Anatomy of Sinuses Acute Rhinosinusitis Viral Common Symptoms

































- Slides: 122
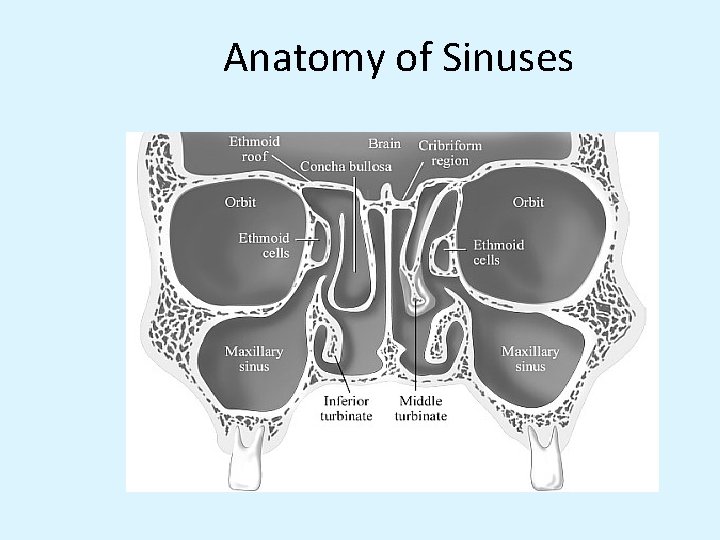
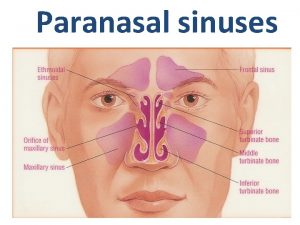
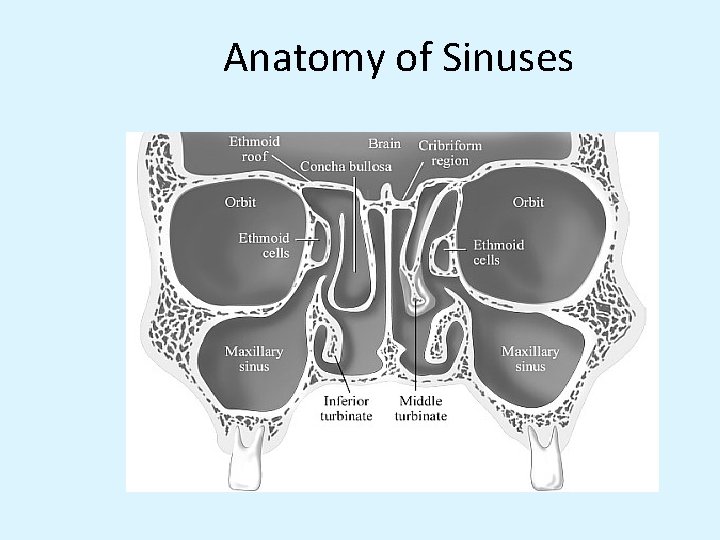
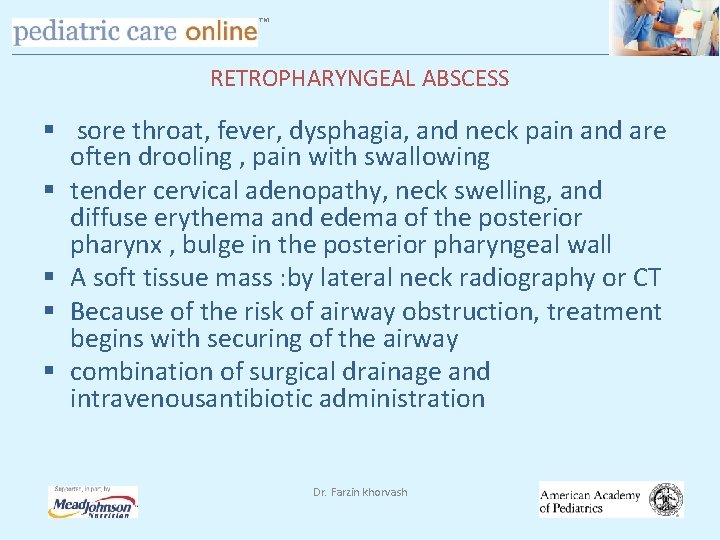
Anatomy of Sinuses
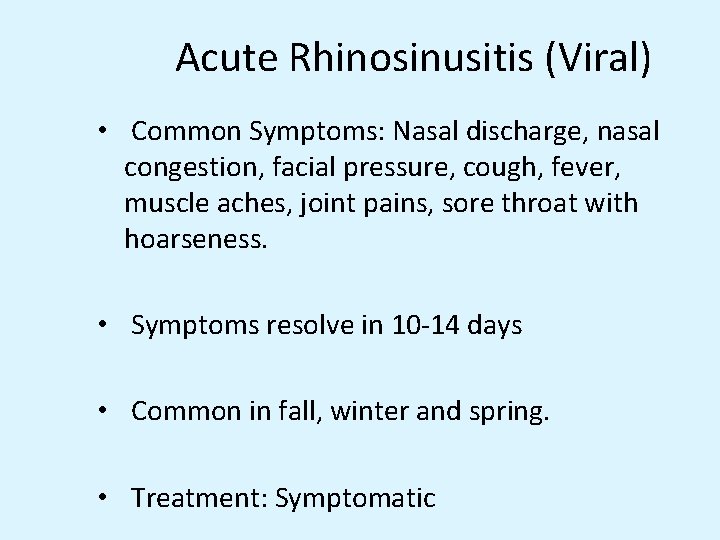
Acute Rhinosinusitis (Viral) • Common Symptoms: Nasal discharge, nasal congestion, facial pressure, cough, fever, muscle aches, joint pains, sore throat with hoarseness. • Symptoms resolve in 10 -14 days • Common in fall, winter and spring. • Treatment: Symptomatic
Acute Bacterial Sinusitis • Causative agents are usually the normal inhabitants of the respiratory tract. • Common agents: Streptococcus pneumoniae Nontypeable Haemophilus Influenzae Moraxella Catarrhalis
Diagnosis • Based on clinical signs and symptoms • Physical Exam: Palpate over the sinuses, look for structural abnormalities like DNS. • X-ray sinuses: not usually needed but may show cloudiness and air fluid levels • Limited coronal CT are more sensitive to inflammatory changes and bone destruction
Signs and Symptoms • Feeling of fullness and pressure over the involved sinuses, nasal congestion and purulent nasal discharge. • Other associated symptoms: Sore throat, malaise, low grade fever, headache, toothache, cough > 1 week duration. • Symptoms may last for more than 10 -14 days.

TM MANIFESTATIONS nasal drainage and congestion facial pain or pressure headache. Thick, purulent or discolored nasal discharge is often thought to indicate bacterial sinusitis, but it also occurs early in viral infections such as the common cold § Other nonspecific symptoms include cough, sneezing, and fever § Tooth pain, most often involving the upper molars, is associated with bacterial sinusitis § § § Dr. Farzin khorvash
TM MANIFESTATIONS § sinus pain or pressure often localizes and be worse when the patient bends over or is supine § symptoms of advanced sphenoid or ethmoid sinus: severe frontal or retroorbital pain radiating to the occiput, thrombosis of the cavernous sinus, and signs of orbital cellulitis § advanced frontal sinusitis , Pott's puffy tumor, swelling and pitting edema over the frontal bone , subperiosteal abscess Dr. Farzin khorvash
TM DIAGNOSIS § illness duration § acute bacterial sinusitis is uncommon in patients whose symptoms have lasted <7 days § facial or tooth pain in combination with purulent nasal discharge that have persisted for >7 days Dr. Farzin khorvash

