An overview of Bronchial Asthma by Prof Nadeem
An overview of Bronchial Asthma by Prof Nadeem Rizvi F. R. C. P. U. K Head of Chest Medicine Jinnah Postgraduate Medical Centre Karachi
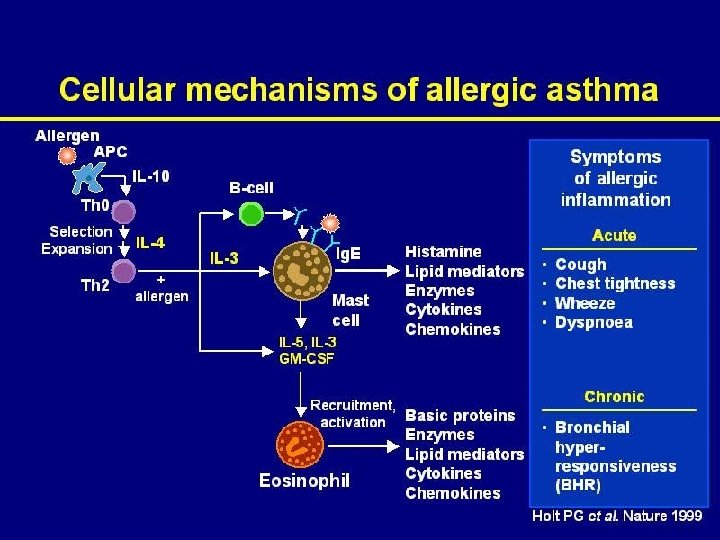
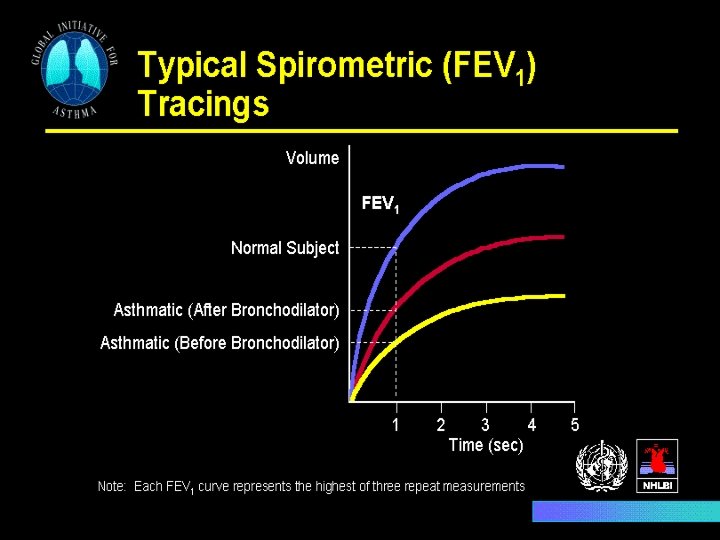
Asthma: Disease State Overview Asthma is a chronic inflammatory disorder of the airways that is characterized, in particular, by the infiltration of activated eosinophils, macrophages, T lymphocytes, and mast cells, resulting in airway hyperresponsiveness and variable and at least partially reversible airflow obstruction.
Magnitude of the Problem • 300 million asthmatics worldwide • Prevalence increasing in most countries by 20% to 50% every 10 years • An estimated 1 million deaths each decade • Significant cause of school/work absence • High healthcare expenditures, especially for emergency services
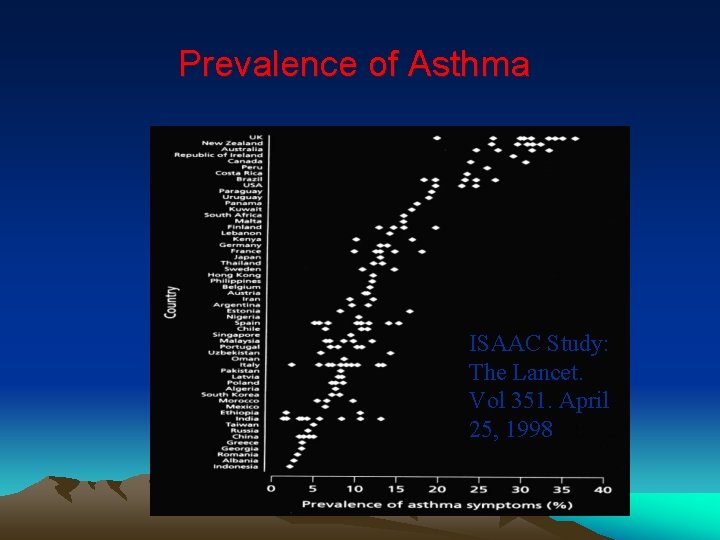
Prevalence of Asthma ISAAC Study: The Lancet. Vol 351. April 25, 1998
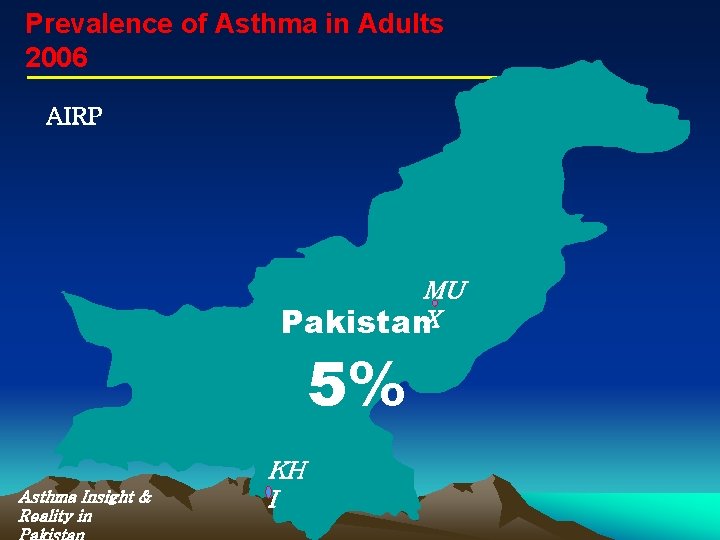
Prevalence of Asthma in Adults 2006 AIRP MU Pakistan. X 5% Asthma Insight & Reality in KH I
