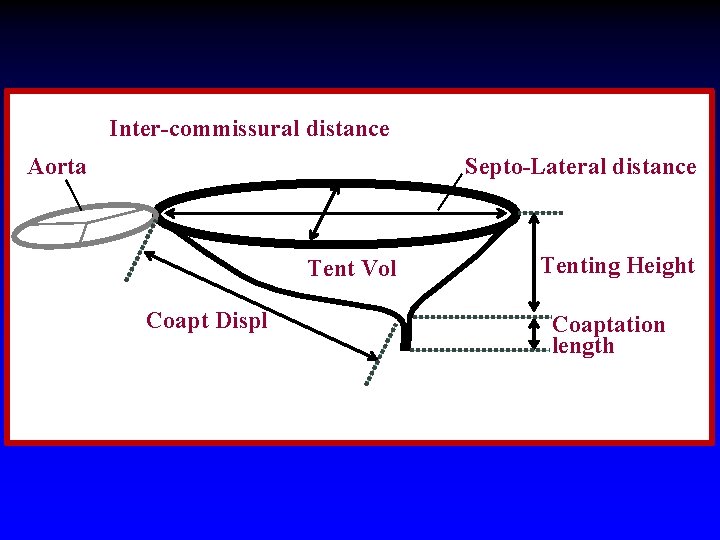
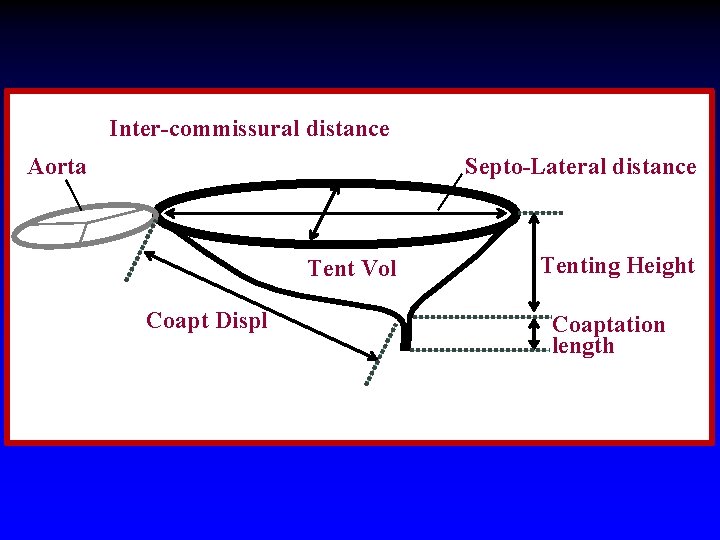
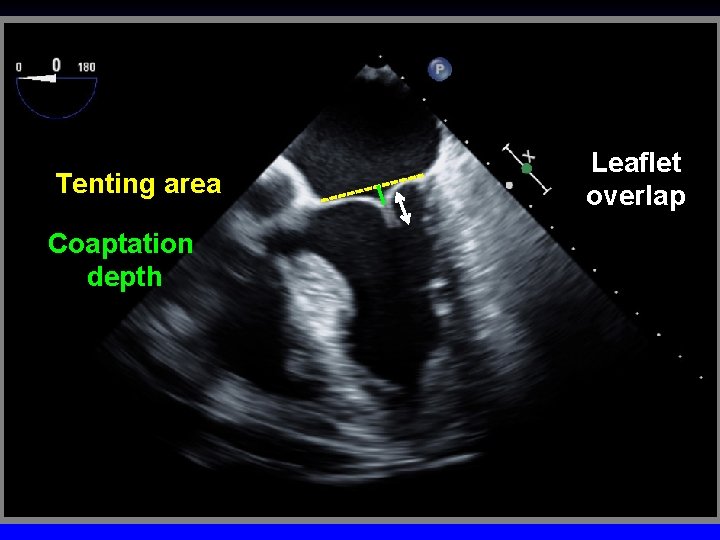
Inter-commissural distance Aorta Septo-Lateral distance Tent Vol Coapt Displ Tenting Height Coaptation length
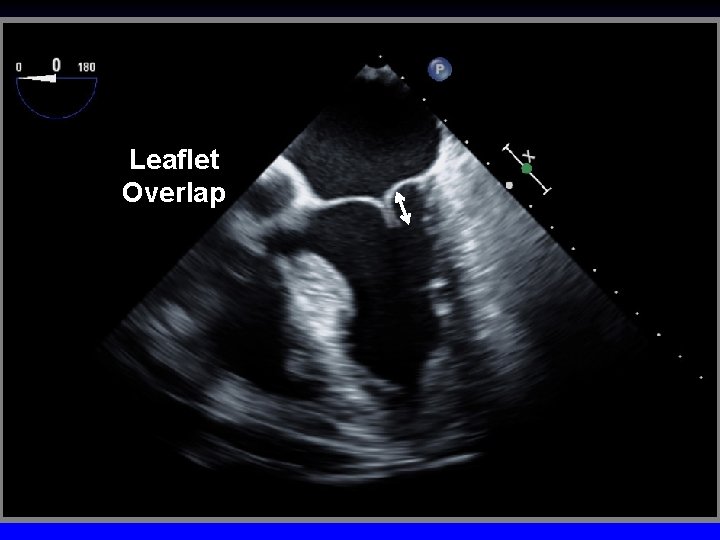
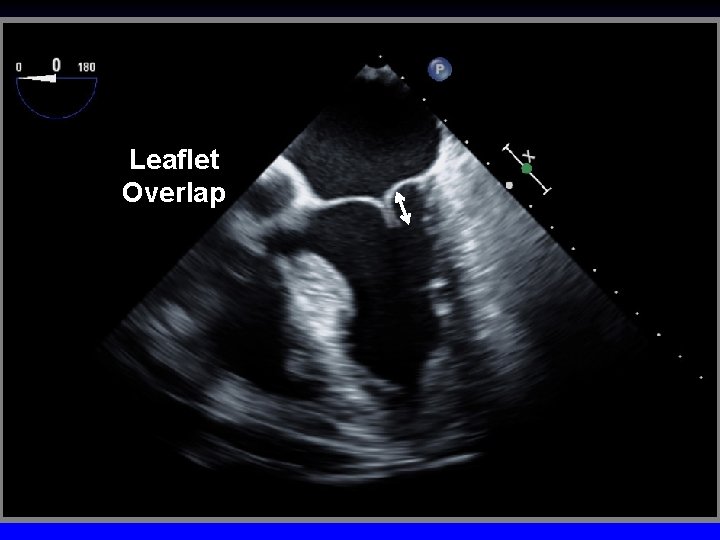
Leaflet Overlap
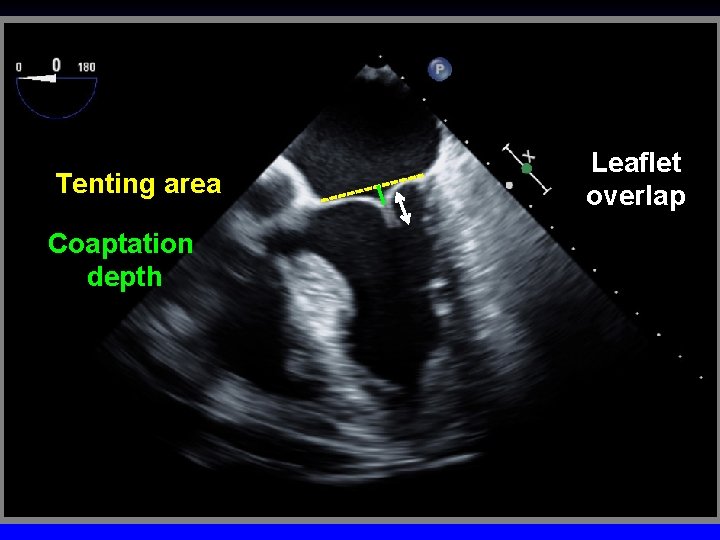
Tenting area Coaptation depth Leaflet overlap
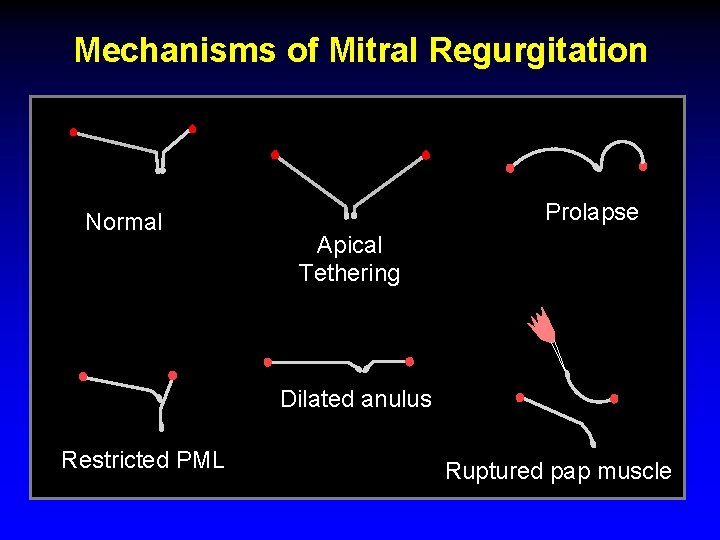
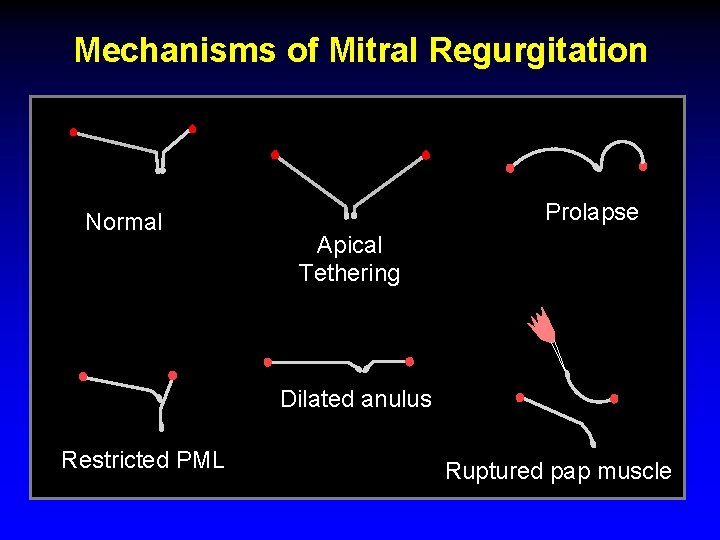
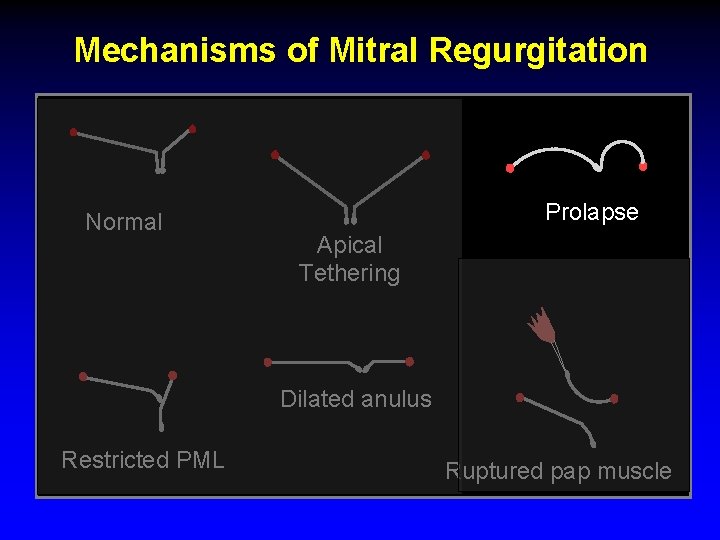
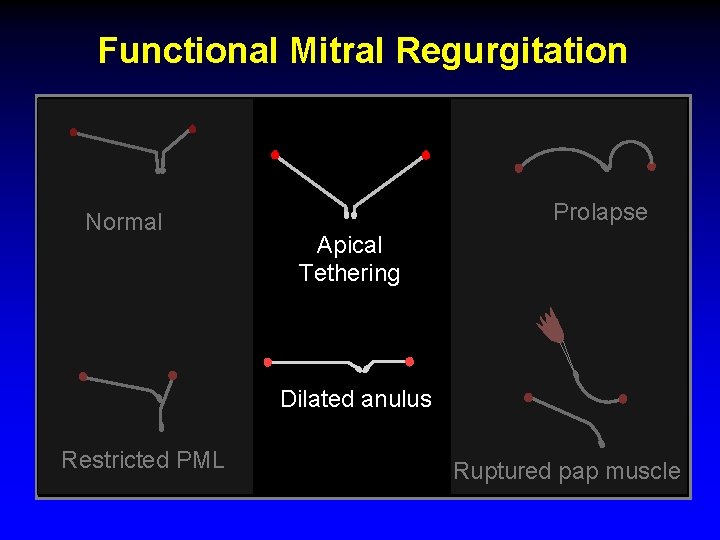
Mechanisms of Mitral Regurgitation Normal Prolapse Apical Tethering Dilated anulus Restricted PML Ruptured pap muscle
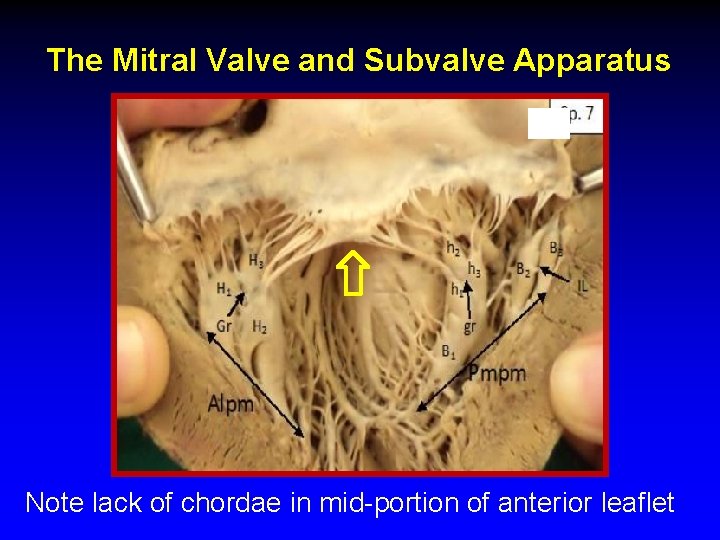
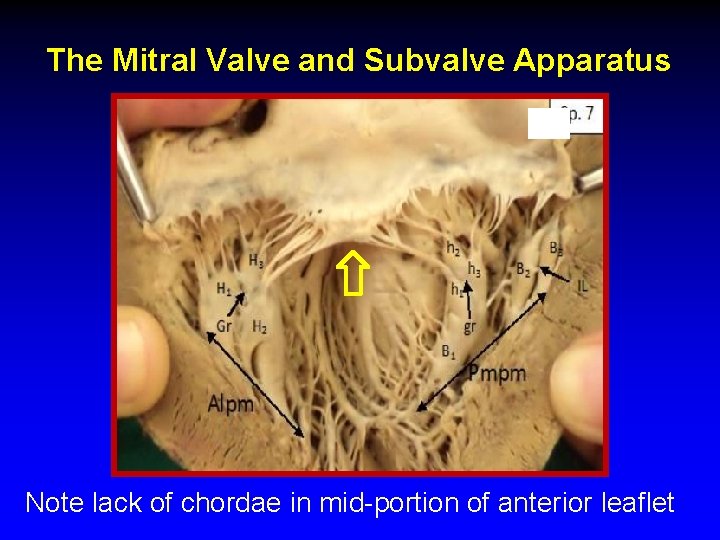
The Mitral Valve and Subvalve Apparatus Note lack of chordae in mid-portion of anterior leaflet
Ruptured cords
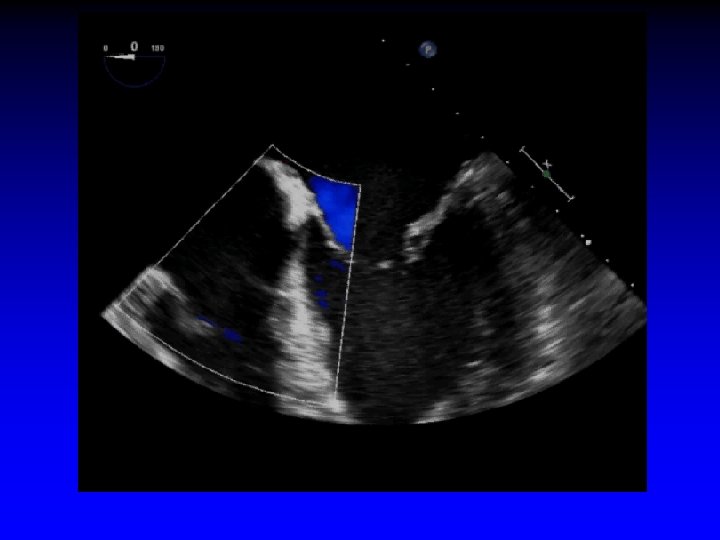
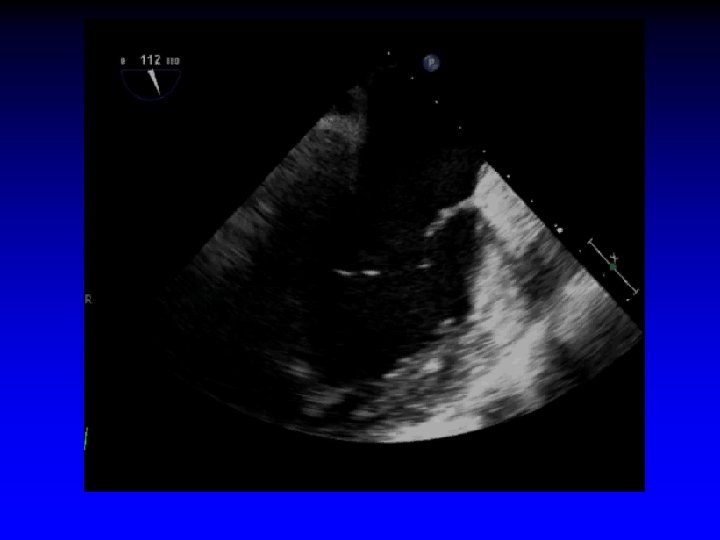
