AMENORRHOEA DR OLADUNNI E K NITMED TUTORIALS INTRODUCTION

- Slides: 53
AMENORRHOEA DR OLADUNNI E. K ©NITMED TUTORIALS
INTRODUCTION q AMENORRHOEA – Amenorrhoea is defined as the absence of menstruation for more than 6 months in a woman of fertile age q. Amenorrhoea is a symptom, not a disease and it has variety of causes q. Traditionally classified into primary or secondary 2
CLASSIFICATION & DEFINITION q PRIMARY AMENORRHOEA Ø Defined as the absence of menstruation by the age of 14 years in the absence of secondary sexual characteristics, or the absence of menstruation by 16 years in the presence of secondary sexual characteristics. ØThe median age of menarche is 10 -15 years and weight 51. 1 kg 3
CLASSIFICATION & DEFINITION • SECONDARY AMENORRHOEA Ø No menses have occurred for 6 months in a woman who previously had normal menstrual function, or for 12 months if her cycles were irregular 4
RELATED TERMS: • OLIGOMENORRHOEA – Interval of >35 days • HYPOMENORRHOEA – Scanty volume & short duration of flow • POLYMENORRHOEA – Interval of < 21 days 5
PATHOPHYSIOLOGY • Menstrual cycle – orderly progression of coordinated hormonal events • 3 physiological phases Ø follicular Ø ovulatory ØLuteal 6
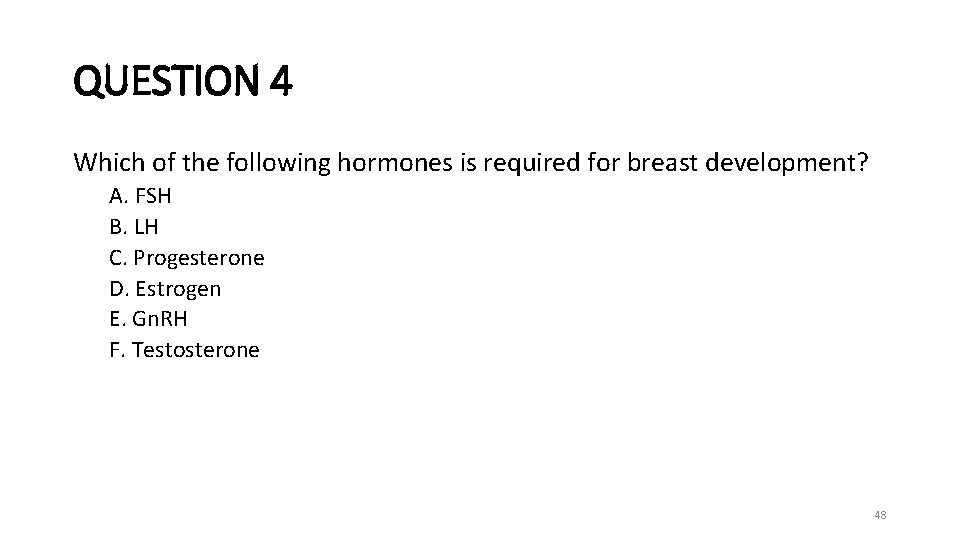
EVENTS OF PUBERTY q. THELARCHE (breast development) ØRequires estrogen q. PUBARCHE/ADRENARCHE ( pubic hair development) Ø requires androgen 7
EVENTS OF PUBERTY CONTINUES • MENARCHE • REQUIRES: ØGNRH from the hypothalamus ØFSH & LH from the pituitary ØEstrogen and progesterone from the ovaries ØNormal outflow tract 8
AETIOLOGY OF AMENORRHOEAPHYSIOLOGICAL 1. PHYSIOLOGICAL AMENORRHOEA Ø Pre- menarche – young girls ØPregnancy ØMenopause 9
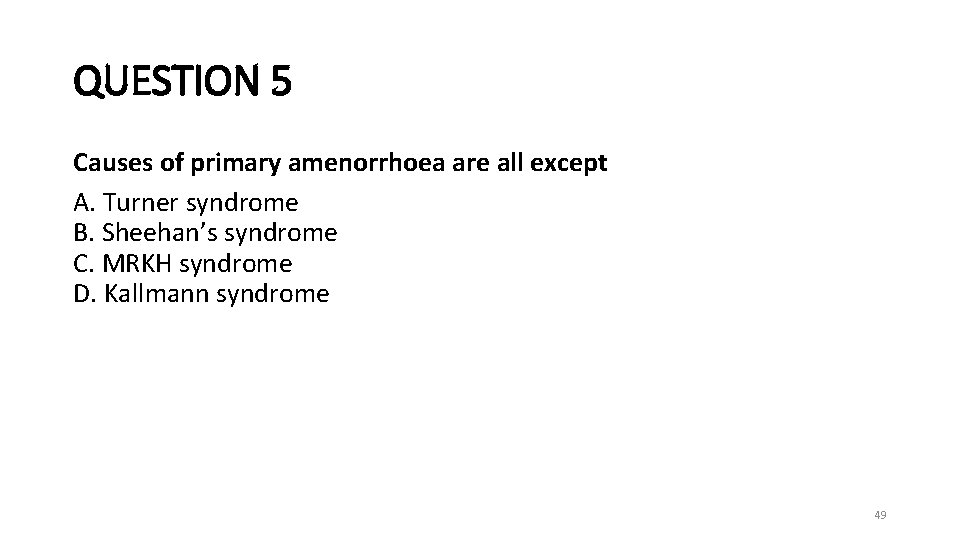
AETIOLOGY OF AMENORRHOEA- ABNORMALITY OF THE HPO AXIS HYPOTHALAMIC DISORDERS- hypogonadotrophic hypogonadism • Excessive exercise, weight loss and stress. • Hypothalamic lesions (craniopharyngioma, glioma), which can compress hypothalamic tissue or block dopamine. • Head injuries. • Kallman’s syndrome (X-linked recessive