TM DIAGNOSIS AND MANAGEMENT OF ACUTE SINUSITIS § Update of 2001 guideline § Focuses on ages 1– 18 years § Not subacute or chronic; not <1 year § Not anatomic abnormalities; immunodeficiencies, cystic fibrosis, ciliary dyskinesia
TM DIAGNOSIS AND MANAGEMENT OF ACUTE SINUSITIS Areas of change: 1. Addition of “worsening course” 2. New data on effectiveness of antibiotics 3. Option to observe for 3 days in “persistent” infection 4. Imaging is not necessary to identify or confirm a diagnosis of acute sinusitis
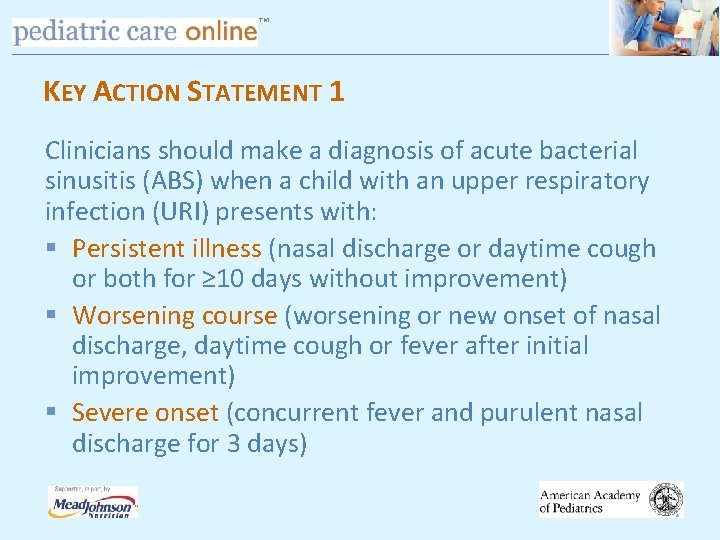
TM KEY ACTION STATEMENT 1 Clinicians should make a diagnosis of acute bacterial sinusitis (ABS) when a child with an upper respiratory infection (URI) presents with: § Persistent illness (nasal discharge or daytime cough or both for ≥ 10 days without improvement) § Worsening course (worsening or new onset of nasal discharge, daytime cough or fever after initial improvement) § Severe onset (concurrent fever and purulent nasal discharge for 3 days)
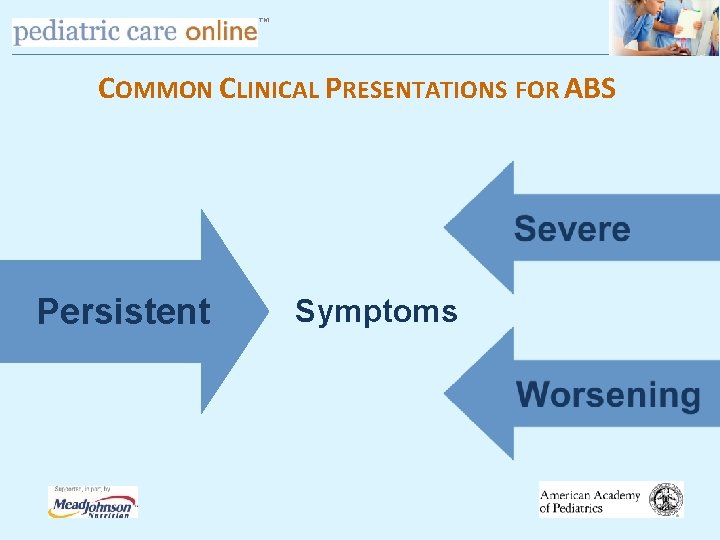
TM COMMON CLINICAL PRESENTATIONS FOR ABS Persistent Symptoms
TM ACUTE SINUSITIS “PERSISTENT SYMPTOMS” § 10– 30 days (no improvement) § Nasal discharge (any quality) § Daytime cough (worse at night) § Fever – variable § Headache and facial pain – variable
TM PERSISTENT SYMPTOMS § Only 6– 8% of children meet criteria Before concluding that child has sinusitis: § Differentiate between sequential episodes of URI and sinusitis § Establish that symptoms are NOT improving

TM ACUTE SINUSITIS “SEVERE SYMPTOMS” § High fever (T ≥ 39 o C) and § Purulent nasal discharge concurrently for at least 3– 4 days § Need to distinguish from uncomplicated viral infections with moderate illness

TM “WORSENING SYMPTOMS” § Typical viral URI symptoms § Nasal discharge or cough or both for 5– 6 days which is improving § Sudden worsening manifests as Increase nasal discharge or cough or both Onset of severe headache Onset of new fever
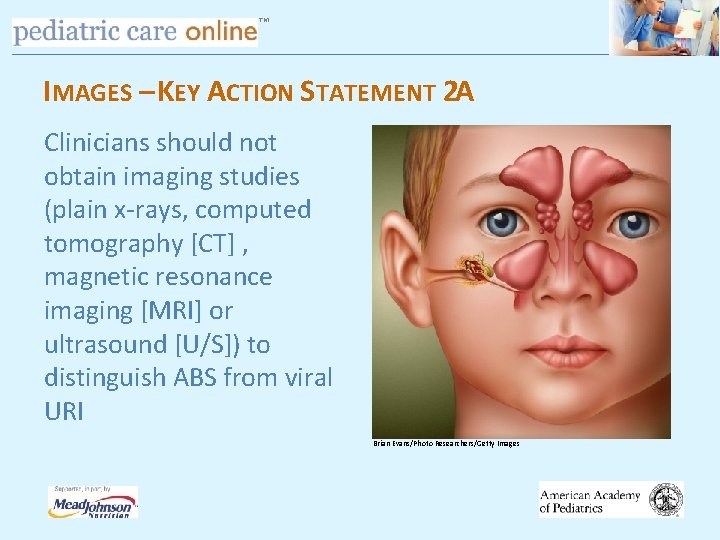
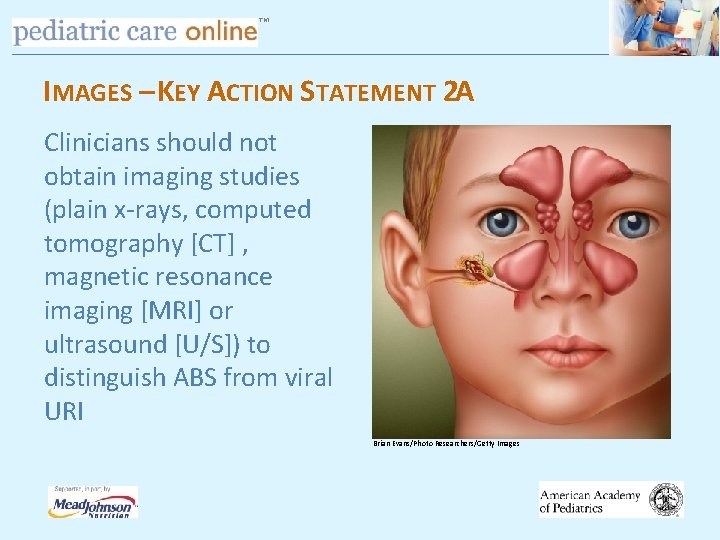
TM IMAGES – KEY ACTION STATEMENT 2 A Clinicians should not obtain imaging studies (plain x-rays, computed tomography [CT] , magnetic resonance imaging [MRI] or ultrasound [U/S]) to distinguish ABS from viral URI Brian Evans/Photo Researchers/Getty Images
TM IMAGES § Historically, imaging was confirmatory § No longer recommended § Continuity of respiratory mucosa leads to diffuse inflammation during viral URI § Responsible for controversy regarding images

TM COMPUTED TOMOGRAPHY, SINUS RADIOGRAPHY § patients who meet these criteria, only 40 to 50% have true bacterial sinusitis § CT or XR is not recommended for routine cases, particularly early in the course of illness (i. e. , at <7 days) § persistent, recurrent, or chronic sinusitis, CT of the sinuses is choice. Dr. Farzin khorvash
TM IMAGING OF SINUSES § 1940 s – Observations made regarding frequency of abnormal sinus radiographs in “healthy” children § 1970 s and 1980 s – Children with URI had frequent abnormalities of paranasal sinuses § As CT scanning of central nervous system (CNS) and skull became prevalent, incidental abnormalities observed § When MRI performed in children with URI, 70% show major abnormalities of mucosa
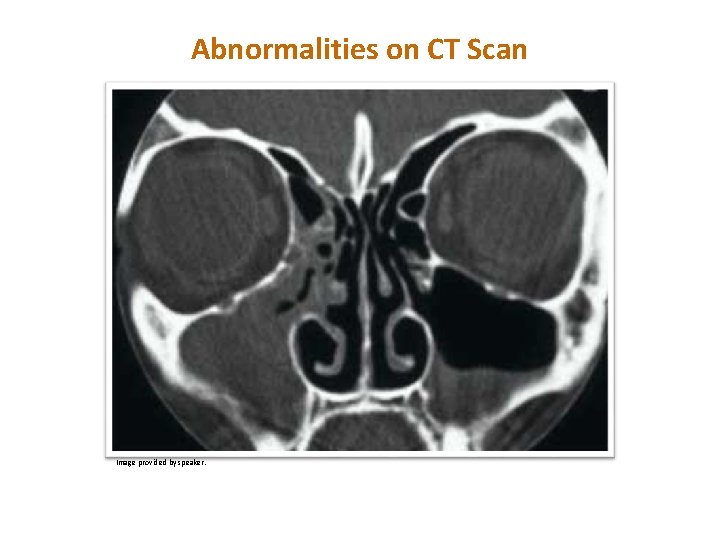
TM COMPUTED TOMOGRAPHIC STUDY OF THE COMMON COLD § 31 healthy young adults with new “cold” § Recruited within 48– 96 hours § To have CT of paranasal sinuses § 87% had significant abnormalities of their maxillary sinuses; with air-fluid level § Conclusion: Common cold associated with frequent and striking abnormalities of sinuses Gwaltney JM Jr, Phillips CD, Miller RD, et al. Computed tomography study of the common cold. N Engl J Med. 1994; 330(1): 25– 30