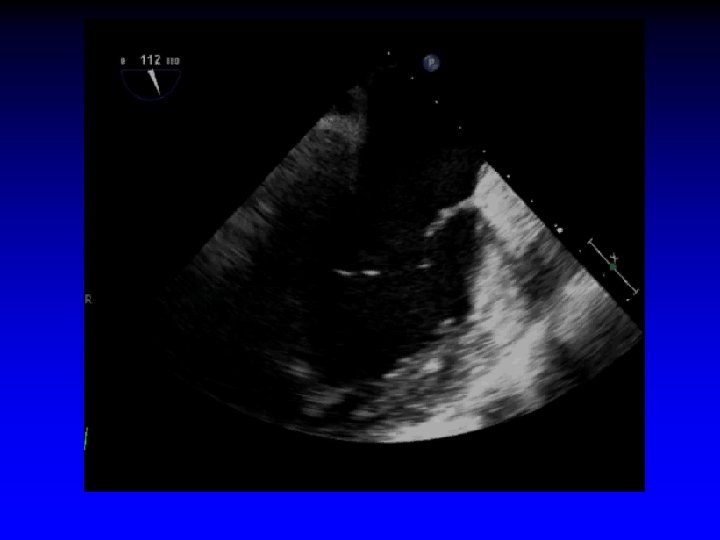
Case 1 Ruptured cords P 2
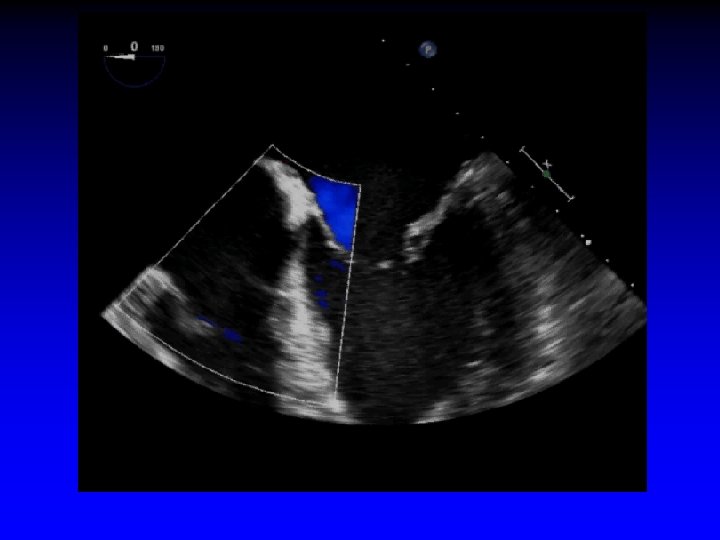
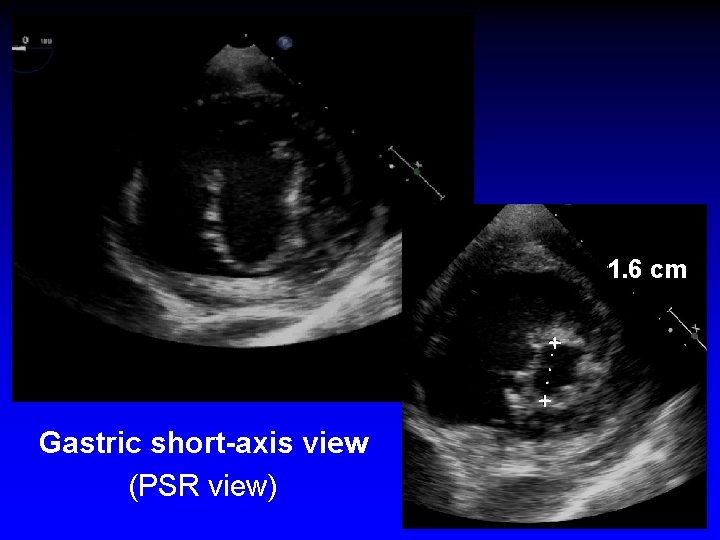
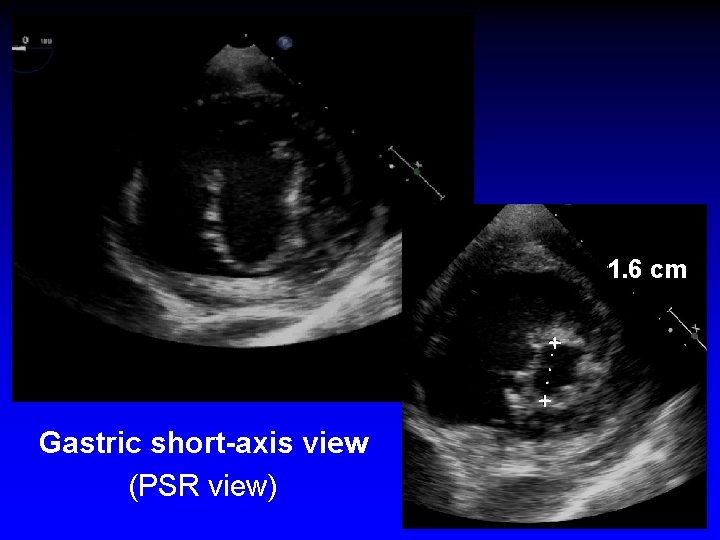
1. 6 cm +. . . + Gastric short-axis view (PSR view)
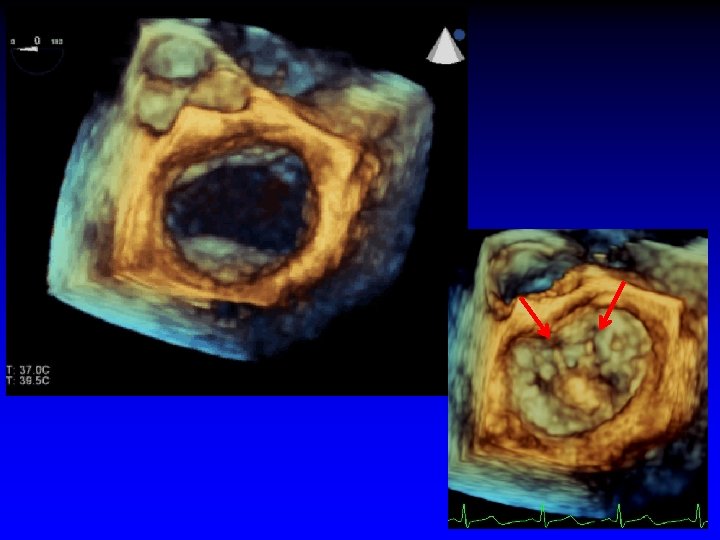
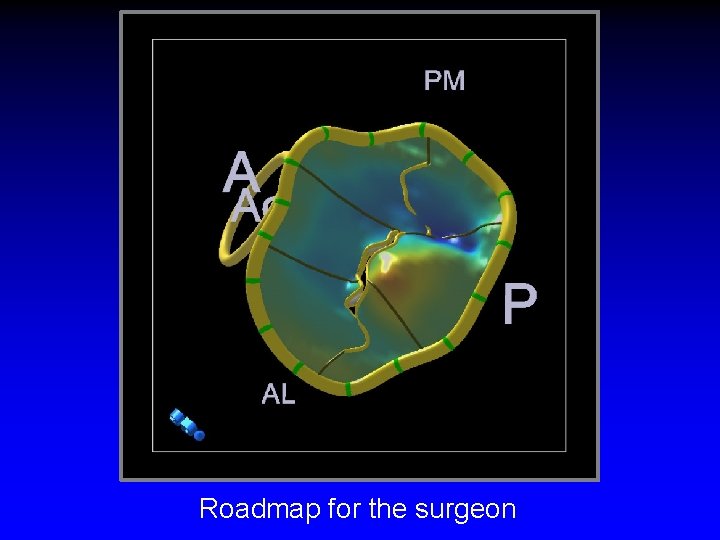
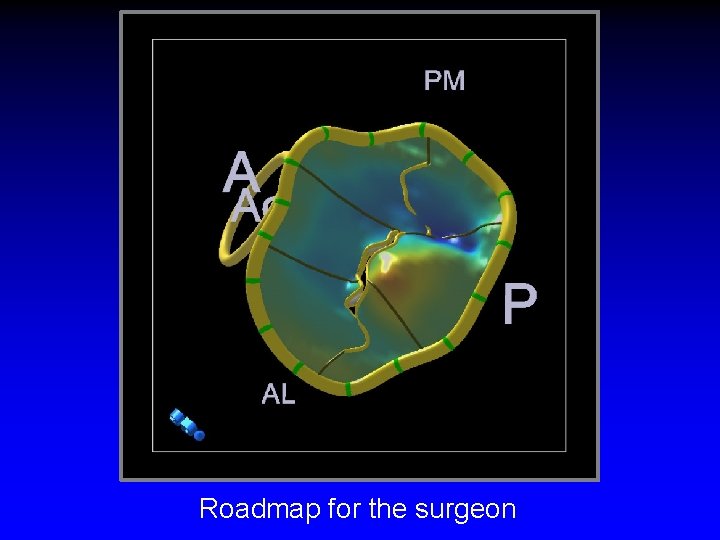
Roadmap for the surgeon
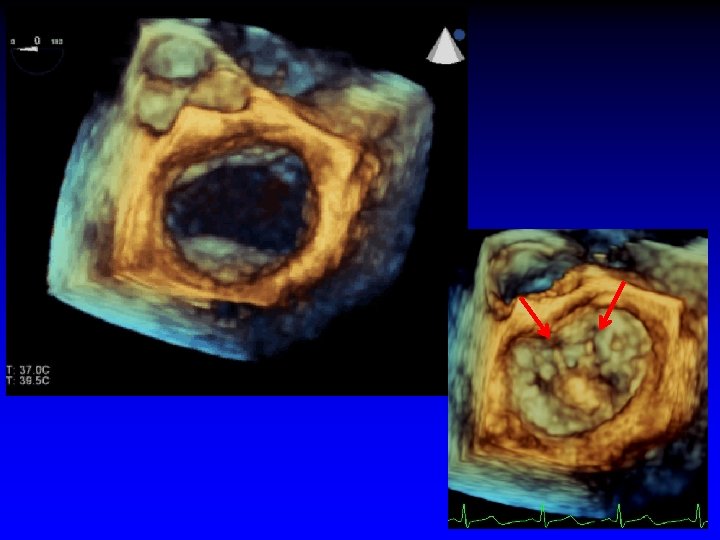
Case 2 Ruptured cord P 2
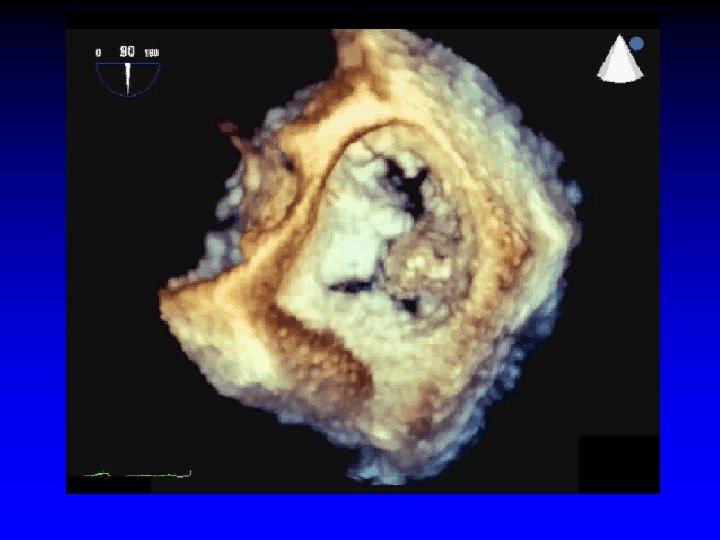
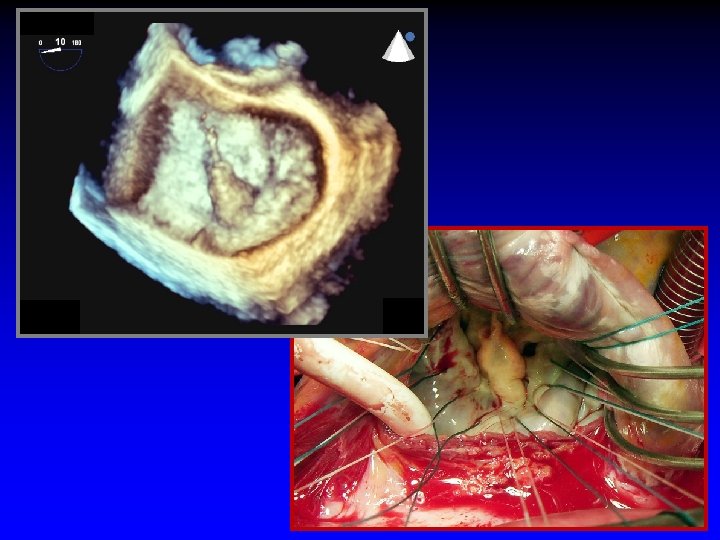
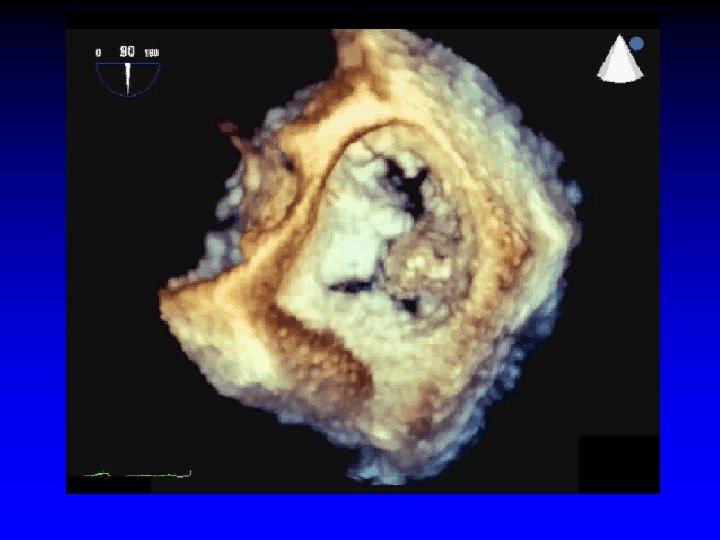
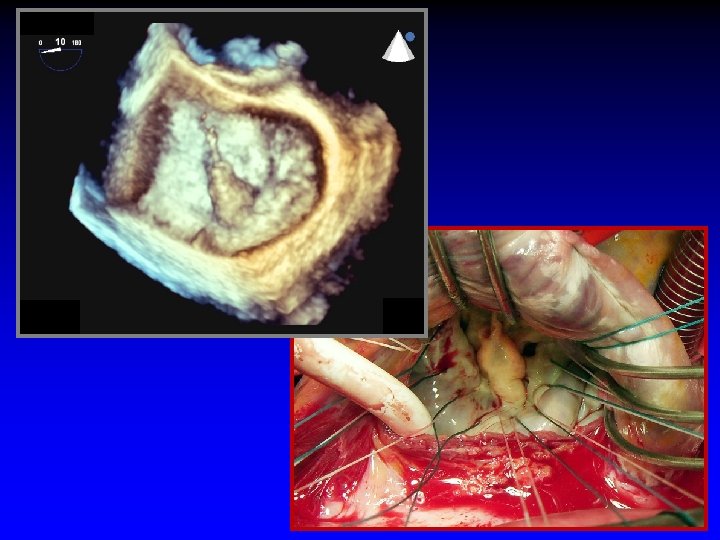
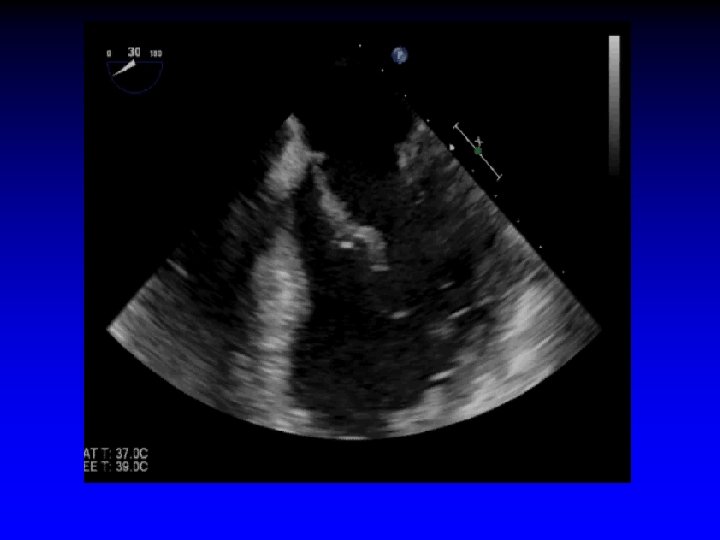
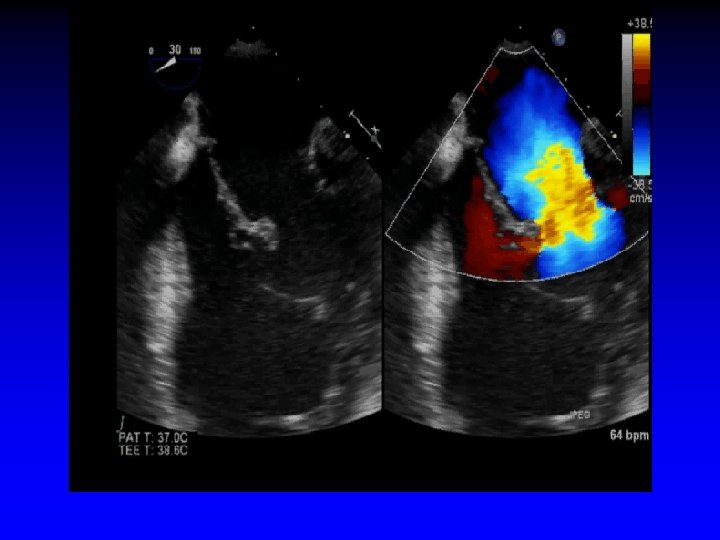
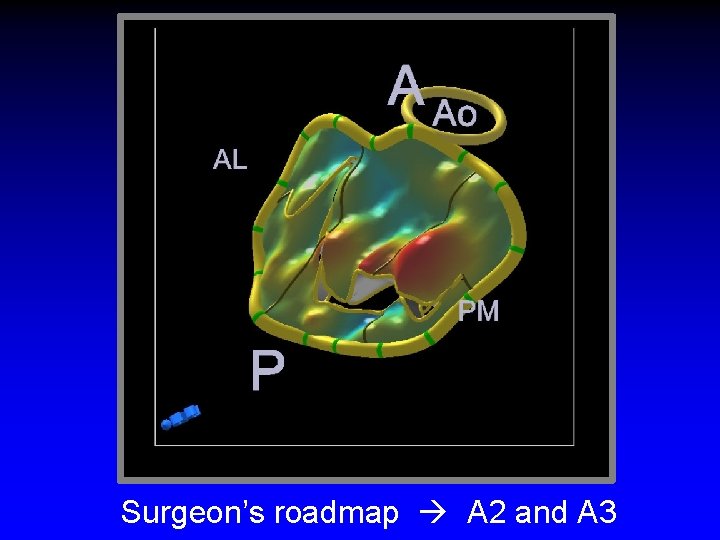
Case 3 Ruptured cords A 2 and A 3
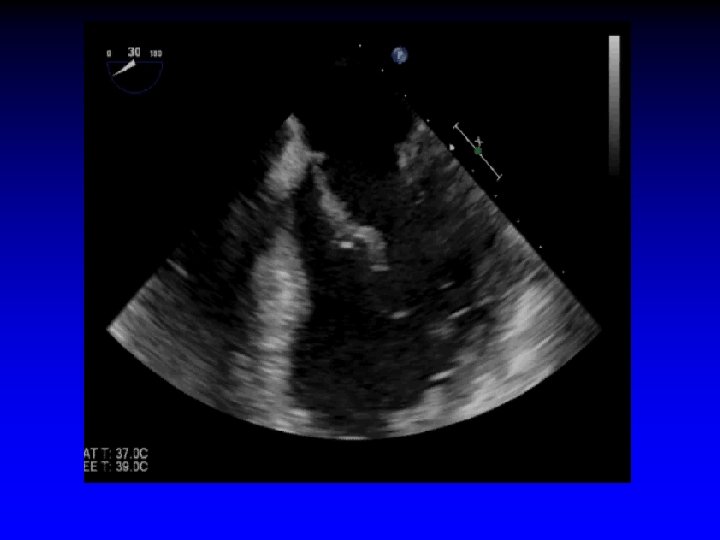
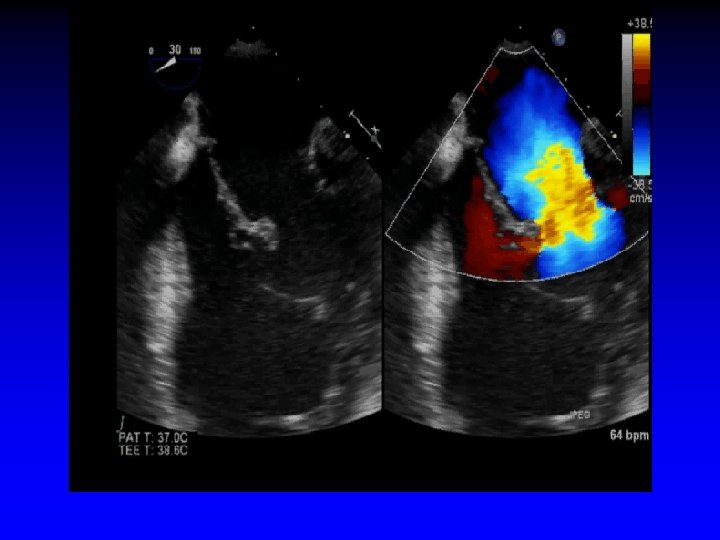
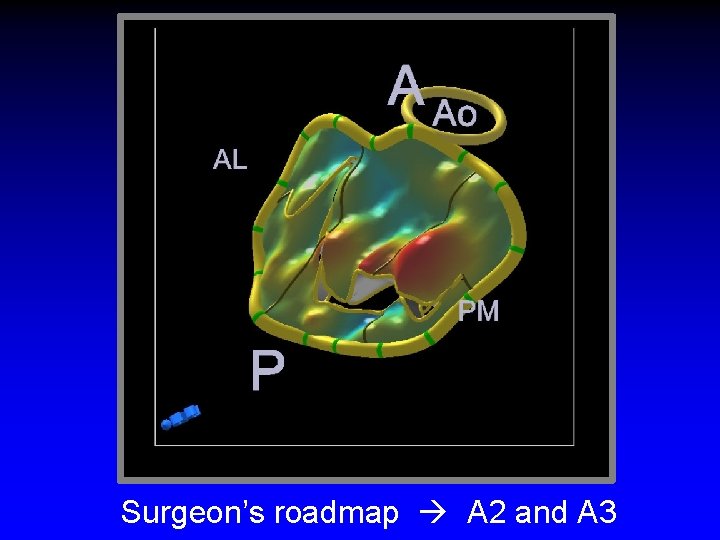
Surgeon’s roadmap A 2 and A 3
MVP
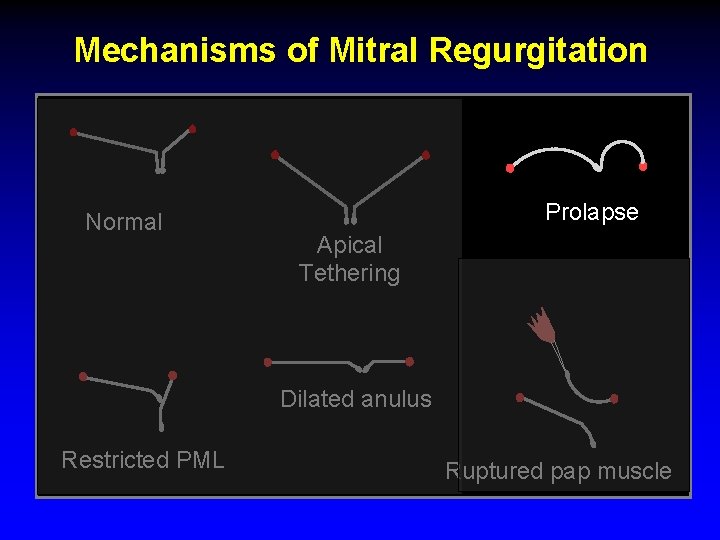
