An Infant with Neuroregression Dr KF Huen TKOH







- Slides: 51
An Infant with Neuro-regression Dr. KF Huen TKOH
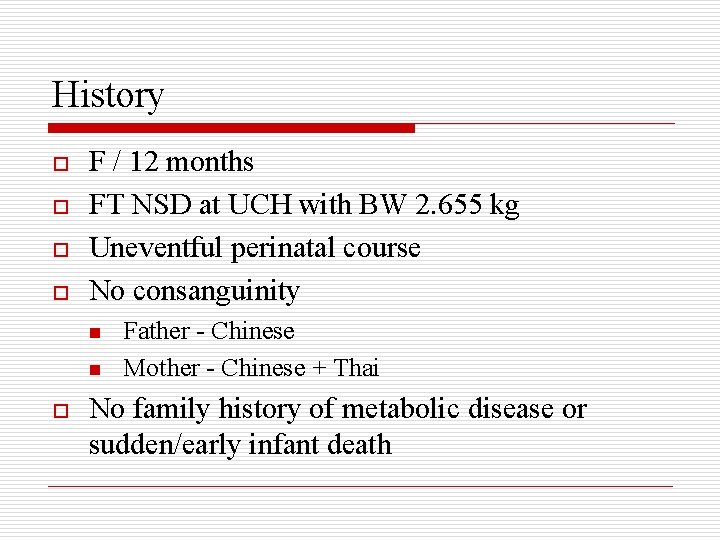
History o o F / 12 months FT NSD at UCH with BW 2. 655 kg Uneventful perinatal course No consanguinity n n o Father - Chinese Mother - Chinese + Thai No family history of metabolic disease or sudden/early infant death
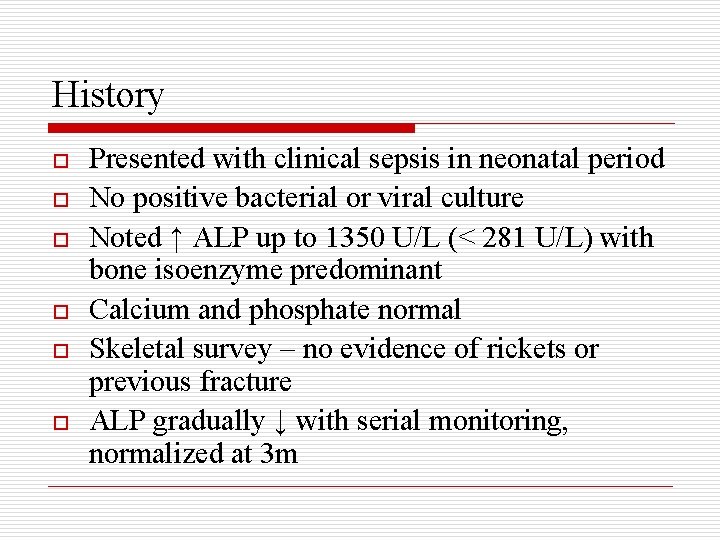
History o o o Presented with clinical sepsis in neonatal period No positive bacterial or viral culture Noted ↑ ALP up to 1350 U/L (< 281 U/L) with bone isoenzyme predominant Calcium and phosphate normal Skeletal survey – no evidence of rickets or previous fracture ALP gradually ↓ with serial monitoring, normalized at 3 m
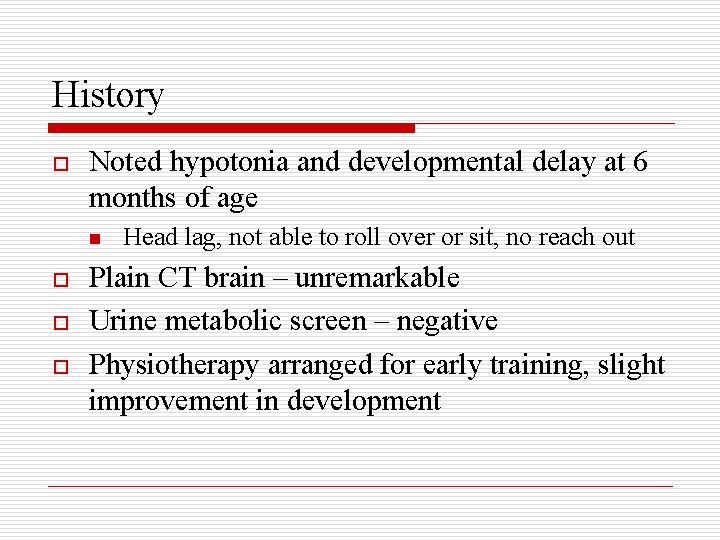
History o Noted hypotonia and developmental delay at 6 months of age n o o o Head lag, not able to roll over or sit, no reach out Plain CT brain – unremarkable Urine metabolic screen – negative Physiotherapy arranged for early training, slight improvement in development

History o o At 9 months of age, better head control, able to sit with curve back with support and able to reach out Noted neuro-regression at 11 months of age, head control lost, not able to sit with support, not able to reach out and no visual fixation and follow More easy choking on oral feeding Assessment in CAC at 12 months – significant global delay (mental age = 1 month)
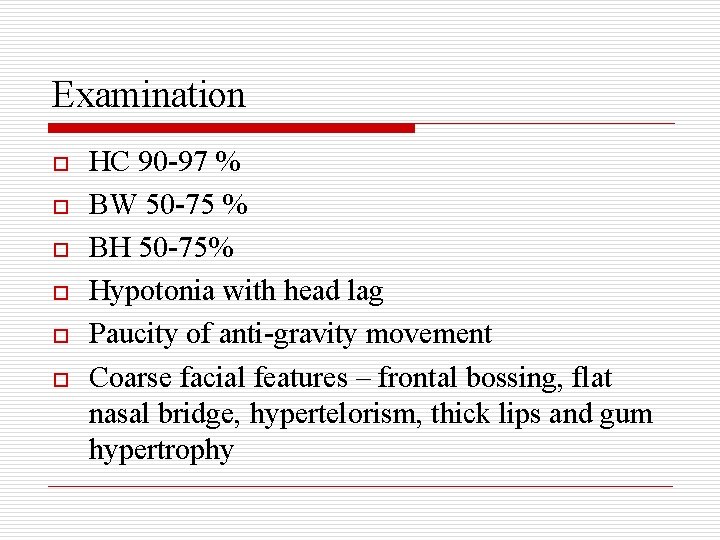
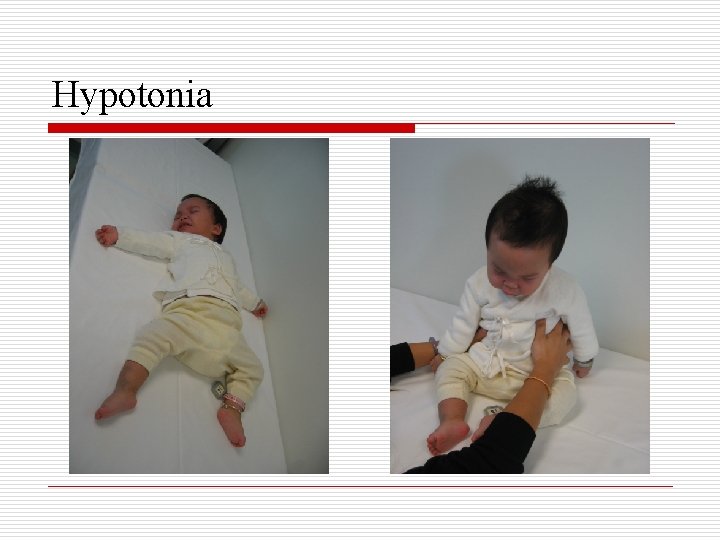
