Anatomy of Blood Vessels Tunics of blood vessel
Anatomy of Blood Vessels
• Tunics of blood vessel walls • Artery, vein, capillary structural differences correlated to functional differences • Artery and vein cross-sections • Major arteries and veins • Local, nervous system, and hormonal control of blood flow and BP
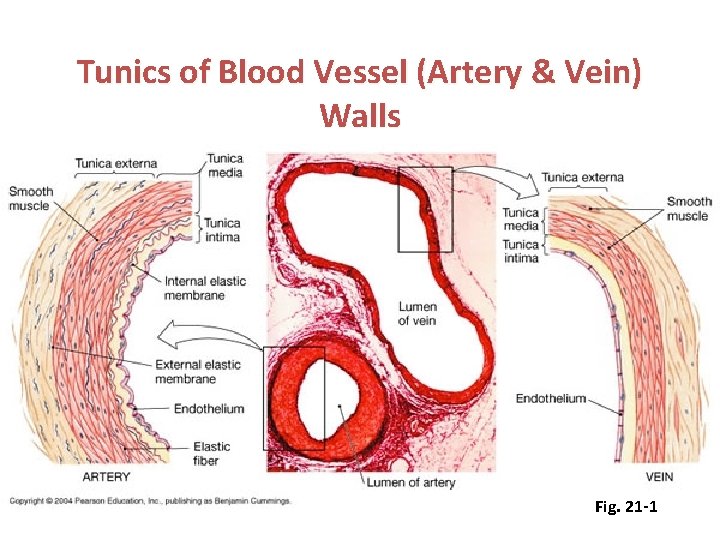
Tunics of Blood Vessel (Artery & Vein) Walls Fig. 21 -1
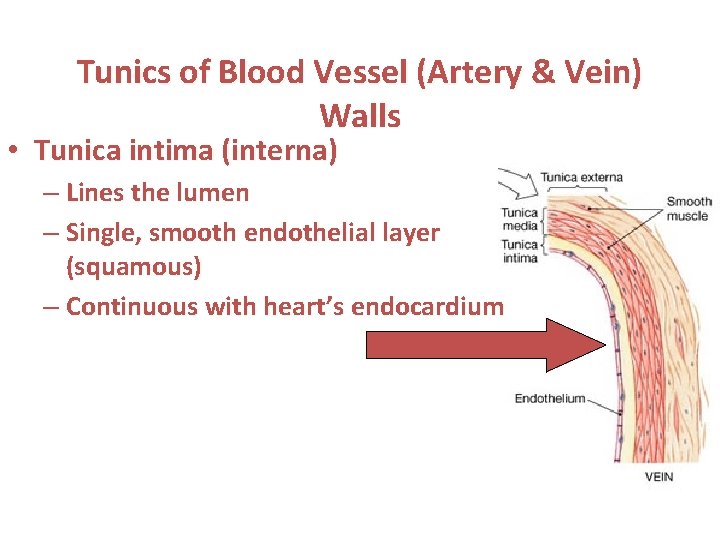
Tunics of Blood Vessel (Artery & Vein) Walls • Tunica intima (interna) – Lines the lumen – Single, smooth endothelial layer (squamous) – Continuous with heart’s endocardium
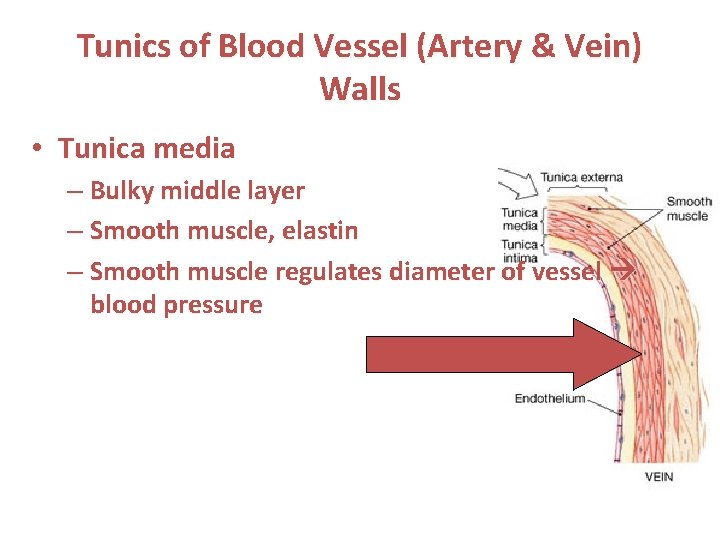
