An Atypical RVAD Transport Case Study Lessons Learned



- Slides: 26
An Atypical RVAD Transport Case Study & Lessons Learned from our First Advanced Hemodynamic Support Transport
First Off • Questions? • Comments? • Concerns? • Disclosure – I am the Medical Director for Lifeguard Air emergency Services. I get No direct Financial Compensation and am compensated with clinical shift reductions only.
Objectives • 3 -5 Objectives of Lecture • Target Audience
Background 27 January 2022
Intro • Nov 2017 –Planning for ECMO transport begins • Multiple dry-runs and loading configurations evaluated • Feb 11 th –Called for possible Transport to KAPA • Bedside evaluation and planning for Feb 12 th Transport
The patient
HPI • 2/12/18 63 –yo male UNMH UC Denver • Ground Level Fall 2/7/18 –L Clavicle and L first rib Fx – Incidental Aortic Anuerysm • AVR with aortic anuerysm and dissection s/p repair with LCA and RCA grafting • Intra-OP/Post-OP complications– • • Very difficult repair –tissue paper , ? RCA embolism with sever R-Heart Failure Cardiogenic Shock Multi-Organ Failure Acute Hypoxic Resp Failure – L pleural effusion AKI 2/2 ATN – pre-renal Sepsis Anemia and hemorrhagic shock – GI Bleed

Just a few gtts • Dobutamine 1000 mg/250 ml –– 6. 5 m. Cg/kg/min • Norepinephrine – 16 mg/250 ml – 0. 04 m. Cg/kg/min • Vasopressin – 0. 08 units/ml – 0. 04 units/min • Amiodarone – 360 mg/20 ml – 0. 5 mg/hr • Cisatacurium – 200 mg/200 ml – 0. 5 mg/hr • Midazolam - 100 mg/100 ml – 10 mg/hr • Fentanyl – 1000 m. Cg/100 ml – 125 m. Cg/hr • D 5 -1/2 NS w/ 20 KCl