TM Image provided by speaker.
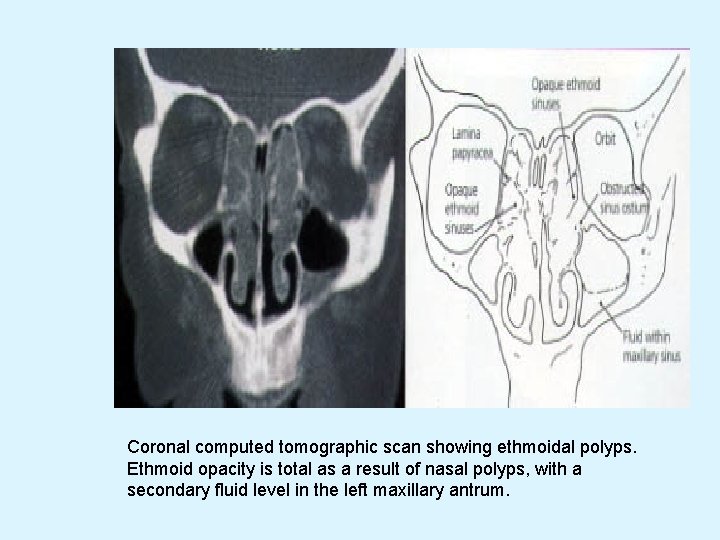
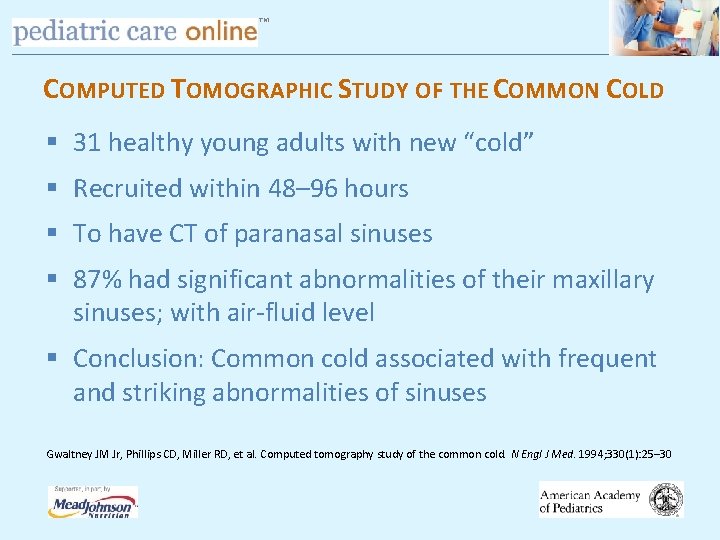
Coronal computed tomographic scan showing ethmoidal polyps. Ethmoid opacity is total as a result of nasal polyps, with a secondary fluid level in the left maxillary antrum.
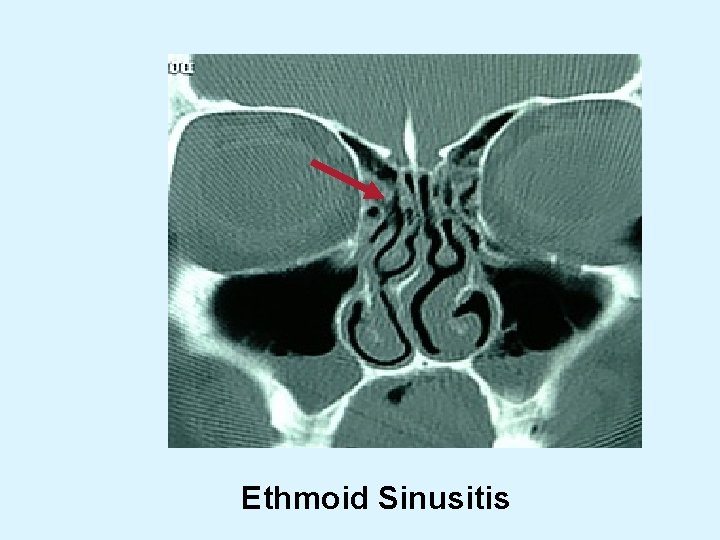
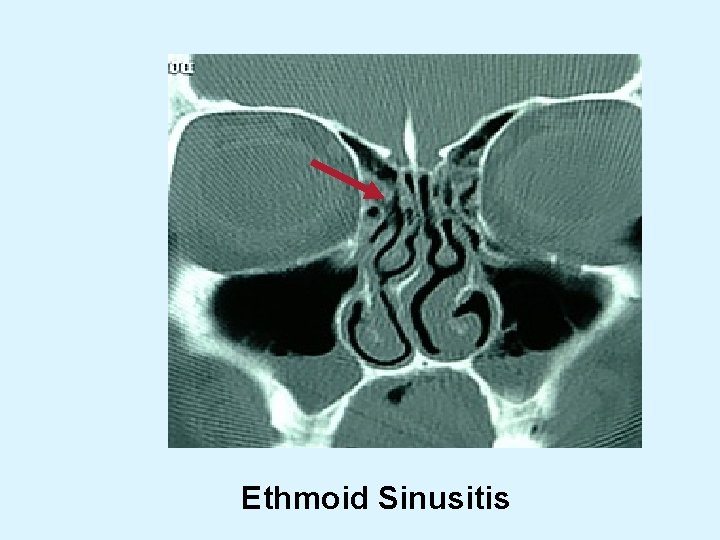
Ethmoid Sinusitis
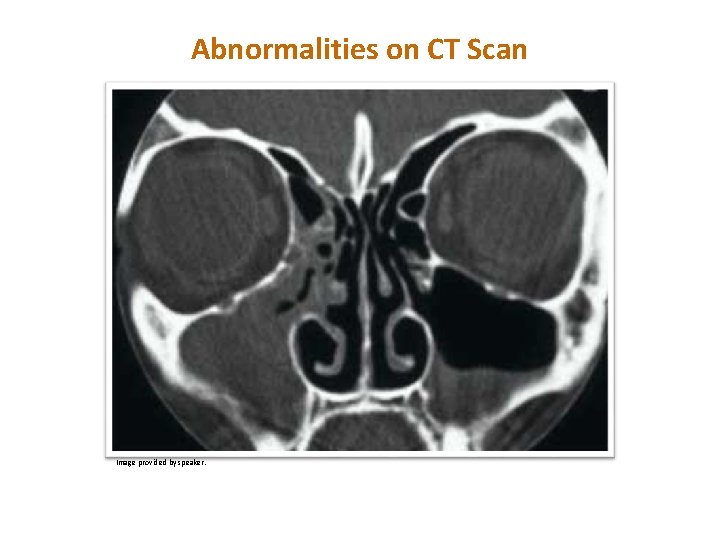
TM Abnormalities on CT Scan Image provided by speaker.
TM SUMMARY OF IMAGING § When paranasal sinuses are imaged in any way in children with uncomplicated URI, majority will be significantly abnormal § Normal images = No sinusitis § Abnormal images cannot confirm diagnosis and are not necessary in children with uncomplicated clinical sinusitis
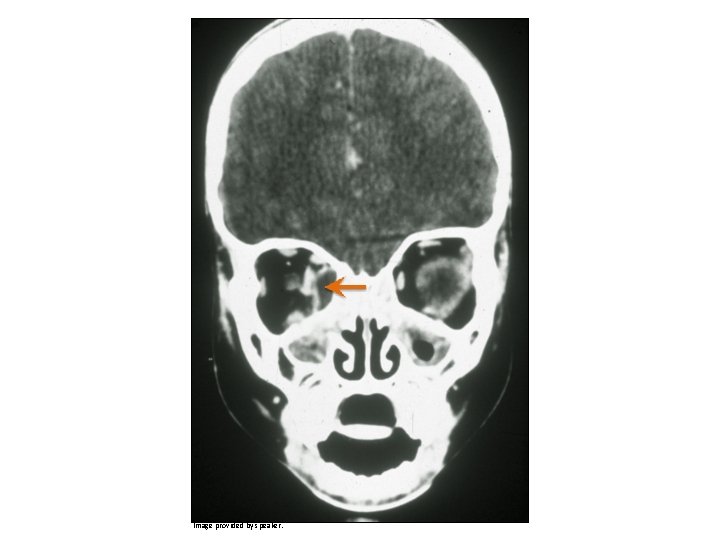
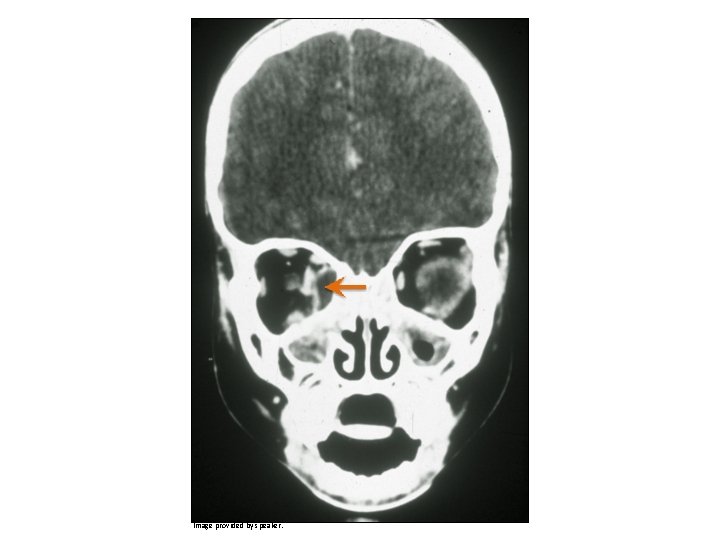
TM IMAGES – KEY ACTION STATEMENT 2 B Clinicians should obtain a contrast-enhanced CT scan of the paranasal sinuses and/or an MRI with contrast whenever a child is suspected of having orbital or CNS complications of ABS
TM COMPLICATIONS OF SINUSITIS Orbital a. sympathetic effusion b. subperiosteal abscess c. orbital abscess d. orbital cellulitis e. cavernous sinus thrombosis
TM ORBITAL COMPLICATIONS OF SINUSITIS § Proptosis – anterior and lateral displacement of globe § Impairment of extraocular movements § Loss of visual acuity § Chemosis – edema of conjunctiva

TM Image provided by speaker.

TM Image provided by speaker.

TM Image provided by speaker.

TM Image provided by speaker.
TM Image provided by speaker.

TM Image provided by speaker.

