Anaphylaxis Anaphylaxis Anaphylaxis comes from the Greek and

- Slides: 42
Anaphylaxis
Anaphylaxis • Anaphylaxis comes from the Greek and means against or without protection. As opposed to prophylaxis for protection
Definition of Anaphylaxis • Systemic allergic reaction – Affects body as a whole – Multiple organ systems may be involved • Onset generally acute • Manifestations vary from mild to fatal
Histamine • • • Coronary vasoconstriction Bronchoconstriction Vascular permeability Intestinal smooth muscle contraction Dysrhythmias
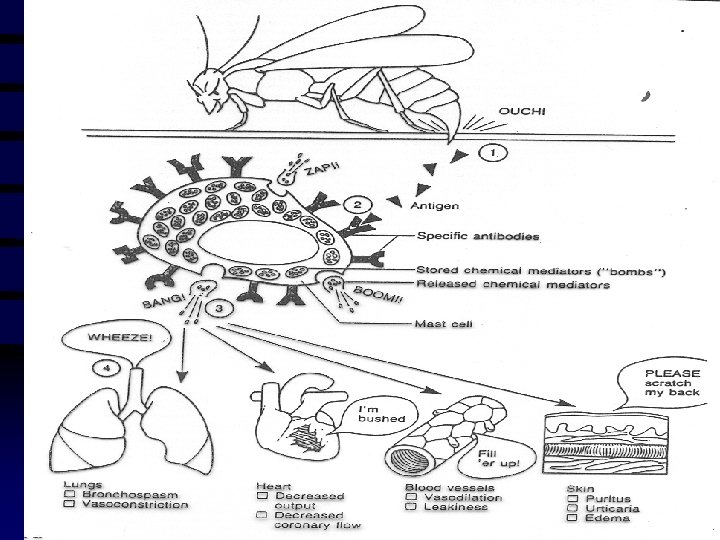
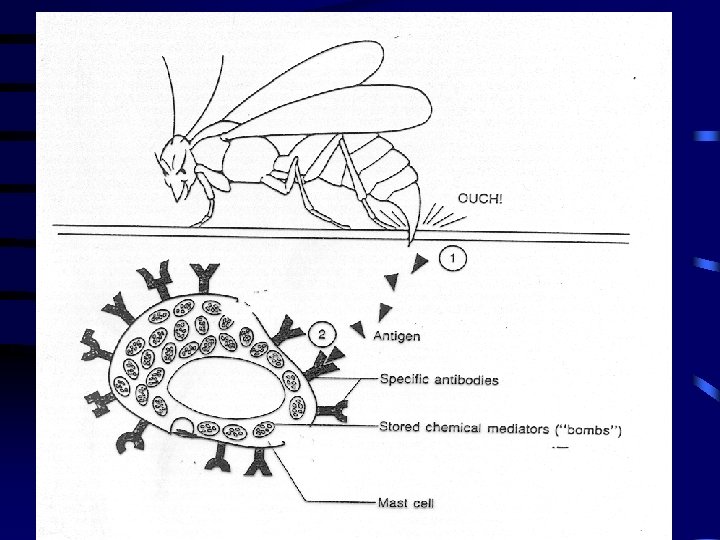
Pathogenesis of Anaphylaxis • Ig. E-mediated (Type I hypersensitivity) • Sensitization stage • Subsequent anaphylactic response
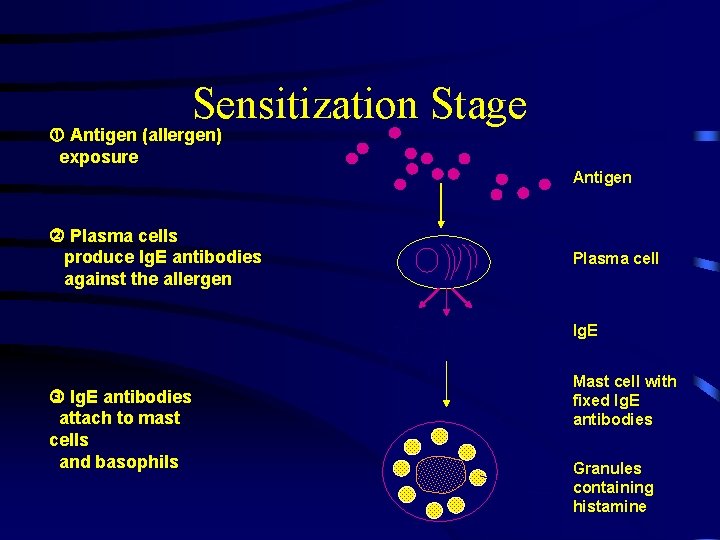
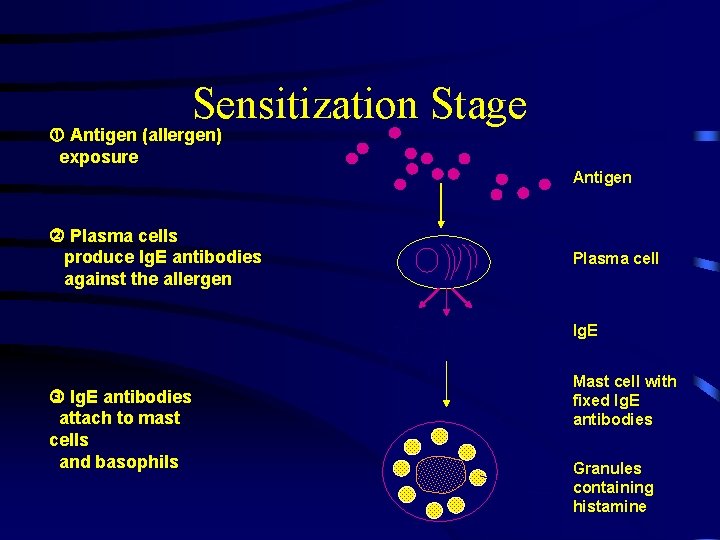
Sensitization Stage Antigen (allergen) exposure Antigen Plasma cells produce Ig. E antibodies against the allergen Plasma cell Ig. E antibodies attach to mast cells and basophils Mast cell with fixed Ig. E antibodies Granules containing histamine
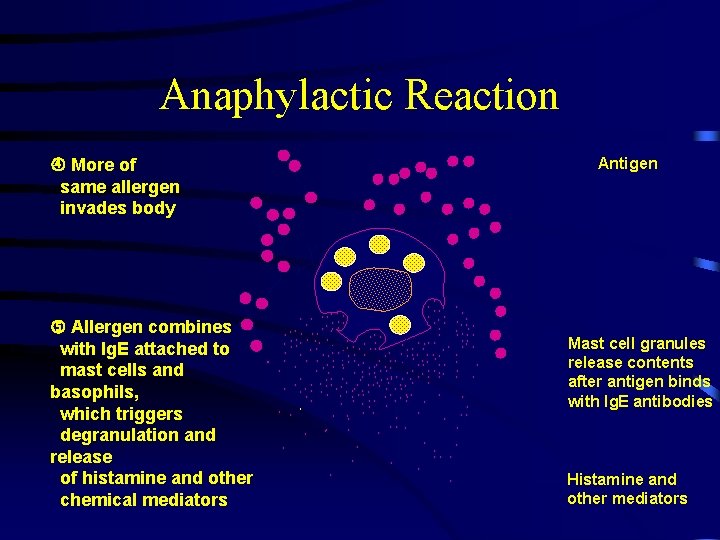
