Amniotic Fluid SON 2122 Chapter 20 hholdorf Outline





- Slides: 63
Amniotic Fluid SON 2122 Chapter 20 hholdorf
Outline Overview Function Physiology Complications Polyhydramnios Oligohydramnios Physiology Amniotic Fluid Index (AFI) Polyhydramnios Oligohydramnios Amniocentesis Misc.
Amniotic Fluid and your food preferences later in life… Food choices during pregnancy and lactation are influenced by a variety of factors. While internal factors, such as cravings and aversions, play an important role especially during the first trimester of pregnancy, environmental factors such as cultural food practices and beliefs often dictate the types of foods eaten throughout pregnancy and lactation.
Such traditional food practices serve to predispose infants to flavors that are characteristic of their mother’s culture and geographical region. Amniotic fluid and human milk are composed of flavors that directly reflect the foods, spices, and beverages eaten by or inhaled by (e. g. , tobacco) the mother. Because the olfactory and taste systems are functioning by the last two trimesters, these flavors are detected early in life, and early experience can bias behavioral response to these flavors later in life.
Although more research is needed to understand the mechanisms involved in early flavor learning, these pre- and early-postnatal flavor exposures likely serve to facilitate the transition from fetal life through the breastfeeding period to the initiation of a varied solid food diet. Such learning is the first, but not the only, way in which children learn to appreciate and prefer the flavors of the foods cherished by their culture.
Physiology and Production In the first trimester it is produced by the fetal kidneys, tissue, and skin. In the second and third trimesters it is primarily produced by fetal urine. Functions are: Cushions the fetus against injury Allows for the free movement of the fetus Essential for the fetal lung development A source of fetal nutrition Aids in maintaining fetal temperature
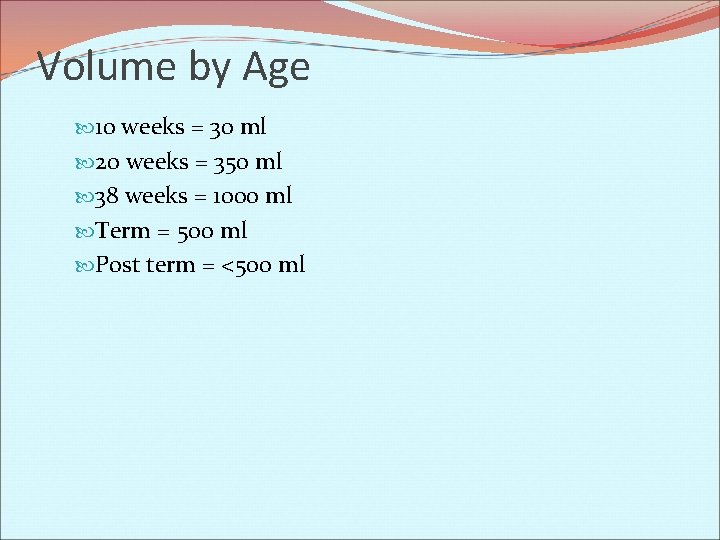
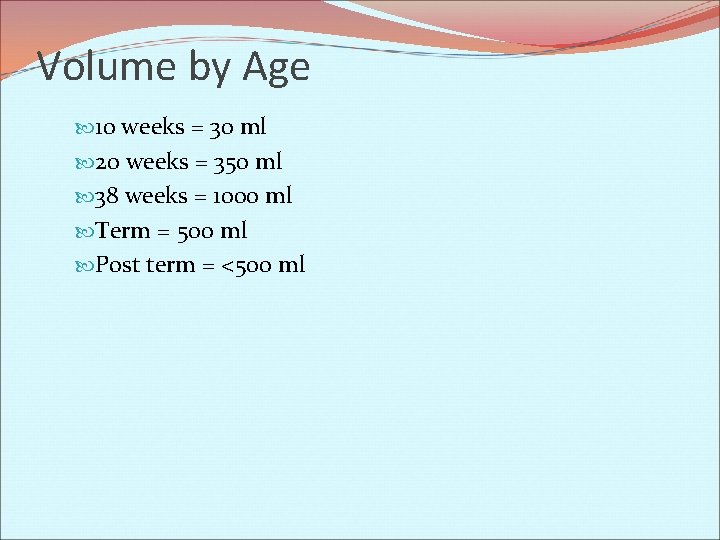
Volume by Age 10 weeks = 30 ml 20 weeks = 350 ml 38 weeks = 1000 ml Term = 500 ml Post term = <500 ml
Amniotic fluid is the nourishing and protecting liquid contained by the amnion of a pregnant woman. The amnion grows and begins to fill, mainly with water, around two weeks after fertilization. After a further 10 weeks the liquid contains proteins, carbohydrates, lipids and phospholipids, urea and electrolytes, all which aid in the growth of the fetus. In the late stages of gestation much of the amniotic fluid consists of fetal urine. The amniotic fluid increases in volume as the fetus grows. The amount of amniotic fluid is greatest at about 34 weeks after conception or 34 weeks (gestational age). At 34 weeks the amount of amniotic fluid is about 800 ml. This amount reduces to about 600 ml at 40 weeks when the baby is born.
