Anatomy Pathology of the Thyroid Teresa M Bieker
Anatomy & Pathology of the Thyroid Teresa M Bieker, MBA, RT, RDMS, RDCS, RVT Lead Diagnostic Medical Sonographer University of Colorado Hospital Denver Colorado
Objectives • Anatomy and Pathology of the thyroid and surrounding structures • Identify suspicious characteristics of thyroid nodules • Types and occurrences rates of thyroid cancers
Embryology of the Thyroid n n n Formation of the thyroid begins approximately at the 4 th week of gestation The two lobes are connected by the thyroglossal duct (at the level of the tongue) By the 7 th week, the thyroid should be descended to the level of the trachea
Anatomy of the Thyroid n n n Right and left lobes are located anterolateral to the trachea & esophagus Right and left lobes are connected midline by the isthmus Size (adults) n Length: 4 -6 cm n AP: 1. 3 -1. 8 cm n Isthmus: 4 -6 mm

Neck Muscles n Strap muscles (anterior) n n n sternohyoid sternothyroid omohyoid Sternocleidomastoid (lateral) Longus colli (posterior)

Neck Vessels n Thyroid Vessels n n n superior thyroid arteries and veins inferior thyroid arteries and veins Major Neck vessels n n carotid artery jugular vein
Function of the Thyroid n Produce, store, secrete thyroid hormones n Thyroid hormones are important for: n Proper growth n Development n Metabolism n Body temperature n Heart rate/rhythm n Iodine metabolism: converts iodine from food into thyroid hormones
Thyroid Hormones n TSH (Thyroid Stimulating Hormone) n T 3 (Triiodothyronine) n T 4 (Thyroxine) n Calcitonin n Antibodies n Thyroglobulin (TG)