Mechanisms of Mitral Regurgitation Normal Prolapse Apical Tethering Dilated anulus Restricted PML Ruptured pap muscle
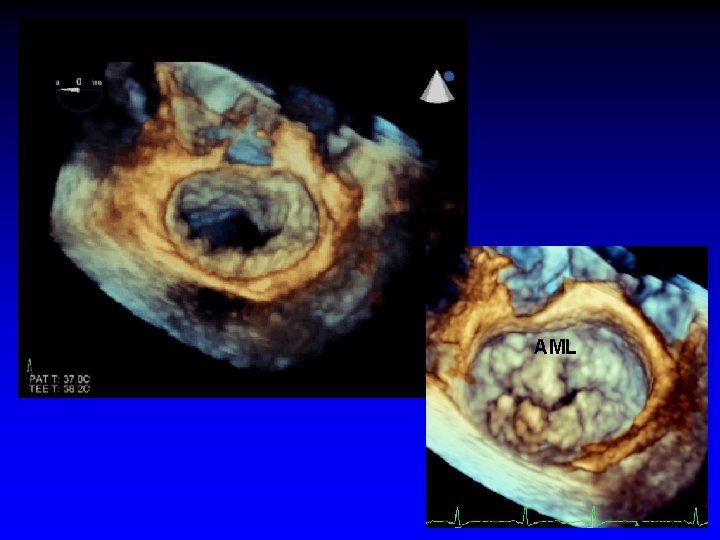
Case 4 Mitral Valve Prolapse

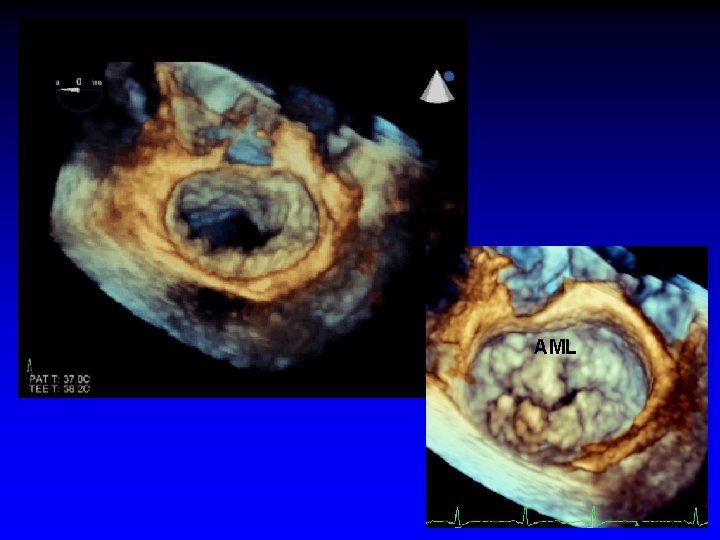
AML
Functional MR
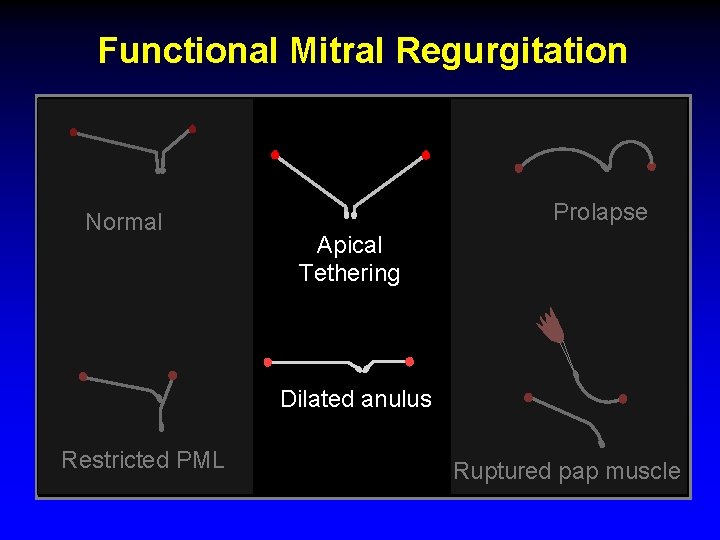
Functional Mitral Regurgitation Normal Prolapse Apical Tethering Dilated anulus Restricted PML Ruptured pap muscle
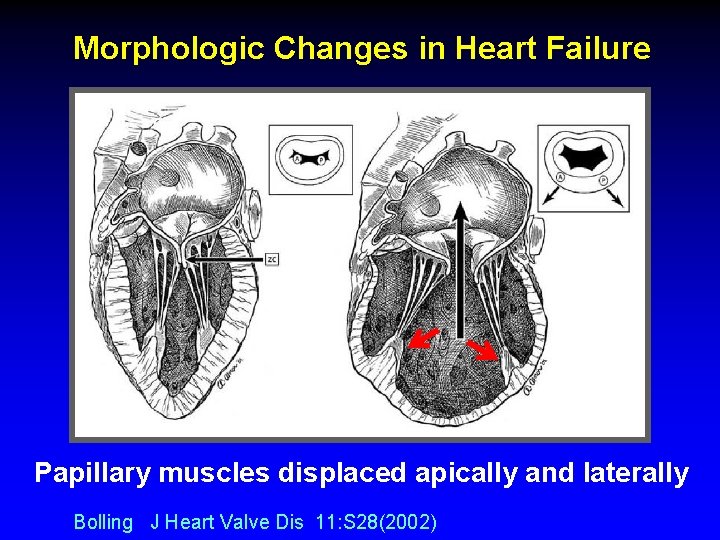
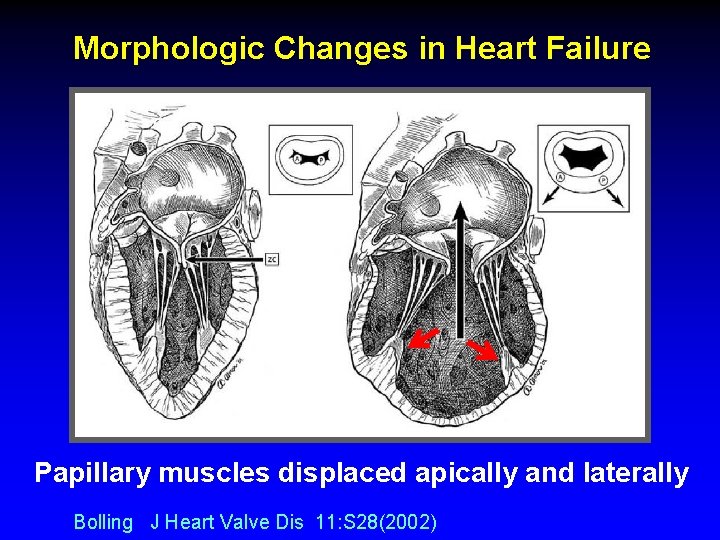
Morphologic Changes in Heart Failure Papillary muscles displaced apically and laterally Bolling J Heart Valve Dis 11: S 28(2002)
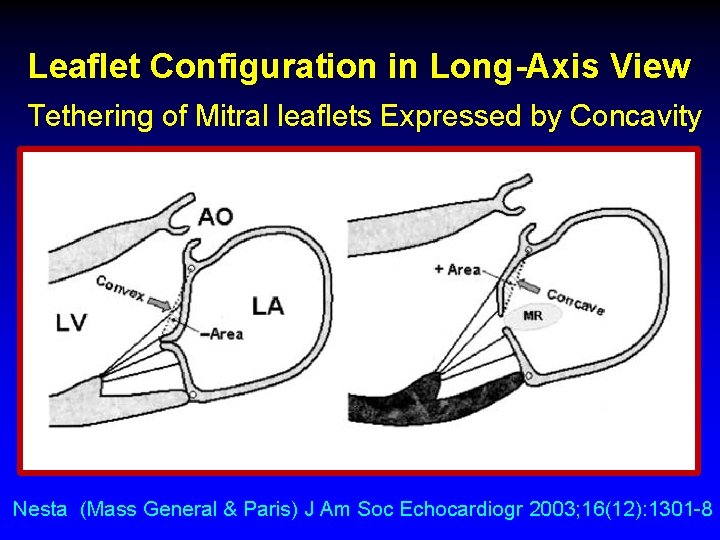
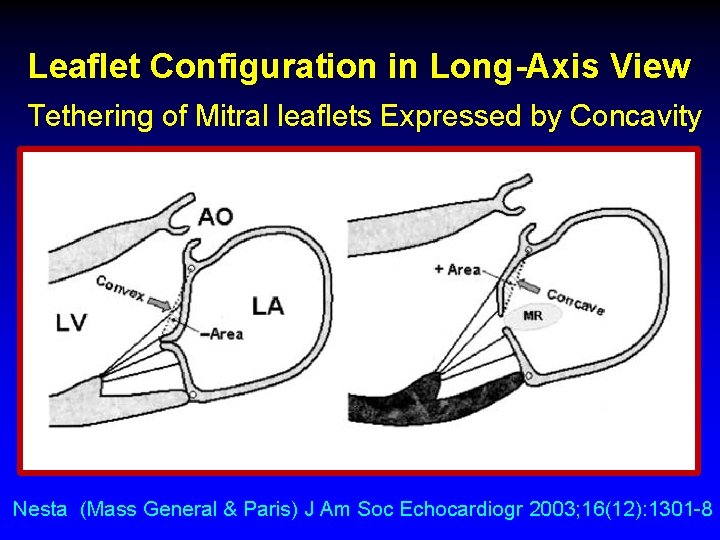
Leaflet Configuration in Long-Axis View Tethering of Mitral leaflets Expressed by Concavity Nesta (Mass General & Paris) J Am Soc Echocardiogr 2003; 16(12): 1301 -8
Carpentier IIIb Restricted posterior leaflet
Example of exclusion
Example of exclusion
Example of exclusion
Example of exclusion
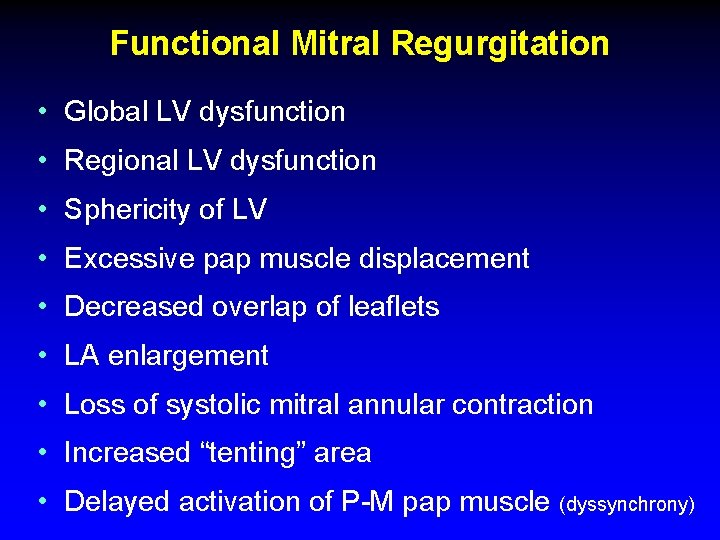
