Anatomy of the Eye Retina Optics Central Visual
- Slides: 51
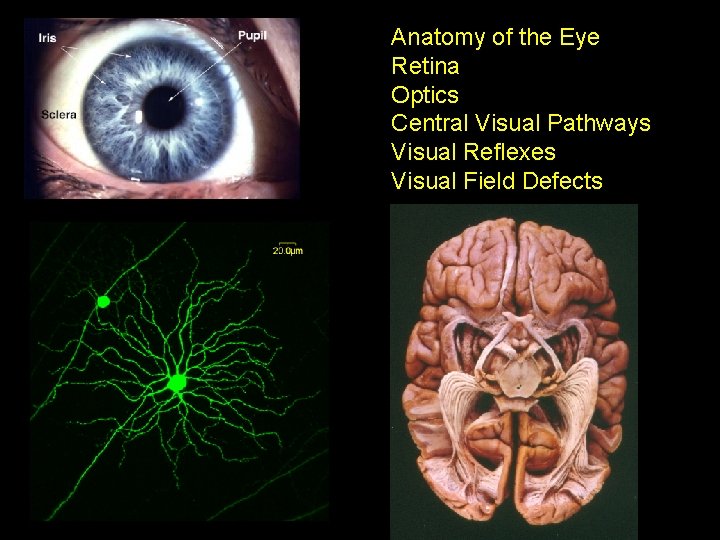
Anatomy of the Eye Retina Optics Central Visual Pathways Visual Reflexes Visual Field Defects
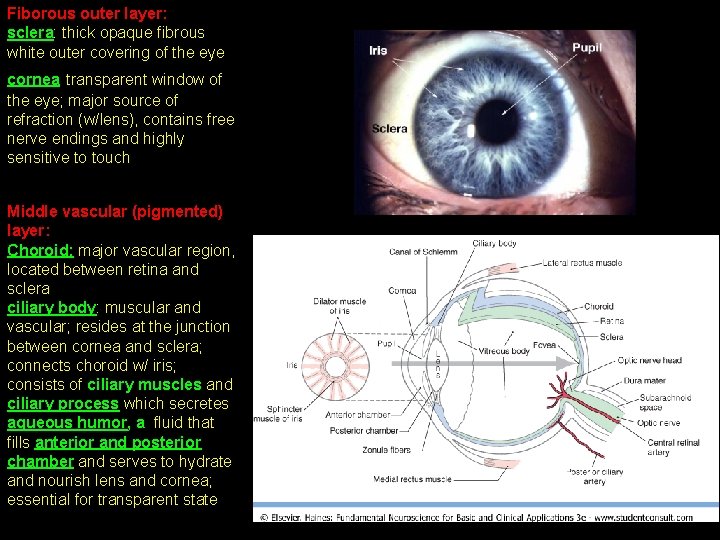
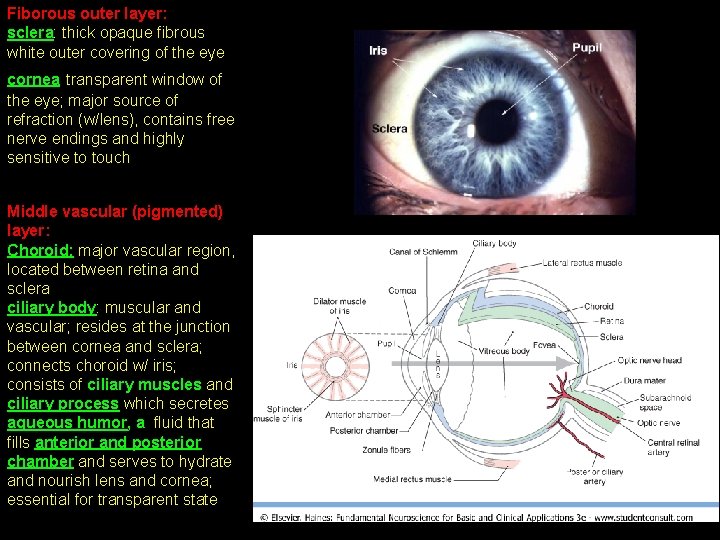
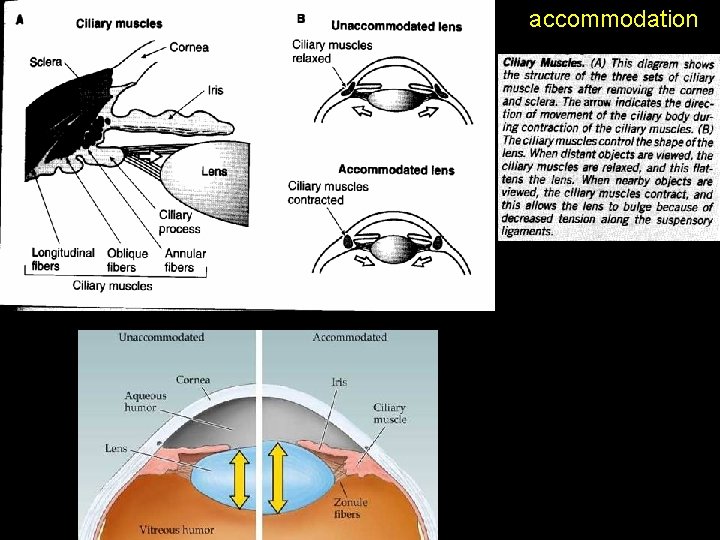
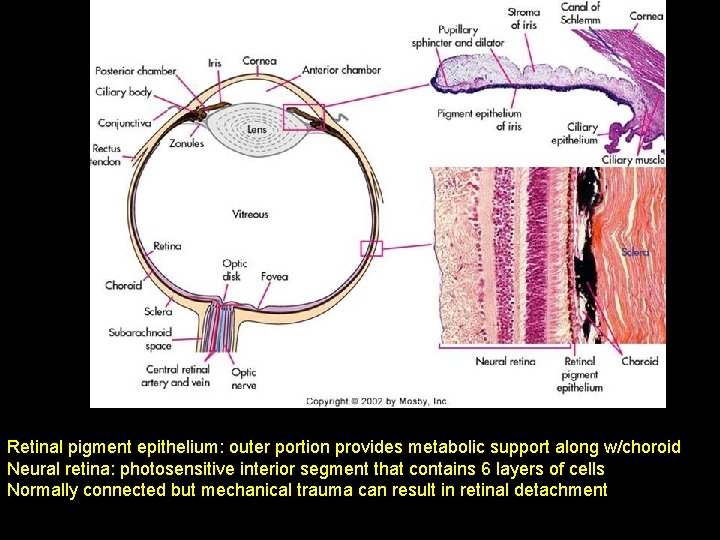
Fiborous outer layer: sclera: thick opaque fibrous white outer covering of the eye cornea transparent window of the eye; major source of refraction (w/lens), contains free nerve endings and highly sensitive to touch Middle vascular (pigmented) layer: Choroid: major vascular region, located between retina and sclera ciliary body: muscular and vascular; resides at the junction between cornea and sclera; connects choroid w/ iris; consists of ciliary muscles and ciliary process which secretes aqueous humor, a fluid that fills anterior and posterior chamber and serves to hydrate and nourish lens and cornea; essential for transparent state
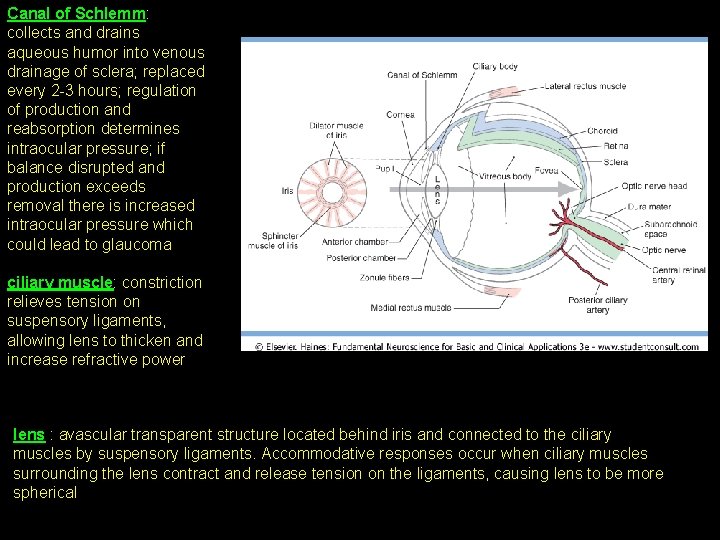
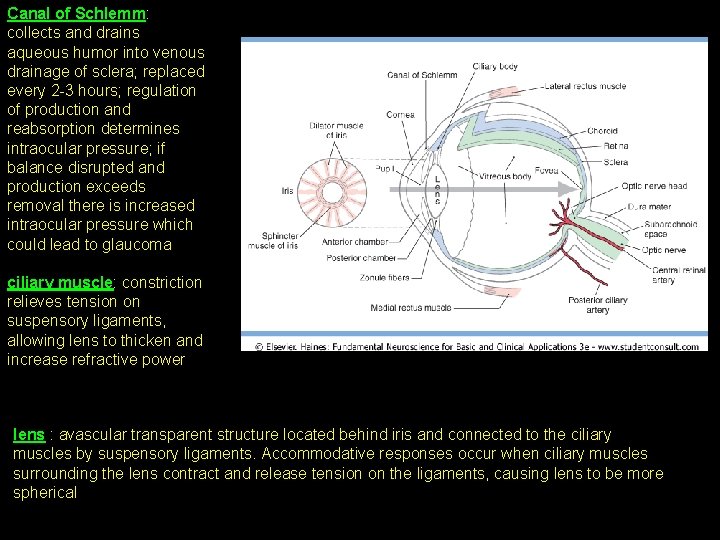
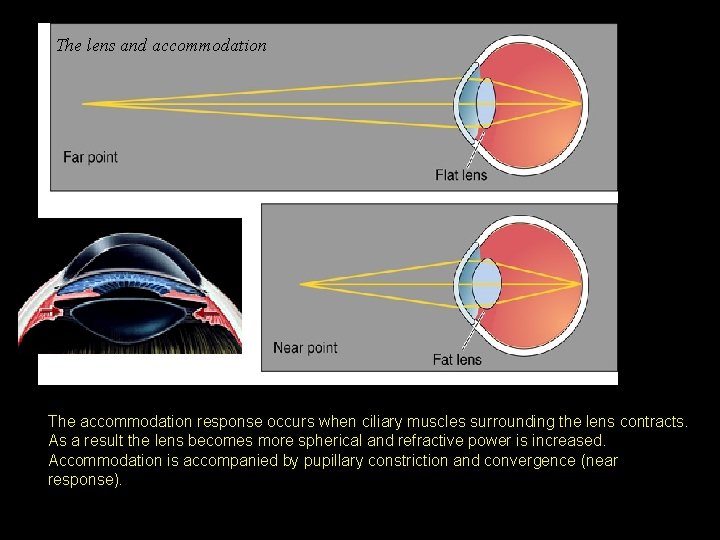
Canal of Schlemm: collects and drains aqueous humor into venous drainage of sclera; replaced every 2 -3 hours; regulation of production and reabsorption determines intraocular pressure; if balance disrupted and production exceeds removal there is increased intraocular pressure which could lead to glaucoma ciliary muscle: constriction relieves tension on suspensory ligaments, allowing lens to thicken and increase refractive power lens : avascular transparent structure located behind iris and connected to the ciliary muscles by suspensory ligaments. Accommodative responses occur when ciliary muscles surrounding the lens contract and release tension on the ligaments, causing lens to be more spherical
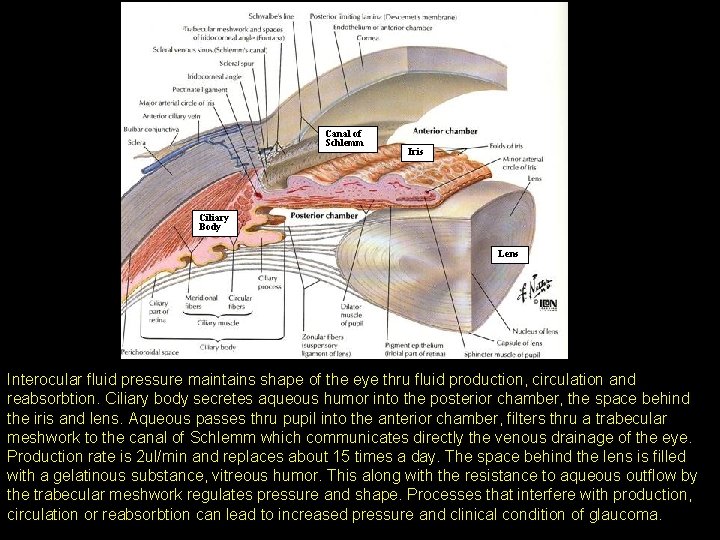
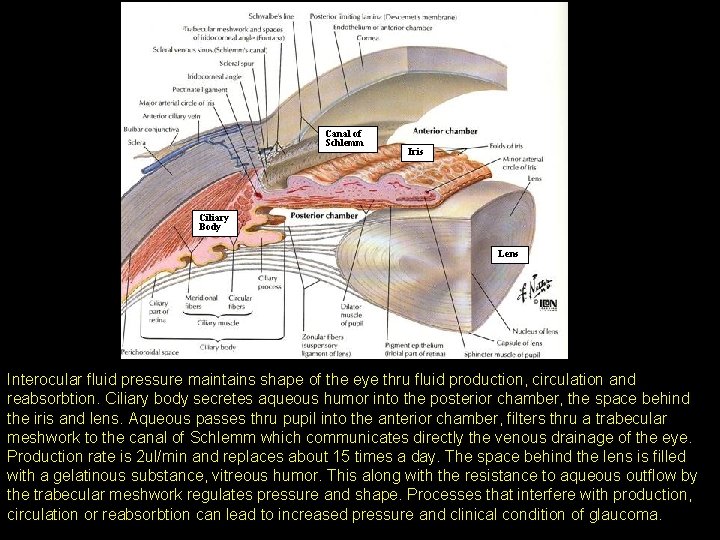
Canal of Schlemm Iris Ciliary Body Lens Interocular fluid pressure maintains shape of the eye thru fluid production, circulation and reabsorbtion. Ciliary body secretes aqueous humor into the posterior chamber, the space behind the iris and lens. Aqueous passes thru pupil into the anterior chamber, filters thru a trabecular meshwork to the canal of Schlemm which communicates directly the venous drainage of the eye. Production rate is 2 ul/min and replaces about 15 times a day. The space behind the lens is filled with a gelatinous substance, vitreous humor. This along with the resistance to aqueous outflow by the trabecular meshwork regulates pressure and shape. Processes that interfere with production, circulation or reabsorbtion can lead to increased pressure and clinical condition of glaucoma.
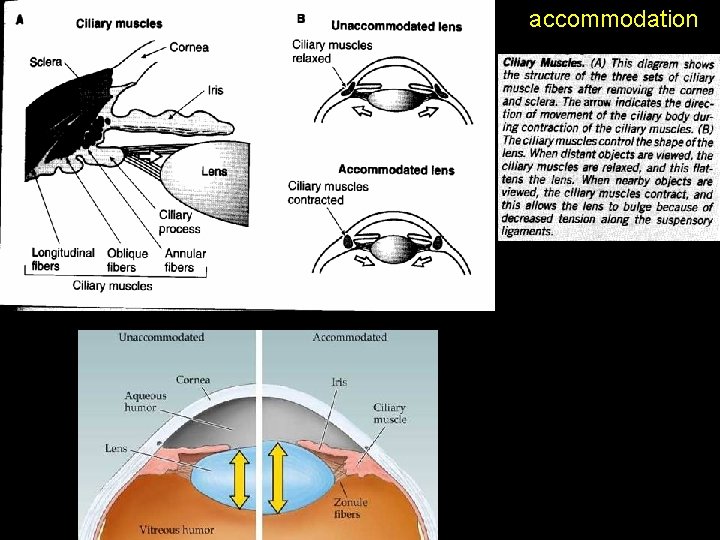
accommodation
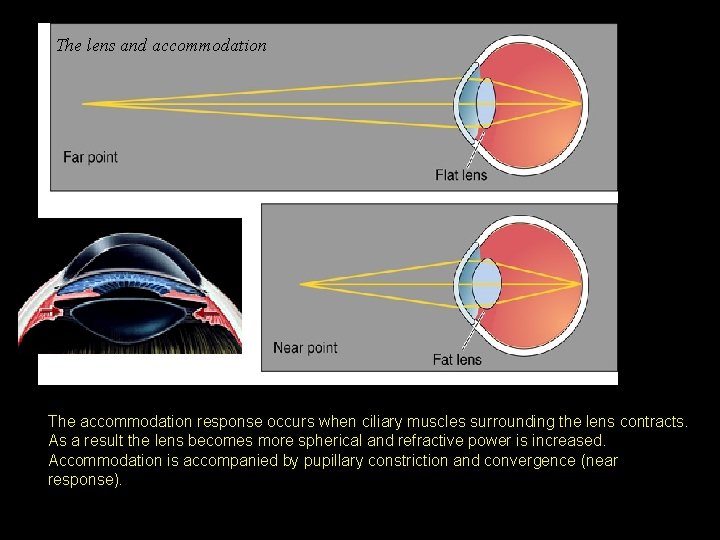
The lens and accommodation The accommodation response occurs when ciliary muscles surrounding the lens contracts. As a result the lens becomes more spherical and refractive power is increased. Accommodation is accompanied by pupillary constriction and convergence (near response).
