AN OTS GUIDE TO ASSESSMENT OF VISUAL SENSORY

- Slides: 20
AN OT’S GUIDE TO ASSESSMENT OF VISUAL & SENSORY DEFICITS EXPERIENCED POST CONCUSSION Margaret A. Waskiewicz MS, OTR/L Unit Supervisor Outpatient Occupational Therapy Rusk Rehabilitation, NYU Langone Health
Disclosures Margaret A. Waskiewicz MS, OTR/L has no relevant financial or non-financial interests to disclose. This continuing education activity is managed and accredited by Affinity. CE in cooperation with NABIS. Disclosure will be made when a product is discussed for an unapproved use. Affinity CE staff, NABIS staff, as well as planners and reviewers, have no relevant financial or non-financial interests to disclose. Commercial support was not received for this activity 2
Learning Outcomes At the conclusion of this section, participants will be able to: 1. Define the role of occupational therapy and identify its role in the management of post concussive symptoms, specifically related to visual and sensory changes after concussion. 2. Identify various assessments and techniques used to identify functional visual dysfunction in the post concussive population. 3. Identify basic treatment techniques to apply to both visual and sensory deficits in order to improve functional independence. 3
4 Division Name or Footer FUNCTIONAL VISUAL ASSESSMENT & TREATMENT CONSIDERATIONS
Defining Vision • More than 20/20 • Ability to interpret and understand what we are seeing • “Vision is the sensory system that integrates or enables us to make sense of all of our other sensory systems. Hence it is the unifying system that facilitates learning and optimal function in our current world. ” (Moore, J. 2005)