Examination o o o HC 90 -97 % BW 50 -75 % BH 50 -75% Hypotonia with head lag Paucity of anti-gravity movement Coarse facial features – frontal bossing, flat nasal bridge, hypertelorism, thick lips and gum hypertrophy
Examination o o o No cataract or corneal clouding No fix and follow Abdomen – hepatosplenomegaly CVS – unremarkable Chest – unremarkable
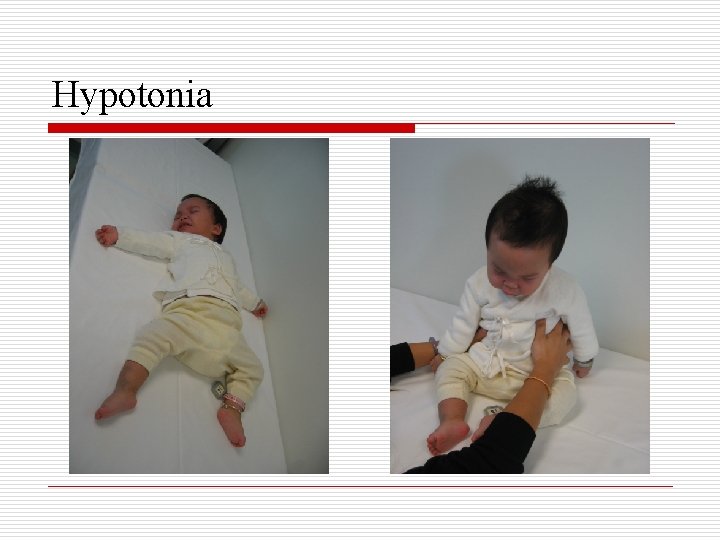
Hypotonia

Coarse Facial Features

Extensive Mongolian Spots
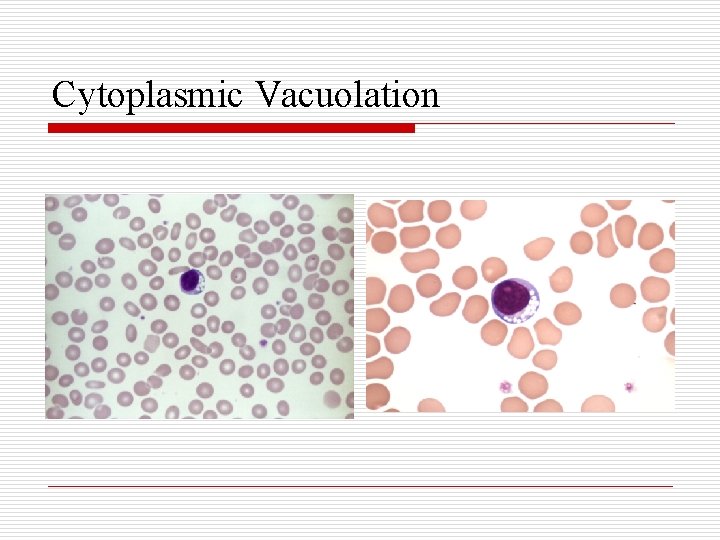
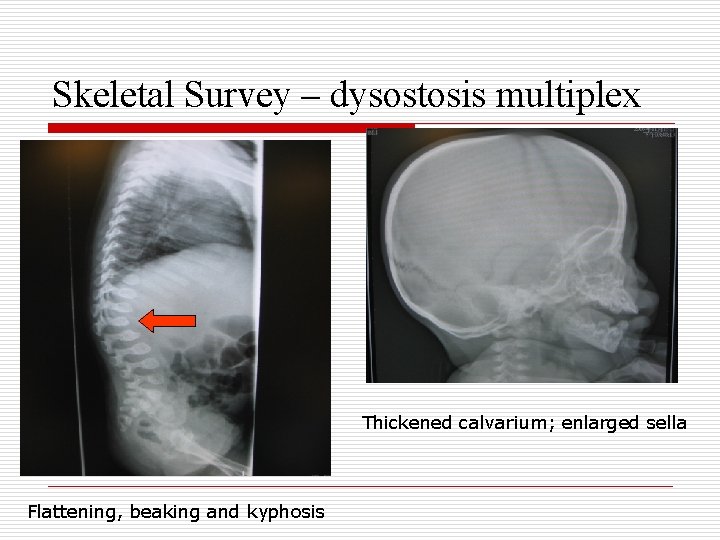
Investigations o o o CBP – atypical lymphocytosis with a number of lymphocytes with prominent cytoplasmic vacuolation LFT – ALP 522 (< 281 U/L), ALT 39 (< 33 U/L) Skeletal survey – ovoid shaped vertebral bodies, anterior beaking of T 12 and especially L 1 with kyphosis, thickened skull vault, normal pituitary fossa
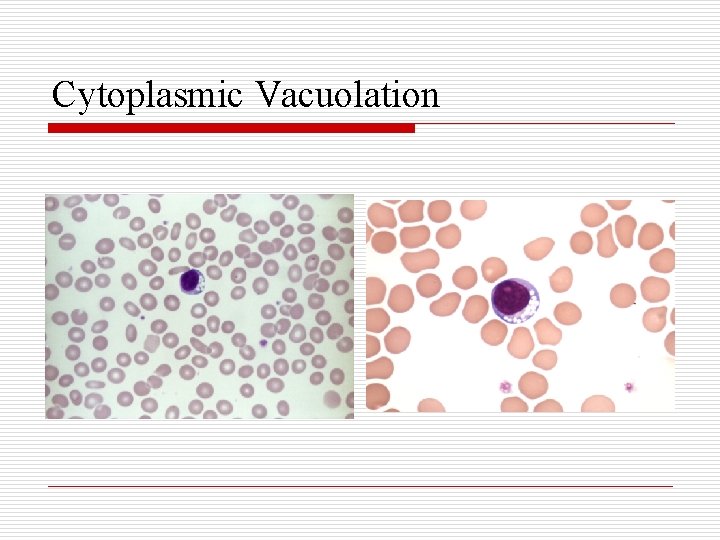
Cytoplasmic Vacuolation
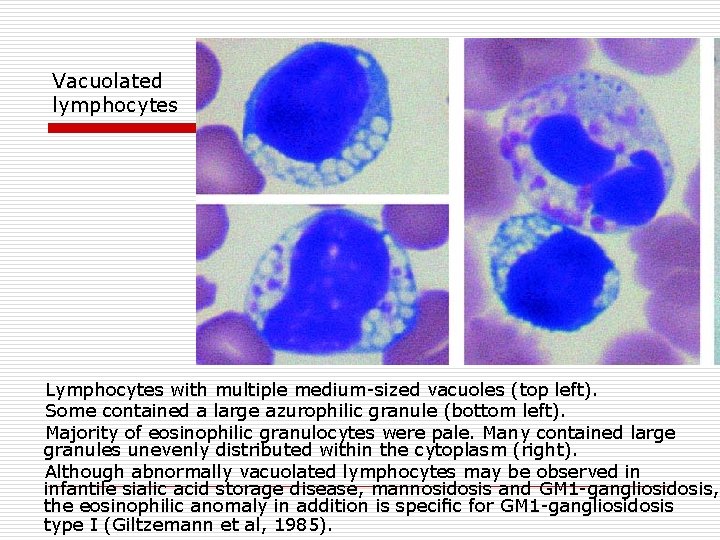
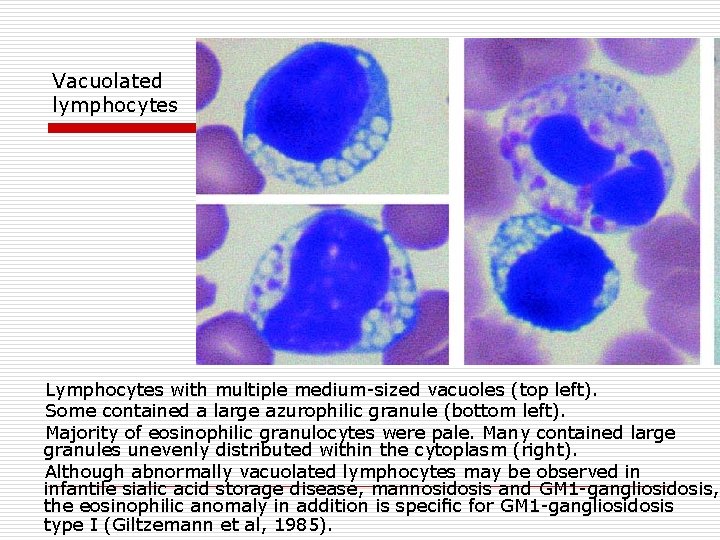
Vacuolated lymphocytes Lymphocytes with multiple medium sized vacuoles (top left). Some contained a large azurophilic granule (bottom left). Majority of eosinophilic granulocytes were pale. Many contained large granules unevenly distributed within the cytoplasm (right). Although abnormally vacuolated lymphocytes may be observed in infantile sialic acid storage disease, mannosidosis and GM 1 gangliosidosis, the eosinophilic anomaly in addition is specific for GM 1 gangliosidosis type I (Giltzemann et al, 1985).