Risk factors for Asthma • Asthma occurs in families • Atopy: the strongest identifiable risk factor for the development of asthma • Allergen exposure and chemical sensitizer • Contributing factors may increase susceptibility to development of asthma in predisposed individuals
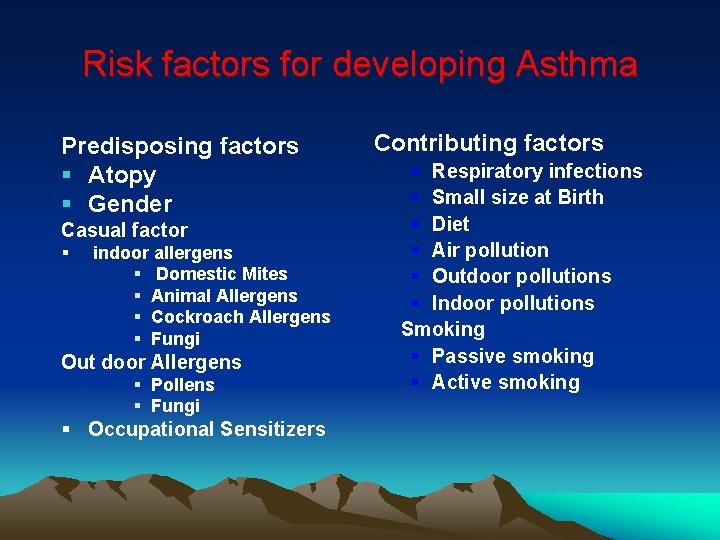
Risk factors for developing Asthma Predisposing factors § Atopy § Gender Casual factor § indoor allergens § Domestic Mites § Animal Allergens § Cockroach Allergens § Fungi Out door Allergens § Pollens § Fungi § Occupational Sensitizers Contributing factors § Respiratory infections § Small size at Birth § Diet § Air pollution § Outdoor pollutions § Indoor pollutions Smoking § Passive smoking § Active smoking
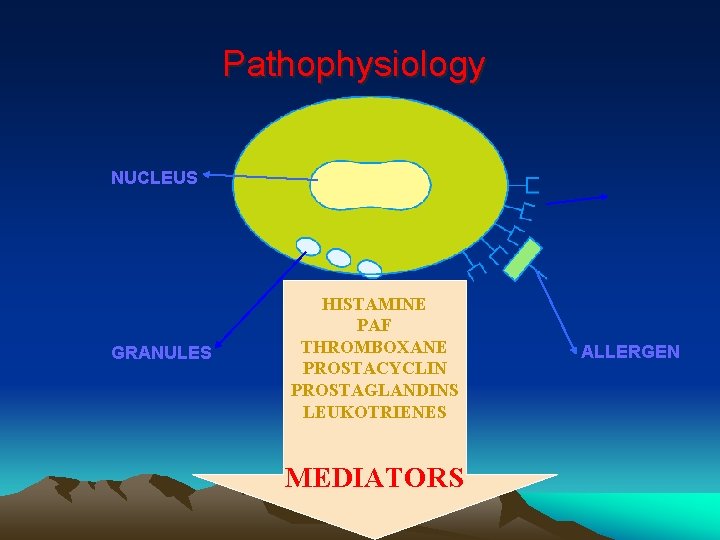
Pathophysiology NUCLEUS GRANULES HISTAMINE PAF THROMBOXANE PROSTACYCLIN PROSTAGLANDINS LEUKOTRIENES MEDIATORS ALLERGEN
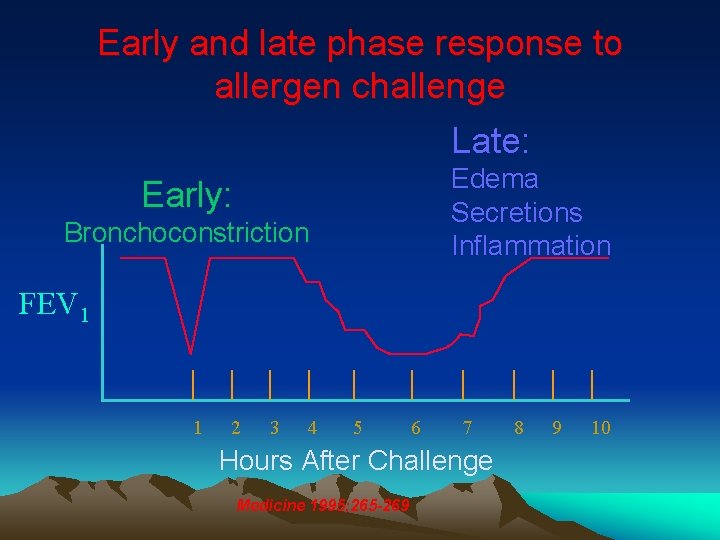
Early and late phase response to allergen challenge Late: Edema Secretions Inflammation Early: Bronchoconstriction FEV 1 1 2 3 4 5 6 7 Hours After Challenge Medicine 1995; 265 -269 8 9 10
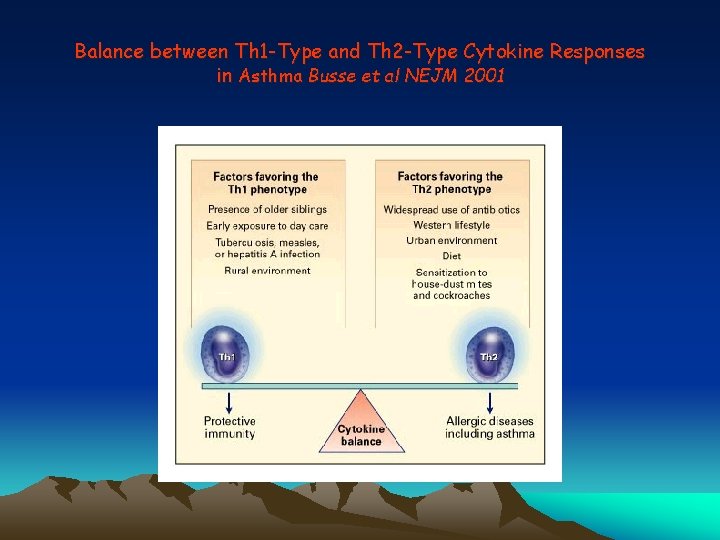
Balance between Th 1 -Type and Th 2 -Type Cytokine Responses in Asthma Busse et al NEJM 2001

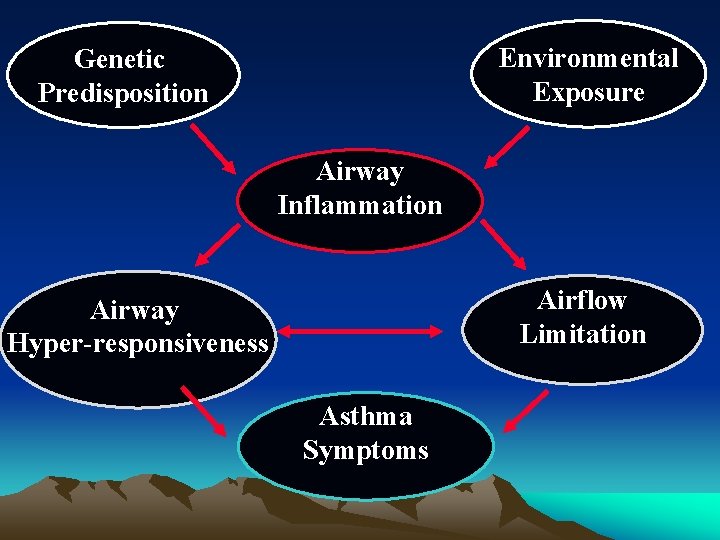