Amniotic fluid is continually being swallowed and "inhaled" and replaced through being "exhaled", as well as being urinated by the baby. It is essential that the amniotic fluid be breathed into the lungs by the fetus in order for the lungs to develop normally. Swallowed amniotic fluid contributes to the formation of meconium. Analysis of amniotic fluid via the amniocentesis procedure, can reveal many aspects of the baby's genetic health. This is because the fluid also contains fetal cells which can be examined for genetic defects. Amniotic fluid also protects the developing baby by cushioning against blows to the mother's abdomen, allows for easier fetal movement, promotes muscular/skeletal development, and helps protect the fetus from heat loss. The fluid is released when the amnion ruptures, commonly known as when a woman's "water breaks". When this occurs during labour at term, it is known as "spontaneous rupture of membranes" (SROM). If the rupture precedes labour at term, however, it is referred to as "premature rupture of membranes" (PROM).
Complications Too little amniotic fluid (oligohydramnios) or too much (polyhydramnios or hydramnios) can be a cause or an indicator of problems for the mother and baby. In both cases the majority of pregnancies proceed normally and the baby is born healthy but this isn't always the case. Babies with too little amniotic fluid can develop contractures of the limbs, clubbing of the feet and hands, and also develop a life threatening condition called hypoplastic lungs. If a baby is born with hypoplastic lungs, which are small underdeveloped lungs, this condition is potentially fatal and the baby can die shortly after birth. Oligohydramnios can be caused by infection, kidney dysfunction or malformation (since much of the late amniotic fluid volume is urine), Oligohydramnios can sometimes be treated with bed rest, oral and intravenous hydration, antibiotics, steroids, and amnio-infusion.
Polyhydramnios is a predisposing risk factor for cord prolapse and is sometimes a side effect of a macrosomic pregnancy. Hydramnios is associated with esophageal atresia. Amniotic fluid is primarily produced by the mother until 16 weeks of gestation. Preterm premature rupture of membranes (PPROM) is a condition where the amniotic sac leaks fluid before 38 weeks of gestation. This can be caused by a bacterial infection or by a defect in the structure of the amniotic sac, uterus, or cervix. In some cases, the leak can spontaneously heal, but in most cases of PPROM, labor begins within 48 hours of membrane rupture. When this occurs, it is necessary that the mother receive treatment to avoid possible infection in the newborn.
Polyhydramnios) is the medical condition of too much amniotic fluid in the amniotic sac. It is seen in 0. 5 to 2% of pregnancies. The opposite to polyhydramnios is oligohydramnios, a deficiency in amniotic fluid.
Causes A single case of polyhydramnios may have one or more causes. About 20% of cases are due to maternal diabetes, which causes hyperglycemia of the fetus, hence fetal polyuria (fetal urine is a major source of amniotic fluid). About another 20% of cases are associated with fetal anomalies that impair the ability of the fetus to swallow (the fetus normally swallows the amniotic fluid). These anomalies includes: gastrointestinal abnormalities such as esophageal atresia, duodenal atresia, and tracheoesophageal fistula chromosomal abnormalities such as Down's syndrome and Edwards Syndrome (which is itself often associated with GI abnormalities) neurological abnormalities such as anencephaly, which impair the swallowing reflex In a multiple gestation pregnancy, the cause of polyhydramnios usually is twin-twin transfusion syndrome
Associated conditions Fetuses with polyhydramnios are at risk for a number of other problems including cord prolapse, placental abruption and perinatal death. At delivery the baby should be checked for congenital abnormalities. Treatment In some cases, amnioreduction has been used in response to polyhydramnios.