Thyroid Hormones • TSH: – Stimulates the thyroid to produce T 4 and then T 3. – Controlled by the pituitary gland • T 4/T 3: – Produced by the thryoid • TSH/T 4 work together
Thyroid Hormones • Calcitonin – Produced by the thryoid – Helps to regulate calcium levels • Antibodies – Typically present in autoimmune thyroid diseases (Graves, Hashimoto’s) • TG – Produced by thyroid tissue – Tumor marker
Indications for Neck Ultrasound • • Palpable enlargement Abnormal thyroid hormone levels Palpable mass Swelling in the neck Asymmetry of the neck Redness and/or tenderness Difficulty swallowing Post thyroidectomy evaluation
Scanning Technique n n Patient Position n Supine with neck extended o n Elevating the head 20 in larger patients may be helpful n Neck rotation Transducer Frequency n 7 -15 MHz Image optimization Scanning Planes
Congenital Anomalies n Pyramidal lobe n n n Shape variations n n 10 -40% of patients Arises superiorly from isthmus Missing isthmus “H” shape Ectopia (rare, follows embryological path) Agenesis n n One lobe Complete
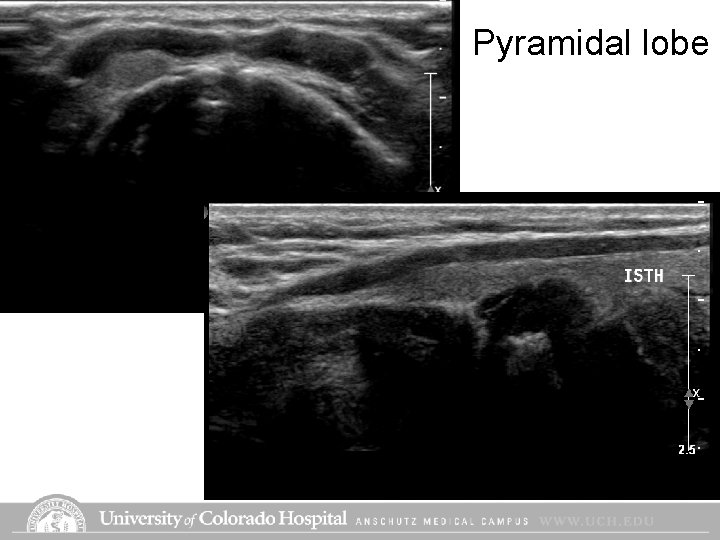
Pyramidal lobe
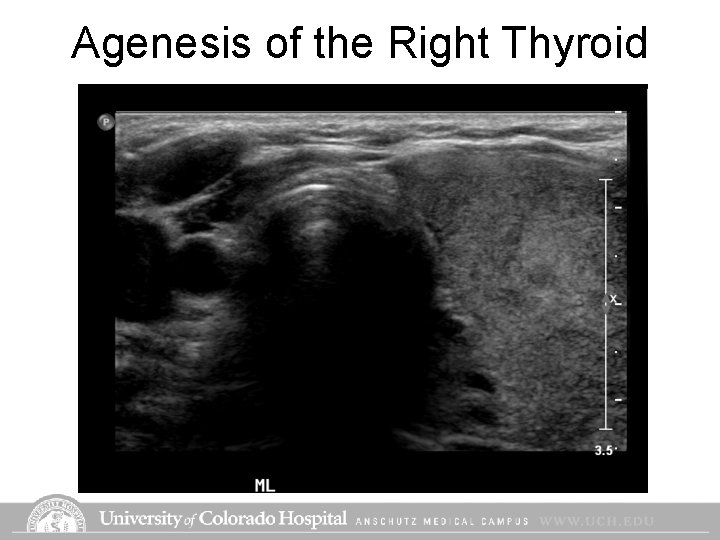
Agenesis of the Right Thyroid
Diffuse Thyroid Pathology n n n Hyperthyroidism (Grave’s Disease) Hypothyroidism Thyroiditis n n Acute Chronic
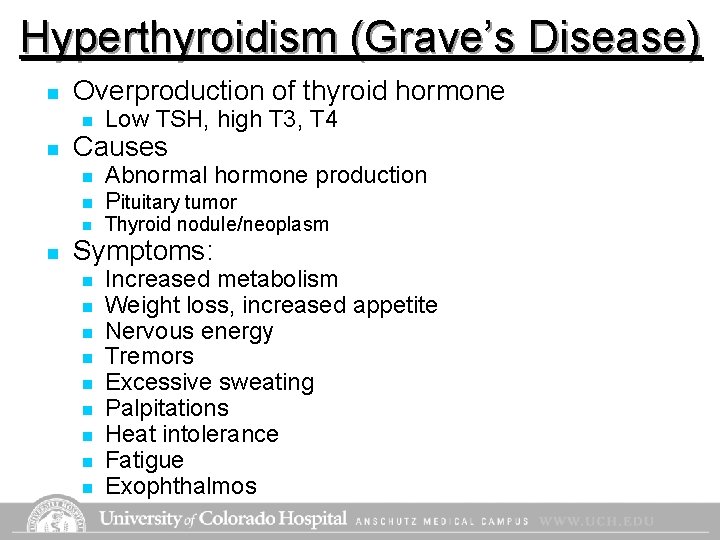
Hyperthyroidism (Grave’s Disease) n Overproduction of thyroid hormone n n Causes n n Low TSH, high T 3, T 4 Abnormal hormone production Pituitary tumor Thyroid nodule/neoplasm Symptoms: n n n n n Increased metabolism Weight loss, increased appetite Nervous energy Tremors Excessive sweating Palpitations Heat intolerance Fatigue Exophthalmos