Environmental Exposure Genetic Predisposition Airway Inflammation Airflow Limitation Airway Hyper-responsiveness Asthma Symptoms
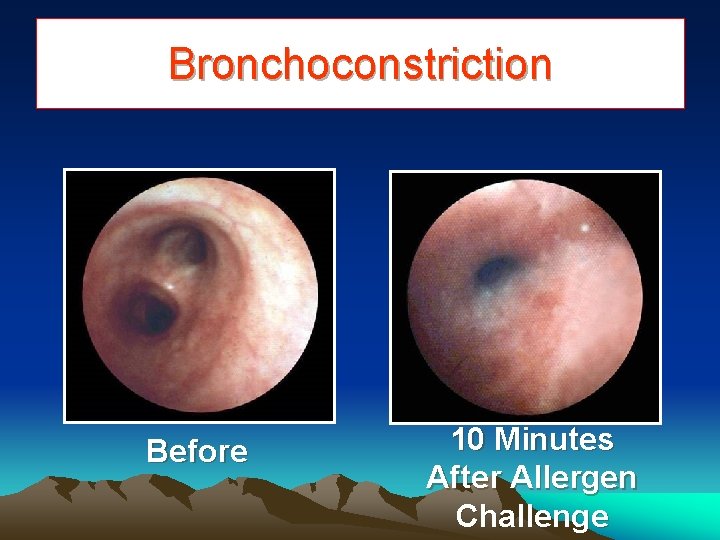
Bronchoconstriction Before 10 Minutes After Allergen Challenge
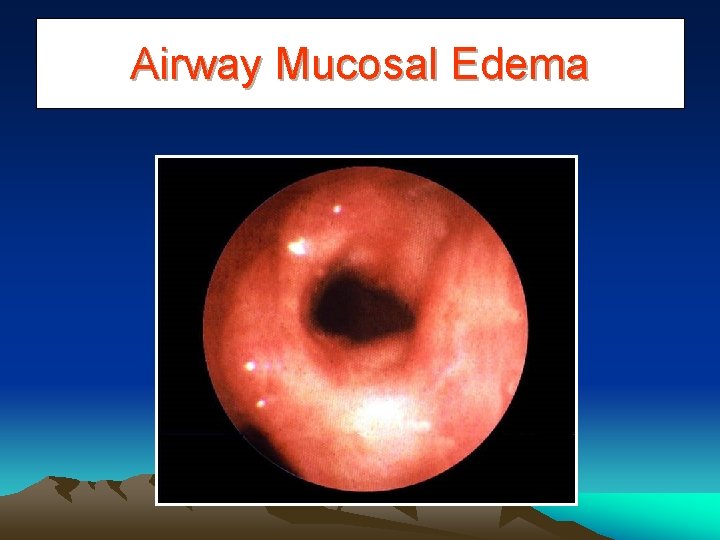
Airway Mucosal Edema
Diagnosis of Asthma “Clinical is Best” • History • Physical examination • Peak flow meter reading (reversibility of 15%)
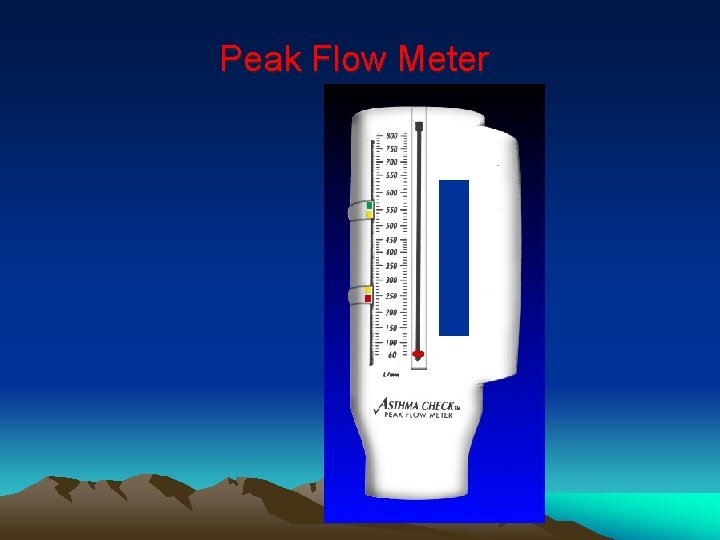
Peak Flow Meter
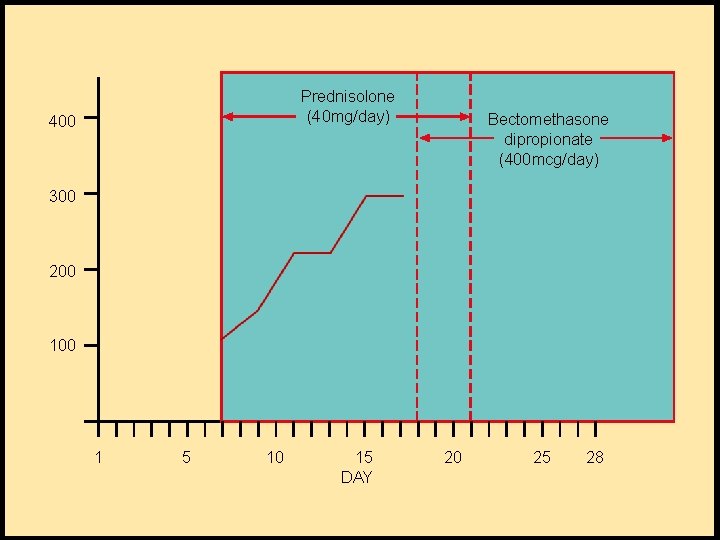
Prednisolone (40 mg/day) 400 Bectomethasone dipropionate (400 mcg/day) 300 200 1 5 10 15 DAY 20 25 28
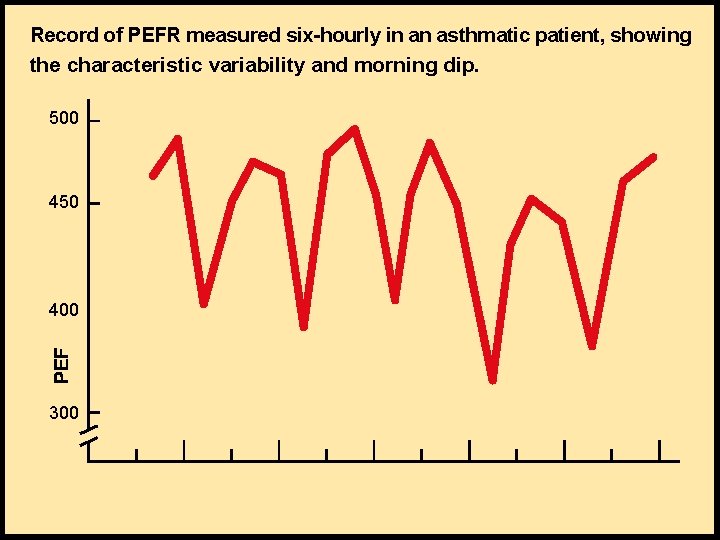
Record of PEFR measured six-hourly in an asthmatic patient, showing the characteristic variability and morning dip. 500 450 400 300
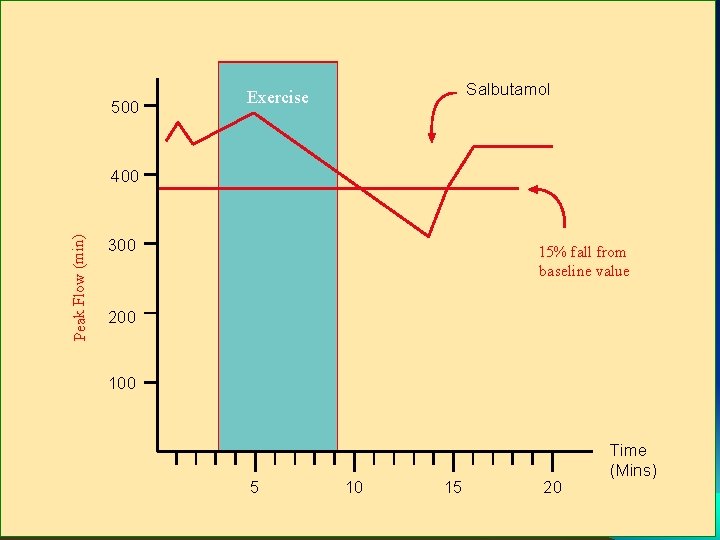
500 Salbutamol Exercise Peak Flow (min) 400 300 15% fall from baseline value 200 100 5 10 15 20 Time (Mins)
Effective Asthma management • Use key indicators to make an accurate, timely diagnosis • Eliminate causal factors • Initiate appropriate therapy • Educate patient and family • Follow up and adjust the treatment plan • Monitor compliance