TM CNS COMPLICATIONS OF ABS Suspected with very severe headache, photophobia, seizure, other focal neurologic findings § Subdural empyema § Epidural empyema § Venous thrombosis § Brain abscess § Meningitis
TM INITIAL MANAGEMENT OF ABS § Key Action Statement 3 A: Clinician should prescribe antibiotic therapy for ABS in children with severe onset or worsening course § Key Action Statement 3 B: Clinician should either prescribe antibiotic therapy OR offer additional outpatient observation for 3 days to children with persistent illness
TM INITIAL MANAGEMENT OF ABS Guidance for clinician regarding management of children with persistent symptoms: Antibiotic therapy – starting as soon as possible after the encounter Additional outpatient observation – for 3 days with plan to begin antibiotics if child does not improve or worsens at any time

TM INITIAL MANAGEMENT OF ABS § Contrasts with 2001 AAP guideline § Acknowledges that although ABS is a bacterial infection spontaneous resolution ~ common 10 days is a guideline; no likely harm in allowing up to 3 more days in persistent onset § Reinforces antibiotic treatment as soon as possible in severe or worsening illness
TM TREATMENT § Most patients , improve without antibiotic therapy § mild to moderate symptoms of <7 days' duration § facilitating sinus drainage, such as oral and topical decongestants, nasal saline lavage § in patients with a history of chronic sinusitis or allergies — nasal glucocorticoids. Dr. Farzin khorvash
TM ANTIBIOTICS § § not improve after 7 days more severe symptoms (regardless of duration) Dr. Farzin khorvash
TM ANTIBIOTICS Empirical therapy , S. pneumoniae and H. influenzae amoxicillin drug-resistant S. pneumoniae Up to 10% of patients do not respond to initial antimicrobial therapy § these patients should be considered for sinus aspiration and/or lavage § prophylactic antibiotics to prevent episodes of recurrent acute bacterial sinusitis is not recommended. § § Dr. Farzin khorvash
TM KEY ACTION STATEMENT 4 Clinicians should prescribe amoxicillin with or without clavulanate as first-line treatment when a decision has been made to initiate antibiotic treatment of ABS
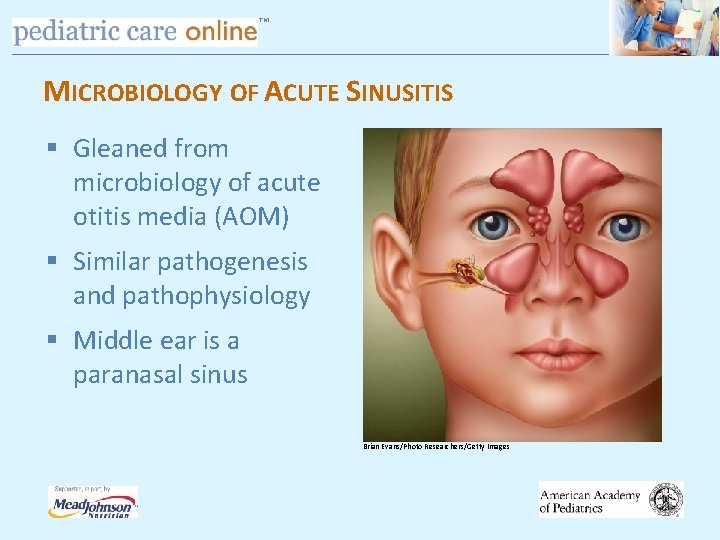
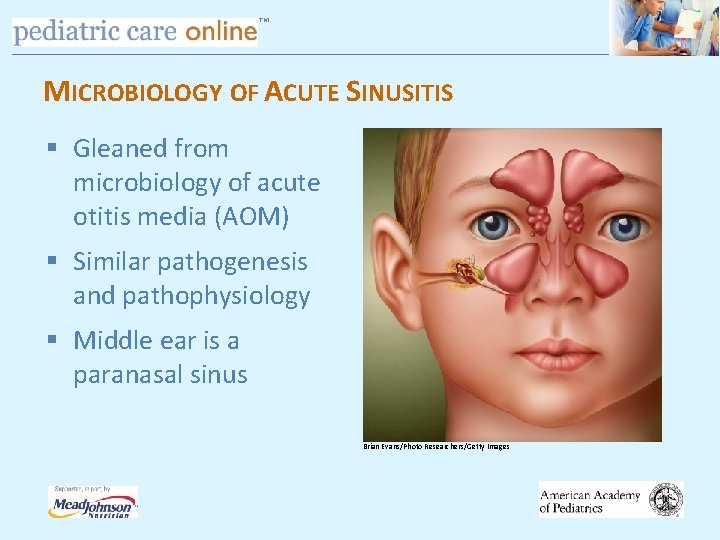
TM MICROBIOLOGY OF ACUTE SINUSITIS § Gleaned from microbiology of acute otitis media (AOM) § Similar pathogenesis and pathophysiology § Middle ear is a paranasal sinus Brian Evans/Photo Researchers/Getty Images
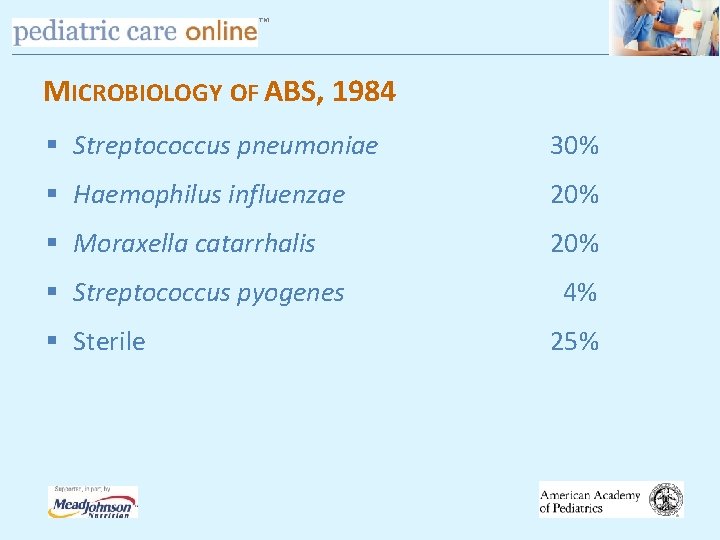
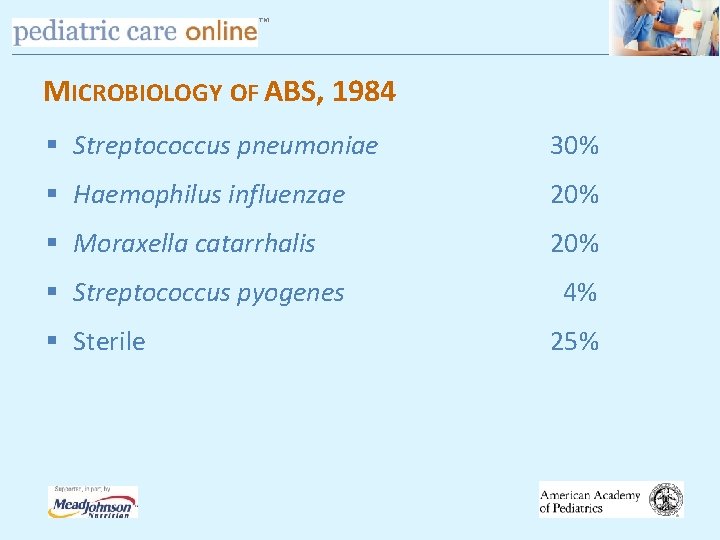
TM MICROBIOLOGY OF ABS, 1984 § Streptococcus pneumoniae 30% § Haemophilus influenzae 20% § Moraxella catarrhalis 20% § Streptococcus pyogenes § Sterile 4% 25%
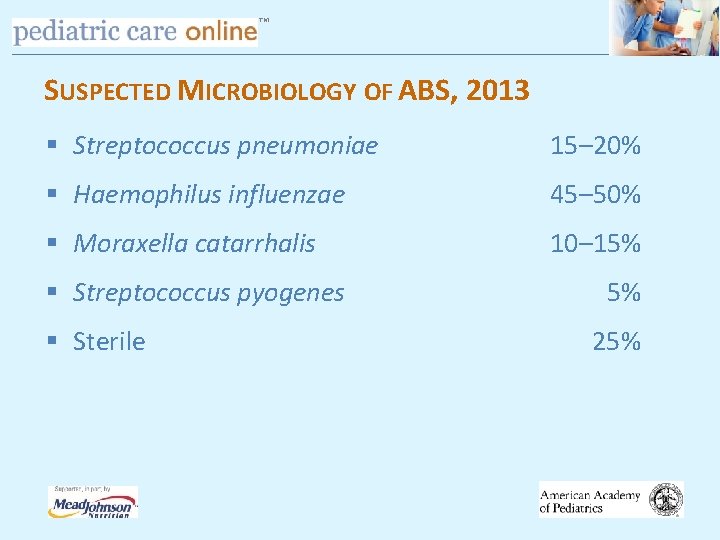
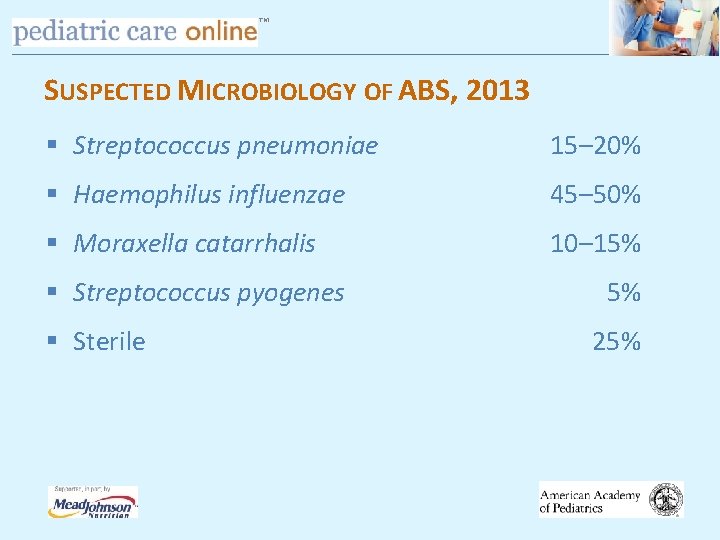
TM SUSPECTED MICROBIOLOGY OF ABS, 2013 § Streptococcus pneumoniae 15– 20% § Haemophilus influenzae 45– 50% § Moraxella catarrhalis 10– 15% § Streptococcus pyogenes § Sterile 5% 25%
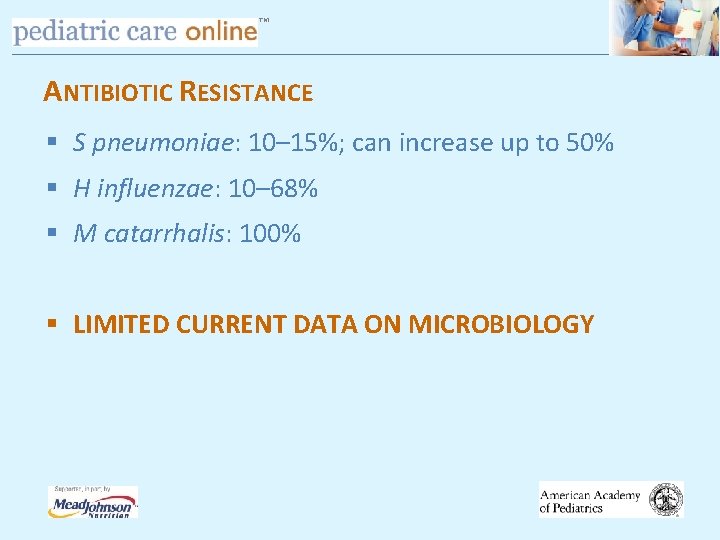
TM ANTIBIOTIC RESISTANCE § S pneumoniae: 10– 15%; can increase up to 50% § H influenzae: 10– 68% § M catarrhalis: 100% § LIMITED CURRENT DATA ON MICROBIOLOGY
Treatment • About 2/3 rd of patients will improve without treatment in 2 weeks. • Antibiotics: Reserved for patients who have symptoms for more than 10 days or who experience worsening symptoms. • OTC decongestant nasal sprays should be discouraged for use more than 5 days • Supportive therapy: Humidification, analgesics, antihistaminics
TM TREATMENT § Amoxicillin – traditional first-line therapy § Amoxicillin at 45 mg/kg/day in 2 doses § If high prevalence of penicillin-resistant S pneumoniae § Amoxicillin at 90 mg/kg/day in 2 doses