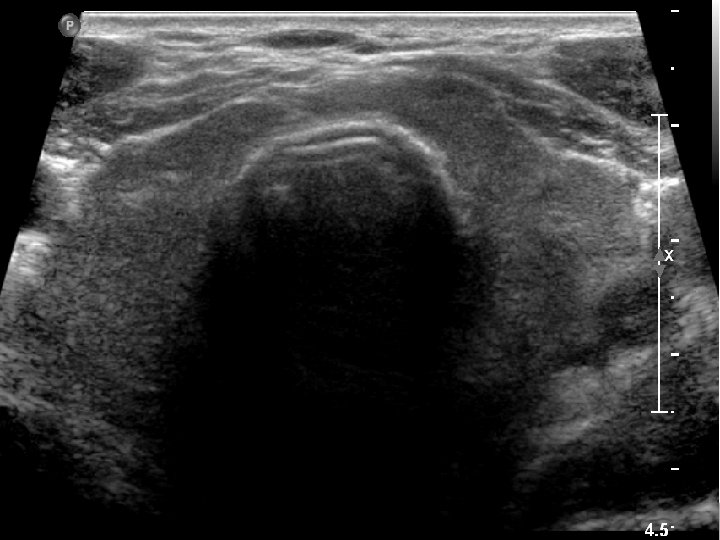
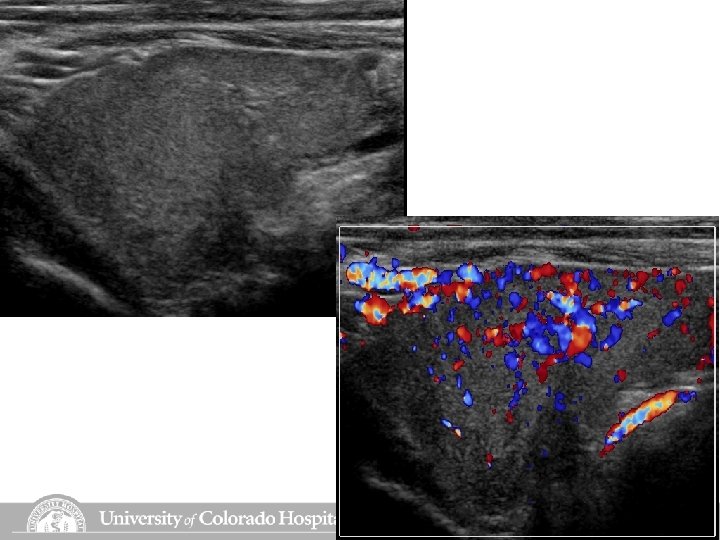
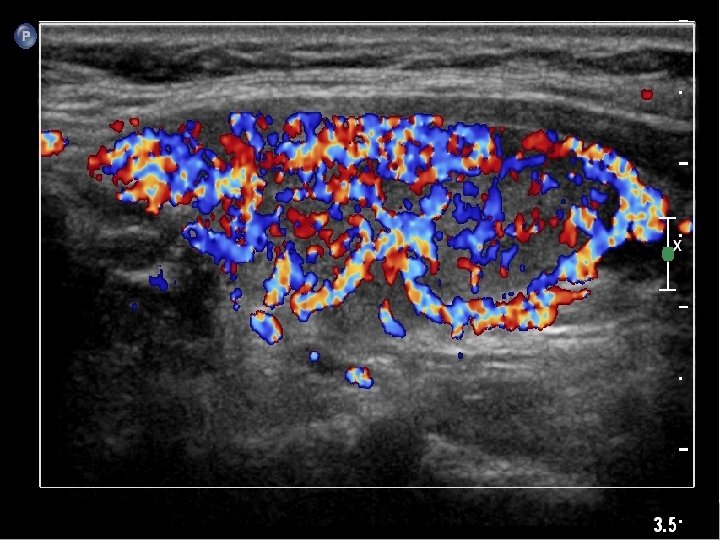
Hyperthyroidism (Grave’s Disease) n Sonographic Appearance: n Enlarged n Heterogeneous n Hypervascular n Treatment: n Radioactive iodine n Medication n Surgery
Hypothyroidism n Under secretion of hormone production n n Causes n n High TSH, low T 3, T 4 Low intake of iodine Thyroid hormone failure Pituitary disease Symptoms: n n n n Weight gain Hair loss Increased tissue around eyes Intellectual and motor slowing Cold intolerance Constipation Deep voice Myxedema (coma, life threatening)
Hypothyroidism n Sonographic appearance n Variable in size and echogencity n Treatment n Medication
Acute/Subacute Thyroiditis n n Acute n Rare, caused by bacterial infection n Painful, firm, enlarged thyroid, may see abscess n Patients have neck swelling, fever, pain Subacute (de Quervain’s Disease) n Diffuse inflammatory disease n Painful enlarged thyroid n Thyroid appears large and hypoechoic
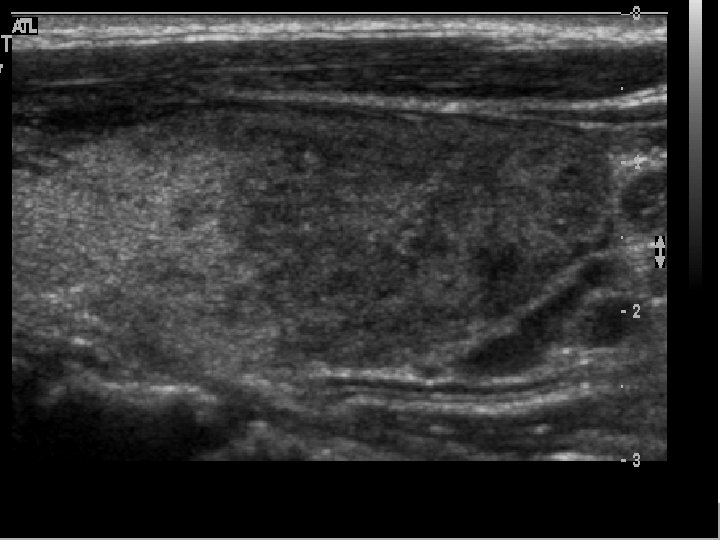
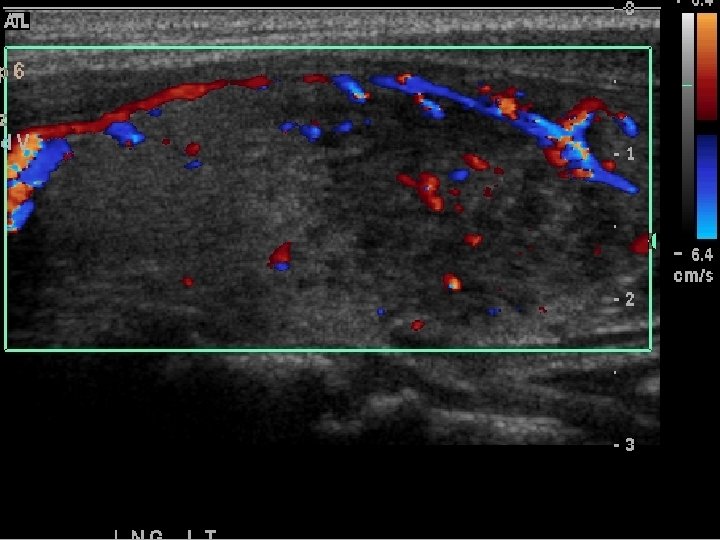
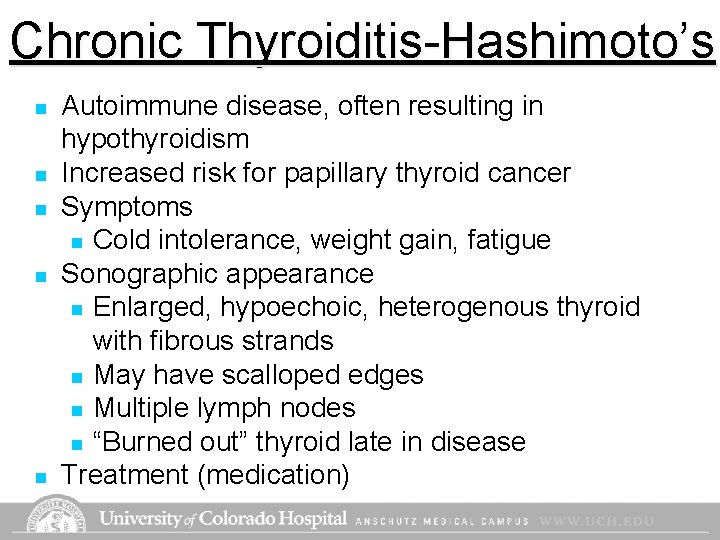
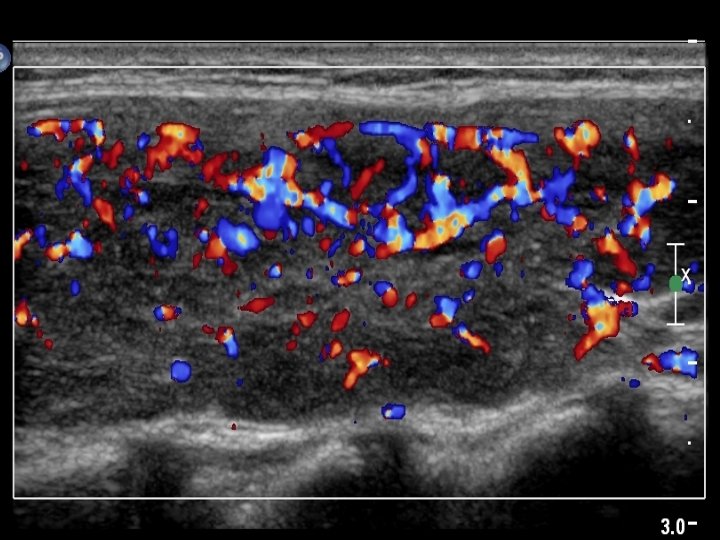
Chronic Thyroiditis-Hashimoto’s n n n Autoimmune disease, often resulting in hypothyroidism Increased risk for papillary thyroid cancer Symptoms n Cold intolerance, weight gain, fatigue Sonographic appearance n Enlarged, hypoechoic, heterogenous thyroid with fibrous strands n May have scalloped edges n Multiple lymph nodes n “Burned out” thyroid late in disease Treatment (medication)
