An Introduction to Tissues Tissues Structures with discrete
- Slides: 47
An Introduction to Tissues • Tissues – Structures with discrete structural and functional properties – Tissues in combination form organs, such as the heart or liver – Organs can be grouped into 11 organ systems
4 -1 Four Types of Tissue • Tissue – Are collections of cells and cell products that perform specific, limited functions – Four types of tissue 1. Epithelial tissue 2. Connective tissue 3. Muscle tissue 4. Neural tissue
4 -1 Four Types of Tissue • Epithelial Tissue – Covers exposed surfaces – Lines internal passageways – Forms glands • Connective Tissue – Fills internal spaces – Supports other tissues – Transports materials – Stores energy
4 -1 Four Types of Tissue • Muscle Tissue – Specialized for contraction – Skeletal muscle, heart muscle, and walls of hollow organs • Neural Tissue – Carries electrical signals from one part of the body to another
4 -2 Epithelial Tissue • Epithelia – Layers of cells covering internal or external surfaces • Glands – Structures that produce secretions
4 -2 Epithelial Tissue • Characteristics of Epithelia – Form cell junctions – Polarity (apical and basal surfaces) – Attachment (basement membrane or basal lamina) – Avascularity – Regeneration
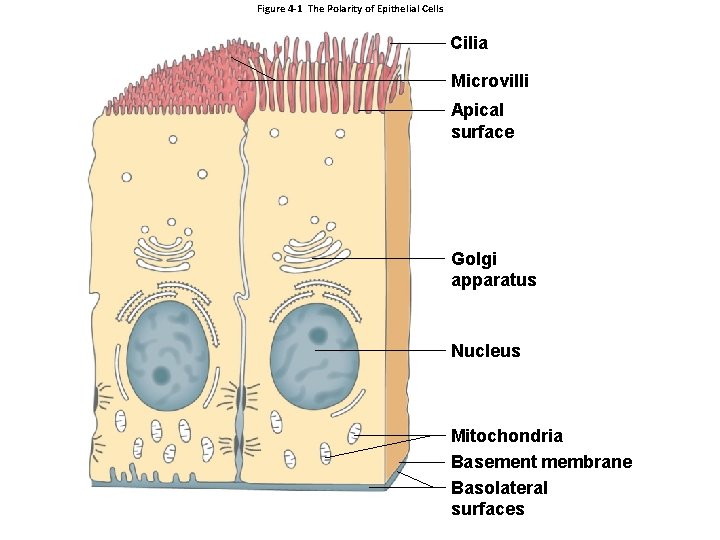
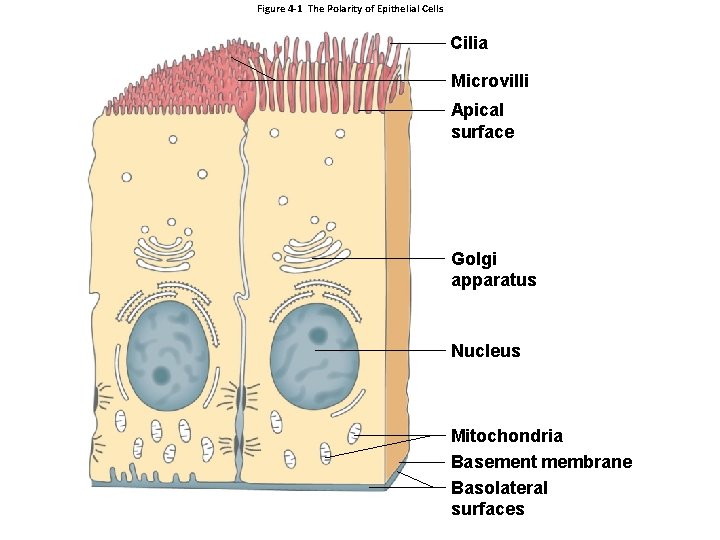
Figure 4 -1 The Polarity of Epithelial Cells Cilia Microvilli Apical surface Golgi apparatus Nucleus Mitochondria Basement membrane Basolateral surfaces
4 -2 Epithelial Tissue • Functions of Epithelial Tissue 1. Provide Physical Protection 2. Control Permeability 3. Provide Sensation 4. Produce Specialized Secretions (glandular epithelium)
4 -2 Epithelial Tissue • Specializations of Epithelial Cells 1. Move fluids over the epithelium 2. Move fluids through the epithelium (permeability) 3. Produce secretions (protection and messengers) • Polarity 1. Apical surfaces • Microvilli increase absorption or secretion • Cilia (ciliated epithelium) move fluid 2. Basolateral surfaces
4 -2 Epithelial Tissue • Maintaining the Integrity of Epithelia 1. Intercellular connections 2. Attachment to the basement membrane 3. Epithelial maintenance and repair