Gap in Asthma treatment • Patients are not detected – do not seek medical attention – no access to health service – missed diagnosis (bronchitis, LRTI) • Patients do not get treated – they do not want treatment (do not accept diagnosis) – they stop treatment (when they feel well) – health service does not provide treatment
Asthma in the Developing World • Ignorance is rampant • Delivery of health care is not satisfactory • Discrimination is still present • Marriage for girls is often difficult without concealing illness • Schooling and play is often affected
Asthma Medications • Controllers – Medications used on a long-term basis to achieve and maintain control of persistent asthma • Relievers – Medications that act quickly to relieve bronchoconstriction and its accompanying acute symptoms; often referred to as rescue medications
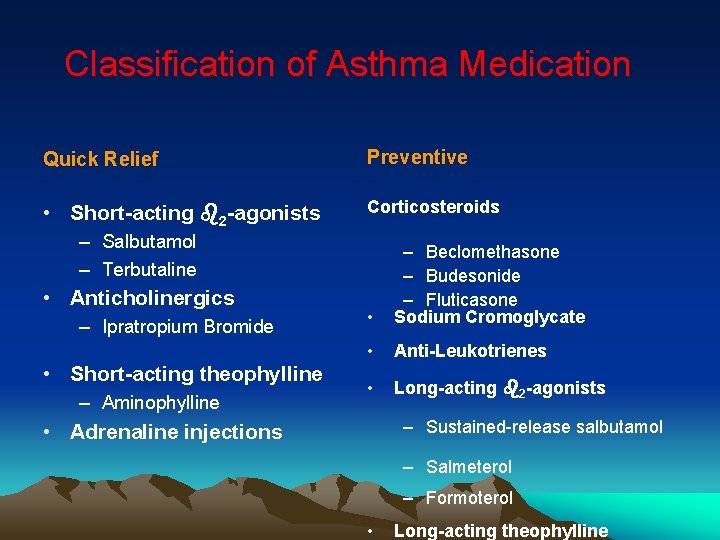
Classification of Asthma Medication Quick Relief Preventive • Short-acting b 2 -agonists Corticosteroids – Salbutamol – Terbutaline • Anticholinergics – Ipratropium Bromide • Short-acting theophylline – Aminophylline • – Beclomethasone – Budesonide – Fluticasone Sodium Cromoglycate • Anti-Leukotrienes • Long-acting b 2 -agonists – Sustained-release salbutamol • Adrenaline injections – Salmeterol – Formoterol • Long-acting theophylline