TM TREATMENT § Amoxicillin ineffective against beta-lactamase producing bacteria § Choices: drug inherently resistant to beta-lactamase combine amoxicillin with irreversible beta-lactamase inhibitor = K clavulanate
TM TREATMENT § If S pneumoniae remains low or continues to decrease and H influenzae remains high or continues to increase (including β-lactamase (+) strains) § Amoxicillin-clavulanate 45 mg/kg/day § Amoxicillin-clavulanate 90 mg/kg/day

TM TREATMENT § 50 mg/kg Ceftriaxone IV or IM Allergy: § Cephalosporins: cefdinir, cefuroxime, cefpodoxime § Clindamycin (or linezolid) + cefixime § Levofloxacin
TM TREATMENT § Optimal duration: no systematic study § Duration of therapy: 10, 14, 21, 28 days § Treat until patient is free of symptoms plus 7 days

TM KEY ACTION STATEMENT 5 A Clinicians should reassess initial management if there is caregiver report of worsening OR failure to improve within 72 hours

TM RESPONSE TO APPROPRIATE MANAGEMENT § Most patients with ABS who are treated with an appropriate antimicrobial agent respond promptly (within 48– 72 hours) § Worsening = progression of signs/symptoms § Failure to improve = not better or worse
TM KEY ACTION STATEMENT 5 B If worsening symptoms or failure to improve clinicians should change antibiotics or initiate antibiotics in child managed with observation
TM MANAGEMENT OF ABS AT 72 HOURS Whether or not antibiotics are used, a system must be in place to either add antibiotic or change the antibiotic if symptoms do not improve in 48– 72 hours

TM MANAGEMENT OF WORSENING OR NO IMPROVEMENT Initial Management Worse in 72 Hours No Improvement in 72 Hours Observation Amoxicillin + clavulanate Observation OR Initiate antibiotic Amoxicillin-clavulanate Observation OR Amoxicillin-clavulanate Clindamycin + cefixime OR Linezolid + cefixime OR Levofloxacin OR Cefuroxime, Cefdinir OR Cefpodoxime Amoxicillin-clavulanate OR Same choices as in preceding box

TM ADJUVANT THERAPIES – NO RECOMMENDATION § Antihistamines § Intranasal steroids § Intranasal saline § Decongestants
TM SUMMARY § Use stringent criteria to diagnose sinusitis in children § Avoid obtaining images § Amoxicillin with or without clavulanate § High-dose amoxicillin plus clavulanate for resistance (most comprehensive) § Adjuvant therapy rarely indicated

TM NOTE: § evidence of fungal hyphal elements and tissue invasion § acute nosocomial sinusitis should be confirmed by a sinus CT scan § sinus aspirate , if possible, for culture and susceptibility testing. Dr. Farzin khorvash
TM TREATMENT OF NOSOCOMIAL SINUSITIS § broad-spectrum antibiotics to cover common pathogens such as S. aureus and gram-negative bacilli § Therapy should then be tailored to the results of culture and susceptibility testing of sinus aspirates. Dr. Farzin khorvash
TM SURGICAL INTERVENTION AND INTRAVENOUS ANTIBIOTICS § severe disease § intracranial complications, such as abscess or orbital involvement § acute invasive fungal sinusitis usually require extensive surgical debridement § Intravenous antifungal such as amphotericin B Dr. Farzin khorvash
TM CHRONIC SINUSITIS symptoms of sinus inflammation lasting >12 weeks bacteria or fungi clinical cure in most cases is very difficult Many patients have undergone repeated courses of antibacterial agents and multiple sinus surgeries § increasing their risk of colonization with antibioticresistant pathogens and of surgical complications § § Dr. Farzin khorvash
TM CHRONIC BACTERIAL SINUSITIS § nasal congestion and sinus pressure, with intermittent periods for years § CT scan be helpful in defining the extent of disease and the response to therapy § endoscopic examinations and obtain tissue samples for histologic examination and culture. Dr. Farzin khorvash
TM CHRONIC BACTERIAL SINUSITIS § impairment of mucociliary clearance from repeated infections rather than to persistent bacterial infection § pathogenesis of this condition is poorly understood § certain conditions (e. g. , cystic fibrosis) § most patients do not have obvious underlying conditions that result in the obstruction of sinus drainage, the impairment of ciliary action, or immune dysfunction Dr. Farzin khorvash

TM CHRONIC FUNGAL SINUSITIS § immunocompetent hosts § usually noninvasive, although slowly progressive § Aspergillus species Dr. Farzin khorvash
TM CHRONIC FUNGAL SINUSITIS § § In mild, indolent disease repeated failures of antibacterial therapy only nonspecific mucosal changes may be seen on sinus CT Endoscopic surgery is usually curative in these patients, with no need for antifungal therapy Dr. Farzin khorvash
TM CHRONIC FUNGAL SINUSITIS § mycetoma (fungus ball) within the sinus § Treatment for this condition is also surgical § systemic antifungal therapy may be warranted in the rare case where bony erosion occurs. Dr. Farzin khorvash
TM CHRONIC FUNGAL SINUSITIS § allergic fungal sinusitis § history of nasal polyposis and asthma § thick, eosinophilic mucus with the consistency of peanut butter that contains sparse fungal hyphae on histologic examination. § Patients often present with pansinusitis. Dr. Farzin khorvash
TM TREATMENT § administration of intranasal glucocorticoids; and mechanical irrigation of the sinus with sterile saline solution § When this management approach fails, sinus surgery may be indicated Dr. Farzin khorvash

TM ACUTE PHARYNGITIS § Millions of visits § the majority by typical respiratory viruses § important is with group A ß-hemolytic Streptococcus (S. pyogenes), which can progress to acute rheumatic fever and acute glomerulonephritis § the risk for both of which can be reduced by timely penicillin therapy. Dr. Farzin khorvash

Acute Pharyngitis • Fewer than 25% of patients with sore throat have true pharyngitis. • Primarily seen in 5 -18 years old. Common in adult women.

