Anaesthesia and Morbid Obesity Facts l 20 adults
Anaesthesia and Morbid Obesity
Facts l 20% adults Obese (1% Morbidly Obese) l BMI >35 with comorbidity / BMI >40 without comorbidity = morbidly obese l BMI > 55 = super-morbidly obese l BMI > 30 – rapid increase in morbidity and mortality l Men – higher risk of CVS problems
Apples and Pears l BMI poor predictor of difficulty l Fat distribution Android Gynaecoid
Causes of Obesity l Multifactorial l Genetic and Environmental l Regulation of appetite and satiety (Hypothalamus) l Leptin, Adiponectin – long term (NB dieting) l Insulin = short term (Hypothalamus) l Ghrelin (Stomach Wall), Peptide YY 3 -36 (Intestine)
Comorbidity
Facts l Obesity associated with: l l l l Htn DM OA Liver Disease Asthma OSA Obesity Hypoventilation Syndrome Risk of cardio-resp comorbidity increases with duration l NB severe comorbidity may be masked by sedentary lifestyle! l
Respiratory System - OSA l Apnoeic attacks due to collapse of pharynx whilst asleep l Increases with obesity and age l Fat in pharyngeal wall l Features Snoring l Frequent apnoeic spells whilst asleep (>10 s) l Daytime somnolescence l Pathophysiological changes – hypercapnia, polycythaemia, pulmonary htn and cor-pulmonale l
Obesity Hypoventilation Syndrome l Affects control of breathing l CO 2 sensitivity and ventilatory drive partly leptin controlled l Leptin insensitivity = reduced ventilatory response to CO 2. l Depressant drugs accentuate l Often combined with OSA
Respiratory Compromise l Features l l l l l Hypoxaemia at rest (worse supine + depressants) Rapid desaturation in apnoea Reduced lung compliance (increased pulm blood volume) Reduced chest wall compliance Small airways collapse + diaphragmatic splinting (Decreased FRC) Increased alveolar-arterial oxygen tension (worse on induction) Closing volume close to FRC – airway closure and V/Q mismatch (shunting) Atelectasis NB Laparoscopy!! Postoperative period
Cardiovascular System Circulating Volume (renin-angiotensin. Polycythaemia). l l l l Ventricular Workload Redistributed to fat beds Cerebral/Renal flows unchanged Oxygen Consumption (Increased BMR) CO 2 production Systemic Htn (LV stress and LVH) Pulm Htn possible (Cor-Pulmonale) Increased metabolic demands of adipose
Cardiovascular System l Arrythmias – Why? l l l l IHD l l l Myocardial hypertrophy and hypoxaemia Hyperkalaemia (Htn Rx) CAD Increased circulating catecholamines OSA Fatty infiltration conducting system Htn DM Cholesterol Sedentary Lifestyle DVT/PE
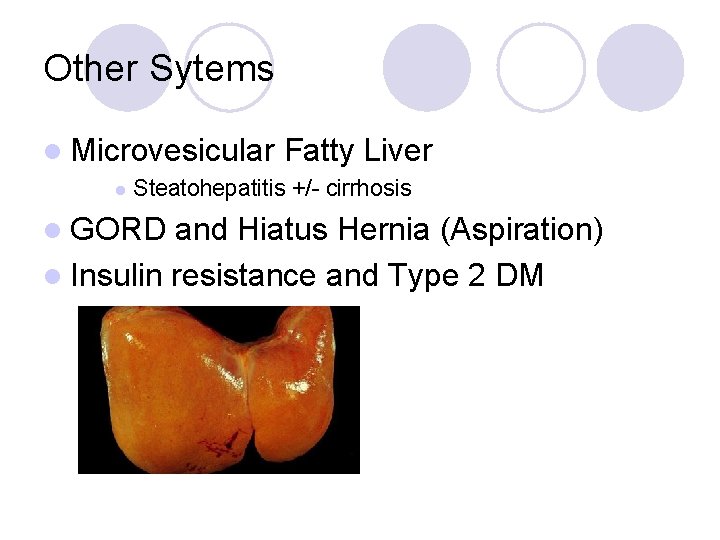
Other Sytems l Microvesicular l Fatty Liver Steatohepatitis +/- cirrhosis l GORD and Hiatus Hernia (Aspiration) l Insulin resistance and Type 2 DM
Preoperative Assessment
Planning Ahead l Beware the Sedentary Patient l Questioning Symptoms and signs of OSA/Heart Failure l Comorbid disease l Ability to tolerate supine position l l Full airway assessment Mouth opening, Mallampati, Neck movement, Collar circumference l Any airway obstruction whilst awake l

Pre-Op Investigations l Individual basis l FBC, U+Es, LFTs, Glucose l ABG in suspected OSA/OHS l ECG l Echo – LV/RV function, Pulm Htn l CXR – cardiac failure l PFTs – poor exercise tolerance
Pre. Med l Antacids / PPI l Prokinetics l Sodium Citrate l TEDs
Conduct of Anaesthesia