Role of Occupational Therapy • Graded return to full activity including: Return to Learn Return to Play Return to Work Return to Everyday Function at the Highest Level Possible! • Recommendations to make activities of daily living more productive and with less symptoms • Improve visual skills, hand eye coordination, reading skills
OT Evaluation • Obtain detailed medical history and details of concussion – History of previous concussions? • Symptoms – Experienced at time of concussion vs at evaluation – How are they impacting functional independence? • Functional status: patient/parent report and clinical observation – Focus on details related to difficulties with IADL, work or school related tasks • Basic AROM • Posture • Eye-hand coordination • Vision screen
OT Vision Screen: • Basic Test of Near & Far Acuity • Oculomotor: – NSUCO • Eye Alignment: – Phoria cards – Cover/Uncover Test • Pursuits • Saccades – Ocular ROM (monocular and binocular) • Consider if symptoms are provoked • Binocular: – Convergence/Divergence – Stereopsis – Worth 4 Dot • Consider if symptoms are provoked • Visual Fields • Accommodation
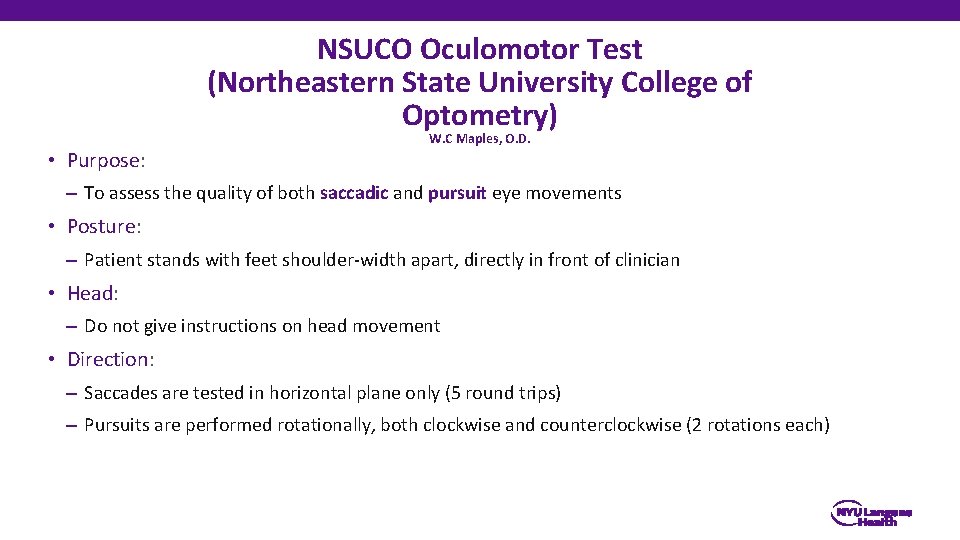