Etiology A) Viral: Most common. Rhinovirus (most common). Symptoms usually last for 3 -5 days. B) Bacterial: Group A beta hemolytic streptococcus (GABHS). Early detection can prevent complications like acute rheumatic fever and post streptococcal GN.
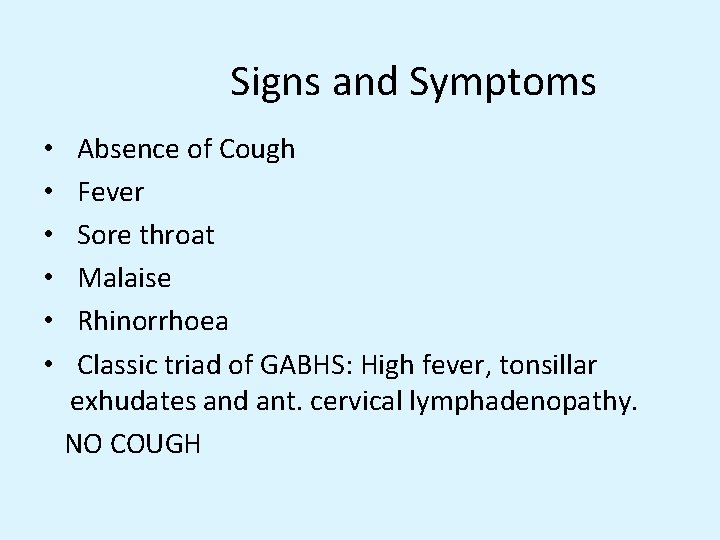
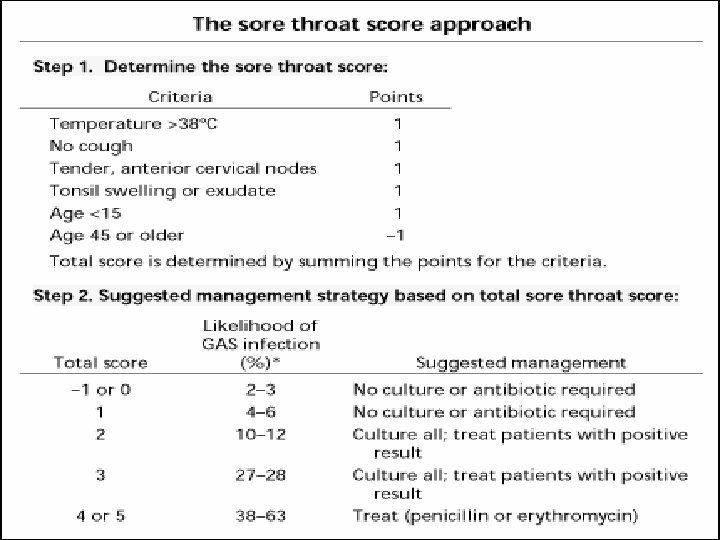
Signs and Symptoms • • • Absence of Cough Fever Sore throat Malaise Rhinorrhoea Classic triad of GABHS: High fever, tonsillar exhudates and ant. cervical lymphadenopathy. NO COUGH

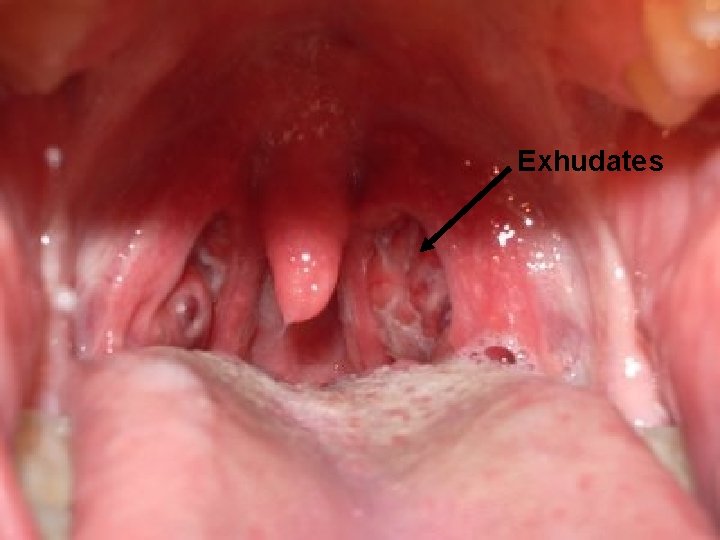
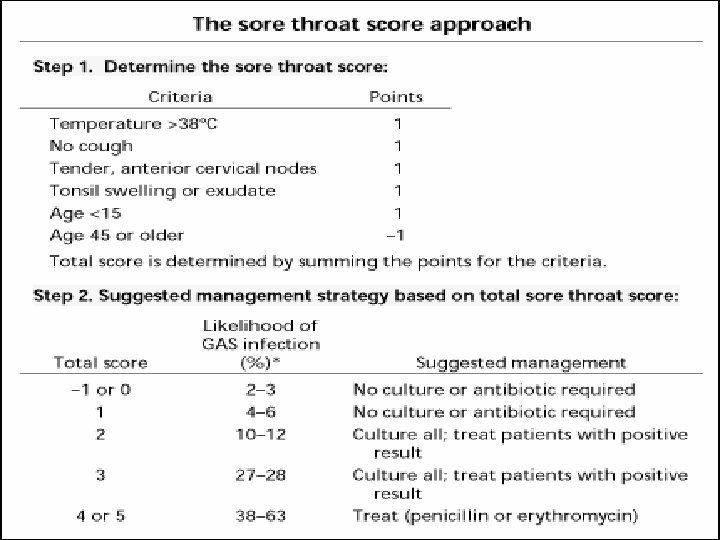
Diagnosis • Physical Exam: Tonsillar exhudates, anterior cervical LAD • Rapid strep: Throat swab. Sensitivity of 80% and specificity of 95%. Throat Cultures: Not required usually. Needed only when suspicion is high and rapid strep is negative.
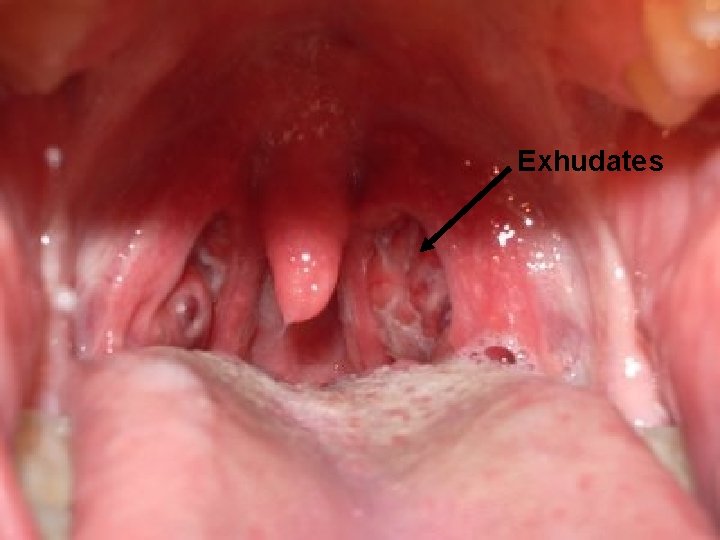
Exhudates
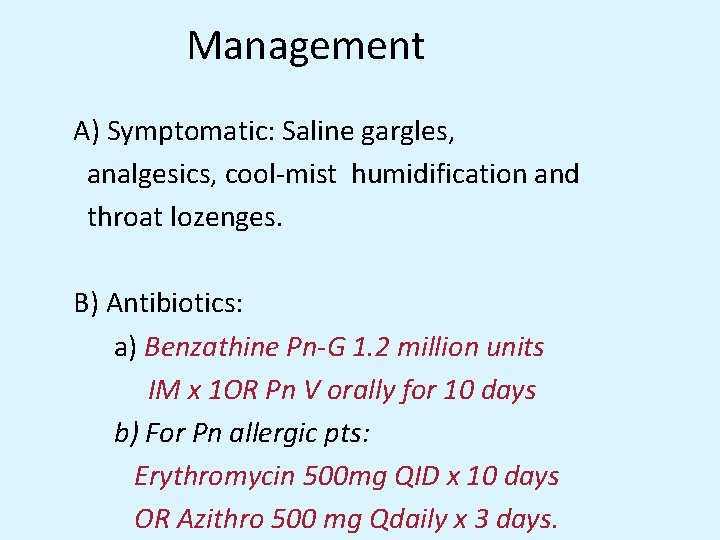
Management A) Symptomatic: Saline gargles, analgesics, cool-mist humidification and throat lozenges. B) Antibiotics: a) Benzathine Pn-G 1. 2 million units IM x 1 OR Pn V orally for 10 days b) For Pn allergic pts: Erythromycin 500 mg QID x 10 days OR Azithro 500 mg Qdaily x 3 days.
TM ACUTE BACTERIAL PHARYNGITIS § § § § § S. pyogenes, (~5 to 15% of all cases ) children 5 to 15 years of age Streptococci of groups C and G account Neisseria gonorrhoeae Corynebacterium diphtheriae Corynebacterium ulcerans Yersinia enterocolitica Treponema pallidum (in secondary syphilis) M. pneumoniae C. pneumoniae Dr. Farzin khorvash
TM ANAEROBIC BACTERIA § Vincent's angina § can contribute to more serious polymicrobial infections § peritonsillar or retropharyngeal abscess Dr. Farzin khorvash
TM COMPLICATIONS § rheumatic feveracute § glomerulonephritis § numerous suppurative conditions, such as peritonsillar abscess , otitis media, mastoiditis, sinusitis, bacteremia, and pneumonia § Therapy of acute streptococcal pharyngitis can prevent the development of rheumatic fever § no evidence that it can prevent acute glomerulonephritis Dr. Farzin khorvash
TM TREATMENT § Antibiotic benefit: S. pyogenes § a decrease in the risk of rheumatic fever § rheumatic fever is now a rare disease, even in untreated patients § When therapy is started within 48 h of illness onset, however, symptom duration is also decreased. § reduce the spread of streptococcal pharyngitis, overcrowding or close contact Dr. Farzin khorvash
TM STREPTOCOCCAL PHARYNGITIS single dose of intramuscular benzathine penicillin 10 -day course of oral penicillin Erythromycin : penicillin Testing for cure is unnecessary and may reveal only chronic colonization. § Penicillin prophylaxis (benzathine penicillin G, 1. 2 million units intramuscularly every 3 to 4 weeks) for patients at risk of recurrent rheumatic fever § § Dr. Farzin khorvash
Non specific URI’s • Common Cold • Etiology: Rhinovirus Adenovirus RSV Parainfluenza Enteroviruses Diagnosis: Clinical Treatment: Adequate fluid intake, rest, humidified air, and over-the-counter analgesics and antipyretics.

