Anaphlaxis Dr Ferdi Menda Anaphylaxis A severe life
- Slides: 37
Anaphlaxis Dr Ferdi Menda
Anaphylaxis ¡ A severe life threatening (Type I) immediate hypersensitivity reaction. ¡ The reaction occurs when the person reexposed to an ‘allergen’, which leads to Ig. E Ab during previous exposure.
Anaphylaxis l. Injected, inhaled or ingested substance –usually drugs, food, insect venomcan serve as the allergen itself.
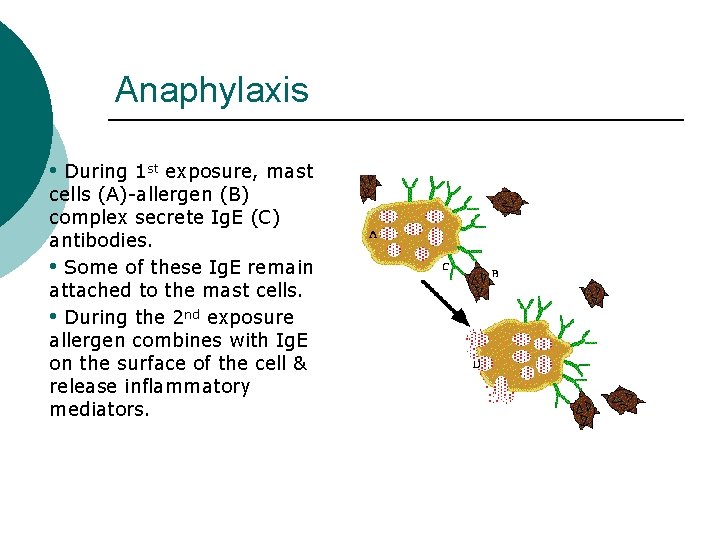
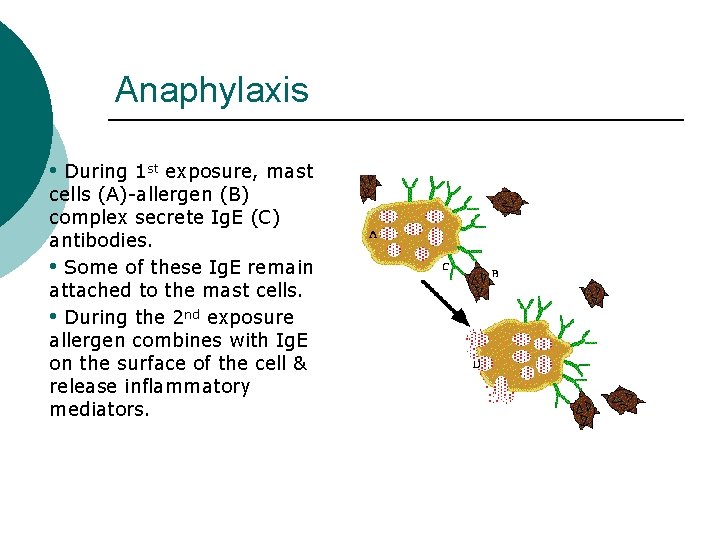
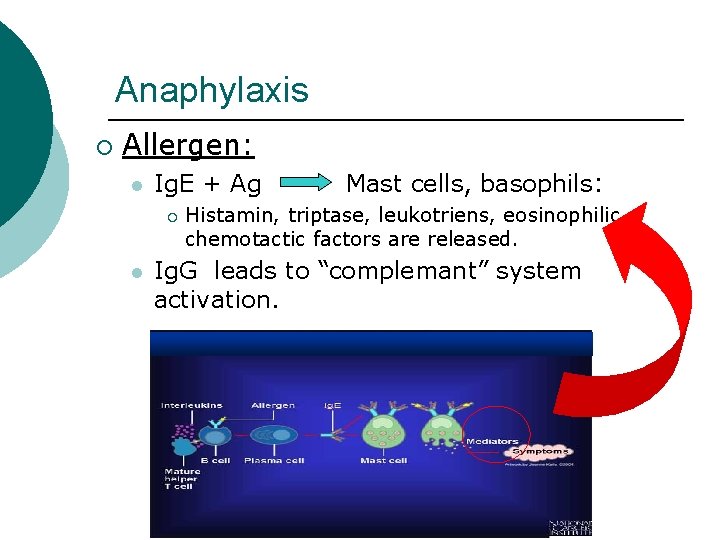
Anaphylaxis • During 1 st exposure, mast cells (A)-allergen (B) complex secrete Ig. E (C) antibodies. • Some of these Ig. E remain attached to the mast cells. • During the 2 nd exposure allergen combines with Ig. E on the surface of the cell & release inflammatory mediators.
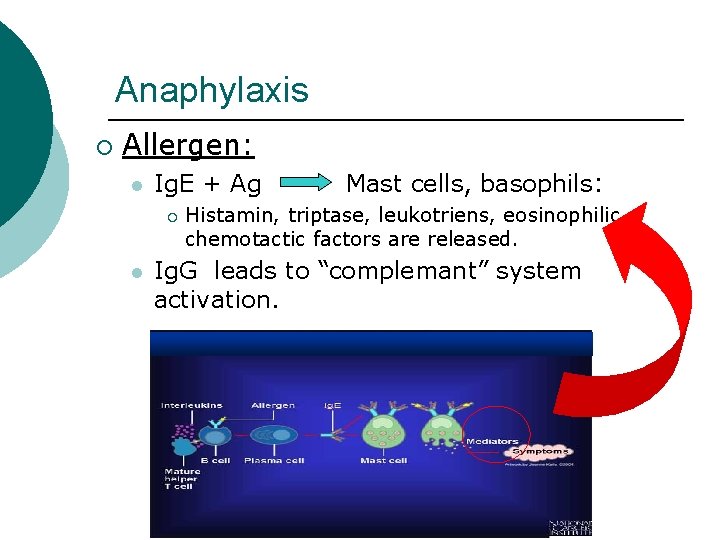
Anaphylaxis ¡ Allergen: l Ig. E + Ag ¡ l Mast cells, basophils: Histamin, triptase, leukotriens, eosinophilic chemotactic factors are released. Ig. G leads to “complemant” system activation.
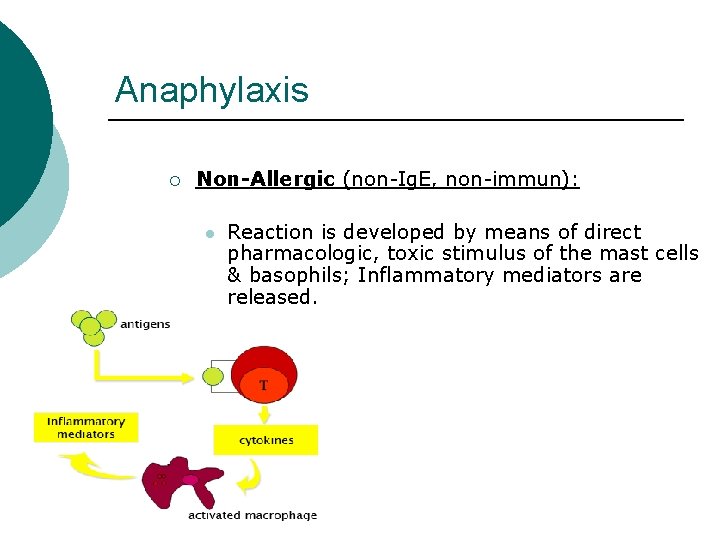
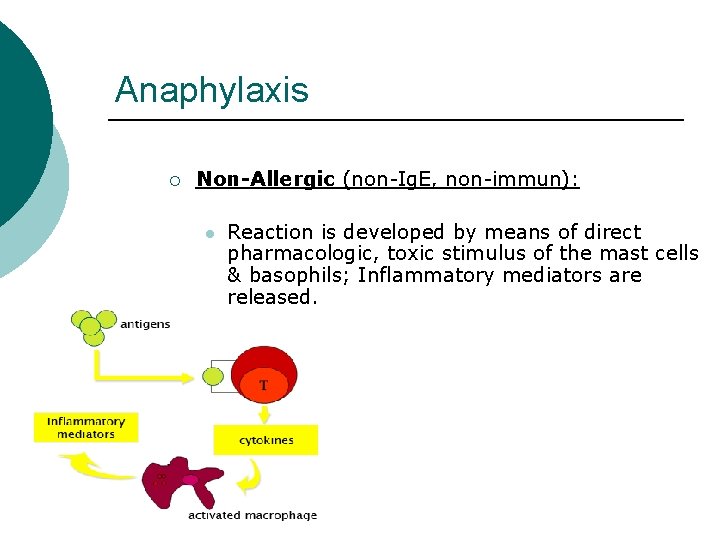
Anaphylaxis ¡ Non-Allergic (non-Ig. E, non-immun): l Reaction is developed by means of direct pharmacologic, toxic stimulus of the mast cells & basophils; Inflammatory mediators are released.