Amniotic Fluid Is the nourishing and protecting liquid contained by the amnion Serves a number of important functions in the normal development of the embryo & fetus Cushions the fetus against physical trauma Allows for fetal growth free from restrictions Provides a thermally stable environment Allows for normal development of respiratory & gastrointestinal tracts & musculoskeletal system Helps prevent infection Provides short term source of fluid & nutrients to developing embryo
Fluid Production The amnion grows and begins to fill, mainly with water, around 2 weeks after fertilization Chorioamnion acts as a molecular sieve, allowing for free passage Also contains solutes, electrolytes, creatine, and urea In late stages of gestation, two primary sources of fluid are fetal kidneys and lungs
Fluid Removal Primary sources of removal Gastrointestinal tract (swallowing) It is essential that the fluid be breathed into the lungs by the fetus for normal lung development Contributes to formation of meconium Absorption into fetal blood perfusing the surface of the placenta
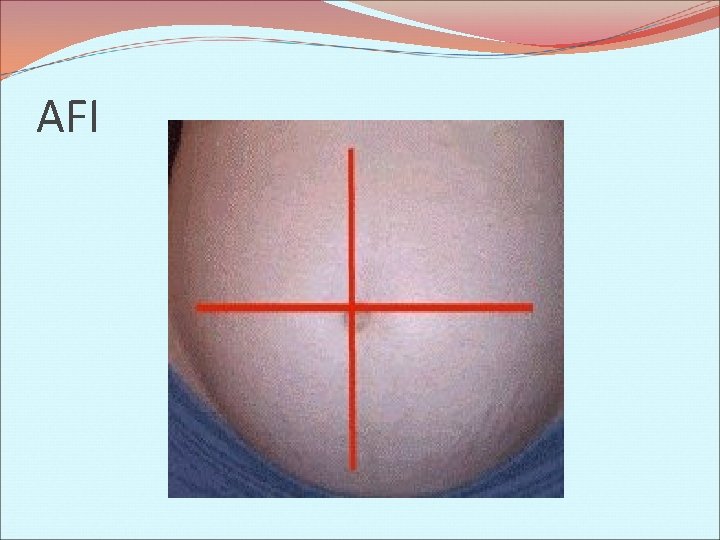
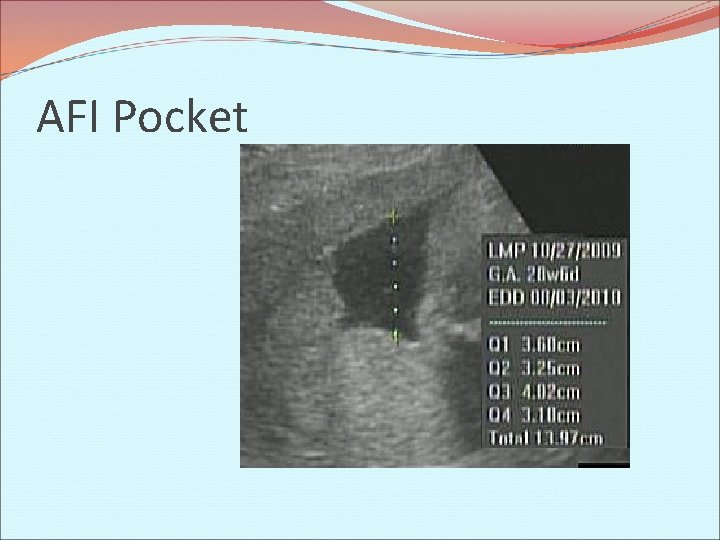
Amniotic Fluid Index Largest vertical measurements are taken each of the four quadrants & summed Normal AFI= 5 -25 cm AF ↑ in volume as fetus grows The amount of AF is greatest at about 34 weeks (800 ml) The AF reduces to about 600 ml at 40 weeks when the baby is born
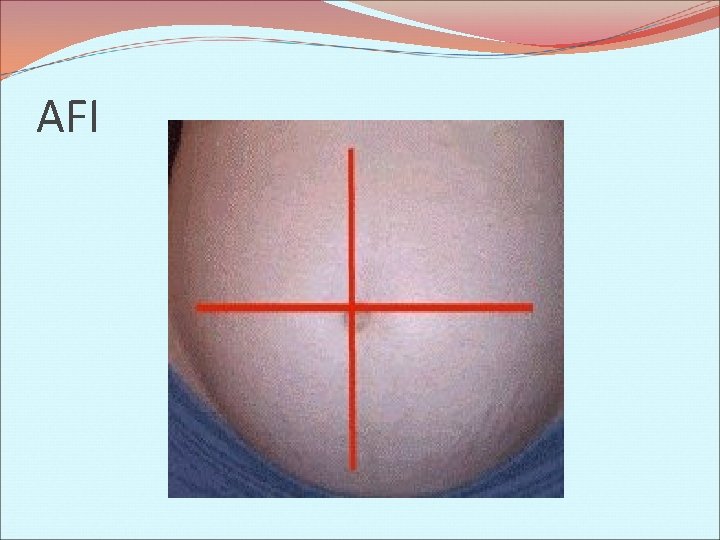
AFI
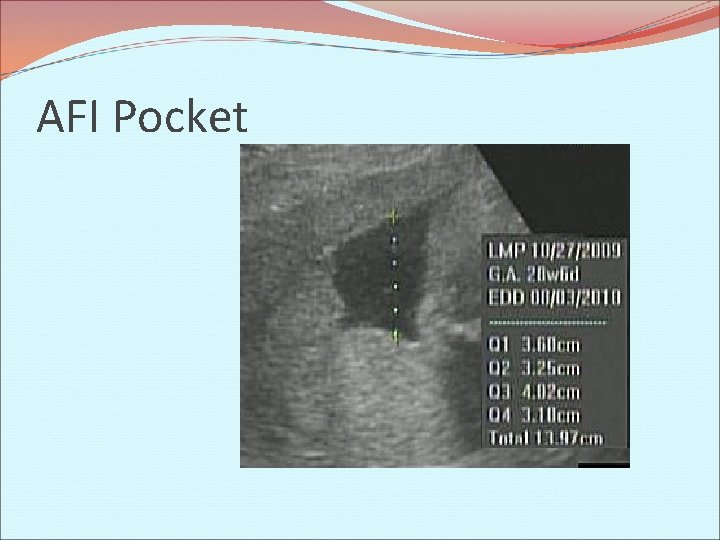
AFI Pocket
Amniotic Fluid Index- In Multiples A single vertical measurement is taken in each of the sacs Measurement < 5 ml = Oligohydramnios Measurement > 8 ml = Polyhydramnios Applies only in diamniotic twins