4 -2 Epithelial Tissue • Intercellular Connections – Support and communication • CAMs (cell adhesion molecules) • Intercellular cement
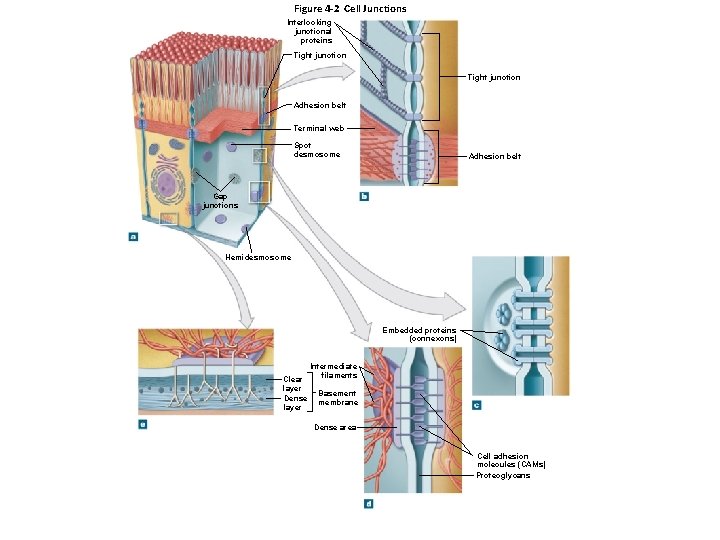
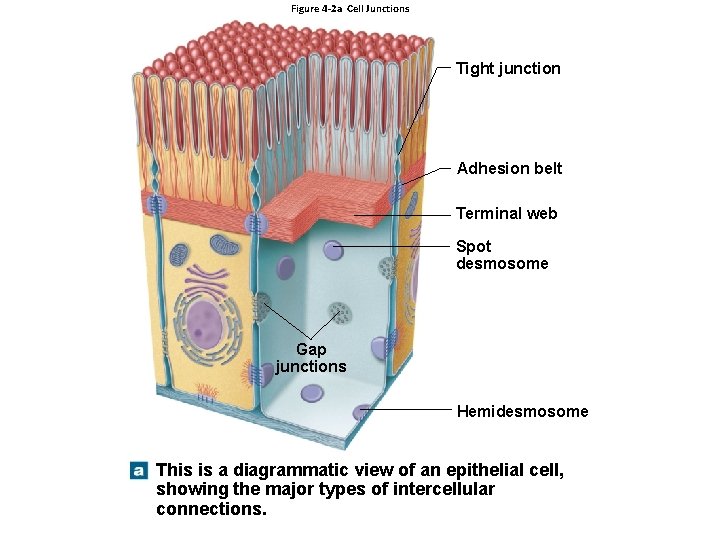
4 -2 Epithelial Tissue • Intercellular Connections – Cell junctions • Form bonds with other cells or extracellular material 1. Tight junctions 2. Gap junctions 3. Desmosomes
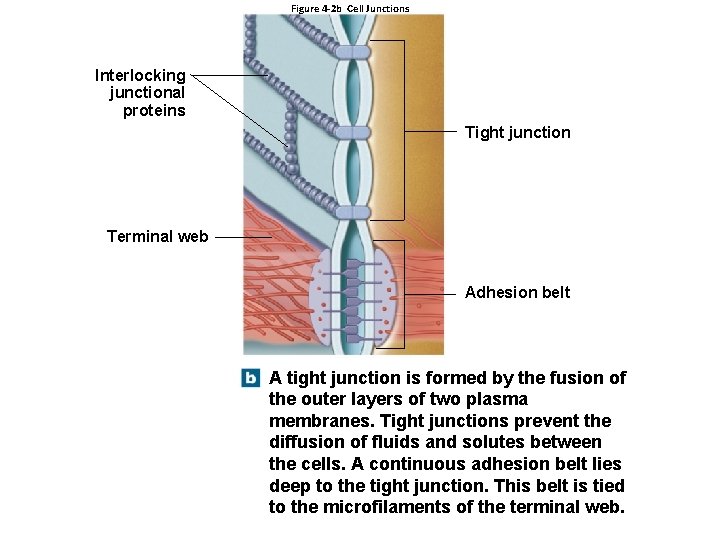
4 -2 Epithelial Tissue • Tight Junctions – Between two plasma membranes – Prevents passage of water and solutes – Isolates wastes in the lumen
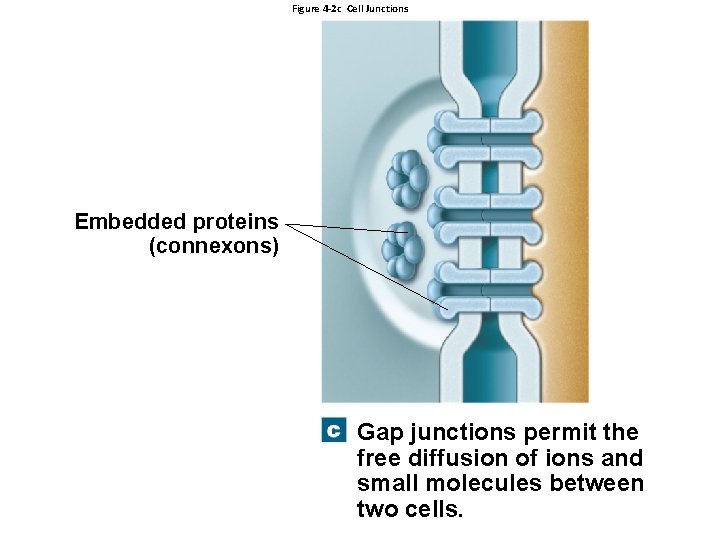
4 -2 Epithelial Tissue • Gap Junctions – Allow rapid communication – Are held together by special channel proteins – Allow ions to pass • Coordinate contractions in heart muscle
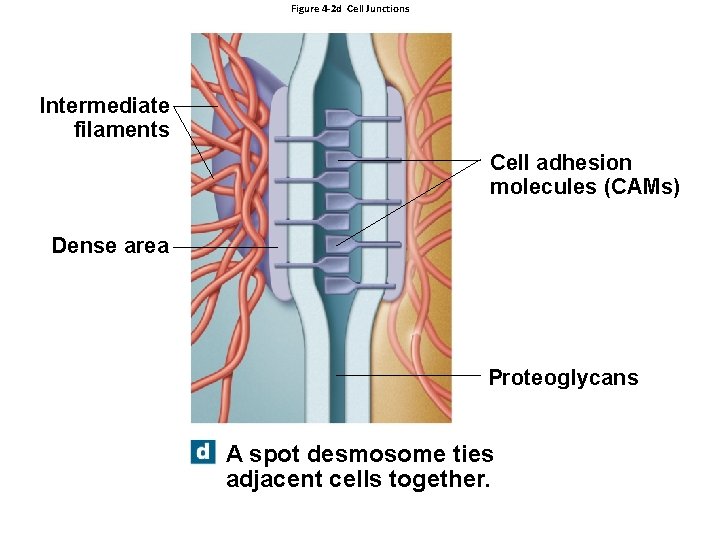
4 -2 Epithelial Tissue • Desmosomes – CAMs, dense areas, and intercellular cement – Spot desmosomes • Tie cells together • Allow bending and twisting
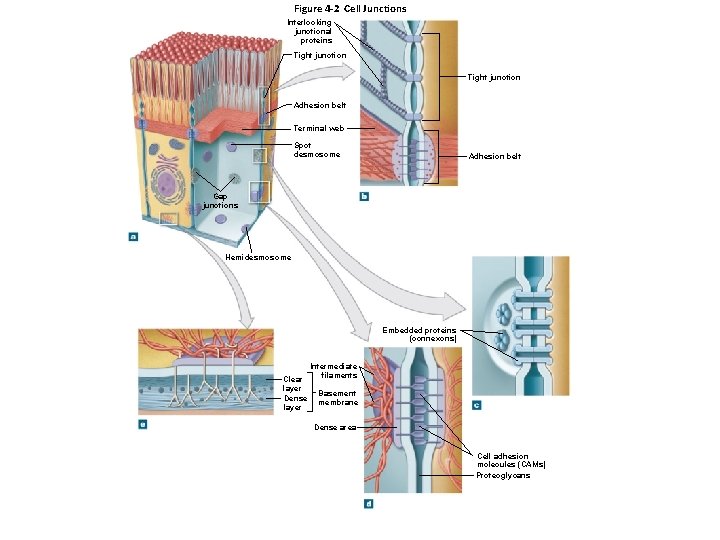
Figure 4 -2 Cell Junctions Interlocking junctional proteins Tight junction Adhesion belt Terminal web Spot desmosome Adhesion belt Gap junctions Hemidesmosome Embedded proteins (connexons) Clear layer Dense layer Intermediate filaments Basement membrane Dense area Cell adhesion molecules (CAMs) Proteoglycans
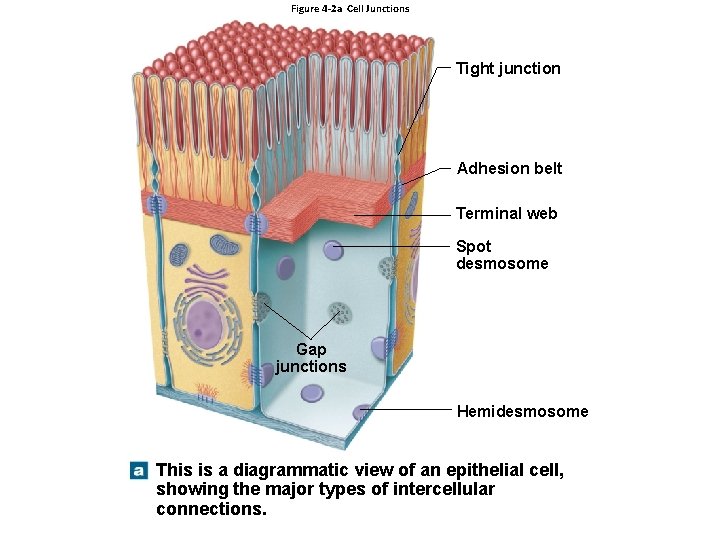
Figure 4 -2 a Cell Junctions Tight junction Adhesion belt Terminal web Spot desmosome Gap junctions Hemidesmosome This is a diagrammatic view of an epithelial cell, showing the major types of intercellular connections.
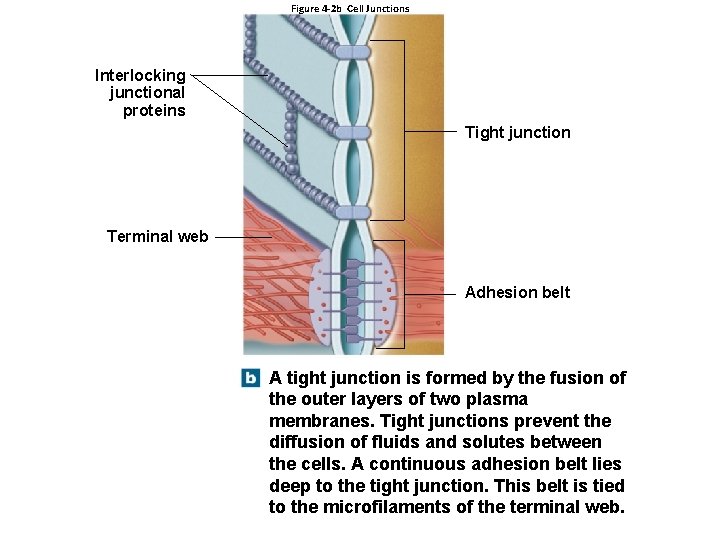
Figure 4 -2 b Cell Junctions Interlocking junctional proteins Tight junction Terminal web Adhesion belt A tight junction is formed by the fusion of the outer layers of two plasma membranes. Tight junctions prevent the diffusion of fluids and solutes between the cells. A continuous adhesion belt lies deep to the tight junction. This belt is tied to the microfilaments of the terminal web.
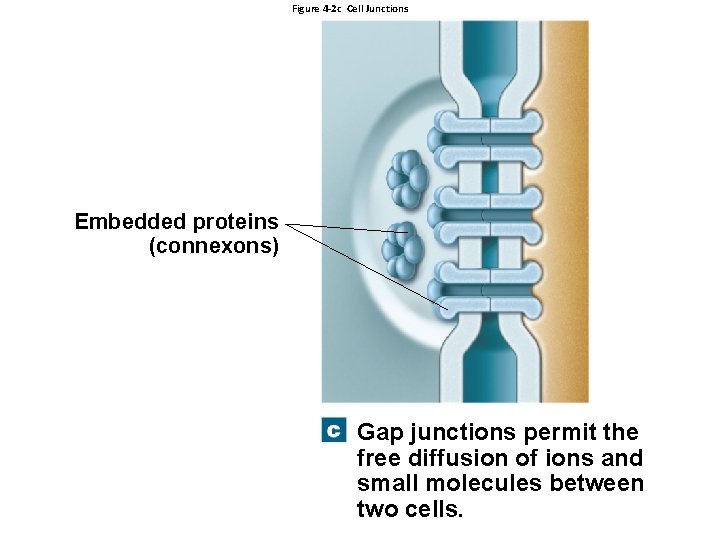
Figure 4 -2 c Cell Junctions Embedded proteins (connexons) Gap junctions permit the free diffusion of ions and small molecules between two cells.