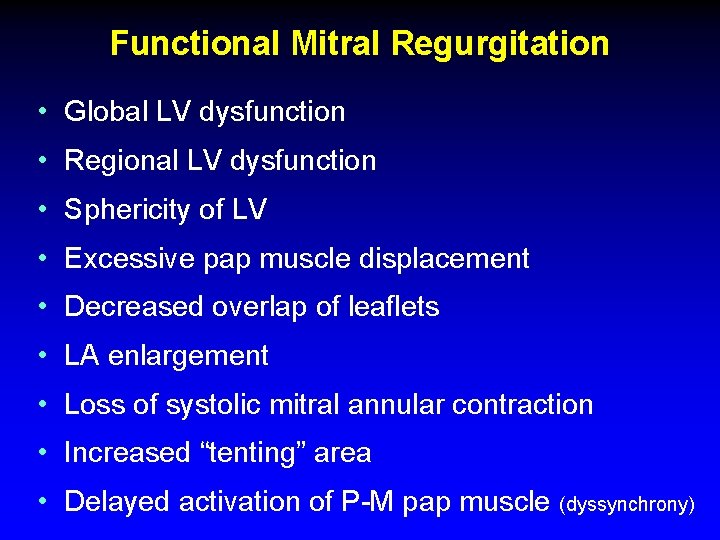
Functional Mitral Regurgitation • Global LV dysfunction • Regional LV dysfunction • Sphericity of LV • Excessive pap muscle displacement • Decreased overlap of leaflets • LA enlargement • Loss of systolic mitral annular contraction • Increased “tenting” area • Delayed activation of P-M pap muscle (dyssynchrony)
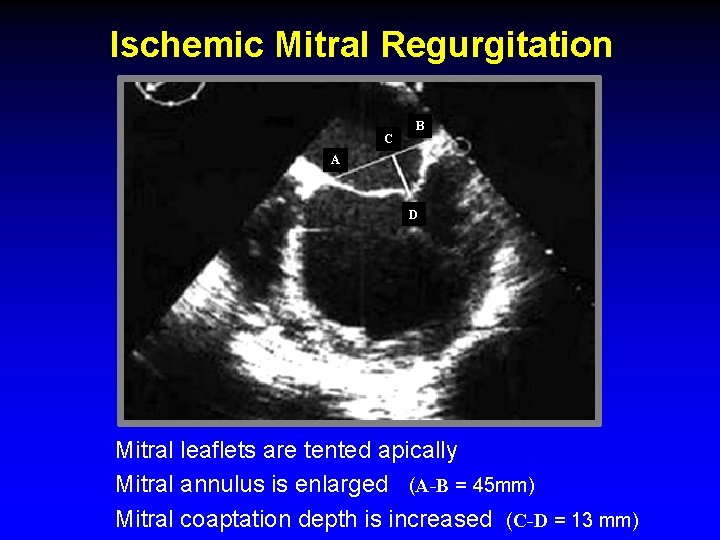
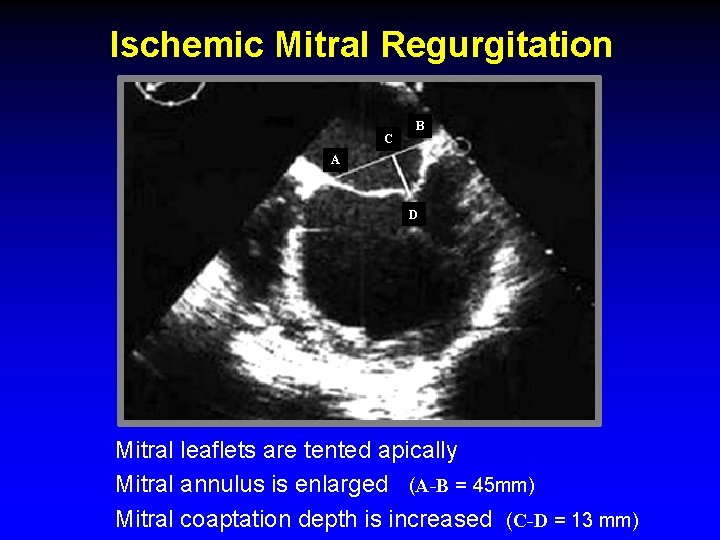
Ischemic Mitral Regurgitation C B A D Mitral leaflets are tented apically Mitral annulus is enlarged (A-B = 45 mm) Mitral coaptation depth is increased (C-D = 13 mm)
Procedural Guidance
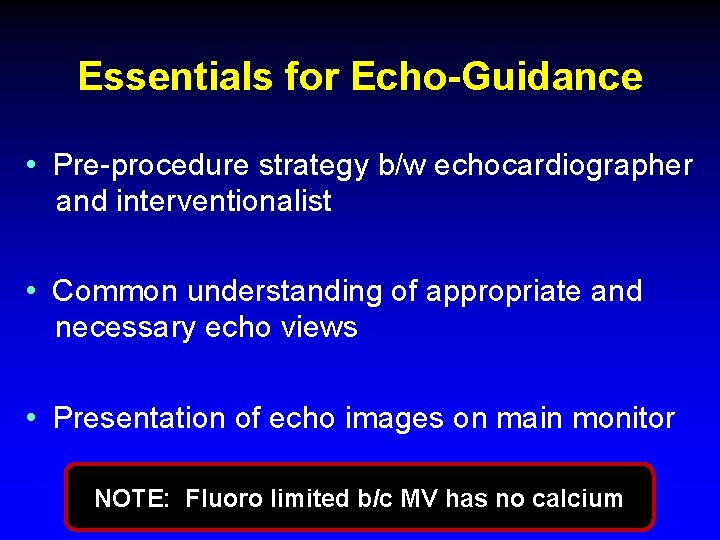
Essentials for Echo-Guidance • Pre-procedure strategy b/w echocardiographer and interventionalist • Common understanding of appropriate and necessary echo views • Presentation of echo images on main monitor NOTE: Fluoro limited b/c MV has no calcium

Wánghòu Queen of Med. Star Structural Heart Disease