condition resulting in deficiency in Gn. RH causing underdeveloped genitalia). • Systemic disorders including sarcoidosis, tuberculosis resulting in an infiltrative process in the hypothalamo-hypophyseal region. • Drugs: progestogens, HRT or dopamine antagonists. • Eating disorders 10
AETIOLOGY OF AMENORRHOEAABNORMALITY OF THE HPO AXIS PITUITARY DISORDER- hypogonadotrophic hypogonadism Ø Hyperprolactinemia ( 10 -40% of women with hyperprolactinaemia present to their physician with amenorrhoea) ØProlactinoma ØIsolated gonadotrophin deficiency ØCraniopharyngioma ØSheehan’s syndrome- postpartum pituitary necrosis 11
AETIOLOGY OF AMENORRHOEAABNORMALITY OF THE HPO AXIS OVARIAN DISORDER ØGonadal dysgenesis ØOvarian insufficiency or premature ovarian failure (onset of menopause before 40 years) Ø Chemotherapy and radiation injury Ø Ovarian insensitivity syndrome ( Savage’s syndrome) ØPolycystic Ovarian Syndrome 12
AETIOLOGY OF AMENORRHOEA- ENZYME ABNORMALITIES THYROID DISORDER ØHypothyroidism ØHyperthyroidism ADRENAL DISORDER Ø Congenital adrenal hyperplasia Ø cushing’s syndrome 13