Influenza • Etiology: Influenza A & B • Symptoms: Fever, myalgias, headache, rhinitis, malaise, nonproductive cough, sore throat • Diagnosis: Influenza A &B antigen testing • Treatment: Supportive care, oseltamivir, amantidine
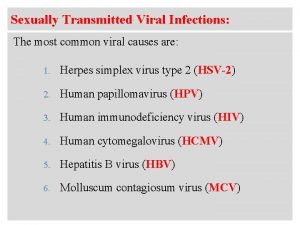
TM ETIOLOGY § 30% have no identified cause. § Respiratory viruses : rhinoviruses , coronaviruses Influenza virus, parainfluenza virus, and adenovirus the latter as part of the more clinically severe syndrome of pharyngoconjunctival fever § HSV types 1 and 2, coxsackievirus A, CMV, EBV § Acute HIV infection Dr. Farzin khorvash
TM MANIFESTATIONS § viruses : not severe and is typically associated with a constellation of coryzal symptoms § Findings on physical examination are uncommon; § fever is rare, § tender cervical adenopathy and pharyngeal exudates are not seen. Dr. Farzin khorvash
TM MANIFESTATIONS § influenza virus can be severe with fever as well as with myalgias, headache, and cough § pharyngoconjunctival fever due to adenovirus infection is similar § Since pharyngeal exudate may be present on examination § adenoviral pharyngitis is distinguished by the presence of conjunctivitis in one-third to one-half of patients. Dr. Farzin khorvash
TM MANIFESTATIONS § primary HSV : mimic streptococcal pharyngitis in some cases, with pharyngeal inflammation and exudate § vesicles and shallow ulcers on the palate § coxsackievirus ( herpangina): small vesicles that develop on the soft palate and uvula and then rupture to form shallow white ulcers Dr. Farzin khorvash
TM INFECTIOUS MONONUCLEOSIS § Acute exudative pharyngitis coupled with fever, fatigue, generalized lymphadenopathy, splenomegaly § CMV, EBV Dr. Farzin khorvash
TM HIV § § § fever acute pharyngitis myalgias, arthralgias, malaise nonpruritic maculopapular rash lymphadenopathy mucosal ulcerations without exudate. Dr. Farzin khorvash

TM STREPTOCOCCI A, C, AND G § ranging from a relatively mild illness without many accompanying symptoms to clinically severe cases § pharyngeal pain, fever, chills, and abdominal pain § A hyperemic pharyngeal membrane with tonsillar hypertrophy and exudate is usually seen § tender anterior cervical adenopathy § Coryzal manifestations, including cough, are typically absent Dr. Farzin khorvash
TM SCARLET FEVER § Strains of S. pyogenes that generate erythrogenic toxin § characterized by an erythematous rash and strawberry tongue Dr. Farzin khorvash
TM DIAGNOSIS § Throat swab culture § Rapid antigen-detection tests offer good specificity (>90%) but lower sensitivity that varies across the clinical spectrum of disease (65 to 90%) Dr. Farzin khorvash
TM RADT § all negative rapid antigen-detection tests in children be confirmed by a throat culture § do not recommend backup culture when adults have a negative rapid antigen-detection test Dr. Farzin khorvash

TM DIAGNOSIS § Cultures and rapid diagnostic tests for influenza virus, adenovirus, HSV, EBV 9, CMV, and M. pneumoniae, are available § the monospot test for EBV § HIV RNA or antigen (p 24) when acute primary HIV infection § cultures : N. gonorrhoeae, C. diphtheriae, or Y. enterocolitica Dr. Farzin khorvash
TM INFLUENZA VIRUS § amantadine, rimantadine, and the two newer agents oseltamivir and zanamivir § All of these agents need to be started within 36 to 48 h of symptom onset to reduce illness duration meaningfully § Of these agents, only oseltamivir and zanamivir are active against both influenza A and influenza B Dr. Farzin khorvash

TM PERITONSILLAR ABSCESS § § § severe pharyngeal pain dysphagia, fever, medial displacement of the tonsil therapy : Oral penicillin , with clindamycin as an alternative Early use of antibiotics in these cases has substantially reduced the need for surgical drainage Dr. Farzin khorvash
TM VINCENT'S ANGINA § acute necrotizing ulcerative gingivitis § painful, inflamed gingiva § ulcerations of the interdental papillae that bleed easily § halitosis , fever, malaise, and lymphadenopathy § oral anaerobes § Treatment : debridement and oral penicillin + metronidazole § clindamycin alone as an alternative. Dr. Farzin khorvash
TM LUDWIG'S ANGINA § is a rapidly progressive, potentially fulminant cellulitis involving the sublingual and submandibular spaces § typically originates from an infected or recently extracted tooth, most commonly the lower second and third molars § dysphagia, odynophagia, and "woody" edema in the sublingual region, forcing the tongue up and back with the potential for airway obstruction. § Fever, dysarthria, and drooling , speak in a "hot potato" voice Dr. Farzin khorvash

TM TREATMENT § Intubation or tracheostomy may be necessary to secure the airway § asphyxiation is the most common cause of death § monitored closely and intravenous antibiotics directed against streptococci and oral anaerobes § ampicillin/sulbactam § high-dose penicillin plus metronidazole. Dr. Farzin khorvash
TM POSTANGINAL SEPTICEMIA (LEMIERRE'S DISEASE) § oropharyngeal infection by Fusobacterium necrophorum § starts as a sore throat (most commonly in adolescents and young adults), exudative tonsillitis or peritonsillar abscess Dr. Farzin khorvash
TM § Infection of the deep pharyngeal tissue allows organisms to drain into the lateral pharyngeal space § which contains the carotid artery and internal jugular vein § Septic thrombophlebitis of the internal jugular vein: pain, dysphagia, and neck swelling and stiffness Dr. Farzin khorvash
TM § Sepsis occurs 3 to 10 days after the onset § metastatic infection to the lung and other distant sites § extend along the carotid sheath and into the posterior mediastinum § mediastinitis, erode into the carotid artery, with the early sign of repeated small bleeds into the mouth § The mortality rate as 50% § Treatment : intravenous antibiotics (penicillin G or clindamycin) and surgical drainage § The concomitant use of anticoagulants to prevent embolization remains controversial but is often advised. Dr. Farzin khorvash

TM LARYNGITIS § inflammatory process involving the larynx § are acute § by the same viruses responsible for many other URI Dr. Farzin khorvash
TM ETIOLOGY § rhinovirus, influenza virus, parainfluenza virus, adenovirus, coxsackievirus, coronavirus, and RSV § acute bacterial respiratory infections, such as group A Streptococcus or C. diphtheriae , M. catarrhalis Dr. Farzin khorvash
TM CHRONIC LARYNGITIS § Mycobacterium tuberculosis § Histoplasma and Blastomyces may cause laryngitis § Candida species : thrush or esophagitis and particularly in immunosuppressed patients § to Coccidioides and Cryptococcus. Dr. Farzin khorvash
TM MANIFESTATIONS § hoarseness § other symptoms and signs of URI, including rhinorrhea, nasal congestion, cough, and sore throat § Direct laryngoscopy : diffuse laryngeal erythema and edema, along with vascular engorgement of the vocal folds § tuberculous laryngitis, mucosal nodules and ulcerations visible on laryngoscopy § these lesions are sometimes mistaken for laryngeal cancer Dr. Farzin khorvash
TM TREATMENT § humidification § voice rest § Antibiotics are not recommended except when group A Streptococcus is cultured § chronic laryngitis usually requires biopsy with culture. § Patients with laryngeal tuberculosis are highly contagious Dr. Farzin khorvash

TM CROUP § viral respiratory illnesses § characterized by marked swelling of the subglottic region of the larynx § Croup primarily affects children <6 years old Dr. Farzin khorvash
TM EPIGLOTTITIS § Acute epiglottitis : acute, rapidly progressive cellulitis of the epiglottis and adjacent § airway obstruction in both children and adults § Before the widespread use of H. influenzae type b (Hib) vaccine, this entity was much more common among children, with a peak incidence at ~3. 5 years of age § a medical emergency, particularly in children, and prompt diagnosis and airway protection are of utmost importance. Dr. Farzin khorvash
TM ETIOLOGY § § § Hib 12 group A Streptococcus S. pneumoniae Haemophilus parainfluenzae S. aureus Viruses have not yet been established as a cause of acute epiglottitis. Dr. Farzin khorvash