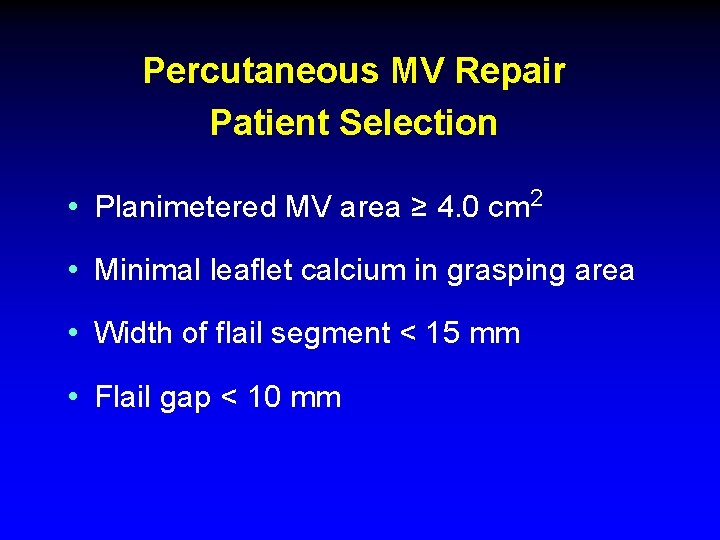
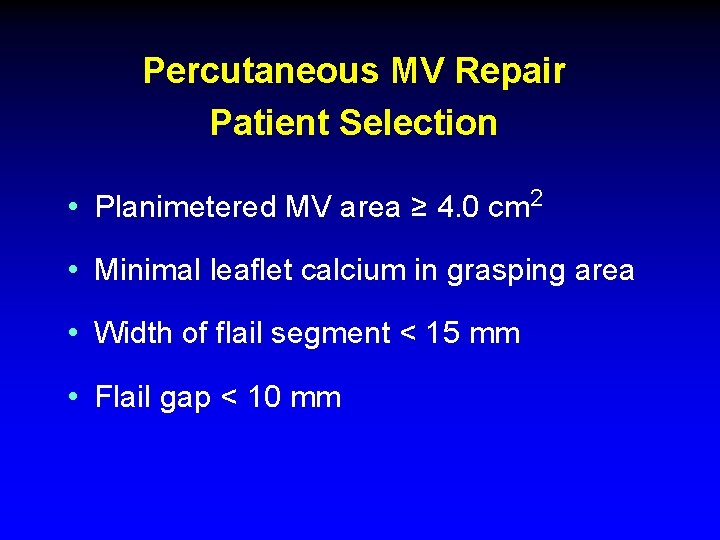
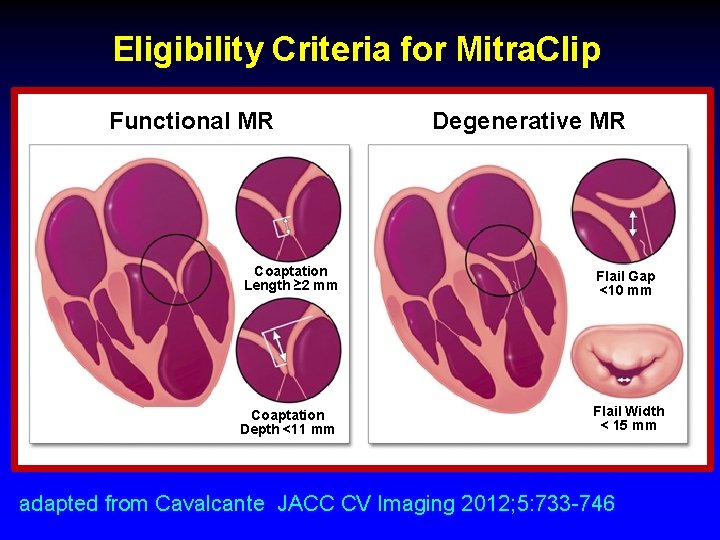
Percutaneous MV Repair Patient Selection • Planimetered MV area ≥ 4. 0 cm 2 • Minimal leaflet calcium in grasping area • Width of flail segment < 15 mm • Flail gap < 10 mm
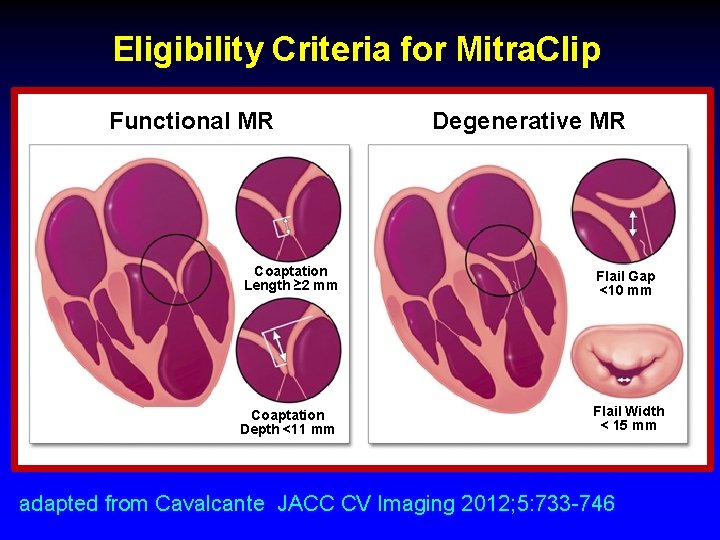
Eligibility Criteria for Mitra. Clip Functional MR Degenerative MR Coaptation Length ≥ 2 mm Flail Gap <10 mm Coaptation Depth <11 mm Flail Width < 15 mm adapted from Cavalcante JACC CV Imaging 2012; 5: 733 -746
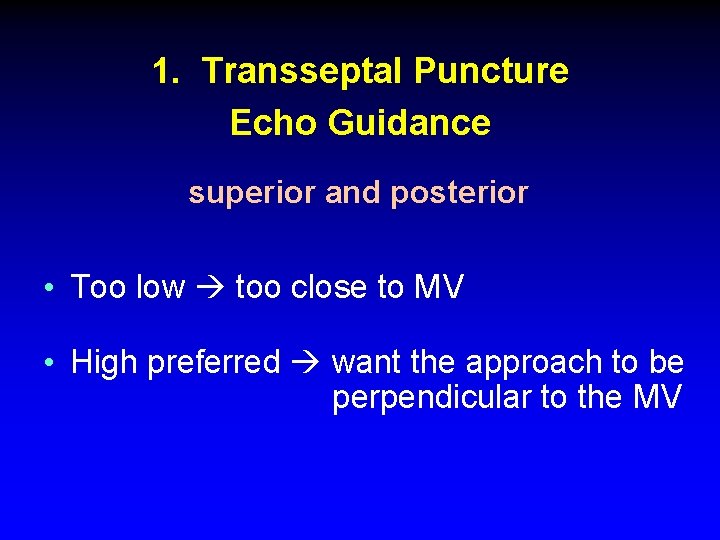
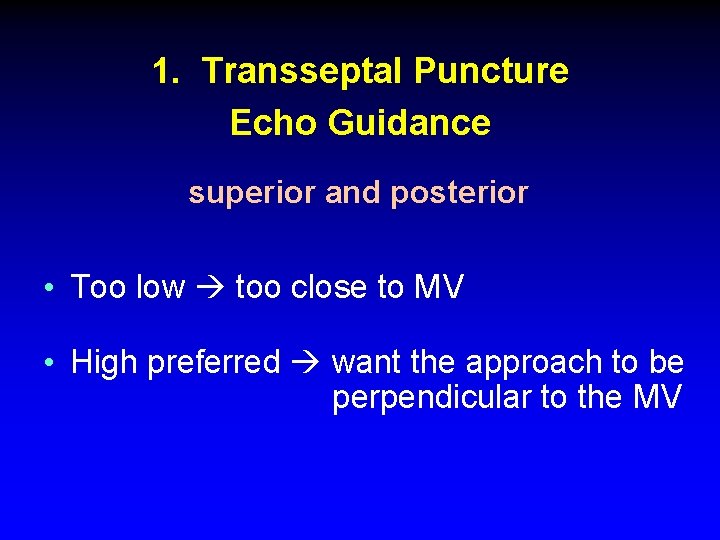
1. Transseptal Puncture Echo Guidance superior and posterior • Too low too close to MV • High preferred want the approach to be perpendicular to the MV
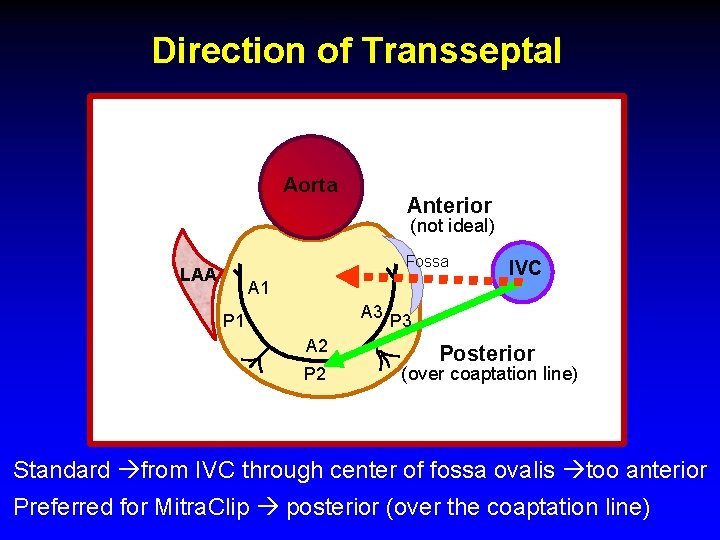
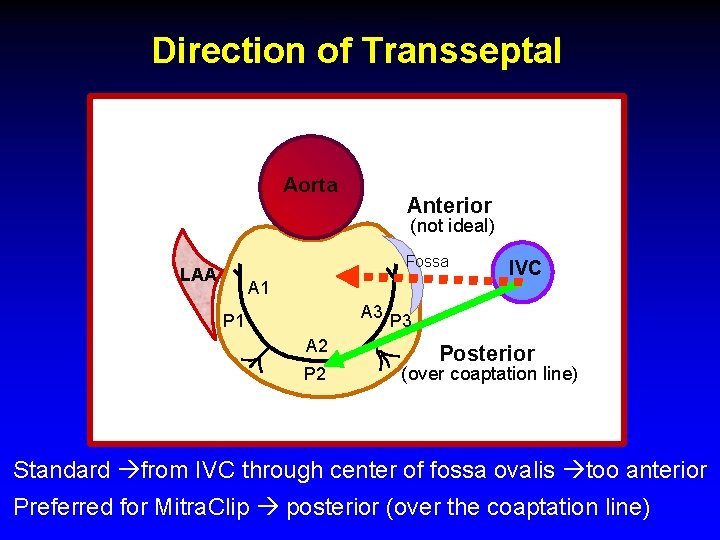
Direction of Transseptal Aorta Anterior (not ideal) Fossa LAA A 1 IVC A 3 P 1 A 2 Posterior (over coaptation line) Standard from IVC through center of fossa ovalis too anterior Preferred for Mitra. Clip posterior (over the coaptation line)