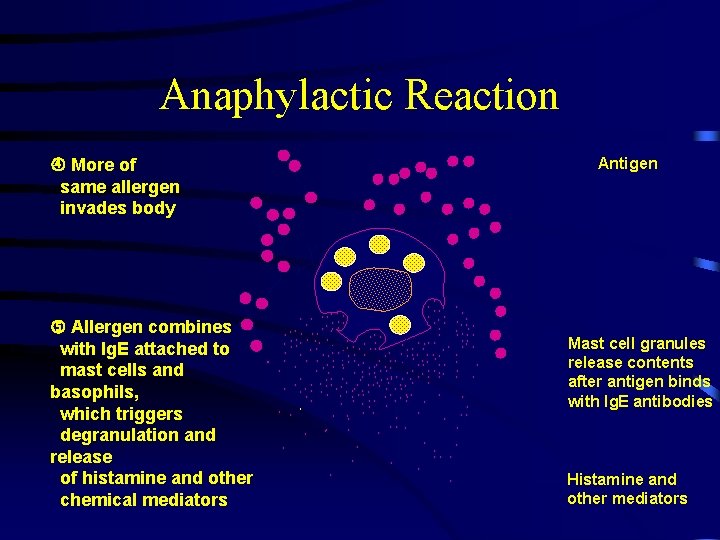
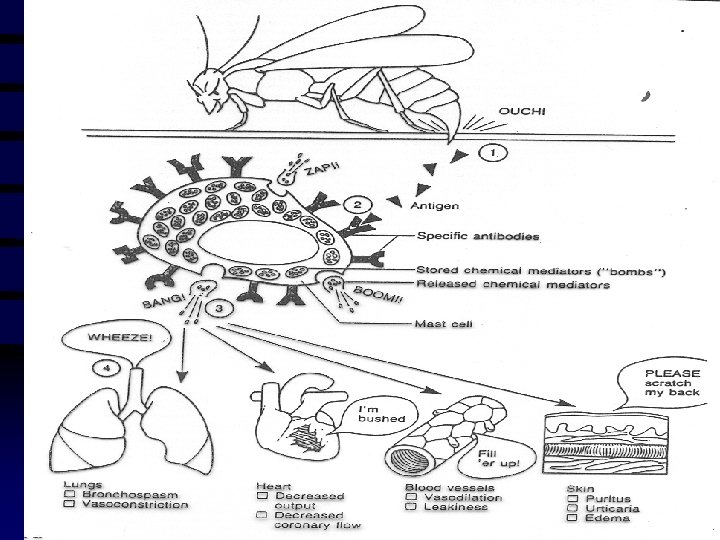
Anaphylactic Reaction Antigen More of same allergen invades body Allergen combines with Ig. E attached to. mast cells and basophils, which triggers degranulation and release of histamine and other chemical mediators • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Mast cell granules release contents after antigen binds with Ig. E antibodies • • Histamine and other mediators
Common Causes of Ig. E-mediated Anaphylaxis • • • Foods Insect venoms Latex Medications Immunotherapy – Insect venom
• Non–Ig. E-anaphylaxis (anaphylactoid reactions) – Complement-mediated • Anaphylatoxins, • Direct stimulation • eg, radiocontrast media – Mechanism unknown • Exercise • NSAIDs
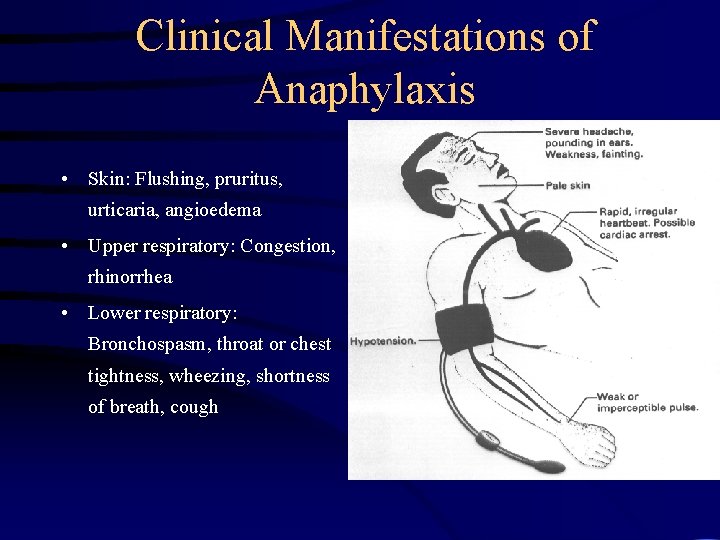
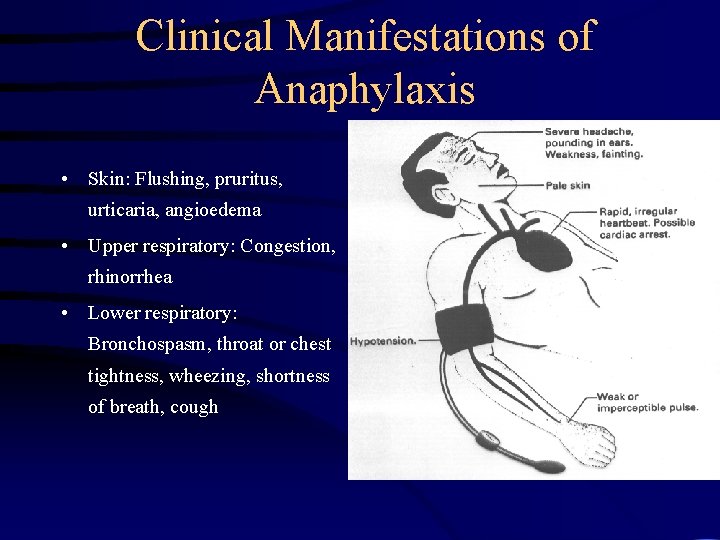
Clinical Manifestations of Anaphylaxis • Skin: Flushing, pruritus, urticaria, angioedema • Upper respiratory: Congestion, rhinorrhea • Lower respiratory: Bronchospasm, throat or chest tightness, wheezing, shortness of breath, cough
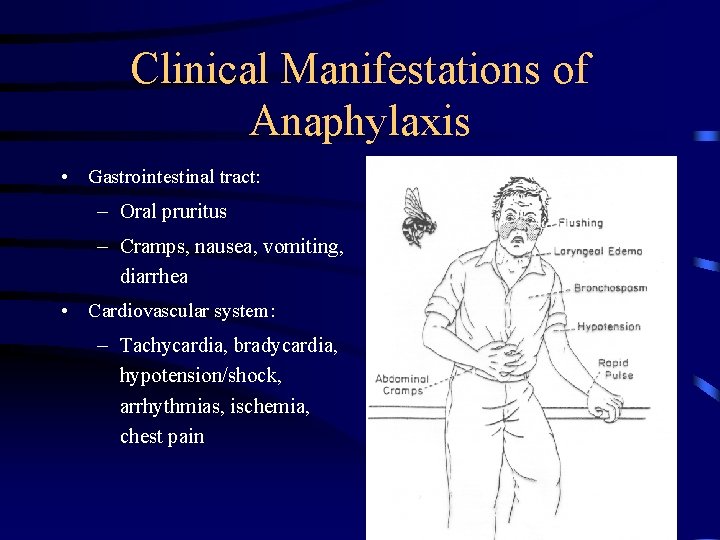