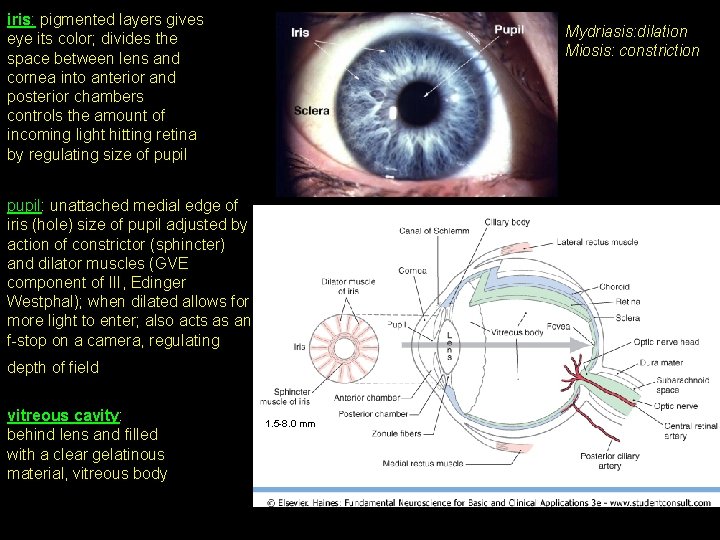
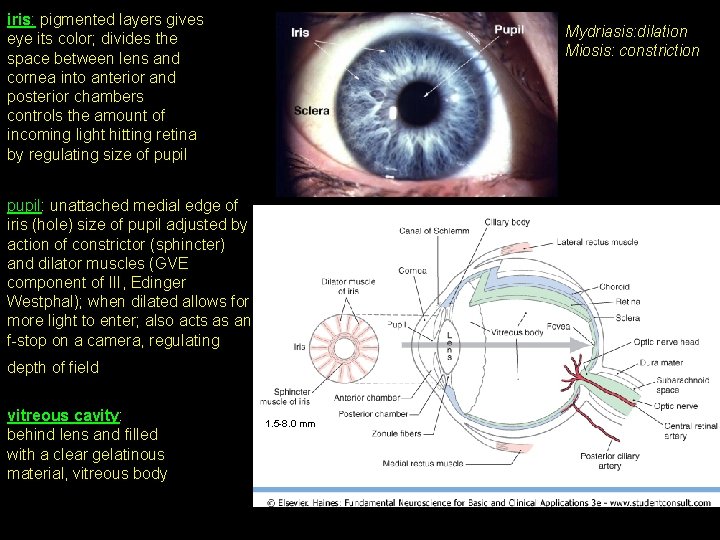
iris: pigmented layers gives eye its color; divides the space between lens and cornea into anterior and posterior chambers controls the amount of incoming light hitting retina by regulating size of pupil Mydriasis: dilation Miosis: constriction pupil: unattached medial edge of iris (hole) size of pupil adjusted by action of constrictor (sphincter) and dilator muscles (GVE component of III, Edinger Westphal); when dilated allows for more light to enter; also acts as an f-stop on a camera, regulating depth of field vitreous cavity: behind lens and filled with a clear gelatinous material, vitreous body 1. 5 -8. 0 mm
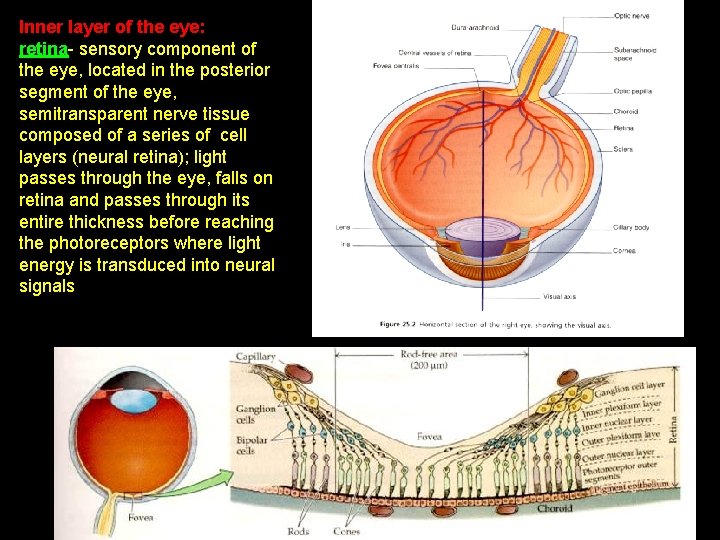
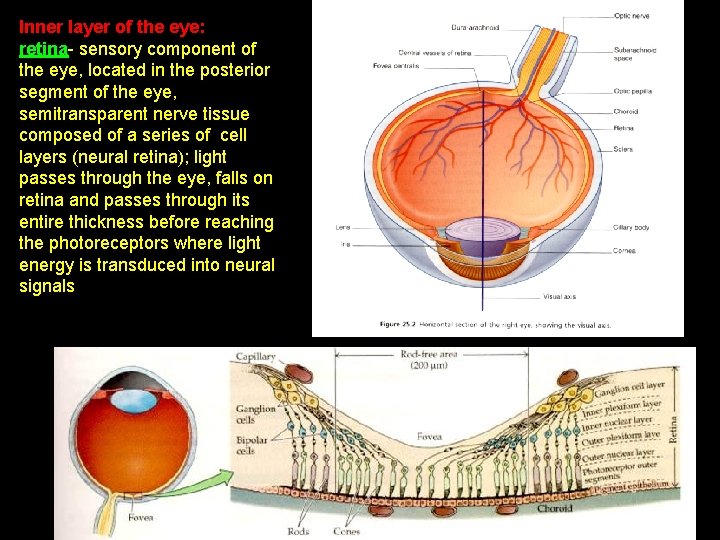
Inner layer of the eye: retina- sensory component of the eye, located in the posterior segment of the eye, semitransparent nerve tissue composed of a series of cell layers (neural retina); light passes through the eye, falls on retina and passes through its entire thickness before reaching the photoreceptors where light energy is transduced into neural signals
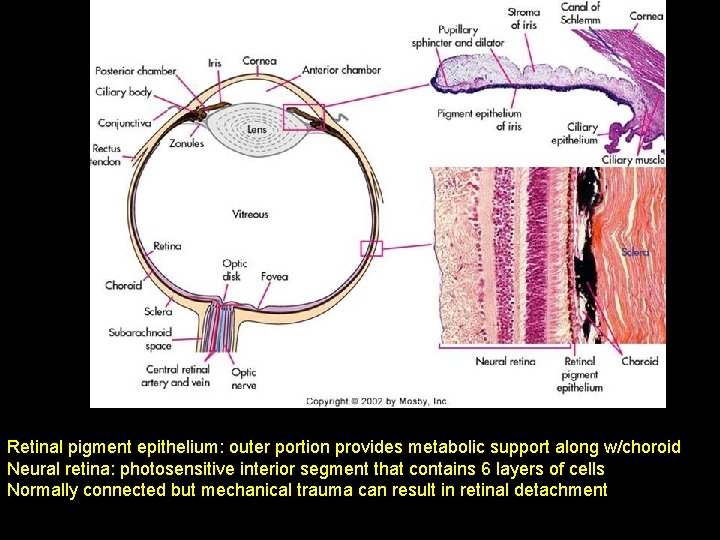
Retinal pigment epithelium: outer portion provides metabolic support along w/choroid Neural retina: photosensitive interior segment that contains 6 layers of cells Normally connected but mechanical trauma can result in retinal detachment
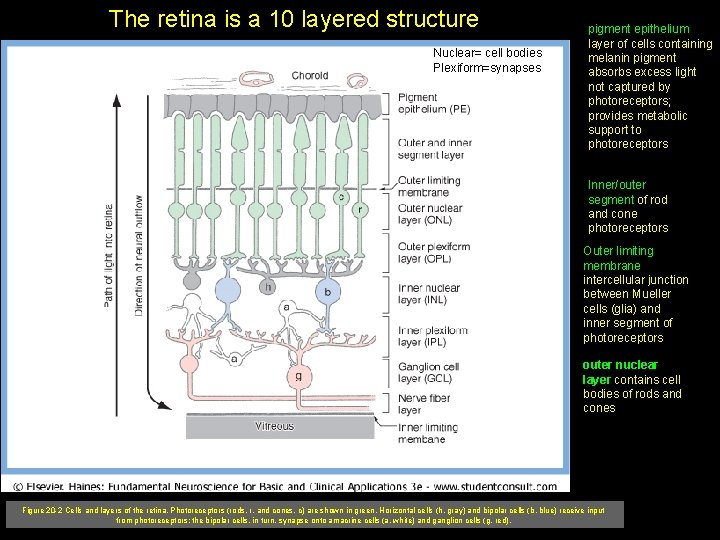
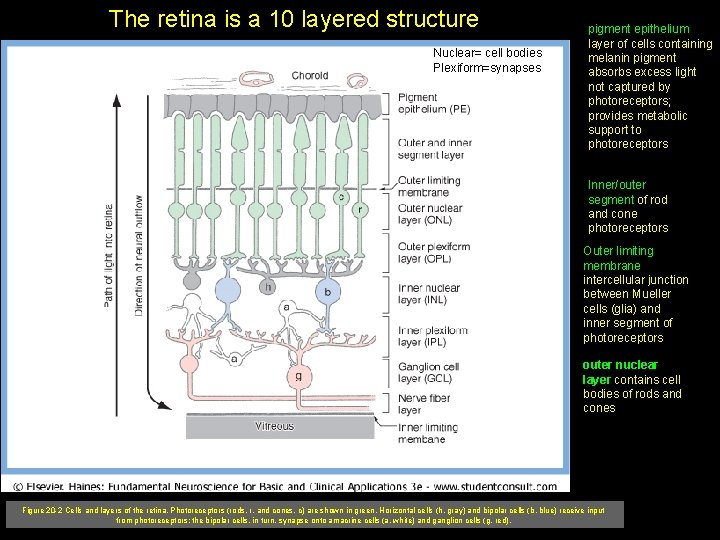
The retina is a 10 layered structure Nuclear= cell bodies Plexiform=synapses pigment epithelium layer of cells containing melanin pigment absorbs excess light not captured by photoreceptors; provides metabolic support to photoreceptors Inner/outer segment of rod and cone photoreceptors Outer limiting membrane intercellular junction between Mueller cells (glia) and inner segment of photoreceptors outer nuclear layer contains cell bodies of rods and cones Figure 20 -2 Cells and layers of the retina. Photoreceptors (rods, r, and cones, c) are shown in green. Horizontal cells (h, gray) and bipolar cells (b, blue) receive input from photoreceptors; the bipolar cells, in turn, synapse onto amacrine cells (a, white) and ganglion cells (g, red).
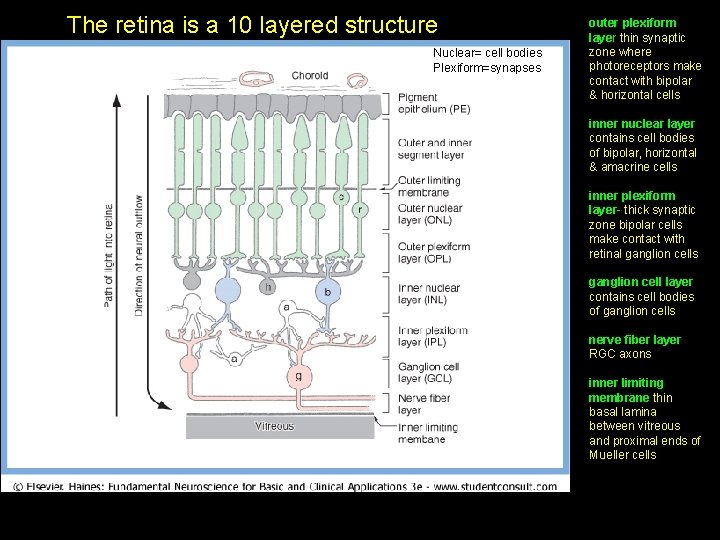
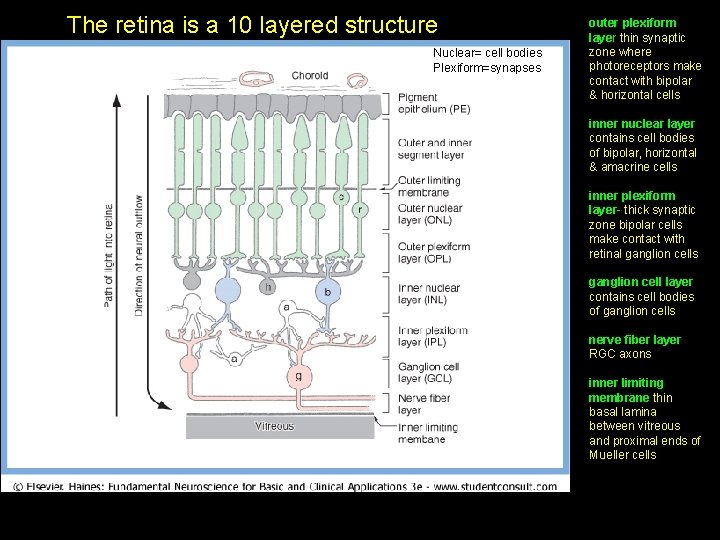
The retina is a 10 layered structure Nuclear= cell bodies Plexiform=synapses outer plexiform layer thin synaptic zone where photoreceptors make contact with bipolar & horizontal cells inner nuclear layer contains cell bodies of bipolar, horizontal & amacrine cells inner plexiform layer- thick synaptic zone bipolar cells make contact with retinal ganglion cells ganglion cell layer contains cell bodies of ganglion cells nerve fiber layer RGC axons inner limiting membrane thin basal lamina between vitreous and proximal ends of Mueller cells
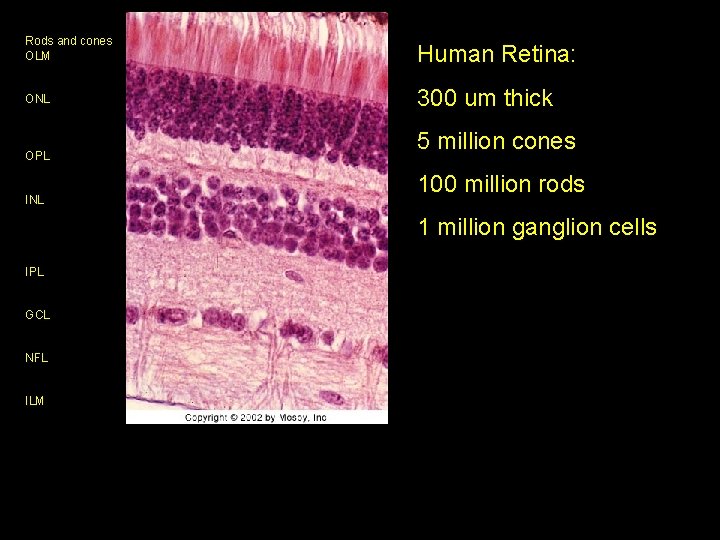
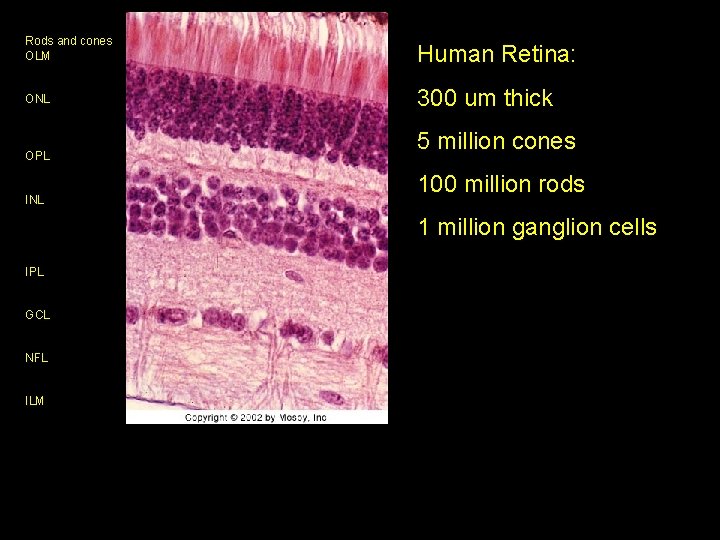
Rods and cones OLM Human Retina: ONL 300 um thick OPL INL 5 million cones 100 million rods 1 million ganglion cells IPL GCL NFL ILM
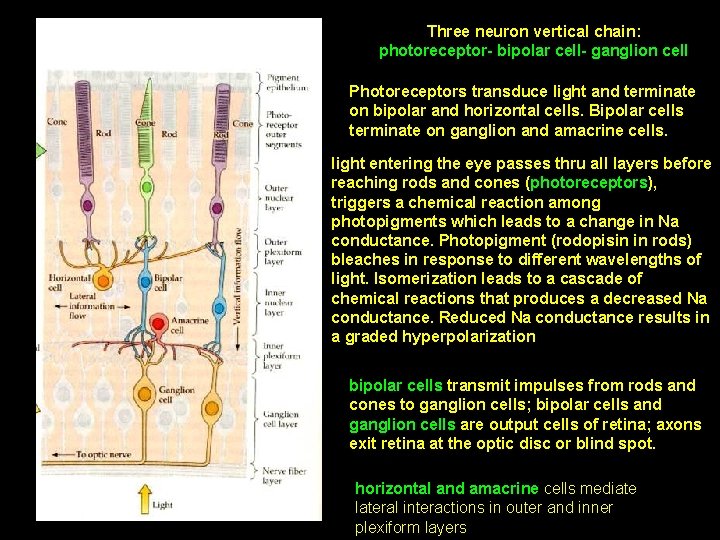
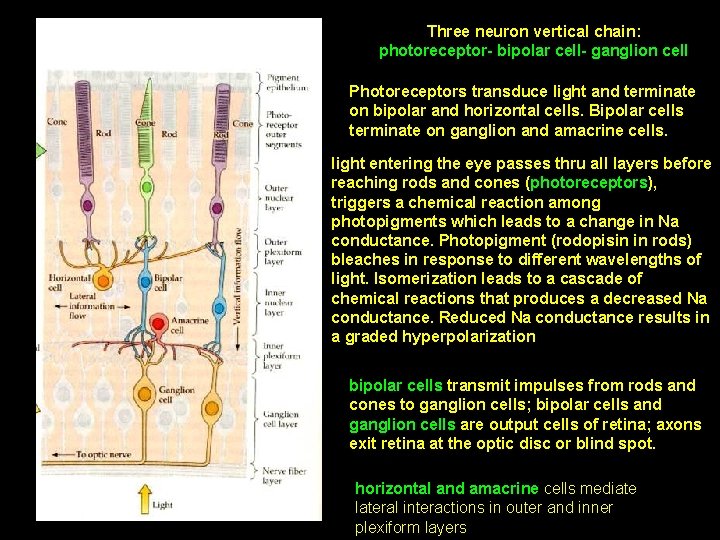
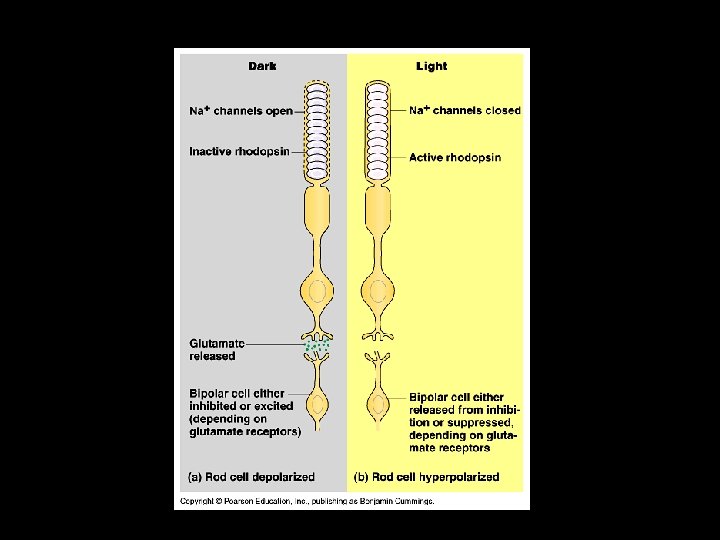