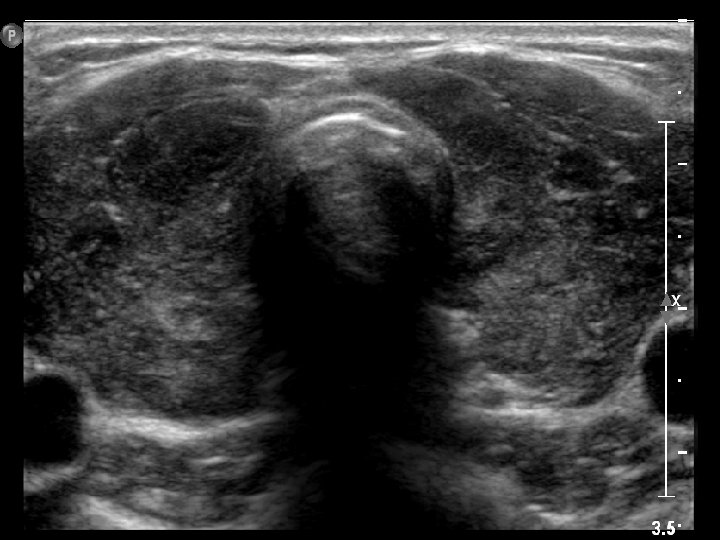
Hashimoto’s Thyroiditis (early)
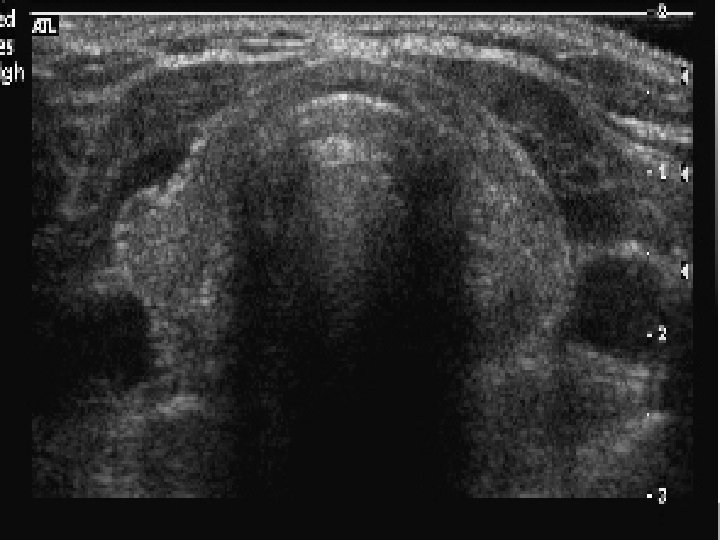
Hashimoto’s Thyroiditis (burn out)
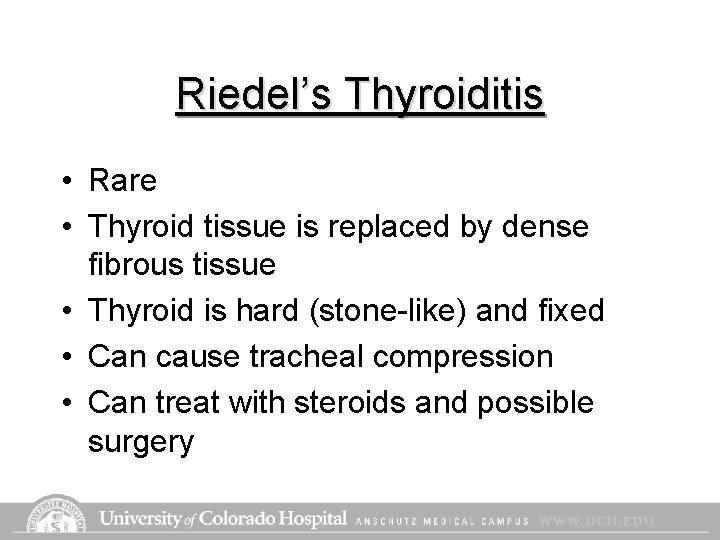
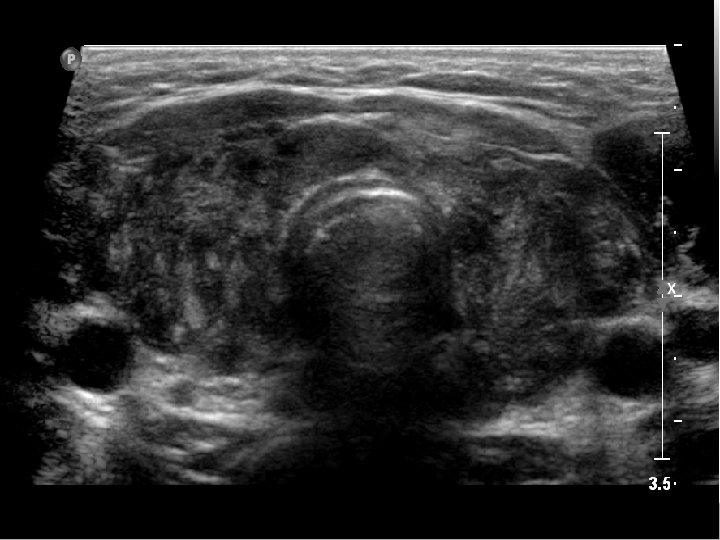
Riedel’s Thyroiditis • Rare • Thyroid tissue is replaced by dense fibrous tissue • Thyroid is hard (stone-like) and fixed • Can cause tracheal compression • Can treat with steroids and possible surgery
Benign Focal Thyroid Pathology n n Colloid Adenomas Goiters Cysts
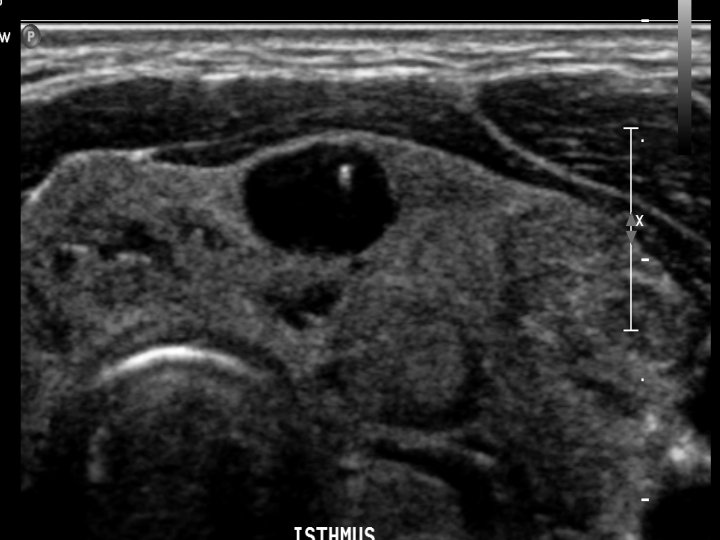
Colloid Nodules • Colloid is product of the thyroid that consists of thyroglobulin and serves as a storage reservoir for thyroid hormones • Reservoirs can form within the thyroid and fill with colloid and colloid crystals • Anechoic with echogenic focus/foci with comet tail artifact • Overwhelmingly benign
Insert colloid pix
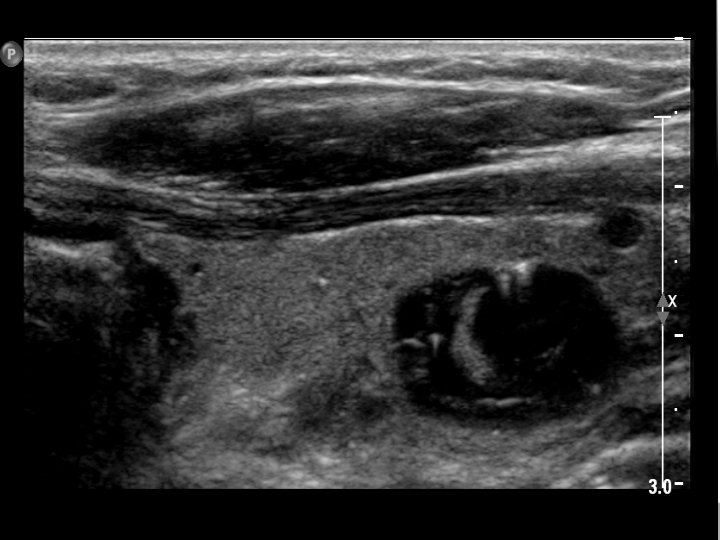
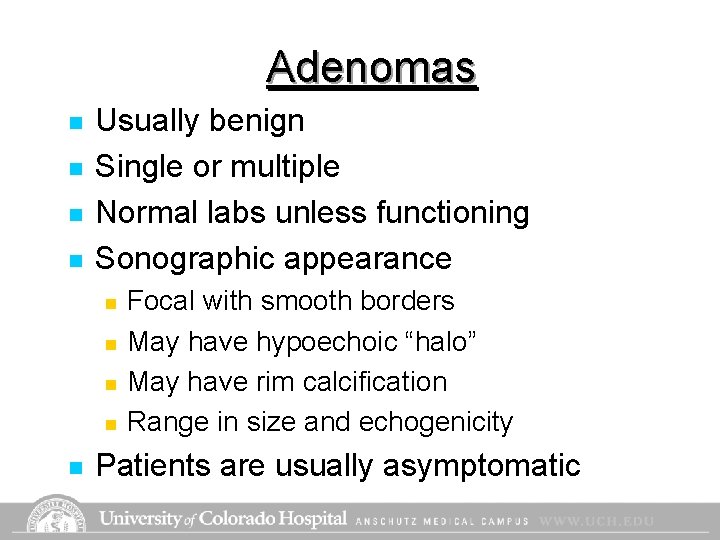
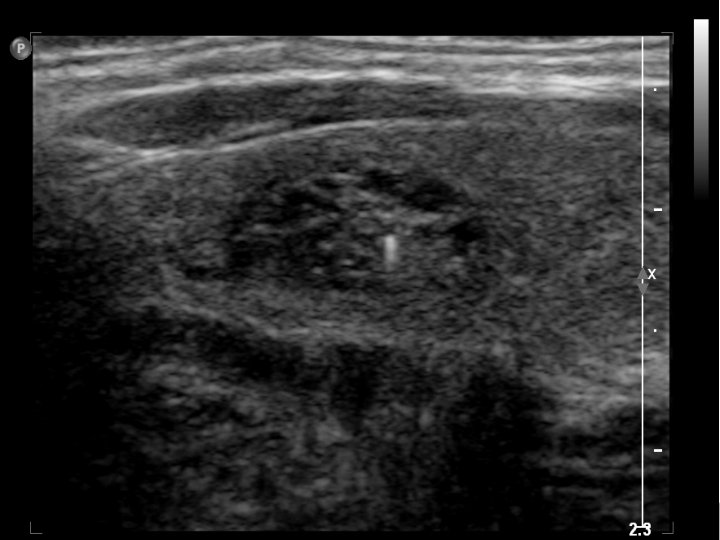
Adenomas n n Usually benign Single or multiple Normal labs unless functioning Sonographic appearance n n n Focal with smooth borders May have hypoechoic “halo” May have rim calcification Range in size and echogenicity Patients are usually asymptomatic
Adenoma
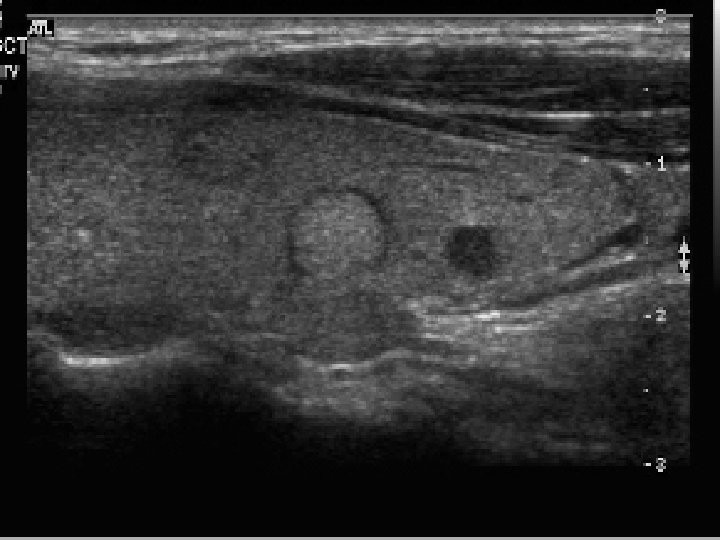
Goiter n n Thyroid is enlarged (can have neck tightness difficulty swallowing) Causes: n n n Iodine deficiency Hereditary Medications Can be associated with Graves disease Toxic vs Non Toxic Goiter: n n Toxic: Nodules are functioning, causing changes in lab values Non Toxic: non functioning