Amniotic Fluid Index (AFI) is a measure of the amount of amniotic fluid and is an index for the fetal wellbeing. It is a part of the Biophysical profile. AFI is the score given to the amount of amniotic fluid (by adding up centimeters of depth of four pockets of fluid) seen on pregnant uterus by ultrasound. An AFI < 5 -6 is considered as Oligohydramnios and an AFI > 18 -22 is considered as Polyhydramnios.
AFI / Amniotic fluid index Measurements are taken in each of four uterine quadrants, and the greatest vertical measurements are summed. A progressive increase in the AFI is noted until approx. 28 weeks. After that, the AFI slowing decreases. NML = 5 -22 cm
Complications- Oligohydramnios Abnormal decrease in amniotic fluid AFI measuring < 5 ml Causes: Urinary tract abnormalities (renal agenesis, bilateral renal obstruction, bilateral renal dysplasia, & posterior urethral valves or atresia) Prerenal abnormalities (uteroplacental insufficiency leading to IUGR, PROM, & post-term pregnancy)
Complications- Oligohydramnios Risks frequently associated with Oligo: Compression of fetal organs resulting in birth defects Increased chance of miscarriage or stillbirth IUGR Preterm Birth Labor complications such as cord compression, meconium stained fluid and cesarean delivery Treatment Close monitoring Amnionfusion Delivery
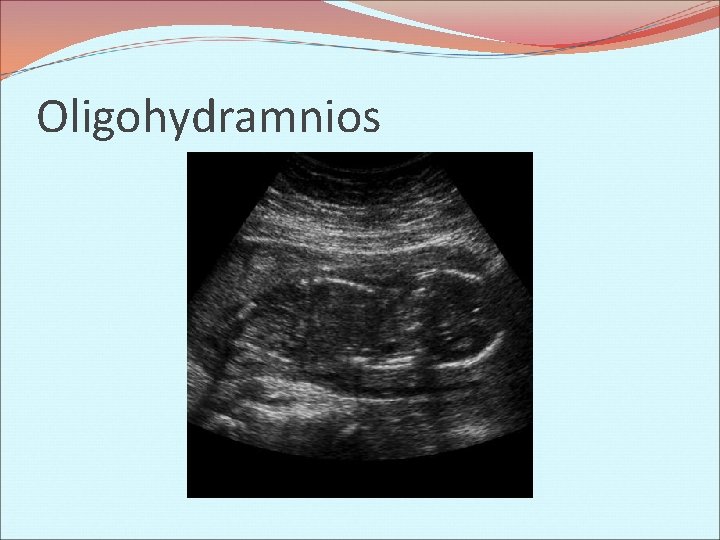
Oligohydramnios
Oligohydramnios Abnormally decreased amount of amniotic fluid. When Oligohydramnios occurs…think DRIPP (Demise, Renal Abnormalities, IUGR, PROM, Post Dates, and Pre -Eclampsia/Eclampsia)
Complications- Polyhydramnios Abnormal increase in amniotic fluid AFI measuring >25 ml Seen in 0. 5 to 2% of pregnancies Causes: Maternal causes Intrinsic or extrinsic obstruction of the gastrointestinal tract Neurologic and neuromuscular problems impairing swallowing Fetal polyuria High-output congestive cardiac failure Congenital infection Idiopathic causes Skeletal dysplasias and syndrome