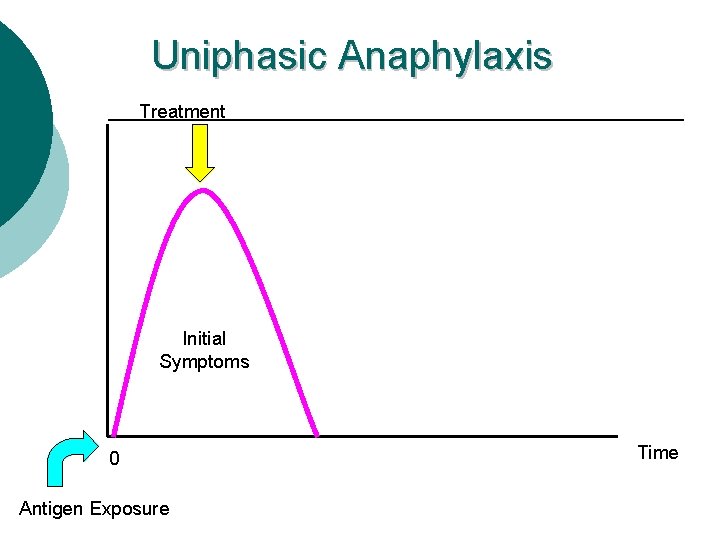
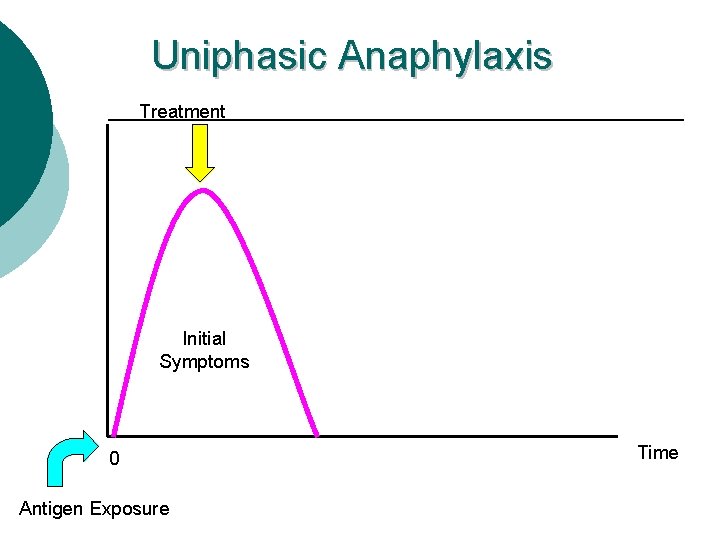
Uniphasic Anaphylaxis Treatment Initial Symptoms 0 Antigen Exposure Time
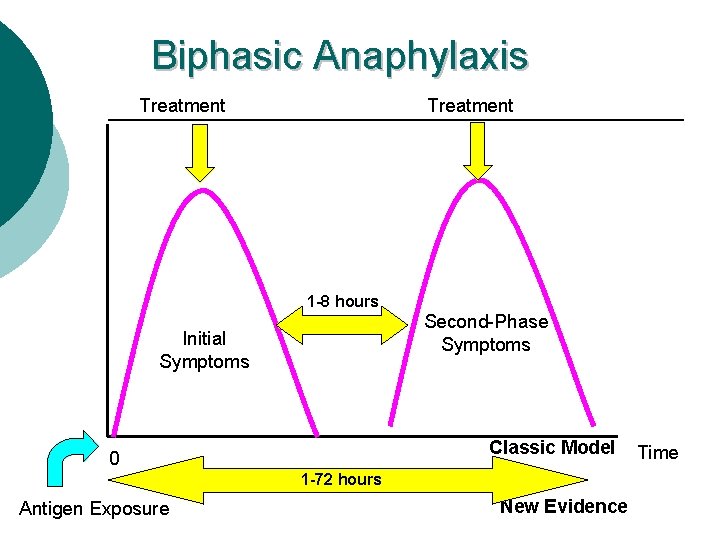
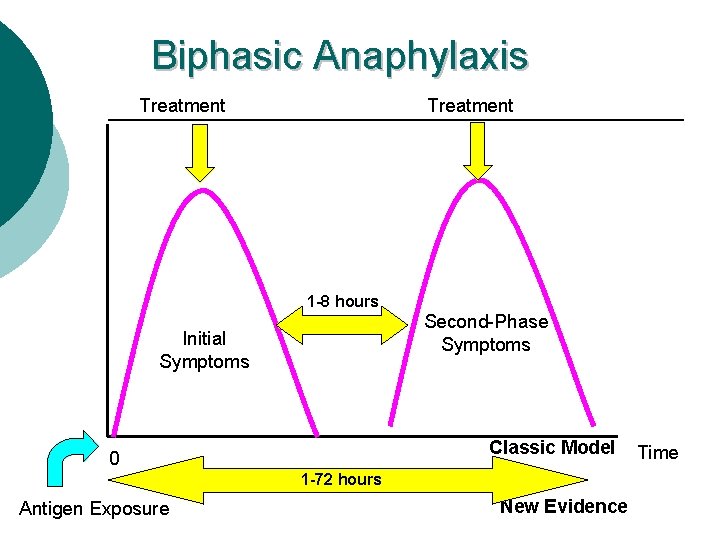
Biphasic Anaphylaxis Treatment 1 -8 hours Second-Phase Symptoms Initial Symptoms Classic Model 0 1 -72 hours Antigen Exposure New Evidence Time
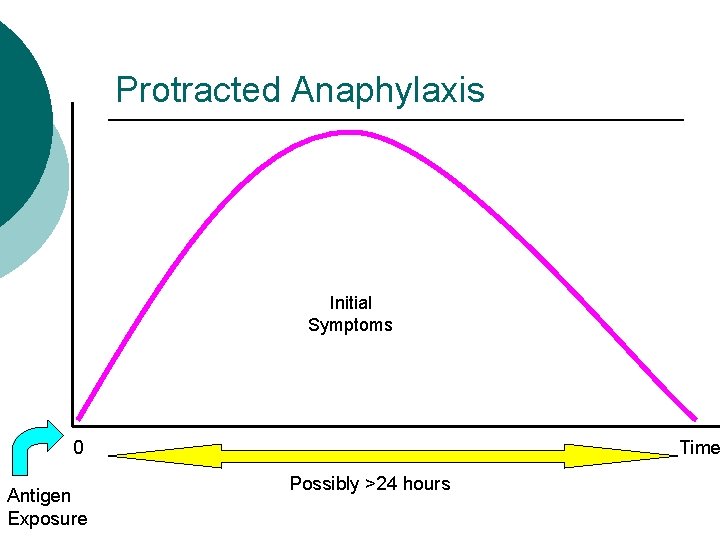
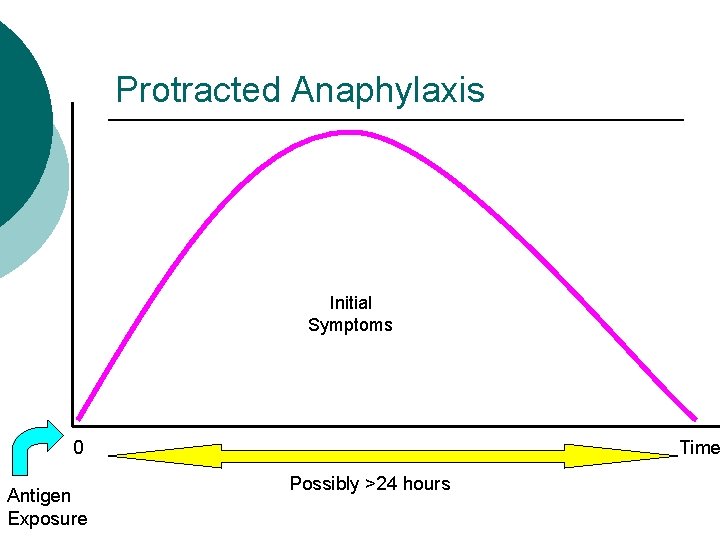
Protracted Anaphylaxis Initial Symptoms 0 Antigen Exposure Time Possibly >24 hours
Anaphylactoid reaction ¡ An identical or very similar clinical response (skin reaction) which is not mediated by Ig. E, or an Antigen-Antibody process.