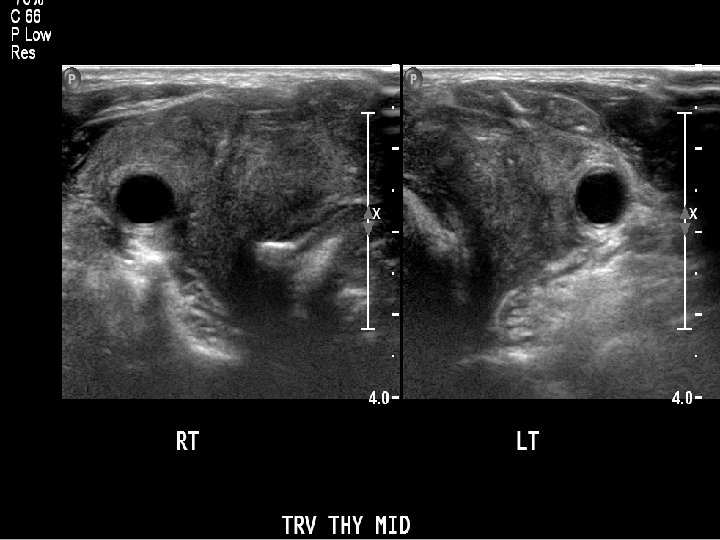
Goiter n Sonographic appearance n n Multiple nodules Nodules vary in size and echogenicity Heterogeneous gland Treatment & Symptoms depend on thyroid size and hormone levels

Goiter

Cysts n n n True cysts are uncommon Cystic appearing lesions are usually degenerating adenomas or colloid nodules Sonographic appearance: n n n display cystic characteristics may have internal echoes and irregular walls Alcohol ablation is a treatment option

Cysts
Malignant Pathology n n n n Papillary Carcinoma Follicular Carcinoma Medullary Carcinoma Huthle Cell Carcinoma Anaplastic Carcinoma (Giant Cell) Lymphoma Metastasis to Thyroid
Papillary Carcinoma n n n Most common type of thyroid cancer Cause usually unknown, but more common in females Symptoms: n Palpable nodule n Asymptomatic n Thyroid hormones can be normal or abnormal Slow growing, least aggressive thyroid cancer Spreads through lymphatic system
Papillary Carcinoma n n Sonographic appearance n One or multiple nodules with irregular borders n Typically hypoechoic, but can vary n Microcalcifications (strong sign) n Increased internal vascularity n May see multiple central or lateral lymph nodes Treatment

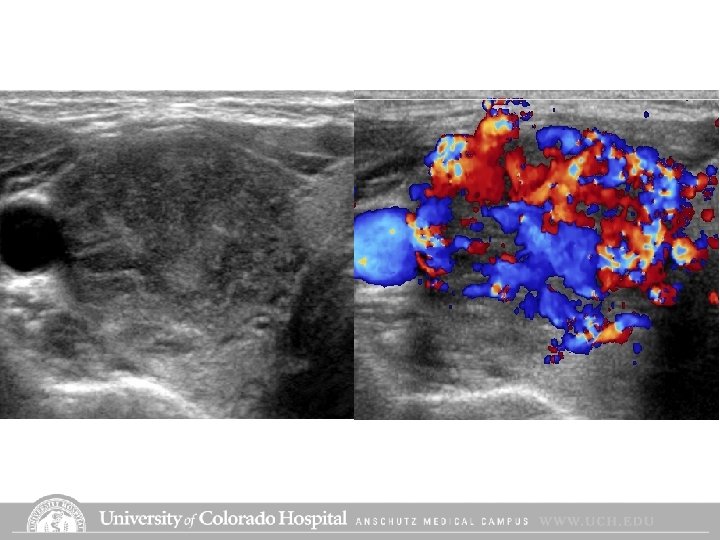

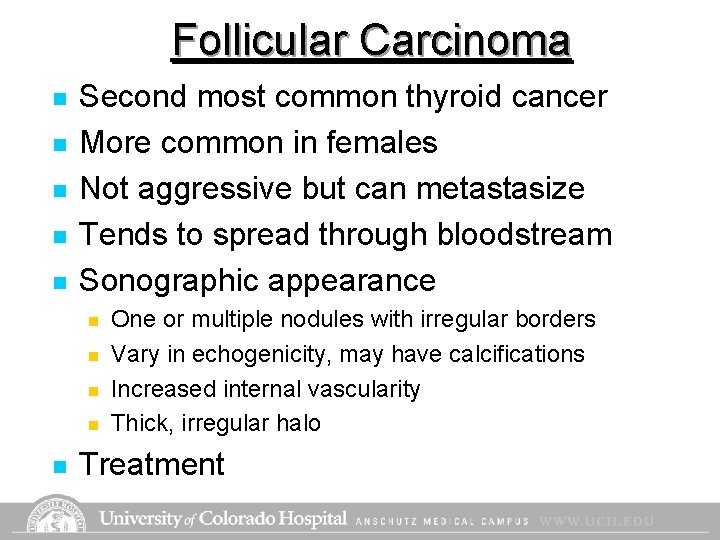
