ANAPHYLAXIS AND URTICARIA GROUP 1 SOMADINA STANLEY OGHOGHORIE




- Slides: 33
ANAPHYLAXIS AND URTICARIA GROUP 1 SOMADINA STANLEY OGHOGHORIE MIRACLE OGBONA ANITA TSADO SWETLANA KAPOOR
ANAPHYLAXIS
DEFINITION – An acute potentially fatal multiorgan system reaction, caused by the release of chemical mediators from mast cells and basophils.
RISK FACTORS/ETIOLOGY – Atopy – Pollen extracts – Non pollen extracts like dust mites, dander of cats, dogs – Food like peanuts, milk, eggs, seafood – Monoclonal antibodies – Drugs like antibiotics, sulfa drugs, which function as haptens and form immunogenic conjugates with host proteins.
Clinical features of anaphylaxis – How anaphylaxis presents in a hospital setting. Onset is usually within 5 -10 mins from injection of the antigen. Remember that it can start minor and RAPIDLY progress. – Anaphylaxis is an acute multi-organ systemic reaction and the most common organ systems affected include: – Cutaneous: Flushing, Urticaria, Angioedema, Cutaneous/ Conjuctival pruritus, warmth and swelling
– Respiratory: Congestion, dyspnea, rhinorhea, throat tightness, wheezing, SOB, Cough and hoarseness – Cardiovascular: Dizziness, weakness, syncope, chest pain, Palpitations – G. I: Dysphagia, nausea, vomiting, cramps and bloating – Neurologic: Headache, dizziness, blurred vision, and seizures (rare and due to hypotension) – Others: Feeling of impending doom, Metallic taste.

Angioedema as a feature of exercise induced anaphylaxis.
Pathophysiology of anaphylaxis – The pathophysiology of anaphylaxis can be grouped into two, it is caused by the release of inflammatory mediators from mast cells and basophils typically due to: – Immune mediated means, but can also be caused by: – Non immunologic mechanisms.
Immune mediated (classic ige binding story) – The key thing here is IGE. The offending antigen gets bound by IGE and the complex activates the receptors on mast cells and basophils, which leads to degranulation (the release of histamine and other mediators from mast cells). The mediators assert their effects on the various organ systems involved (contraction of smooth muscle, vasodilation and heart muscvle depression).