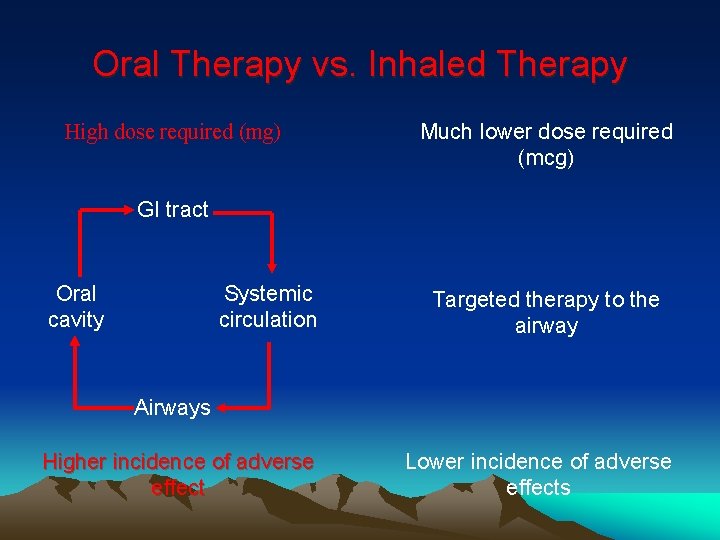
Oral Therapy vs. Inhaled Therapy High dose required (mg) Much lower dose required (mcg) GI tract Oral cavity Systemic circulation Targeted therapy to the airway Airways Higher incidence of adverse effect Lower incidence of adverse effects
‘If a patient uses quick-relief medications every day, or even more than three or four times a week, daily long-term preventive medications should be added to the treatment plan. ’
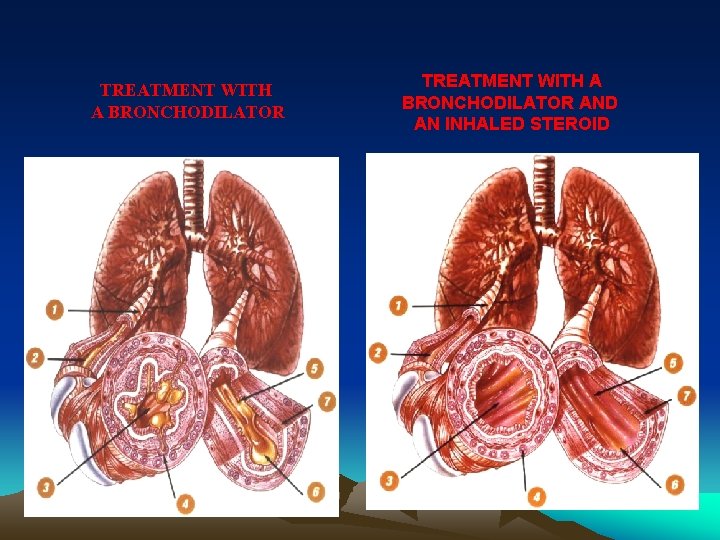
TREATMENT WITH A BRONCHODILATOR AND AN INHALED STEROID
Asthma Management • At present, inhaled glucocorticosteroids are the most effective controller medications and are recommended for persistent asthma at any step of severity • Long-term treatment with inhaled glucocorticosteroids markedly reduces the frequency and severity of exacerbations
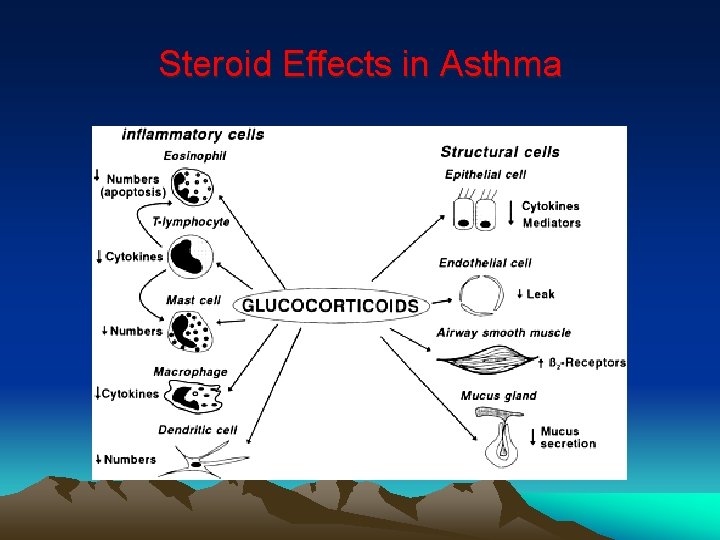
Steroid Effects in Asthma
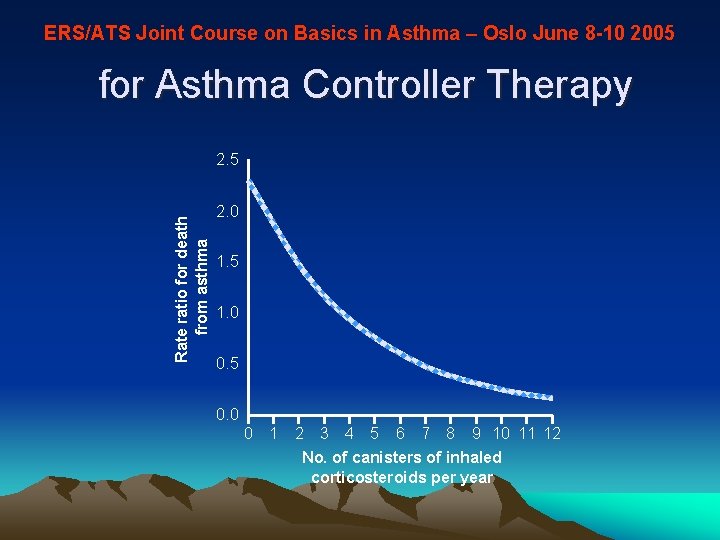
ERS/ATS Joint Course on Basics in Asthma – Oslo June 8 -10 2005 for Asthma Controller Therapy Rate ratio for death from asthma 2. 5 2. 0 1. 5 1. 0 0. 5 0. 0 0 1 2 3 4 5 6 7 8 9 10 11 12 No. of canisters of inhaled corticosteroids per year
