American Academy of Sleep Medicine SLEEP ALERTNESS and







- Slides: 34
American Academy of Sleep Medicine SLEEP, ALERTNESS, and FATIGUE EDUCATION in RESIDENCY Page 1 © American Academy of Sleep Medicine
The official requirement • The program must educate all faculty and residents to recognize the signs of fatigue and sleep deprivation; alertness management and fatigue mitigation processes; and adopt fatigue mitigation processes to manage the potential negative effects of fatigue on patient care and learning. • ACGME Requirements 2015 Page 2
American Academy of Sleep Medicine The REAL requirement “Patients have a right to expect a healthy, alert, responsible, and responsive physician. ” January 1994 statement by American College of Surgeons Re-approved and re-issued June 2002 Page 3 © American Academy of Sleep Medicine
Objectives 1. 2. 3. 4. 5. 6. Recognize universal need for adequate sleep Review risks of sleep deprivation Consider methods to promote alertness when sleep-deprived Consider methods to reduce risk of fatiguerelated errors Identify methods to recover from sleep deprivation Review preventive measures Page 4
Humans need adequate sleep Adequate means both duration and quality Page 5
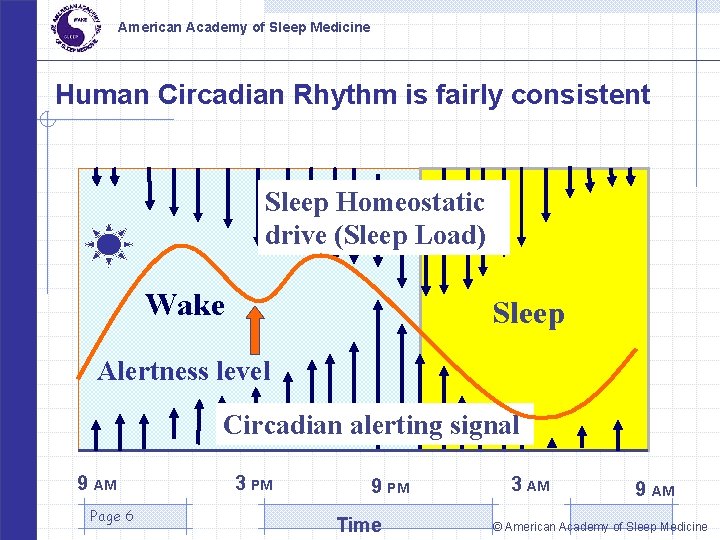
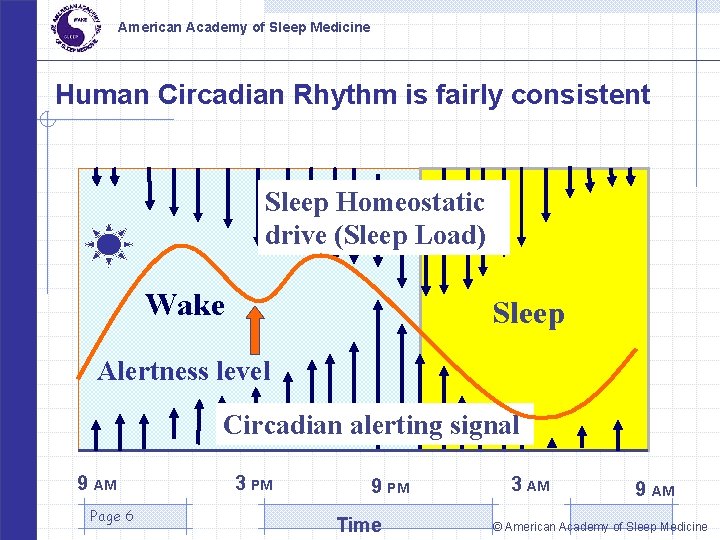
American Academy of Sleep Medicine Human Circadian Rhythm is fairly consistent Sleep Homeostatic drive (Sleep Load) Wake Sleep Alertness level Circadian alerting signal 9 AM Page 6 3 PM 9 PM Time 3 AM 9 AM © American Academy of Sleep Medicine
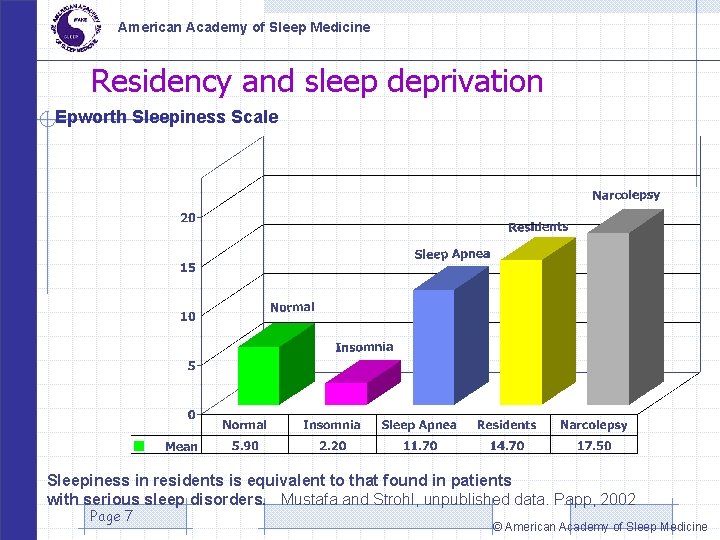
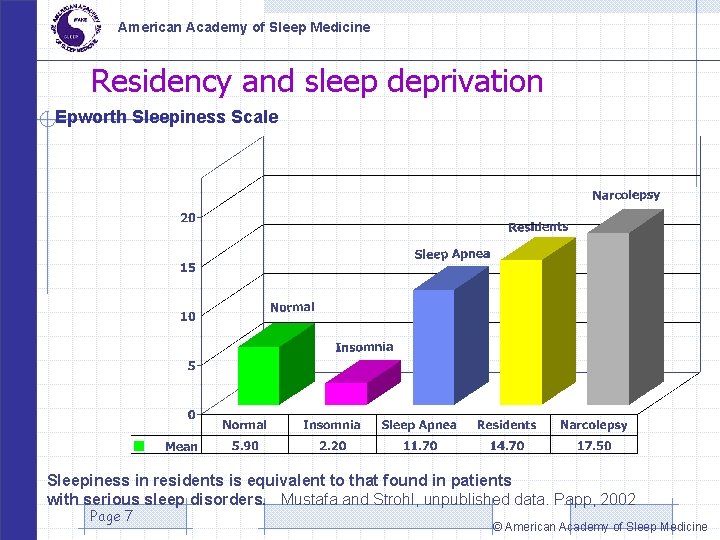
American Academy of Sleep Medicine Residency and sleep deprivation Epworth Sleepiness Scale Sleepiness in residents is equivalent to that found in patients with serious sleep disorders. Mustafa and Strohl, unpublished data. Papp, 2002 Page 7 © American Academy of Sleep Medicine
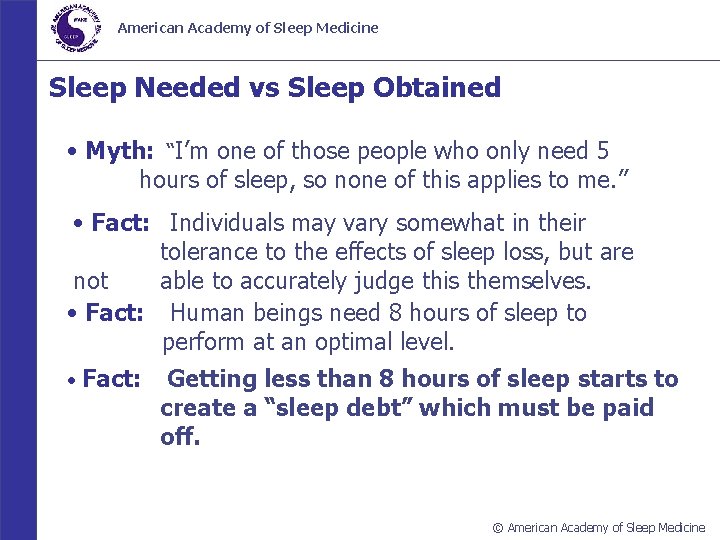