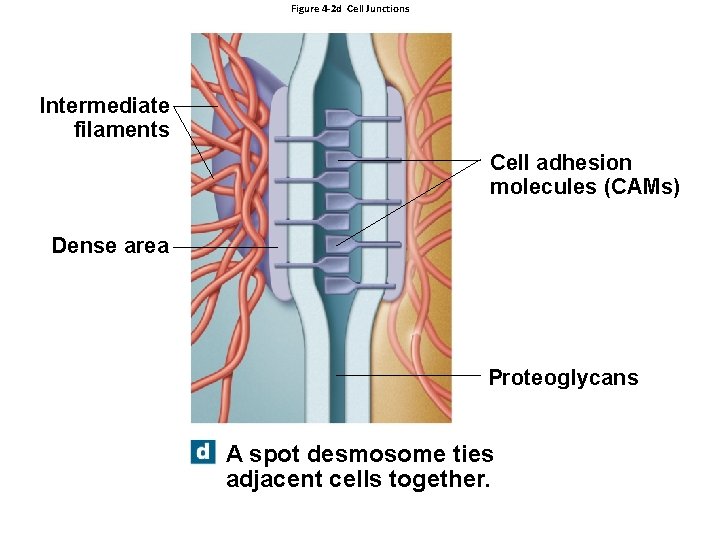
Figure 4 -2 d Cell Junctions Intermediate filaments Cell adhesion molecules (CAMs) Dense area Proteoglycans A spot desmosome ties adjacent cells together.
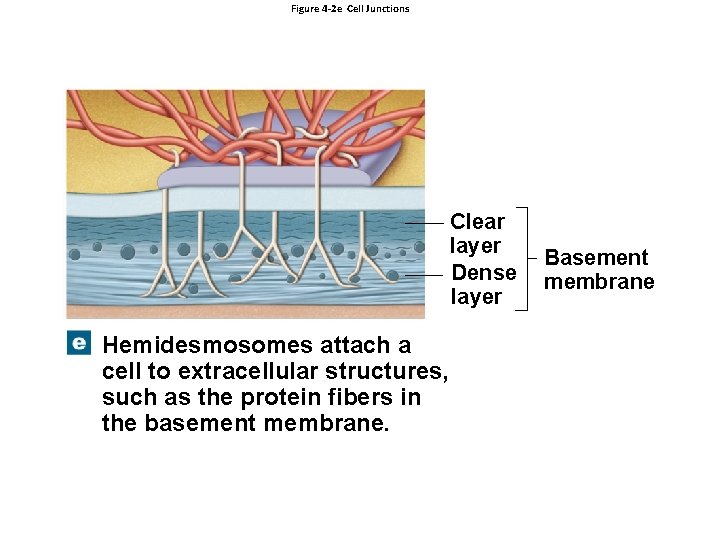
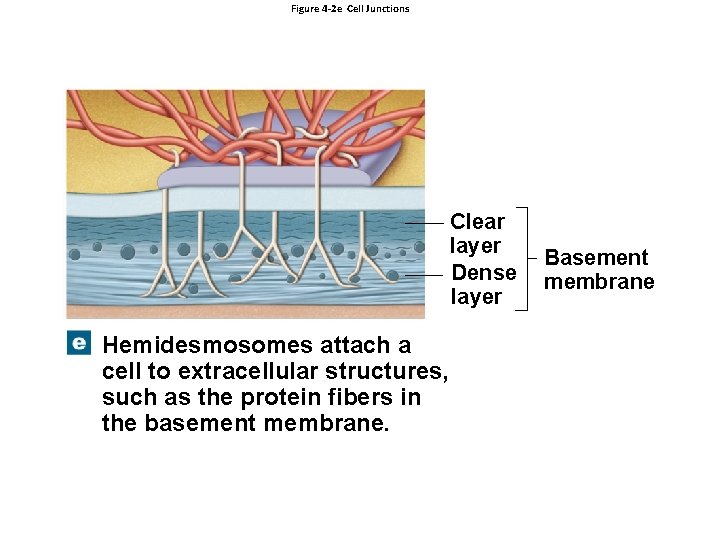
Figure 4 -2 e Cell Junctions Clear layer Dense layer Hemidesmosomes attach a cell to extracellular structures, such as the protein fibers in the basement membrane. Basement membrane
4 -2 Epithelial Tissue • Epithelial Maintenance and Repair – Epithelia are replaced by division of germinative cells (stem cells) – Near basement membrane
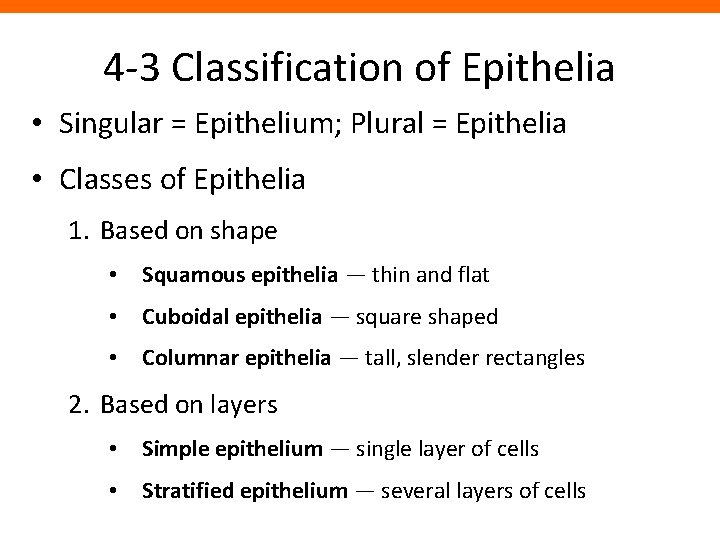
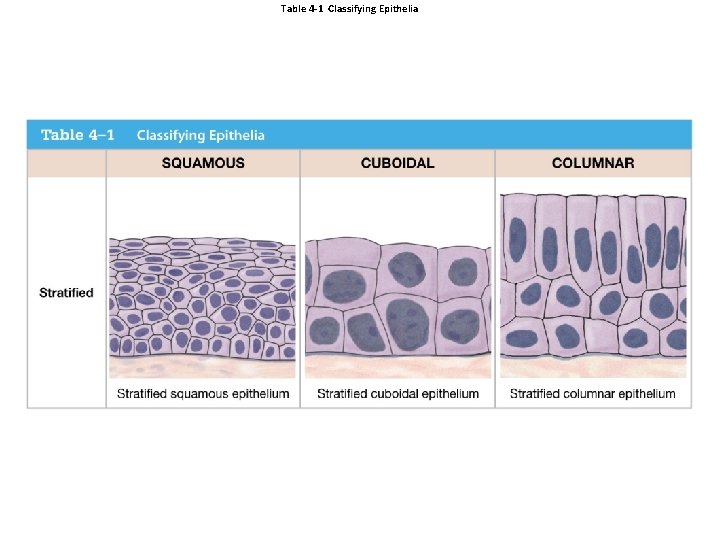
4 -3 Classification of Epithelia • Singular = Epithelium; Plural = Epithelia • Classes of Epithelia 1. Based on shape • Squamous epithelia — thin and flat • Cuboidal epithelia — square shaped • Columnar epithelia — tall, slender rectangles 2. Based on layers • Simple epithelium — single layer of cells • Stratified epithelium — several layers of cells
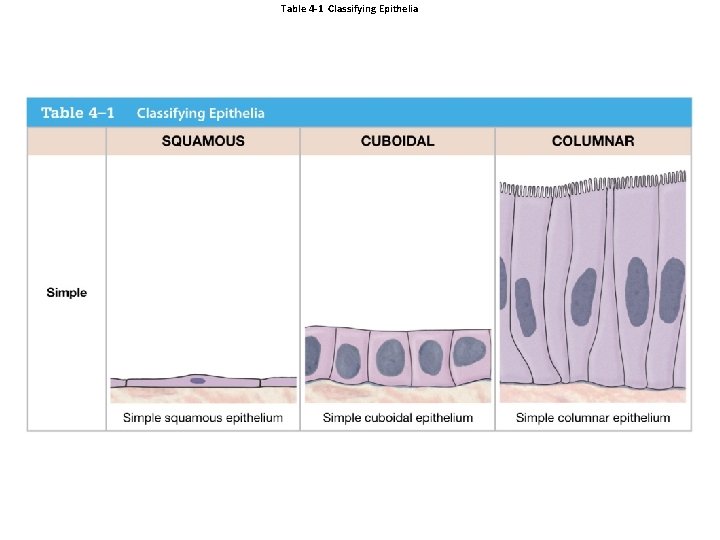
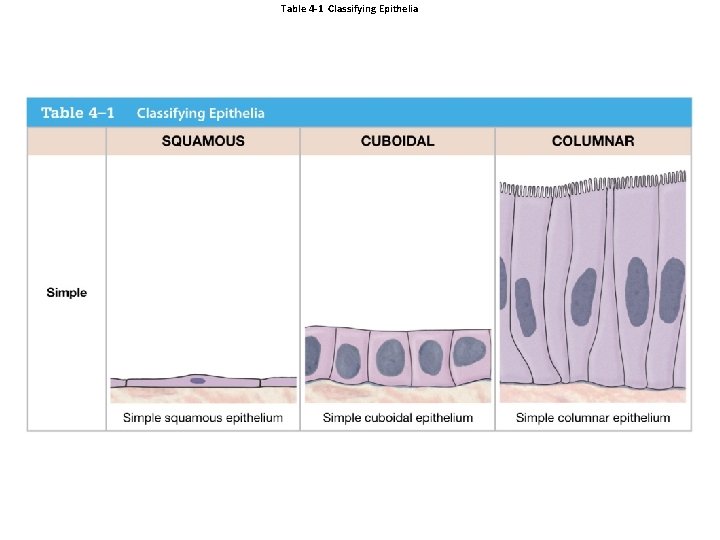
Table 4 -1 Classifying Epithelia
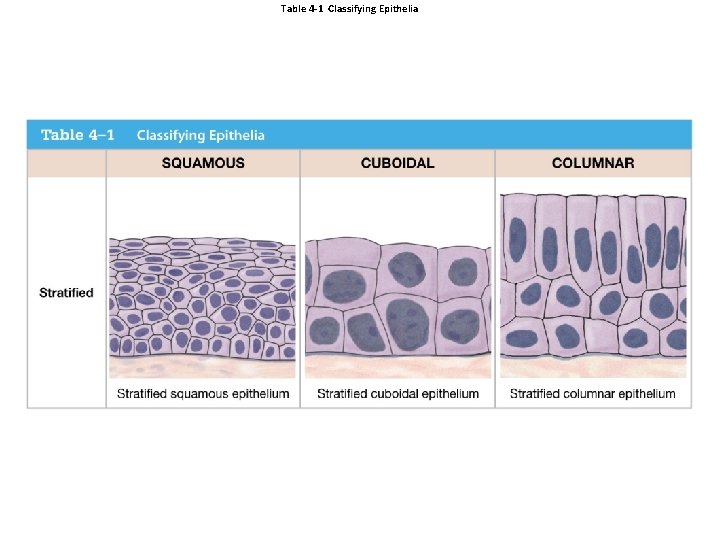
Table 4 -1 Classifying Epithelia
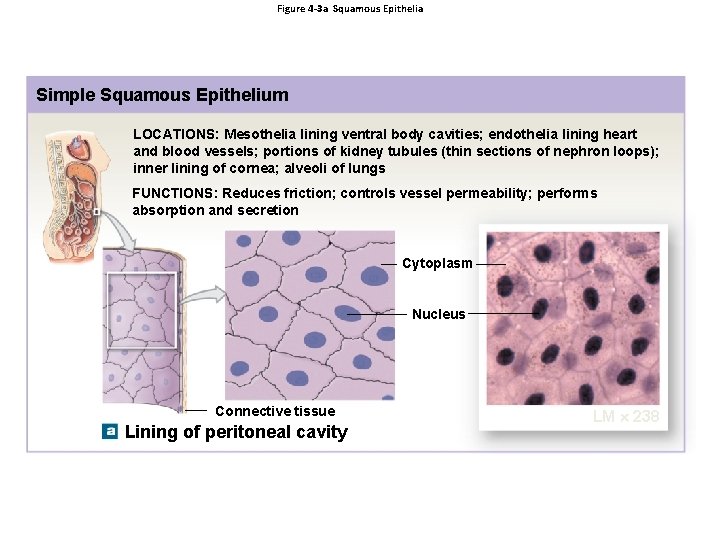
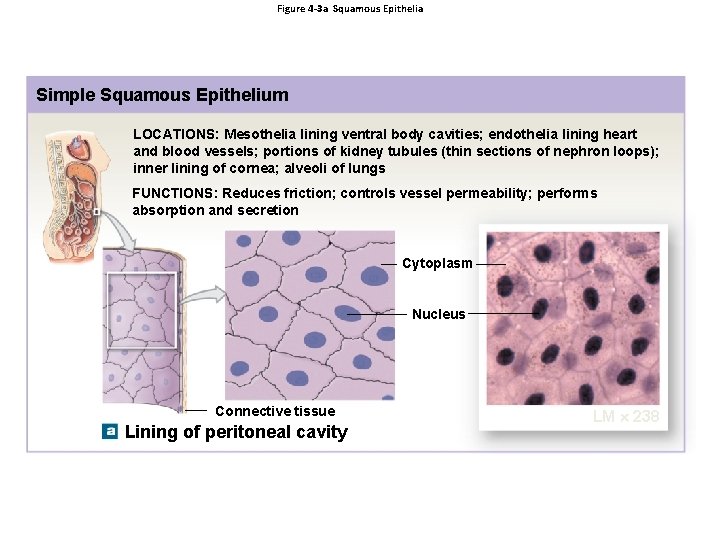