Three neuron vertical chain: photoreceptor- bipolar cell- ganglion cell Photoreceptors transduce light and terminate on bipolar and horizontal cells. Bipolar cells terminate on ganglion and amacrine cells. light entering the eye passes thru all layers before reaching rods and cones (photoreceptors), triggers a chemical reaction among photopigments which leads to a change in Na conductance. Photopigment (rodopisin in rods) bleaches in response to different wavelengths of light. Isomerization leads to a cascade of chemical reactions that produces a decreased Na conductance. Reduced Na conductance results in a graded hyperpolarization bipolar cells transmit impulses from rods and cones to ganglion cells; bipolar cells and ganglion cells are output cells of retina; axons exit retina at the optic disc or blind spot. horizontal and amacrine cells mediate lateral interactions in outer and inner plexiform layers
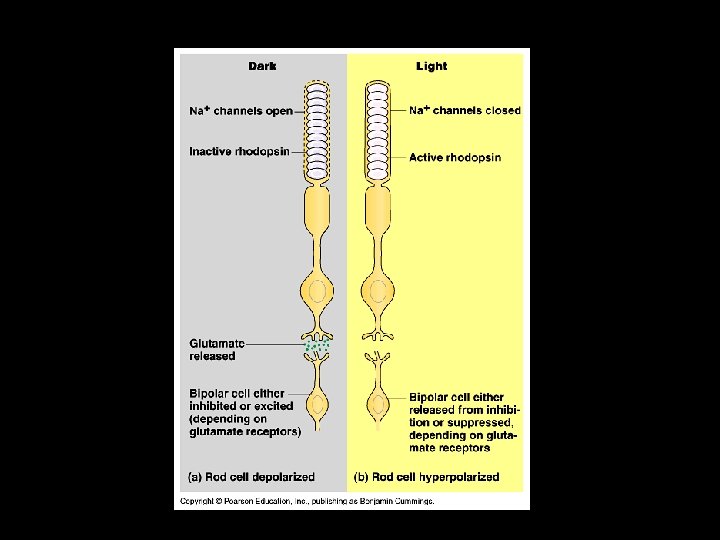
3 -Phototransduction
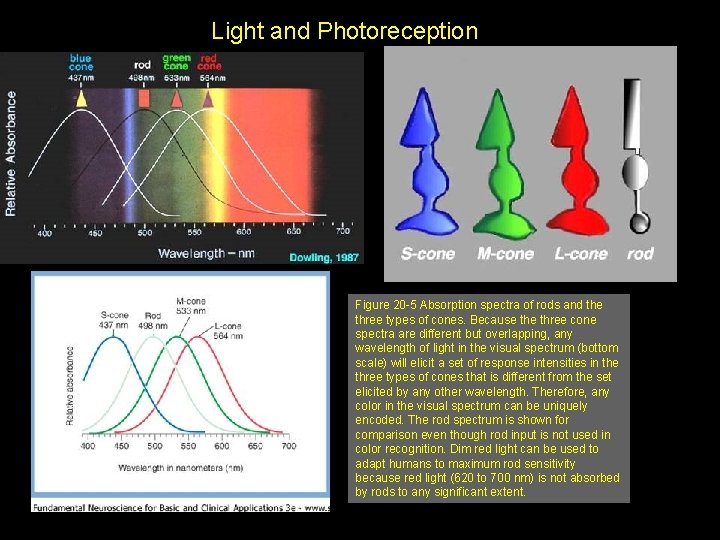
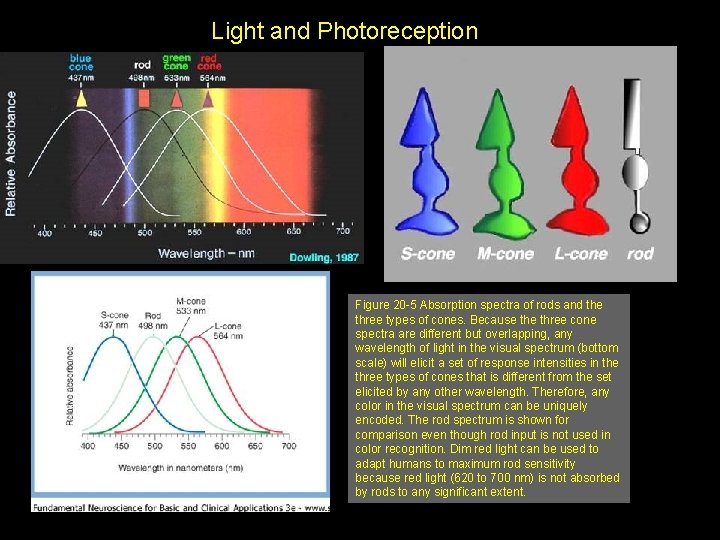
Light and Photoreception Figure 20 -5 Absorption spectra of rods and the three types of cones. Because three cone spectra are different but overlapping, any wavelength of light in the visual spectrum (bottom scale) will elicit a set of response intensities in the three types of cones that is different from the set elicited by any other wavelength. Therefore, any color in the visual spectrum can be uniquely encoded. The rod spectrum is shown for comparison even though rod input is not used in color recognition. Dim red light can be used to adapt humans to maximum rod sensitivity because red light (620 to 700 nm) is not absorbed by rods to any significant extent. Downloaded from: Student. Consult (on 16 February 2007 03: 52 PM) © 2005 Elsevier
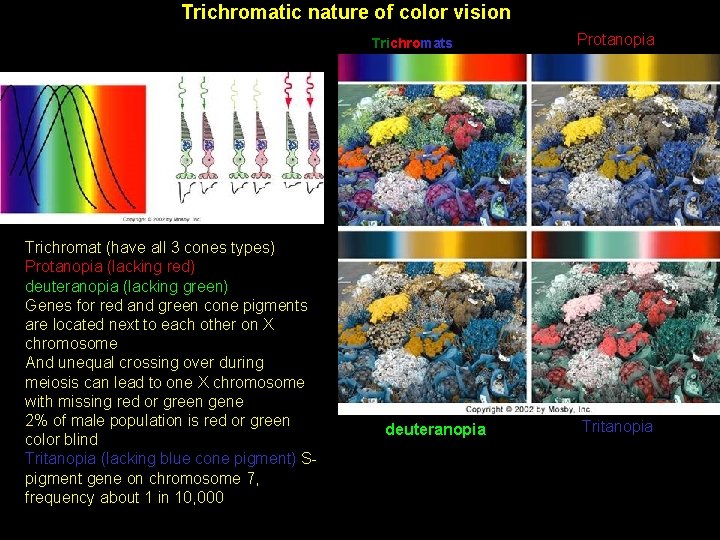
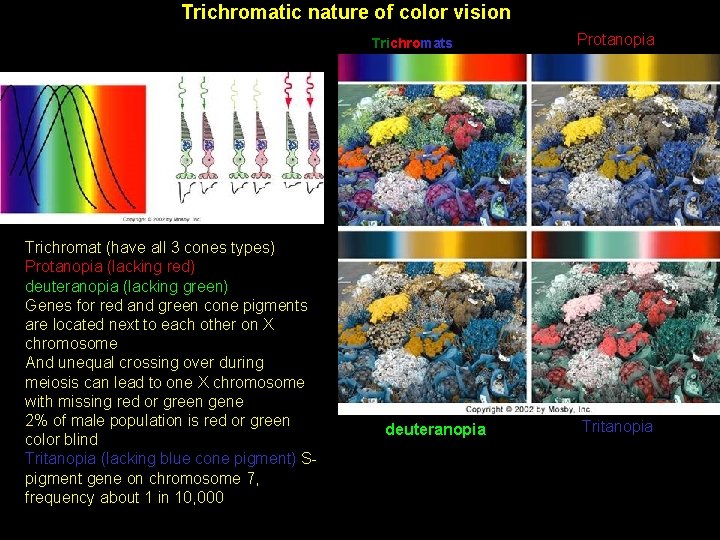
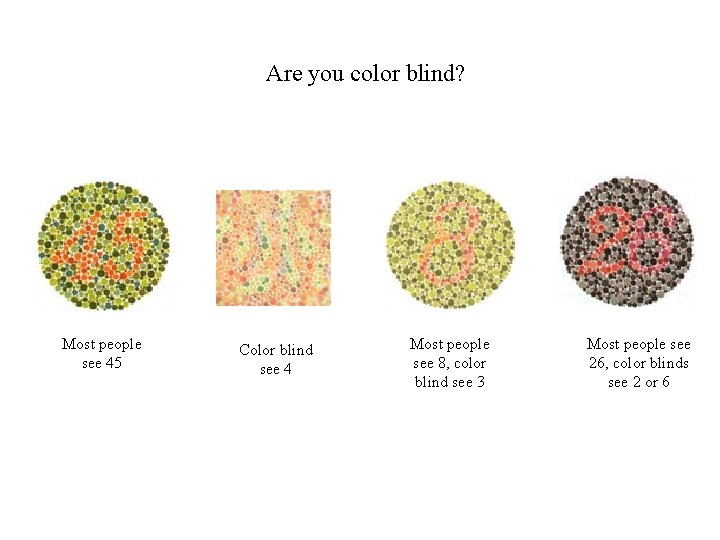
R Trichromatic nature of color vision Trichromats Trichromat (have all 3 cones types) Protanopia (lacking red) deuteranopia (lacking green) Genes for red and green cone pigments are located next to each other on X chromosome And unequal crossing over during meiosis can lead to one X chromosome with missing red or green gene 2% of male population is red or green color blind Tritanopia (lacking blue cone pigment) Spigment gene on chromosome 7, frequency about 1 in 10, 000 deuteranopia Protanopia Tritanopia
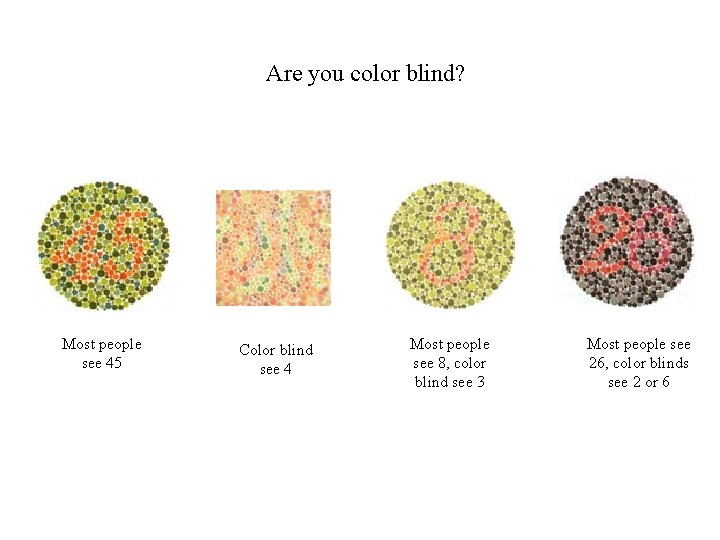
Are you color blind? Most people see 45 Color blind see 4 Most people see 8, color blind see 3 Most people see 26, color blinds see 2 or 6
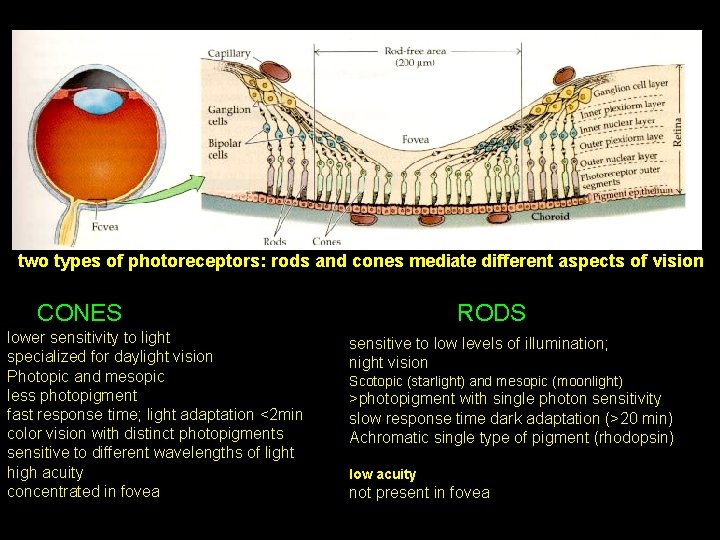
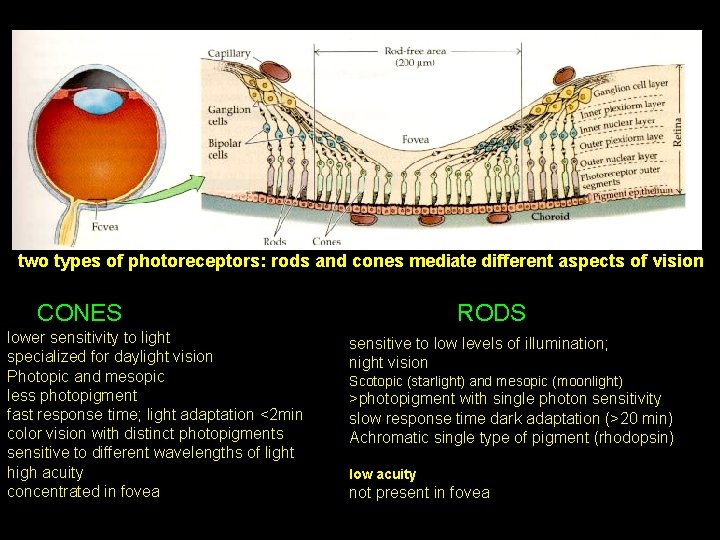
two types of photoreceptors: rods and cones mediate different aspects of vision CONES lower sensitivity to light specialized for daylight vision Photopic and mesopic less photopigment fast response time; light adaptation <2 min color vision with distinct photopigments sensitive to different wavelengths of light high acuity concentrated in fovea RODS sensitive to low levels of illumination; night vision Scotopic (starlight) and mesopic (moonlight) >photopigment with single photon sensitivity slow response time dark adaptation (>20 min) Achromatic single type of pigment (rhodopsin) low acuity not present in fovea
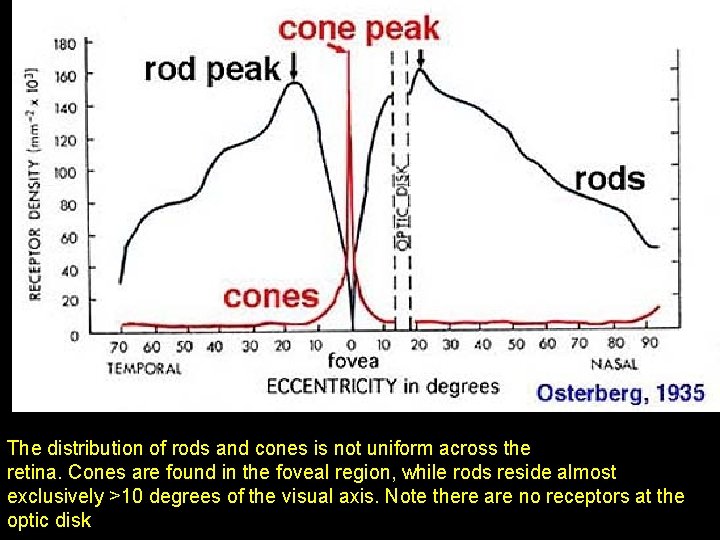