American Academy of Sleep Medicine Sleep Needed vs Sleep Obtained • Myth: “I’m one of those people who only need 5 hours of sleep, so none of this applies to me. ” • Fact: Individuals may vary somewhat in their tolerance to the effects of sleep loss, but are not able to accurately judge this themselves. • Fact: Human beings need 8 hours of sleep to perform at an optimal level. • Fact: Getting less than 8 hours of sleep starts to create a “sleep debt” which must be paid off. © American Academy of Sleep Medicine

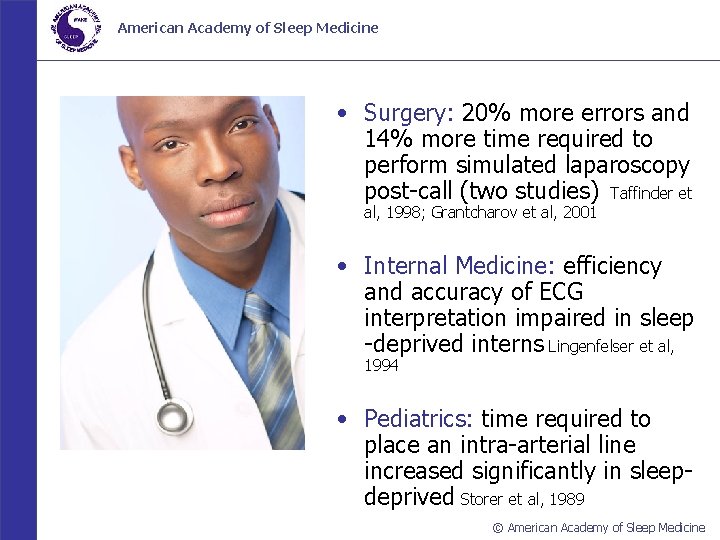
Sleep deprivation is hazardous to others Page 9
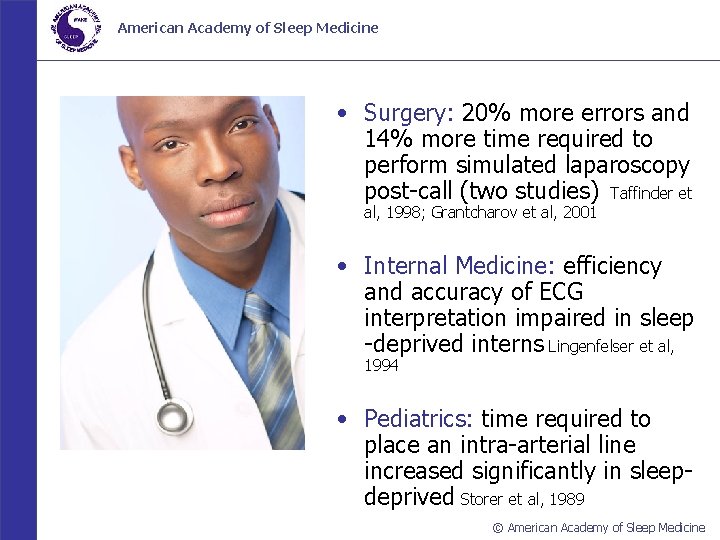
American Academy of Sleep Medicine • Surgery: 20% more errors and 14% more time required to perform simulated laparoscopy post-call (two studies) Taffinder et al, 1998; Grantcharov et al, 2001 • Internal Medicine: efficiency and accuracy of ECG interpretation impaired in sleep -deprived interns Lingenfelser et al, 1994 • Pediatrics: time required to place an intra-arterial line increased significantly in sleepdeprived Storer et al, 1989 © American Academy of Sleep Medicine
Sleep deprivation is hazardous to you Page 11 “Dan, moments before he fell asleep at the wheel”
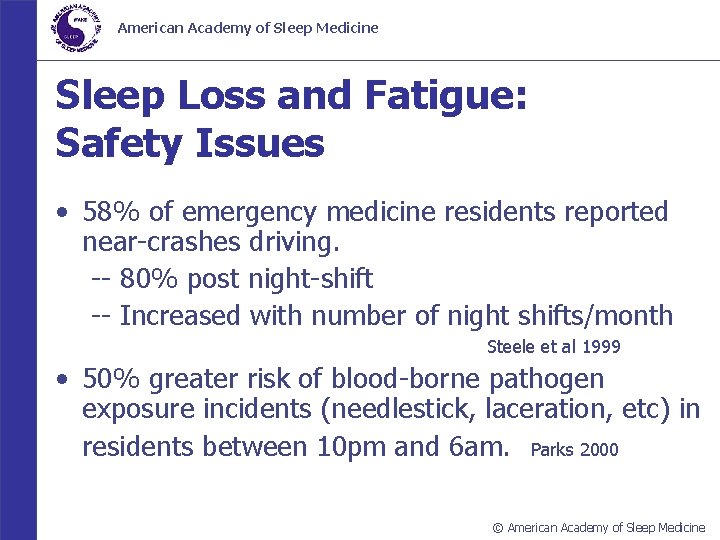
American Academy of Sleep Medicine Sleep Loss and Fatigue: Safety Issues • 58% of emergency medicine residents reported near-crashes driving. -- 80% post night-shift -- Increased with number of night shifts/month Steele et al 1999 • 50% greater risk of blood-borne pathogen exposure incidents (needlestick, laceration, etc) in residents between 10 pm and 6 am. Parks 2000 © American Academy of Sleep Medicine
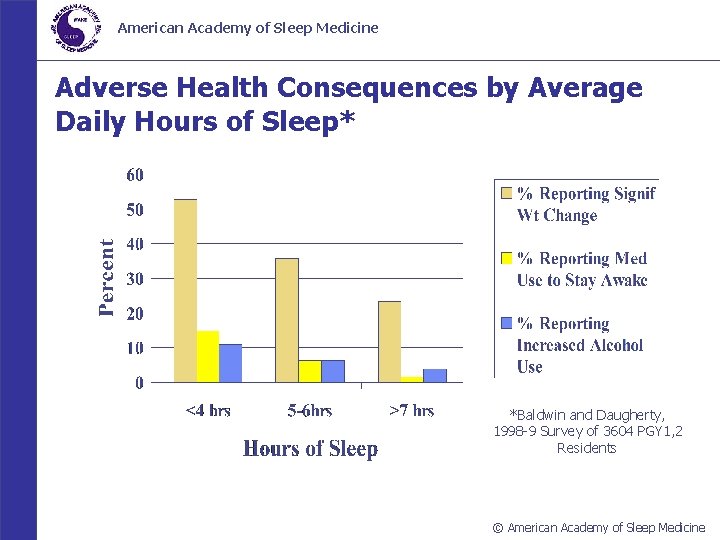
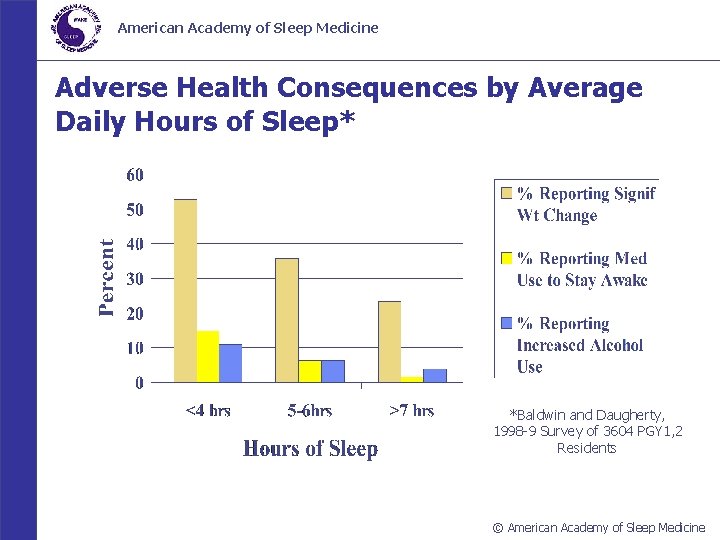
American Academy of Sleep Medicine Adverse Health Consequences by Average Daily Hours of Sleep* *Baldwin and Daugherty, 1998 -9 Survey of 3604 PGY 1, 2 Residents © American Academy of Sleep Medicine