Complications- Polyhydramnios Associated with: Neural tube defects GI obstructive anomalies Hydrops Trisomy 18 Cystic hygroma Placental abnormalities Twin to twin transfusion Treatment Medication Amniocentesis Induction of labor

Polyhydramnios

Polyhydramnios Abnormally increased amount of amniotic fluid. Frequently the primary sign of an underlying fetal disorder Associated with Fetal neural tube defects Upper GI tract obstructions Fetal Hydrops Trisomy 18 (usually due to esophageal atresia) Cystic Hygroma Placental abnormalities Twin-twin transfusion syndrome Others
Amniocentesis Medical procedure used in prenatal diagnosis of genetic abnormalities and fetal infections A small amount of amniotic fluid, containing fetal tissues, is extracted from the amnion with the use of a needle Local anesthetic is used & needle is inserted thru the abdominal wall or vagina
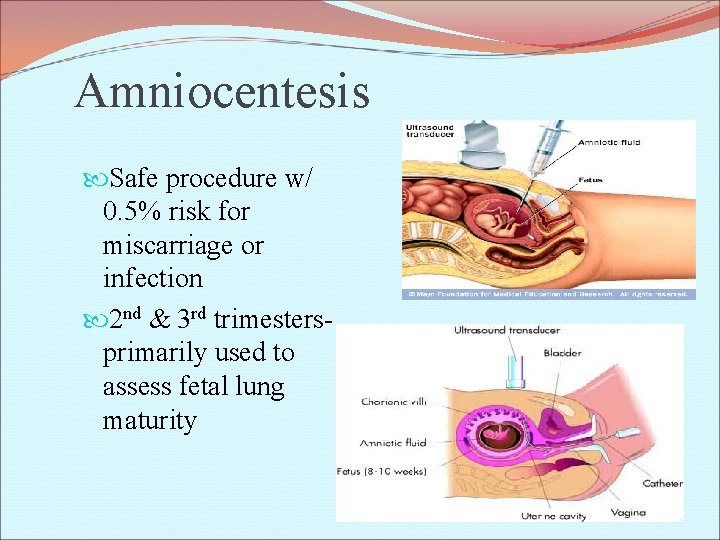
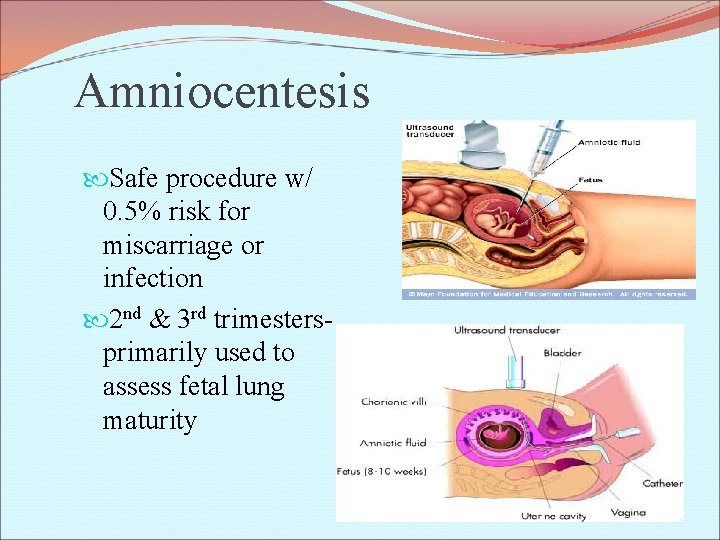
Amniocentesis Safe procedure w/ 0. 5% risk for miscarriage or infection 2 nd & 3 rd trimestersprimarily used to assess fetal lung maturity
Amniocentesis- Risks Failure of puncture to heal properly: Result in leakage & infection Serious complication- miscarriage Other complications: Preterm labor & delivery Respiratory distress Postural deformities Fetal trauma Rhesus disease
Amniocentesis (also referred to as amniotic fluid test or AFT), is a medical procedure used in prenatal diagnosis of genetic abnormalities and fetal infections, in which a small amount of amniotic fluid, which contains fetal tissues, is extracted from the amnion or amniotic sac surrounding a developing fetus, and the fetal DNA is examined for genetic abnormalities.