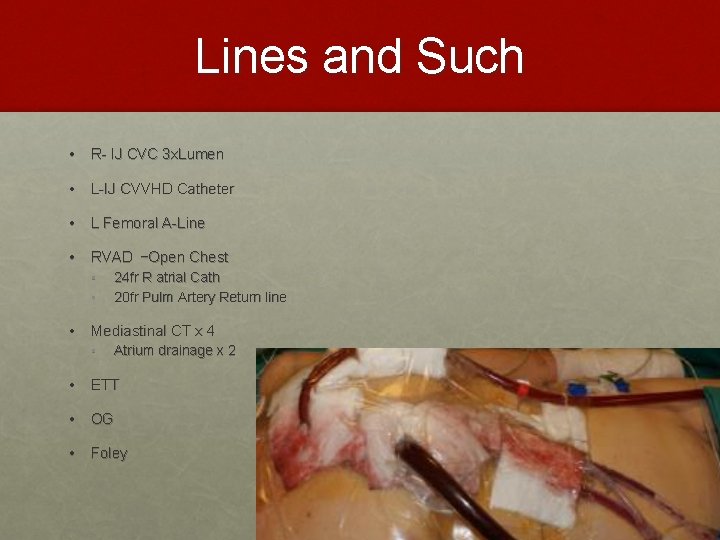
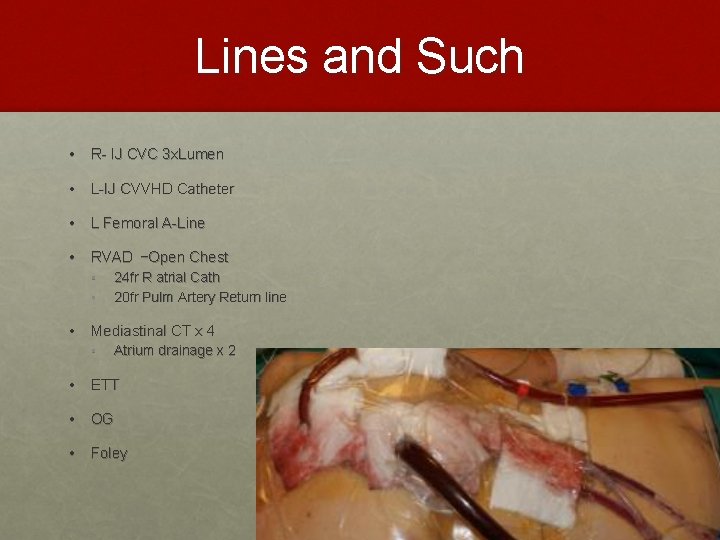
Lines and Such • R- IJ CVC 3 x. Lumen • L-IJ CVVHD Catheter • L Femoral A-Line • RVAD –Open Chest • 24 fr R atrial Cath • 20 fr Pulm Artery Return line • Mediastinal CT x 4 • Atrium drainage x 2 • ETT • OG • Foley
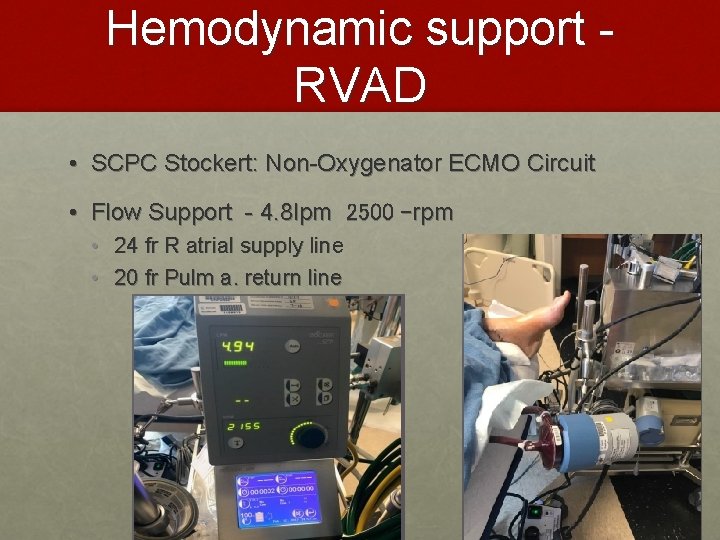
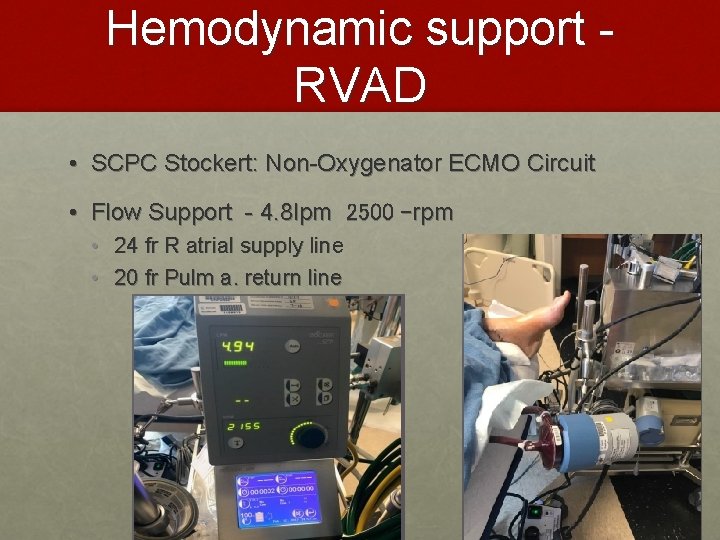
Hemodynamic support RVAD • SCPC Stockert: Non-Oxygenator ECMO Circuit • Flow Support - 4. 8 lpm 2500 –rpm • 24 fr R atrial supply line • 20 fr Pulm a. return line
The team
Intro • All hands on deck! • No less than 15 people at pt bedside! • • All on duty crew CCS Team (contracted perfusion management team) ICU staff Family, Wife • Teams – • Gtts • Monitoring/Vent • Packaging

The transport Team • Lifeguard • • • L. Tafoya, RN, CFRN D. Dixon, MD, FACEP R. Hewitt, Pilot • Perfusion team • B. Sperry, ECMO Perfusionist • T. Dettmer, MD, ED Intensivist • Support Team • Collette, Aaron, Nikki, Donovan, Natalie
Initial logistics • Total time at bedside ~ 75 min • 2 vehicles • Ground amb • Extended cab van
The transport
First phase • Movement from TSI ABQ Sunport • Uneventful • Arrival at Hanger –LG 3 brought in to hangar to prevent exposure • The Wife is going with us? ? • Depart for KAPA • 47 min flight – hemodynamically stable • Not even a blip from the 3 mini-Med Pumps !!!