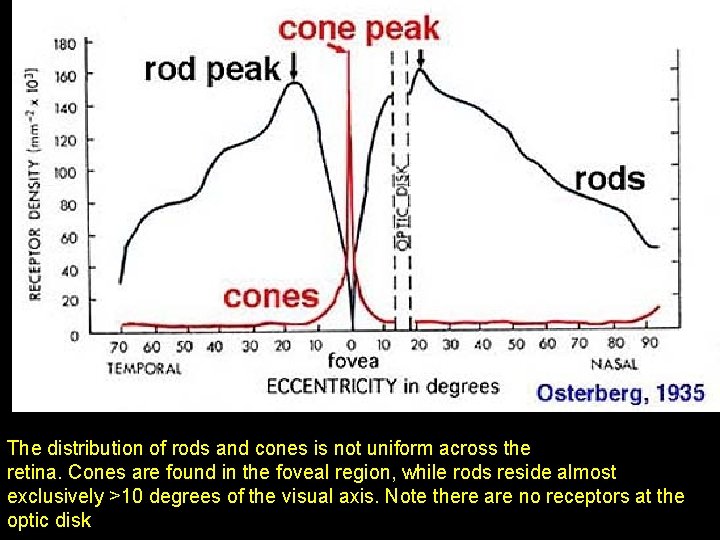
The distribution of rods and cones is not uniform across the retina. Cones are found in the foveal region, while rods reside almost exclusively >10 degrees of the visual axis. Note there are no receptors at the optic disk
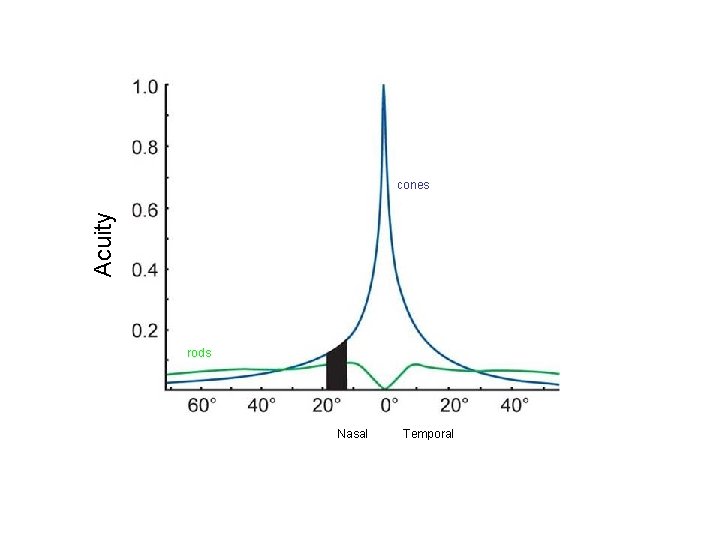
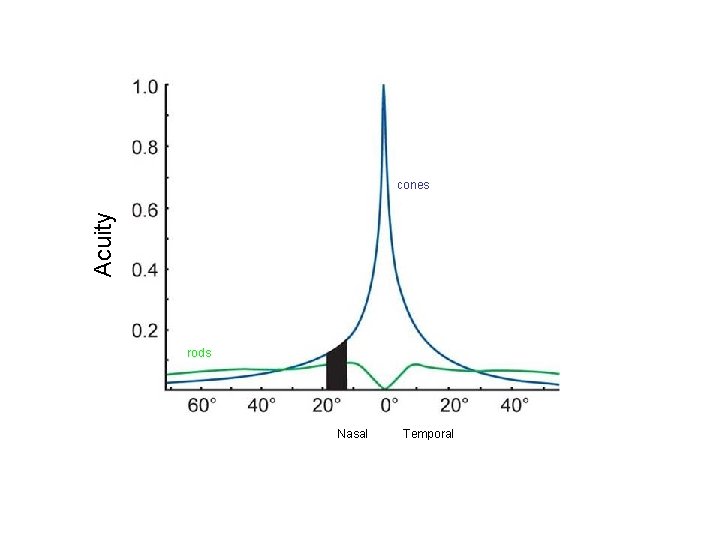
Acuity cones rods Nasal Temporal
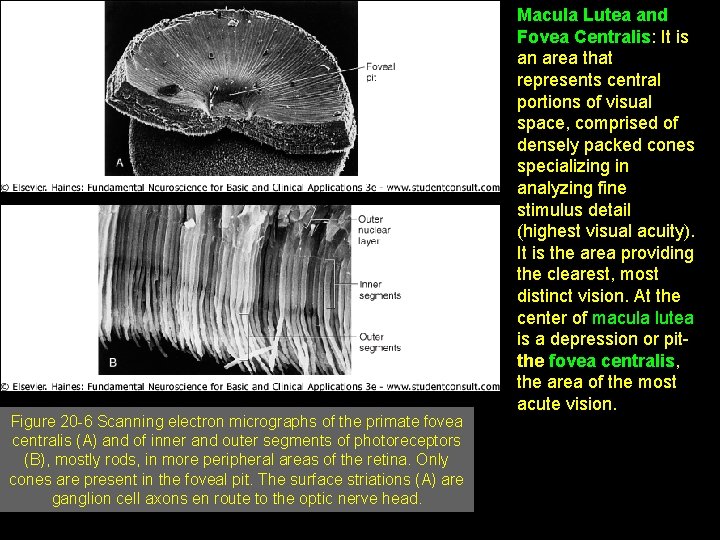
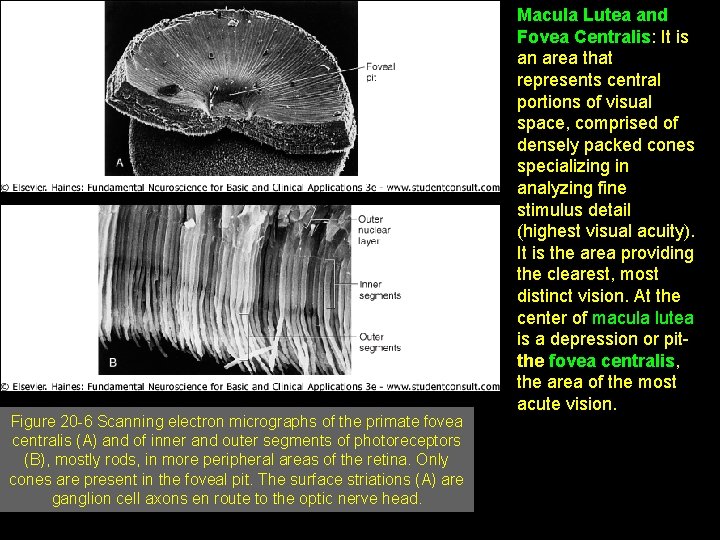
Figure 20 -6 Scanning electron micrographs of the primate fovea centralis (A) and of inner and outer segments of photoreceptors (B), mostly rods, in more peripheral areas of the retina. Only cones are present in the foveal pit. The surface striations (A) are ganglion cell axons en route to the optic nerve head. Macula Lutea and Fovea Centralis: It is an area that represents central portions of visual space, comprised of densely packed cones specializing in analyzing fine stimulus detail (highest visual acuity). It is the area providing the clearest, most distinct vision. At the center of macula lutea is a depression or pitthe fovea centralis, the area of the most acute vision. © 2005 Elsevier
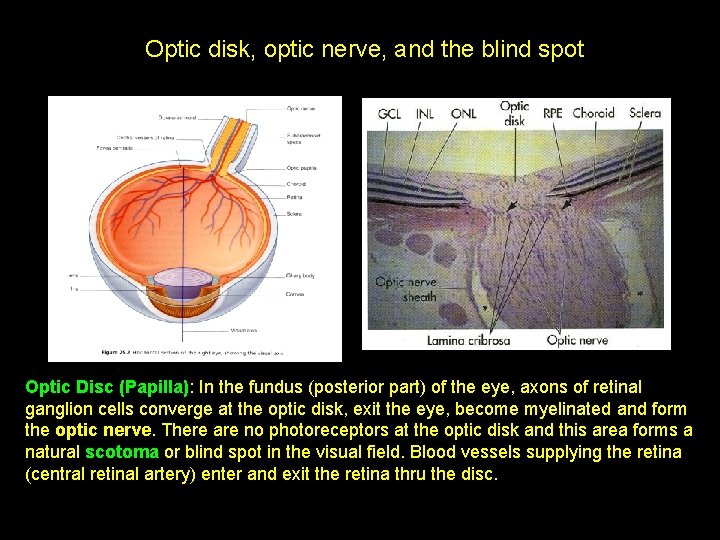
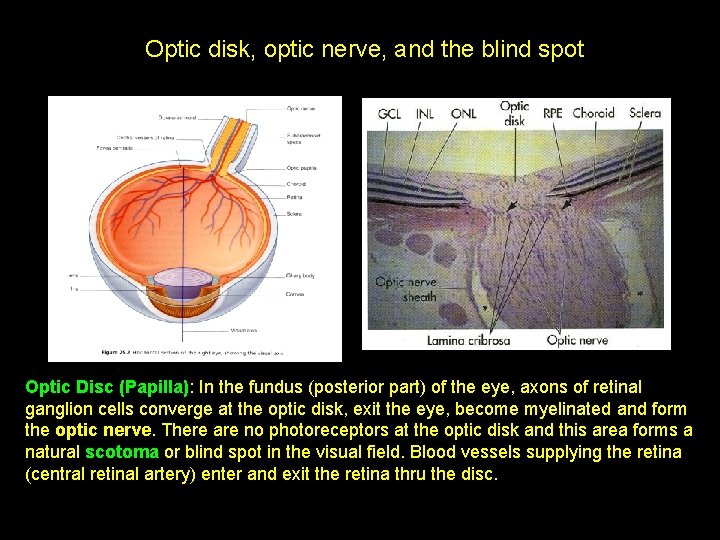
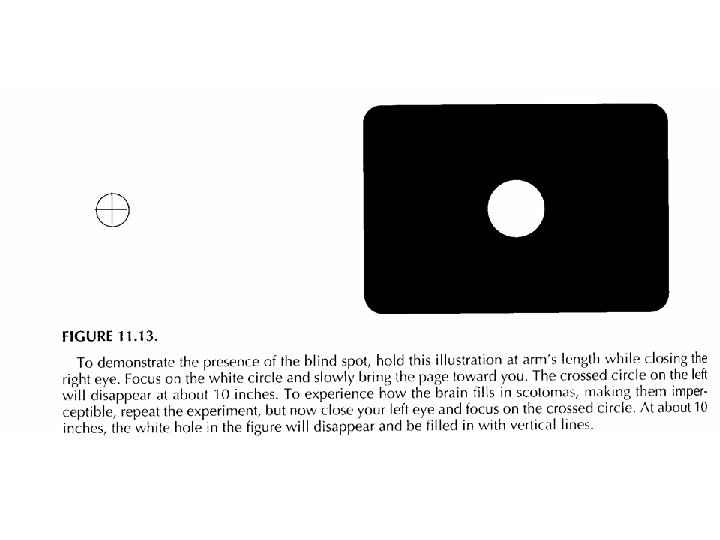
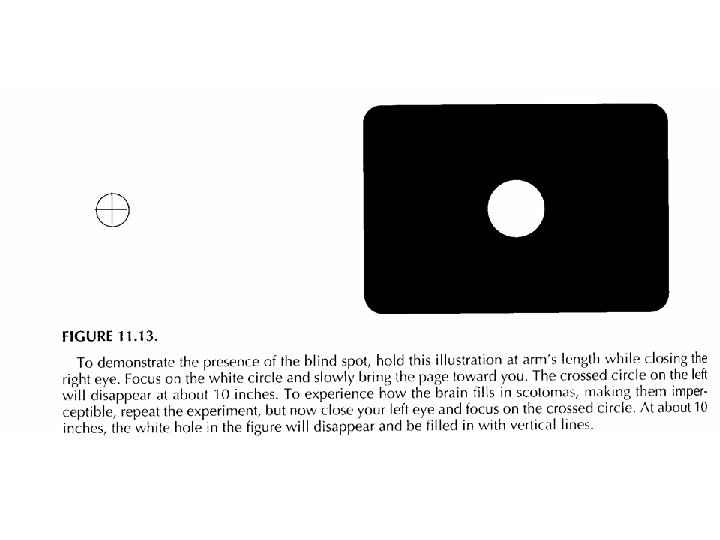
Optic disk, optic nerve, and the blind spot Optic Disc (Papilla): In the fundus (posterior part) of the eye, axons of retinal ganglion cells converge at the optic disk, exit the eye, become myelinated and form the optic nerve. There are no photoreceptors at the optic disk and this area forms a natural scotoma or blind spot in the visual field. Blood vessels supplying the retina (central retinal artery) enter and exit the retina thru the disc.
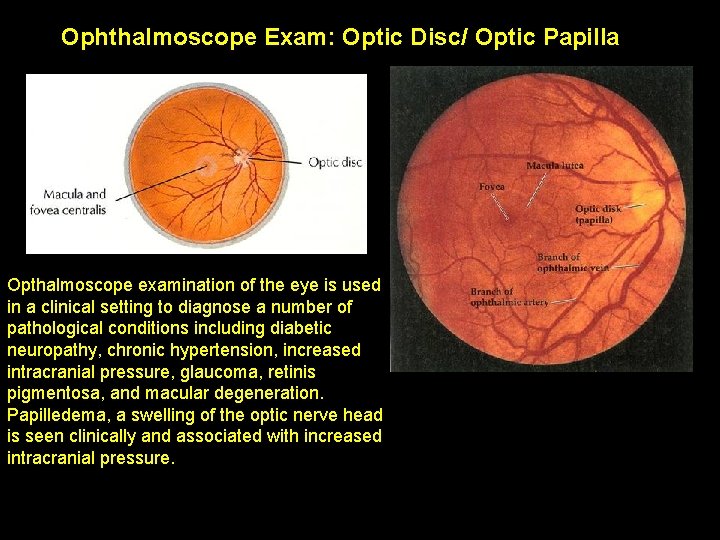
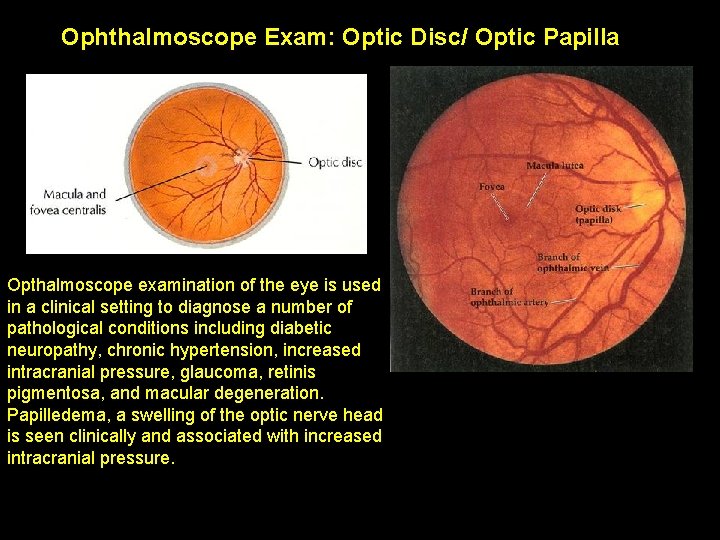
Ophthalmoscope Exam: Optic. Disc/Optic. Papilla Opthalmoscope examination of the eye is used in a clinical setting to diagnose a number of pathological conditions including diabetic neuropathy, chronic hypertension, increased intracranial pressure, glaucoma, retinis pigmentosa, and macular degeneration. Papilledema, a swelling of the optic nerve head is seen clinically and associated with increased intracranial pressure.
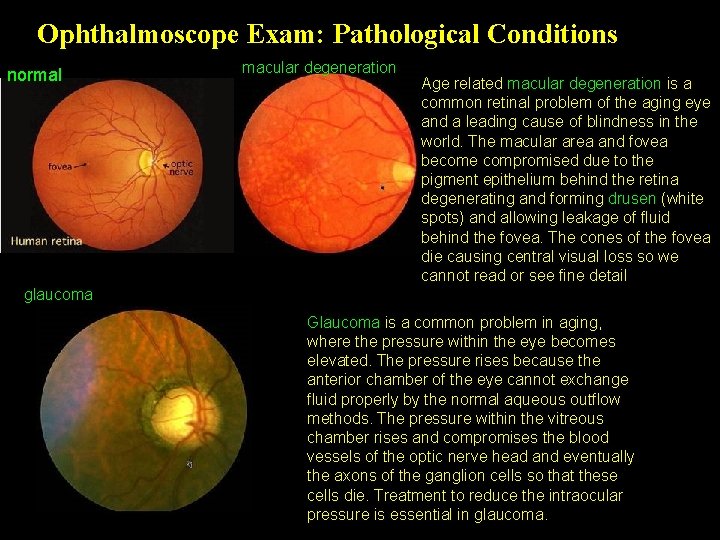
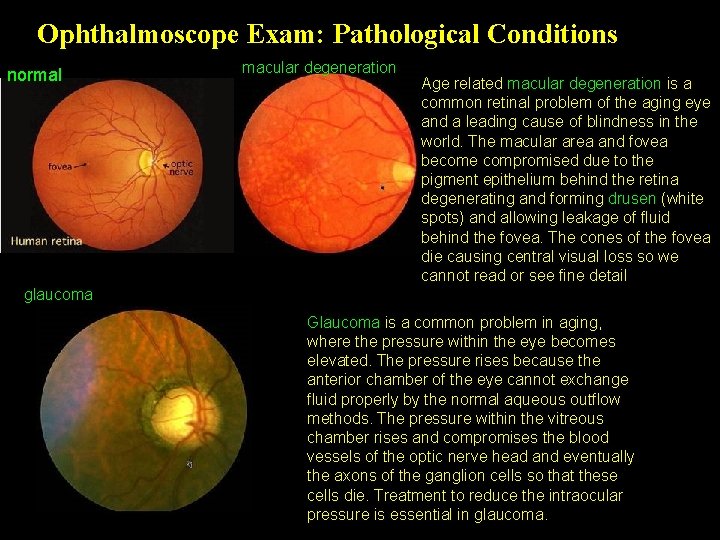
Ophthalmoscope Exam: Pathological Conditions normal macular degeneration Age related macular degeneration is a common retinal problem of the aging eye and a leading cause of blindness in the world. The macular area and fovea become compromised due to the pigment epithelium behind the retina degenerating and forming drusen (white spots) and allowing leakage of fluid behind the fovea. The cones of the fovea die causing central visual loss so we cannot read or see fine detail glaucoma Glaucoma is a common problem in aging, where the pressure within the eye becomes elevated. The pressure rises because the anterior chamber of the eye cannot exchange fluid properly by the normal aqueous outflow methods. The pressure within the vitreous chamber rises and compromises the blood vessels of the optic nerve head and eventually the axons of the ganglion cells so that these cells die. Treatment to reduce the intraocular pressure is essential in glaucoma.