Inhaler use in Pakistan
Asthma Management according to Guide lines
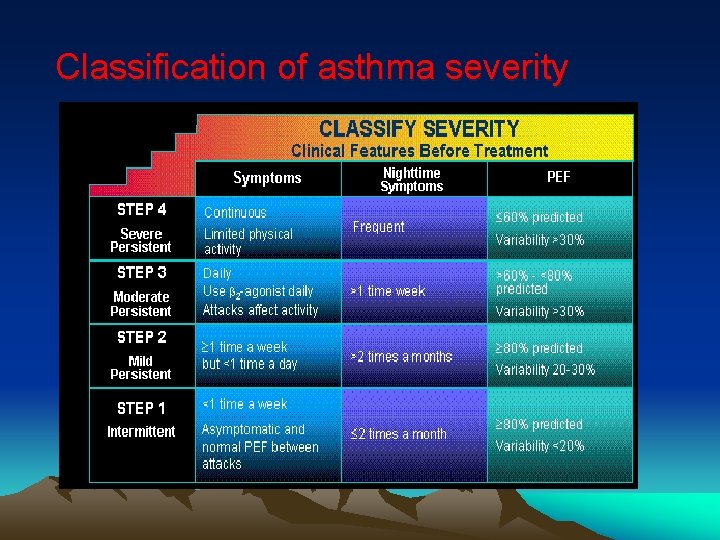
Classification of asthma severity
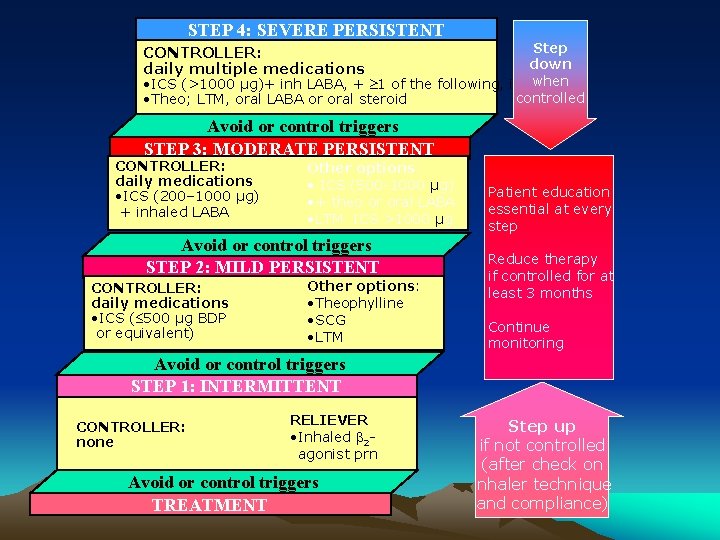
STEP 4: SEVERE PERSISTENT Step CONTROLLER: down daily multiple medications when • ICS (>1000 µg)+ inh LABA, + 1 of the following, if needed: controlled • Theo; LTM, oral LABA or oral steroid Avoid or control triggers STEP 3: MODERATE PERSISTENT CONTROLLER: daily medications • ICS (200– 1000 µg) + inhaled LABA Other options: • ICS (500 -1000 µg) • + theo or oral LABA • LTM ICS >1000 µg Avoid or control triggers STEP 2: MILD PERSISTENT CONTROLLER: daily medications • ICS ( 500 µg BDP or equivalent) Other options: • Theophylline • SCG • LTM Patient education essential at every step Reduce therapy if controlled for at least 3 months Continue monitoring Avoid or control triggers STEP 1: INTERMITTENT CONTROLLER: none RELIEVER • Inhaled 2 agonist prn Avoid or control triggers TREATMENT Step up if not controlled (after check on inhaler technique and compliance)
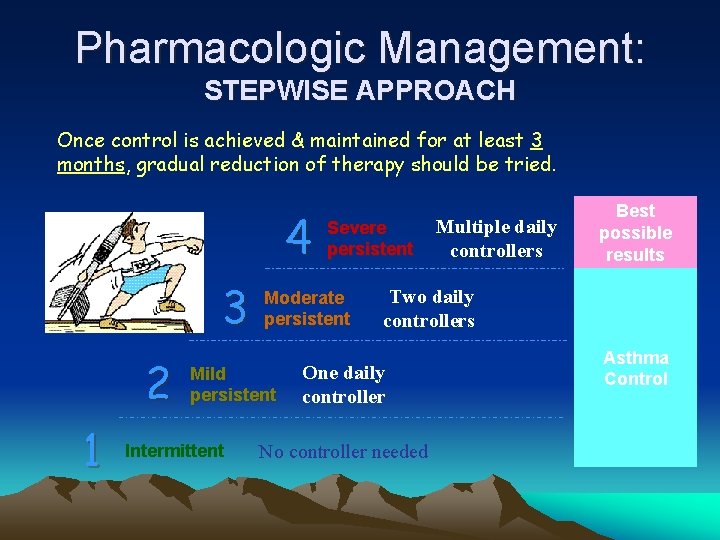