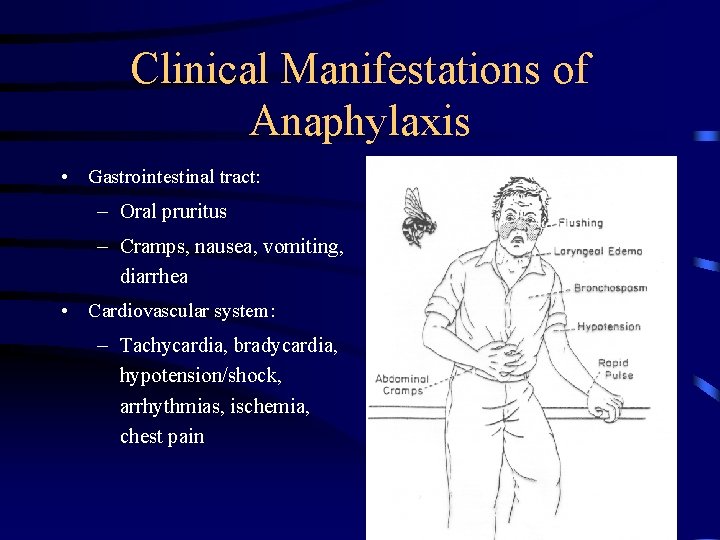
Clinical Manifestations of Anaphylaxis • Gastrointestinal tract: – Oral pruritus – Cramps, nausea, vomiting, diarrhea • Cardiovascular system: – Tachycardia, bradycardia, hypotension/shock, arrhythmias, ischemia, chest pain
Clinical Manifestations of Anaphylaxis • • Urticaria Angioedema Upper airway edema Dyspnea and wheezing • Flush • Dizziness, syncope, and hypotension • Gastrointestinal symptoms • Rhinitis • Headache • Substernal pain • Itch without rash – Pruritus
Clinical Course of Anaphylaxis • Uniphasic • Biphasic – Recurrence up to 8 hours later
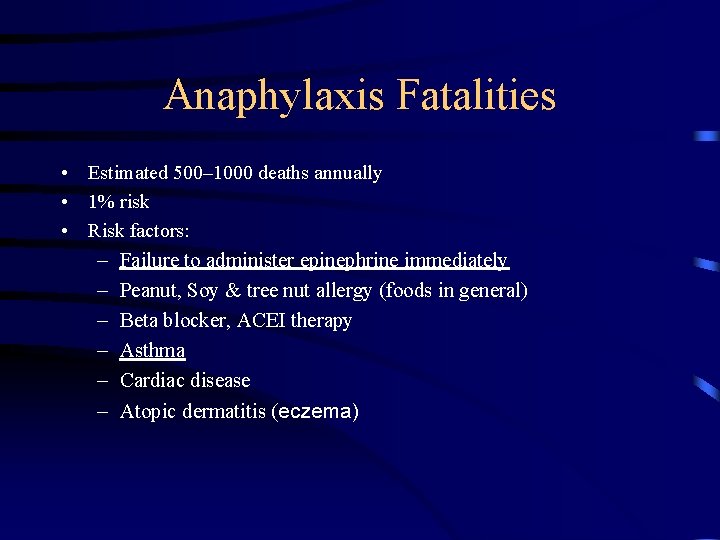
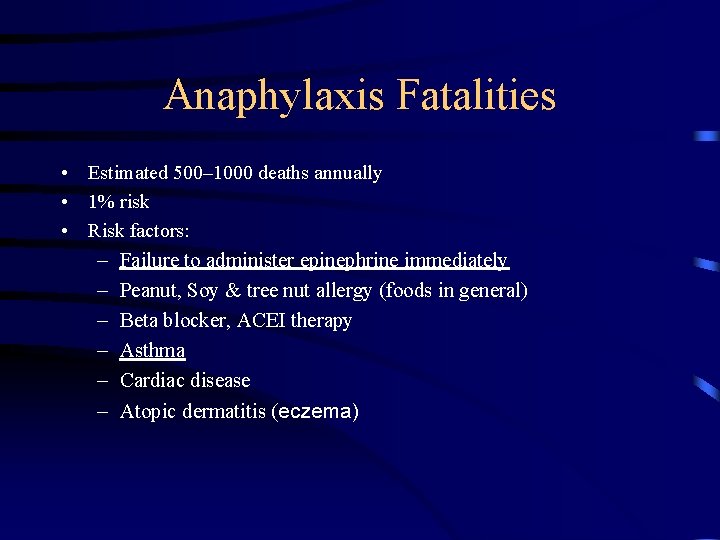
Anaphylaxis Fatalities • Estimated 500– 1000 deaths annually • 1% risk • Risk factors: – Failure to administer epinephrine immediately – Peanut, Soy & tree nut allergy (foods in general) – Beta blocker, ACEI therapy – Asthma – Cardiac disease – Atopic dermatitis (eczema)
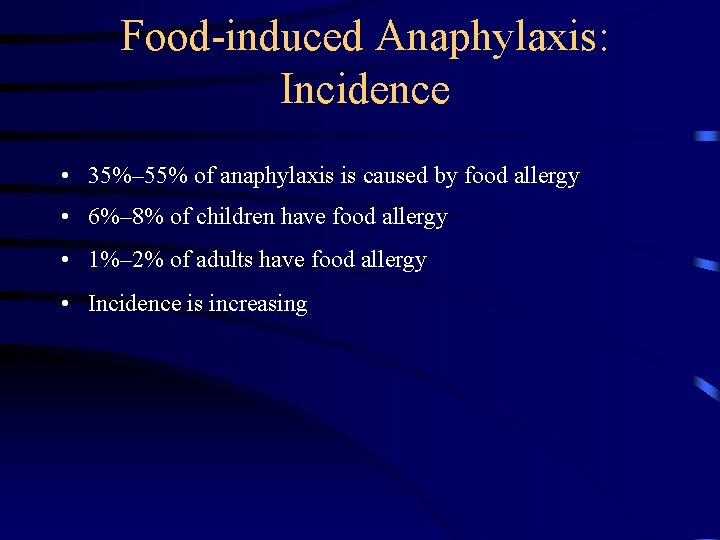
Food-induced Anaphylaxis: Incidence • 35%– 55% of anaphylaxis is caused by food allergy • 6%– 8% of children have food allergy • 1%– 2% of adults have food allergy • Incidence is increasing
