Anatomy and histology of the female genital tract







- Slides: 26
Anatomy and histology of the female genital tract
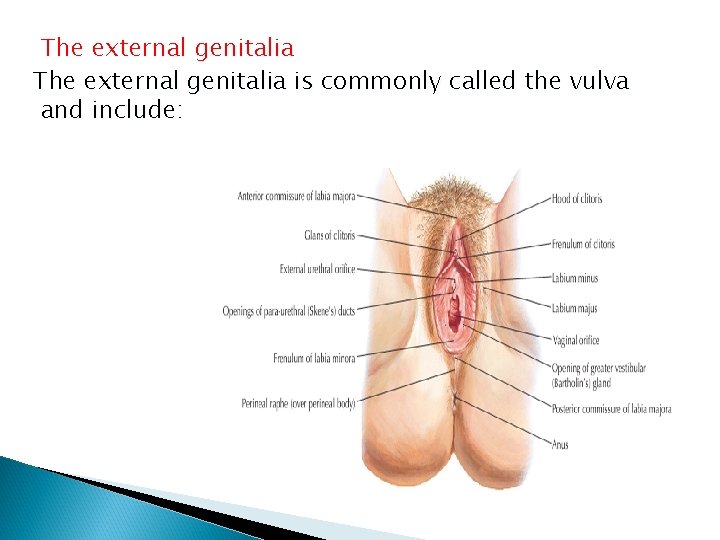
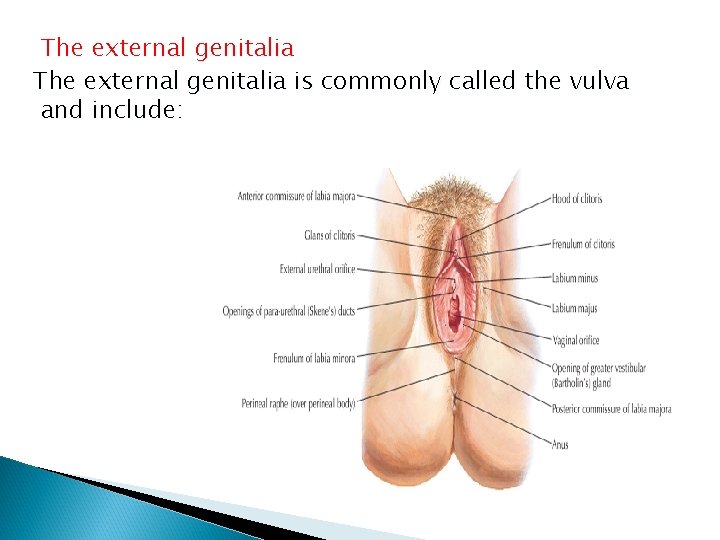
The external genitalia is commonly called the vulva and include:

6 -Bulbs of the vestibule paired of erectile tissue which lie medial aspect of labia minor and enlarge by ongy tissue. 7 -Greater vestibular glands are pairs of glands posterior to the bulb of the vestibule which secretes mucous around sexual arousal. 8 -Fourchete is the meeting point of each labia posterior to the vestibule
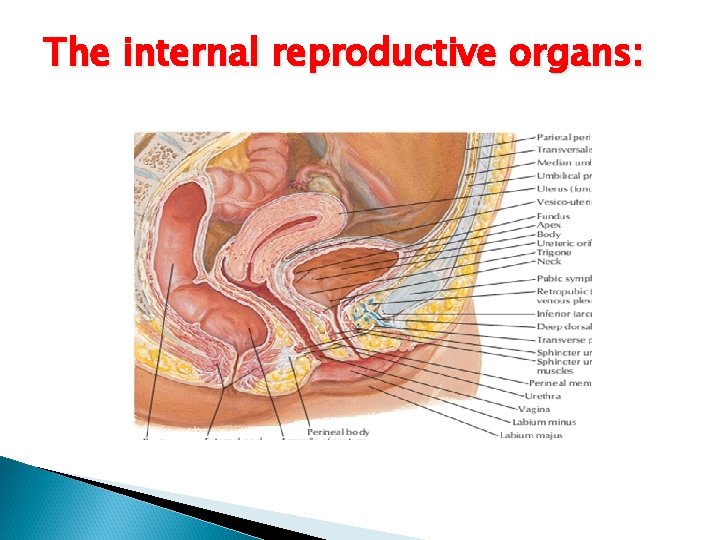
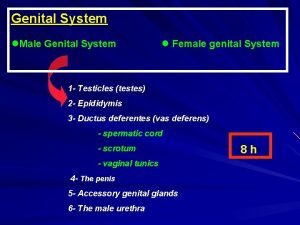
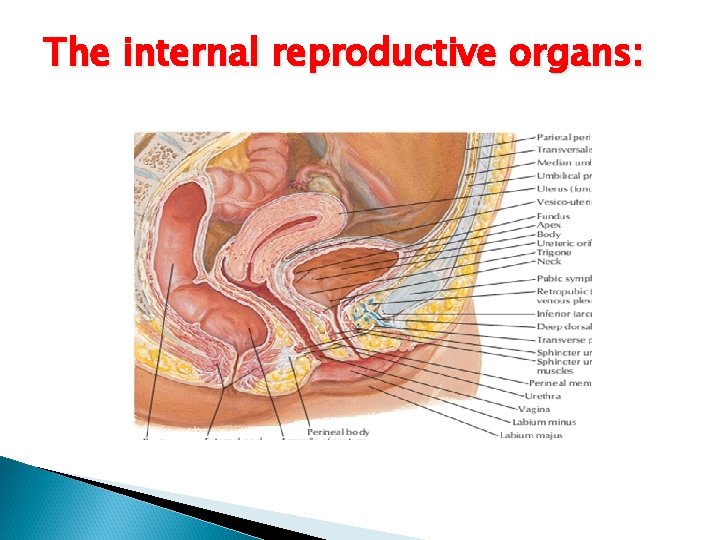
The internal reproductive organs:
The vagina: It is a fibromuscular canal lined with stratified squamous epithelium that lead from the uterus to the vulva. It is longer in the posterior wall(9 cm) than the anterior wall(7 cm). Doderleins bacillus is a normal commensal of the vaginal flora producing a PH of 4. 5.
The uterus: Inverted pear tapering inferiorly to the cx. it is hollow and has thick , muscular walls. Its maximum external dimensions are 7. 5 cm long, 5 cm wide, and 3 cm thick. An adult uterus weight 70 gm. The area of insertion of each fallopian tube is termed cornua and that part of the body above the cornua is called fundus. the uterus tapers to a small constricted area, the isthmus, and below this is the cx.
The uterus consists of three layers: outer serous layer(peritoneum), the middle muscular layer(myometrium) and the inner mucous layer (endometrium). Its lined with single layer of columnar epithelium.
The cervix: The cervix is narrower than the body of the uterus and about 2. 5 cm in length. The upper part mostly consists of involuntary muscle, whereas the lower part is mainly fibrous connective tissue. The epithelium of the endocervix is columnar , this changes to stratified squamous epithelium around the region of the external os and the junction of these two types of epithelium is called the squamocolumnar junction or the transformation zone.
The fallopian tube: The fallopian tube extends outwards from the uterine cornua to end near the ovary. It open to the peritoneal cavity via the osteum. Each tube is about 10 cm long and consists of: 1 -the interstitial portion. 2 -the isthmus. 3 -the ampulla. 4 -the infundibulum or fimbrial part.
The muscular fibers of the wall of the tube arranged in an inner circular and an outer longitudinal layer. The epithelium of the tubes contains two functional cell types: the ciliated and the secretory cells.