American Academy of Sleep Medicine Drive Smart; Drive Safe • AVOID driving if drowsy. • If you are really sleepy, get a ride home, take a taxi, or use public transportation. • Take a 20 minute nap and/or drink a cup of coffee before going home post-call. • Stop driving if you notice the warning signs of sleepiness. • Pull off the road at a safe place, take a short nap. © American Academy of Sleep Medicine

American Academy of Sleep Medicine Drowsy Driving: What Does Not Work • • • Turning up the radio Opening the car window Chewing gum Blowing cold air (water) on your face Slapping (pinching) yourself hard Promising yourself a reward for staying awake © American Academy of Sleep Medicine
“Alertness management” strategies Caffeine Exercise Light Napping Medication Page 16
Caffeine Time use judiciously e. g. before circadian low point Onset: 15 - 30 min Effects last 3 -4 hours But, sleep-disruptive: if possible, d/c 3 -4 hours before planned sleep Page 17

Exercise Stretch, run in place, or do jumping jacks Walk briskly from house to car, car to hospital Page 18
Light Best: fullspectrum light (e. g. sunlight) Any bright light helps Page 19
Napping 20 -45 minutes Up to 2: 00 (allows REM + restorative sleep) BUT longer naps > risk of sleep inertia Page 20
Medication Modafinil ONLY IF PRESCRIBED by your personal physician Page 21

And watch out for these Microsleeps Sleep inertia Circadian lows Isolation Self-deception High risk jobs Page 22
Microsleeps “Faceplants”, or “nodding off” Sleeper often unaware Alert your colleagues! Response: thank colleague; exercise; talk Page 23

Sleep Inertia: 10 -120 min of grogginess, cognitive slowing, decreased vigilance after awakening. Worsened by sleep deprivation Page 24
Circadian lows 12 -4 a. m. 12 -4 p. m. Page 25
Isolation: • sleepiness predicts underestimates of level of sleepiness and overestimates of alertness; • residents in 1 study did not perceive themselves to be asleep almost half of the time they had actually fallen asleep (Howard et al, 2002) Page 26
Self-deception • “If I can just get through the night (on call), I’m fine in the morning. ” • “I’m better off ‘toughing it out’, napping just makes me feel worse. ” • “I get used to night shifts right away; no problem. ” Page 27