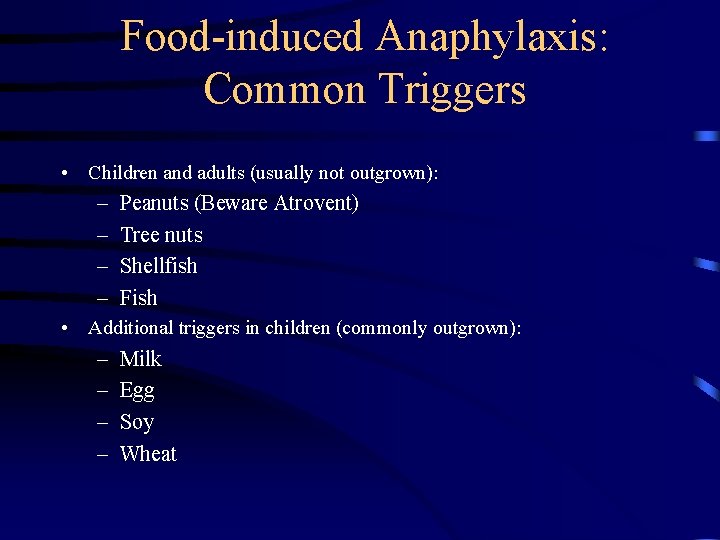
Food-induced Anaphylaxis: Common Triggers • Children and adults (usually not outgrown): – – Peanuts (Beware Atrovent) Tree nuts Shellfish Fish • Additional triggers in children (commonly outgrown): – – Milk Egg Soy Wheat
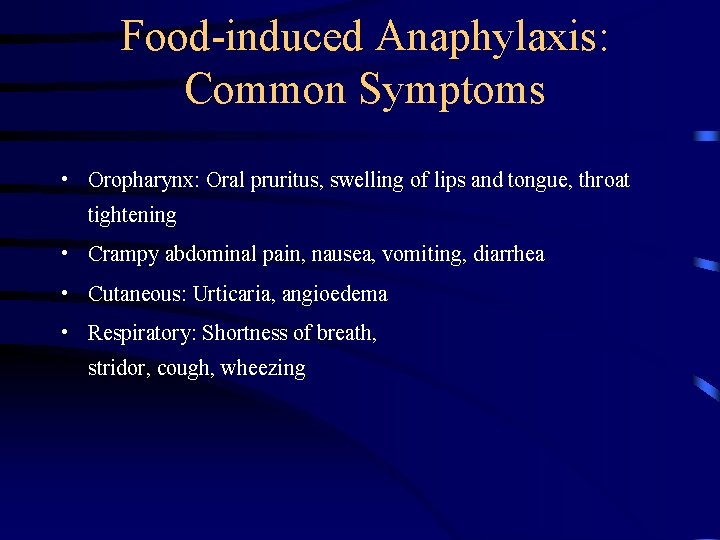
Food-induced Anaphylaxis: Common Symptoms • Oropharynx: Oral pruritus, swelling of lips and tongue, throat tightening • Crampy abdominal pain, nausea, vomiting, diarrhea • Cutaneous: Urticaria, angioedema • Respiratory: Shortness of breath, stridor, cough, wheezing
Food-induced Anaphylaxis: Fatal Reactions • Fatal reactions are on the rise – ~150 deaths per year – Usually caused by a known allergy • Patients at risk: – Peanut and tree nut allergy – Asthma – Prior anaphylaxis – Failure to treat promptly w/epinephrine • Many cases exhibit biphasic reaction
Fatal Food-induced Anaphylaxis (Bock SA, et al. JACI 2001; 107: 191– 193) • 32 cases of fatal anaphylaxis • Adolescents or young adults • 20 of 21 with complete history had asthma • Most did not have epinephrine available