Follicular Carcinoma n n n Second most common thyroid cancer More common in females Not aggressive but can metastasize Tends to spread through bloodstream Sonographic appearance n n n One or multiple nodules with irregular borders Vary in echogenicity, may have calcifications Increased internal vascularity Thick, irregular halo Treatment

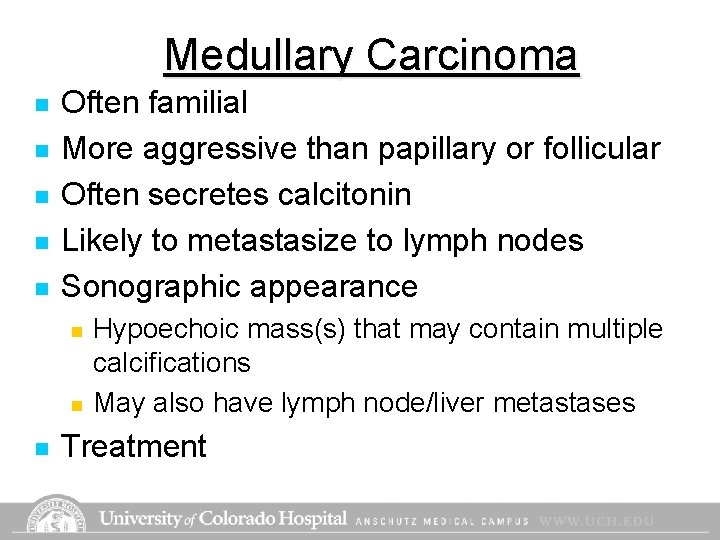
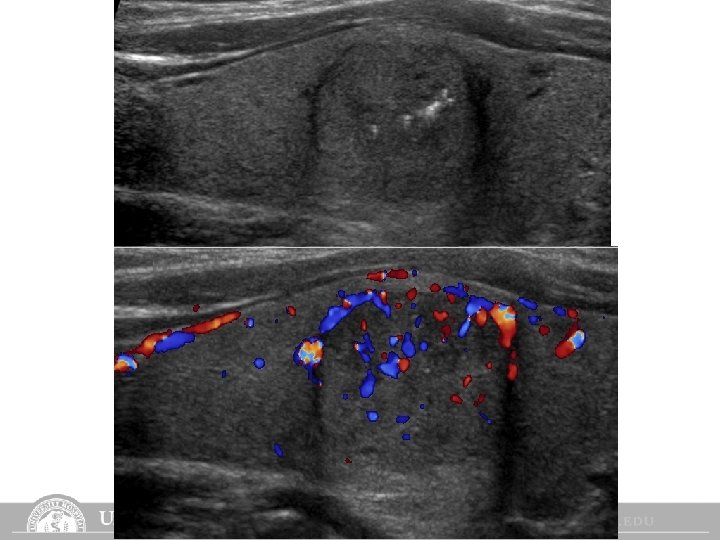
Medullary Carcinoma n n n Often familial More aggressive than papillary or follicular Often secretes calcitonin Likely to metastasize to lymph nodes Sonographic appearance n n n Hypoechoic mass(s) that may contain multiple calcifications May also have lymph node/liver metastases Treatment
Hurthle Cell n n Uncommon Not aggressive but likely to metastasize (nodes, blood, lungs, bone) Sonographic appearance is variable Treatment
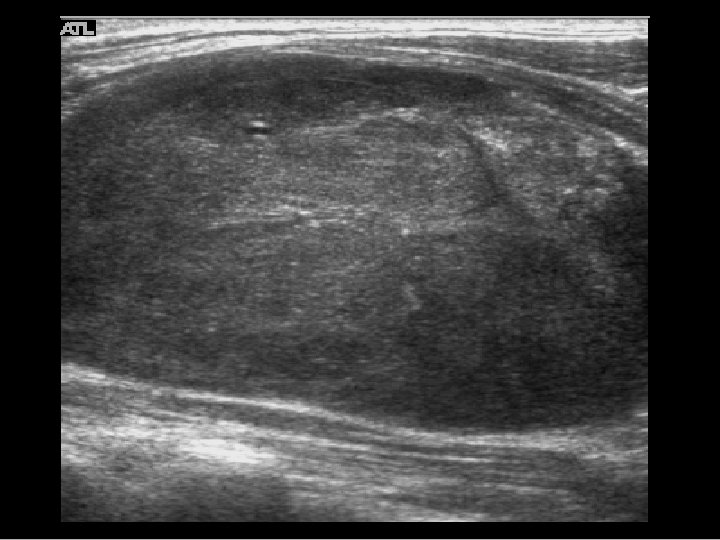
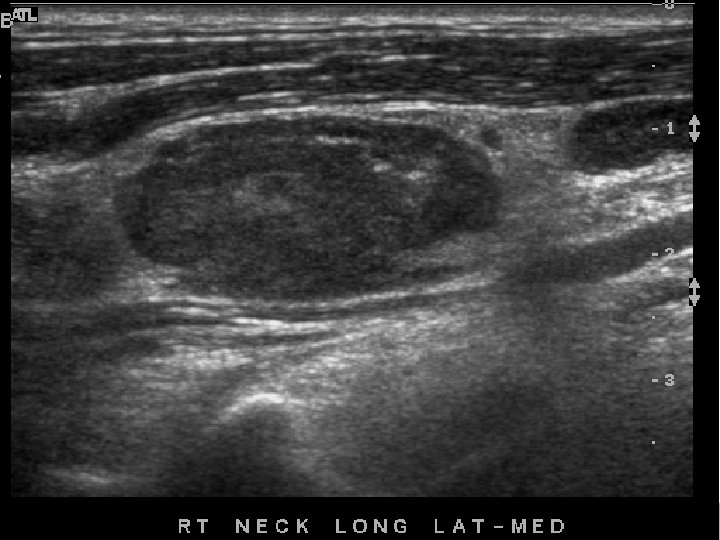
Anaplastic (Giant cell) n n n Least common, most aggressive, most lethal Neck is tender, mass is hard and fixed Rapidly growing Invades neck muscles, vessels, trachea Sonographic appearance n n large hypoechoic mass Treatment
Lymphoma • Typically non-Hodgkin’s type • Rapidly growing, hypoechoic, lobulated mass • Prognosis varies depending on stage
Metastsis to Thyroid n n Typically from melanoma, breast and renal cell Primary is typically diagnosed Patients feels neck fullness, palpable mass Sonographic appearance n Solid, homogeneous, hypoechoic without calcifications
Parathyroid Glands n n n Anatomy Hormones Pathology n n n Adenomas Hypoparathyroidism Hyperparathyroidism primary n secondary n