Anaphylaxis during Anesthesia ¡ Anaphylaxis incidence during anesthesia is: 1/5. 000 -1/20. 000 ¡ Multiple drug use duing general anesthesia may mask the symptoms. ¡ Diagnosis during anesthesia is DIFFICULT !
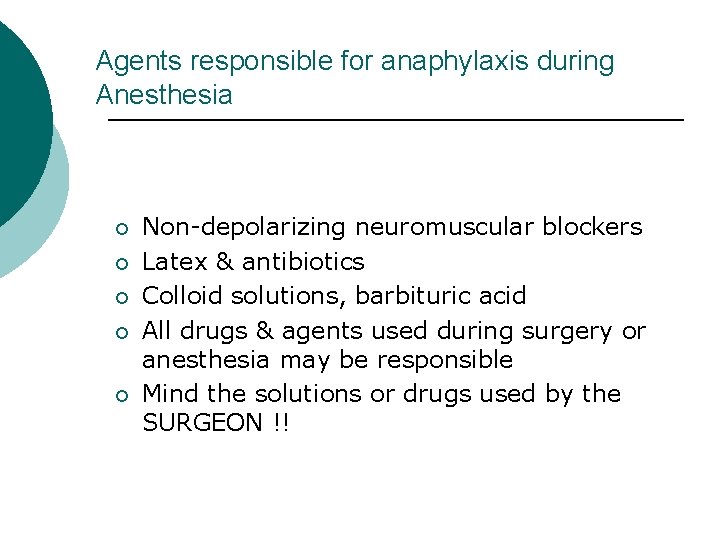
Agents responsible for anaphylaxis during Anesthesia ¡ ¡ ¡ Non-depolarizing neuromuscular blockers Latex & antibiotics Colloid solutions, barbituric acid All drugs & agents used during surgery or anesthesia may be responsible Mind the solutions or drugs used by the SURGEON !!
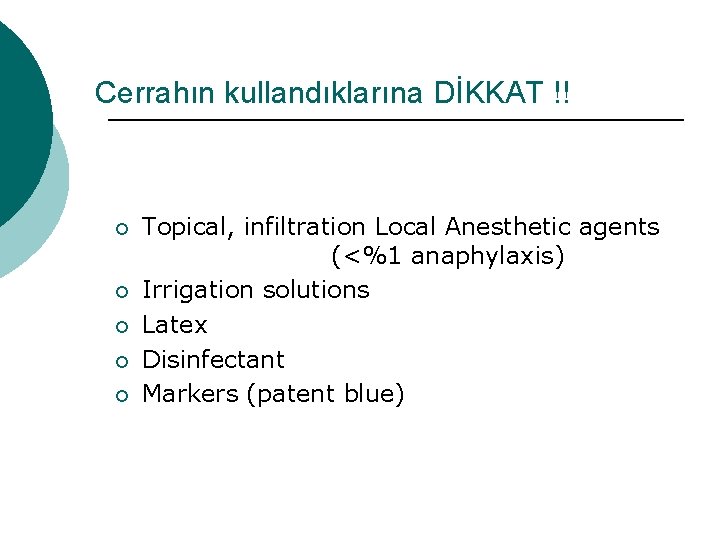
Cerrahın kullandıklarına DİKKAT !! ¡ ¡ ¡ Topical, infiltration Local Anesthetic agents (<%1 anaphylaxis) Irrigation solutions Latex Disinfectant Markers (patent blue)
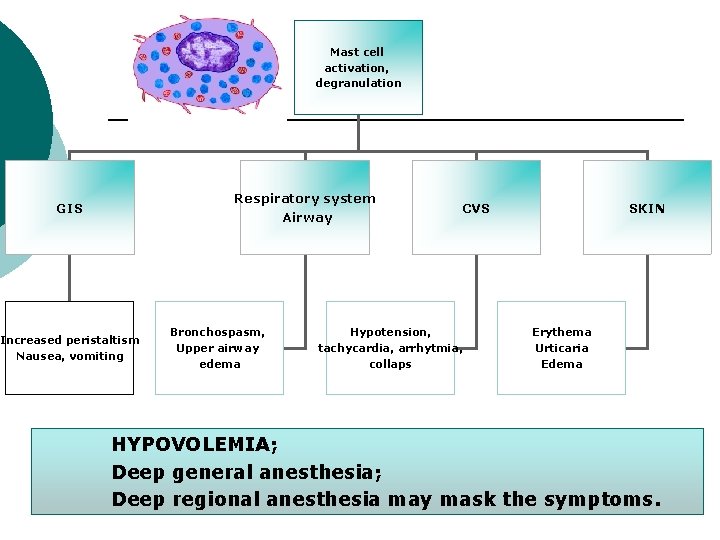
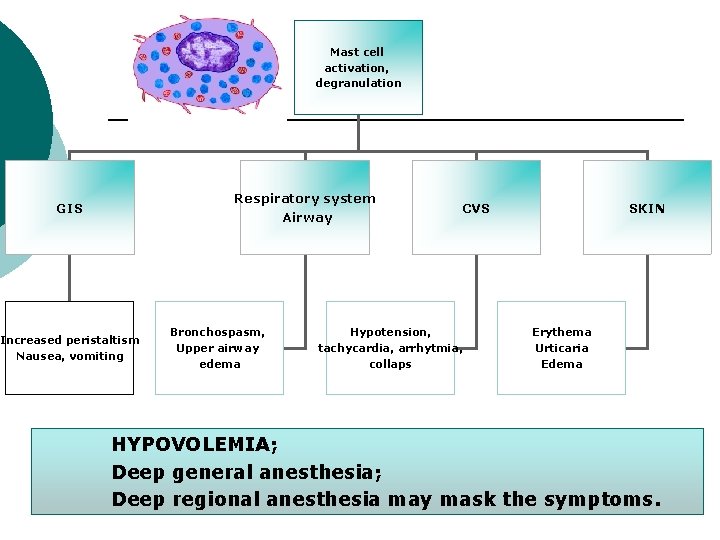
Mast cell activation, degranulation Respiratory system Airway GIS Increased peristaltism Nausea, vomiting Bronchospasm, Upper airway edema CVS Hypotension, tachycardia, arrhytmia, collaps SKIN Erythema Urticaria Edema HYPOVOLEMIA; Deep general anesthesia; Deep regional anesthesia may mask the symptoms.