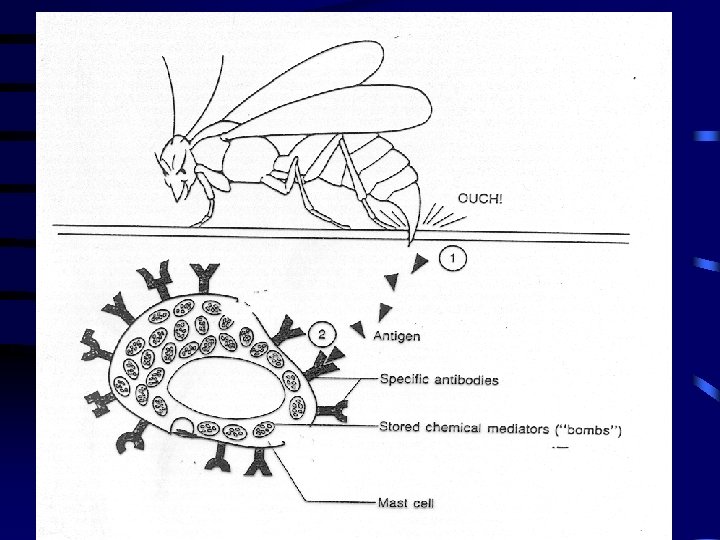
Venom-induced Anaphylaxis: Incidence • 0. 5%– 5% (13 million) Americans are sensitive to one or more insect venoms • Incidence rising due to more outdoor activities • At least 40– 100 deaths per year
Venom-induced Anaphylaxis: Common Culprits • Hymenoptera – – – Bees Wasps Yellow jackets Hornets Fire ants
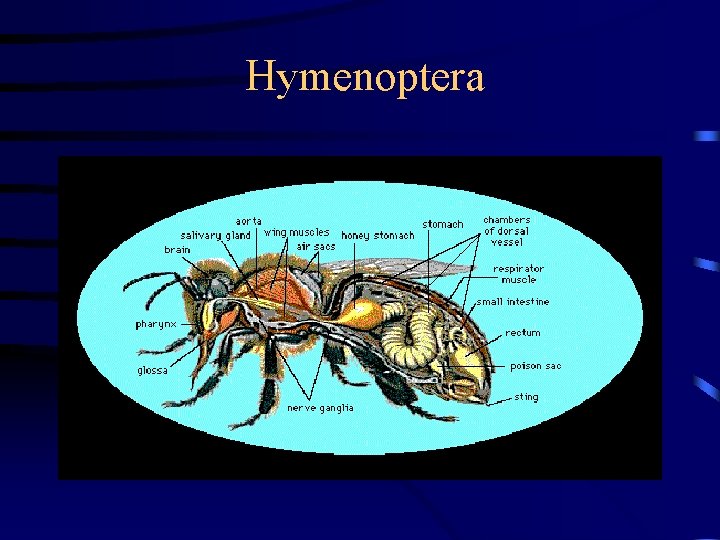
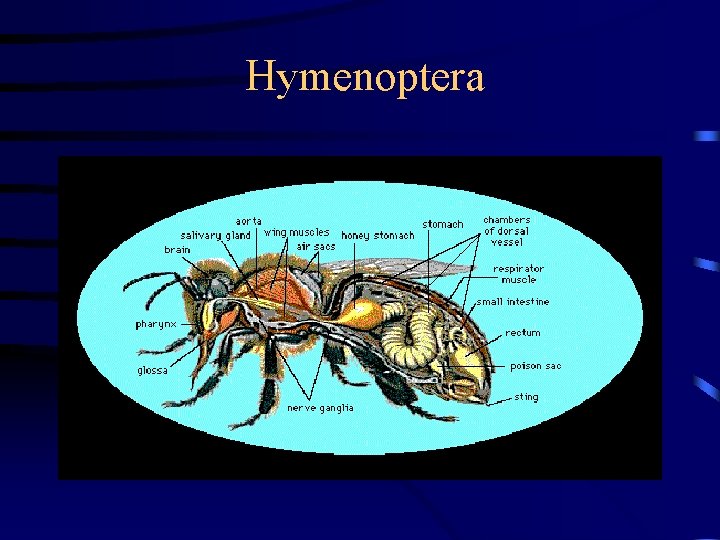
Hymenoptera
Venom-induced Reactions: Common Symptoms • Normal: Local pain, erythema, mild swelling • Large local: Extended swelling, erythema • Anaphylaxis: Usual onset within 15– 20 minutes – Cutaneous: urticaria, flushing, angioedema – Respiratory: dyspnea, stridor – Cardiovascular: hypotension, dizziness, – 30%– 60% of patients will experience a systemic reaction with subsequent stings
Venom-induced Anaphylaxis: Prevention Risk Management Keep Epi. Pen or Epi. Pen Jr on hand at all times Educate and train on Epi. Pen use Develop emergency action plan Consult an allergist to determine need for venom immunotherapy
Venom-induced Anaphylaxis: Immunotherapy Risk of anaphylaxis 10%-15% of patients experience systemic reactions during early weeks of treatment Sx generally occur within 20 minutes Patients at risk: asthma, prior reactions, beta blocker or ACEI therapy
Immunotherapy-induced Anaphylaxis Risk management Epinephrine immediately available Monitor closely for 20– 30 minutes Consider supply of Epi. Pen for those at high risk
Exercise-Induced Anaphylaxis • First reported in 1979 • Mechanism of action is unclear • Predisposing factors: – ASA , – Food, including shell fish, cheese, dense fruits, • Triggered by almost any physical exertion • Most common in very athletic children
Exercise-Induced Anaphylaxis • Four Phases – Prodromal phase is characterized by fatigue, warmth, pruritus, and cutaneous erythema – The early phase: urticarial eruption that progresses from giant hives may include angioedema of the face, palms, and soles. – Fully established phase: hypotension, syncope, loss of consciousness, choking, stridor, nausea, and vomiting ( 30 minutes to 4 hours. ) – Late or postexertional phase, Prolonged urticaria and headache persisting for 24 -74 hours.