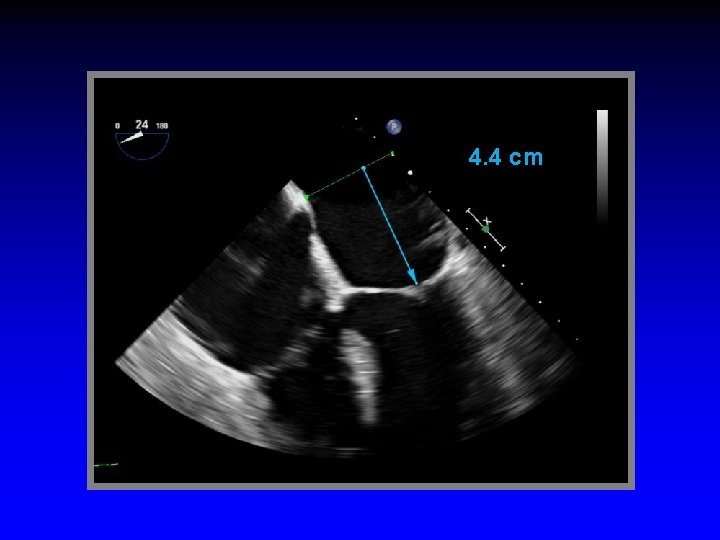
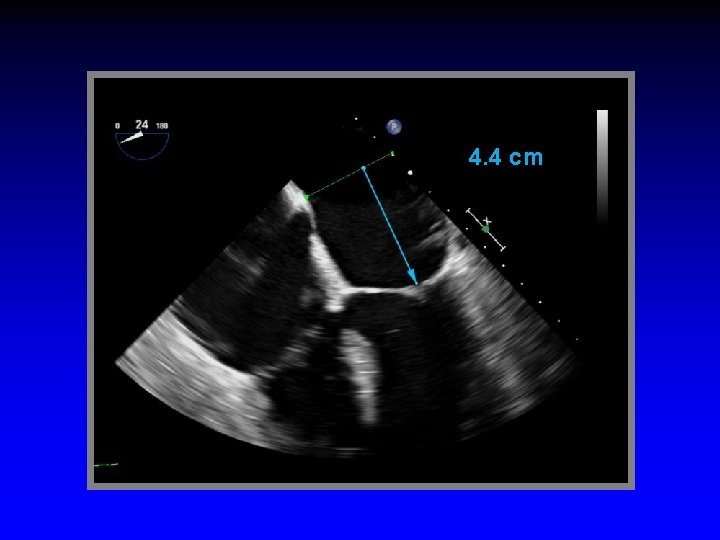
4. 4 cm

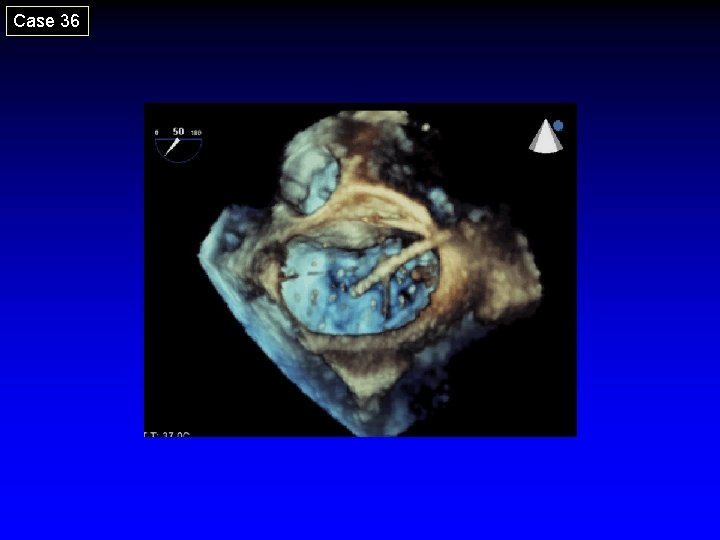
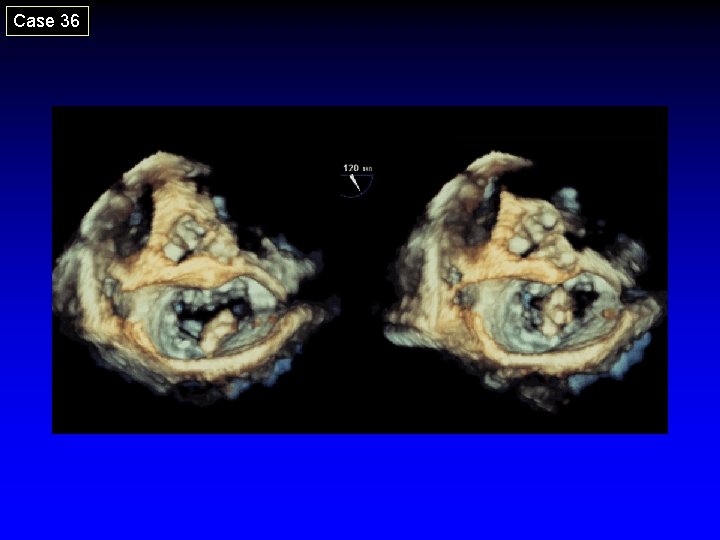
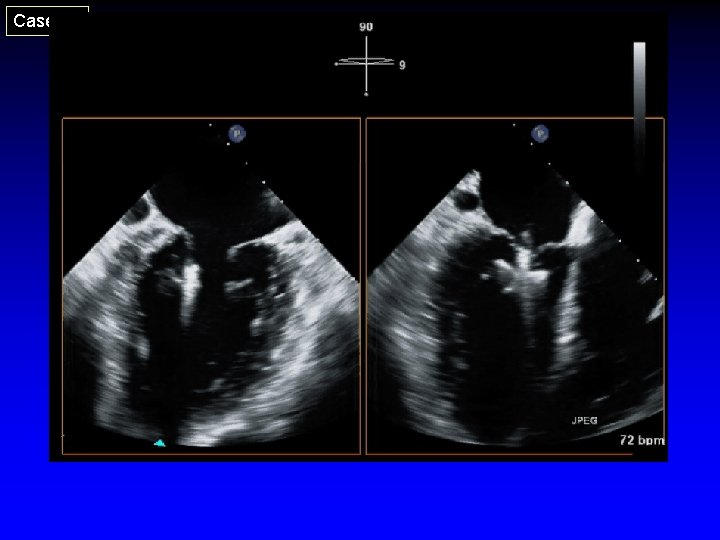
Case 36
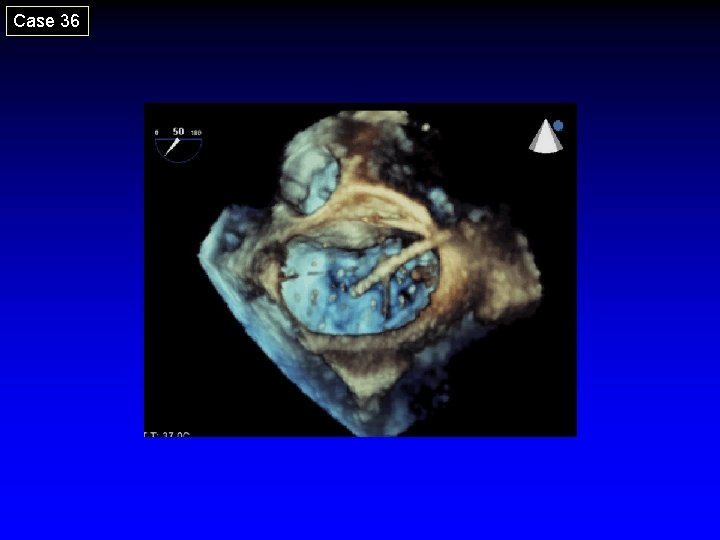
Case 36
2. Introduction of Steerable Guide Catheter (SGC) into LA • Advance SGC over stiff wire (wire in L-UPV) • Done with fluoro and TEE guidance (to avoid injury to free LA wall) • Double ring needs to be in LA • Dilator and stiff wire retrieved
3. Advancement of Clip Delivery System (CDS) into LA • Advance SGC over stiff wire (wire in L-UPV) • Done with fluoro and TEE guidance (to avoid injury to free LA wall) • Double ring needs to be in LA • Dilator and stiff wire retrieved
4. Steering Clip Perpendicular to Coaptation Line - Echo Guidance • Align clip arms perpendicular to the line of coaptation • Maintain clip open to at 180º to help visualize the clip arms • Advance clip into LV just below the leaflet edges prior to grasping