Figure 4 -3 a Squamous Epithelia Simple Squamous Epithelium LOCATIONS: Mesothelia lining ventral body cavities; endothelia lining heart and blood vessels; portions of kidney tubules (thin sections of nephron loops); inner lining of cornea; alveoli of lungs FUNCTIONS: Reduces friction; controls vessel permeability; performs absorption and secretion Cytoplasm Nucleus Connective tissue Lining of peritoneal cavity LM 238
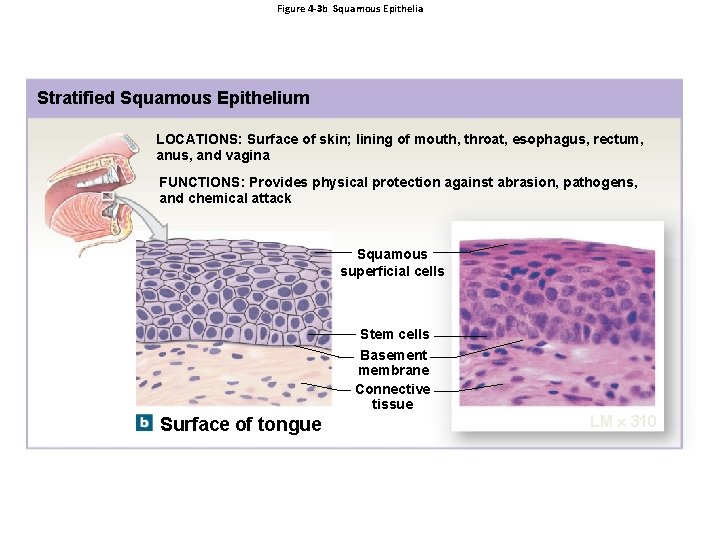
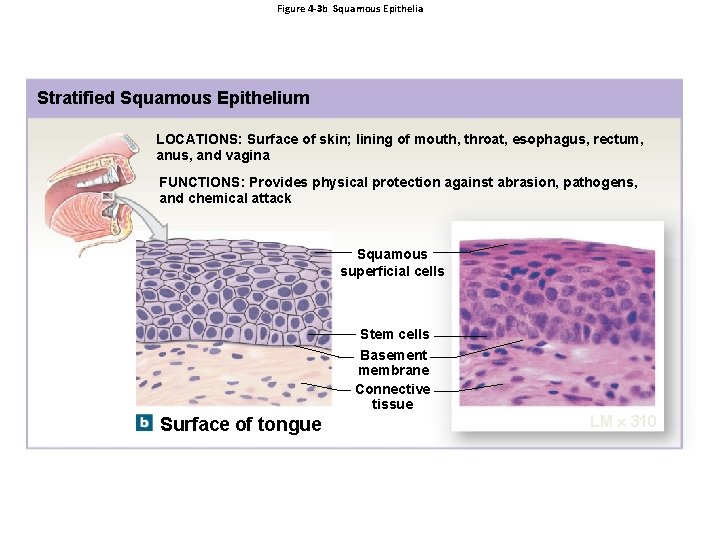
Figure 4 -3 b Squamous Epithelia Stratified Squamous Epithelium LOCATIONS: Surface of skin; lining of mouth, throat, esophagus, rectum, anus, and vagina FUNCTIONS: Provides physical protection against abrasion, pathogens, and chemical attack Squamous superficial cells Stem cells Basement membrane Connective tissue Surface of tongue LM 310
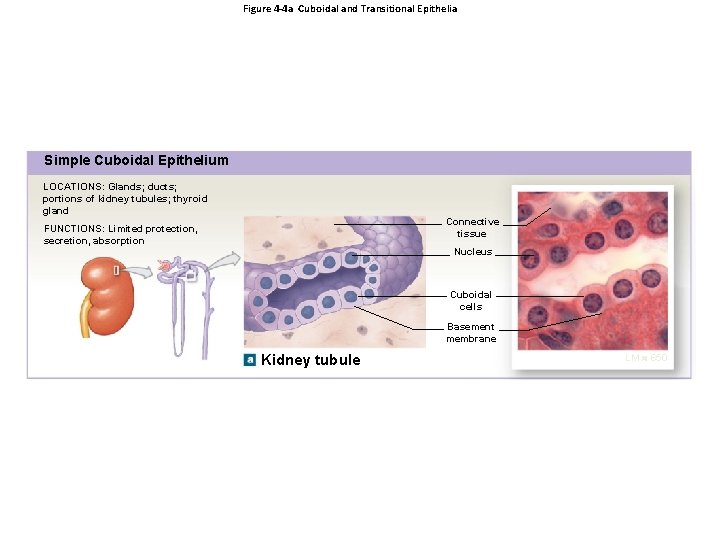
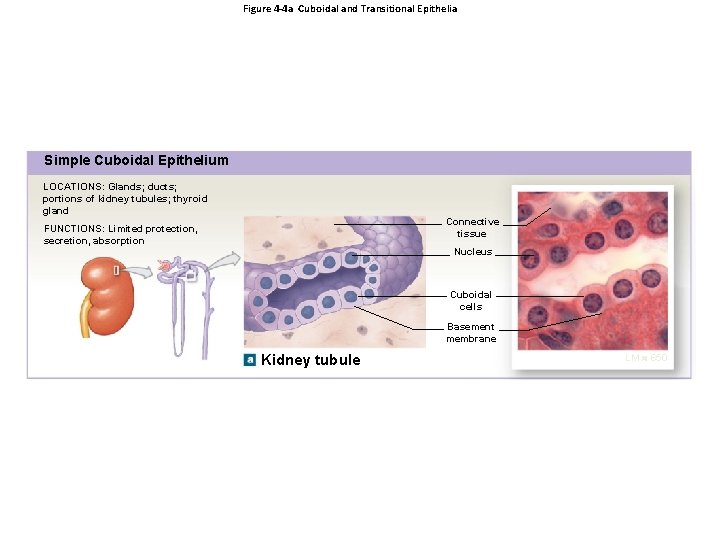
Figure 4 -4 a Cuboidal and Transitional Epithelia Simple Cuboidal Epithelium LOCATIONS: Glands; ducts; portions of kidney tubules; thyroid gland Connective tissue FUNCTIONS: Limited protection, secretion, absorption Nucleus Cuboidal cells Basement membrane Kidney tubule LM 650
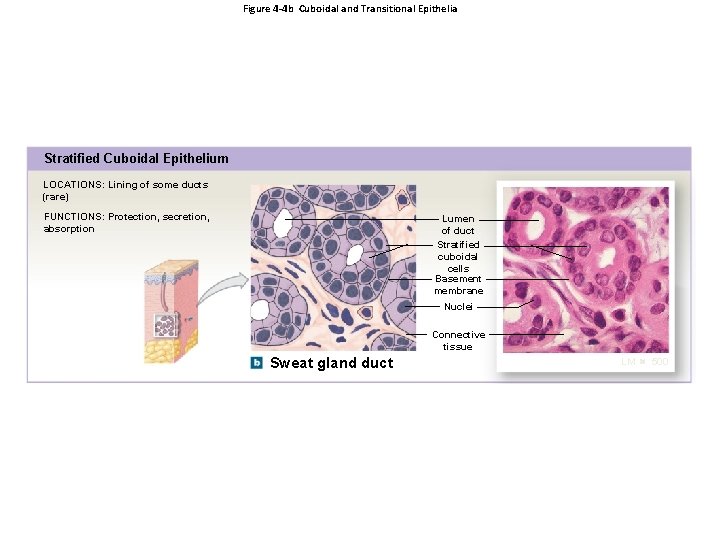
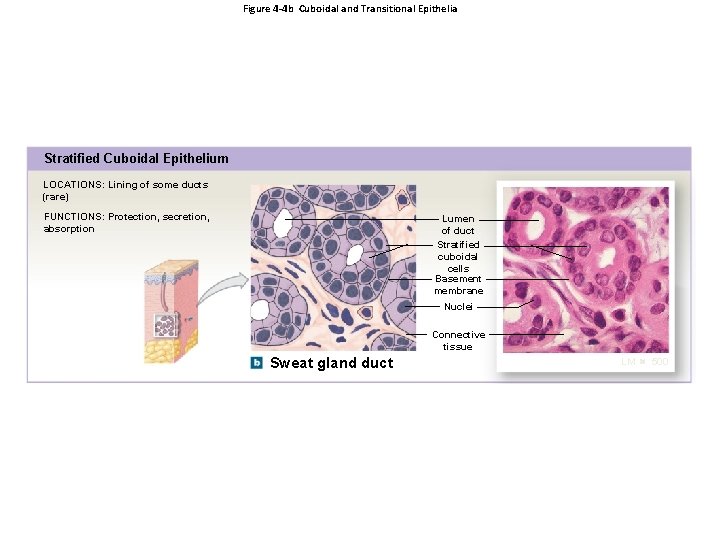
Figure 4 -4 b Cuboidal and Transitional Epithelia Stratified Cuboidal Epithelium LOCATIONS: Lining of some ducts (rare) FUNCTIONS: Protection, secretion, absorption Lumen of duct Stratified cuboidal cells Basement membrane Nuclei Connective tissue Sweat gland duct LM 500