Other Causes of Anaphylactic and Anaphylactoid Reactions • Drugs – Antibiotics – Chemotherapeutic agents – Aspirin, NSAIDs – Streptokinaise – Biologicals (vaccines, monoclonal antibodies) • Radiocontrast media (iodine) • Idiopathic
Diagnosing Anaphylaxis • Based on clinical presentation, • Cutaneous, respiratory most common • Some cases may be difficult to diagnose
Diagnosing Anaphylaxis • Careful history to identify possible causes • Can be confirmed by serum tryptase – Specific for mast cell degranulation – Remains elevated for up to 6 hours • Other labs to rule out other diagnoses • Refer to allergist for specific testing
Diagnosing Anaphylaxis Allergists can identify specific causes by: • Skin tests/RAST – Foods – Insect venoms – Drugs • Challenge tests – Foods – NSAIDs – Exercise
Use of Epi Pen • Immediate treatment with epinephrine imperative – No contraindications in anaphylaxis – Failure or delay associated with fatalities – i. m. may produce more rapid, higher peak levels vs s. c. – Must be available at all times
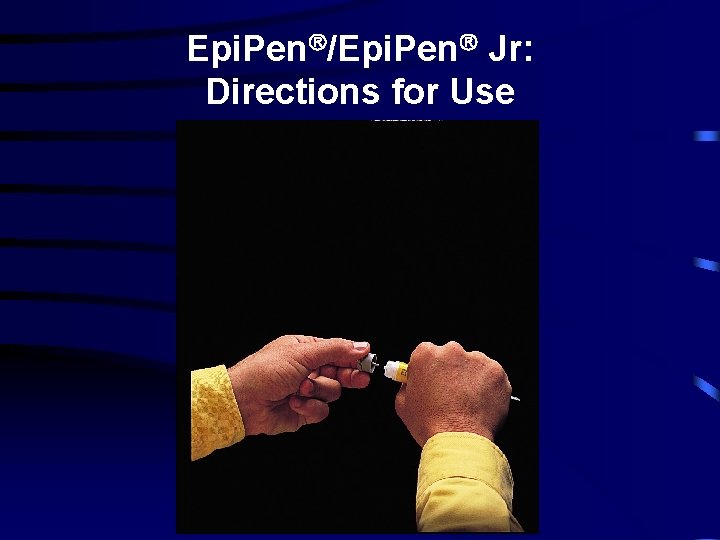
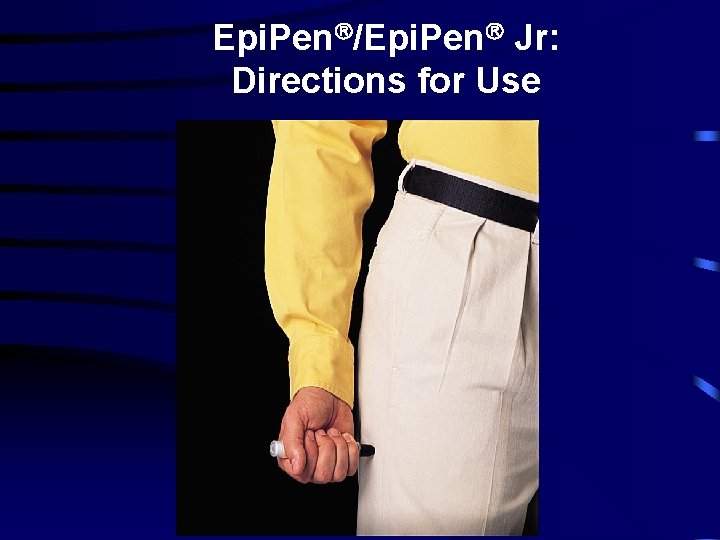
