Amniotic fluid is found around the developing fetus

- Slides: 22
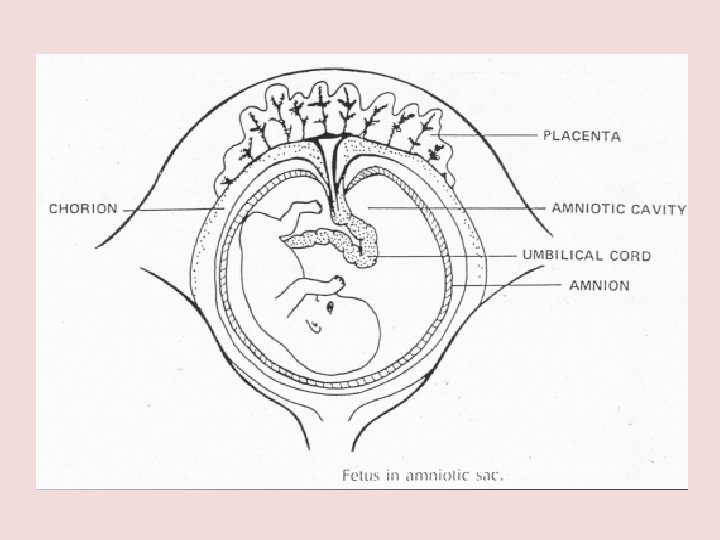
Amniotic fluid is found around the developing fetus, inside a membraneous sac, called amnion
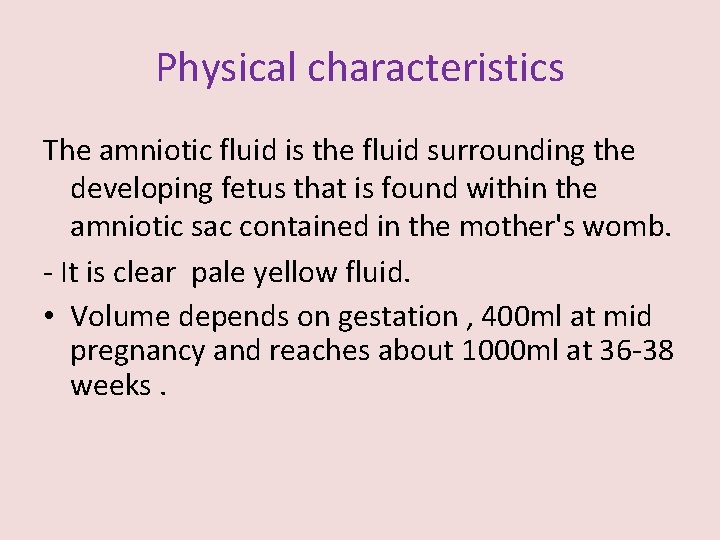
Physical characteristics The amniotic fluid is the fluid surrounding the developing fetus that is found within the amniotic sac contained in the mother's womb. - It is clear pale yellow fluid. • Volume depends on gestation , 400 ml at mid pregnancy and reaches about 1000 ml at 36 -38 weeks.
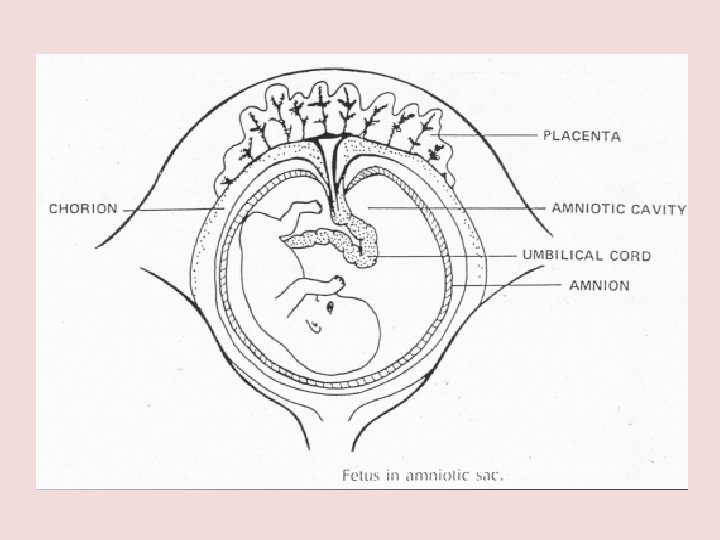
- Amniotic fluid is found around the developing fetus, inside a membraneous sac, called amnion -Amniotic fluid immediately begins to fill the sac. In the early weeks of pregnancy, amniotic fluid consists mainly of water supplied by the mother. After about 20 weeks, fetal urine makes up most of the fluid. - Amniotic fluid also contains nutrients, hormones and disease-fighting antibodies
Amniotic fluid function • This fluid protects the developing fetus. • Serves a key role in the exchange of water and molecules between the fetus and the maternal circulation. • It helps the developing fetus to move in the womb, which allows for proper bone growth and muscle development. Helps prevent compression of the umbilical cord. • Contains Ig that also help in fighting pathogens.