Non-Immune mediated – This pathophysiologic mechanism involves direct degranulation of mast cells and basophils by a substance (Not IGE, hence non-immune. ). The substance can be contrast medium, opioids or even temperature and vibration.
Diagnosis of anaphylaxis – The presence of any of these 3 after mins or hours of exposure to allergen. – Involvement of skin or mucosa – Respiratory difficulty – Low blood pressure – Gastrointestinal symptoms
Diagnosis of anaphylaxis – Tryptase testing – Histamine testing NONE SPECIFIC TESTS
Diagnosis of anaphylaxis – Skin testing – Blood Ig. E testing. Post Mortem findings Empty heart. lung and heart eosinophilia.
Management – Airway – Breathing – Circulation – Epinephrine or IV glucagon – Antihistamines – Steroids – Salbutamol – Medical alert bracelets – Immunotherapy
Prevention – Avoid triggers – Desensitization – Avoid cross reacting products
URTICARIA
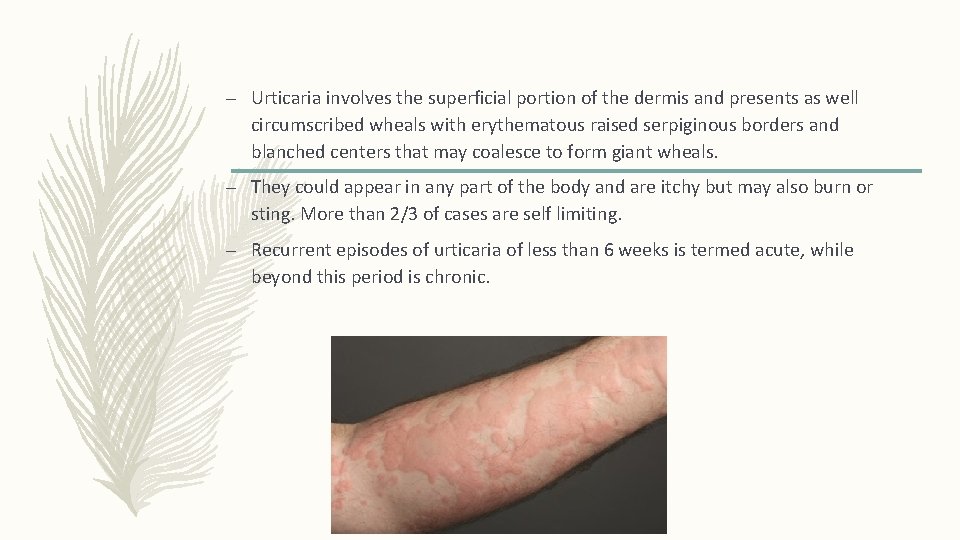
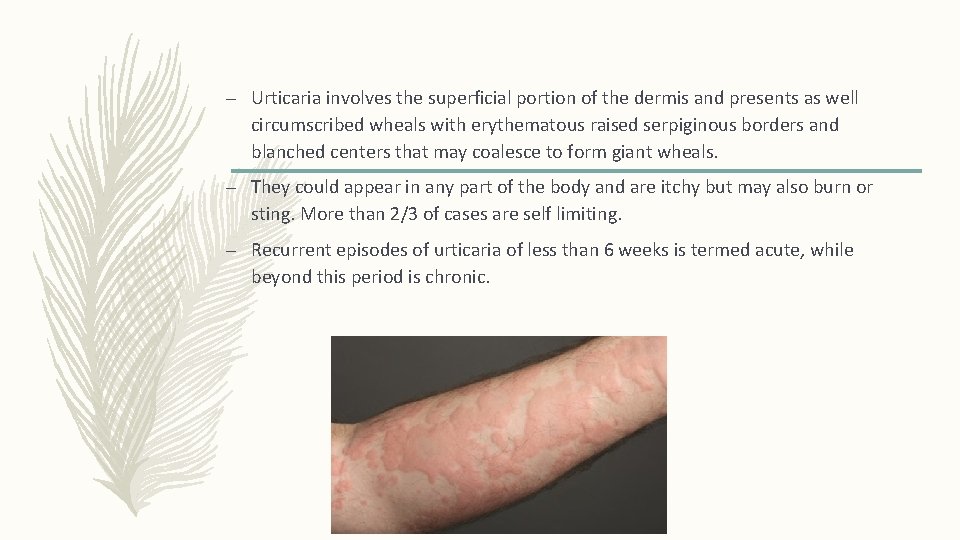
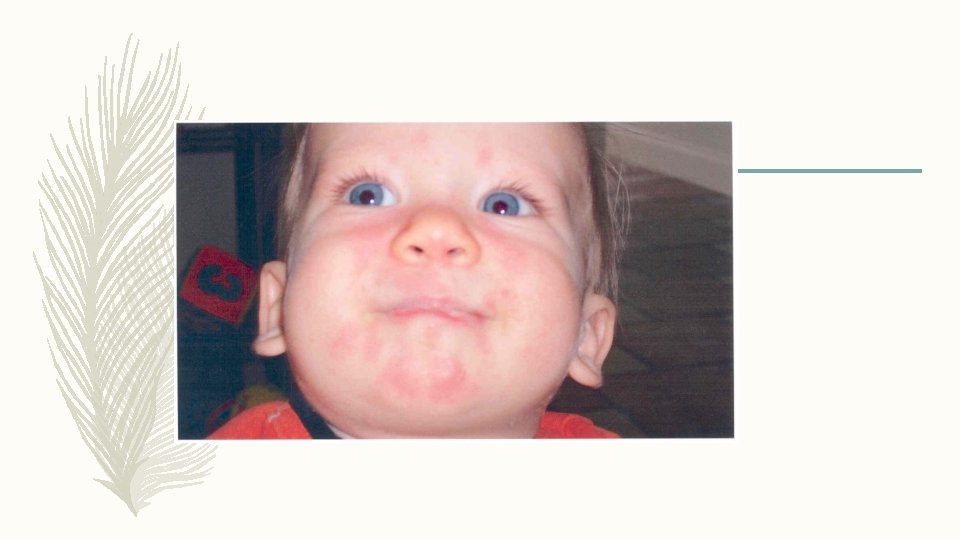
– Urticaria involves the superficial portion of the dermis and presents as well circumscribed wheals with erythematous raised serpiginous borders and blanched centers that may coalesce to form giant wheals. – They could appear in any part of the body and are itchy but may also burn or sting. More than 2/3 of cases are self limiting. – Recurrent episodes of urticaria of less than 6 weeks is termed acute, while beyond this period is chronic.
PREDISPOSING FACTORS AND ETIOLOGY – Urticaria can occur in any age group but there is increased frequency after adolescence. – It could occur during appropriate seasons in people with seasonal allergy. – Exposure to animals or molds, which involves inhalation or physical contact with pollens, animal dander and mold spores. – Ingestion of allergens, like fruits, seafood, milk products, chocolate, legumes and various drugs. – Physical stimuli like cold, heat, solar rays, exercise and mechanical irritation.