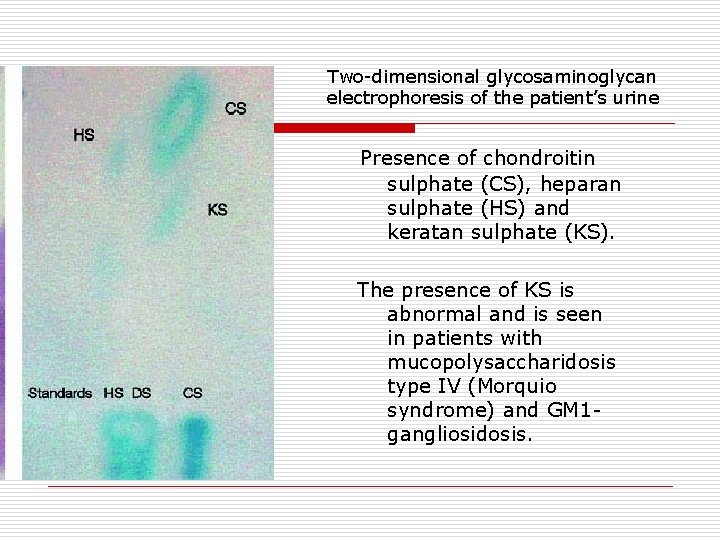
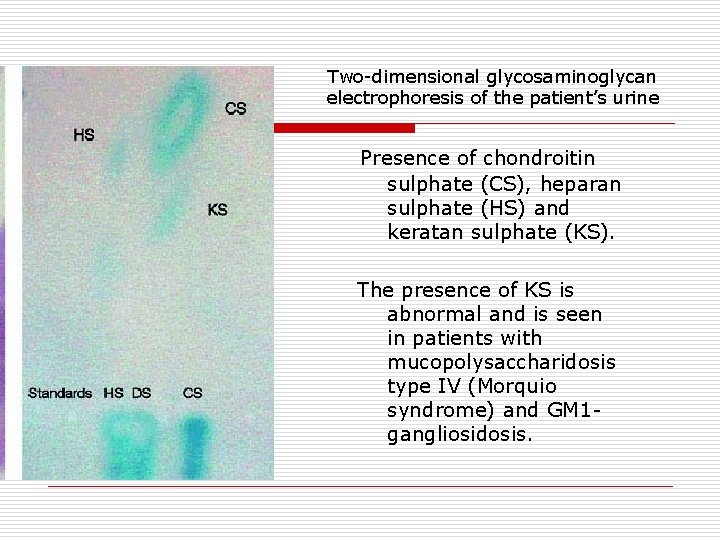
Two dimensional glycosaminoglycan electrophoresis of the patient’s urine Presence of chondroitin sulphate (CS), heparan sulphate (HS) and keratan sulphate (KS). The presence of KS is abnormal and is seen in patients with mucopolysaccharidosis type IV (Morquio syndrome) and GM 1 gangliosidosis.
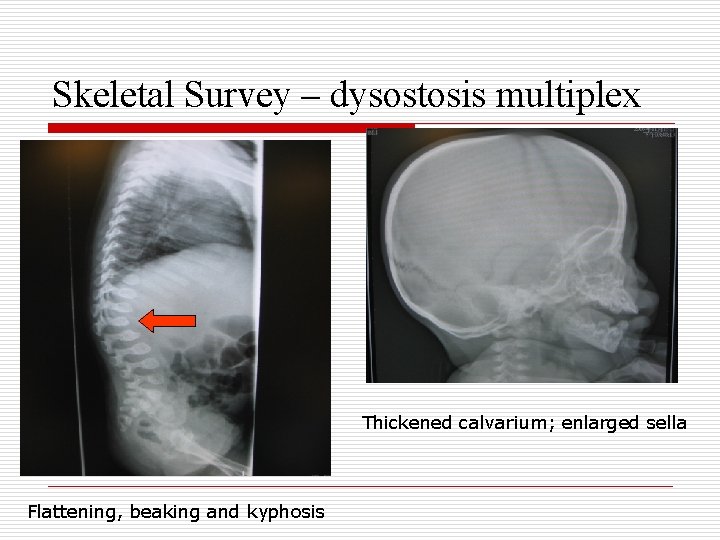
Skeletal Survey – dysostosis multiplex Thickened calvarium; enlarged sella Flattening, beaking and kyphosis
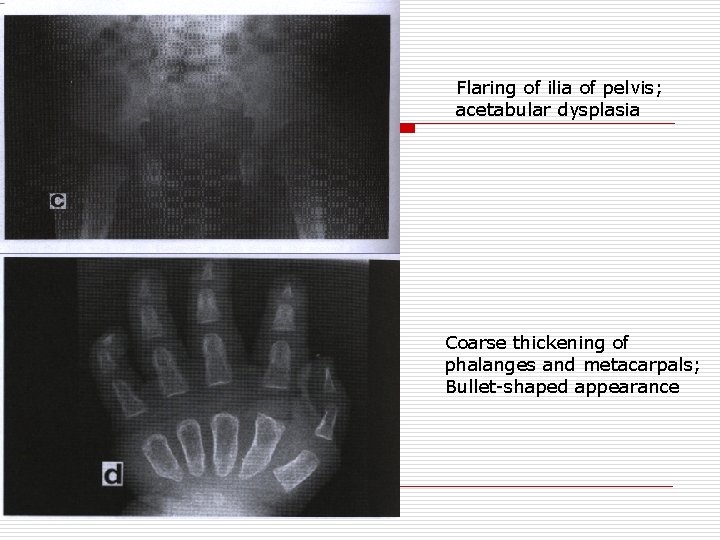
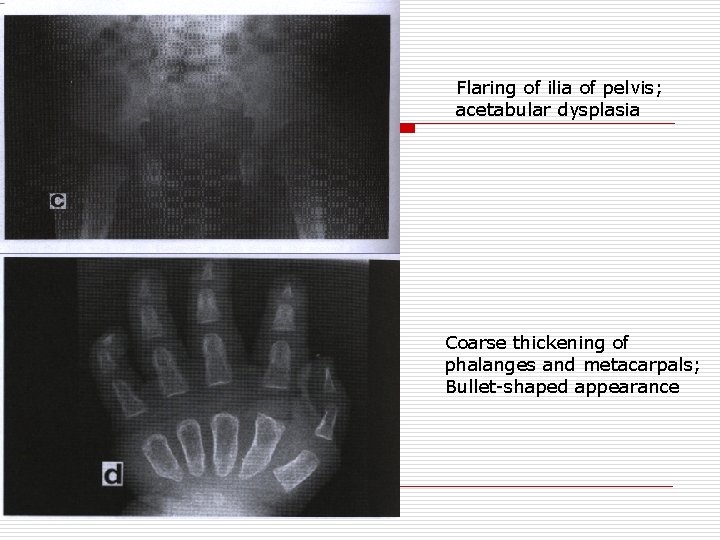
Flaring of ilia of pelvis; acetabular dysplasia Coarse thickening of phalanges and metacarpals; Bullet shaped appearance
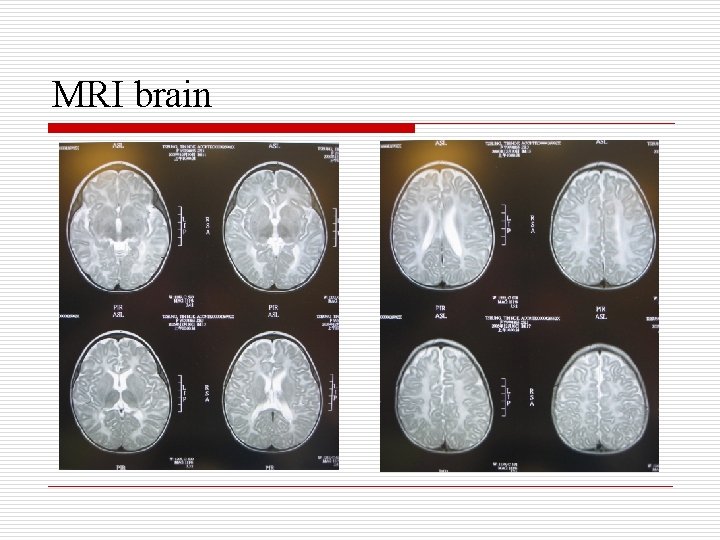
Investigations o o o Echo – no cardiomyopathy, normal LV function Ophthalmologic exam – bilateral cherry red spots ENT exam – both vocal cords smooth and mobile, bilateral moderate-severe sensorineural hearing deficit, bilateral flat tympanometry Speech therapist assessment – impaired swallowing but normal vocal cord function MRI brain – gross delay in myelination process
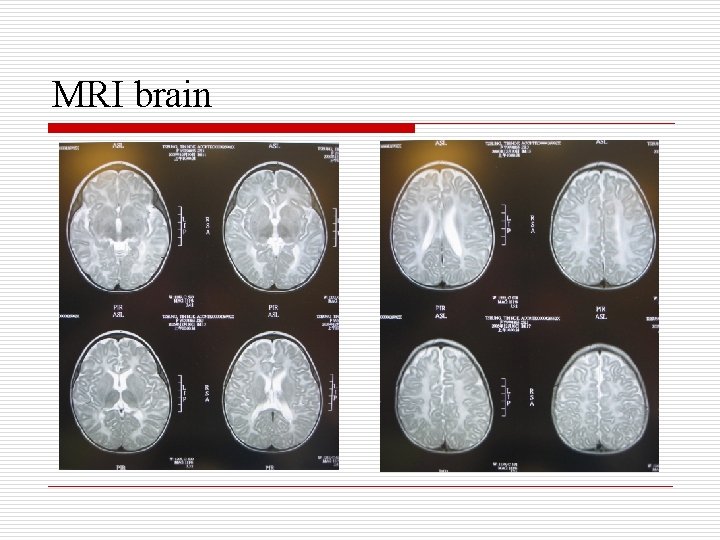
MRI brain
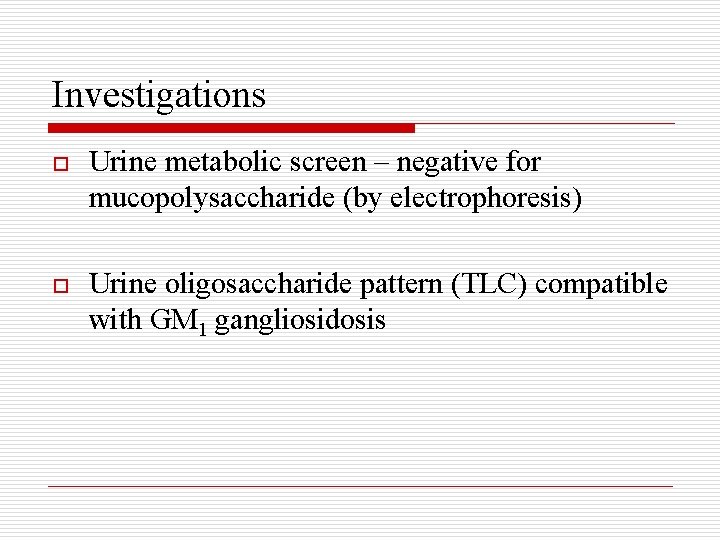
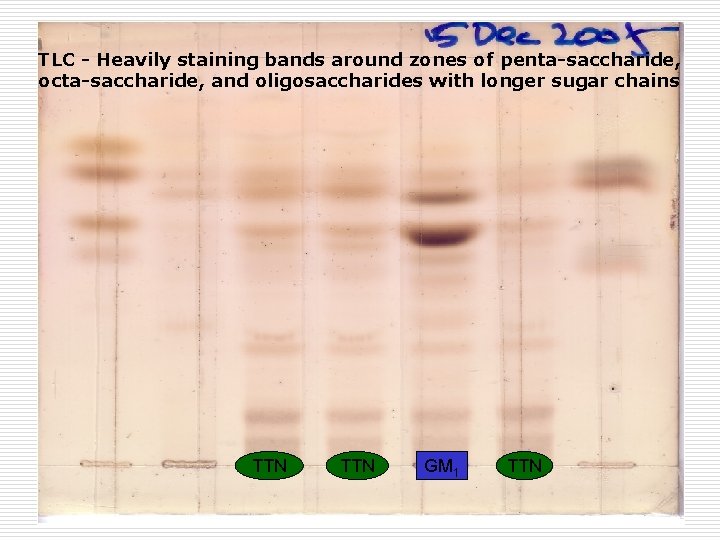
Investigations o Urine metabolic screen – negative for mucopolysaccharide (by electrophoresis) o Urine oligosaccharide pattern (TLC) compatible with GM 1 gangliosidosis
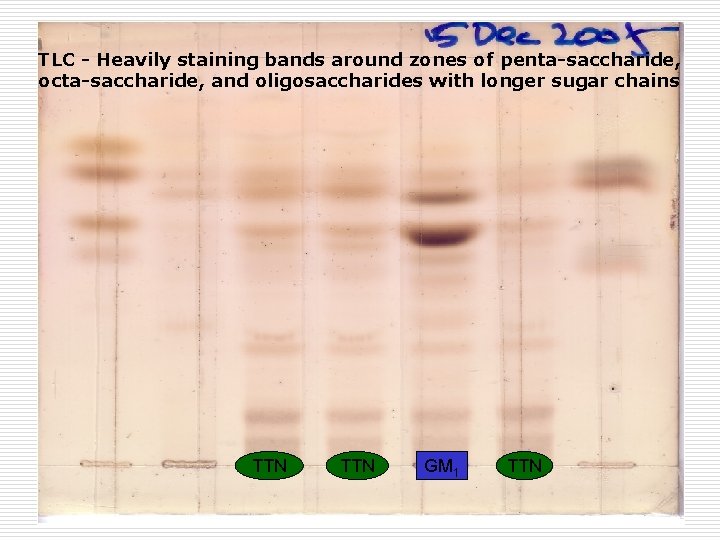
TLC - Heavily staining bands around zones of penta-saccharide, octa-saccharide, and oligosaccharides with longer sugar chains TTN GM 1 TTN
Investigations Leucocytes for enzyme assay – n Hexosaminidase A & B activity normal (GM 2 gangliosidosis – Tay-Sachs, Sandhoff) n α-galactosidase activity normal (Fabry, Schindler) n Deficient β-galactosidase activity 0. 10 (1. 0 – 6. 0 nmol/min/mg protein) o
Investigations o β-galactosidase (GLB 1) gene mutation analysis n Index: compound heterozygous for c. 495 -7 del. TCT and c. 1734 G>T n Mother: heterozygous for c. 1734 G>T n Father: mutation not detected
Diagnosis GM 1 gangliosidosis
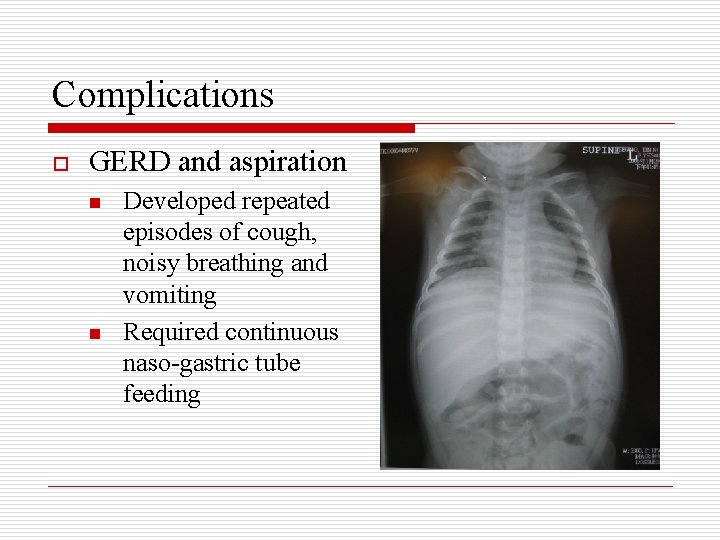
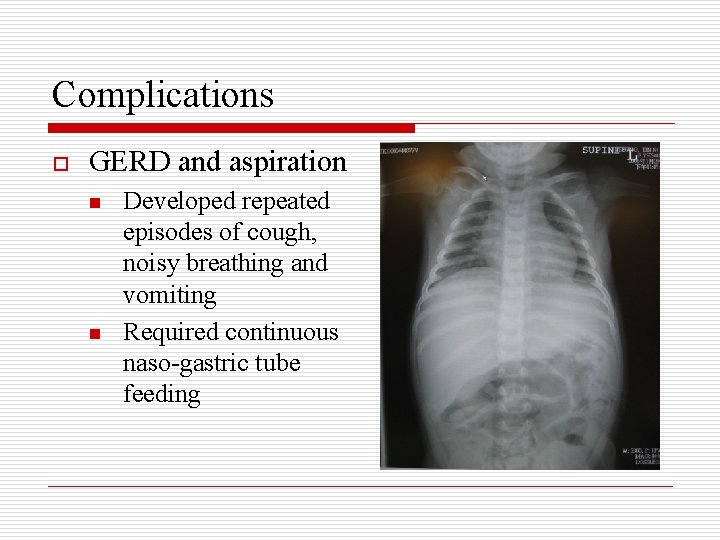
Complications o GERD and aspiration n n Developed repeated episodes of cough, noisy breathing and vomiting Required continuous naso-gastric tube feeding
Complications o Seizure n n n Developed repeated episodes of apnoea & desaturation and generalised tonic clonic convulsion EEG – epileptic tendency Required phenobarbitone, phenytoin and clobazam for seizure control
Complications o Spasticity n n Spasticity over extremeties and tight Achilles tendons Required physiotherapy and nocturnal anklefoot orthosis