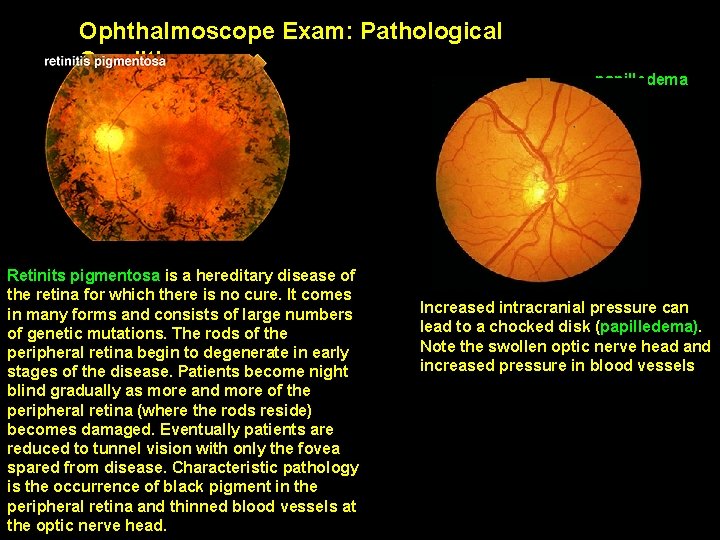
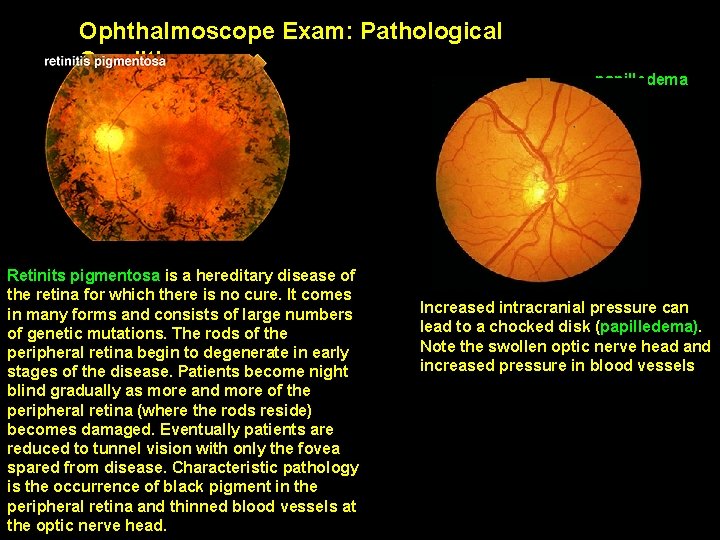
Ophthalmoscope Exam: Pathological Conditions Retinits pigmentosa is a hereditary disease of the retina for which there is no cure. It comes in many forms and consists of large numbers of genetic mutations. The rods of the peripheral retina begin to degenerate in early stages of the disease. Patients become night blind gradually as more and more of the peripheral retina (where the rods reside) becomes damaged. Eventually patients are reduced to tunnel vision with only the fovea spared from disease. Characteristic pathology is the occurrence of black pigment in the peripheral retina and thinned blood vessels at the optic nerve head. papilledema Increased intracranial pressure can lead to a chocked disk (papilledema). Note the swollen optic nerve head and increased pressure in blood vessels
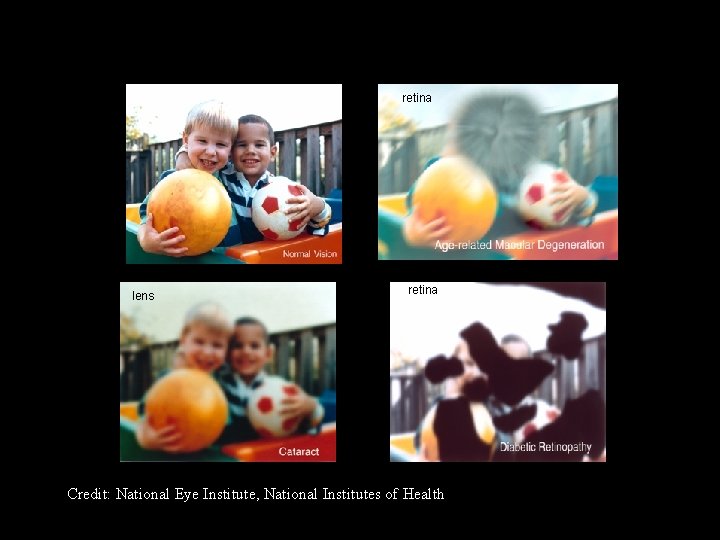
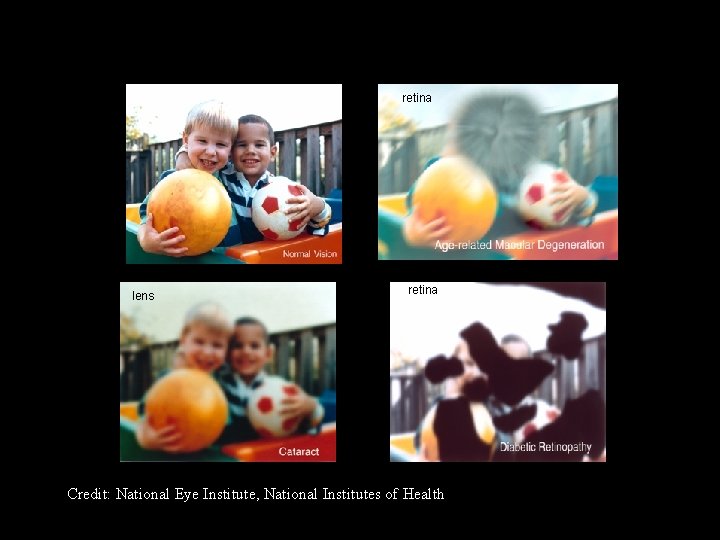
retina lens retina Credit: National Eye Institute, National Institutes of Health
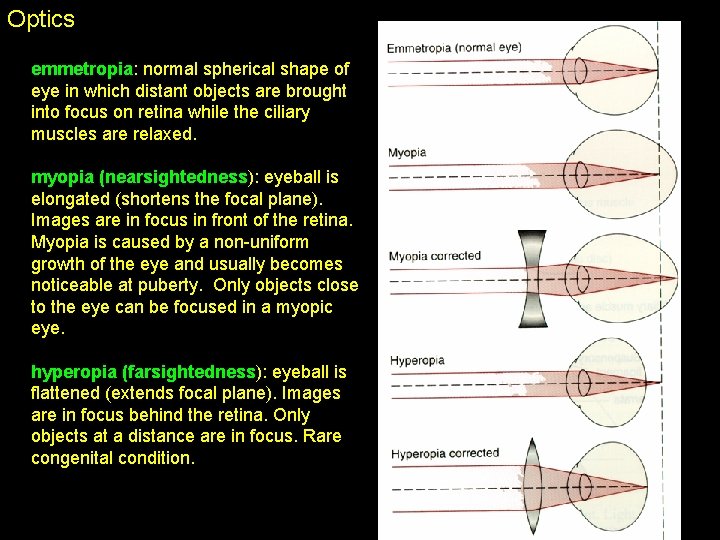
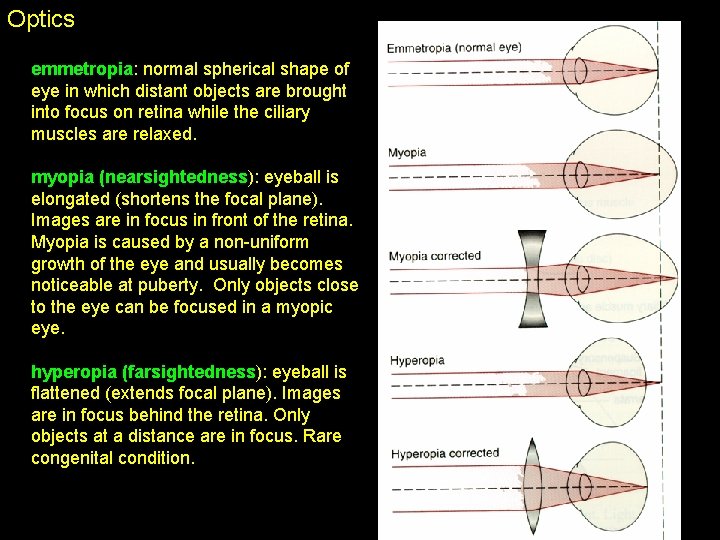
Optics emmetropia: normal spherical shape of eye in which distant objects are brought into focus on retina while the ciliary muscles are relaxed. myopia (nearsightedness): eyeball is elongated (shortens the focal plane). Images are in focus in front of the retina. Myopia is caused by a non-uniform growth of the eye and usually becomes noticeable at puberty. Only objects close to the eye can be focused in a myopic eye. hyperopia (farsightedness): eyeball is flattened (extends focal plane). Images are in focus behind the retina. Only objects at a distance are in focus. Rare congenital condition.
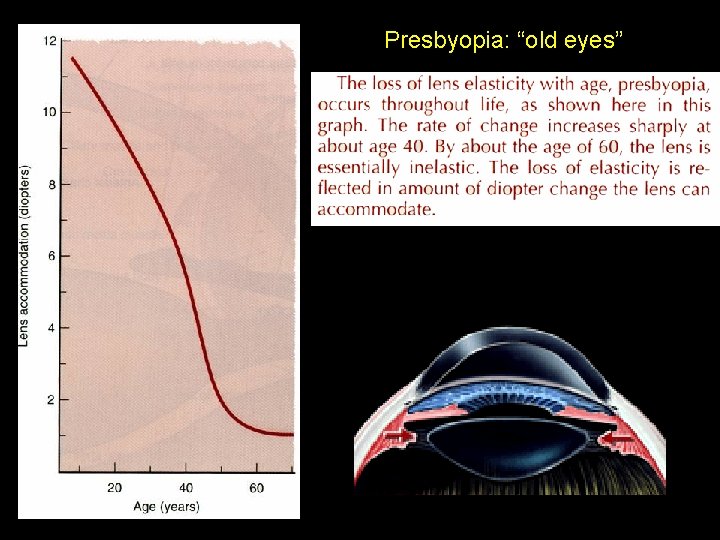
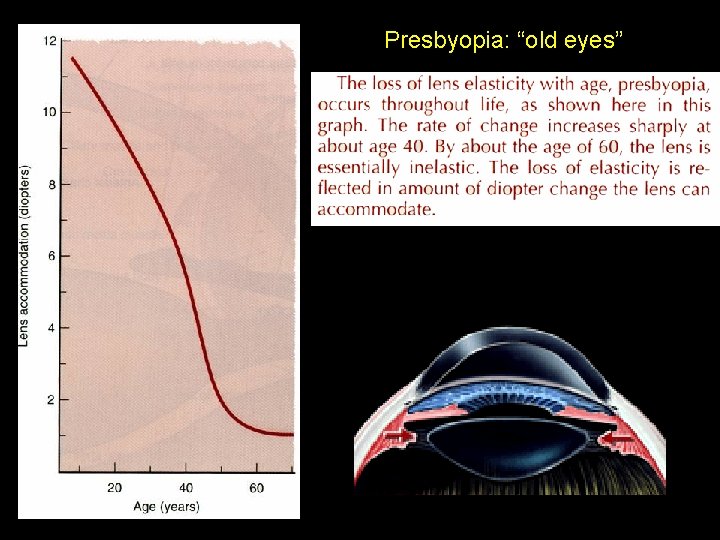
Presbyopia: “old eyes”
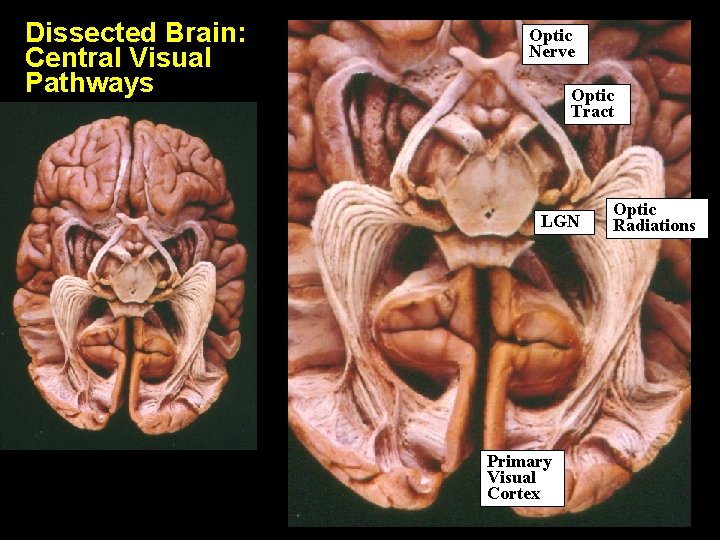
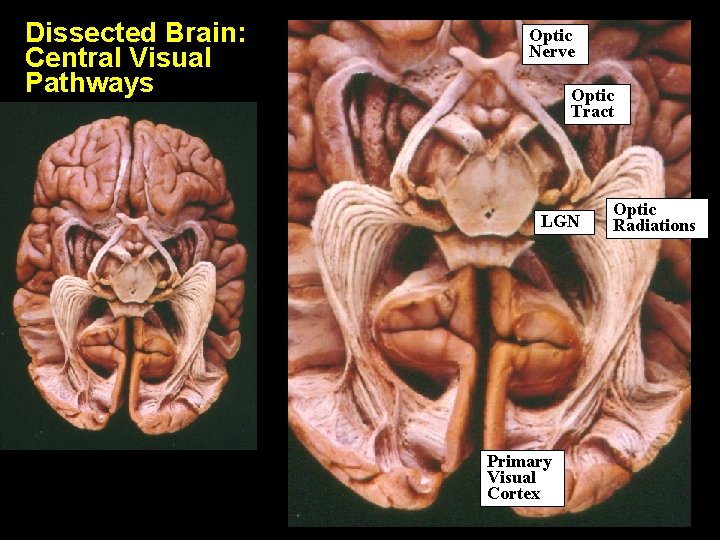
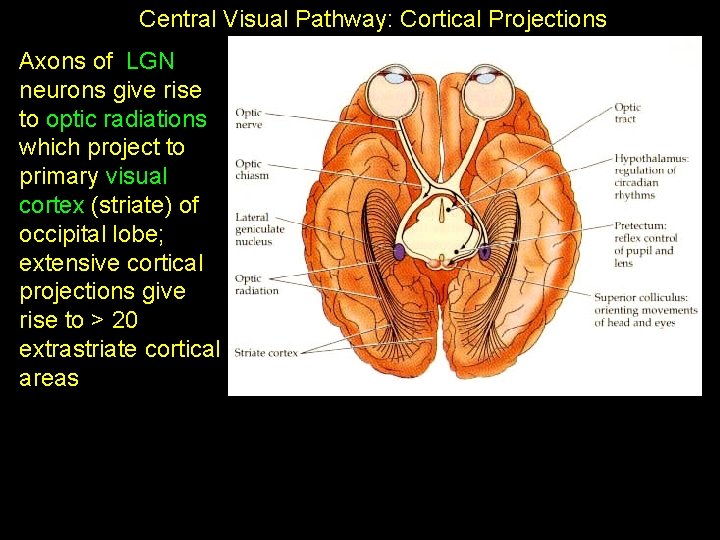
Dissected Brain: Central Visual Pathways Optic Nerve Optic Tract LGN Primary Visual Cortex Optic Radiations
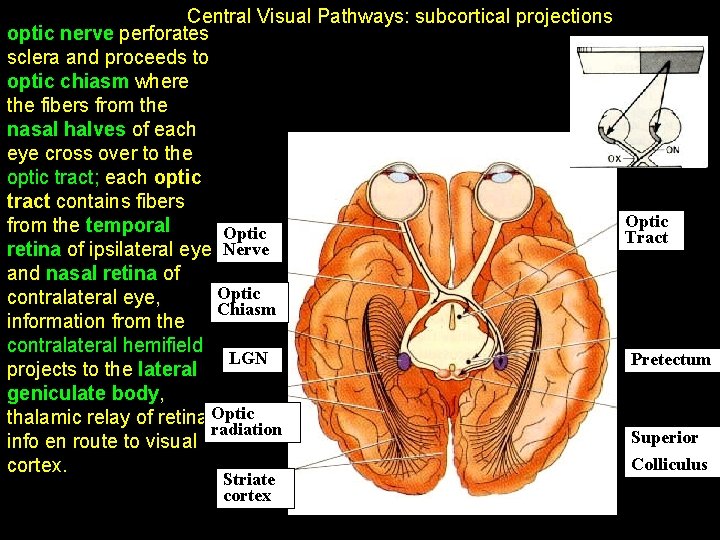
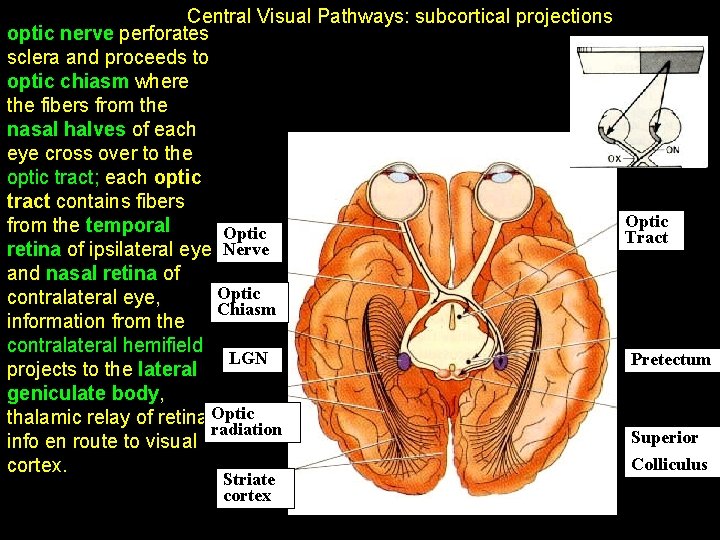
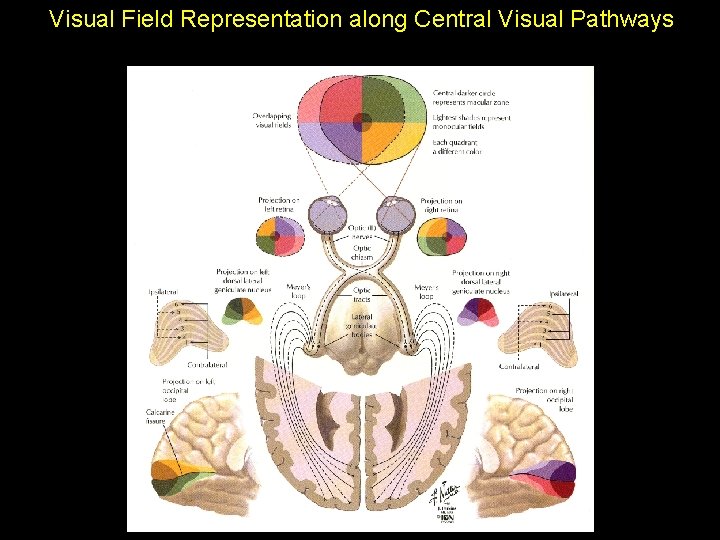
Central Visual Pathways: subcortical projections optic nerve perforates sclera and proceeds to optic chiasm where the fibers from the nasal halves of each eye cross over to the optic tract; each optic tract contains fibers from the temporal Optic retina of ipsilateral eye Nerve and nasal retina of Optic contralateral eye, Chiasm information from the contralateral hemifield LGN projects to the lateral geniculate body, thalamic relay of retinal. Optic radiation info en route to visual cortex. Striate cortex Optic Tract Pretectum Superior Colliculus