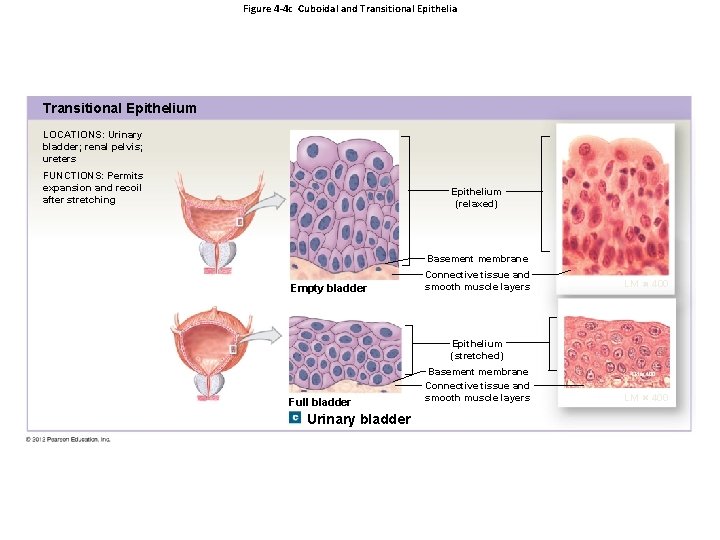
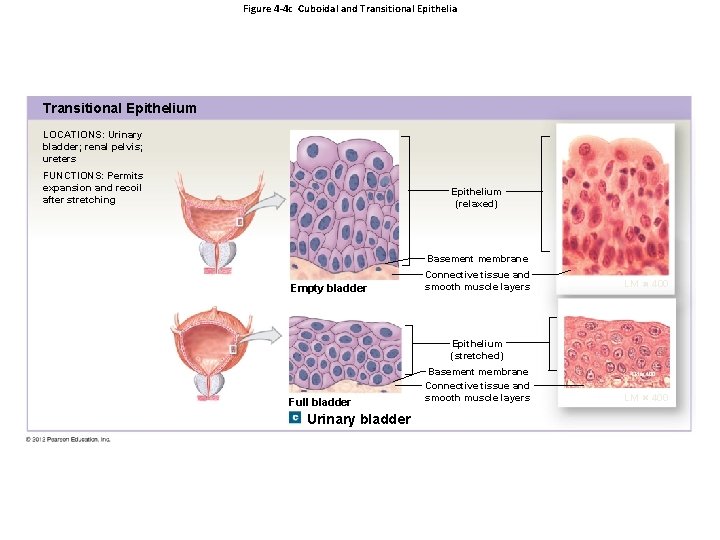
Figure 4 -4 c Cuboidal and Transitional Epithelia Transitional Epithelium LOCATIONS: Urinary bladder; renal pelvis; ureters FUNCTIONS: Permits expansion and recoil after stretching Epithelium (relaxed) Basement membrane Empty bladder Connective tissue and smooth muscle layers LM 400 Epithelium (stretched) Full bladder Urinary bladder Basement membrane Connective tissue and smooth muscle layers LM 400
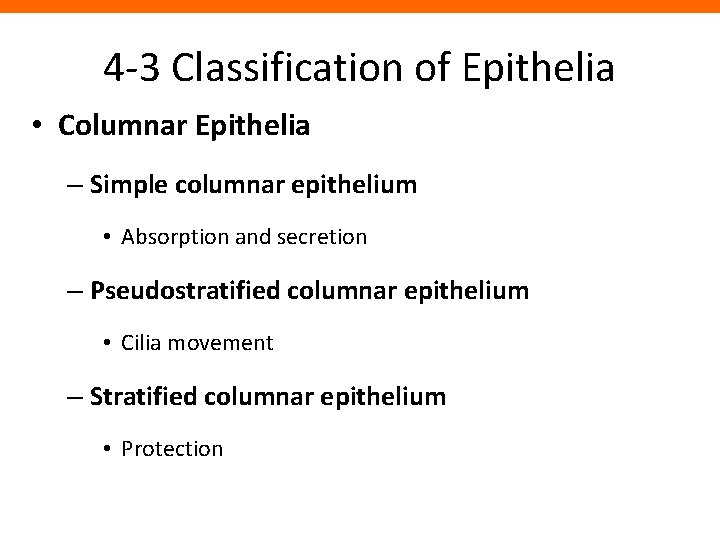
4 -3 Classification of Epithelia • Columnar Epithelia – Simple columnar epithelium • Absorption and secretion – Pseudostratified columnar epithelium • Cilia movement – Stratified columnar epithelium • Protection
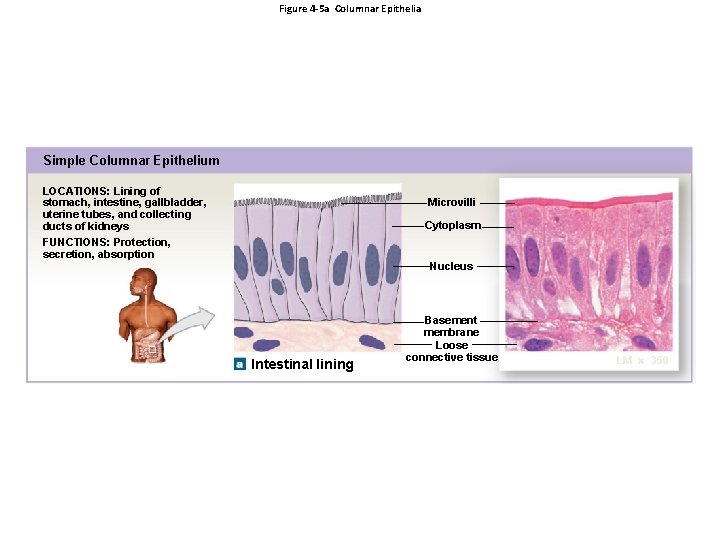
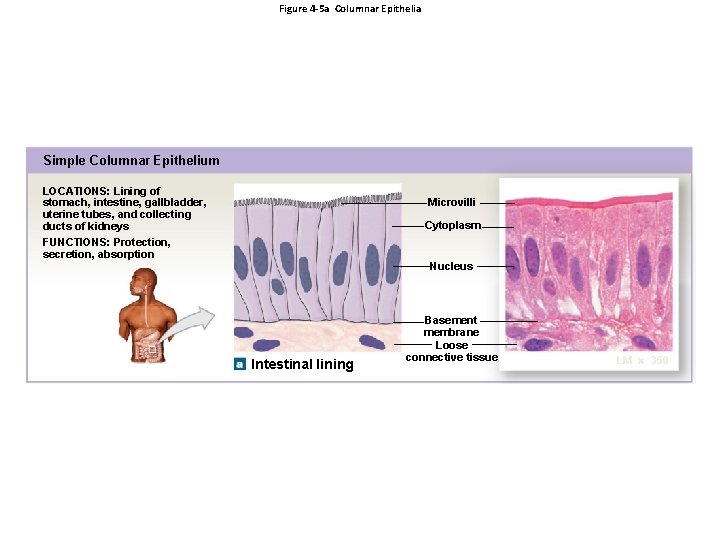
Figure 4 -5 a Columnar Epithelia Simple Columnar Epithelium LOCATIONS: Lining of stomach, intestine, gallbladder, uterine tubes, and collecting ducts of kidneys FUNCTIONS: Protection, secretion, absorption Microvilli Cytoplasm Nucleus Intestinal lining Basement membrane Loose connective tissue LM 350
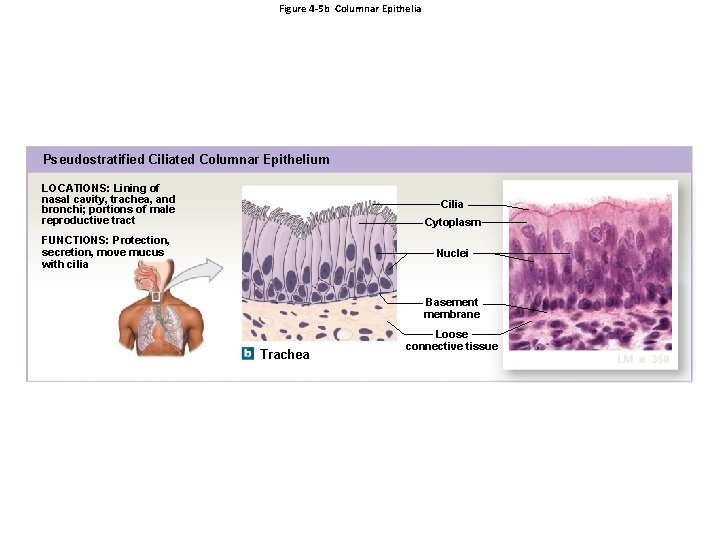
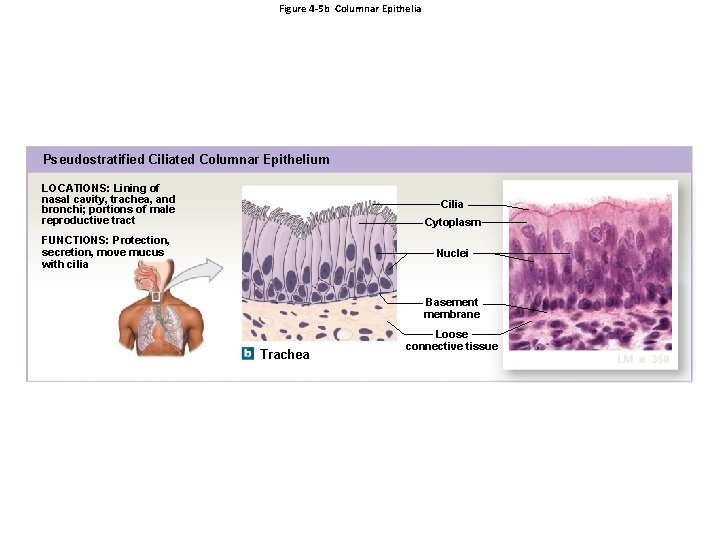