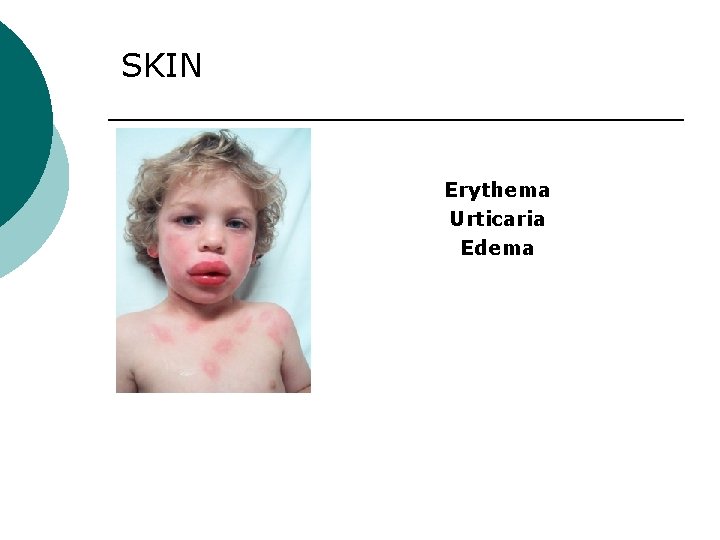
SKIN Erythema Urticaria Edema
UPPER AIRWAY • Stridor • Hoarseness • Angioedema • Sneezing
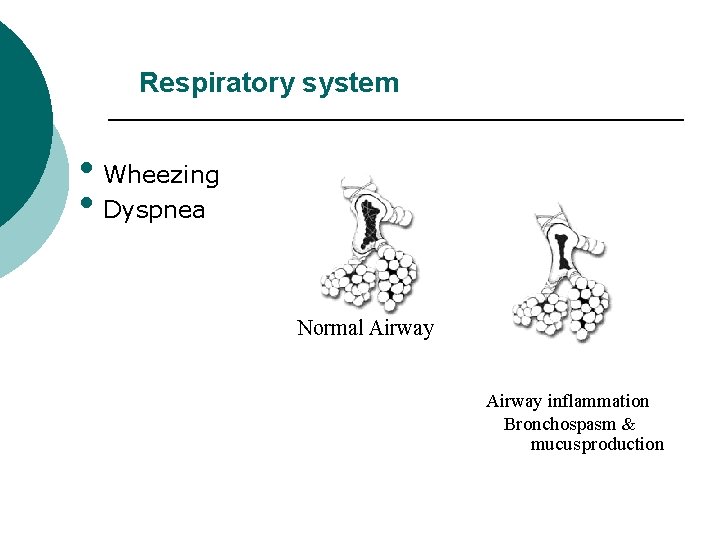
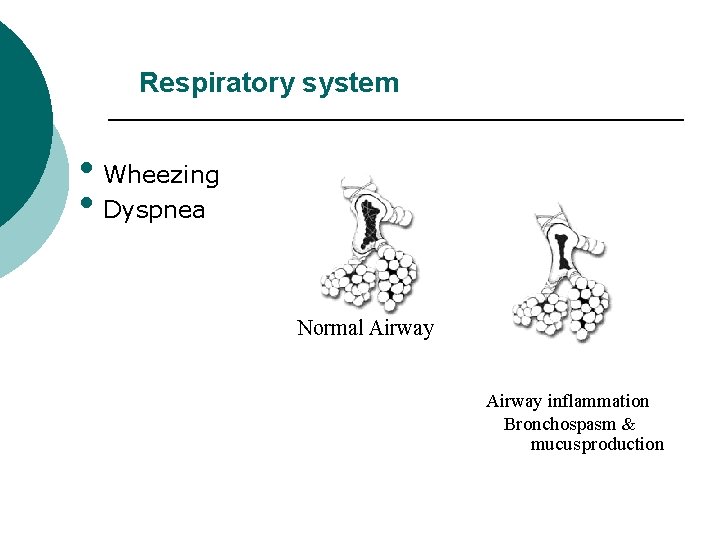
Respiratory system • Wheezing • Dyspnea Normal Airway inflammation Bronchospasm & mucusproduction
Cardiovascular symptoms arrhythmias
Gastrointestinal symptoms § § § Nausea, vomiting, Diarrhea, Abdominal cramp like pain: uncommon except with food allergies.
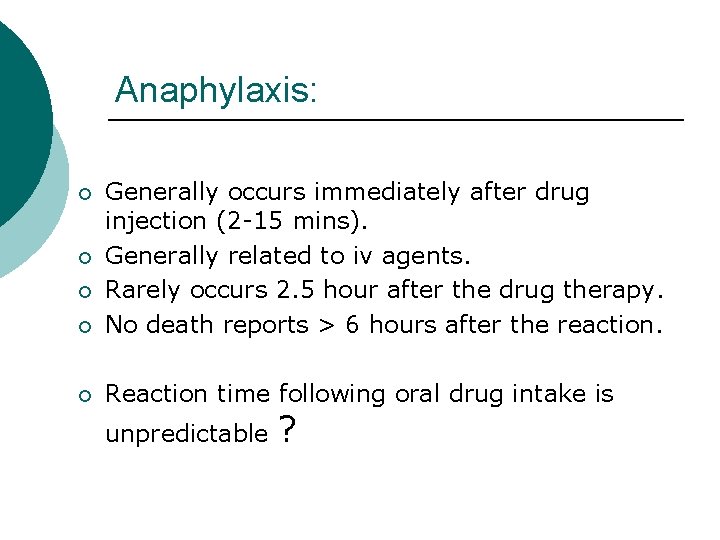
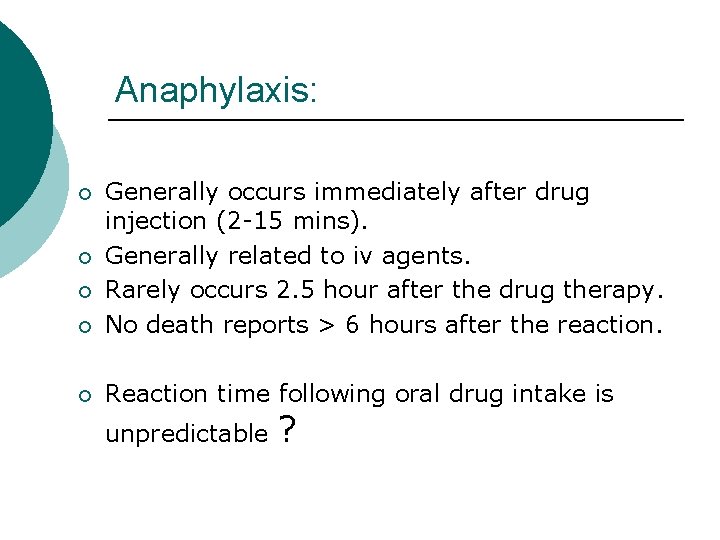
Anaphylaxis: ¡ Generally occurs immediately after drug injection (2 -15 mins). Generally related to iv agents. Rarely occurs 2. 5 hour after the drug therapy. No death reports > 6 hours after the reaction. ¡ Reaction time following oral drug intake is ¡ ¡ ¡ unpredictable ?