Tunics of Blood Vessel (Artery & Vein) Walls • Tunica media – Bulky middle layer – Smooth muscle, elastin – Smooth muscle regulates diameter of vessel blood pressure
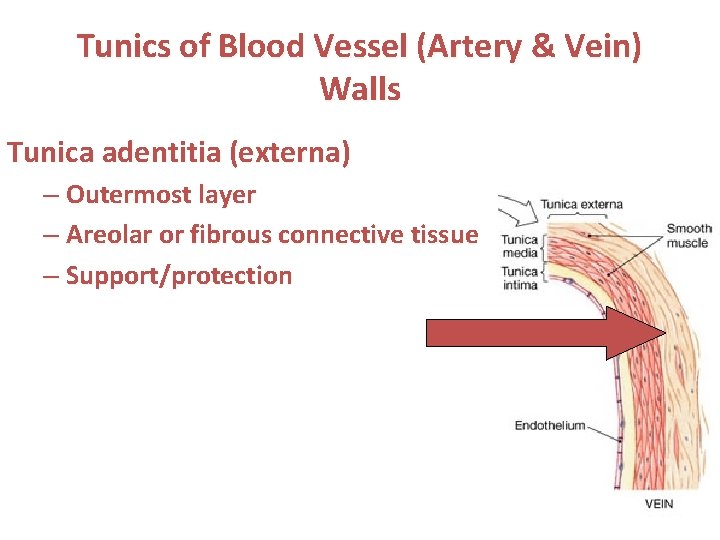
Tunics of Blood Vessel (Artery & Vein) Walls Tunica adentitia (externa) – Outermost layer – Areolar or fibrous connective tissue – Support/protection
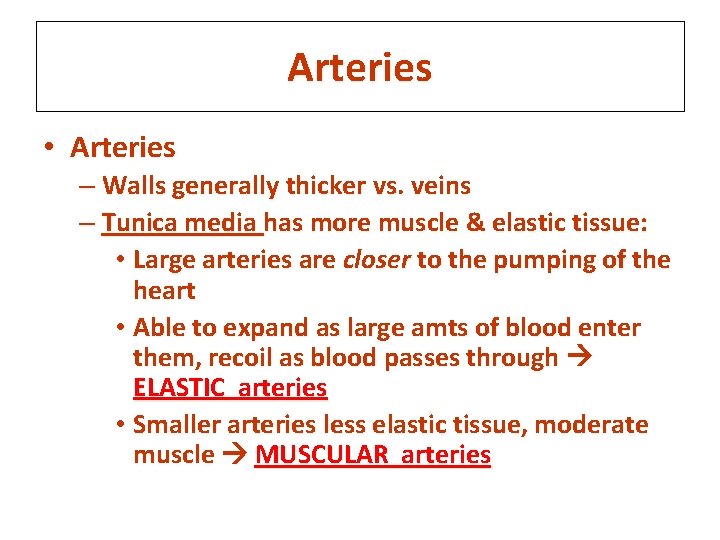
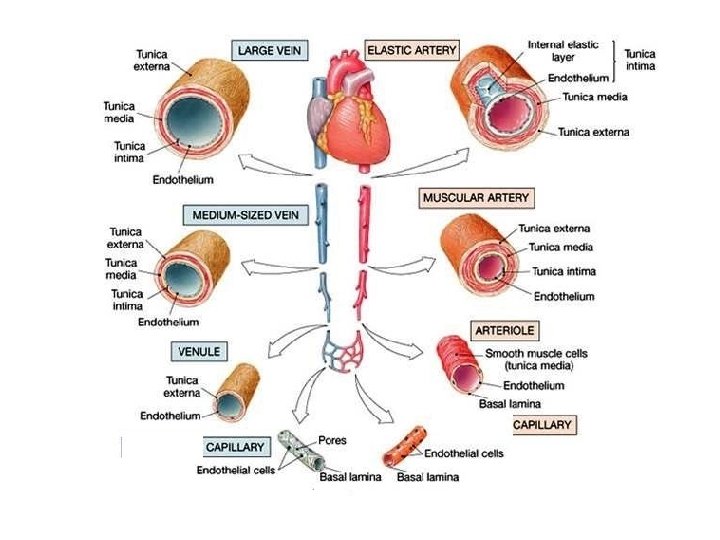
Arteries • Arteries – Walls generally thicker vs. veins – Tunica media has more muscle & elastic tissue: • Large arteries are closer to the pumping of the heart • Able to expand as large amts of blood enter them, recoil as blood passes through ELASTIC arteries • Smaller arteries less elastic tissue, moderate muscle MUSCULAR arteries