Procedure: Before the actual procedure, a local anesthetic is sometimes given to relieve the pain when inserting the needle used to withdraw the fluid. A needle is usually inserted through the mother's abdominal wall and through the wall of the uterus into the amniotic sac. With assistance from ultrasound, a physician aims towards an area of the sac that is away from the fetus and extracts a small amount of amniotic fluid for testing. The puncture heals, and the amniotic sac replenishes the liquid over a day or so. After the amniotic fluid is extracted, the fetal cells are separated from it using a centrifuge, and the fetal chromosomes are examined for abnormalities.
Various genetic testing may be performed, but the three most common abnormalities tested for are Down's syndrome, Trisomy 18 and spina bifida. Amniocentesis can be performed as soon as sufficient amniotic fluid surrounds the fetus to allow a sample to be recovered relatively safely, usually no earlier than the 14 th week of pregnancy. Often, genetic counseling is offered in conjunction with amniocentesis.
In addition to the fetal cells, some tests may examine the amniotic fluid for indications of non-genetic diseases the fetus might have. Levels of chemical substances such as alpha-fetoprotein can be measured to detect other health problems such as hydrocephalus. A side benefit of genetic analysis through amniocentesis is that the sex of the fetus may be determined with 100% accuracy.
Risks Although the procedure is routine, possible complications include infection of the amniotic sac from the needle, and failure of the puncture to heal properly, which can result in leakage or infection. Serious complications can result in miscarriage. Other possible complications include preterm labor and delivery, respiratory distress, postural deformities, and fetal trauma.
The risk of amniocentesis-related miscarriage is generally thought to be 1 in 200, although a recent study has indicated this may actually be much lower, perhaps 1 in 1, 600. In contrast, the risk of miscarriage for CVS is believed to be approximately 1 in 100, although CVS may be done up to four weeks earlier, and may be preferable if the possibility of genetic defects is thought to be higher.
Misc. Intrauterine growth restriction Post-term patients Pulmonary hypoplasia
IUGR Intrauterine growth restriction (IUGR) refers to a condition in which an unborn fetus is smaller than it should be because it is not growing at a normal rate inside the womb IUGR has many possible causes. A common cause is a problem with the placenta. The condition can also occur as the result of certain health problems in the mother, such as: Advanced diabetes High blood pressure or heart disease Infections such as rubella cytomegalovirus, toxoplasmosis, and syphilis Kidney disease or lung disease
Post Term Patients Fetal and Neonatal Risks 1. Reduced placental perfusion—Once a pregnancy has surpassed the 40 week gestation period, doctors closely monitor the mother for signs of placental deterioration. Towards the end of pregnancy calcium is deposited on the walls of blood vessels and proteins are deposited on the surface of the placenta, which changes the placenta. This limits the blood flow through the placenta and ultimately leads to placental insufficiency and the baby is no longer properly nourished. Induced labor is strongly encouraged if this happens. 2. Oligohydramnios 3. Meconium aspiration
Pulmonary Hypoplasia Pulmonary hypoplasia is incomplete development of the lungs, resulting in an abnormally low number or size of bronchopulmonary segments or alveoli. A congenital malformation, it most often occurs secondary to other fetal abnormalities that interfere with normal development of the lungs. Oligohydramnios can prevent the normal development of the lungs. Primary (idiopathic) pulmonary hypoplasia is rare and usually not associated with other maternal or fetal abnormalities.
Think Tank – Amniotic Fluid
Question One In the first trimester, Amniotic fluid is produced by the fetal _______, and _______ In the second and third trimesters it is primarily produced by fetal ______
Question two List three functions of the amniotic fluid.
Question three The amniotic fluid increases in volume as the fetus grows. The amount of amniotic fluid is greatest at about ___weeks
Question four Define oligohydramnios
Question five Define polyhydramnios

Question six List several causes of oligohydramnios
Question seven Amniotic fluid is primarily produced by the mother until ____weeks of gestation
Question Eight List several causes of polyhydramnios
Question nine The two Primary sources of amniotic removal are…
Question ten What is the range for a normal Amniotic Fluid Index (AFI)?