Amniotic Fluid composition The composition of the amniotic fluid changes with gestation in early pregnancy it is similar to maternal and fetal serum. - 98 -99% of the amniotic fluid is water. - A large number of dissolved substances such as creatinine, urea, bile pigments , renin, glucose , fructose, proteins (albumin and globulin) lipids, hormones(estrogen and progestrone ), enzymes , minerals (Na+ , K+ Cl- ) . - Suspended in it are some undissolved material such as some fetal epithelial cells
The amount of amniotic fluid increases until 28 to 32 weeks of pregnancy. After that time, the level of fluid generally stays constant until the baby is full term (37 to 40 weeks), when the level begins to decline. In some pregnancies, however, there may be too little or too much amniotic fluid. • Having too little amniotic fluid is called: oligohydramnios. • Having too much amniotic fluid is called: polyhydramnios
oligohydramnios • About 4% of pregnant women have oligohydramnios. • It can develop at any time during pregnancy, although it is most common in the last trimester. • 12 percent of women whose pregnancies last about two weeks beyond their due dates (42 weeks gestation) develop oligohydramnios, because the level of amniotic fluid tends to decrease by that time in gestation
Does oligohydramnios pose risks to mother or baby? • The problems associated with oligohydramnios differ depending on the stage of the pregnancy. • Oligohydramnios is more likely to have serious consequences if it occurs in the first half of pregnancy than if it occurs in the last trimester. These consequences include : • Birth defects (too little amniotic fluid early in pregnancy can lead to compression of fetal organs, resulting in lung and limb defects) • Miscarriage • Premature birth • Stillbirth
• When oligohydramnios occurs in the second half of pregnancy, it may be associated with poor fetal growth. Near term, oligohydramnios may increase the risk of complications of labor and delivery, including compression of the umbilical cord. Ø This can deprive the baby of oxygen, sometimes resulting in stillbirth. Women with oligohydramnios are more likely than unaffected women to need a cesarean section.
polyhydramnios • About 1 percent of pregnant women have too much amniotic fluid. • Most cases are minor and result from a gradual build up of excess fluid in the second half of pregnancy. • However, a small number of women have a rapid build up of fluid occurring as early as 16 weeks of pregnancy that usually results in very early delivery
What complications can polyhydramnios cause for mother and baby? v Polyhydramnios may increase the risk of pregnancy complications including : • Premature delivery • Placental abruption (the placenta partially or completely peels away from the uterine wall before delivery) • Stillbirth • Postpartum hemorrhage (severe bleeding after delivery) • Fetal malposition (the baby is not lying in a head-down position and may need to be delivered by cesarean section)

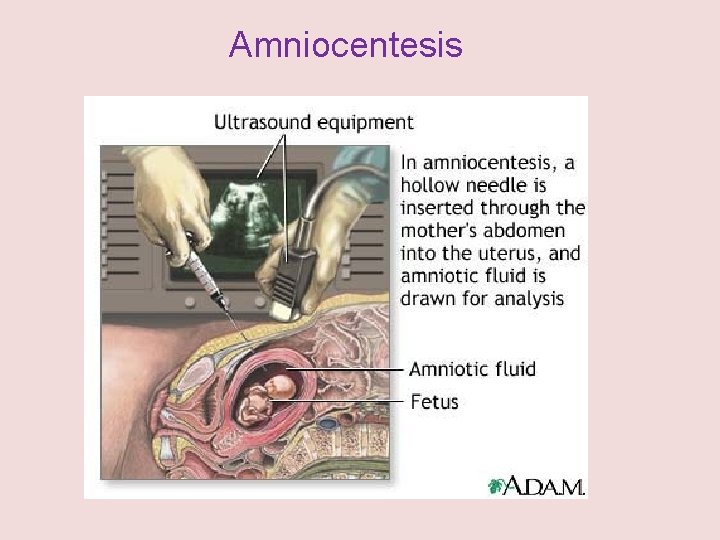
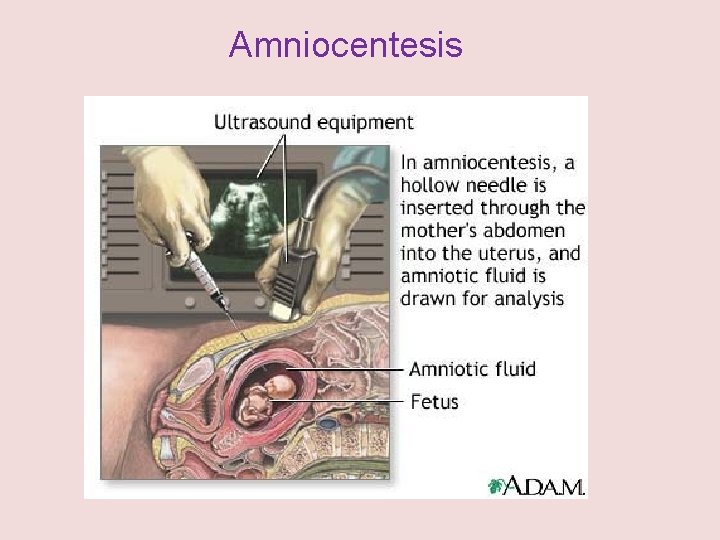
Amniocentesis
• Amniocentesis is used to determine the health of an unborn baby. • Amniotic fluid contains cells that are normally shed from the fetus. Samples of these cells are obtained by withdrawing some amniotic fluid.