Pharmacologic Management: STEPWISE APPROACH Once control is achieved & maintained for at least 3 months, gradual reduction of therapy should be tried. 4 3 2 1 Moderate persistent Mild persistent Intermittent Severe persistent Multiple daily controllers Best possible results Two daily controllers One daily controller No controller needed Asthma Control
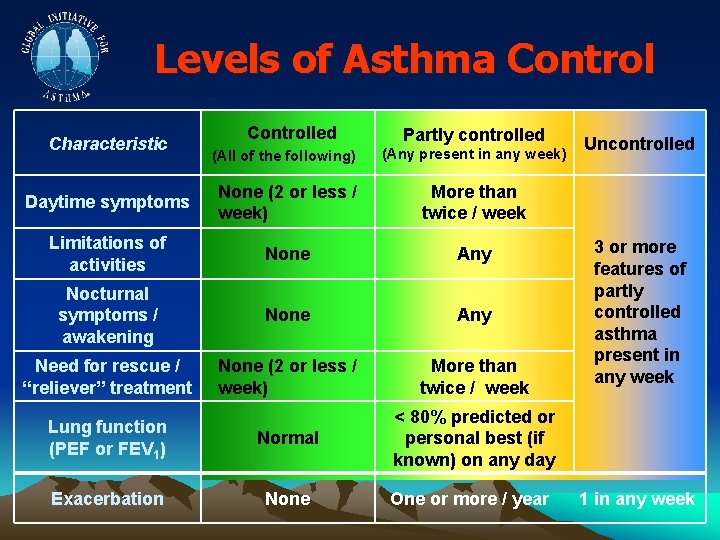
Levels of Asthma Control Characteristic Controlled Partly controlled (All of the following) (Any present in any week) Daytime symptoms None (2 or less / week) More than twice / week Limitations of activities None Any Nocturnal symptoms / awakening None Any Need for rescue / “reliever” treatment None (2 or less / week) More than twice / week Lung function (PEF or FEV 1) Normal < 80% predicted or personal best (if known) on any day Exacerbation None One or more / year Uncontrolled 3 or more features of partly controlled asthma present in any week 1 in any week
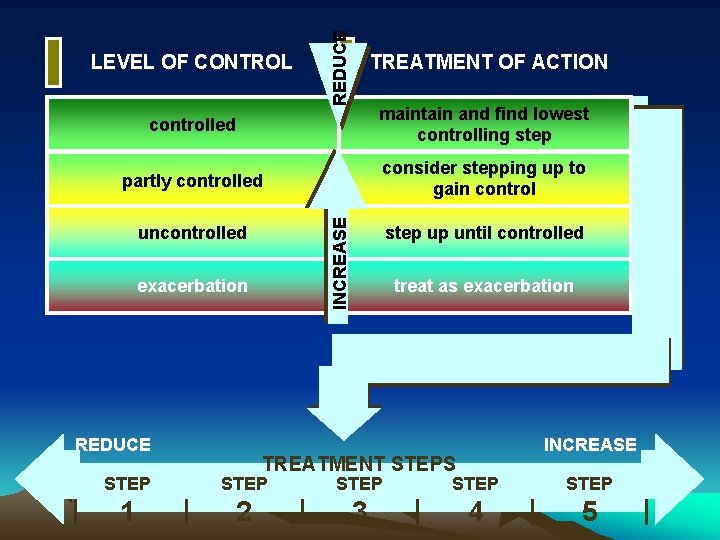
REDUCE LEVEL OF CONTROL TREATMENT OF ACTION maintain and find lowest controlling step partly controlled consider stepping up to gain control INCREASE controlled uncontrolled exacerbation REDUCE step up until controlled treat as exacerbation INCREASE TREATMENT STEPS STEP STEP 1 2 3 4 5