NSUCO Oculomotor Test (Northeastern State University College of Optometry) • Purpose: W. C Maples, O. D. – To assess the quality of both saccadic and pursuit eye movements • Posture: – Patient stands with feet shoulder-width apart, directly in front of clinician • Head: – Do not give instructions on head movement • Direction: – Saccades are tested in horizontal plane only (5 round trips) – Pursuits are performed rotationally, both clockwise and counterclockwise (2 rotations each)
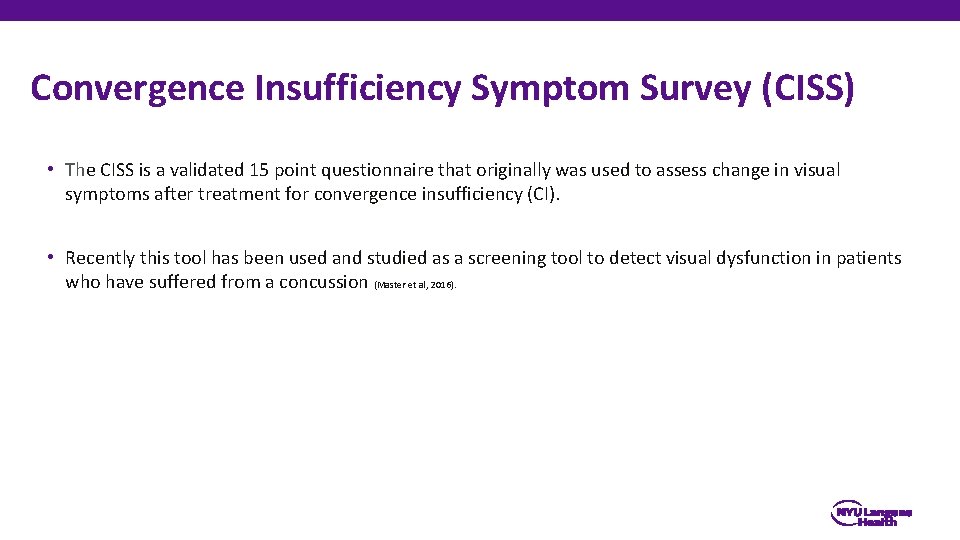
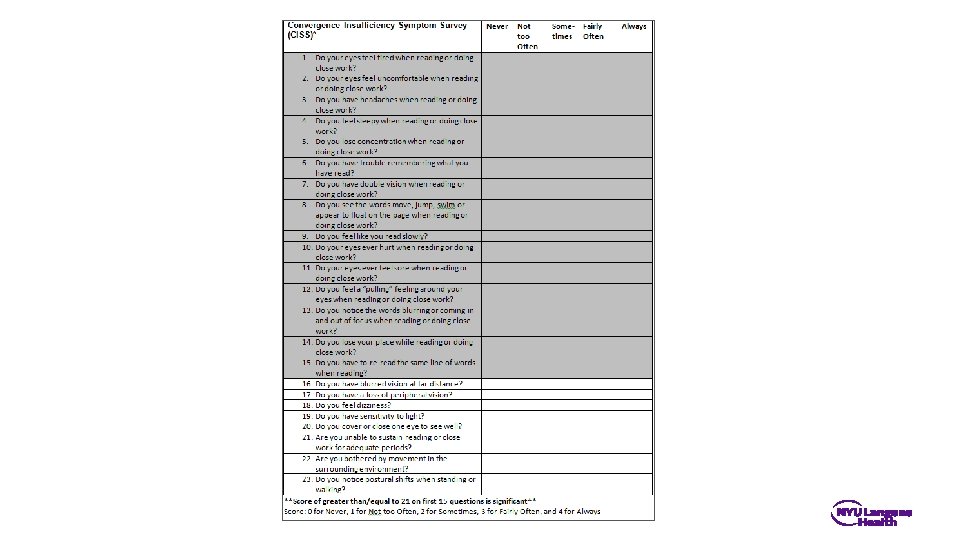
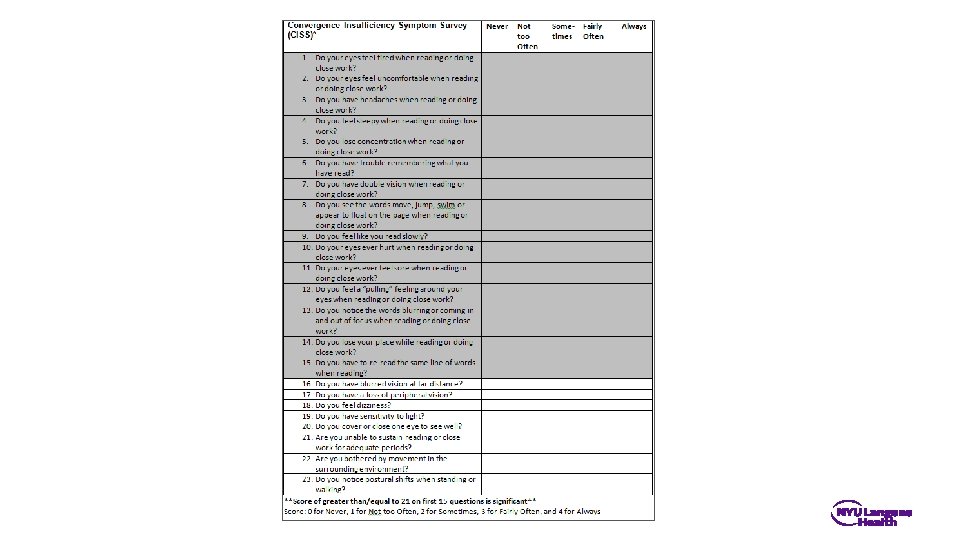
Convergence Insufficiency Symptom Survey (CISS) • The CISS is a validated 15 point questionnaire that originally was used to assess change in visual symptoms after treatment for convergence insufficiency (CI). • Recently this tool has been used and studied as a screening tool to detect visual dysfunction in patients who have suffered from a concussion (Master et al, 2016).

12 Division Name or Footer TRANSLATION TO FUNCTION & TREATMENT
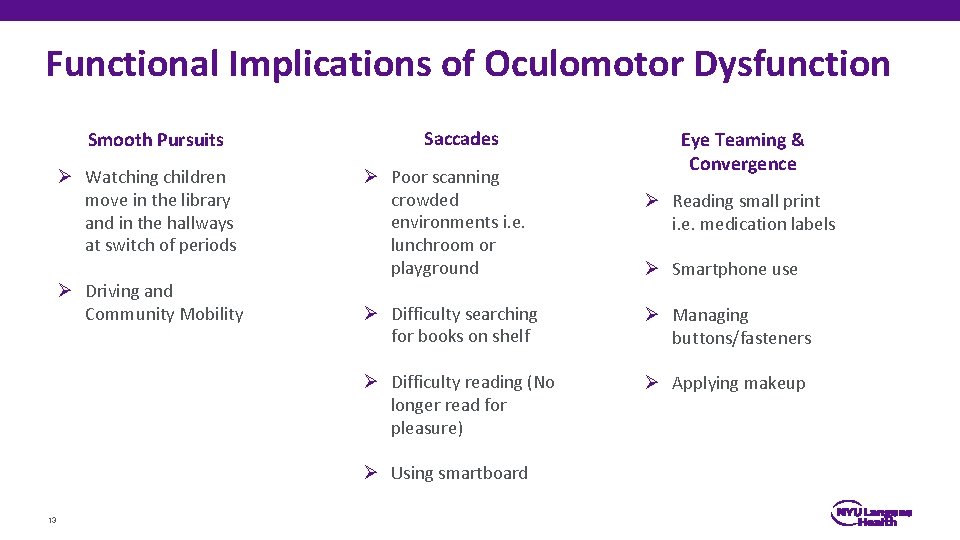
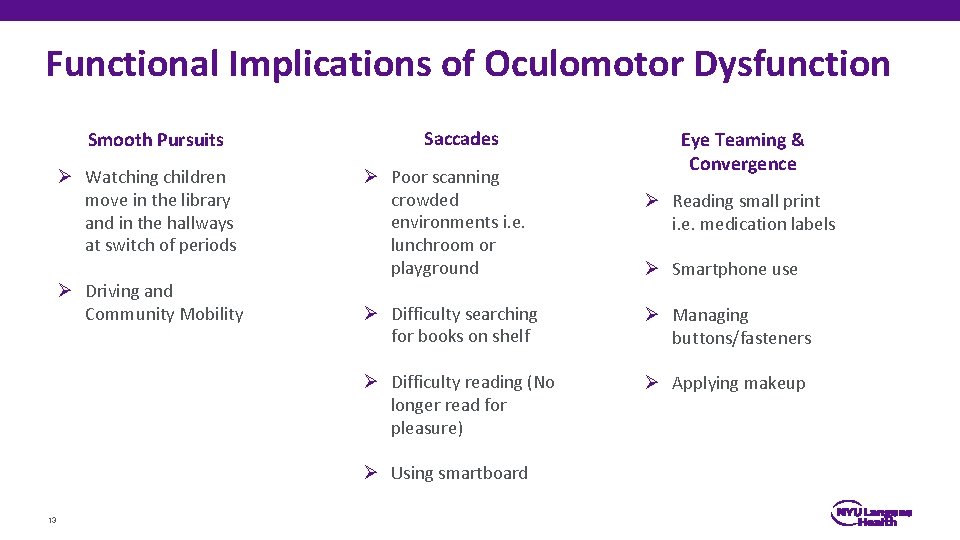
Functional Implications of Oculomotor Dysfunction Smooth Pursuits Ø Watching children move in the library and in the hallways at switch of periods Ø Driving and Community Mobility Saccades Ø Poor scanning crowded environments i. e. lunchroom or playground Ø Reading small print i. e. medication labels Ø Smartphone use Ø Difficulty searching for books on shelf Ø Managing buttons/fasteners Ø Difficulty reading (No longer read for pleasure) Ø Applying makeup Ø Using smartboard 13 Eye Teaming & Convergence
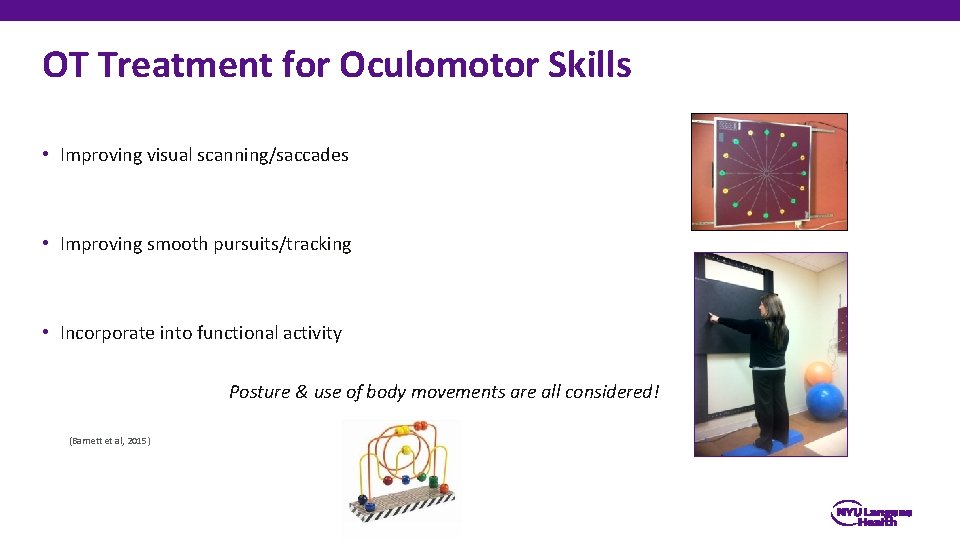