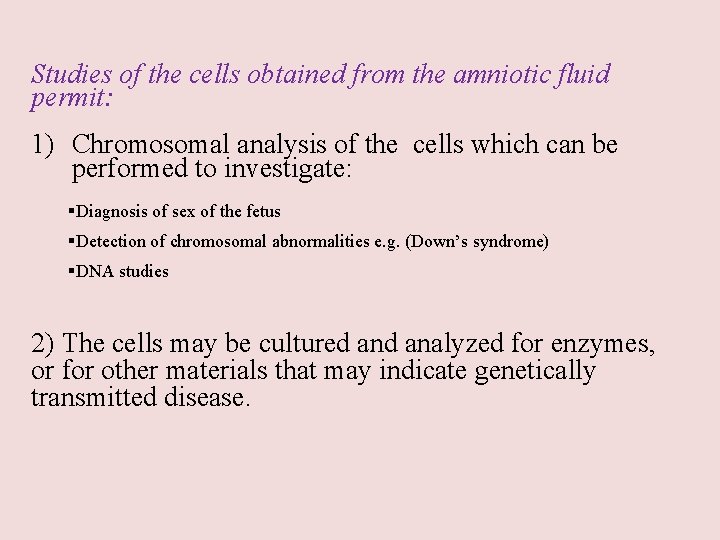
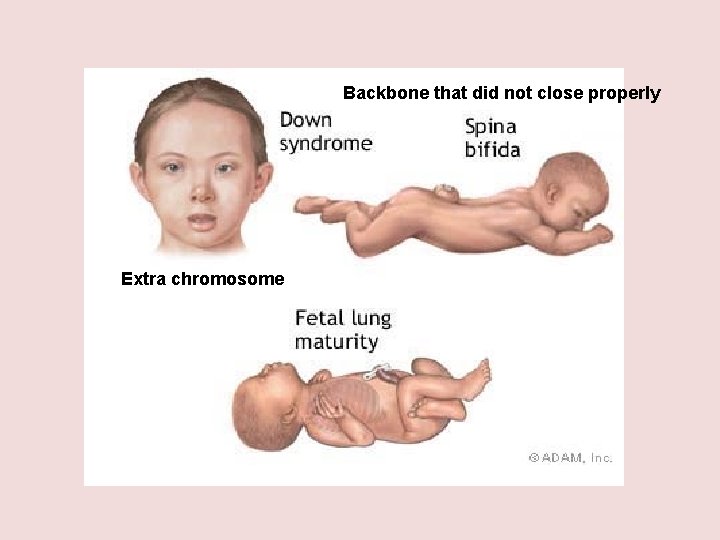
Studies of the cells obtained from the amniotic fluid permit: 1) Chromosomal analysis of the cells which can be performed to investigate: §Diagnosis of sex of the fetus §Detection of chromosomal abnormalities e. g. (Down’s syndrome) §DNA studies 2) The cells may be cultured analyzed for enzymes, or for other materials that may indicate genetically transmitted disease.