AETIOLOGY OF AMENORRHOEA- OUTFLOW TRACT ABNORMALITY • UTERINE ANOMALY ü Androgen insensitivity üMullerian agenesis ( Mayer-Rokitansky-kuster Hauser syndrome) ü Uterine adhesion ( Asheman syndrome) ü Cervical agenesis 14
AETIOLOGY OF AMENORRHOEA- OUTFLOW TRACT ABNORMALITY VAGINAL ANOMALY Ø Imperforate hymen ØTransverse vaginal septum ØVaginal agenesis 15
AETIOLOGY OF PRIMARY AMENORRHOEA SECONDARY SEXUAL CHARACTERISTICS PRESENT ü Constitutional delay ü Genito-urinary malformation – imperforate hymen, transverse vaginal septum, absent vagina with or without functioning uterus ü Androgen insensitivity üResistant ovary syndrome üPregnancy 16
AETIOLOGY OF PRIMARY AMENORRHOEA • SECONDARY SEXUAL CHARACTERISTIC ABSENT ØHypothalamic dysfunction ØGonadotrophin deficiency ØHypopituitarism ØHyperprolactinaemia ØHypothyroidism ØGonadal failure 17
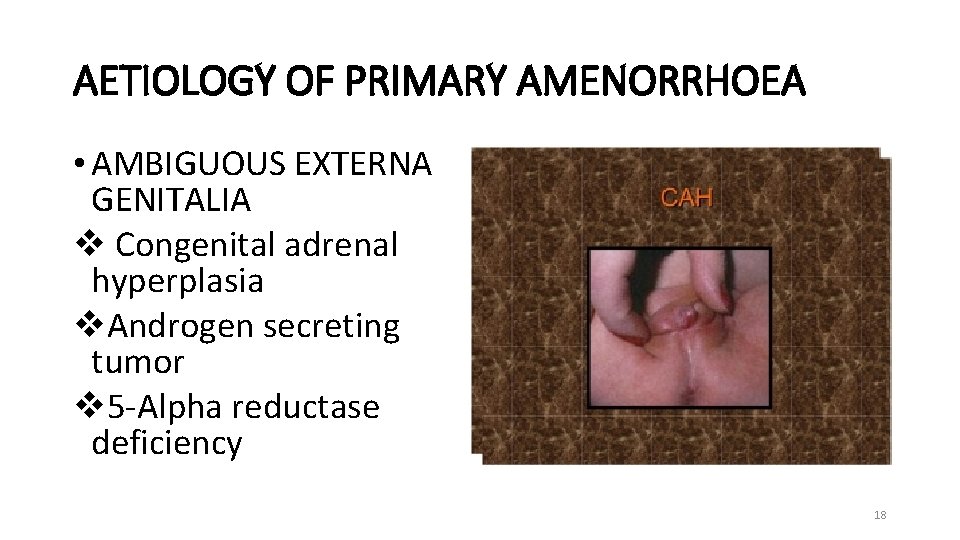
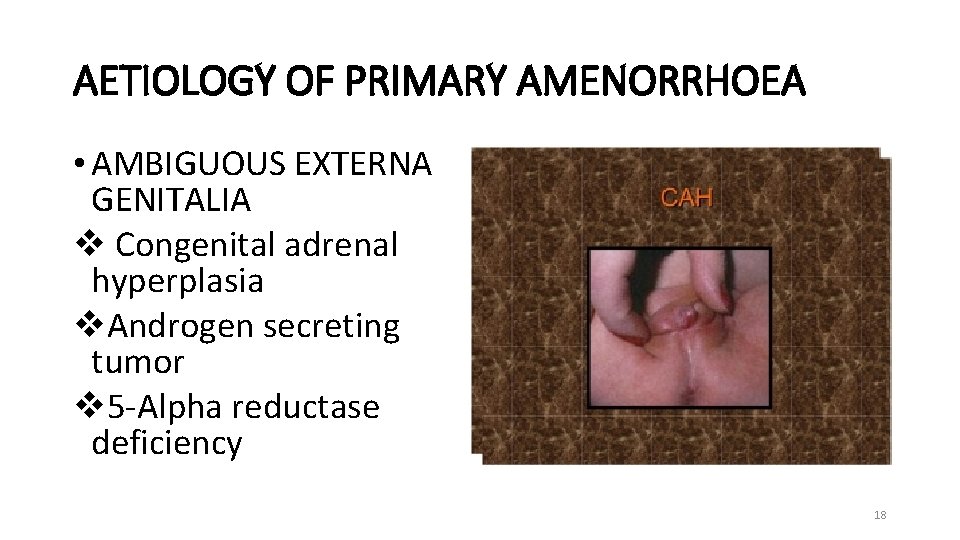