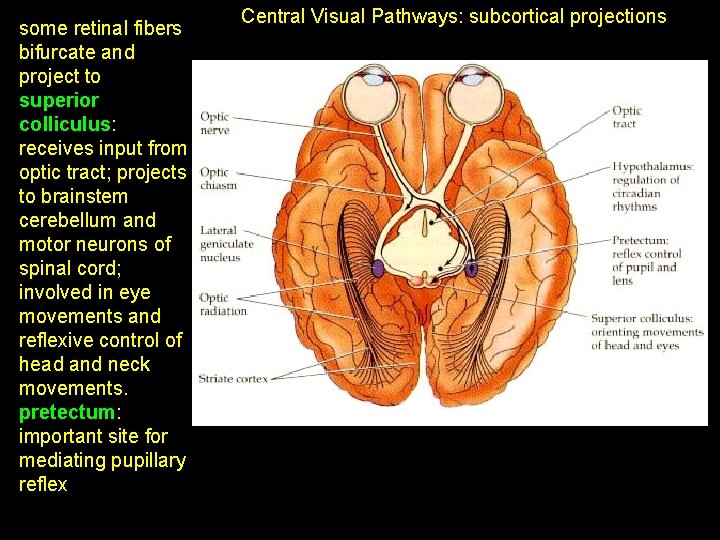
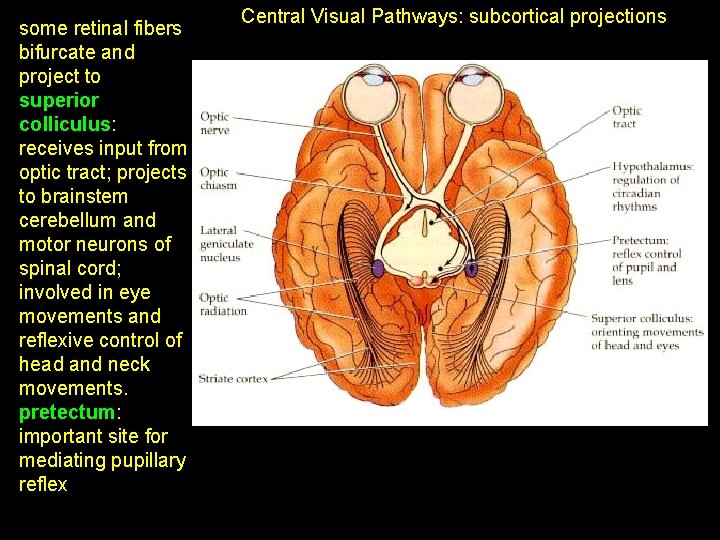
some retinal fibers bifurcate and project to superior colliculus: receives input from optic tract; projects to brainstem cerebellum and motor neurons of spinal cord; involved in eye movements and reflexive control of head and neck movements. pretectum: important site for mediating pupillary reflex Central Visual Pathways: subcortical projections
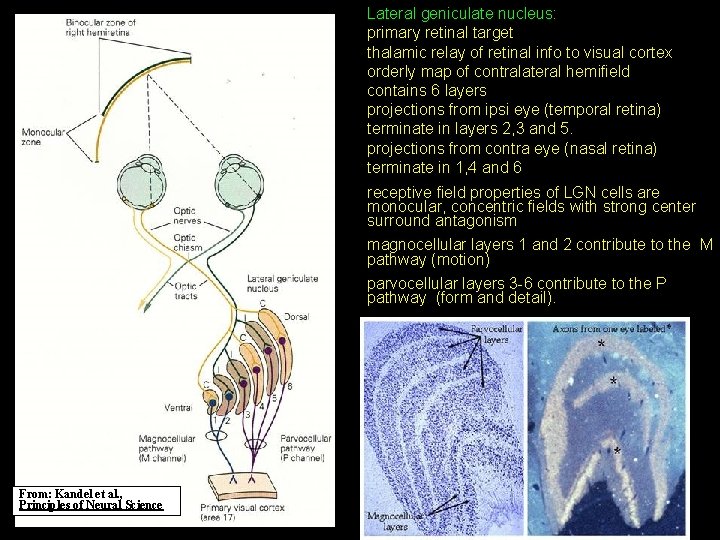
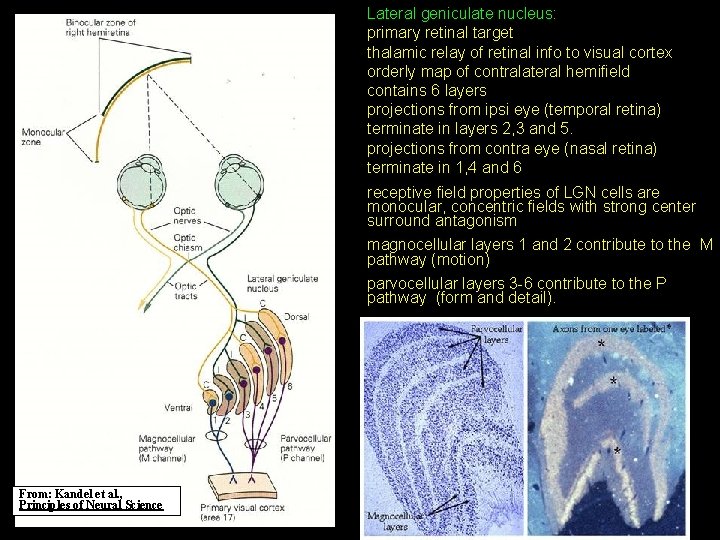
Lateral geniculate nucleus: primary retinal target thalamic relay of retinal info to visual cortex orderly map of contralateral hemifield contains 6 layers projections from ipsi eye (temporal retina) terminate in layers 2, 3 and 5. projections from contra eye (nasal retina) terminate in 1, 4 and 6 receptive field properties of LGN cells are monocular, concentric fields with strong center surround antagonism magnocellular layers 1 and 2 contribute to the M pathway (motion) parvocellular layers 3 -6 contribute to the P pathway (form and detail). From: Kandel et al. , Principles of Neural Science
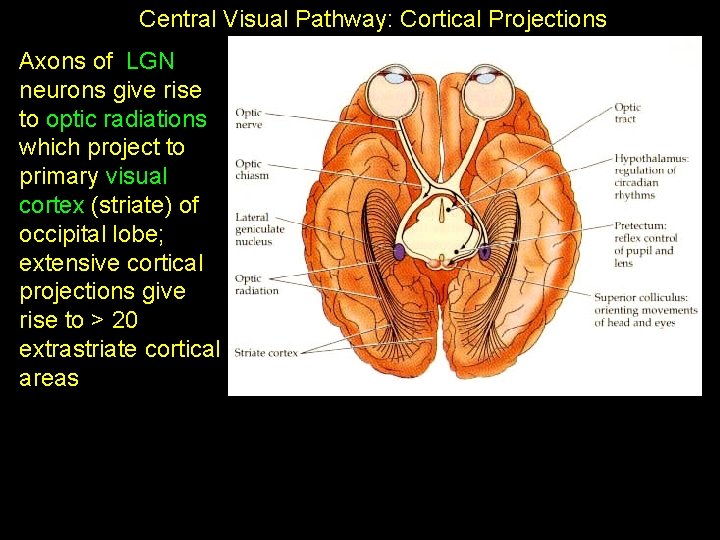
Central Visual Pathway: Cortical Projections Axons of LGN neurons give rise to optic radiations which project to primary visual cortex (striate) of occipital lobe; extensive cortical projections give rise to > 20 extrastriate cortical areas
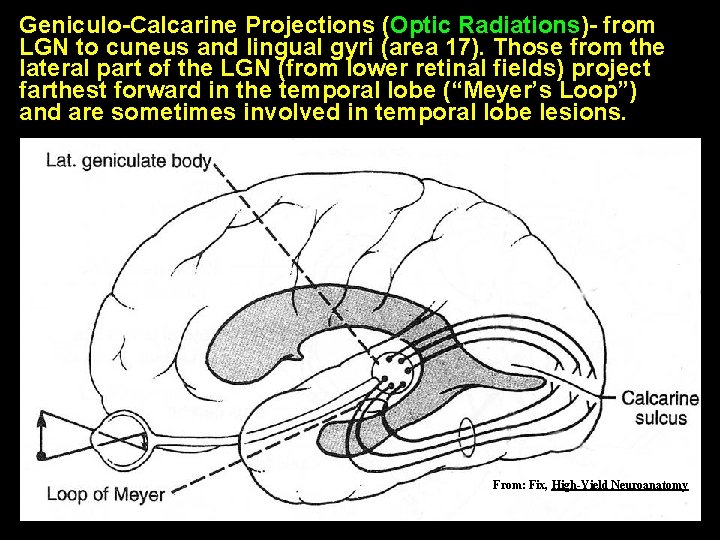
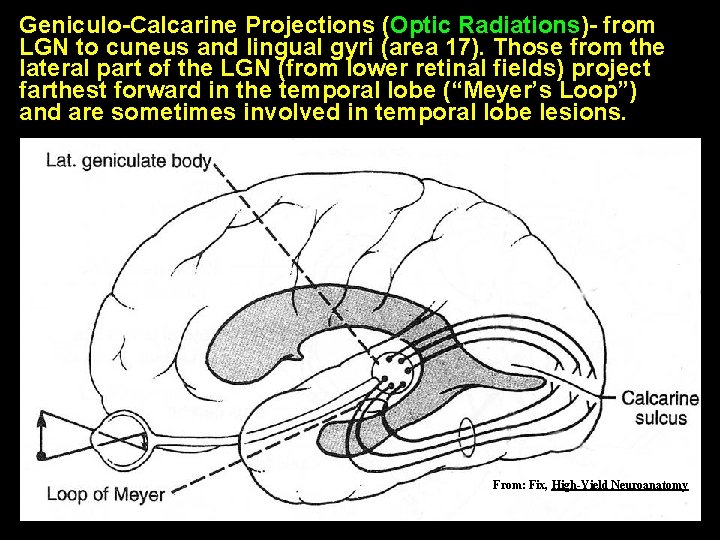
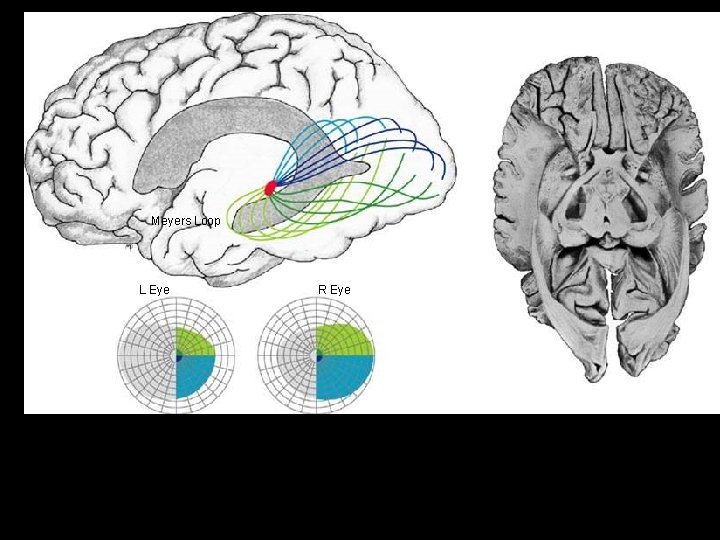
Geniculo-Calcarine Projections (Optic Radiations)- from LGN to cuneus and lingual gyri (area 17). Those from the lateral part of the LGN (from lower retinal fields) project farthest forward in the temporal lobe (“Meyer’s Loop”) and are sometimes involved in temporal lobe lesions. From: Fix, High-Yield Neuroanatomy
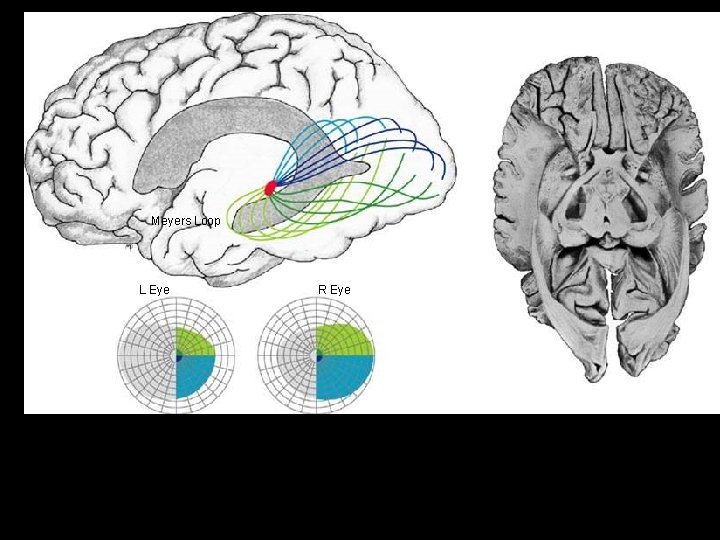
Meyers Loop L Eye R Eye
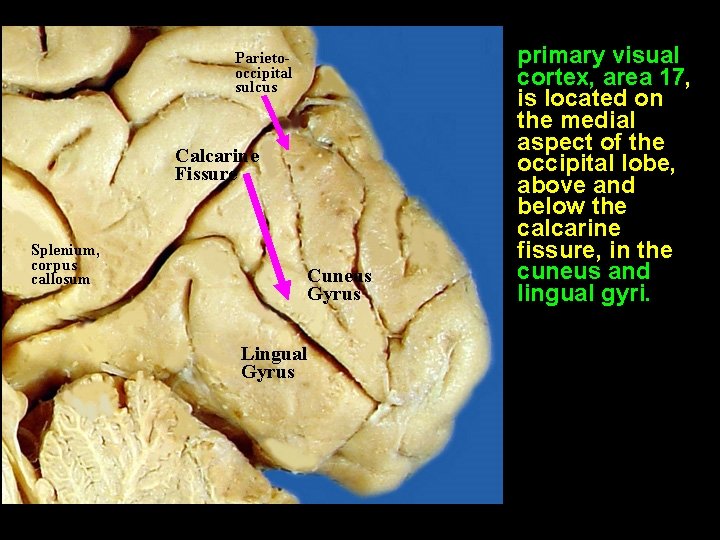
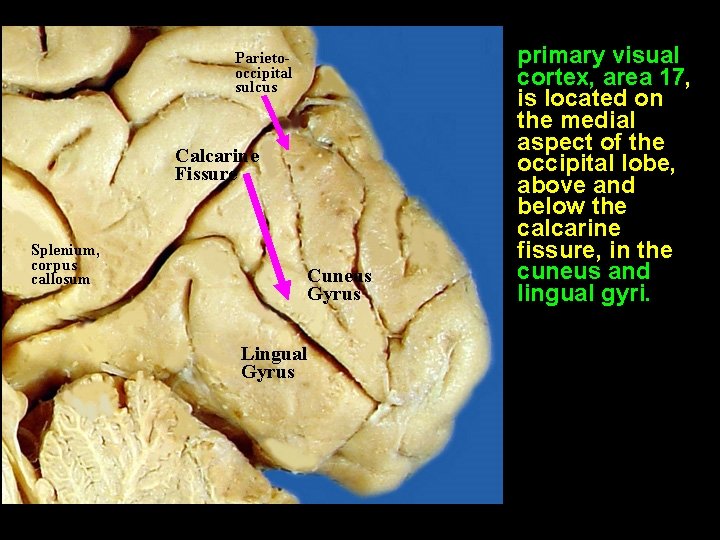
Parietooccipital sulcus Calcarine Fissure Splenium, corpus callosum Cuneus Gyrus Lingual Gyrus primary visual cortex, area 17, is located on the medial aspect of the occipital lobe, above and below the calcarine fissure, in the cuneus and lingual gyri.