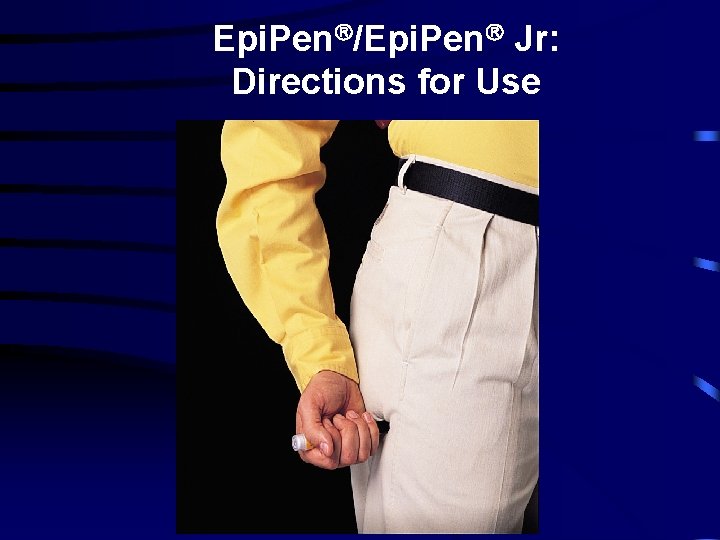
Epi. Pen /Epi. Pen Jr: Directions for Use
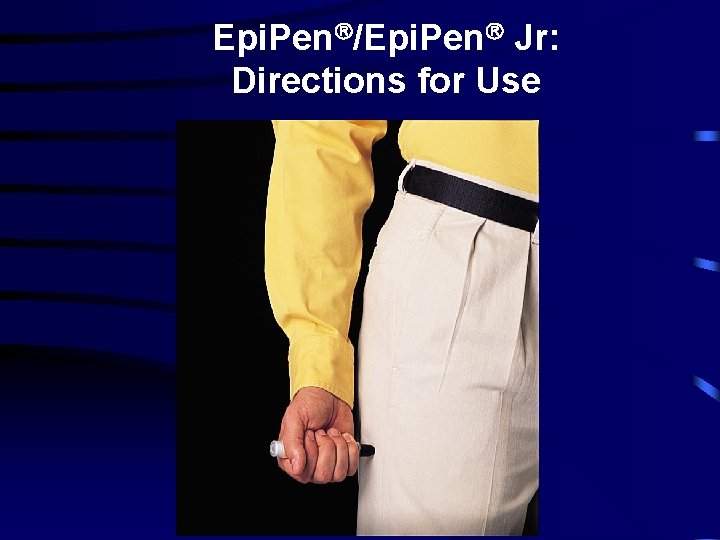
Epi. Pen /Epi. Pen Jr: Directions for Use
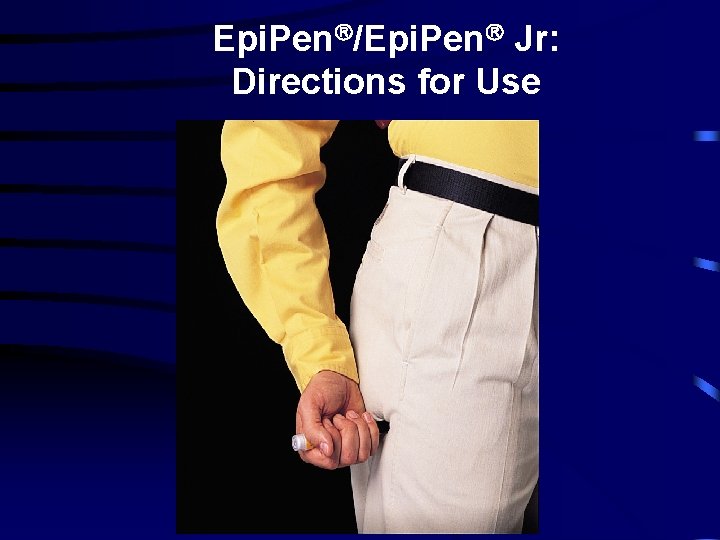
Epi. Pen /Epi. Pen Jr: Directions for Use
Treatment of Anaphylaxis • Simple BLS (O 2, position, etc) • Anti Histamines – Clemastine i. v. • Corticosteroids – Decadron, Solu-medrol, etc • Treat Hypotension – i. v. fluids – Dopamine 5 -20 mcg/min
Treatment of Anaphylaxis • Broncheodiators – Albuterol MDI or Neb • Observe for a minimum 8 -12 hours – Insure F/U with PMD, – Benadryl for 24 hours. • Rebound or persitant S/S – Repeat epinephrine if Sx persist or increase after 10 -15 minutes – Repeat antihistamine ± H 2 blocker if Sx persist
Screening Patients at Risk Did you ever have a severe allergic reaction: • To any food? • To any medicine? • To an insect sting? • To latex? • Side effect or allergic reaction? • That caused breathing trouble? Severe hives and swelling? Severe vomiting or diarrhea? Dizziness? • That required you to go to the hospital?

® Epi. Pen 2 -Pak