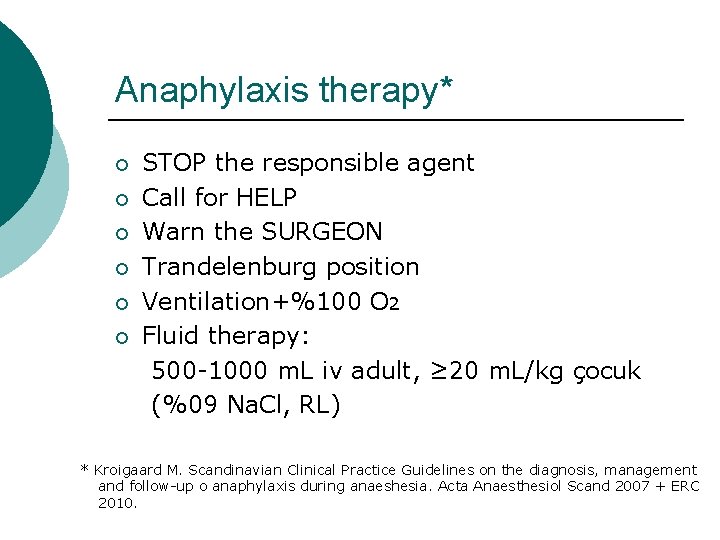
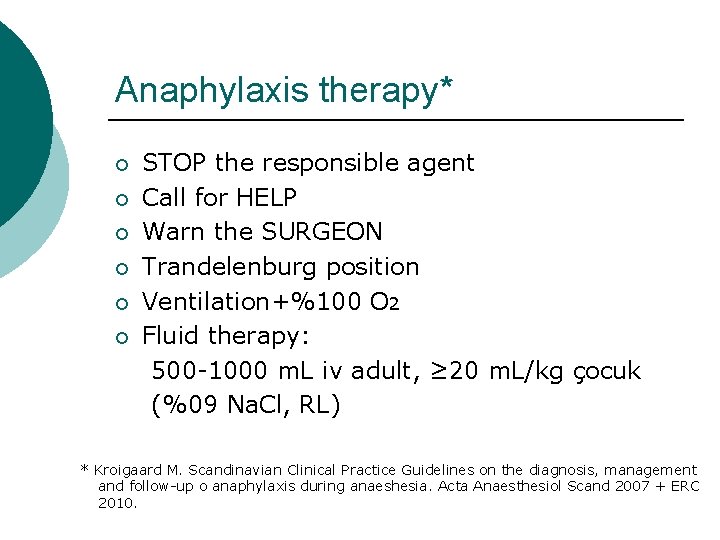
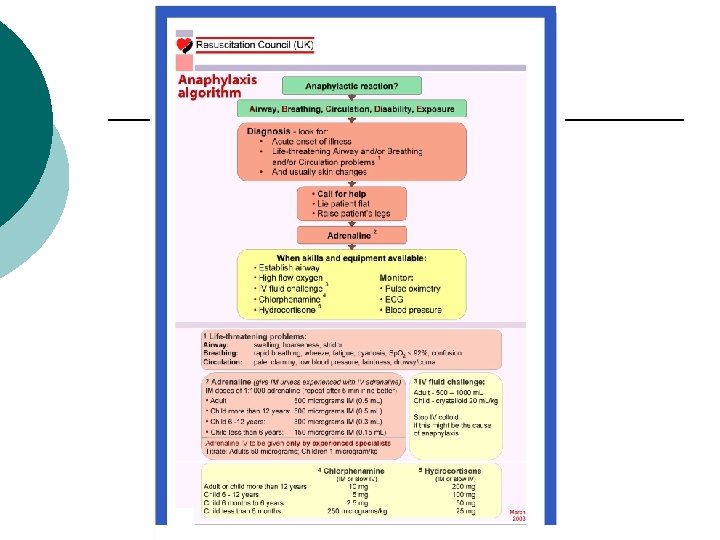
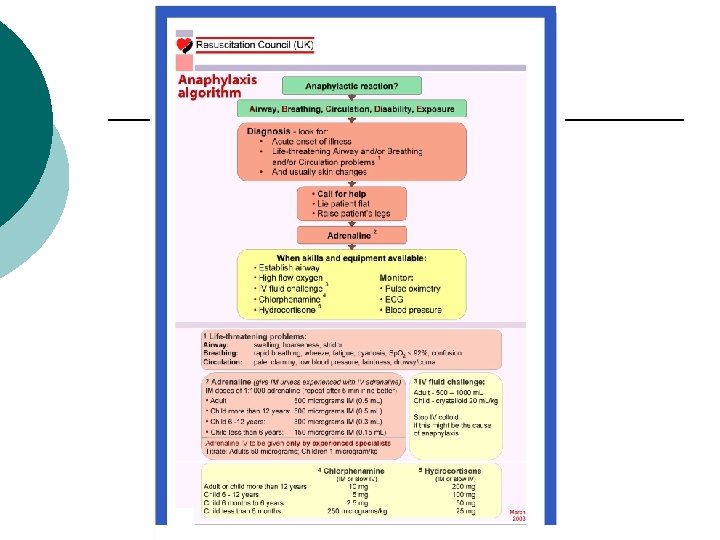
Anaphylaxis therapy* ¡ ¡ ¡ STOP the responsible agent Call for HELP Warn the SURGEON Trandelenburg position Ventilation+%100 O 2 Fluid therapy: 500 -1000 m. L iv adult, ≥ 20 m. L/kg çocuk (%09 Na. Cl, RL) * Kroigaard M. Scandinavian Clinical Practice Guidelines on the diagnosis, management and follow-up o anaphylaxis during anaeshesia. Acta Anaesthesiol Scand 2007 + ERC 2010.
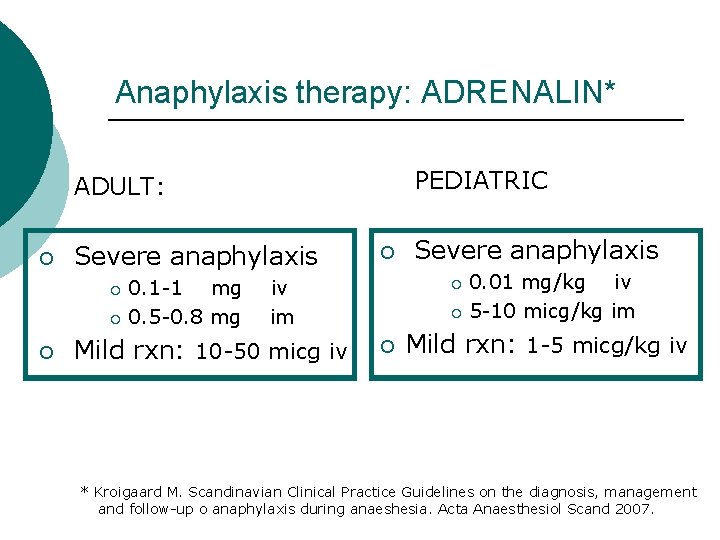
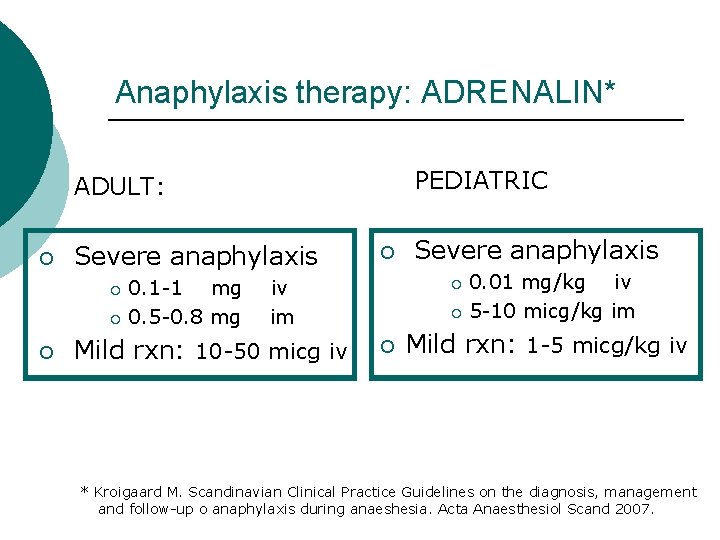
Anaphylaxis therapy: ADRENALIN* PEDIATRIC ADULT: ¡ Severe anaphylaxis 0. 1 -1 mg ¡ 0. 5 -0. 8 mg ¡ ¡ ¡ 0. 01 mg/kg iv ¡ 5 -10 micg/kg im iv im Mild rxn: 10 -50 micg iv Severe anaphylaxis ¡ ¡ Mild rxn: 1 -5 micg/kg iv * Kroigaard M. Scandinavian Clinical Practice Guidelines on the diagnosis, management and follow-up o anaphylaxis during anaeshesia. Acta Anaesthesiol Scand 2007.