AETIOLOGY OF PRIMARY AMENORRHOEA • AMBIGUOUS EXTERNA GENITALIA v Congenital adrenal hyperplasia v. Androgen secreting tumor v 5 -Alpha reductase deficiency 18
TURNER SYNDROME • COMPLETE ABSENCE OR a partial abnormality of one of the two X chromosome • About 50% has mosaic form such as 45 X/46 XX or 45 X/ 47 XY 19
TURNER SYNDROME • FEATURES ØShort stature - web neck ØLymphedema -wide carrying angle Ø shield chest with widely spaced nipples ØCoarctation of the aorta ØStreak ovaries 20
UTEROVAGINAL AGENESIS Ø 15% primary amenorrhoea ØNormal secondary sexual development & external female genitalia ØNormal female range testosterone level 21
UTEROVAGINAL AGENESIS CONTD • Absent uterus and upper Vagina& normal ovaries • karyotype 46 xx • 15 -30% associated renal, skeletal middle ear anomalies 22
23
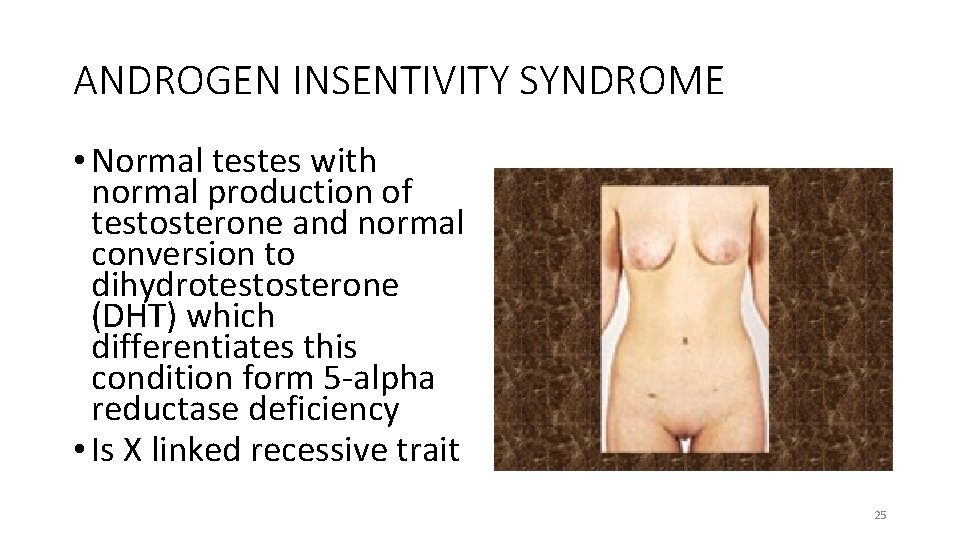
ANDROGEN INSENTIVITY SYNDROME • Formerly known as testicular feminization • 46 XY • Failure of normal masculinization of the external genitalia in chromosomally male individuals. • Defective androgen receptor 24