Question eleven How is the AFI obtained? How do you obtain an AFI?
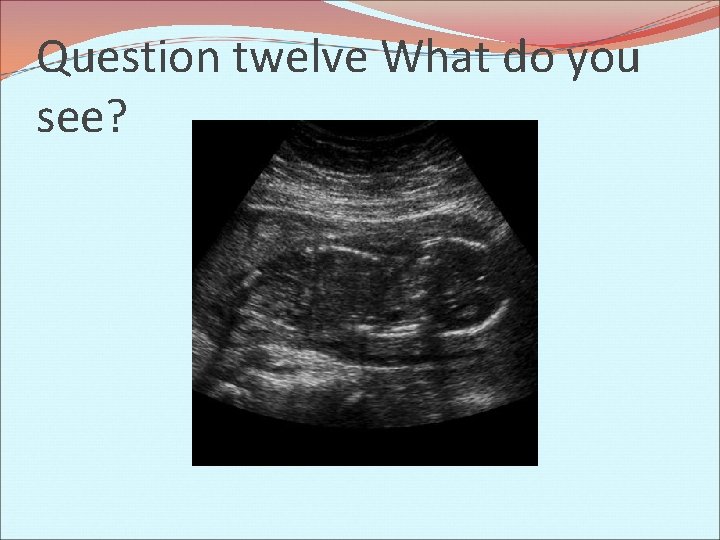
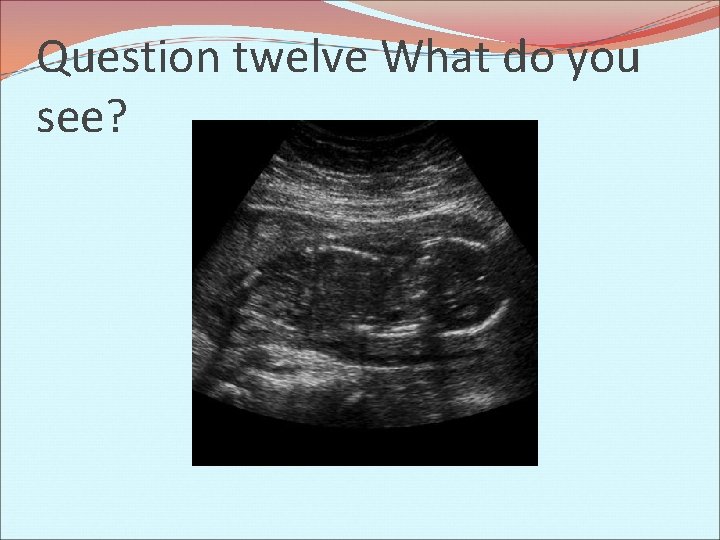
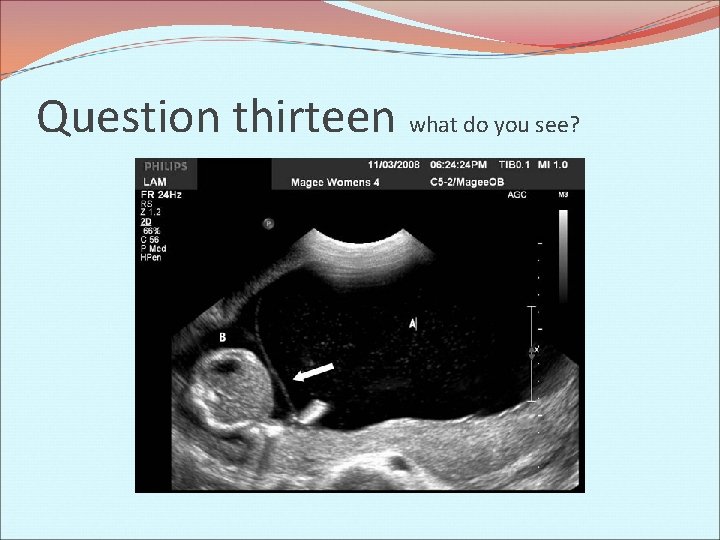
Question twelve What do you see?