Who is indicated amniocentesis? - That the pregnancy is 35 years or more. - Family history of genetic alterations
When we will have an amniocentesis? Usually made between 15 to 18 weeks, reaching even to 11 or 12. What are the risks of amniocentesis? - Abortion: about 1 in 200 to 400 women aborted (higher risk if done in the first quarter) - Uterine infection: 1 in 1000
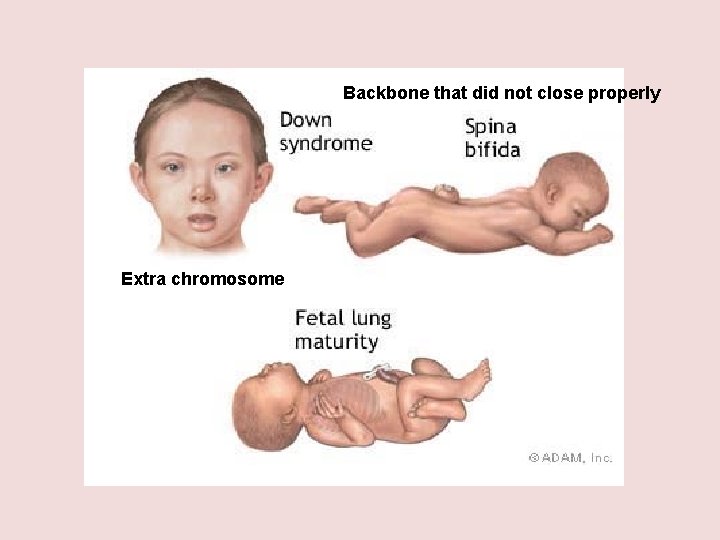
Backbone that did not close properly Extra chromosome
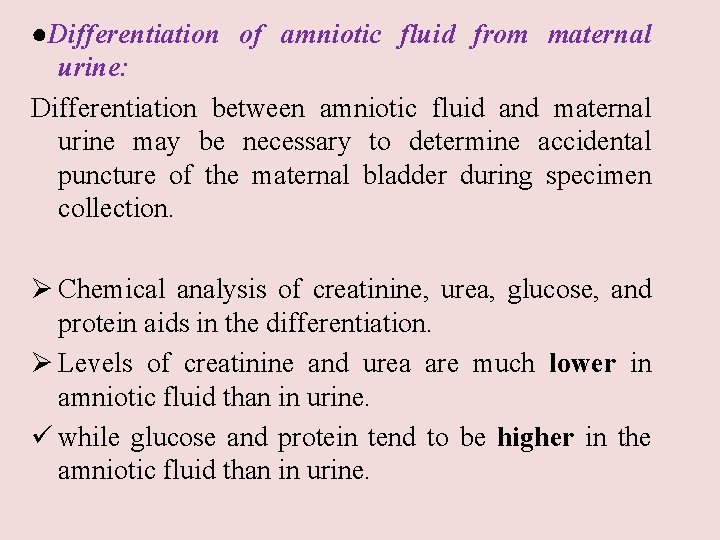
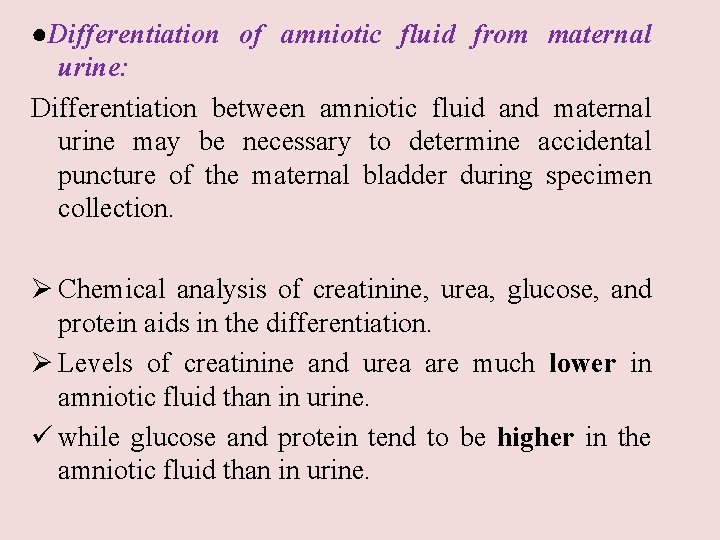
●Differentiation of amniotic fluid from maternal urine: Differentiation between amniotic fluid and maternal urine may be necessary to determine accidental puncture of the maternal bladder during specimen collection. Ø Chemical analysis of creatinine, urea, glucose, and protein aids in the differentiation. Ø Levels of creatinine and urea are much lower in amniotic fluid than in urine. ü while glucose and protein tend to be higher in the amniotic fluid than in urine.
Fetal lung maturity test: Lecithin – sphingomyelin ratio: Measurment of the lecithine/sphingomyelin ratio. - This test is done to assess the maturation of the fetal lungs. - A lecithin- sphingomyelin ratio of 2 or greater is associated with fetal pulmonary system maturity.
Fetal distress testing: - Erythroblastosis fetalis is caused when mother develops antibodies to an antigen on the fetal erythrocytes and these antibodies cross the placenta to destroy many fetal RBCs. - Measurment of bilirubin indicates the degree of fetal red blood cell destruction.