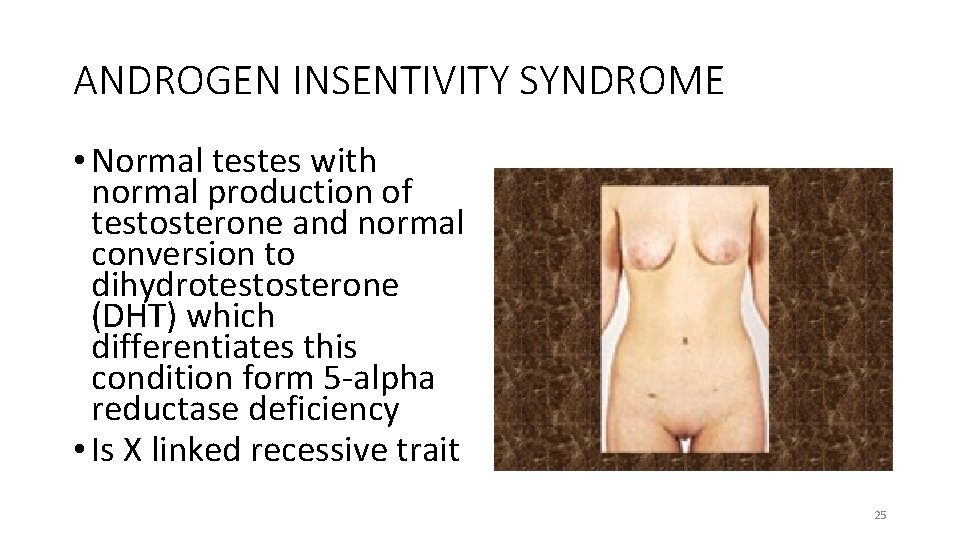
ANDROGEN INSENTIVITY SYNDROME • Normal testes with normal production of testosterone and normal conversion to dihydrotestosterone (DHT) which differentiates this condition form 5 -alpha reductase deficiency • Is X linked recessive trait 25
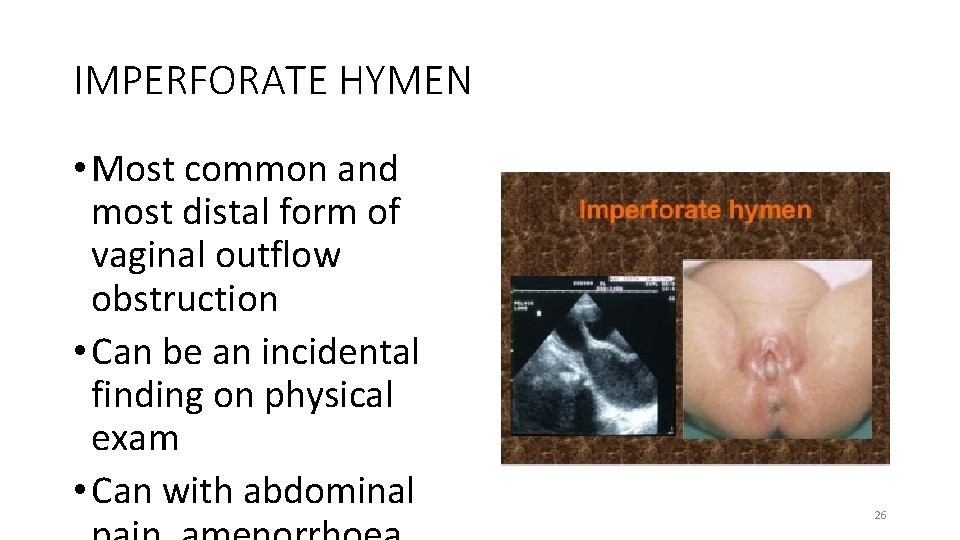
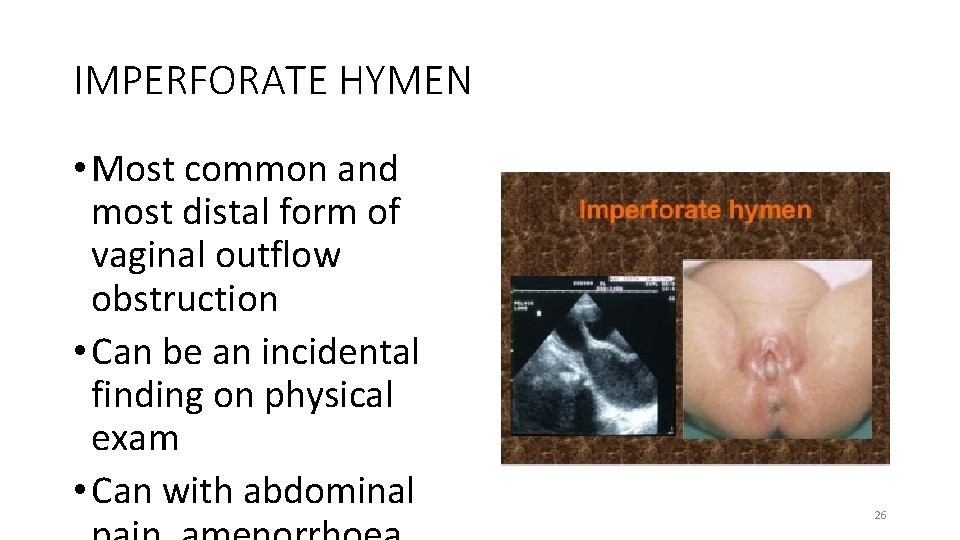
IMPERFORATE HYMEN • Most common and most distal form of vaginal outflow obstruction • Can be an incidental finding on physical exam • Can with abdominal 26
CONSTITUTIONAL DELAY • No anatomical abnormality • Endocrine investigations show normal result • Caused by immature pulsatile release of gonadotrophin-releasing hormone • Maturation eventually occurs spontaneously 27
AETIOLOGY OF SECONDARY AMENORRHOEA • OVARIAN CAUSES – Premature ovarian failure, resistant ovarian syndrome • Hypothalamic causes – weight loss, exercise, psychological distress, chronic illness, idiopathic • Pituitary causes: Hyperprolactinaemia, hypopituitarism, Sheehan’s syndrome 28