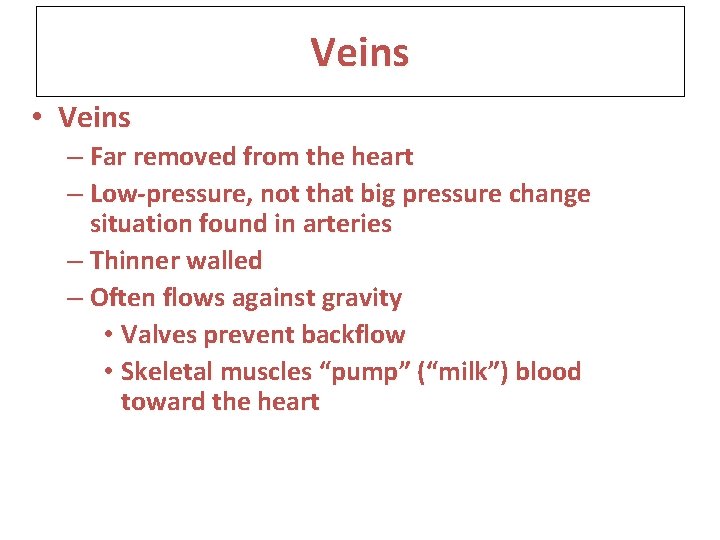
Veins • Veins – Far removed from the heart – Low-pressure, not that big pressure change situation found in arteries – Thinner walled – Often flows against gravity • Valves prevent backflow • Skeletal muscles “pump” (“milk”) blood toward the heart
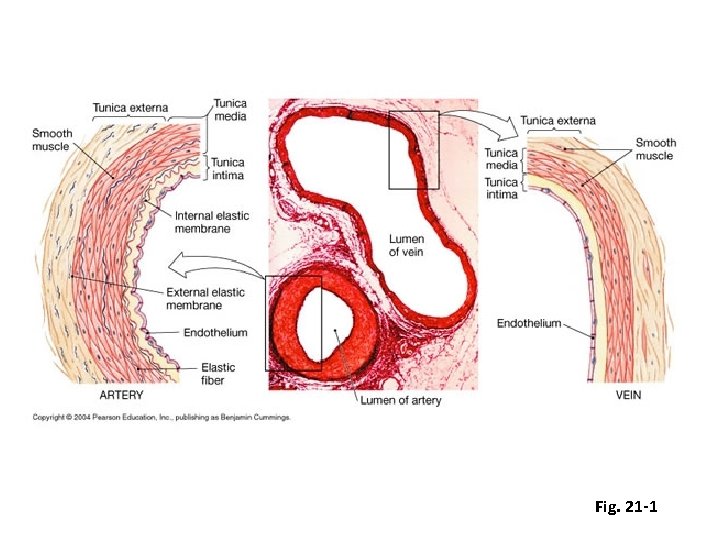
Fig. 21 -1
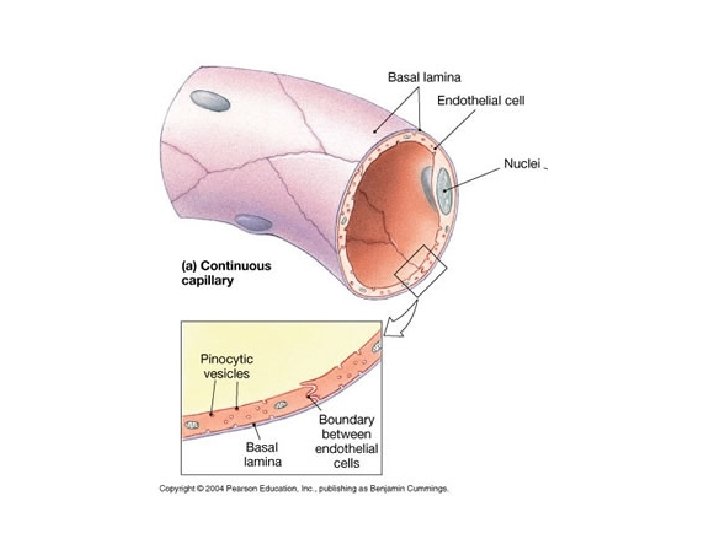
Capillaries • Capillaries –Walls are one cell thick –Gas, nutrient, waste exchange between blood and tissue’s cells
Which of these layers in the wall of blood vessels contains smooth muscle? A) tunica adventitia B) tunica intima C) tunica media D) both b and c