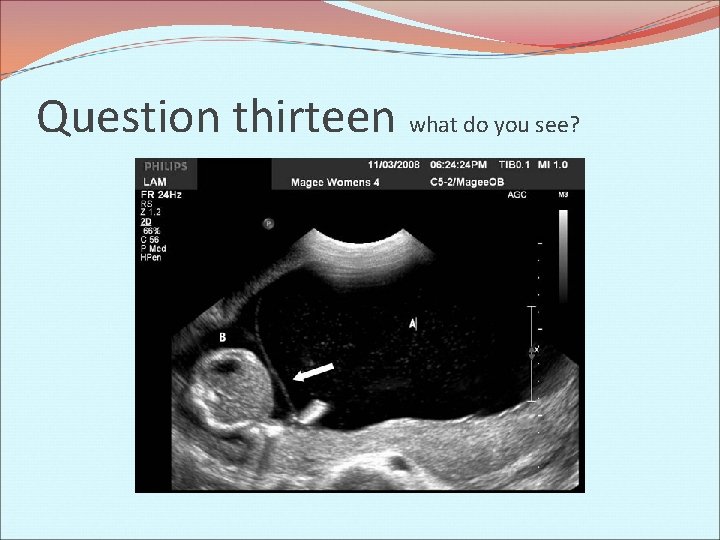
Question thirteen what do you see?
Question fourteen Why would an Amniocentesis be performed? What is its purpose?
Question fifteen Are there any risk factors associated with an Amniocentesis? Explain.

Question Sixteen Extra Credit Genius or stupid?
 Fy 2122
Fy 2122 What is amniotic fluid embolism
What is amniotic fluid embolism Amniotic fluid color
Amniotic fluid color Normal amniotic fluid
Normal amniotic fluid Polyhydramnios causes
Polyhydramnios causes Amniotic fluid color
Amniotic fluid color Color of amniotic fluid
Color of amniotic fluid Placenta marginata
Placenta marginata Amniotic fluid embolism
Amniotic fluid embolism Olygohydramnios
Olygohydramnios Liquor in pregnancy
Liquor in pregnancy Preterm classification
Preterm classification Labor induction methods
Labor induction methods Sources of amniotic fluid
Sources of amniotic fluid Sources of amniotic fluid
Sources of amniotic fluid How much amniotic fluid is normal
How much amniotic fluid is normal Fluid sf
Fluid sf Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Total body water
Total body water Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Hypoosmotic
Hypoosmotic Timeline in fluid mechanics
Timeline in fluid mechanics Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Ascitic fluid neutrophil count
Ascitic fluid neutrophil count Amniotic eggs
Amniotic eggs Stage development
Stage development Amniotic cavity
Amniotic cavity Chorion
Chorion Amniotic cavity
Amniotic cavity Amniotic cavity and yolk sac
Amniotic cavity and yolk sac Quote sandwich format
Quote sandwich format Specific weight unit
Specific weight unit Chapter 8 fluid mechanics
Chapter 8 fluid mechanics Chapter 9 vehicle maintenance
Chapter 9 vehicle maintenance Fluid mechanics chapter 3
Fluid mechanics chapter 3 U tube manometer formula
U tube manometer formula Chapter 26 fluid electrolyte and acid-base balance
Chapter 26 fluid electrolyte and acid-base balance Fluid mechanics chapter 8 solutions
Fluid mechanics chapter 8 solutions Diet care logo
Diet care logo Chapter 25 fluid electrolyte and acid-base balance
Chapter 25 fluid electrolyte and acid-base balance Normal electrolytes values
Normal electrolytes values A repetition of or return to criminal behavior *
A repetition of or return to criminal behavior * Romans outline by chapter
Romans outline by chapter Research proposal components
Research proposal components Foner chapter 27
Foner chapter 27 Methodology chapter outline
Methodology chapter outline Chapter 38 a world without borders outline
Chapter 38 a world without borders outline Vbscript
Vbscript Hunger games chapter 27
Hunger games chapter 27 Chapter 31 societies at crossroads
Chapter 31 societies at crossroads General hero
General hero Chapter 2 learning goals outline sociology answers
Chapter 2 learning goals outline sociology answers Chapter 1 outline
Chapter 1 outline Chapter 1 outline
Chapter 1 outline Chapter 30
Chapter 30 Chapter 2 outline
Chapter 2 outline Outline book of acts
Outline book of acts Government spending multiplier
Government spending multiplier 24 chapter outline
24 chapter outline Apush chapter 16 conquering a continent outline
Apush chapter 16 conquering a continent outline Sustantivo primitivo ejemplos
Sustantivo primitivo ejemplos Colombia ______ next to paraguay
Colombia ______ next to paraguay Texto de cenicienta
Texto de cenicienta