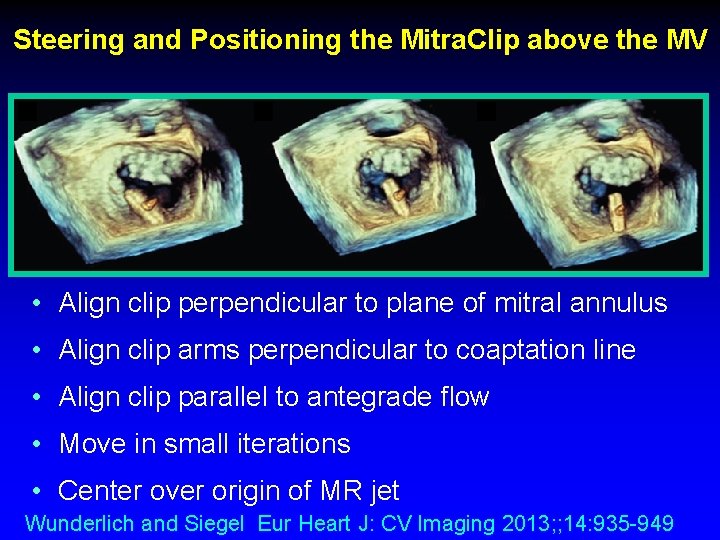
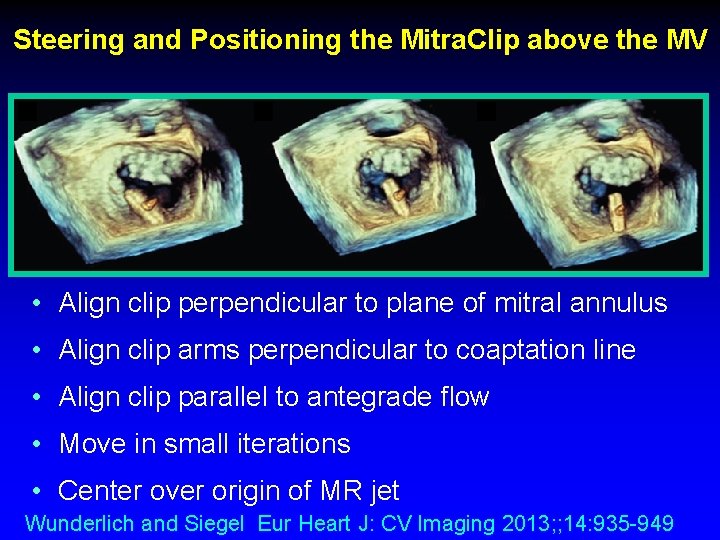
Steering and Positioning the Mitra. Clip above the MV • Align clip perpendicular to plane of mitral annulus • Align clip arms perpendicular to coaptation line • Align clip parallel to antegrade flow • Move in small iterations • Center over origin of MR jet Wunderlich and Siegel Eur Heart J: CV Imaging 2013; ; 14: 935 -949
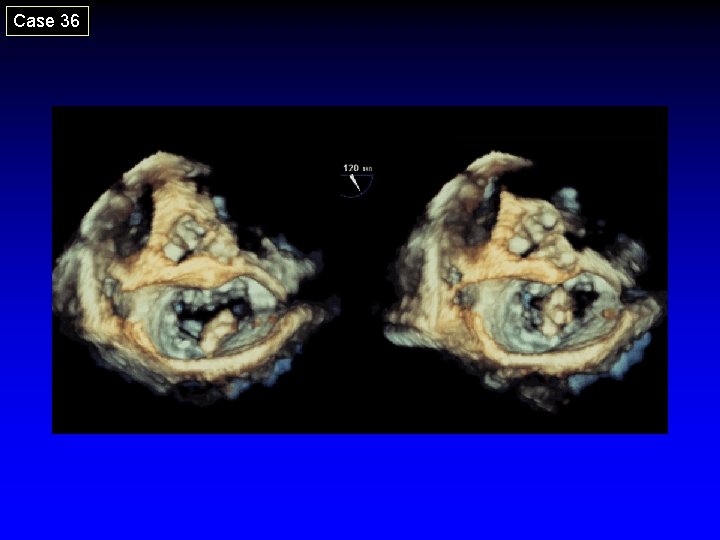
Case 36
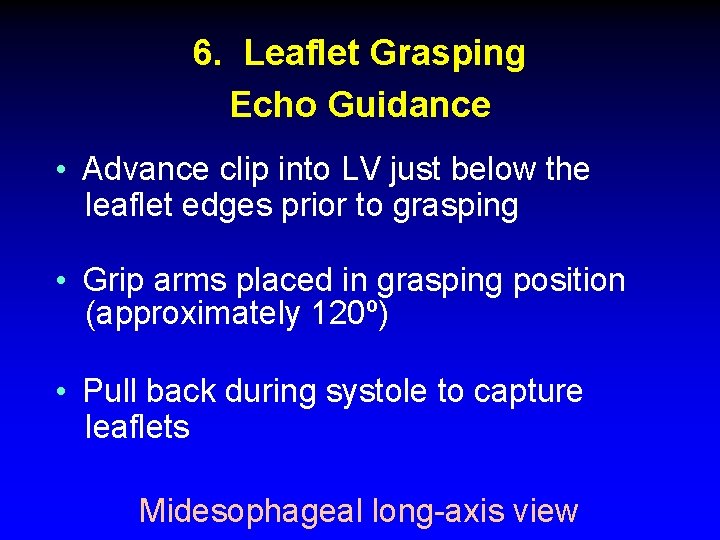
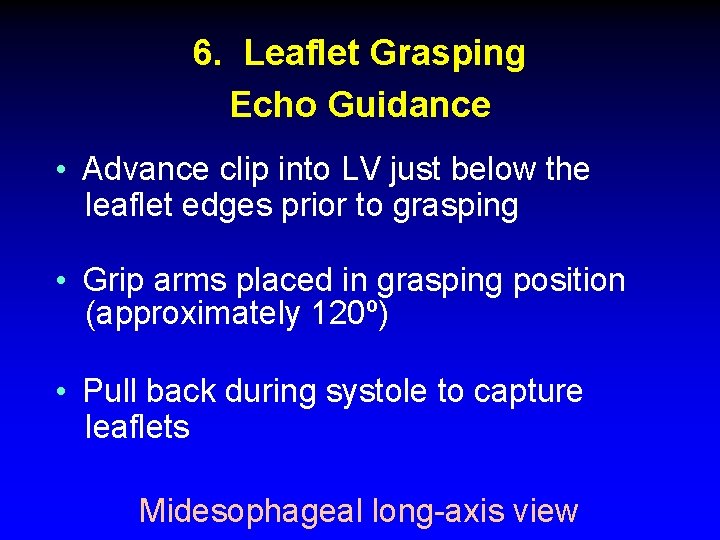
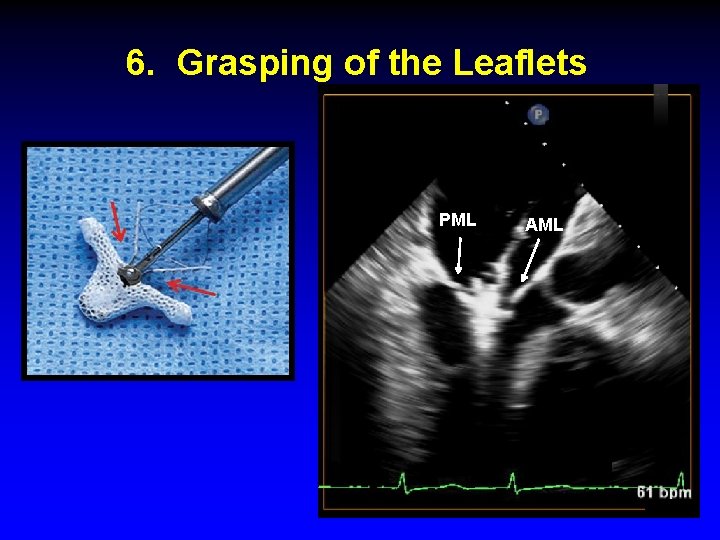
6. Leaflet Grasping Echo Guidance • Advance clip into LV just below the leaflet edges prior to grasping • Grip arms placed in grasping position (approximately 120º) • Pull back during systole to capture leaflets Midesophageal long-axis view
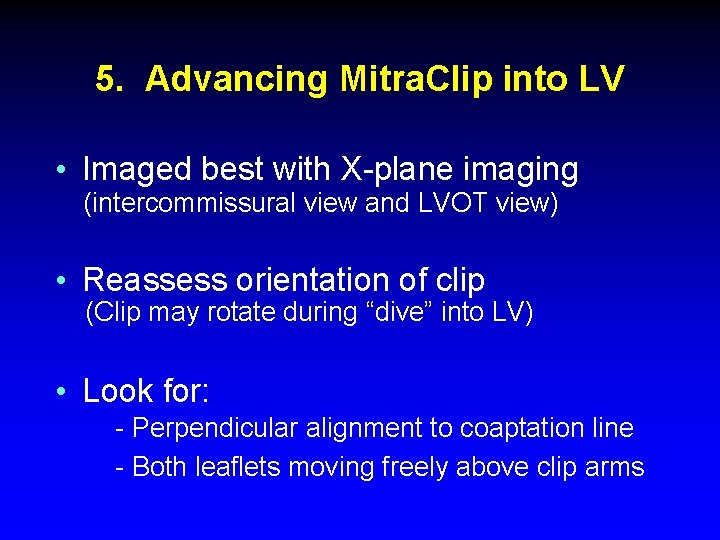