Veins greater than 2 mm in diameter have A) no tunica adventitia. B) thicker walls than arteries. C) valves. D) no endothelial lining. E) No valves
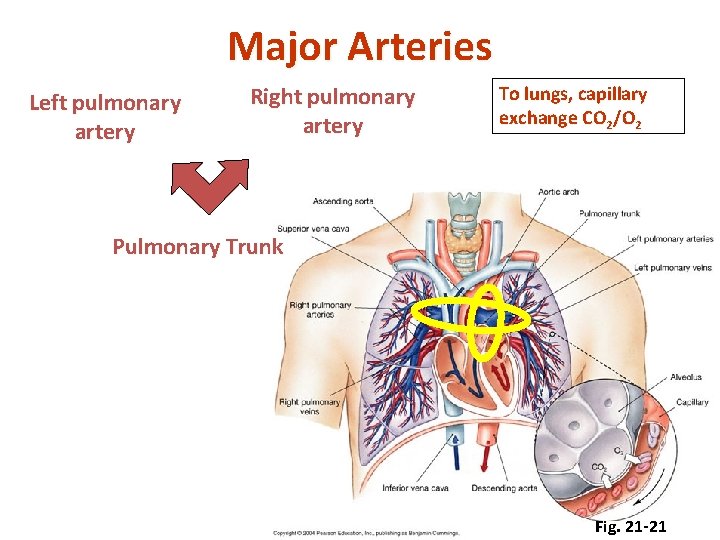
Major Arteries Left pulmonary artery Right pulmonary artery To lungs, capillary exchange CO 2/O 2 Pulmonary Trunk Fig. 21 -21
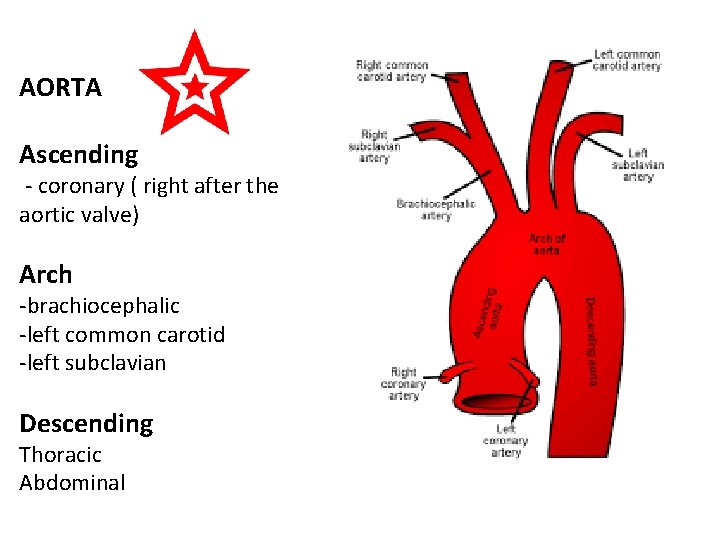
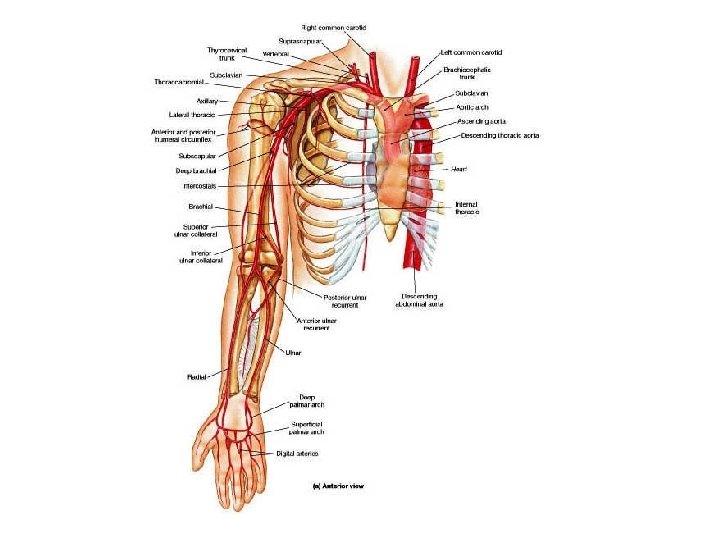
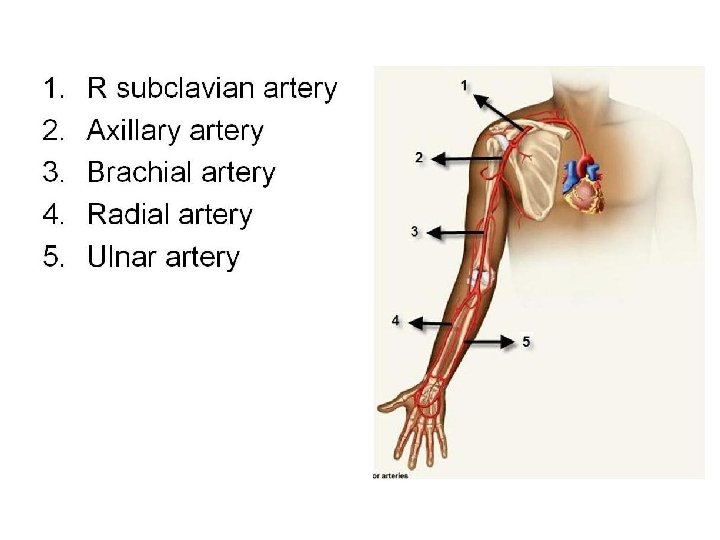
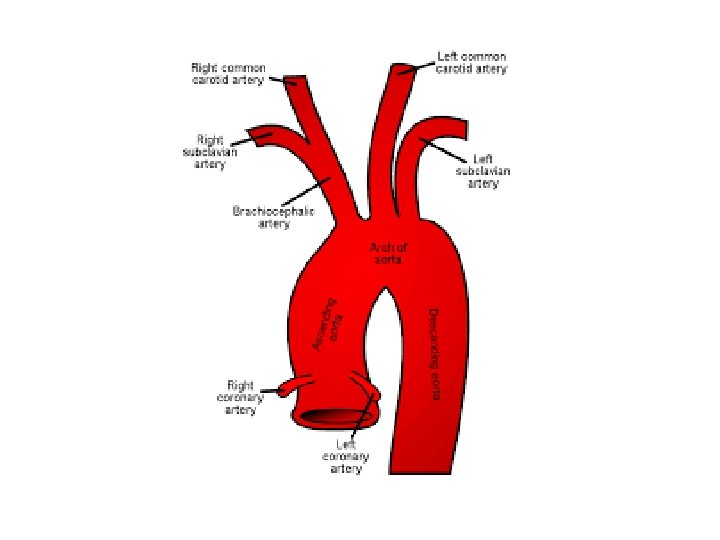
AORTA Ascending - coronary ( right after the aortic valve) Arch -brachiocephalic -left common carotid -left subclavian Descending Thoracic Abdominal
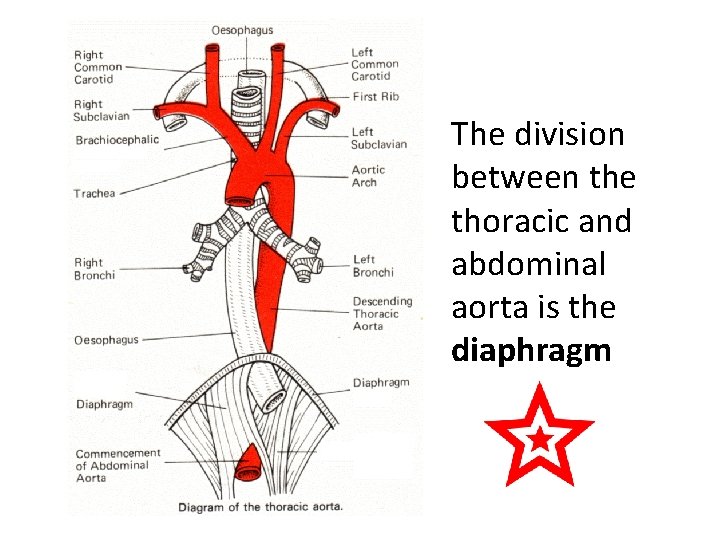
The division between the thoracic and abdominal aorta is the diaphragm