Progress o o o Parents preferred naso-gastric tube feeding than gastrostomy feeding Experienced few episodes of gastro-esophageal reflux and aspiration At 18 months of age, developed aspiration pneumonia and hence respiratory failure, finally succumbed
Review GM 1 gangliosidosis
Background o o Autosomal recessive lysosomal storage disorder characterized by the generalized accumulation of GM 1 ganglioside, oligosaccharides, and the mucopolysaccharide keratan sulfate and their derivatives Deficiency of the lysosomal hydrolase, acid βgalactosidase (GLB 1), causes GM 1 gangliosidosis and Morquio disease type B (ie. mucopolysaccharidosis type IVB).
Background Three clinical subtypes classified by age of onset: o Infantile (type 1) n Combines the features of a neurolipidosis (neurodegeneration, macular cherry-red spots) with those of a mucopolysaccharidosis (visceromegaly, dysostosis multiplex, coarse facial features) n Most frequently presents in early infancy and may be evident at birth o Juvenile (type 2) n Slightly later age of onset and clinical variability in the classic physical features o Adult (type 3) n Normal early neurologic development with no physical stigmata and subsequent development of a slowly progressive dementia with parkinsonian features, extrapyramidal disease and dystonia
Pathophysiology o o o Acid β-galactosidase is a lysosomal hydrolase that catalyzes the removal of the terminal β-linked galactose from glycoconjugates (eg. GM 1 ganglioside), generating GM 2 ganglioside Degrades other β-galactose-containing glycoconjugates, such as keratan sulfate Deficiency of acid β-galactosidase results in the accumulation of glycoconjugates in body tissues and their excretion in urine GM 1 ganglioside and its derivative asialo-GM 1 ganglioside (GA 1), glycoprotein-derived oligosaccharides, and keratan sulfate are found at elevated intracellular concentrations Gangliosides are normal components of cell membranes, particularly neurons, and GM 1 is the major ganglioside in the vertebrate brain Accumulation of toxic asialo- and lyso-compound GM 1 ganglioside derivatives is believed to be neuropathic
Epidemiology o Frequency n n o Race n o Rare disorder, incidence not widely available High incidence of 1 per 3700 live births in Malta Found in all race, large number of Japanese patients with adult form has been reported Sex n Autosomal recessive traits, equal sex distributions