Figure 4 -5 b Columnar Epithelia Pseudostratified Ciliated Columnar Epithelium LOCATIONS: Lining of nasal cavity, trachea, and bronchi; portions of male reproductive tract Cilia Cytoplasm FUNCTIONS: Protection, secretion, move mucus with cilia Nuclei Basement membrane Trachea Loose connective tissue LM 350
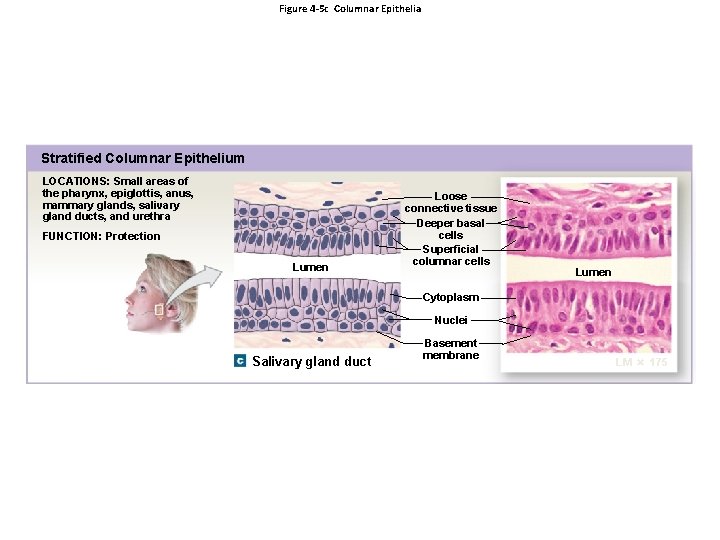
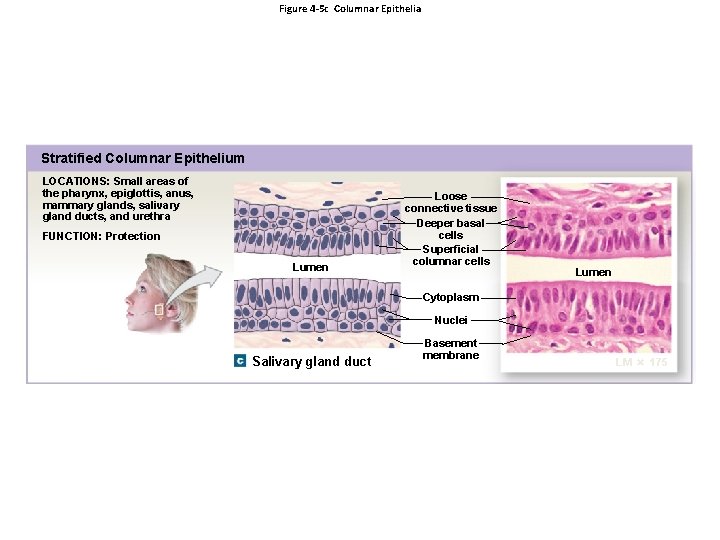
Figure 4 -5 c Columnar Epithelia Stratified Columnar Epithelium LOCATIONS: Small areas of the pharynx, epiglottis, anus, mammary glands, salivary gland ducts, and urethra FUNCTION: Protection Lumen Loose connective tissue Deeper basal cells Superficial columnar cells Lumen Cytoplasm Nuclei Salivary gland duct Basement membrane LM 175
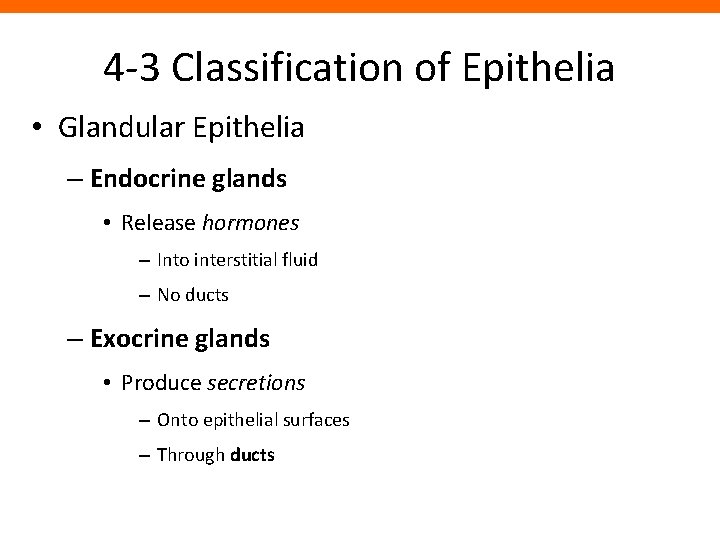
4 -3 Classification of Epithelia • Glandular Epithelia – Endocrine glands • Release hormones – Into interstitial fluid – No ducts – Exocrine glands • Produce secretions – Onto epithelial surfaces – Through ducts
4 -3 Classification of Epithelia • Glandular Epithelia – Modes of Secretion 1. Merocrine secretion 2. Apocrine secretion 3. Holocrine secretion
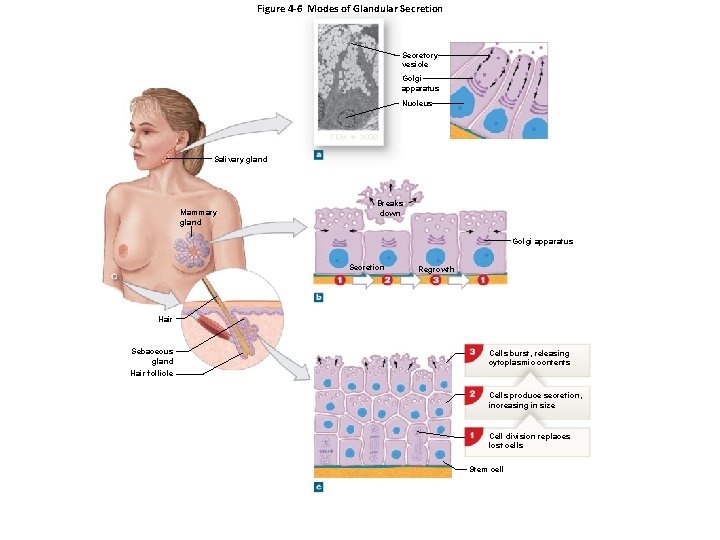
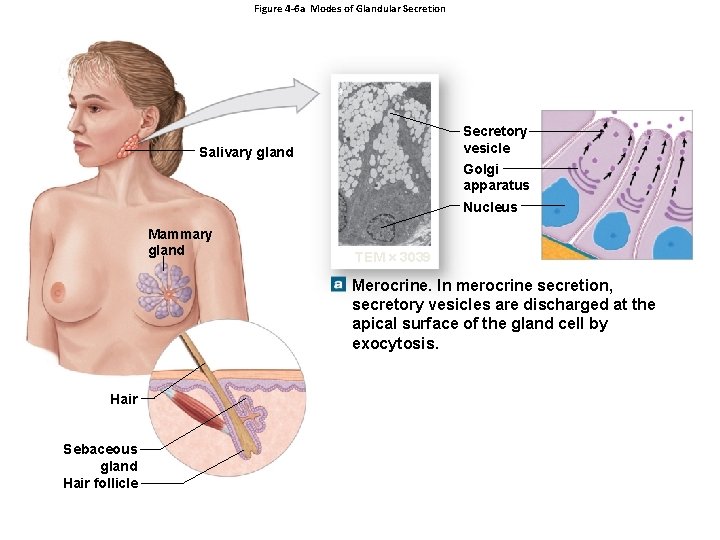
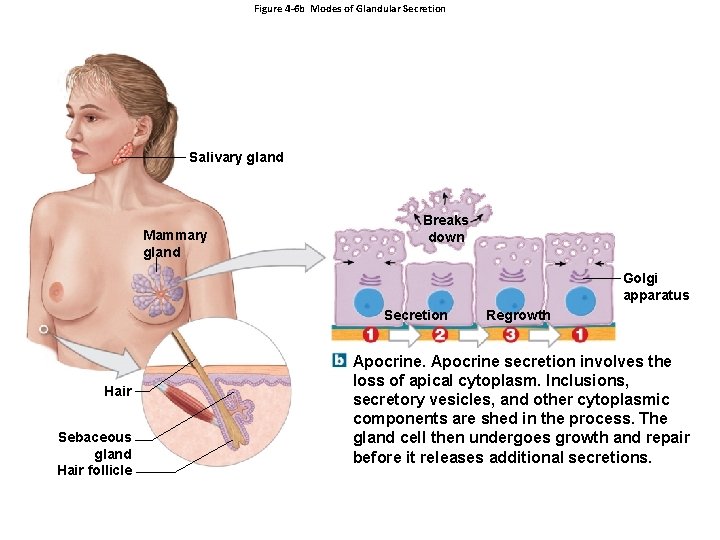
4 -3 Classification of Epithelia – Merocrine Secretion • Produced in Golgi apparatus • Released by vesicles (exocytosis) • For example, sweat glands – Apocrine Secretion • Produced in Golgi apparatus • Released by shedding cytoplasm • For example, mammary glands