TM MANIFESTATIONS § more acutely in young children than in adolescents or adults § On presentation, most children have had symptoms for <24 h, including high fever, severe sore throat, tachycardia, systemic toxicity, and drooling while sitting forward § Symptoms and signs of respiratory obstruction may also be present and may progress rapidly Dr. Farzin khorvash
TM PHYSICAL EXAMINATION § moderate or severe respiratory distress § inspiratory stridor and retractions of the chest wall § These findings diminish as the disease progresses and the patient tires Dr. Farzin khorvash
TM DIAGNOSIS § often made on clinical grounds § direct fiberoptic laryngoscopy is frequently performed in a controlled environment : "cherry-red" epiglottis and to facilitate placement of an endotracheal tube § Direct visualization in an examination room (e. g. , with a tongue blade and indirect laryngoscopy) is not recommended Dr. Farzin khorvash
TM § Lateral neck radiographs and laboratory tests § but may delay the critical securing of the airway § Neck radiographs : enlarged edematous epiglottis (the "thumbprint sign"), usually with a dilated hypopharynx and normal subglottic structures. § Laboratory tests : mild to moderate leukocytosis with a predominance of neutrophils § Blood cultures are positive in a significant proportion of cases. Dr. Farzin khorvash
TM TREATMENT § Security of the airway § blood and epiglottis specimens have been obtained for culture § intravenous antibiotics, particularly H. influenzae § Because rates of ampicillin resistance in this organism have risen § therapy : a ß-lactam/ß-lactamase inhibitor combination or a second- or third-generation cephalosporin Dr. Farzin khorvash
TM § ampicillin/sulbactam, cefuroxime, cefotaxime, or ceftriaxone § clindamycin and TMP-SMX reserved for patients allergic to ß-lactams § continued for 7 to 10 days § household contacts of a patient with H. influenzae epiglottitis include an unvaccinated child under the age of 4, all members of the household (including the patient) should receive prophylactic rifampin for 4 days to eradicate H. influenzae carriage. Dr. Farzin khorvash
TM RETROPHARYNGEAL ABSCESS § sore throat, fever, dysphagia, and neck pain and are often drooling , pain with swallowing § tender cervical adenopathy, neck swelling, and diffuse erythema and edema of the posterior pharynx , bulge in the posterior pharyngeal wall § A soft tissue mass : by lateral neck radiography or CT § Because of the risk of airway obstruction, treatment begins with securing of the airway § combination of surgical drainage and intravenousantibiotic administration Dr. Farzin khorvash
TM RETROPHARYNGEAL ABSCESS § streptococci, oral anaerobes, and S. aureus § ampicillin/sulbactam, clindamycin alone, or clindamycin plus ceftriaxone § Complications : rupture into the posterior pharynx, which may lead to aspiration pneumonia and empyema § Extension may also occur to the lateral pharyngeal space and mediastinum: mediastinitis and pericarditis § or into nearby major blood vessels Dr. Farzin khorvash
Questions?
 Rhinosinusitis
Rhinosinusitis An acute highly contagious viral disease
An acute highly contagious viral disease Ethmoid sinus anatomy
Ethmoid sinus anatomy Acute tubular necrosis causes
Acute tubular necrosis causes Differentiation syndrome
Differentiation syndrome Dr rista
Dr rista Tender nipples sign of early pregnancy
Tender nipples sign of early pregnancy Olfactory groove keros classification
Olfactory groove keros classification Ombl radiography
Ombl radiography Palpate frontal and maxillary sinuses
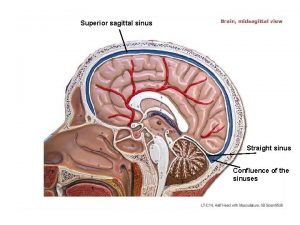
Palpate frontal and maxillary sinuses Dural venous sinuses
Dural venous sinuses Blood supply of mediastinum
Blood supply of mediastinum Gray matter and white matter
Gray matter and white matter Atrioventricular orifice
Atrioventricular orifice Superficial palmar arch
Superficial palmar arch Paranasal sinuses
Paranasal sinuses Sinuses
Sinuses Human heart border
Human heart border Ethmoidal infundibulum
Ethmoidal infundibulum Pericardial cavity
Pericardial cavity Chapter 18 common chronic and acute conditions
Chapter 18 common chronic and acute conditions Aerochamber definition
Aerochamber definition Vrus
Vrus Section 24-1 viral structure and replication
Section 24-1 viral structure and replication Inklüzyon cisimcikleri
Inklüzyon cisimcikleri Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Viral inoculation in embryonated egg
Viral inoculation in embryonated egg Egg inoculation technique
Egg inoculation technique Spasmodic croup
Spasmodic croup Dea anggraini viral
Dea anggraini viral Morfologia viral
Morfologia viral Sample rejection criteria
Sample rejection criteria Meningitis
Meningitis Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever Ciclo viral
Ciclo viral Capsid capsomere
Capsid capsomere Viral
Viral Viral recombination
Viral recombination Vaccins à vecteur viral
Vaccins à vecteur viral Viral receptors
Viral receptors Streptococcus
Streptococcus Equine viral rhinopneumonitis
Equine viral rhinopneumonitis Viral dna
Viral dna Rotarix live attenuated
Rotarix live attenuated Viral entry
Viral entry The dynamics of viral marketing
The dynamics of viral marketing Hgado
Hgado Menigitis csf
Menigitis csf Viral arthritis
Viral arthritis Viral life cycle
Viral life cycle Antiperytique
Antiperytique Viral shedding
Viral shedding Eline's viral
Eline's viral Viral communications
Viral communications Viral integration
Viral integration Vacina trplice viral
Vacina trplice viral Lowest common denominator and greatest common factor
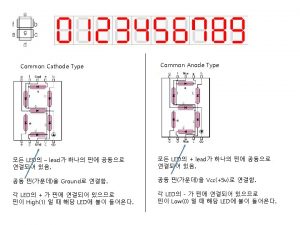
Lowest common denominator and greatest common factor Common anode and common cathode
Common anode and common cathode Common factors and common multiples
Common factors and common multiples Lowest common factor
Lowest common factor Lcm of 48 and 60
Lcm of 48 and 60 Multiples of 9 and 21
Multiples of 9 and 21 Name 2 objects with acute angles
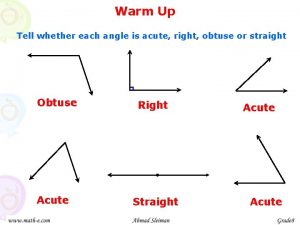
Name 2 objects with acute angles Angioectasia icd 10
Angioectasia icd 10 Angles name
Angles name Acute glomerulonephritis causes
Acute glomerulonephritis causes Classifying triangles and quadrilaterals
Classifying triangles and quadrilaterals Acute bronchospasm
Acute bronchospasm An acute angled isosceles triangle
An acute angled isosceles triangle Real life example of angle
Real life example of angle Right triangles congruence theorems
Right triangles congruence theorems Spasmodic croup
Spasmodic croup Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Respiratory acidosis
Respiratory acidosis Acute tubular necrosis
Acute tubular necrosis Acute glomerulonephritis causes
Acute glomerulonephritis causes Square rectangle rhombus trapezoid
Square rectangle rhombus trapezoid Negative explanatory style
Negative explanatory style Acute angle closure glaucoma
Acute angle closure glaucoma Diagnosis of post traumatic stress disorder
Diagnosis of post traumatic stress disorder Globulin function
Globulin function What is a negative acute phase protein
What is a negative acute phase protein Acute inflammation
Acute inflammation Acute cholecystitis clinical features
Acute cholecystitis clinical features Pagwash
Pagwash Acute resuscitation plan form
Acute resuscitation plan form Moderate acute malnutrition
Moderate acute malnutrition Pancreatic pseudocyst diet
Pancreatic pseudocyst diet Acute interstitial nephritis urine findings
Acute interstitial nephritis urine findings Urinalysis
Urinalysis Parietal pain
Parietal pain Acute spasmodic laryngitis
Acute spasmodic laryngitis Inflammation
Inflammation Ukons triage tool version 3
Ukons triage tool version 3 Cellular events of acute inflammation
Cellular events of acute inflammation Cardinal features
Cardinal features Granuloom long
Granuloom long Health hazards pictogram
Health hazards pictogram Classify each triangle as acute equiangular obtuse or right
Classify each triangle as acute equiangular obtuse or right Gallstone anatomy
Gallstone anatomy Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Stroke protocol
Stroke protocol Acute subacute chronic
Acute subacute chronic Gall bladder drawing
Gall bladder drawing Magnesium sulfate and urine output
Magnesium sulfate and urine output Site:slidetodoc.com
Site:slidetodoc.com Malnutrition case study
Malnutrition case study Acute blood loss anemia
Acute blood loss anemia Acute spasmodic laryngitis
Acute spasmodic laryngitis Chapter 10 sentence check 2 answers
Chapter 10 sentence check 2 answers Acute intermittent porphyria
Acute intermittent porphyria Sns neurotransmitters
Sns neurotransmitters 4th stage renal failure
4th stage renal failure Types of aim
Types of aim Acute specific surgical infection
Acute specific surgical infection Acute pancreatitis diagnosis criteria
Acute pancreatitis diagnosis criteria Fhf
Fhf Cushings triad
Cushings triad Hepatic encephalopathy stages
Hepatic encephalopathy stages Vascular response in acute inflammation
Vascular response in acute inflammation Cellular events of acute inflammation
Cellular events of acute inflammation Acute defenition
Acute defenition Stages of appendicitis
Stages of appendicitis