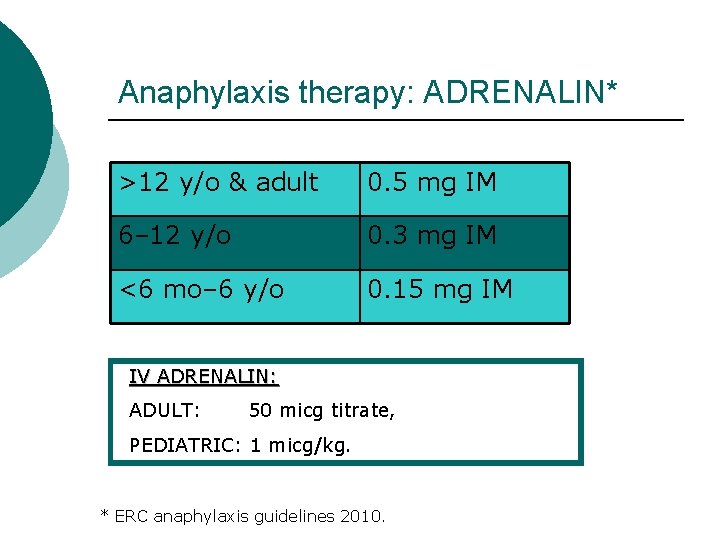
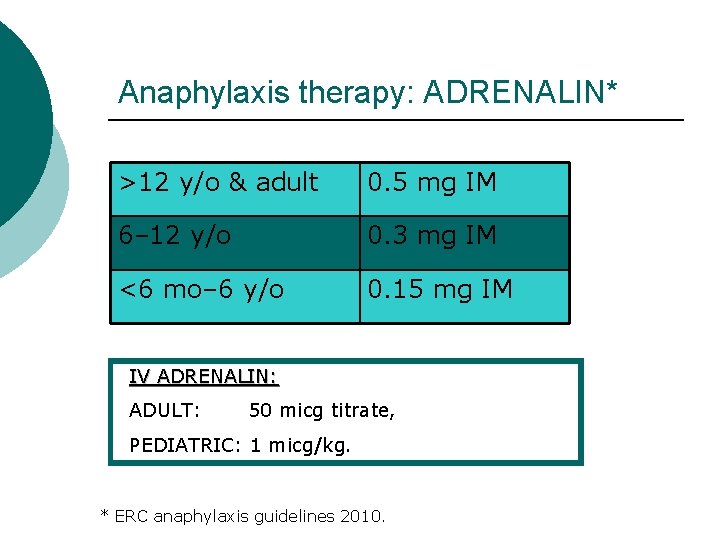
Anaphylaxis therapy: ADRENALIN* >12 y/o & adult 0. 5 mg IM 6– 12 y/o 0. 3 mg IM <6 mo– 6 y/o 0. 15 mg IM IV ADRENALIN: ADULT: 50 micg titrate, PEDIATRIC: 1 micg/kg. * ERC anaphylaxis guidelines 2010.
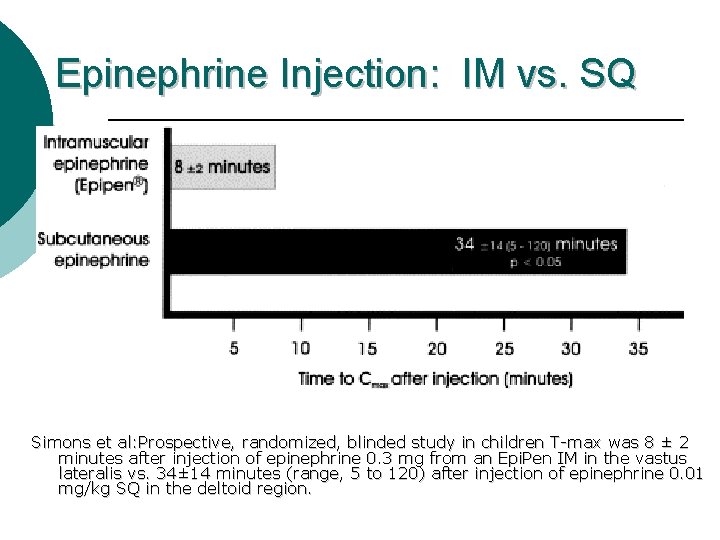
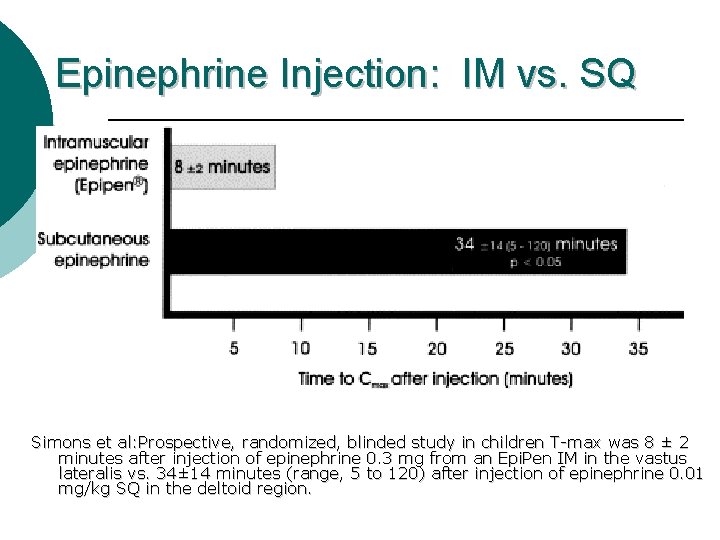
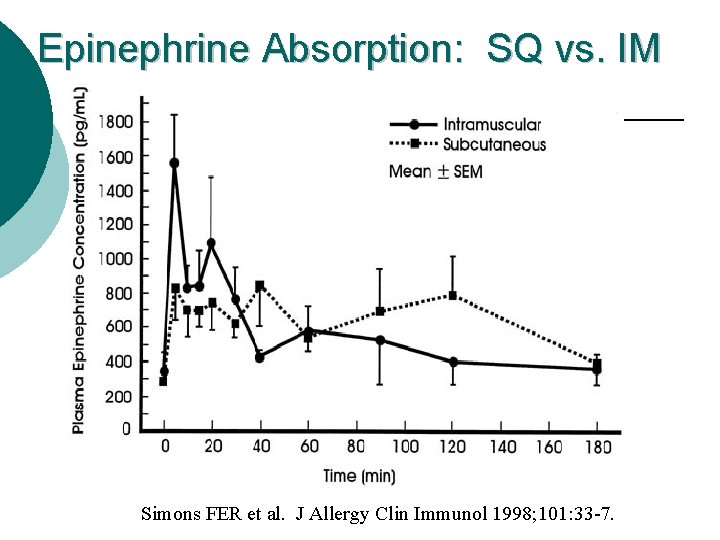
Epinephrine Injection: IM vs. SQ Simons et al: Prospective, randomized, blinded study in children T-max was 8 ± 2 minutes after injection of epinephrine 0. 3 mg from an Epi. Pen IM in the vastus lateralis vs. 34± 14 minutes (range, 5 to 120) after injection of epinephrine 0. 01 mg/kg SQ in the deltoid region.