CLASSIFICATION – Ig. E- dependent i. Specific antigen sensitivity (pollens, foods, drugs, fungi, molds, helminths) ii. Physical: dermographism, cold, solar, pressure, cholinergic iii. Autoimmune – Complement- mediated i. Necrotizing vasculitis
i. Serum sickness ii. Reactions to blood products – Nonimmunologic i. Direct mast cell releasing agents (opiates, antibiotics, radiocontrast media) ii. Agents that alter arachidonic acid metabolism (aspirin and NSAIDs) – Idiopathic

Cholinergic urticaria Cold urticaria dermographism Chronic urticaria
Pathophysiology – Reaction mediated by activated mast cells and basophils in superficial dermis 2 – When activated, mast cells release histamine causing itching and vasodilators which cause swelling – Same process occurs in angioedema but in deeper layers of the skin and subcutaneous tissues
Characteristics – – – – Pruritic (most severely at night) Erythematous Often exhibit central pallor Blanches Oval, round or irregular shape or plaques Plaques “move” to different locations over minutes to hours Last less than 24 hours Leave no residual marks (other than those created by scratching)
Presentation – Pruritus and rash are the primary manifestation, permanent hyperpigmentation or hypopigmentation is rare. – Lesions typically appear over the course of minutes, enlarge, and then disappear within hours – Individual wheals rarely last more than 12 hrs – Surrounding erythema will blanch with pressure – An entire episode of urticaria often lasts 24 -48 hrs. – Rarely, acute urticaria can last 3 -6 wks.
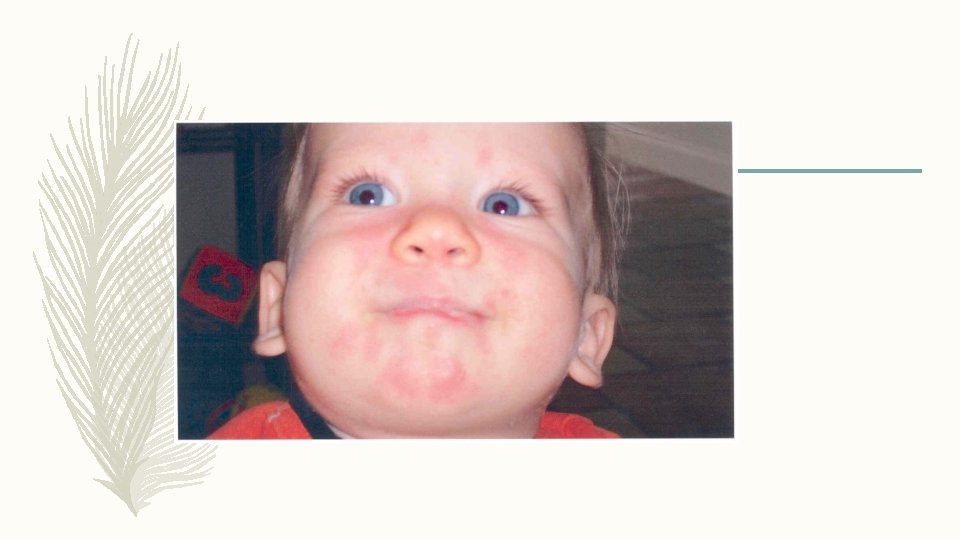


Diagnosis – Detailed history – including has pt ever had urticaria before – were there any unusual exposures immediately prior to the episode – Does the patient have pictures? – Physical Exam – If the patient does not have lesions at time of exam, consider showing them photos of urticaria as an example – Skin test to determine the allergent
Diagnosis (cont) – Laboratory testing – Acute Urticaria- less than 6 wks – Allergy testing if specific trigger can be implicated (would possibly include skin prick testing or immunocap testing for Ig. E to specific food or drug) – Laboratory testing – Chronic Urticaria*- more than 6 wks – CBC – TSH – ESR – ANA Other results may be considered and include Routine blood tests to determine presence of systemic illness Punch biopsy- if urticaria vasculitis is suspected
Treatment of Urticaria – Search for triggers –tx the treatable causes – H 1 antihistamines First generation: diphenhydramine, chlorpheniramine, hydroxyzine Second generation: cetirizine, loratadine, fexofenadine
Treatment of Urticaria (cont) – First generation antihistamines: – more sedating, require more frequent dosing – Second generation antihistamines: – higher dosing than standard dosing to obtain positive effects – Can be sedating at higher dosages – Pregnant women or those breastfeeding may use loratidine or cetirizine
Treatment of Urticaria (cont) – Epinephrine- severe hives/angioedema outbreak – Consider referral to an allergy/immunology specialist for episodes with clear trigger or those which don’t respond to your treatment
– If that is not enough, the guideline recommends adjunctive therapy with omalizumab, Cyclosporin A or a leukotriene antagonist. Omalizumab is approved for the treatment of urticaria in Europe for above 12 years olds. There are numerous clinical studies that show that omalizumab is effective and safe. If symptoms are not controlled, cortisone can be used as a tablet or injection. Cortisone is not suitable as a long-term treatment of urticaria and should only be used as a short-term therapy, start 1 mg/kg/day.