The ovary: in young adult they are almond-shaped and measure 3 cm long , 1. 5 cm wide and 1 cm thick. Each ovary attached to the cornua by ovarian ligament and at the hilum to the broad ligament by mesovarium which contain its blood supply. The ovary has central medulla consisting of loose connective tissue containing many elastin fibers and non-striated muscle cells. It has an outer thicker cortex consist of reticular fibers and fusiform cells. The surface of the ovaries is covered by single layer of cuboidal cells, the germinal epithelium. The primordial cells found mostly in the cortex
Muscular structure of the pelvis: The pelvic diaphragm: Is formed by the levator ani muscles which are broad, flat muscle the fiber of which pass downward and inward.

The muscle is described in two parts: The pubococcygeus. The iliococcygeus.
The levator ani is composed of striated voluntary muscle fibers and only special exercises may elicit its action, this muscle is the main base for all the pelvis viscera to rest on it firmly. In addition to that this muscle contributes significantly to the integrity of both sphincter muscles especially the sphincter urethrae. Weakening of this sphincter may follow pregnancy especially after delivery leading to stress incontinence with leak of urine upon any maneuver which
increases intra abdominal pressure like cough straining at defection and other related condition. For this purpose special exercise has been advocated like Kegel pelvic floor exercise which aims to increase the number of muscle fibers supplied to this muscle. On the other hand especially among women with grand multi parity damage to this muscle may lead to herniation of the bladder into the anterior vaginal wall a condition called cystocele. Otherwise may lead to herniation of the rectum to posterior vaginal wall which lead to rectocele. Both of the last conditions are treated usually by special surgery for correction of those conditions.

Urogenital diaphragm: Triangular ligament is made up of two layers of pelvic fascia which fill the gap between the descending pubic rami and lies beneath the levator ani. the deep transverse perineal muscles lies between the two layers and the diaphragm is pierced by the urethra and vagina.
Menstruation is defined as monthly shedding of endometrial dead tissue which herald failure to achieve pregnancy. Menstrual blood is a mixture of dead endometrial tissue, blood components and pus cells. The normal limits of human cycle are 3 -7 days in duration, with frequency 21 - 35 days with average 28 days. The total blood loss should not exceed 7080 ml and usually above 30 - 40 ml.

Phases of human menstrual cycle: The follicular phase: which involves maturating single primordial follicle in fully matured 18 - 22 mm diameter. The changes are all brought about by FSH from the pituitary. In addition to maturing ovarian follicle the uterus lining is re grown by the estrogen which is secreted from the follicle itself. Normally the correlation between estrogen and FSH is negative feedback mechanism. However for very short period this correlation becomes positive leading to ovulation with start of the second phase of the ovary.
The luteal phase: is brought about after the rupture mature follicle as induced by brief increase in the frequency and amplitude of the Gn. RH at the hypothalamus and release of FSH, LH converting the follicle into corpus luteum. Which start to secrete estrogen and progesterone. It is quite important to understand the luteal phase age is only 14 days. During this period the endometrial lining is converted into the secretory which is the only one compatible with implantation of 8 - 16 cell stage embryo
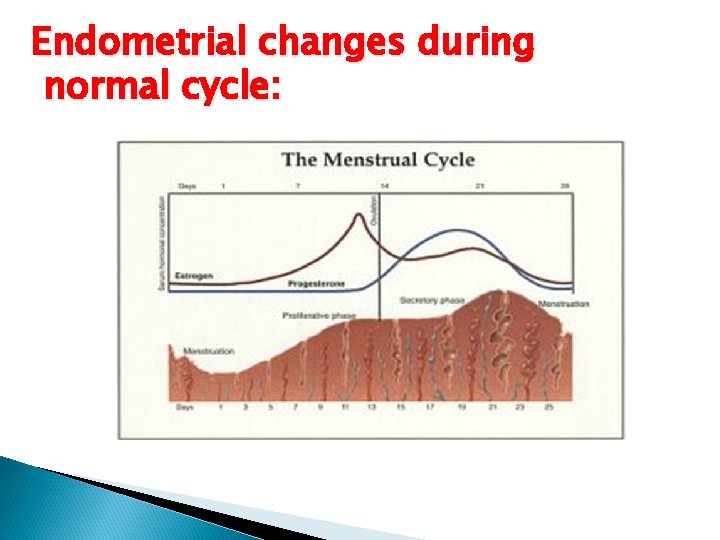
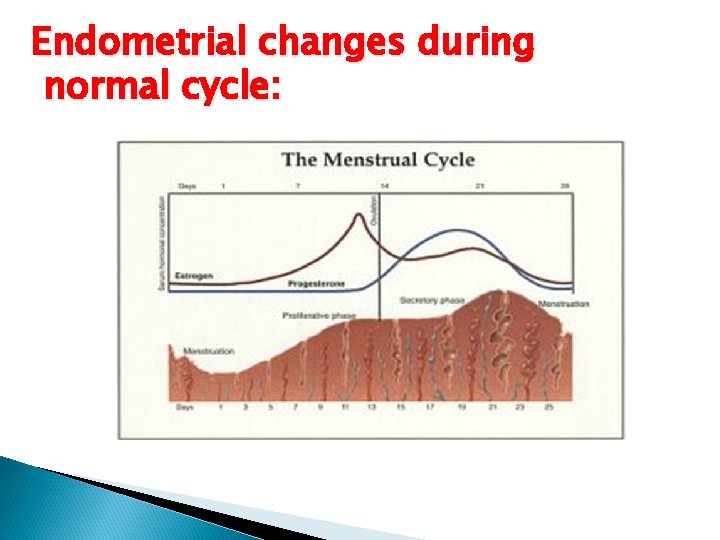
Endometrial changes during normal cycle:
The follicular or proliferative phase: occurs when the ovary is developing the primordial ovarian follicles into 1 single mature follicle. In this phase the endometrium is under estrogen only. The epithelial lining the endometrial glands changes from single layer of columnar cells to pseudostratified epithelium with frequent mitosis. From the surface epithelium few ducts start to appear and go deeper. The stroma infitrates by fibroblast cell. The spiral vessels are initially few and less coiled yet gradually increase in number as well as in coiling with advent of follicular phase.