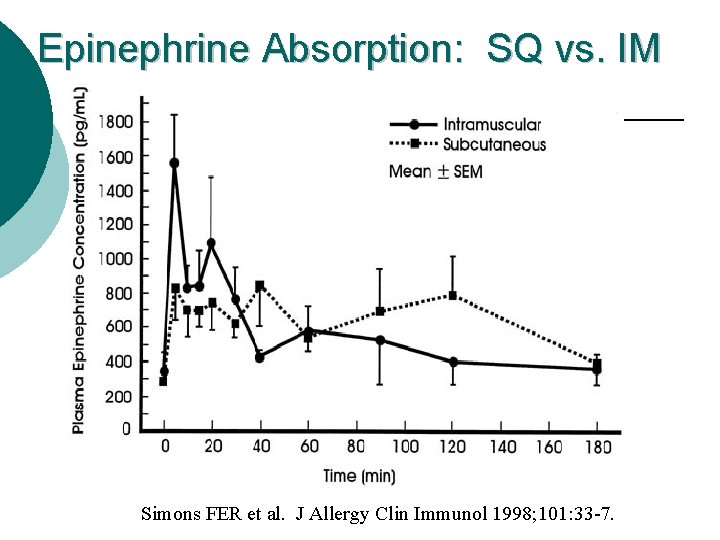
Epinephrine Absorption: SQ vs. IM Simons FER et al. J Allergy Clin Immunol 1998; 101: 33 -7.
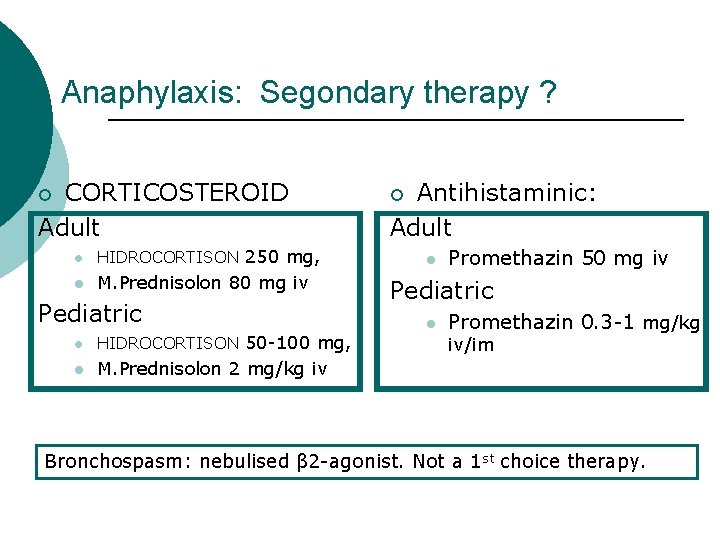
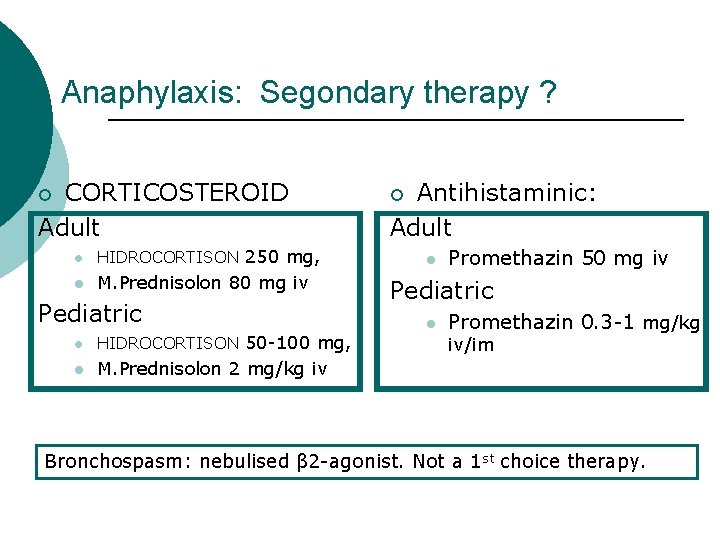
Anaphylaxis: Segondary therapy ? CORTICOSTEROID Adult ¡ l HIDROCORTISON 250 mg, l M. Prednisolon 80 mg iv Pediatric l HIDROCORTISON 50 -100 mg, l M. Prednisolon 2 mg/kg iv Antihistaminic: Adult ¡ l Promethazin 50 mg iv Pediatric l Promethazin 0. 3 -1 mg/kg iv/im Bronchospasm: nebulised β 2 -agonist. Not a 1 st choice therapy.
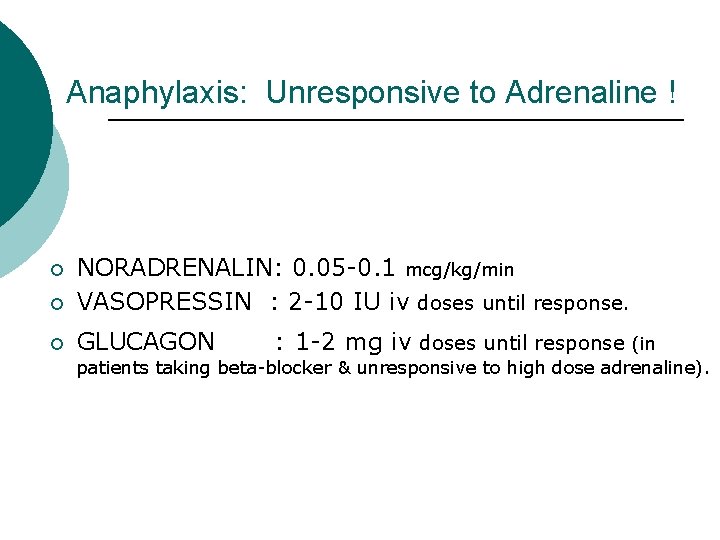
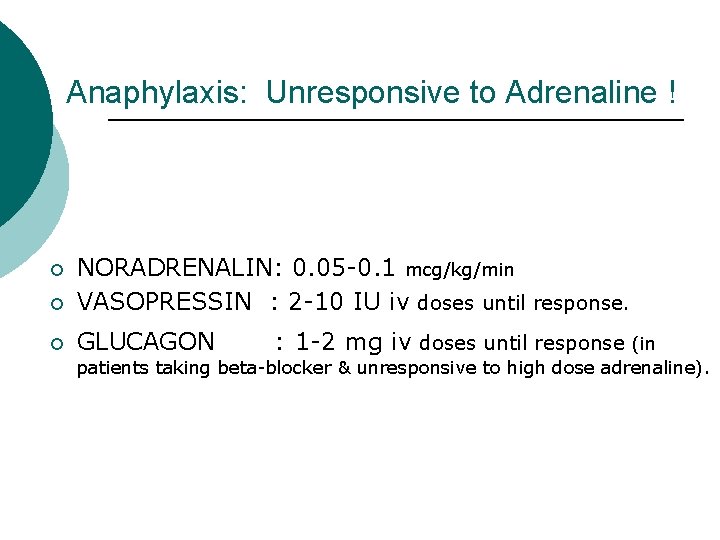
Anaphylaxis: Unresponsive to Adrenaline ! ¡ NORADRENALIN: 0. 05 -0. 1 mcg/kg/min VASOPRESSIN : 2 -10 IU iv doses until response. ¡ GLUCAGON ¡ : 1 -2 mg iv doses until response (in patients taking beta-blocker & unresponsive to high dose adrenaline).
Patients having anaphylactic rxn previously with Polen, animal fur, dust atopy ¡ Former prolonged latex exposure ¡ may develop reaction with LATEX.
RECOMMENDATIONS ¡ ¡ ¡ Anaphylaxis with Local Anesthetics is RARE; prefer Regional or local anesthesia. Agent of choice for General anesthesia is VOLATILE. “No Anaphylaxis is reported” AVOID Latex & Neuromusculer blockers ! Antihistaminic/steroid premedication will probably not prevent “anaphylactic shock” ? If known to cause a previous reaction, avoid using that drug/agent.