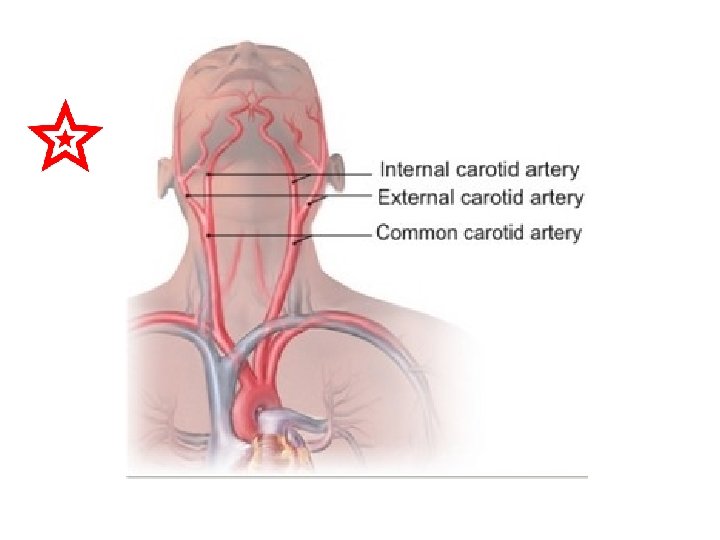
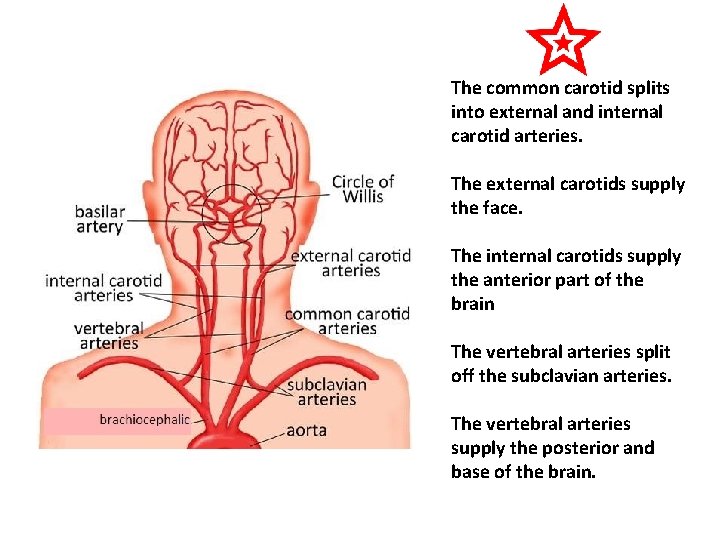
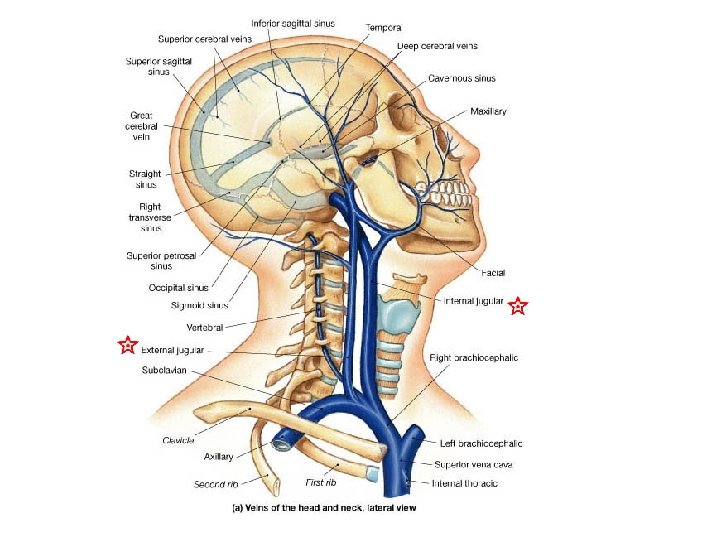
The common carotid splits into external and internal carotid arteries. The external carotids supply the face. The internal carotids supply the anterior part of the brain The vertebral arteries split off the subclavian arteries. The vertebral arteries supply the posterior and base of the brain.
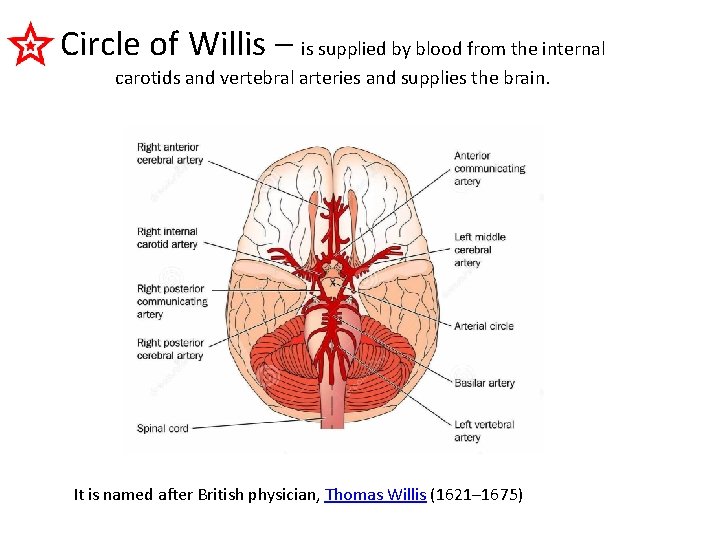
Circle of Willis – is supplied by blood from the internal carotids and vertebral arteries and supplies the brain. It is named after British physician, Thomas Willis (1621– 1675)
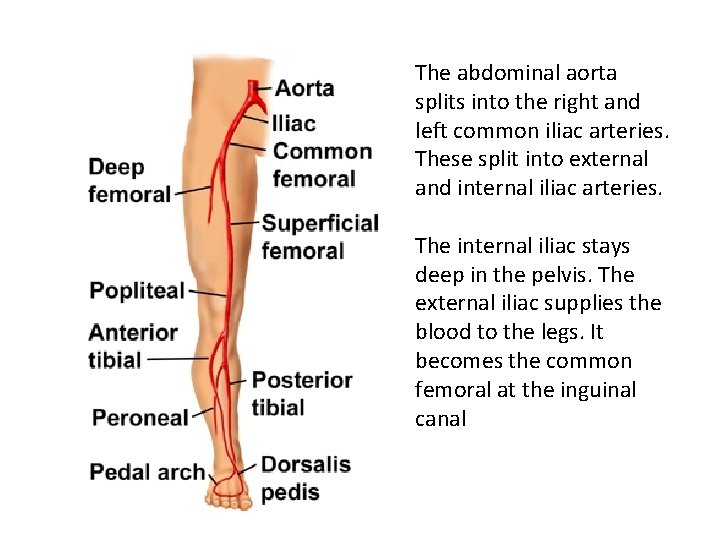