AETIOLOGY OF SECONDARY AMENORRHOEA • FEATURES OF ANDROGEN EXCESS PRESENT ØPolycystic Ovarian Syndrome ØCushing’s syndrome Ø late onset congenital adrenal hyperplasia ØAdrenal or ovarian androgen – producing tumour 29
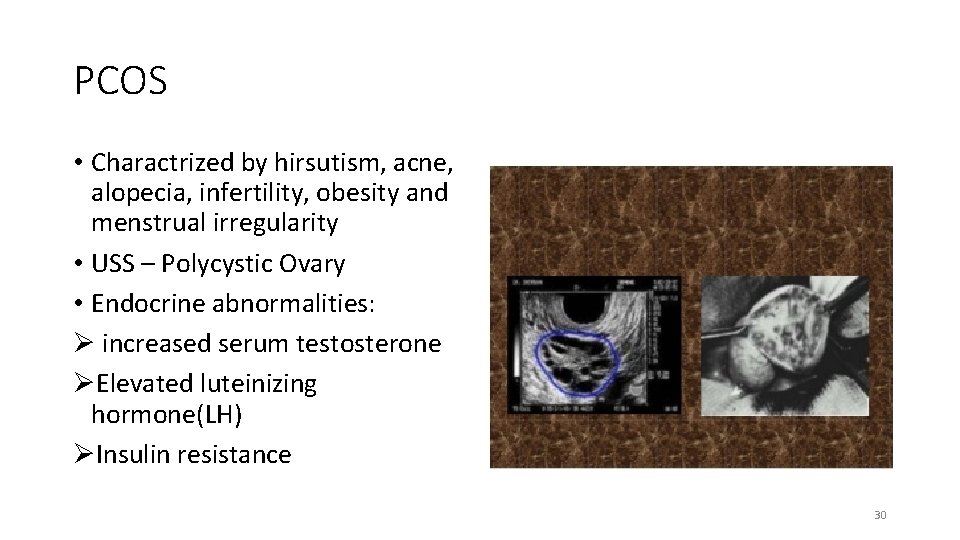
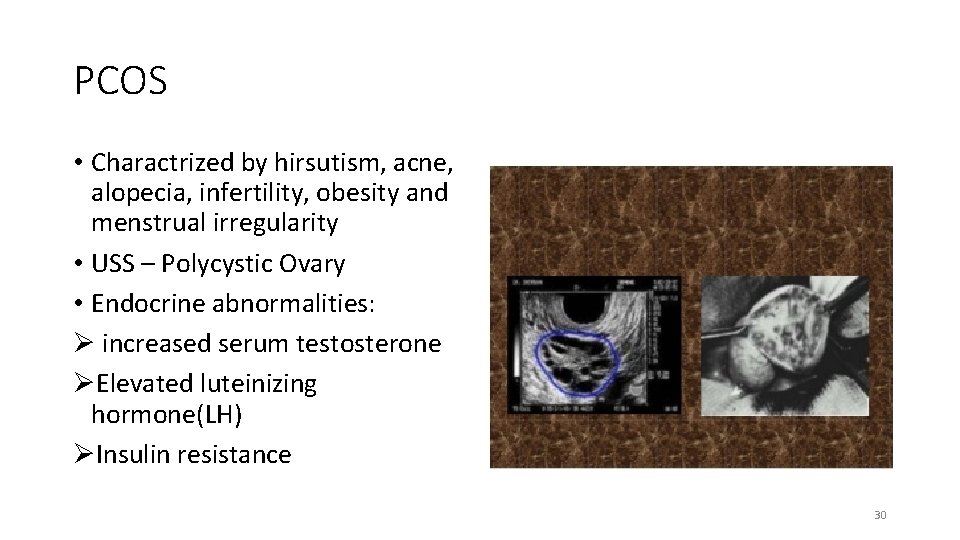
PCOS • Charactrized by hirsutism, acne, alopecia, infertility, obesity and menstrual irregularity • USS – Polycystic Ovary • Endocrine abnormalities: Ø increased serum testosterone ØElevated luteinizing hormone(LH) ØInsulin resistance 30
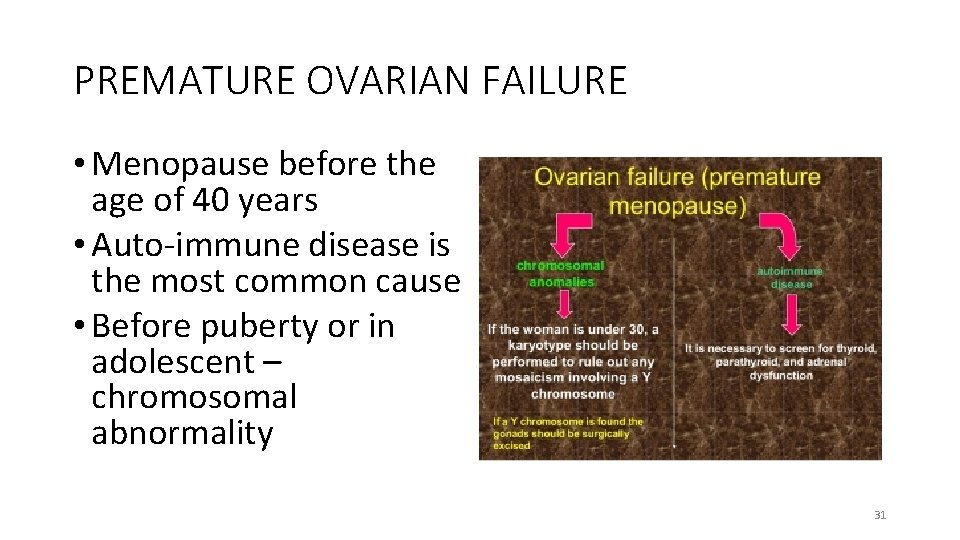
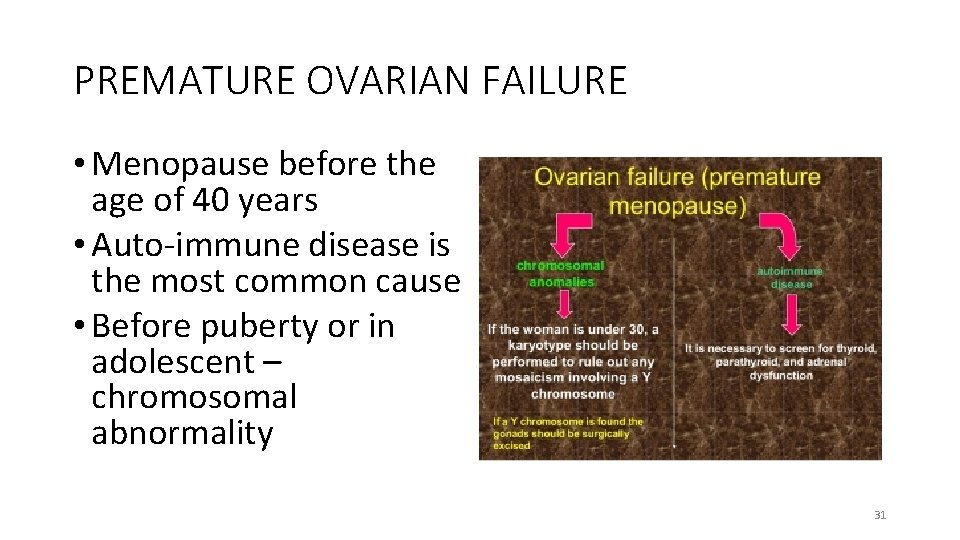
PREMATURE OVARIAN FAILURE • Menopause before the age of 40 years • Auto-immune disease is the most common cause • Before puberty or in adolescent – chromosomal abnormality 31
HYPERPROLACTINEMIA • PROLACTINOMA- commonest cause (60%) • Non functioning pituitary adenoma • Dopaminergic antagonist drugs – phenothiazides, haloperidol, methldopa • Prolactin acts directly on the hypothalamus to reduce amplitude and frequency of pulse of GNRH 32