OT Treatment for Oculomotor Skills • Improving visual scanning/saccades • Improving smooth pursuits/tracking • Incorporate into functional activity Posture & use of body movements are all considered! (Barnett et al, 2015)
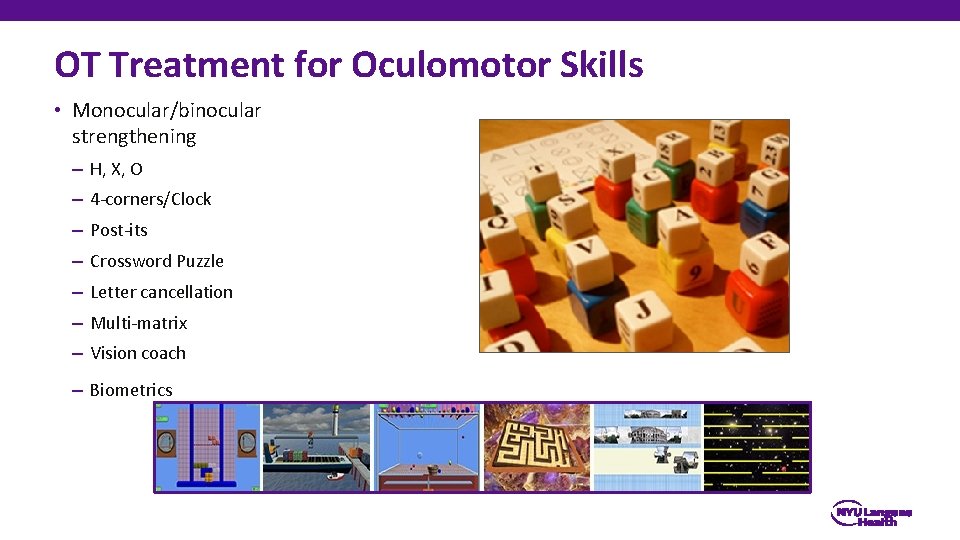
OT Treatment for Oculomotor Skills • Monocular/binocular strengthening – H, X, O – 4 -corners/Clock – Post-its – Crossword Puzzle – Letter cancellation – Multi-matrix – Vision coach – Biometrics
Smooth Pursuits • In order to be functional, patient should be: – Able to track a moving target of varying speeds – Able to disassociate head and eye movement – Symptom free – Smooth in all directions, close and far – Remain smooth and symptom free with: • varying degrees of balance challenges • during functional mobility • in complex, stimulating environments
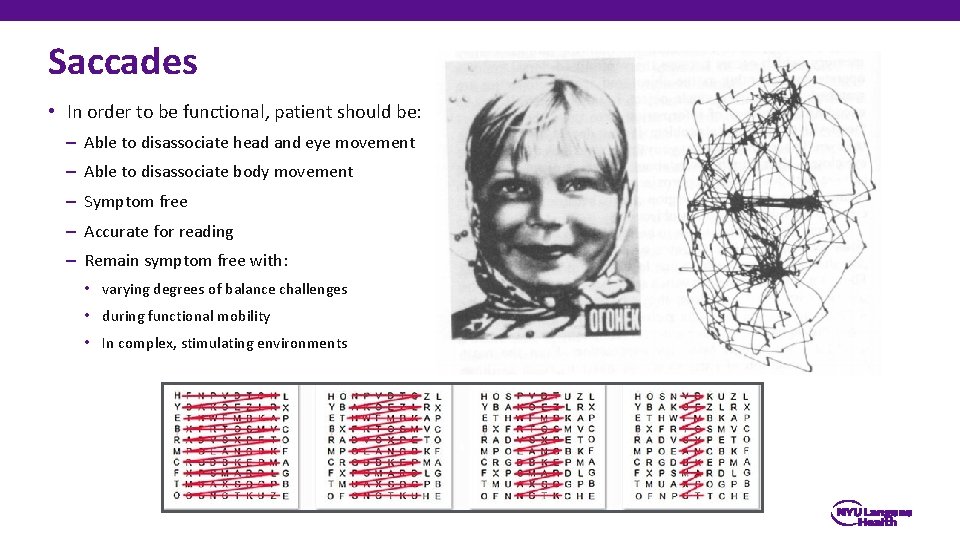
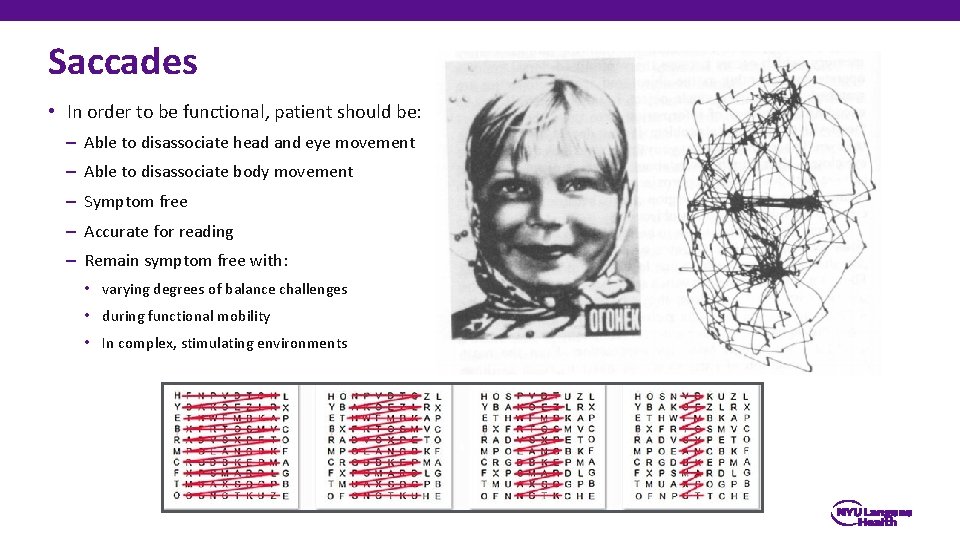
Saccades • In order to be functional, patient should be: – Able to disassociate head and eye movement – Able to disassociate body movement – Symptom free – Accurate for reading – Remain symptom free with: • varying degrees of balance challenges • during functional mobility • In complex, stimulating environments
Convergence & Binocular Vision • In order to be functional, eye movements should be: – Automatic and effortless – Stable with head movement, different body positions and in complex environments – Able to switch from near<->far without difficulty – Both eyes should work equally or close to equally