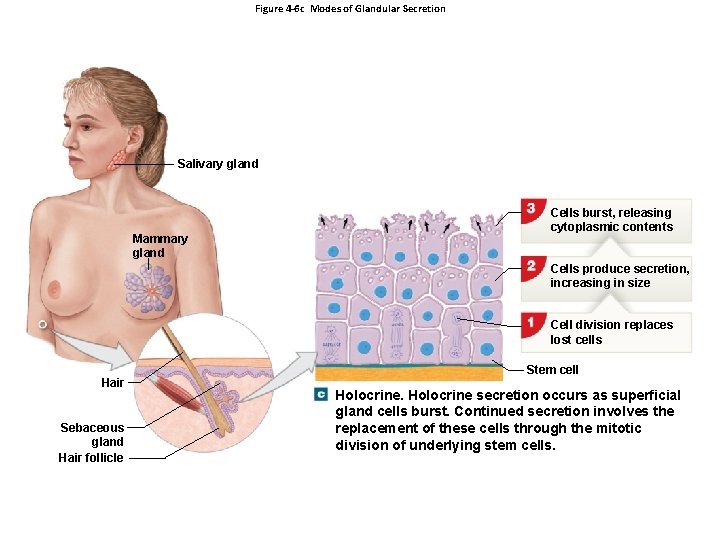
4 -3 Classification of Epithelia – Holocrine Secretion • Released by cells bursting, killing gland cells • Gland cells replaced by stem cells • For example, sebaceous glands
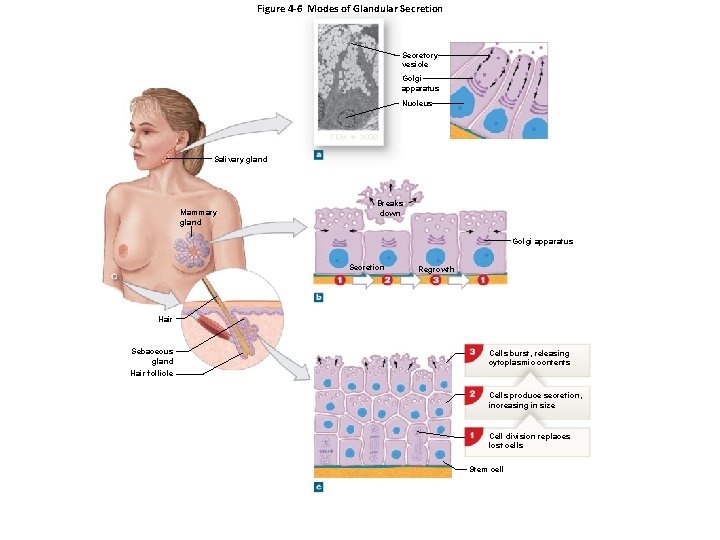
Figure 4 -6 Modes of Glandular Secretion Secretory vesicle Golgi apparatus Nucleus TEM 3039 Salivary gland Mammary gland Breaks down Golgi apparatus Secretion Regrowth Hair Sebaceous gland Cells burst, releasing cytoplasmic contents Hair follicle Cells produce secretion, increasing in size Cell division replaces lost cells Stem cell
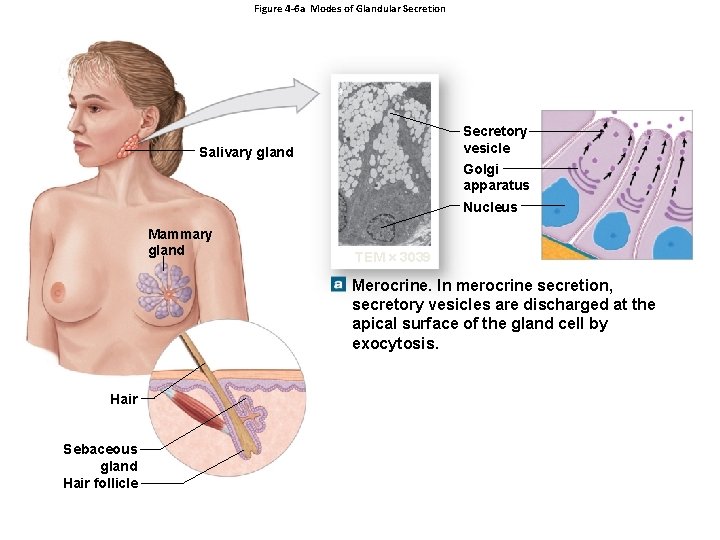
Figure 4 -6 a Modes of Glandular Secretion Secretory vesicle Golgi apparatus Salivary gland Nucleus Mammary gland TEM 3039 Merocrine. In merocrine secretion, secretory vesicles are discharged at the apical surface of the gland cell by exocytosis. Hair Sebaceous gland Hair follicle
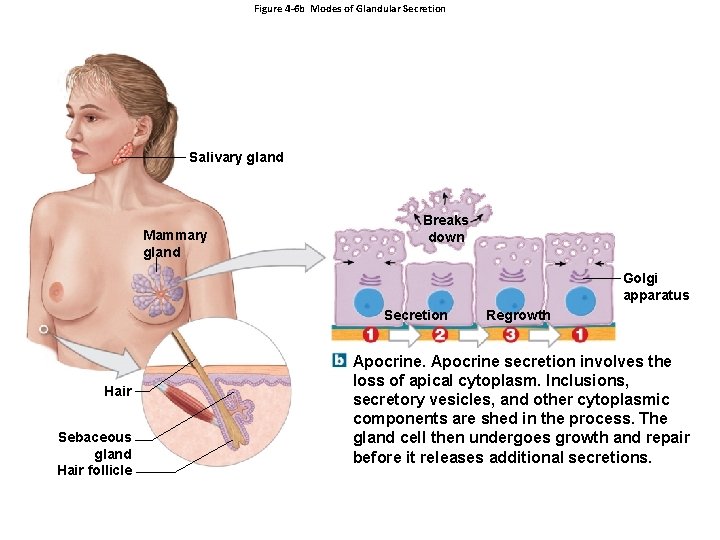
Figure 4 -6 b Modes of Glandular Secretion Salivary gland Mammary gland Breaks down Golgi apparatus Secretion Hair Sebaceous gland Hair follicle Regrowth Apocrine secretion involves the loss of apical cytoplasm. Inclusions, secretory vesicles, and other cytoplasmic components are shed in the process. The gland cell then undergoes growth and repair before it releases additional secretions.