Parathyroid Anatomy n Four parathyroid glands n n n Normal glands are small n n 2 superior 2 inferior (more variable in location) 1 x 3 x 5 mm Function n Produce parathyroid hormone which regulates blood calcium levels
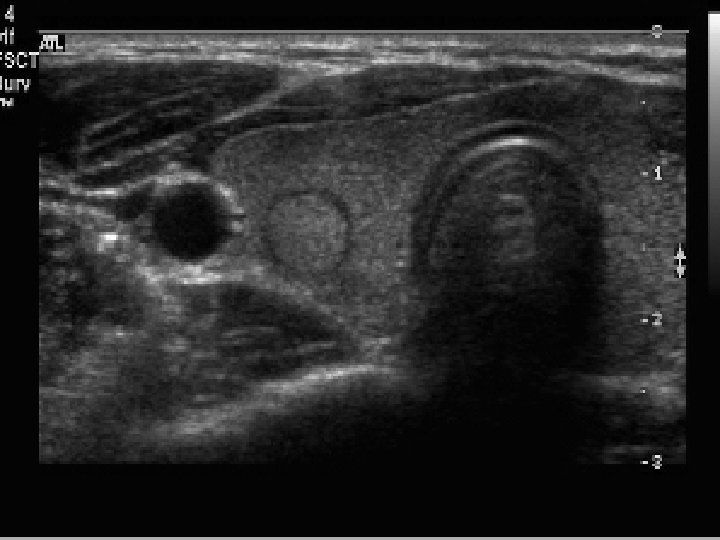
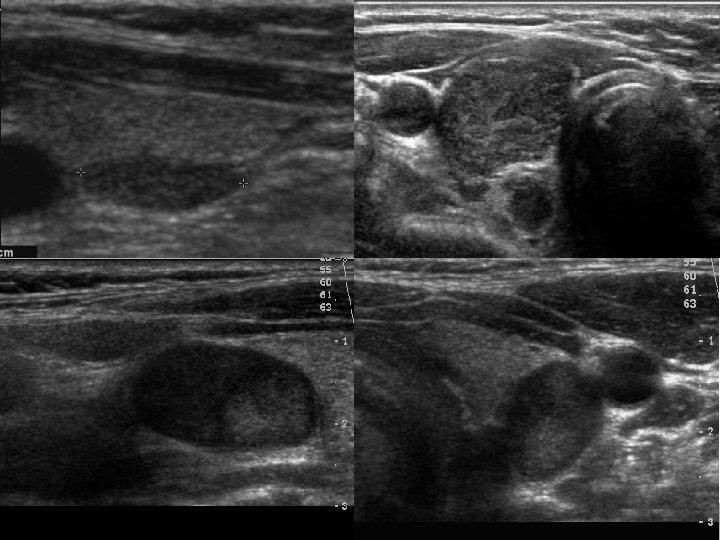
Parathyroid Adenomas n n Typically just one gland is affected Sonographic appearance n n enlarged round homogeneous and hypoechoic Treatment
Hypoparathyroidism n n n Post thyroidectomy complication Clinical diagnosis Symptoms: Numbness at mouth, then into extremities n Seizures n Cardiac arrhythmias/arrest n n n Temporary or chronic Treatment: n Calcium and Vitamin D supplements (IV and oral)

Primary Hyperparathyroidism n Usually caused by functioning adenomas High calcium levels during routine lab work n Symptoms: n n n Sonographic appearance n n Often asymptomatic Can develop fatigue, depression, weakness Severe symptoms: constipation, confusion, painful bones, renal stones Enlarged Round Homogeneous and hypoechoic Treatment

Secondary Hyperparathyroidism n Found in patients with chronic renal failure n n Sonographic appearance n n unable to produce vitamin D leading to decrease in calcium levels. More parathyroid hormone is produced trying to increase calcium levels enlarged parathyroids, often bilateral Uncommon (due to the success of dialysis)
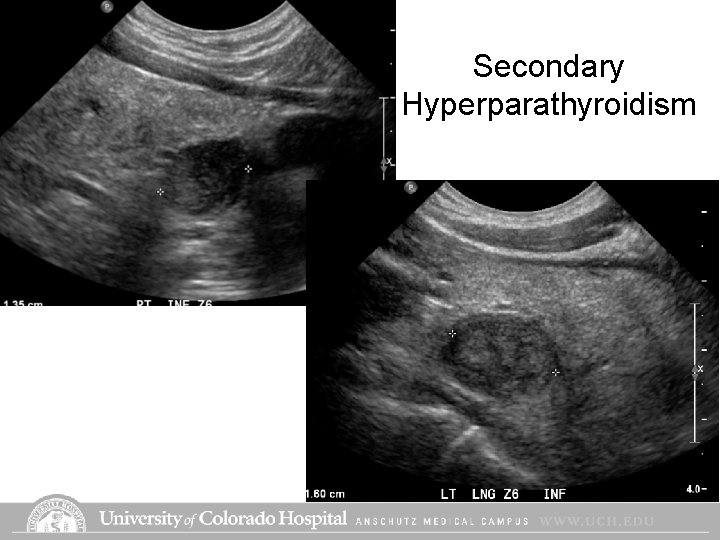
Secondary Hyperparathyroidism
Salivary Glands n Location n n Parotid Submandibular Sublingual Appearance Pathology
Salivary Glands • Parotid – Anterior to ear, largest gland, triangular • Submandibular – Deep to mandible • Sublingual – Under tongue, small, not seen well by ultrasound • Sonographic appearance – Homogeneous and echogenic