High-risk jobs low stimulation + high need for vigilance Page 28
American Academy of Sleep Medicine Adapting To Night Shifts • Myth: “I get used to night shifts right away; no problem. ” • Fact: It takes at least a week for circadian rhythms and sleep patterns to adjust. • Fact: Adjustment often includes physical and mental symptoms (think jet lag). • Fact: Direction of shift rotation affects adaptation (forward/clockwise easier to adapt). © American Academy of Sleep Medicine
American Academy of Sleep Medicine How To Survive Night Float • Protect your sleep. • Nap before work. • Consider “splitting” sleep into two 4 hour periods. • Have as much exposure to bright light as possible when you need to be alert. • Avoid light exposure in the morning after night shift (be cool and wear dark glasses driving home from work). © American Academy of Sleep Medicine

Recovering from sleep deprivation On average, two nights’ recovery sleep (approx 9 h) needed Page 31

Preventive measures • Sleep ahead: • Optimize your sleep environment – Cool, dark, quiet • Practice good sleep hygiene – Presleep relaxation, reduce alerting stimuli, make bed a cue for sleep Page 32
American Academy of Sleep Medicine In Summary… • Sleepiness and fatigue can’ t be eliminated in • • residency, but can be managed. Recognizing sleepiness and fatigue in yourself and your colleagues is the 1 st step Practice alertness management strategies regularly Don’t overlook recovery periods If self-management isn’t working, talk to your seniors and/or program director Page 33 © American Academy of Sleep Medicine
Page 34
 Aapm&r job board
Aapm&r job board Predictive index vs disc
Predictive index vs disc Osha theories of accidents
Osha theories of accidents Alertness pathfinder
Alertness pathfinder Module 16 sleep patterns and sleep theories
Module 16 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Www.hisdchoice.com to apply online