Clinical Course o Infantile form (type 1) n n o Juvenile form (type 2) n n n o Typically presents between birth and age 6 months with progressive organomegaly, dysostosis multiplex, facial coarsening, and rapid neurologic deterioration within the first year of life Death usually occurs during the second year of life because of aspiration pneumonia and cardiopulmonary failure Typically presents at age 1 -2 years with progressive psychomotor retardation Little visceromegaly and milder skeletal disease Death usually occurs before the second decade of life Adult form (type 3) n n n Typically presents during childhood or adolescence as a slowly progressive dementia with prominent parkinsonian features and extrapyramidal disease, particularly dystonia. Marked phenotypic variability Age at death vary greatly
Clinical Features o Neurologic findings n n n n n Developmental delay, arrest, and regression Generalized hypotonia initially, developing into spasticity Exaggerated startle response Hyperreflexia Seizures Extrapyramidal disease (adult subtype) Dystonia (adult subtype) Ataxia (adult subtype) Dementia (adult subtype)
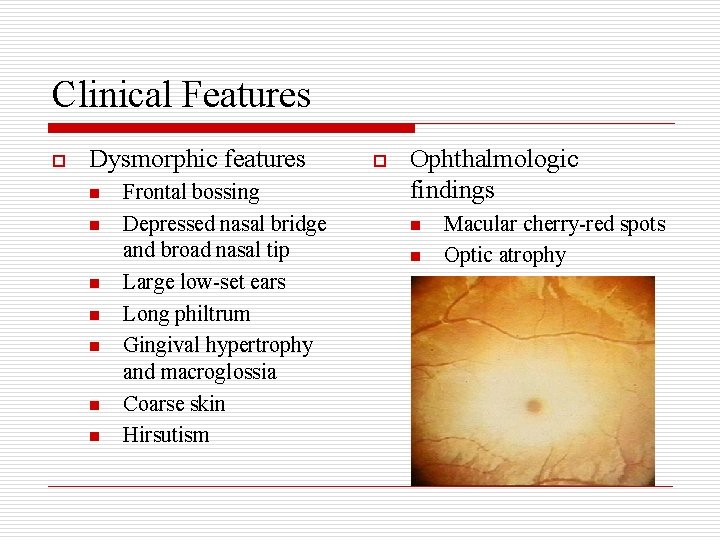
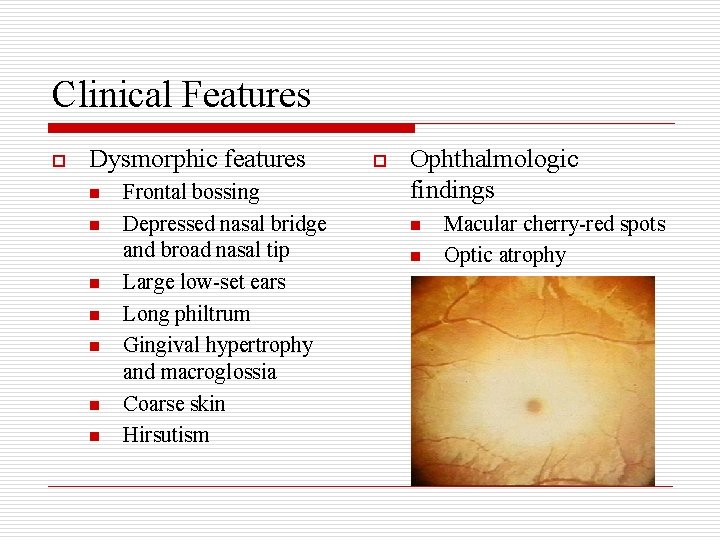
Clinical Features o Dysmorphic features n n n n Frontal bossing Depressed nasal bridge and broad nasal tip Large low-set ears Long philtrum Gingival hypertrophy and macroglossia Coarse skin Hirsutism o Ophthalmologic findings n n n Macular cherry-red spots Optic atrophy Corneal clouding
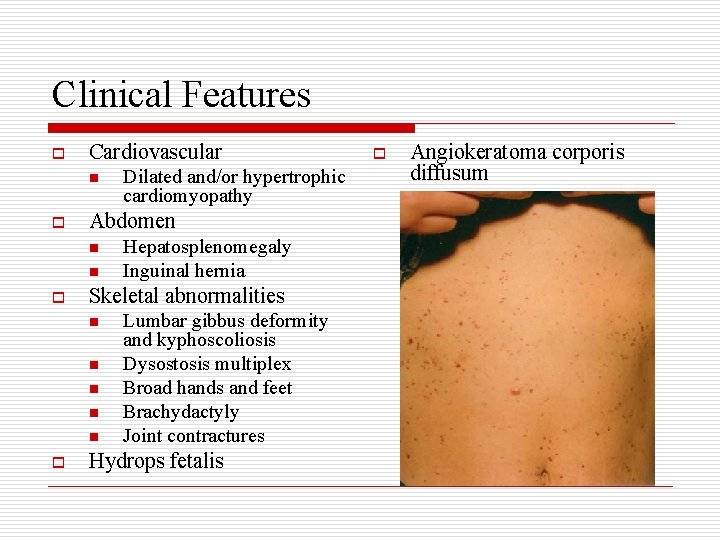
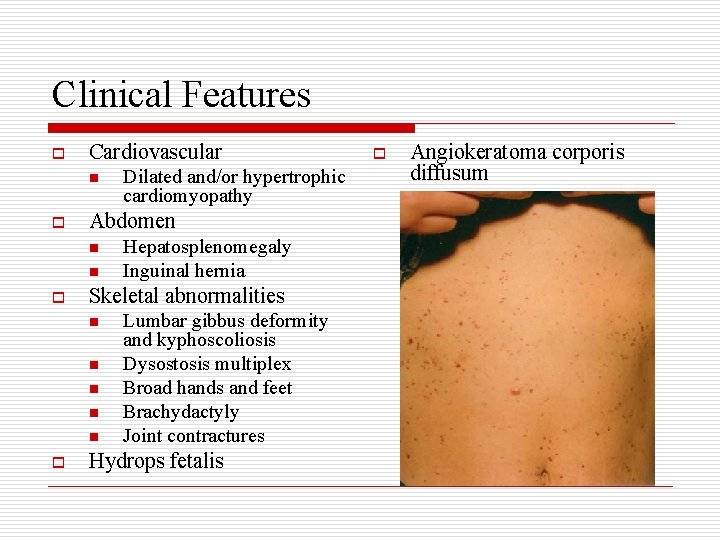
Clinical Features o Cardiovascular n o Abdomen n n o Hepatosplenomegaly Inguinal hernia Skeletal abnormalities n n n o Dilated and/or hypertrophic cardiomyopathy Lumbar gibbus deformity and kyphoscoliosis Dysostosis multiplex Broad hands and feet Brachydactyly Joint contractures Hydrops fetalis o Angiokeratoma corporis diffusum
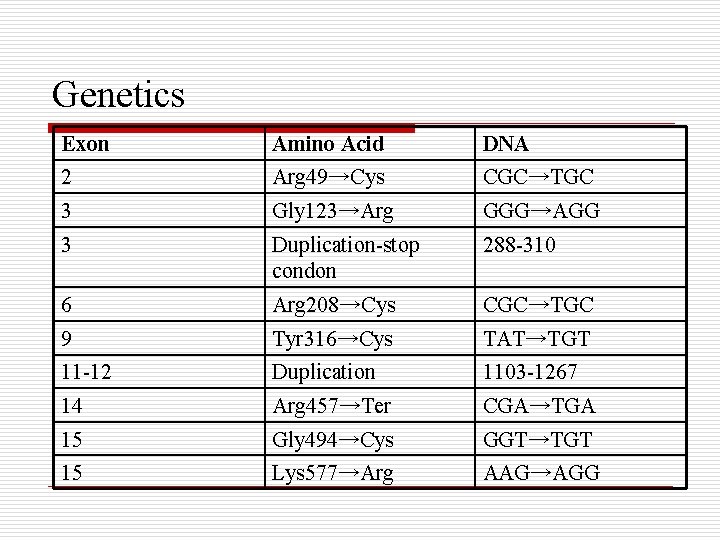
Genetics o o o Gene located on chromosome band 3 p 21. 33 Cloning and sequencing of c. DNA encoding human GLB 1 in 1988 by Oshima and others Various types of mutations identified in the acid βgalactosidase gene, including missense/nonsense, duplication/insertion and splice site abnormalities Genotype and phenotype correlations provides a molecular explanation for clinical variability Amount of residual enzyme activity determines disease subtype and severity
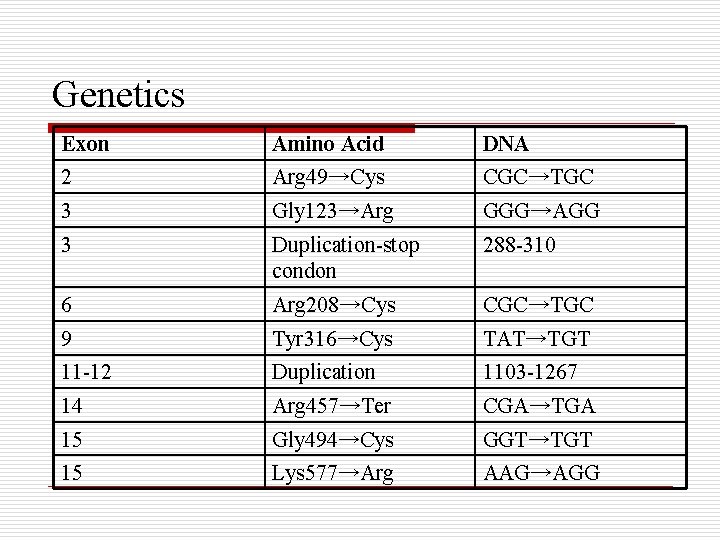
Genetics Exon Amino Acid DNA 2 Arg 49→Cys CGC→TGC 3 Gly 123→Arg GGG→AGG 3 Duplication-stop condon 288 -310 6 Arg 208→Cys CGC→TGC 9 Tyr 316→Cys TAT→TGT 11 -12 Duplication 1103 -1267 14 Arg 457→Ter CGA→TGA 15 Gly 494→Cys GGT→TGT 15 Lys 577→Arg AAG→AGG
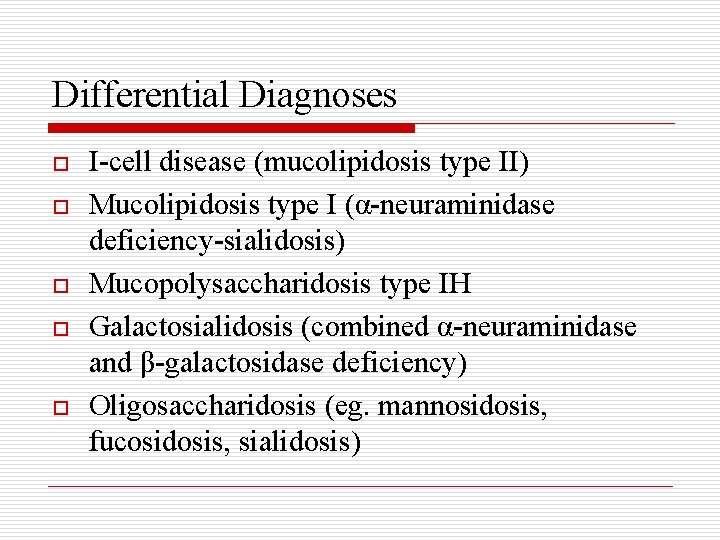
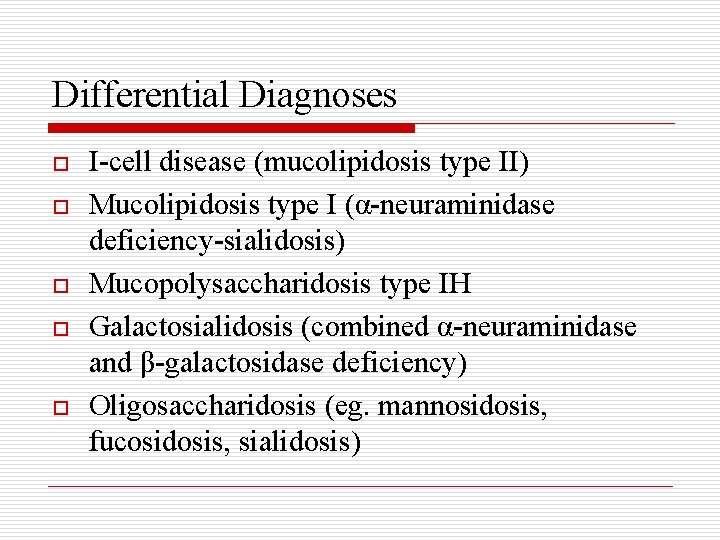
Differential Diagnoses o o o I-cell disease (mucolipidosis type II) Mucolipidosis type I (α-neuraminidase deficiency-sialidosis) Mucopolysaccharidosis type IH Galactosialidosis (combined α-neuraminidase and β-galactosidase deficiency) Oligosaccharidosis (eg. mannosidosis, fucosidosis, sialidosis)