Follow-up ¡ After a moderate-severe anaphylactic rxn: l l l ¡ Follow-up with blood (triptase), then skin test. Skin test: skin prick, intradermal test (Ig. E) or If there is a local or disseminated urticeria related to Chlorhexidin skin test is necessary. Follow-up is not necessary: l Erhythema around the injection site, isolated bronchospasm in patients with previous bronchial reactivity.
When we decide an Alergy test, the following should be reported: ¡ ¡ ¡ ¡ Symptoms Severity of the reaction Onset time and length of the reaction, Therapy All the agents used before the reaction Anesthesia form, notes Fill the advers event form.
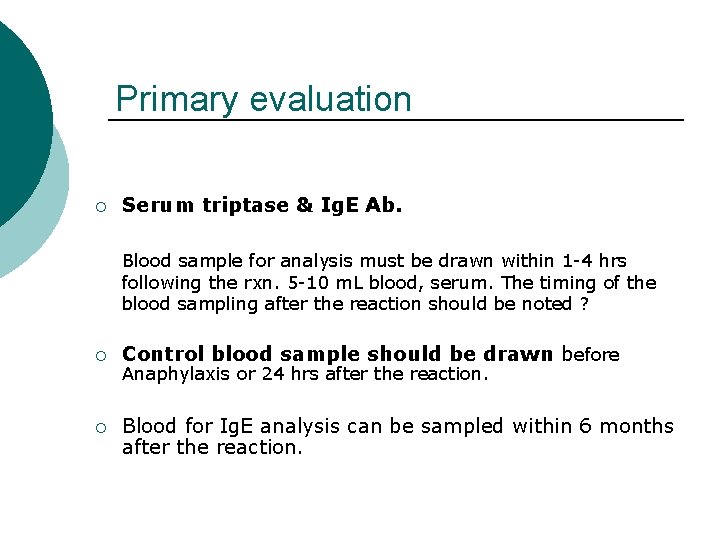
Primary evaluation ¡ Serum triptase & Ig. E Ab. Blood sample for analysis must be drawn within 1 -4 hrs following the rxn. 5 -10 m. L blood, serum. The timing of the blood sampling after the reaction should be noted ? ¡ Control blood sample should be drawn before ¡ Blood for Ig. E analysis can be sampled within 6 months after the reaction. Anaphylaxis or 24 hrs after the reaction.
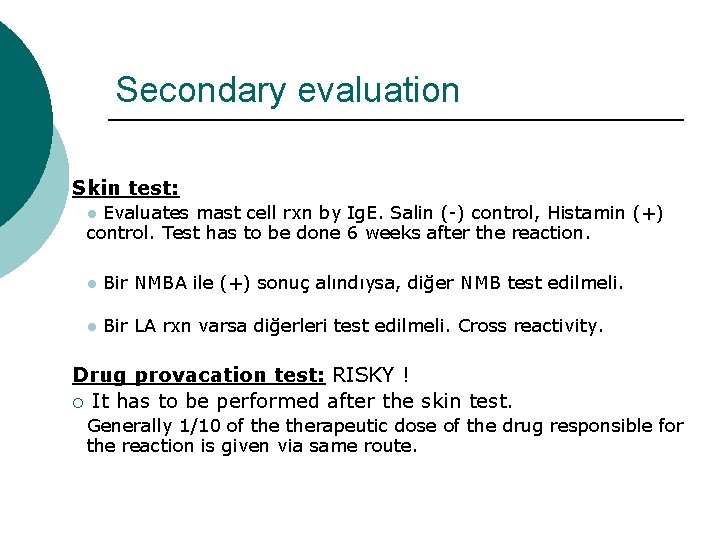
Secondary evaluation Skin test: Evaluates mast cell rxn by Ig. E. Salin (-) control, Histamin (+) control. Test has to be done 6 weeks after the reaction. l l Bir NMBA ile (+) sonuç alındıysa, diğer NMB test edilmeli. l Bir LA rxn varsa diğerleri test edilmeli. Cross reactivity. Drug provacation test: RISKY ! ¡ It has to be performed after the skin test. Generally 1/10 of therapeutic dose of the drug responsible for the reaction is given via same route.
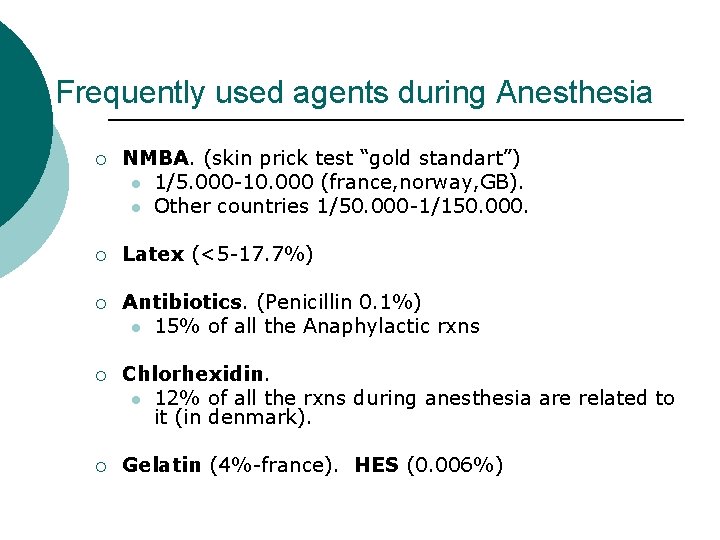
Frequently used agents during Anesthesia ¡ NMBA. (skin prick test “gold standart”) l 1/5. 000 -10. 000 (france, norway, GB). l Other countries 1/50. 000 -1/150. 000. ¡ Latex (<5 -17. 7%) ¡ Antibiotics. (Penicillin 0. 1%) l 15% of all the Anaphylactic rxns ¡ Chlorhexidin. l 12% of all the rxns during anesthesia are related to it (in denmark). ¡ Gelatin (4%-france). HES (0. 006%)
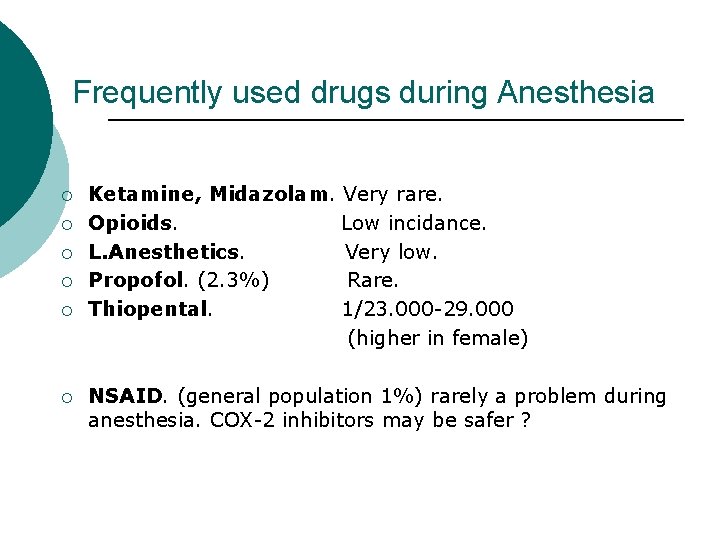
Frequently used drugs during Anesthesia ¡ ¡ ¡ Ketamine, Midazolam. Very rare. Opioids. Low incidance. L. Anesthetics. Very low. Propofol. (2. 3%) Rare. Thiopental. 1/23. 000 -29. 000 (higher in female) NSAID. (general population 1%) rarely a problem during anesthesia. COX-2 inhibitors may be safer ?
WARN the patient Bracelet ¡ Detailed epicrisis ¡