Pharmacokinetics l Most drugs affected by adipose tissue – lipophilic drugs l How do you calculate doses? ! l Volume of central compartment similar (periph increased) l Increased Volume of Distribution (Vd) Increased redistribution l Increased elimination t 1/2 l
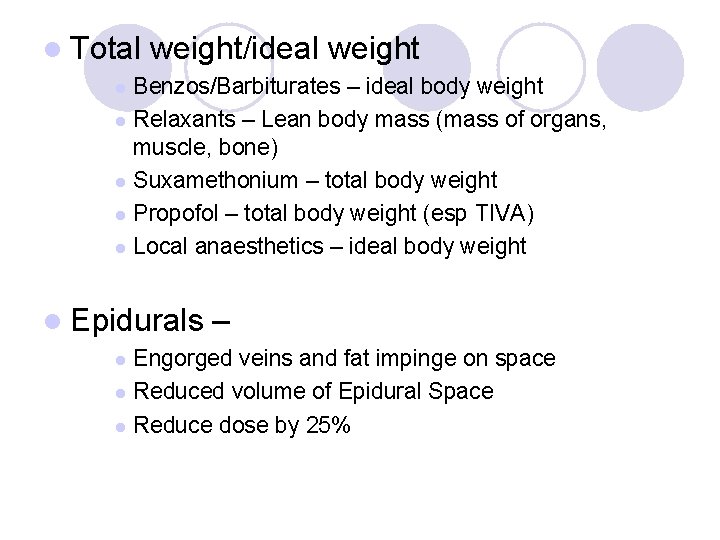
l Total weight/ideal weight Benzos/Barbiturates – ideal body weight l Relaxants – Lean body mass (mass of organs, muscle, bone) l Suxamethonium – total body weight l Propofol – total body weight (esp TIVA) l Local anaesthetics – ideal body weight l l Epidurals – Engorged veins and fat impinge on space l Reduced volume of Epidural Space l Reduce dose by 25% l
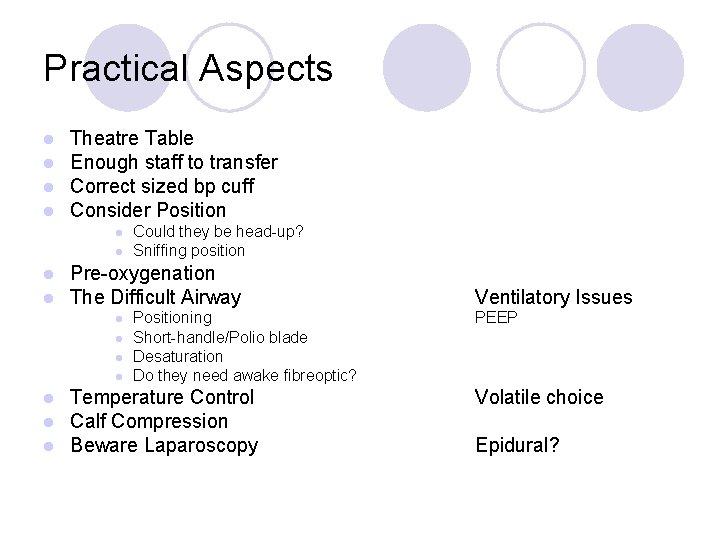
Practical Aspects l l Theatre Table Enough staff to transfer Correct sized bp cuff Consider Position l l Pre-oxygenation The Difficult Airway l l l l Could they be head-up? Sniffing position Positioning Short-handle/Polio blade Desaturation Do they need awake fibreoptic? Temperature Control Calf Compression Beware Laparoscopy Ventilatory Issues PEEP Volatile choice Epidural?
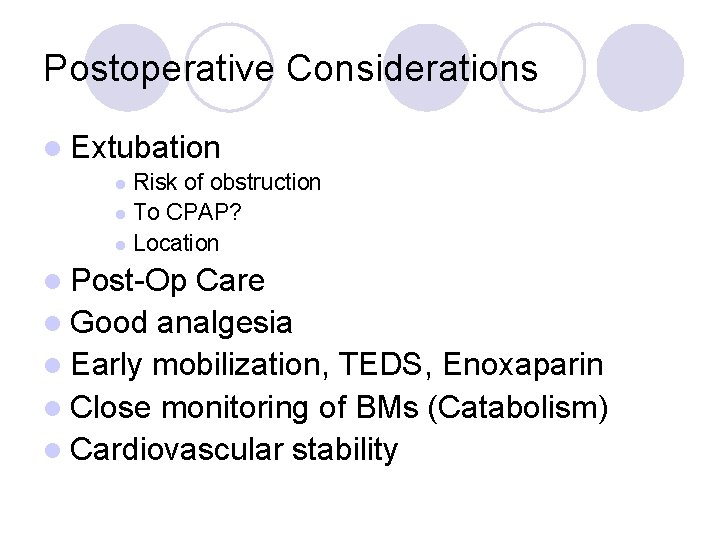
Postoperative Considerations l Extubation Risk of obstruction l To CPAP? l Location l l Post-Op Care l Good analgesia l Early mobilization, TEDS, Enoxaparin l Close monitoring of BMs (Catabolism) l Cardiovascular stability

Any Questions?
- Slides: 22