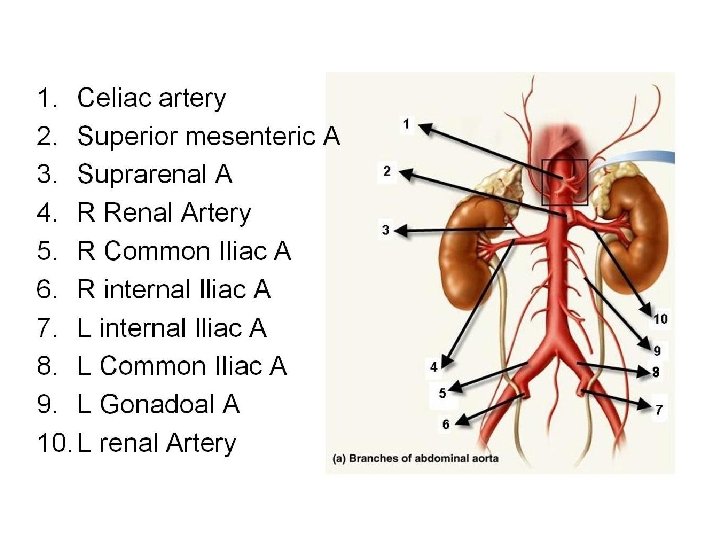
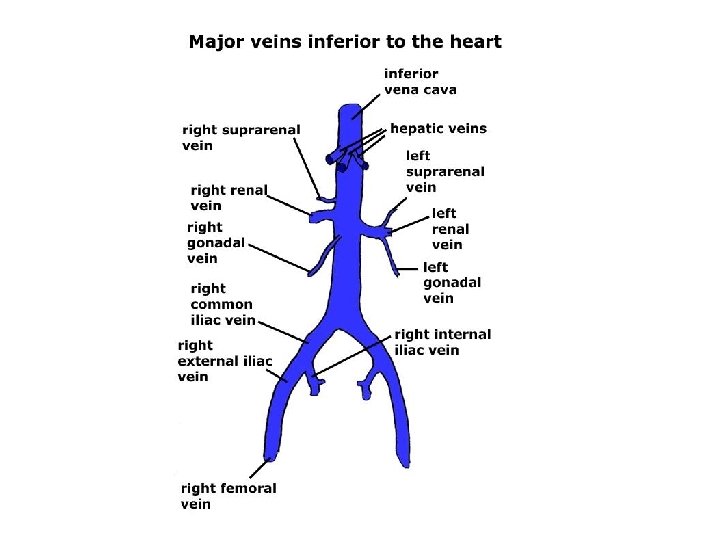
The abdominal aorta splits into the right and left common iliac arteries. These split into external and internal iliac arteries. The internal iliac stays deep in the pelvis. The external iliac supplies the blood to the legs. It becomes the common femoral at the inguinal canal
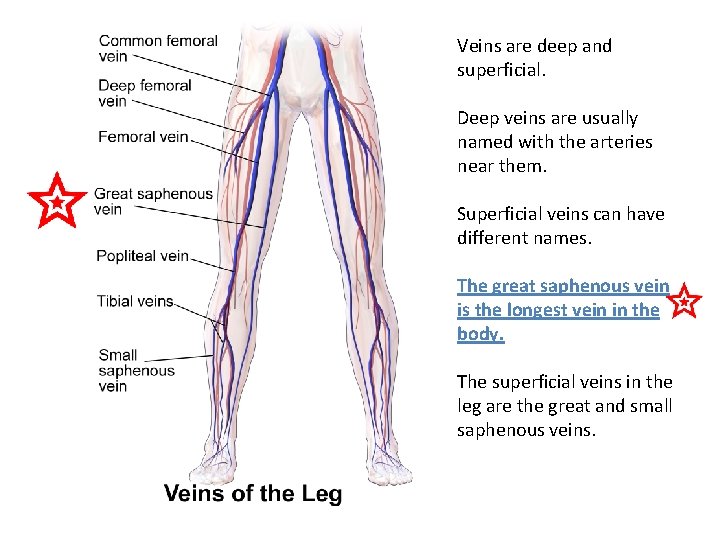
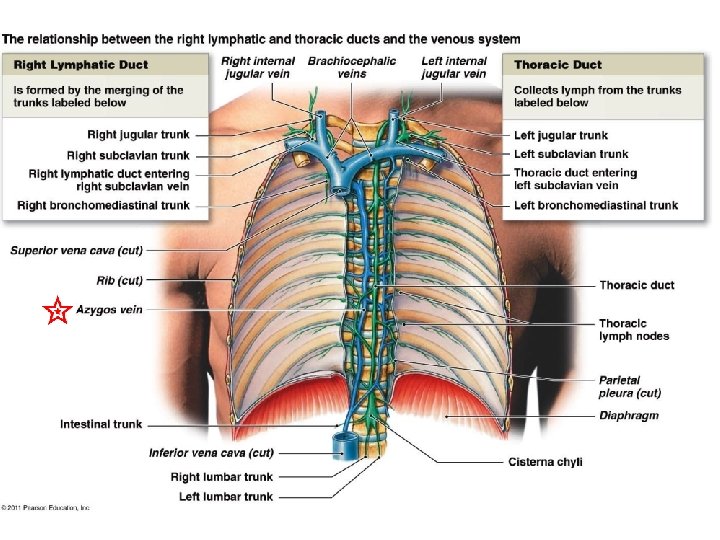
Veins are deep and superficial. Deep veins are usually named with the arteries near them. Superficial veins can have different names. The great saphenous vein is the longest vein in the body. The superficial veins in the leg are the great and small saphenous veins.