Www.hisdchoice.com to apply online American academy of oral and maxillofacial radiology
American academy of oral and maxillofacial radiology American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Come sleep o sleep
Come sleep o sleep Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Medicine wheel colours meaning
Medicine wheel colours meaning American board of cardiovascular medicine
American board of cardiovascular medicine Splenae
Splenae American academy of financial management
American academy of financial management American academy of private physicians
American academy of private physicians Beauty academy online course
Beauty academy online course American academy of witchcraft arts
American academy of witchcraft arts University of medicine and pharmacy timisoara
University of medicine and pharmacy timisoara School of public health monash
School of public health monash Faculty of medicine nursing and health sciences
Faculty of medicine nursing and health sciences Victor babeş university of medicine and pharmacy
Victor babeş university of medicine and pharmacy Victor babes university of medicine and pharmacy
Victor babes university of medicine and pharmacy Internal medicine jeopardy questions and answers
Internal medicine jeopardy questions and answers Fick's law of diffusion
Fick's law of diffusion God of poetry music medicine and light
God of poetry music medicine and light Empiric era of pharmacy
Empiric era of pharmacy National center for disaster medicine and public health
National center for disaster medicine and public health Internal medicine society of australia and new zealand
Internal medicine society of australia and new zealand Consumer health ppt
Consumer health ppt Chapter 11 complementary and alternative medicine
Chapter 11 complementary and alternative medicine Match and medicine stamps
Match and medicine stamps Miami j cto brace
Miami j cto brace Duke family medicine and community health
Duke family medicine and community health