Compensatory Strategies • Mindfulness • Sleep Hygiene • Computer & Device Modifications • Workstation Modifications • Palming • Energy Conservation/Rest Breaks • 20: 20 Rule 19
References • Brahm KD, Wilgenburg HM, Kirby J, Ingalla S, Chang C & Goodrich GL. Visual impairment and dysfunction in combat-injured servicemembers with traumatic brain injury. Optom Vis Sci 2009; 86: 817– 825. • Bonfield, C. M. , Lam, S. , Lin, Y. , & Greene, S. (2013). The impact of attention deficit hyperactivity disorder on recovery from mild traumatic brain injury: Clinical article. Journal of Neurosurgery: Pediatrics, 12(2), 97 -102. • Brown, N. J. , Mannix, R. C. , O’Brien, M. J. , Gostine, D. , Collins, M. W. , & Meehan, W. P. (2014). Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics, 133(2), e 299 -e 304. • Cubon, V. A. , Putukian, M. , Boyer, C. , & Dettwiler, A. (2011). A diffusion tensor imaging study on the white matter skeleton in individuals with sports-related concussion. Journal of neurotrauma, 28(2), 189 -201. • Eisenberg, M. A. , Andrea, J. , Meehan, W. , & Mannix, R. (2013). Time interval between concussions and symptom duration. Pediatrics, 132(1), 8 -17. • Gallaway, M. , Scheiman, M. , and Mitchell, L. (2017). Vision therapy for Post-concussion vision disorders. Optometry and Vision Science. 94: 1 • Goodrich, G. L. , Kirby, J. , Cockerham, G. , Ingalla, S. P. , & Lew, H. L. (2007). Visual function in patients of a polytrauma rehabilitation center: A descriptive study. Journal of Rehabilitation Research & Development, 