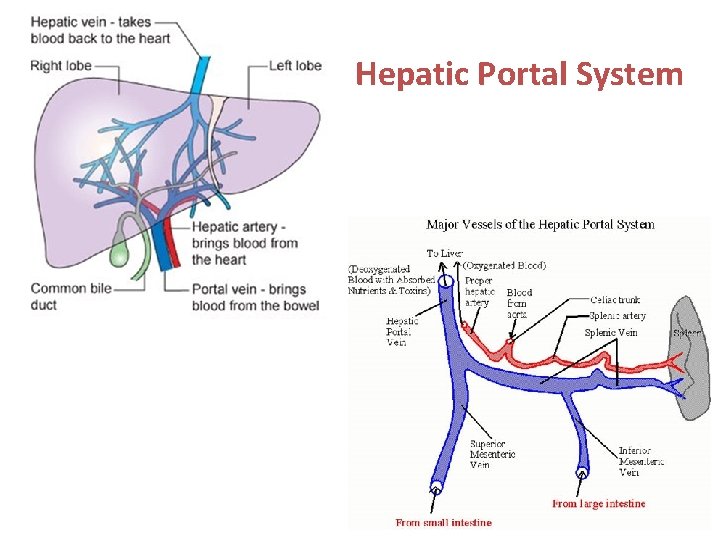
Hepatic Portal System
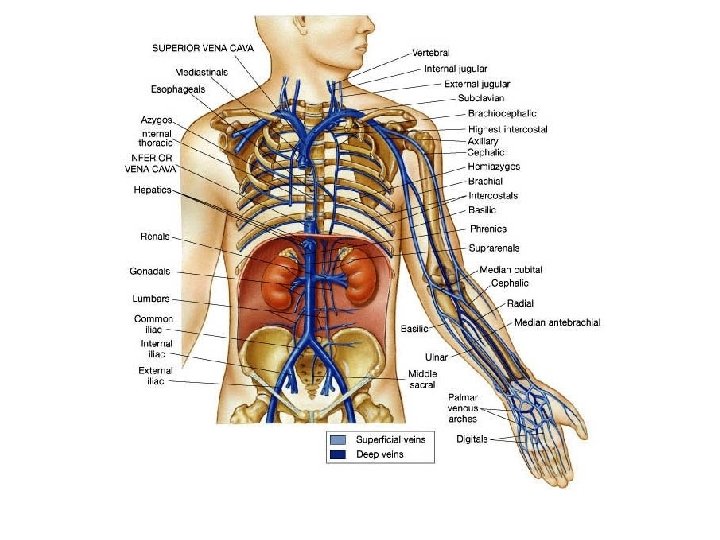
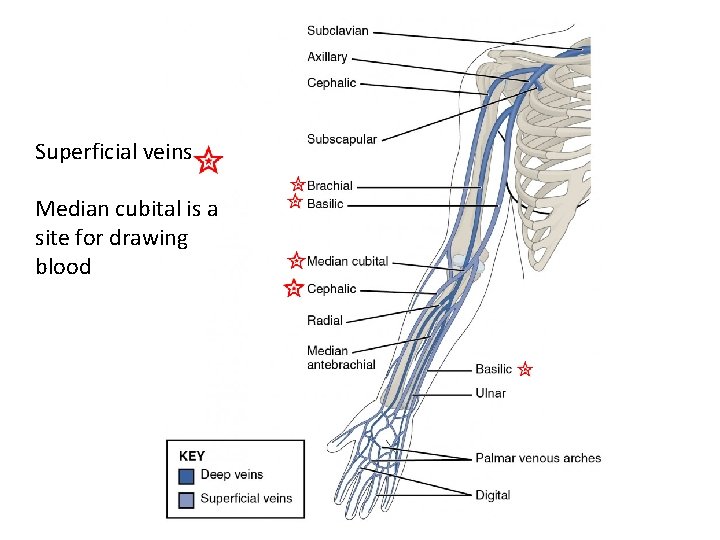
Superficial veins Median cubital is a site for drawing blood
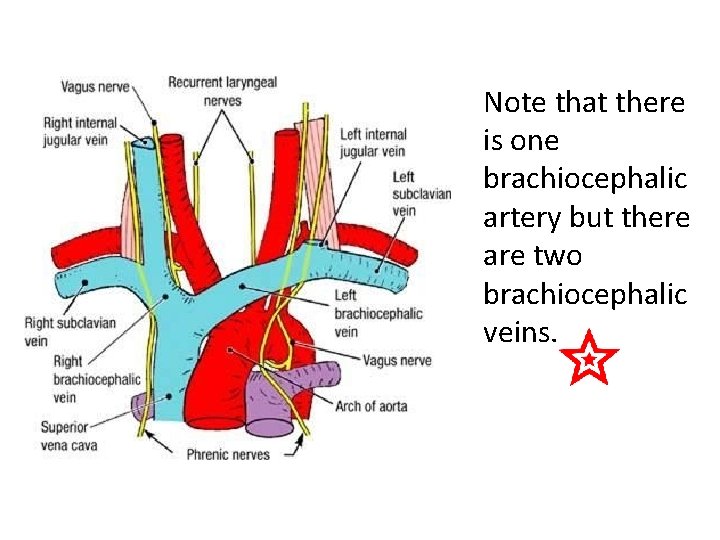
Note that there is one brachiocephalic artery but there are two brachiocephalic veins.
The first artery to branch from the aortic arch is the A. B. C. D. E. Brachiocephalic Left common carotid Right common carotid Left subclavian artery Right subclavian artery The first arteries to branch from the ascending aorta are? The right and left coronary arteries are the only arteries that branch off the ascending aorta.