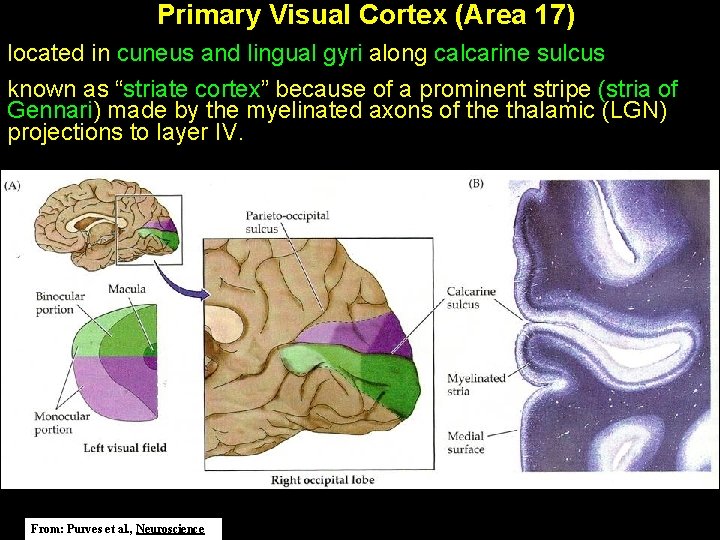
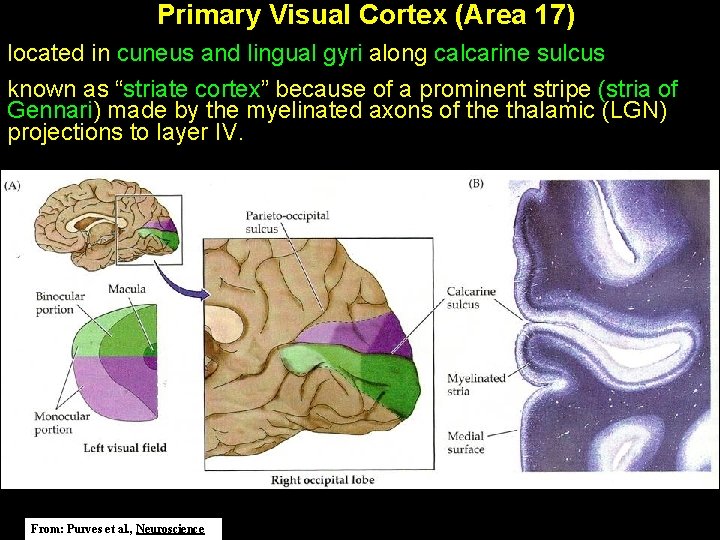
Primary Visual Cortex (Area 17) located in cuneus and lingual gyri along calcarine sulcus known as “striate cortex” because of a prominent stripe (stria of Gennari) made by the myelinated axons of the thalamic (LGN) projections to layer IV. From: Purves et al. , Neuroscience
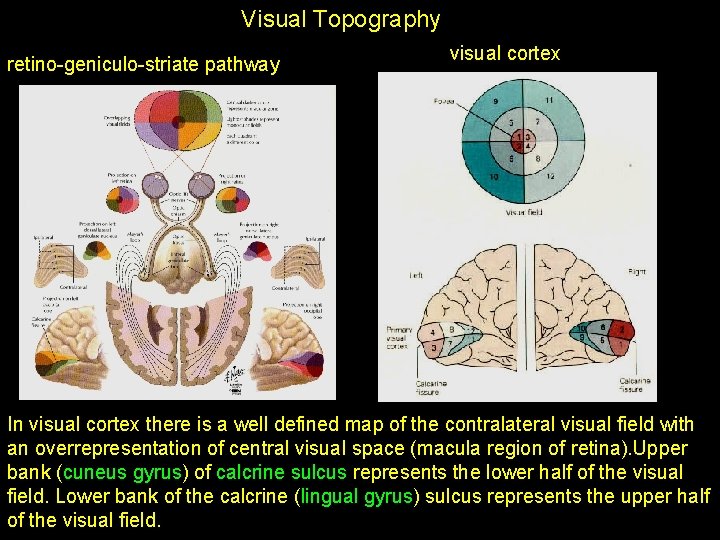
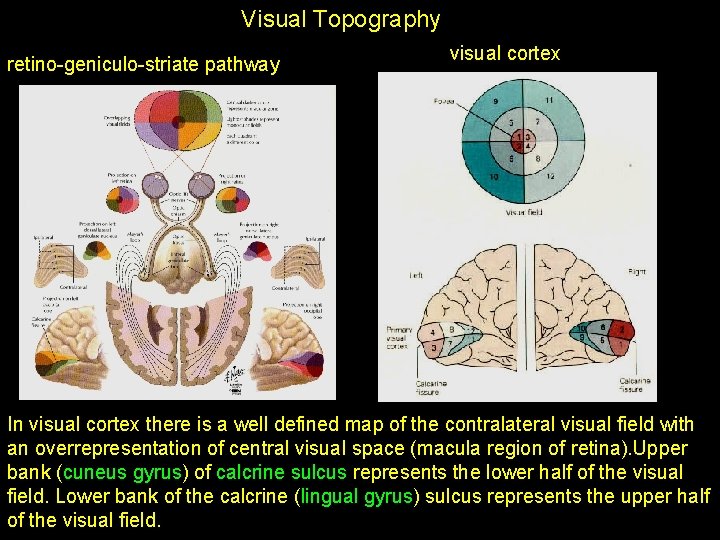
Visual Topography retino-geniculo-striate pathway visual cortex In visual cortex there is a well defined map of the contralateral visual field with an overrepresentation of central visual space (macula region of retina). Upper bank (cuneus gyrus) of calcrine sulcus represents the lower half of the visual field. Lower bank of the calcrine (lingual gyrus) sulcus represents the upper half of the visual field.
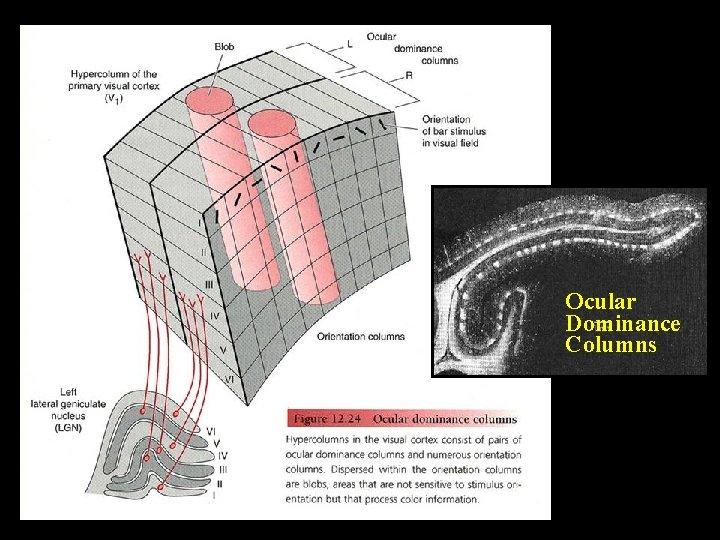
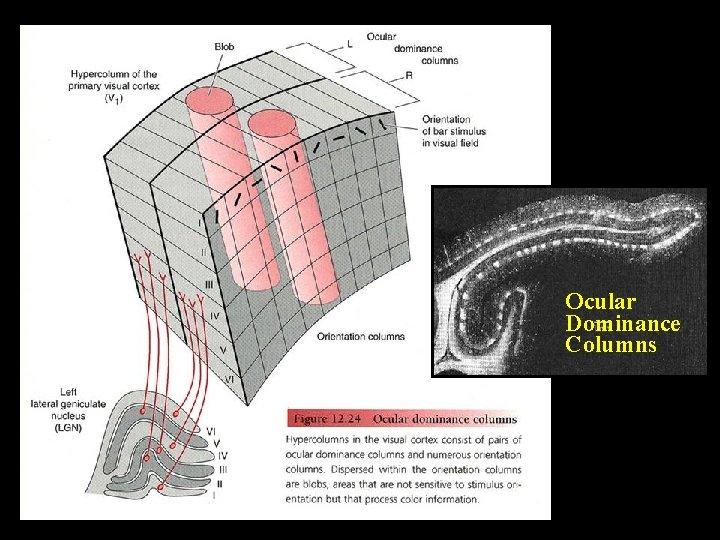
Ocular Dominance Columns
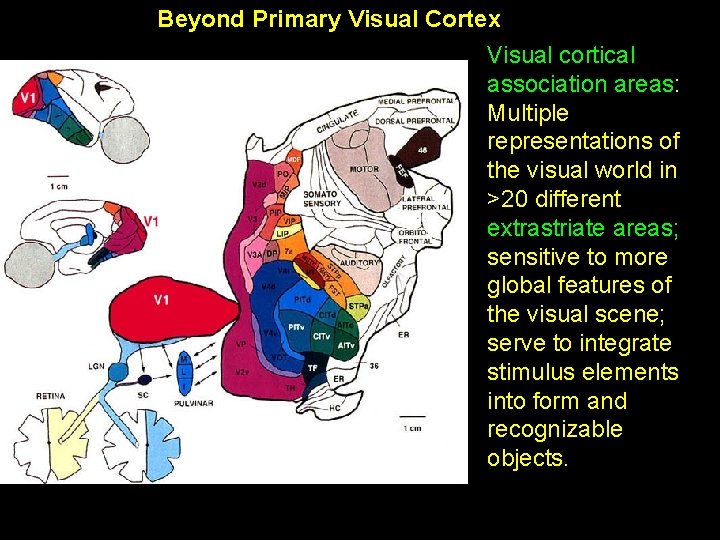
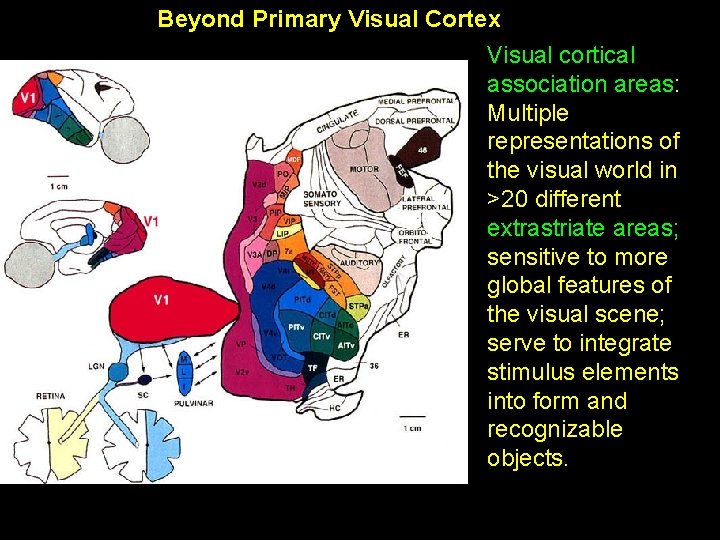
Beyond Primary Visual Cortex Visual cortical association areas: Multiple representations of the visual world in >20 different extrastriate areas; sensitive to more global features of the visual scene; serve to integrate stimulus elements into form and recognizable objects.
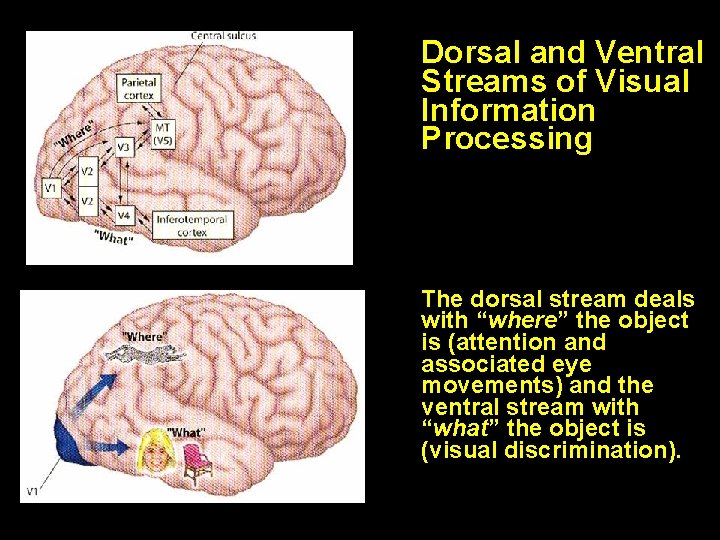
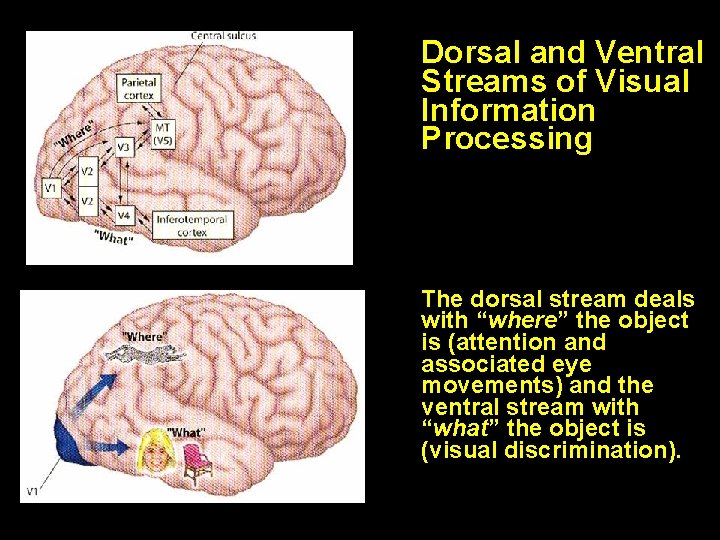
Dorsal and Ventral Streams of Visual Information Processing The dorsal stream deals with “where” the object is (attention and associated eye movements) and the ventral stream with “what” the object is (visual discrimination).
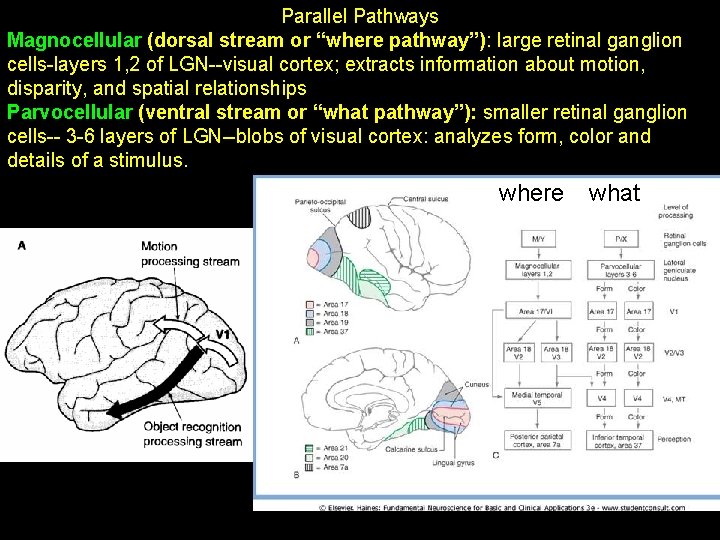
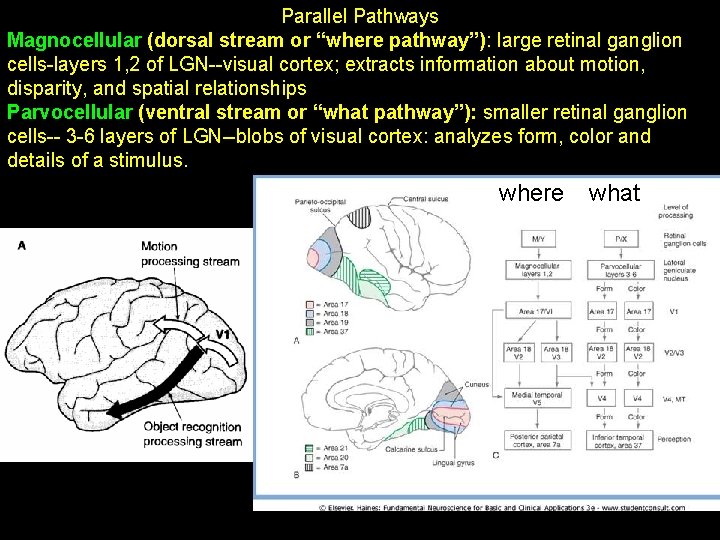
Parallel Pathways Magnocellular (dorsal stream or “where pathway”): large retinal ganglion cells-layers 1, 2 of LGN--visual cortex; extracts information about motion, disparity, and spatial relationships Parvocellular (ventral stream or “what pathway”): smaller retinal ganglion cells-- 3 -6 layers of LGN--blobs of visual cortex: analyzes form, color and details of a stimulus. where what
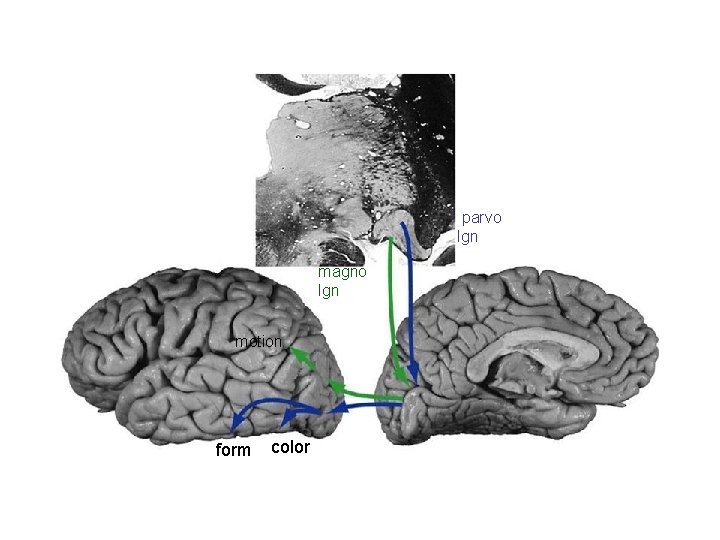
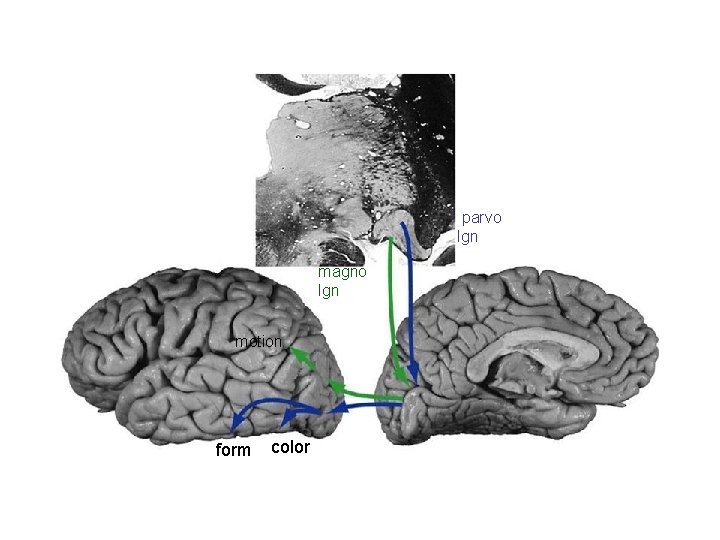
parvo lgn magno lgn motion form color
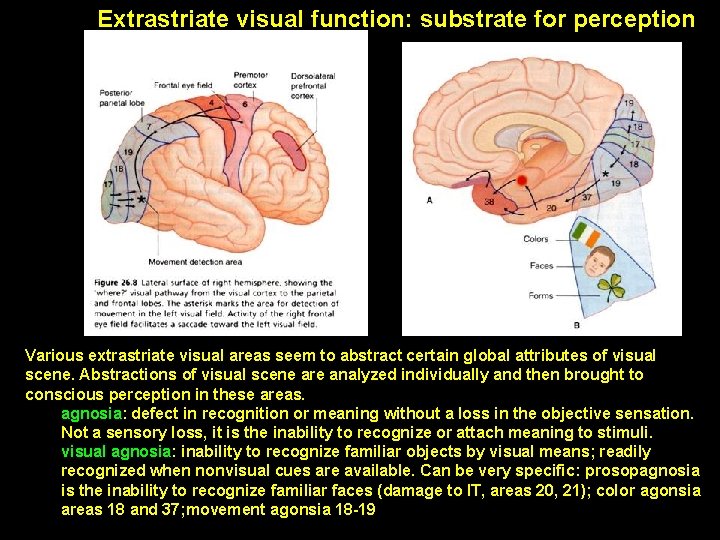
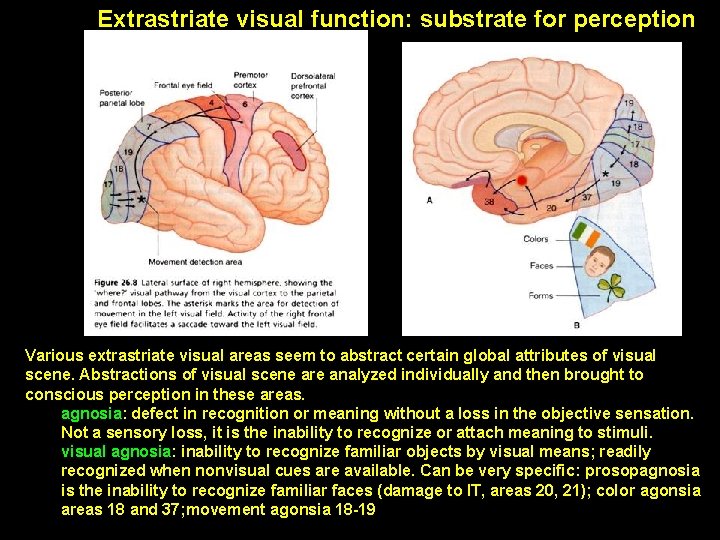
Extrastriate visual function: substrate for perception Various extrastriate visual areas seem to abstract certain global attributes of visual scene. Abstractions of visual scene are analyzed individually and then brought to conscious perception in these areas. agnosia: defect in recognition or meaning without a loss in the objective sensation. Not a sensory loss, it is the inability to recognize or attach meaning to stimuli. visual agnosia: inability to recognize familiar objects by visual means; readily recognized when nonvisual cues are available. Can be very specific: prosopagnosia is the inability to recognize familiar faces (damage to IT, areas 20, 21); color agonsia areas 18 and 37; movement agonsia 18 -19
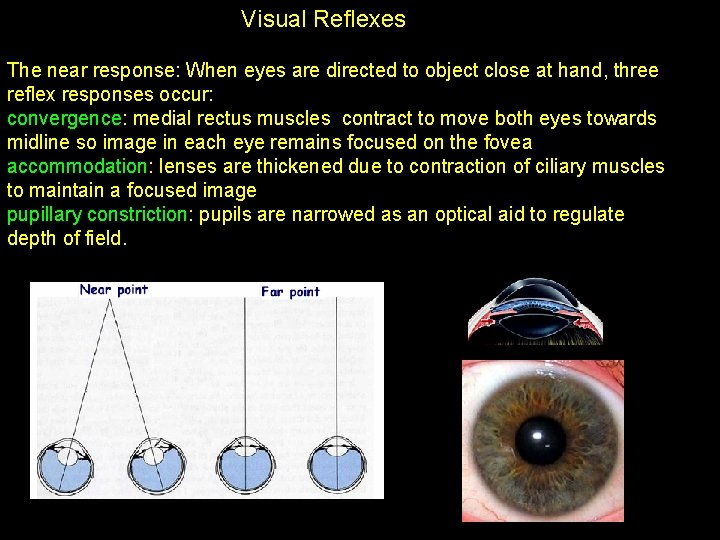
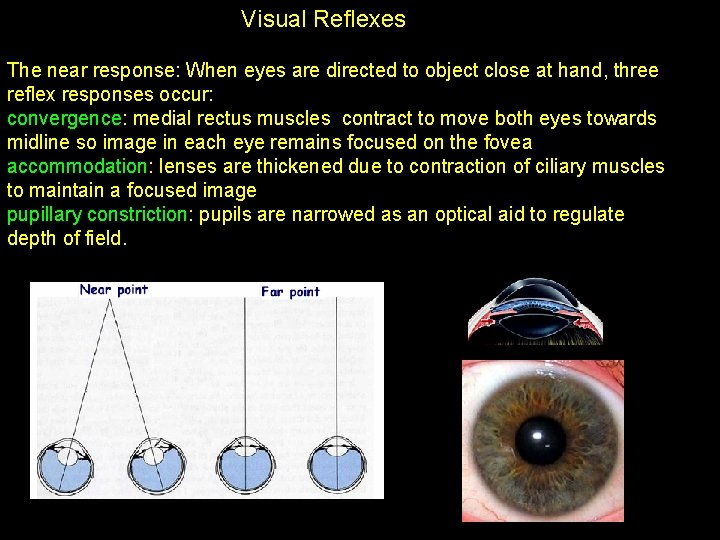
Visual Reflexes The near response: When eyes are directed to object close at hand, three reflex responses occur: convergence: medial rectus muscles contract to move both eyes towards midline so image in each eye remains focused on the fovea accommodation: lenses are thickened due to contraction of ciliary muscles to maintain a focused image pupillary constriction: pupils are narrowed as an optical aid to regulate depth of field.