44(7). • Kinnaman, K. A. , Mannix, R. C. , Dawn Comstock, R. , & Meehan, W. P. (2013). Management strategies and medication use for treating paediatric patients with concussions. Acta Paediatrica, 102(9), e 424 -e 428. • Leddy, J. J. , Baker, J. G. , Kozlowski, K. , Bisson, L. , & Willer, B. (2011). Reliability of a graded exercise test for assessing recovery from concussion. Clinical Journal of Sport Medicine, 21(2), 89 -94. • Master, C. , Scheiman, M. , Gallaway, M. , Goodman, A. , Robinson, R. , Master, S and Grady, M. (2016). Vision Diagnoses Are Common After Concussion in Adolescents. Clinical Pediatrics, 55(3) 260 -267. • Mc. Crory P, Meeuwisse WH, Aubry M, et al, Br J Sports Med 2013; 47: 250 -258. Consensus Statement on concussion in sport: the 4 th International Conference on Concussion in Sport held in Zurich, November 2012 • Mc. Crory, P. , Meeuwisse, W. H. , Aubry, M. , Cantu, B. , Dvořák, J. , Echemendia, R. J. , . . . & Turner, M. (2013). Consensus statement on concussion in sport: the 4 th International Conference on Concussion in Sport held in Zurich, November 2012. British Journal of Sports Medicine, 47(5), 250 -258. • Poltavski, D. V. , & Biberdorf, D. (2014). Screening for lifetime concussion in athletes: Importance of oculomotor measures. Brain Injury, (0), 1 -11. • Sigurdardottir, S. , Andelic, N. , Roe, C. , Jerstad, T. , & Schanke, A. K. (2009). Post-concussion symptoms after traumatic brain injury at 3 and 12 months post-injury: a prospective study. Brain Injury, 23(6), 489497.