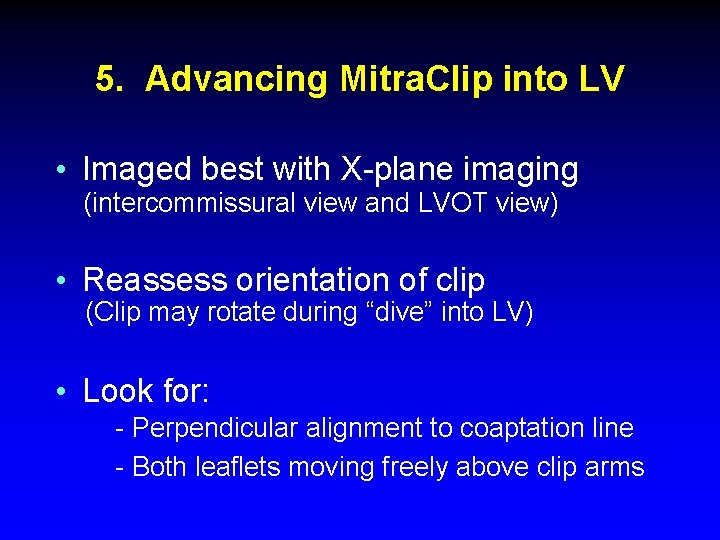
5. Advancing Mitra. Clip into LV • Imaged best with X-plane imaging (intercommissural view and LVOT view) • Reassess orientation of clip (Clip may rotate during “dive” into LV) • Look for: - Perpendicular alignment to coaptation line - Both leaflets moving freely above clip arms
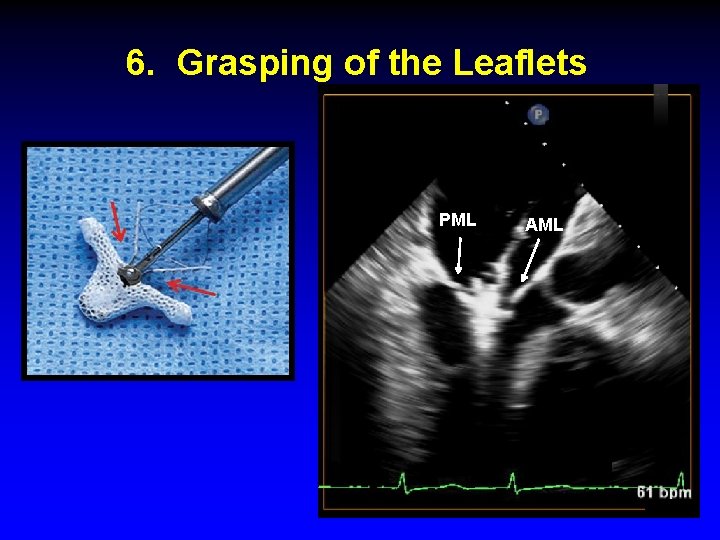
6. Grasping of the Leaflets PML AML
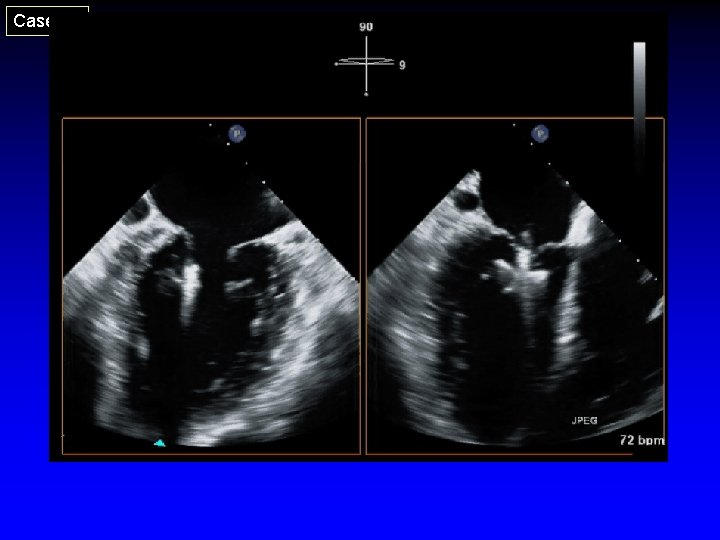
Case 20
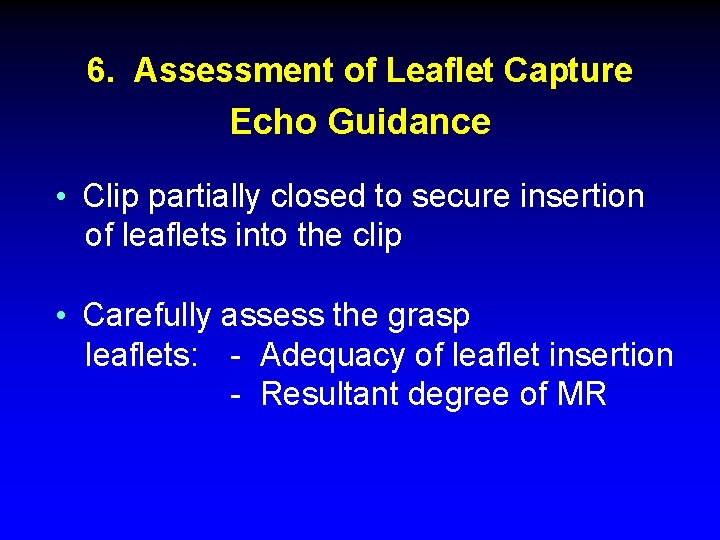
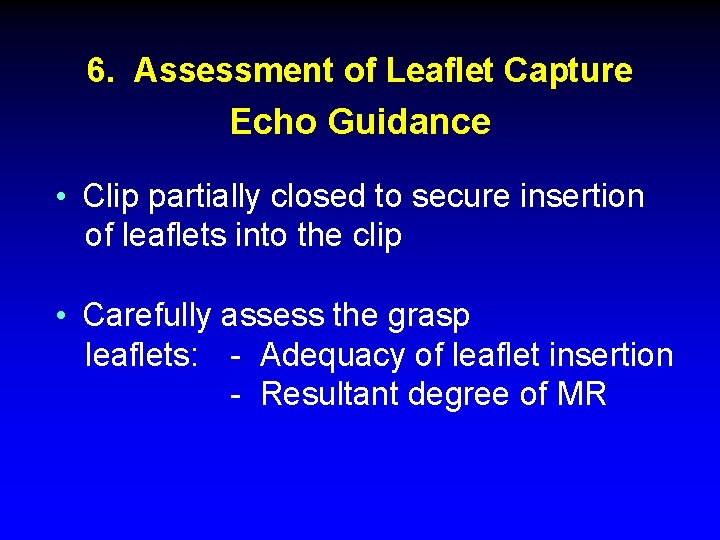
6. Assessment of Leaflet Capture Echo Guidance • Clip partially closed to secure insertion of leaflets into the clip • Carefully assess the grasp leaflets: - Adequacy of leaflet insertion - Resultant degree of MR
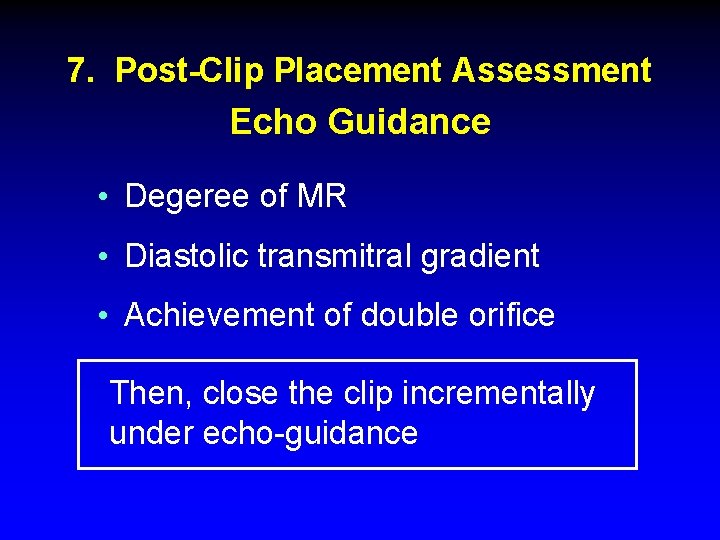
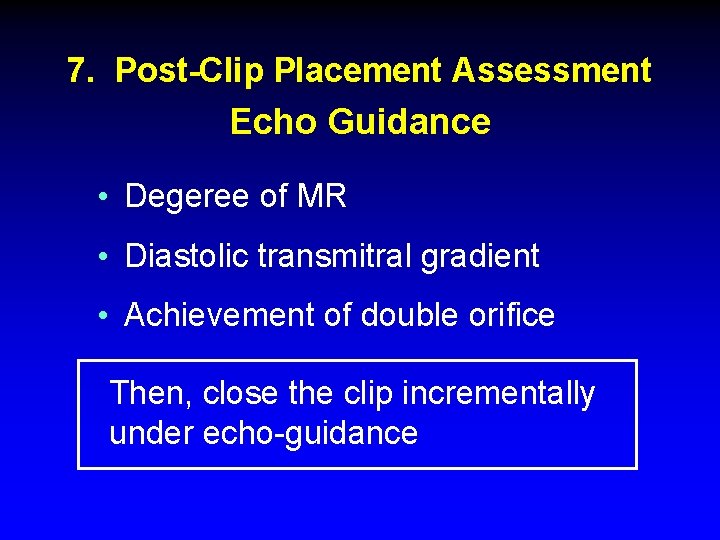
7. Post-Clip Placement Assessment Echo Guidance • Degeree of MR • Diastolic transmitral gradient • Achievement of double orifice Then, close the clip incrementally under echo-guidance