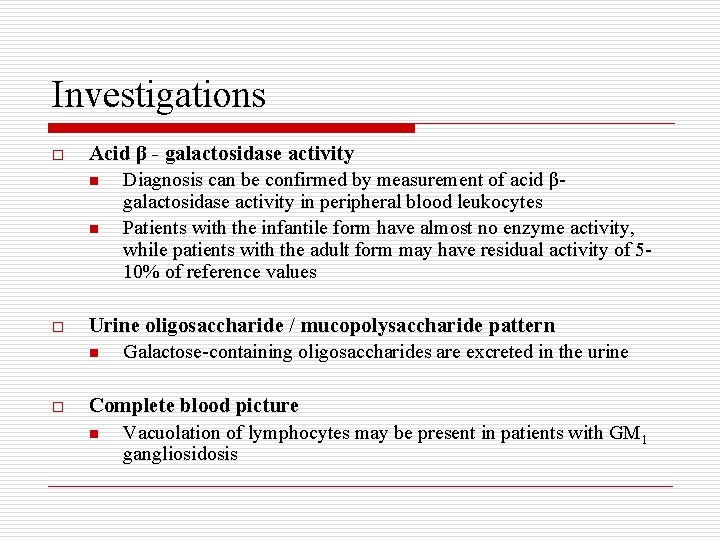
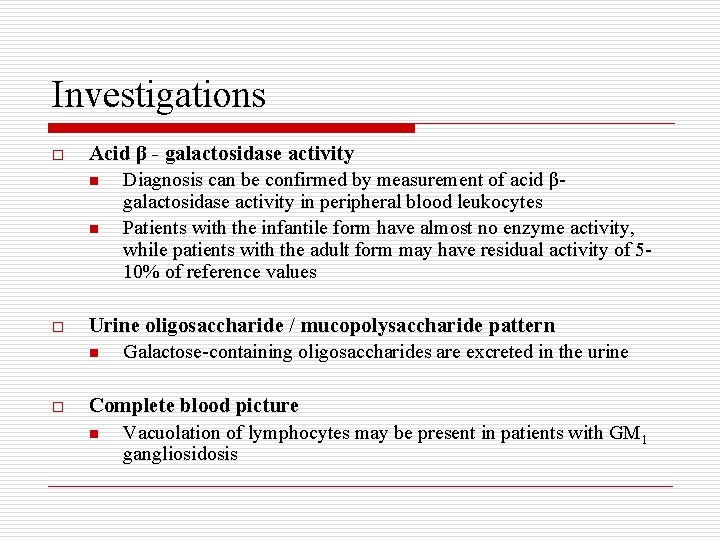
Investigations o Acid β - galactosidase activity n Diagnosis can be confirmed by measurement of acid βgalactosidase activity in peripheral blood leukocytes n Patients with the infantile form have almost no enzyme activity, while patients with the adult form may have residual activity of 510% of reference values o Urine oligosaccharide / mucopolysaccharide pattern n Galactose-containing oligosaccharides are excreted in the urine o Complete blood picture n Vacuolation of lymphocytes may be present in patients with GM 1 gangliosidosis
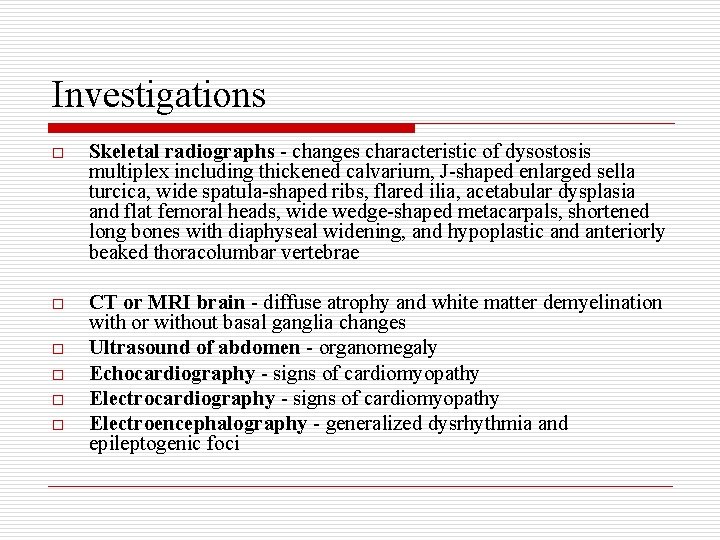
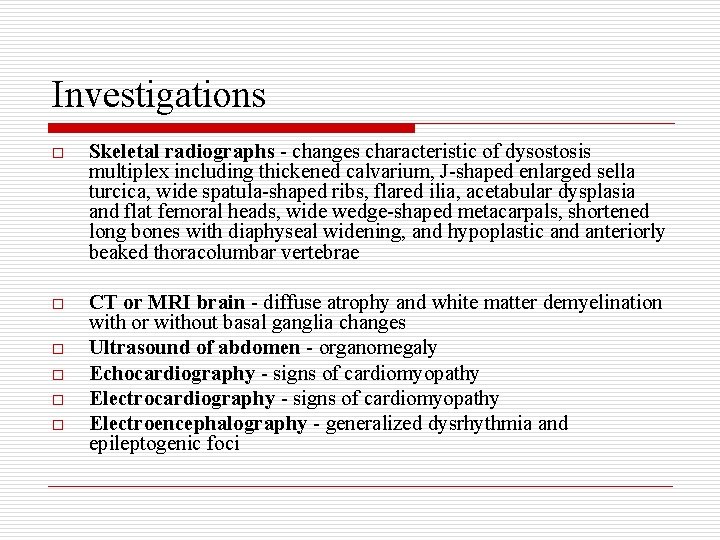
Investigations o Skeletal radiographs - changes characteristic of dysostosis multiplex including thickened calvarium, J-shaped enlarged sella turcica, wide spatula-shaped ribs, flared ilia, acetabular dysplasia and flat femoral heads, wide wedge-shaped metacarpals, shortened long bones with diaphyseal widening, and hypoplastic and anteriorly beaked thoracolumbar vertebrae o CT or MRI brain - diffuse atrophy and white matter demyelination with or without basal ganglia changes Ultrasound of abdomen - organomegaly Echocardiography - signs of cardiomyopathy Electroencephalography - generalized dysrhythmia and epileptogenic foci o o
Treatment o o o o o No effective medical treatment available for the underlying disorder Symptomatic treatment for some neurologic sequelae but not alter the clinical course significantly Active research in the areas of enzyme replacement and gene therapy for GM 1 gangliosidosis Multidisciplinary approach Clinical geneticist - for initial evaluation and diagnosis, to counsel families regarding recurrence risk, and to help provide prenatal testing for future pregnancies Neurologist - for symptomatic therapy of multiple neurologic sequelae Cardiologist - to evaluate for cardiomyopathy Orthopaedic surgeon - to evaluate for dysostosis multiplex Ophthalmologist - to evaluate for ocular stigmata Otolaryngologist and audiologist - to assess for hearing loss
Treatment o Diet n n n o No specific dietary modifications significantly alter the clinical course May require tube feeding to provide adequate intake of energy; however, not change the disease course some families may choose to forgo invasive alimentation procedures Activity n Neurologic and orthopaedic sequelae may preclude adequate physical activity, benefit from physical and occupational therapy
Discussion
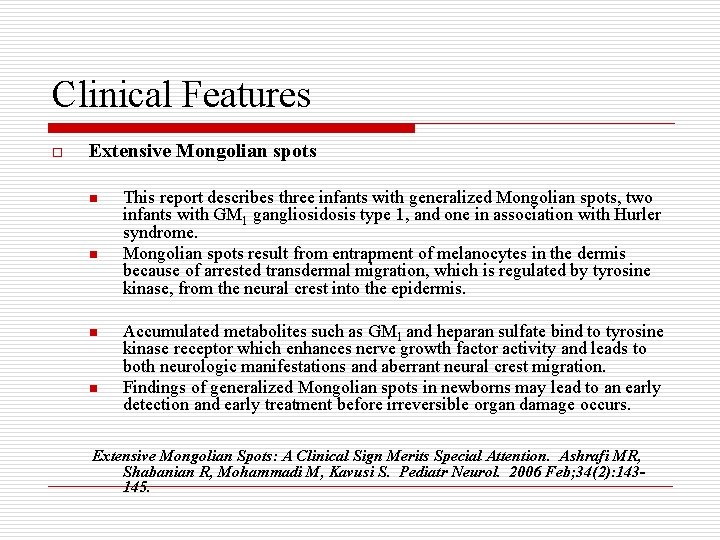