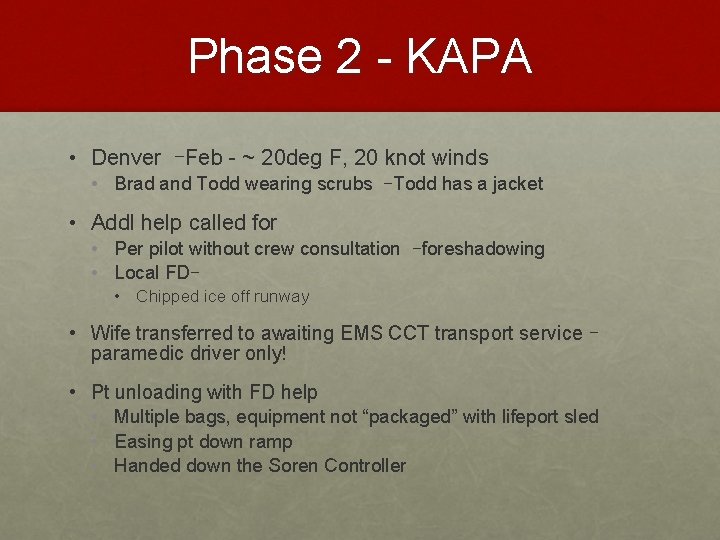
Phase 2 - KAPA • Denver –Feb - ~ 20 deg F, 20 knot winds • Brad and Todd wearing scrubs –Todd has a jacket • Addl help called for • Per pilot without crew consultation –foreshadowing • Local FD– • Chipped ice off runway • Wife transferred to awaiting EMS CCT transport service – paramedic driver only! • Pt unloading with FD help • Multiple bags, equipment not “packaged” with lifeport sled • Easing pt down ramp • Handed down the Soren Controller
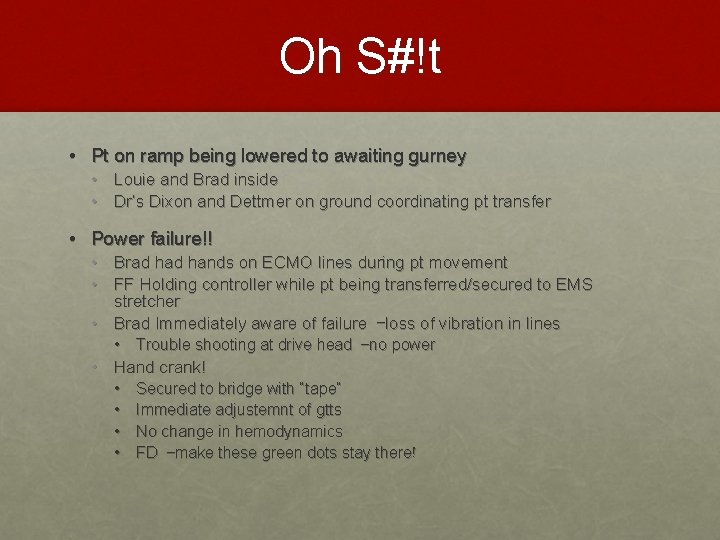
Oh S#!t • Pt on ramp being lowered to awaiting gurney • Louie and Brad inside • Dr’s Dixon and Dettmer on ground coordinating pt transfer • Power failure!! • Brad hands on ECMO lines during pt movement • FF Holding controller while pt being transferred/secured to EMS stretcher • Brad Immediately aware of failure –loss of vibration in lines • Trouble shooting at drive head –no power • Hand crank! • Secured to bridge with “tape” • Immediate adjustemnt of gtts • No change in hemodynamics • FD –make these green dots stay there!
Phase 3 • Soren powered up when plugged in to amb DC power • Back on base systems, hemodynamics stable • Code 3 transport to UC hosp • Cart for the Soren? ? • Slinky effect • Pt Hand-off • Systems compatible so direct transfer of drive head

Lessons Learned
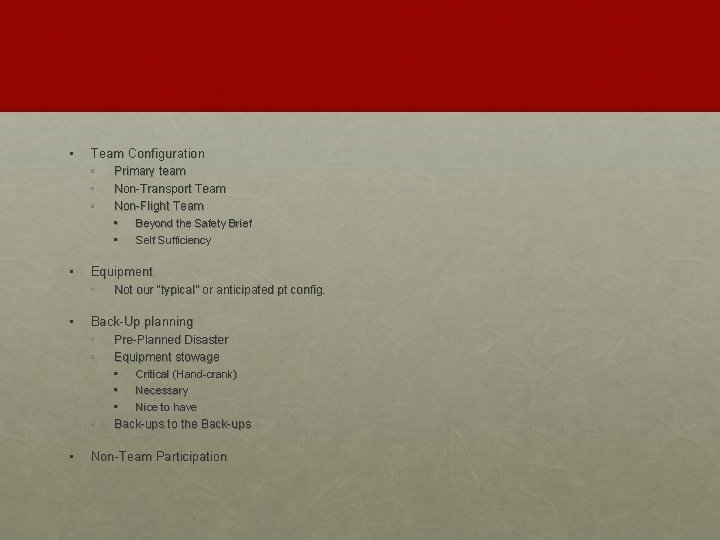
• Team Configuration • Primary team • Non-Transport Team • Non-Flight Team • • Beyond the Safety Brief Self Sufficiency • Equipment • Not our “typical” or anticipated pt config. • Back-Up planning • Pre-Planned Disaster • Equipment stowage • • • Critical (Hand-crank) • Necessary • Nice to have Back-ups to the Back-ups Non-Team Participation
• The Good • PT packaging teamwork and initial load out • The Bad • Critical Failure/Power Loss during critical transition phase • The Ugly • Pt Outcome –Ultimately placed in comfort care and passed away 12 days after transport.
DOD Slide
Questions? • ? ? ?