• Asthma is chronic inflammatory disorder • Inhaled steroids is a corner stone of asthma management • Use of peak flow meter is essential, in diagnosing and assessing severity • Management should depend on the level of asthma control • Choice of delivery device should be acceptable and east to use
Teach People to ‘Live with asthma’ TO G IN N S R M A E O L T , P T YM NO S H T I W E LIV

Thank you
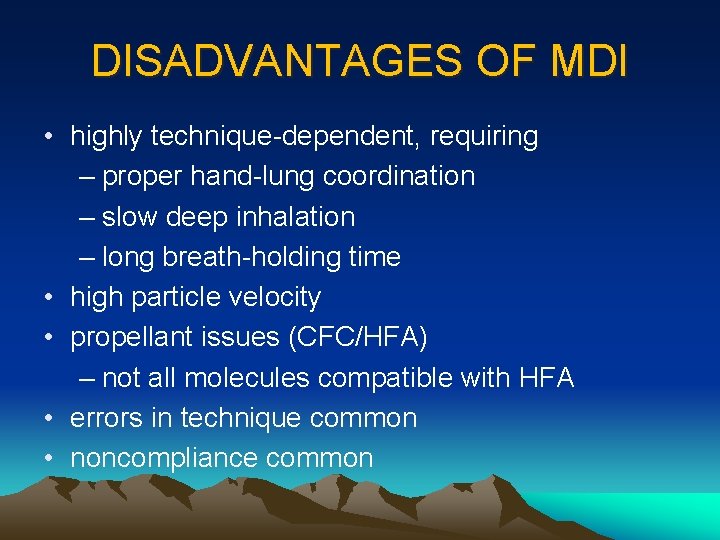
DISADVANTAGES OF MDI • highly technique-dependent, requiring – proper hand-lung coordination – slow deep inhalation – long breath-holding time • high particle velocity • propellant issues (CFC/HFA) – not all molecules compatible with HFA • errors in technique common • noncompliance common
Asthma Management according to Guide lines

Where we are now! (in the U. S. ) Metered-Dose Inhaler Handihaler® Aerolizer™ Twisthaler® Turbuhaler® Autohaler® Spacer Devices Diskus® Small Volume Nebulizer
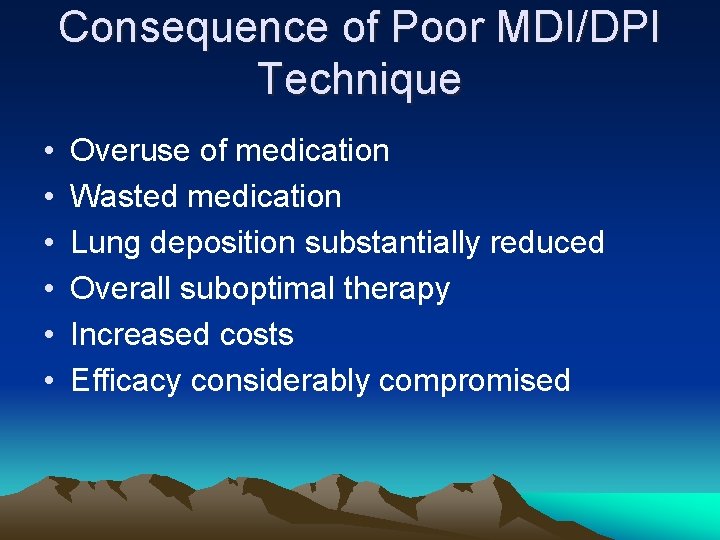
Consequence of Poor MDI/DPI Technique • • • Overuse of medication Wasted medication Lung deposition substantially reduced Overall suboptimal therapy Increased costs Efficacy considerably compromised
- Slides: 46