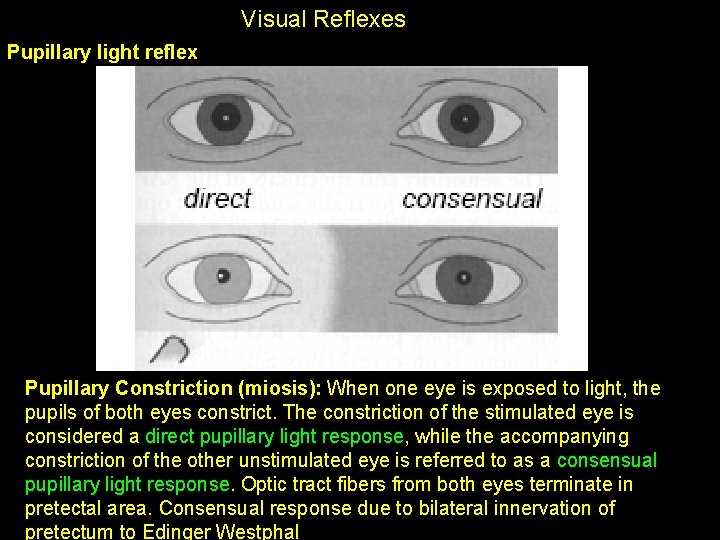
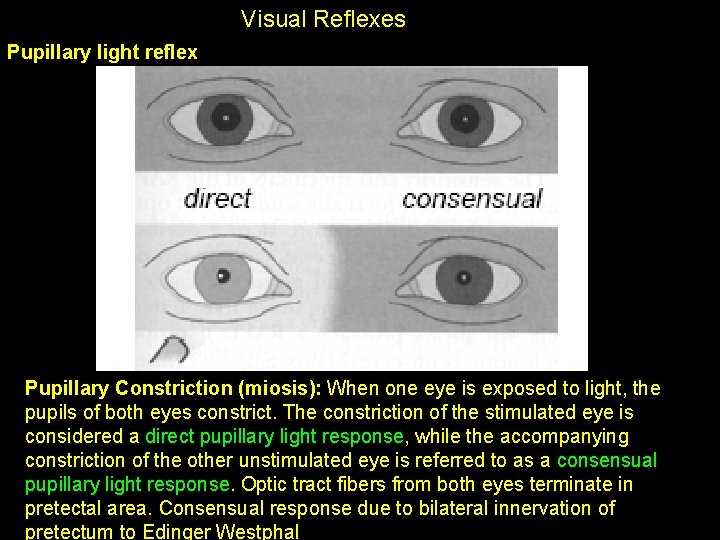
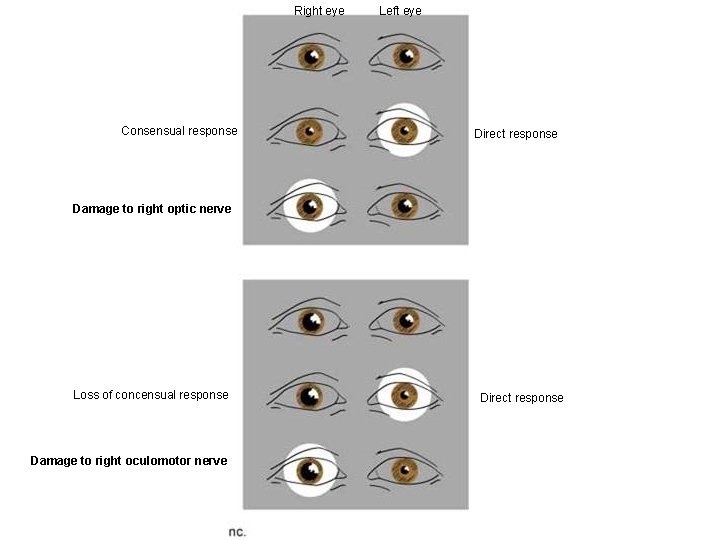
Visual Reflexes Pupillary light reflex Pupillary Constriction (miosis): When one eye is exposed to light, the pupils of both eyes constrict. The constriction of the stimulated eye is considered a direct pupillary light response, while the accompanying constriction of the other unstimulated eye is referred to as a consensual pupillary light response. Optic tract fibers from both eyes terminate in pretectal area. Consensual response due to bilateral innervation of pretectum to Edinger Westphal
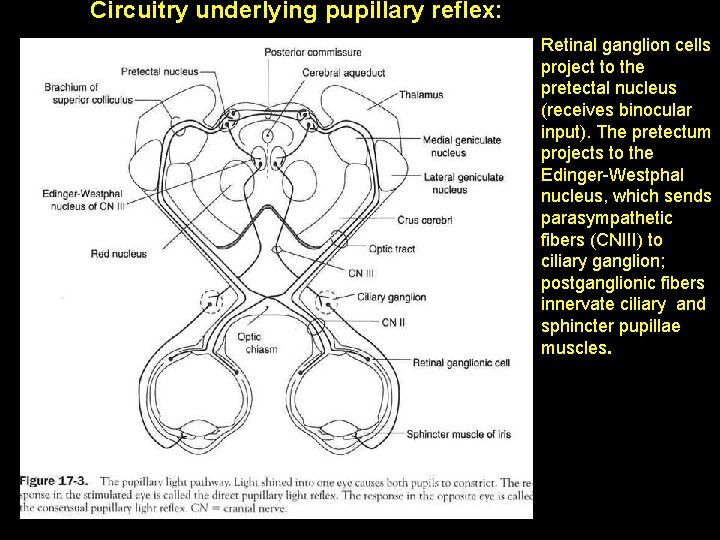
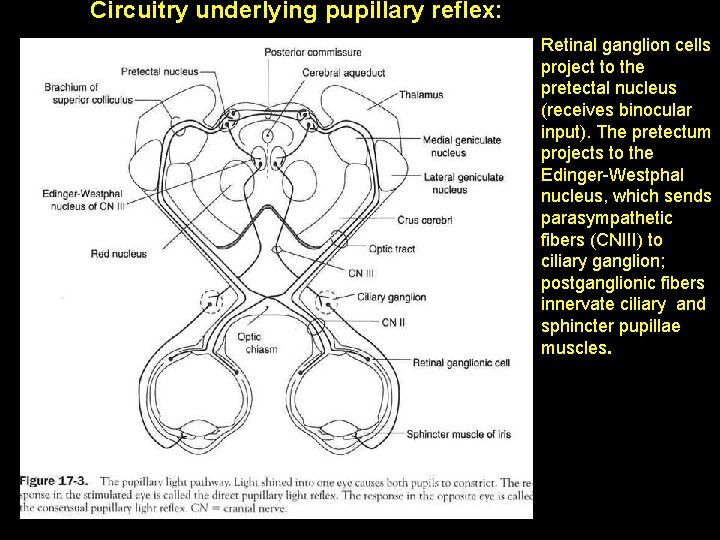
Circuitry underlying pupillary reflex: Retinal ganglion cells project to the pretectal nucleus (receives binocular input). The pretectum projects to the Edinger-Westphal nucleus, which sends parasympathetic fibers (CNIII) to ciliary ganglion; postganglionic fibers innervate ciliary and sphincter pupillae muscles.
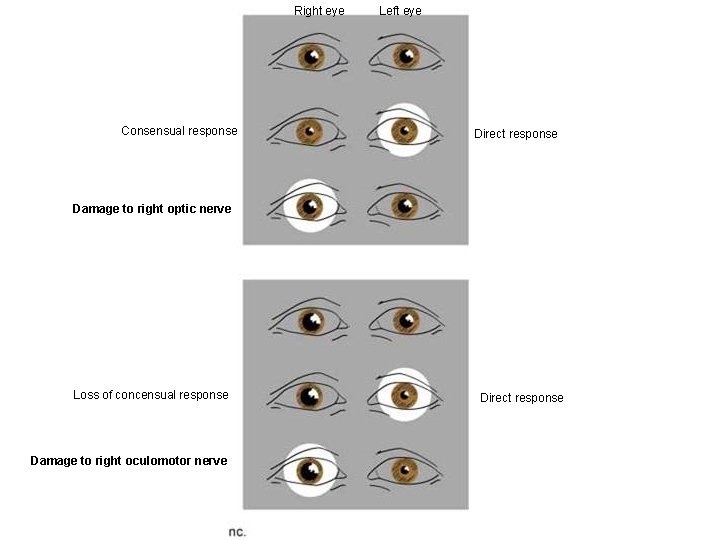
Right eye Consensual response Left eye Direct response Damage to right optic nerve Loss of concensual response Damage to right oculomotor nerve Direct response
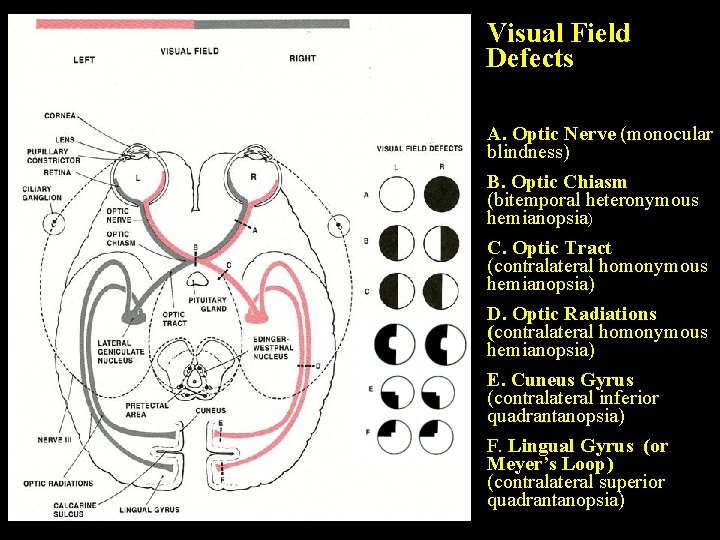
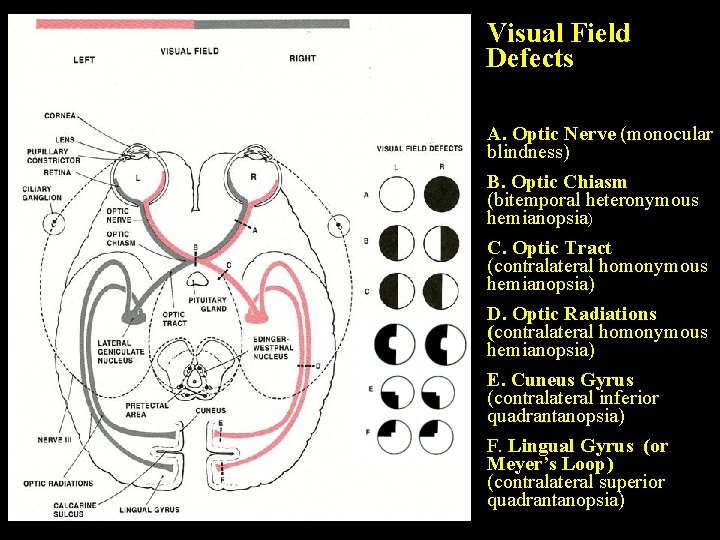
Visual Field Defects A. Optic Nerve (monocular blindness) B. Optic Chiasm (bitemporal heteronymous hemianopsia) C. Optic Tract (contralateral homonymous hemianopsia) D. Optic Radiations (contralateral homonymous hemianopsia) E. Cuneus Gyrus (contralateral inferior quadrantanopsia) F. Lingual Gyrus (or Meyer’s Loop) (contralateral superior quadrantanopsia)
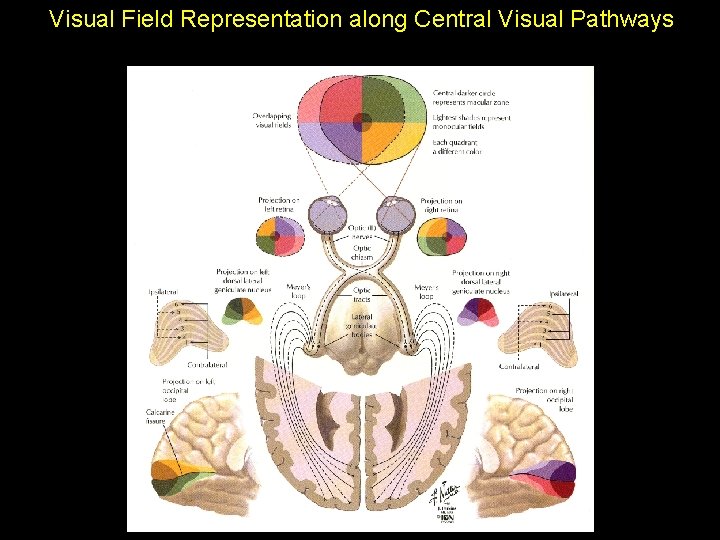
Visual Field Representation along Central Visual Pathways