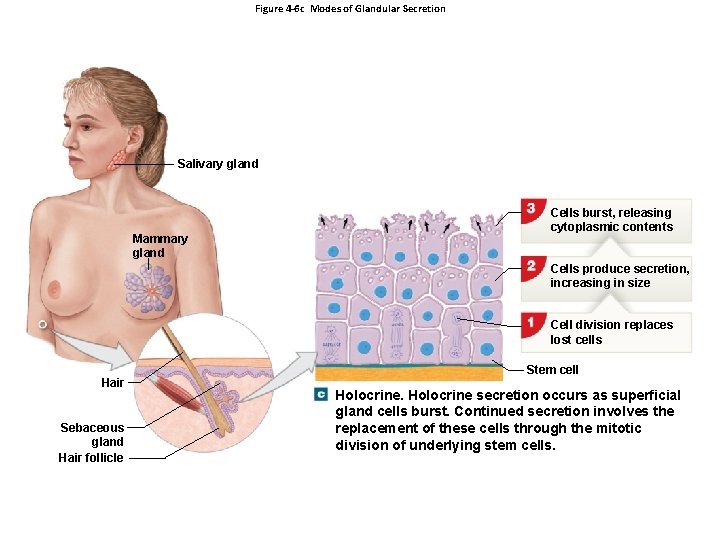
Figure 4 -6 c Modes of Glandular Secretion Salivary gland Mammary gland Cells burst, releasing cytoplasmic contents Cells produce secretion, increasing in size Cell division replaces lost cells Hair Sebaceous gland Hair follicle Stem cell Holocrine secretion occurs as superficial gland cells burst. Continued secretion involves the replacement of these cells through the mitotic division of underlying stem cells.
4 -3 Classification of Epithelia • Glandular Epithelia – Types of Secretions • Serous glands – Watery secretions • Mucous glands – Secrete mucins • Mixed exocrine glands – Both serous and mucous
4 -3 Classification of Epithelia • Glandular Epithelia – Gland Structure • Unicellular glands • Multicellular glands
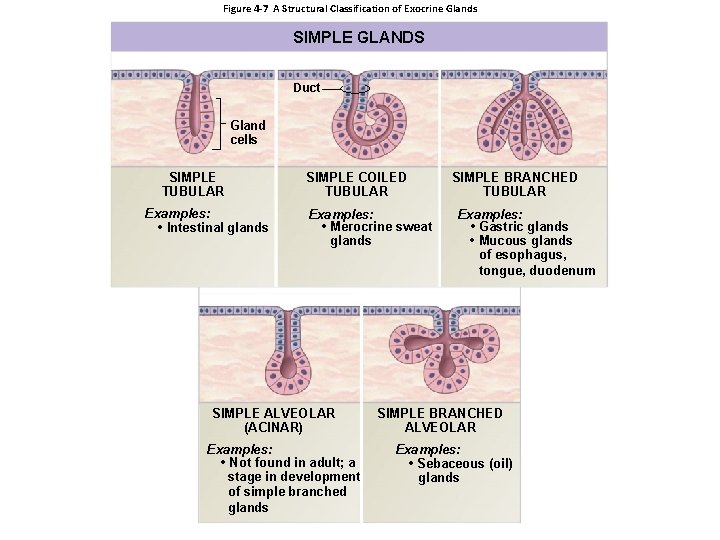
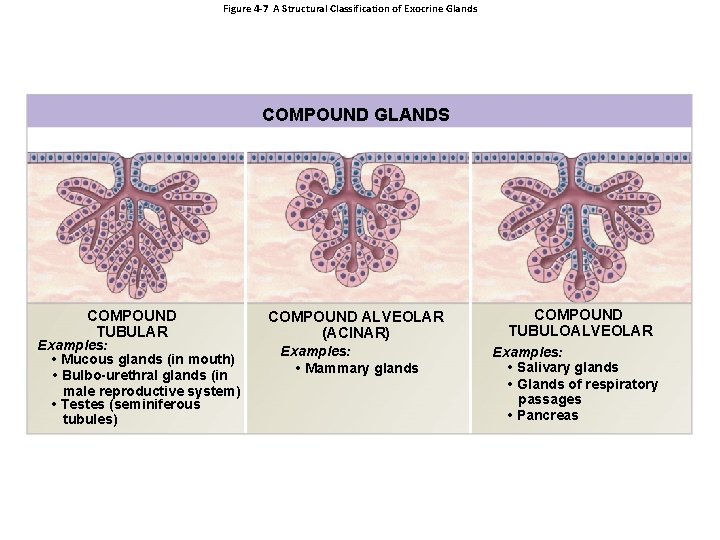
4 -3 Classification of Epithelia • Gland Structure • Multicellular glands 1. Structure of the duct » Simple (undivided) » Compound (divided) 2. Shape of secretory portion of the gland » Tubular (tube shaped) » Alveolar or acinar (blind pockets) 3. Relationship between ducts and glandular areas » Branched (several secretory areas sharing one duct)
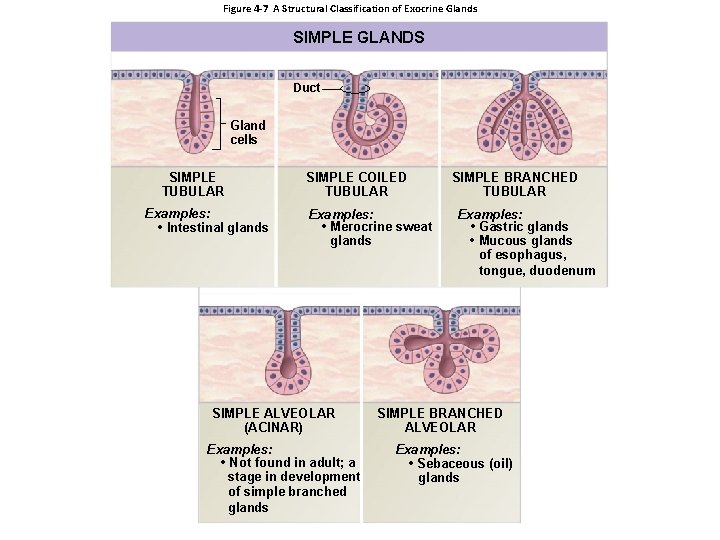
Figure 4 -7 A Structural Classification of Exocrine Glands SIMPLE GLANDS Duct Gland cells SIMPLE TUBULAR Examples: • Intestinal glands SIMPLE COILED TUBULAR Examples: • Merocrine sweat glands SIMPLE ALVEOLAR (ACINAR) Examples: • Not found in adult; a stage in development of simple branched glands SIMPLE BRANCHED TUBULAR Examples: • Gastric glands • Mucous glands of esophagus, tongue, duodenum SIMPLE BRANCHED ALVEOLAR Examples: • Sebaceous (oil) glands
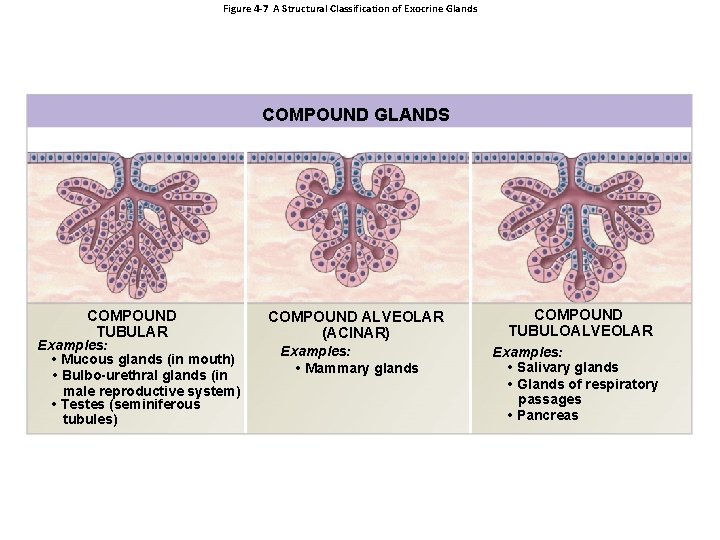
Figure 4 -7 A Structural Classification of Exocrine Glands COMPOUND GLANDS COMPOUND TUBULAR Examples: • Mucous glands (in mouth) • Bulbo-urethral glands (in male reproductive system) • Testes (seminiferous tubules) COMPOUND ALVEOLAR (ACINAR) Examples: • Mammary glands COMPOUND TUBULOALVEOLAR Examples: • Salivary glands • Glands of respiratory passages • Pancreas