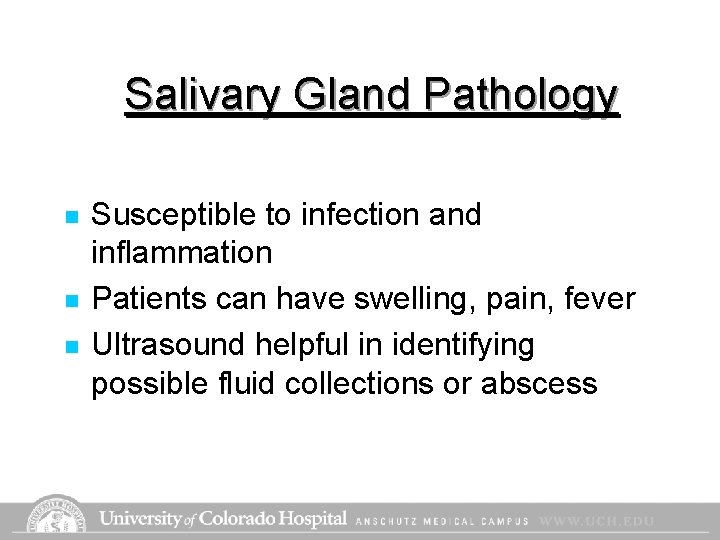
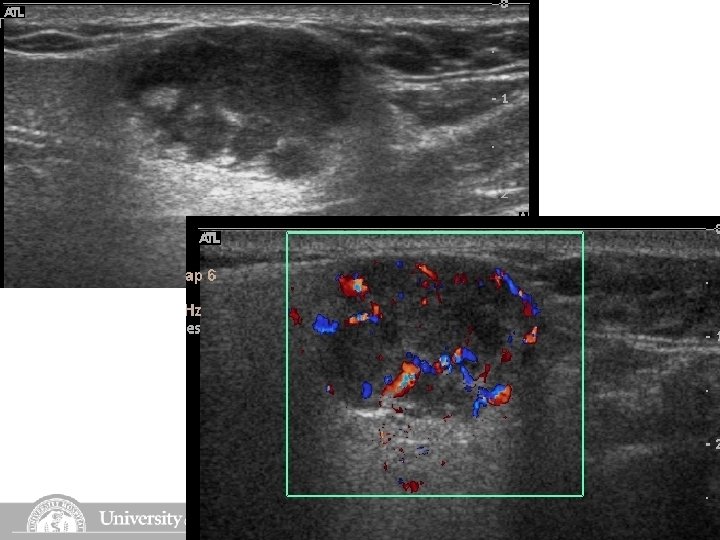
Salivary Gland Pathology n n n Susceptible to infection and inflammation Patients can have swelling, pain, fever Ultrasound helpful in identifying possible fluid collections or abscess
Other Neck Lesions n n n Thyroglossal Duct Cyst Branchial Cleft Cyst Carotid Body Tumor
Thyroglossal Duct Cyst n n Congenital anomaly Located midline, anterior to trachea More commonly seen in children Sonographic appearance n n n Anechoic to hypoechoic Can contain debris or fluid level Treatment
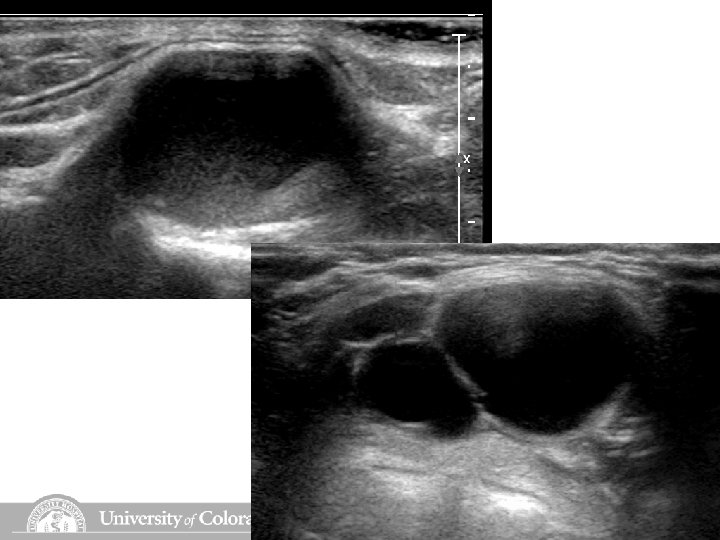
Branchial Cleft Cyst n n n Fetal remnant Located slightly to the right or left of midline and anterior to the sternocleidomastoid Sonographic appearance n n n Anechoic to hypoechoic Can contain debris or fluid level Treatment

Carotid Body Tumor/Paraganglioma n n Rare, typically benign, slow growing Usually unilateral, located at carotid bifurcation, and fed by the ECA Patients feel neck mass or have a sudden change in blood pressure Sonographic appearance n n n Round, smooth borders Typically hypervascular Treatment

Carotid Body Tumor
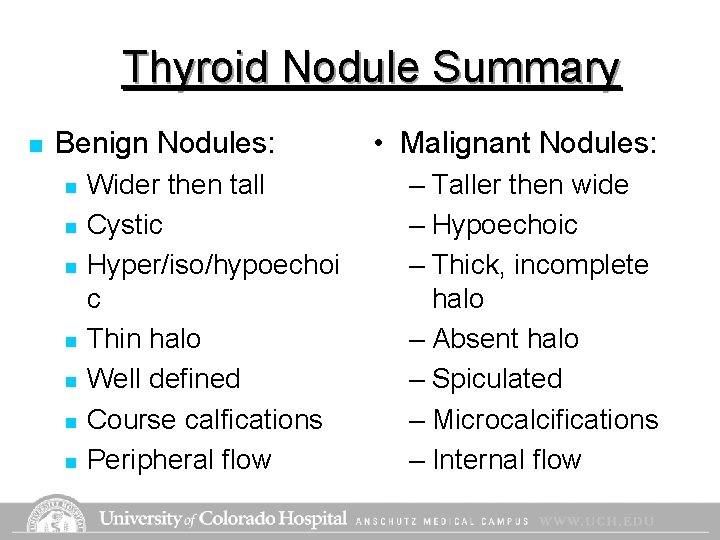
Thyroid Nodule Summary n Benign Nodules: n n n n Wider then tall Cystic Hyper/iso/hypoechoi c Thin halo Well defined Course calfications Peripheral flow • Malignant Nodules: – Taller then wide – Hypoechoic – Thick, incomplete halo – Absent halo – Spiculated – Microcalcifications – Internal flow
- Slides: 91