Clinical Features o Extensive Mongolian spots n n This report describes three infants with generalized Mongolian spots, two infants with GM 1 gangliosidosis type 1, and one in association with Hurler syndrome. Mongolian spots result from entrapment of melanocytes in the dermis because of arrested transdermal migration, which is regulated by tyrosine kinase, from the neural crest into the epidermis. Accumulated metabolites such as GM 1 and heparan sulfate bind to tyrosine kinase receptor which enhances nerve growth factor activity and leads to both neurologic manifestations and aberrant neural crest migration. Findings of generalized Mongolian spots in newborns may lead to an early detection and early treatment before irreversible organ damage occurs. Extensive Mongolian Spots: A Clinical Sign Merits Special Attention. Ashrafi MR, Shabanian R, Mohammadi M, Kavusi S. Pediatr Neurol. 2006 Feb; 34(2): 143145.
Clinical Features o Hyperphosphatasemia n Hyperphosphatasemia in infantile GM 1 gangliosidosis: possible association with microscopic bone marrow osteoblastosis. Mogilner BM, Barak Y, Amitay M, Zlotogora J. J Pediatr. 1990 Nov; 117(5): 758 -61. n Hyperphosphatasemia in GM 1 gangliosidosis. Denis R, Wayenberg JL, Vermeulen n Hyperphosphatasemia in early diagnosed infantile GM 1 gangliosidosis presenting as transient hydrops fetalis. Denis R, Wayenberg JL, Vermeulen M, Gorus F, Liebaers I, Vamos E. J Pediatr. 1992 Jan; 120(1): 164. The authors report a case of unsuspected fetal storage disorder initially diagnosed by placental examination performed because of a transient ascites at 28 weeks of gestation. At birth mild dysmorphic features and gradual neurological deterioration were observed. Highly elevated alkaline phosphatase levels were repeatedly noticed. Deficiency of beta galactosidase was documented confirming GM 1 gangliosidosis. Previous reports described the placental pathology after positive prenatal diagnoses of lysosomal diseases. In the present case, the postnatal diagnosis was made in view of the placental pathologic findings. Our observation indicates the need for thorough investigations in hydrops fetalis, in search for metabolic diseases. Gorus F, Gerlo E, Lissens W, Liebaers I, Jauniaux E, Vamos E. Acta Clin Belg.
Treatment o Bone marrow transplantation n Donor bone marrow engraftment, which resulted in complete normalization of white cell β-galactosidase levels in a patient with presymptomatic juvenile onset GM 1 -gangliosidosis, did not improve long-term clinical outcome. n Bone marrow transplantation correcting β-galactosidase activity does not influence neurological outcome in juvenile GM 1 -gangliosidosis. Shield JPH, Stone J, Steward CG. J Inherit Metab Dis. 2005; 28(5): 797 -8.