Luteal phase or secretory phase: Here the endometrial glands will become more tortuous, spiral arteries will grow and fluid is secreted into glandular cells and into the uterine lumen. later in the secretory phase the progesterone induces the formation of a temporary layer, known as the decidua in the endometrial stroma with represent the sit for embryo implantation.

 Womens anatomy
Womens anatomy Defence mechanism of female genital tract
Defence mechanism of female genital tract Labium
Labium Rete testis
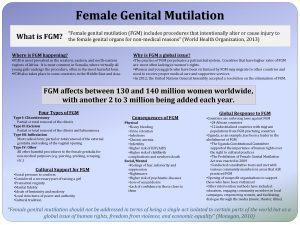
Rete testis Female genital mutilation
Female genital mutilation What does fgm
What does fgm Internal genital organs female
Internal genital organs female Pyramidal tract vs extrapyramidal tract
Pyramidal tract vs extrapyramidal tract Rubrospinal tract
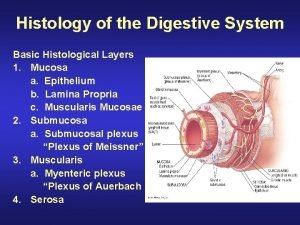
Rubrospinal tract Histology of digestive tract
Histology of digestive tract Gi tract histology
Gi tract histology Gi tract histology
Gi tract histology Digestive system histology
Digestive system histology Seminal vesicle function
Seminal vesicle function Layers of fallopian tube
Layers of fallopian tube Anatomy and histology of liver
Anatomy and histology of liver Upper respiratory diagram
Upper respiratory diagram Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Anatomy of the urinary tract
Anatomy of the urinary tract Respiratory system nasal cavity
Respiratory system nasal cavity Http://www.biologycorner.com/anatomy/histology/
Http://www.biologycorner.com/anatomy/histology/ Anatomy histology slides
Anatomy histology slides Sheep brain
Sheep brain Pancreas histology slide
Pancreas histology slide Woman anatomy
Woman anatomy Hernia types pictures
Hernia types pictures Anatomy of a pig
Anatomy of a pig