21. 8 Control of Blood Flow in Tissues • Local control: in most tissues, blood flow is proportional to metabolic needs of tissues • Nervous System: responsible for routing blood flow and maintaining blood pressure • Hormonal Control: sympathetic nervous system stimulates adrenal medulla to secrete epinephrine and norepinephrine. 21 -35
Local Control of Blood Flow • Vasodilation and vasoconstriction of small arterioles and contraction/relaxation of precapillary sphincters. • Autoregulation- can maintain blood flow when BP or metabolic needs change. 21 -36
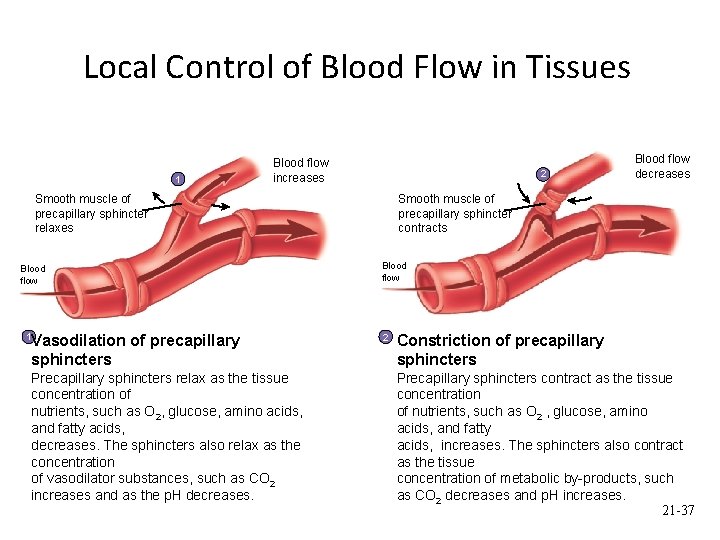
Local Control of Blood Flow in Tissues 1 Blood flow increases 2 Smooth muscle of precapillary sphincter relaxes Blood flow 1 Vasodilation of precapillary sphincters Precapillary sphincters relax as the tissue concentration of nutrients, such as O 2, glucose, amino acids, and fatty acids, decreases. The sphincters also relax as the concentration of vasodilator substances, such as CO 2 increases and as the p. H decreases. Blood flow decreases Smooth muscle of precapillary sphincter contracts Blood flow 2 Constriction of precapillary sphincters Precapillary sphincters contract as the tissue concentration of nutrients, such as O 2 , glucose, amino acids, and fatty acids, increases. The sphincters also contract as the tissue concentration of metabolic by-products, such as CO 2 decreases and p. H increases. 21 -37
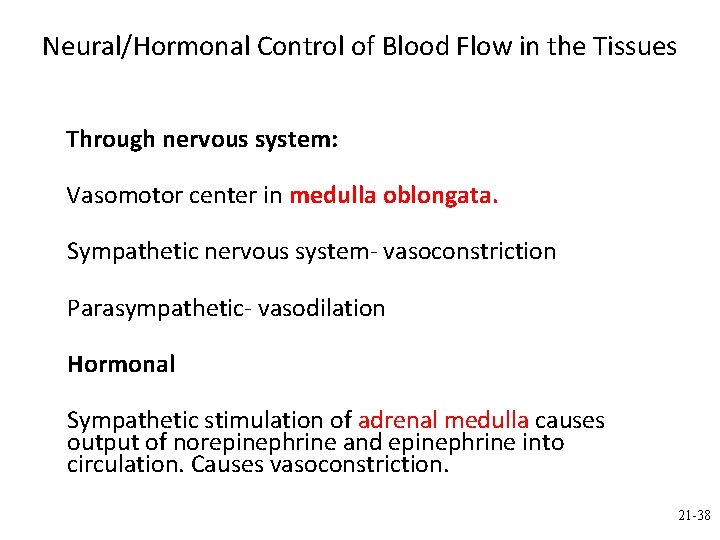
Neural/Hormonal Control of Blood Flow in the Tissues Through nervous system: Vasomotor center in medulla oblongata. Sympathetic nervous system- vasoconstriction Parasympathetic- vasodilation Hormonal Sympathetic stimulation of adrenal medulla causes output of norepinephrine and epinephrine into circulation. Causes vasoconstriction. 21 -38
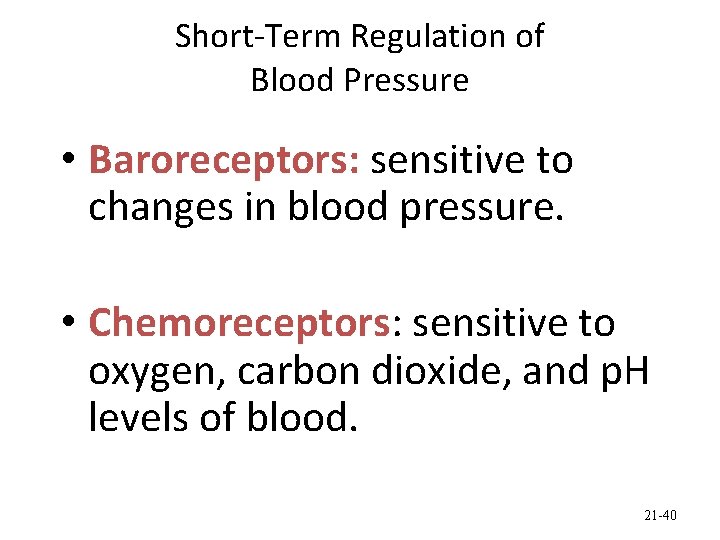
Short-Term Regulation of Blood Pressure • Baroreceptors: sensitive to changes in blood pressure. • Chemoreceptors: sensitive to oxygen, carbon dioxide, and p. H levels of blood. 21 -40
Long-Term Regulation of Blood Pressure • Aldosterone – increases sodium retention by kidneys • Vasopressin (ADH) – increases water retention by kidneys.
Which process is involved in long term management of arterial blood pressure? A. Chemoreceptors that detect C 02, O 2, and p. H changes B. Chemoreceptors that detect changes in blood pressure C. Baroreceptors that detect changes in blood pressure D. Vasoconstriction E. Hormones – ADH and Aldosterone
- Slides: 42