Thank you



 Keeping an infant safe and well section 7-3
Keeping an infant safe and well section 7-3 Infant reflexes
Infant reflexes Catherine maguire infant mental health
Catherine maguire infant mental health Pallor cyanosis
Pallor cyanosis Kenmore park infant and nursery school
Kenmore park infant and nursery school Infant mortality rate formula
Infant mortality rate formula Keeping an infant safe and well section 7-3
Keeping an infant safe and well section 7-3 Phoenix infant academy
Phoenix infant academy Papoose infant spinal immobilizer
Papoose infant spinal immobilizer Infant industries apush
Infant industries apush Saguaro infant care and preschool
Saguaro infant care and preschool Botulism symptoms
Botulism symptoms Infant death rate
Infant death rate Assessment of pain
Assessment of pain Baby shoes hemingway
Baby shoes hemingway Drdp essential view
Drdp essential view Social impulses foster infant language
Social impulses foster infant language Cpr learning objectives
Cpr learning objectives Femoral pulse infant
Femoral pulse infant Infant mortality rate definition ap human geography
Infant mortality rate definition ap human geography Infant personality development
Infant personality development Infant hip
Infant hip Infant reflexes chart
Infant reflexes chart Infant mortality rate formula
Infant mortality rate formula Primitive reflexes chart
Primitive reflexes chart Walter infant
Walter infant Infant industry
Infant industry Imr equation
Imr equation Neocate formula recall
Neocate formula recall Woolston infant school
Woolston infant school Sparhawk infant and nursery school
Sparhawk infant and nursery school What is sudden infant death syndrome
What is sudden infant death syndrome Pinewood infant school
Pinewood infant school Llf first aid
Llf first aid Infant
Infant Jaundice chart
Jaundice chart Infant-industry argument
Infant-industry argument Social impulses foster infant language
Social impulses foster infant language Dormers wells infant school
Dormers wells infant school Infant development
Infant development Weight gain in infant
Weight gain in infant Infant blood pressure
Infant blood pressure Think pair share example
Think pair share example What is habituation
What is habituation Wood street infant school
Wood street infant school Infant
Infant Basic life support
Basic life support Infant/toddler sensory profile score sheet
Infant/toddler sensory profile score sheet Infant child and adolescent berk 8th edition chapter 1
Infant child and adolescent berk 8th edition chapter 1 Jama 2017
Jama 2017 Growth refers to
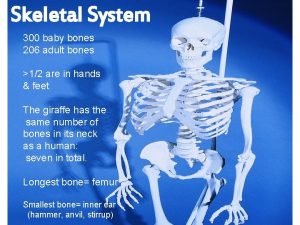
Growth refers to Baby bones vs adult bones
Baby bones vs adult bones