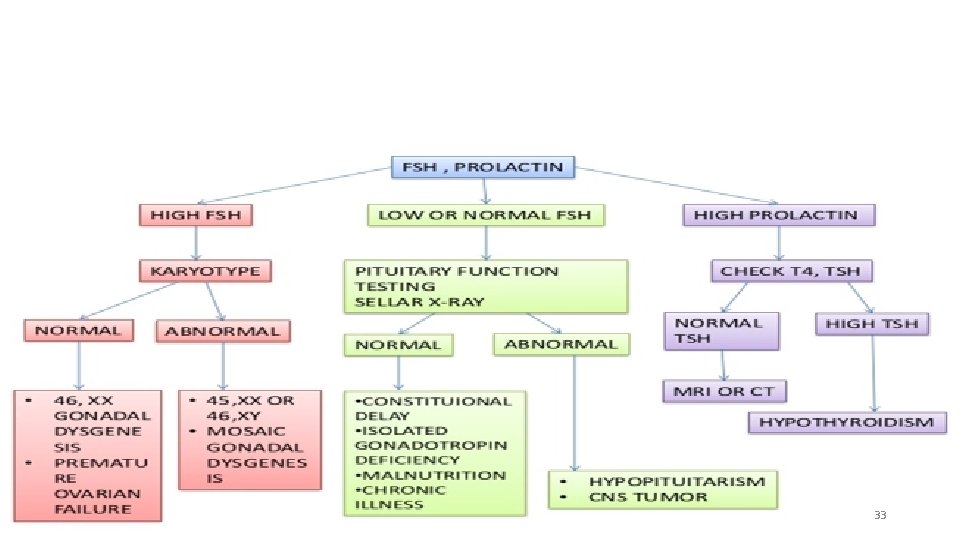
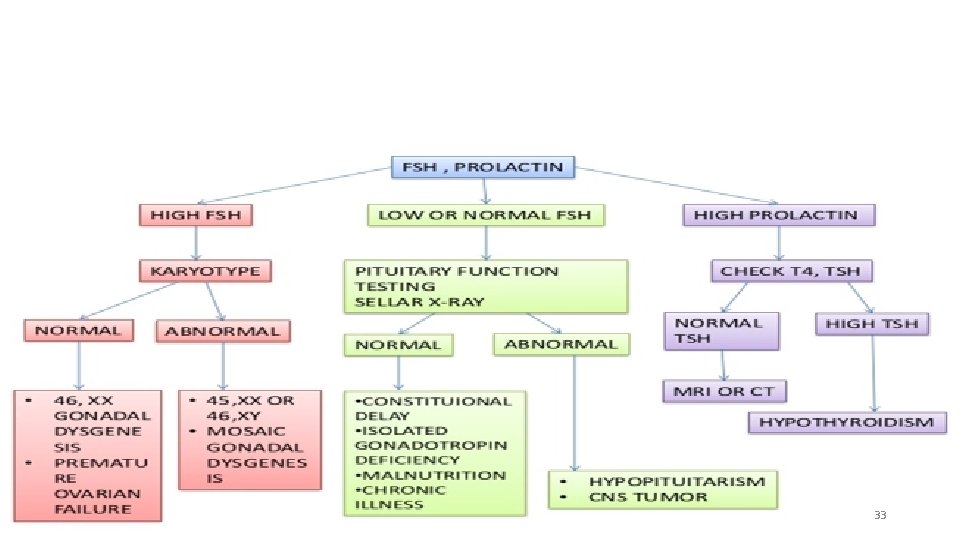
33
CLINICAL EVALUATION OF AMENORRHOEIC PT • History taking • Physical examination • Investigation • Treatment. 34
HISTORY • Pregnancy is the most common cause of amenorrhoea • Ask about sexual activity • Use of contraceptives methods • Difficulty with dates, menstrual calendar for 3 months • Breast development • Pubic hair development 35
HISTORY CONTD • Hx of evacuation • Postpartum endometritis • Hot flashes, night sweats • Hx of chemotherapy or radiation • Recent surgery e. g TAH 36
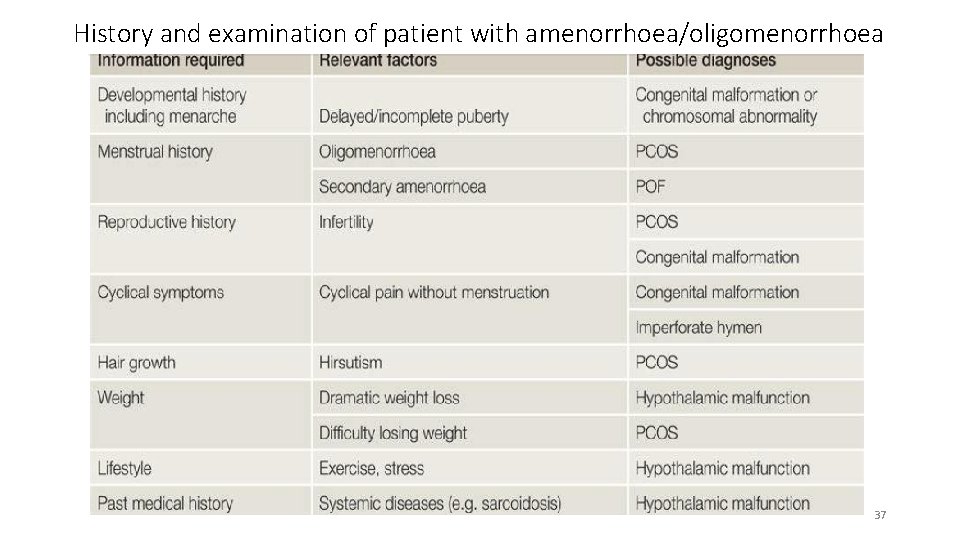
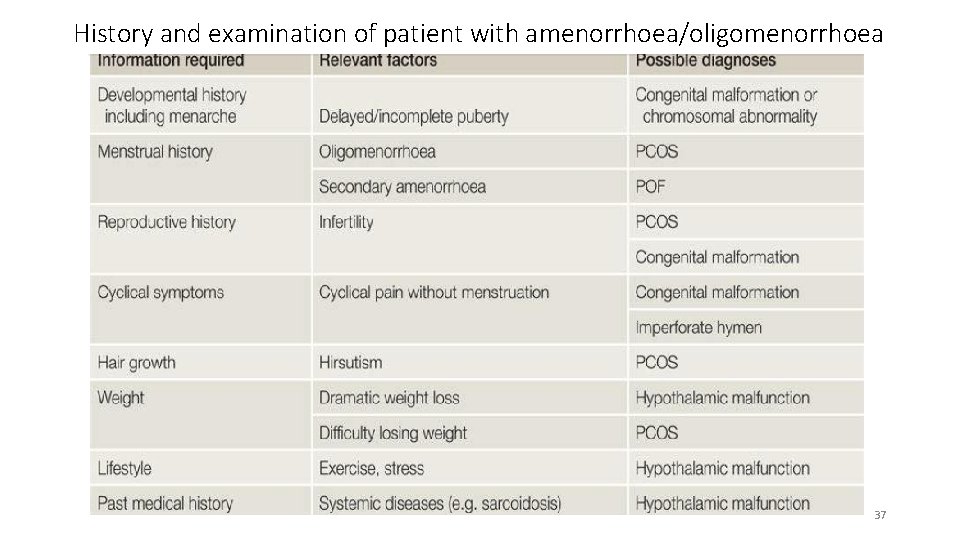
History and examination of patient with amenorrhoea/oligomenorrhoea 37
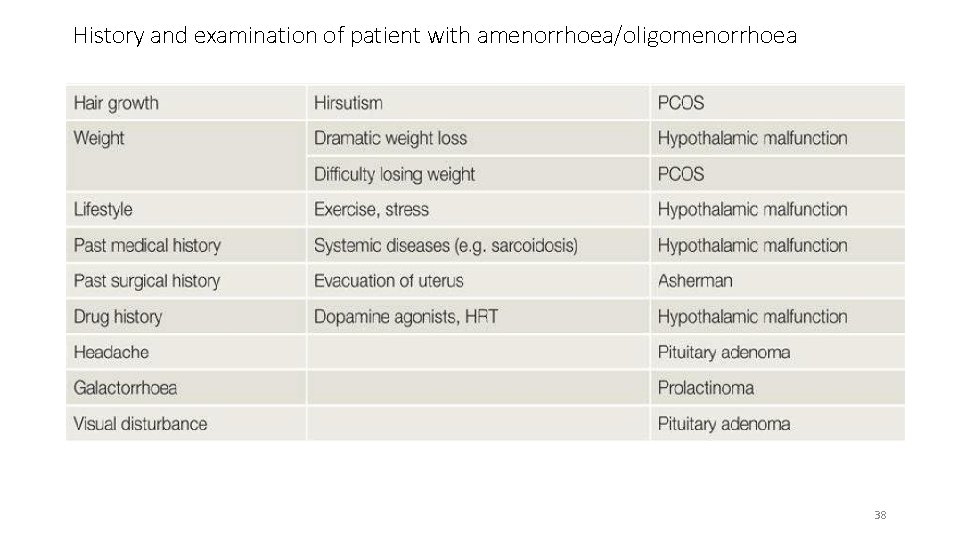
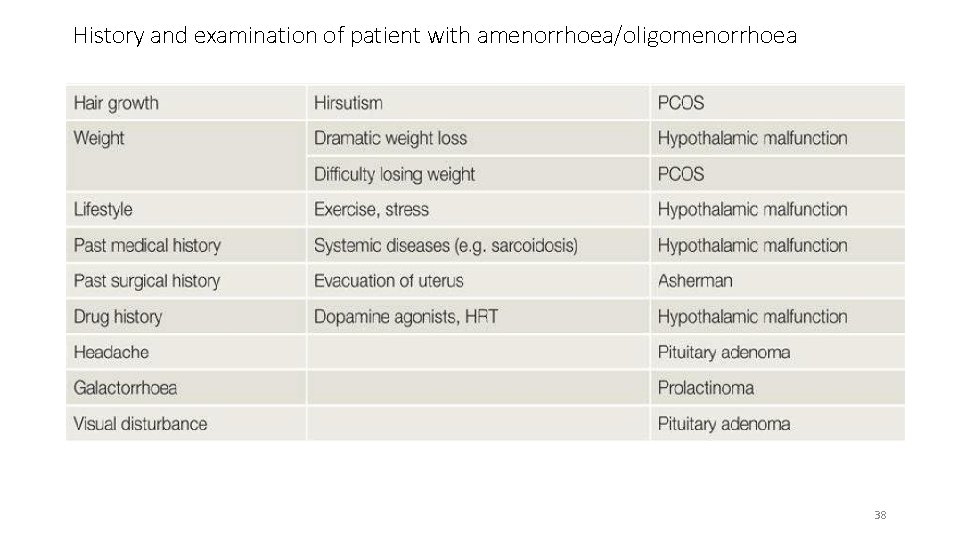
History and examination of patient with amenorrhoea/oligomenorrhoea 38

EXAMINATION • General examination • Secondary sexual characteristics • Visual field • Abdominal examination • Pelvic examination 39
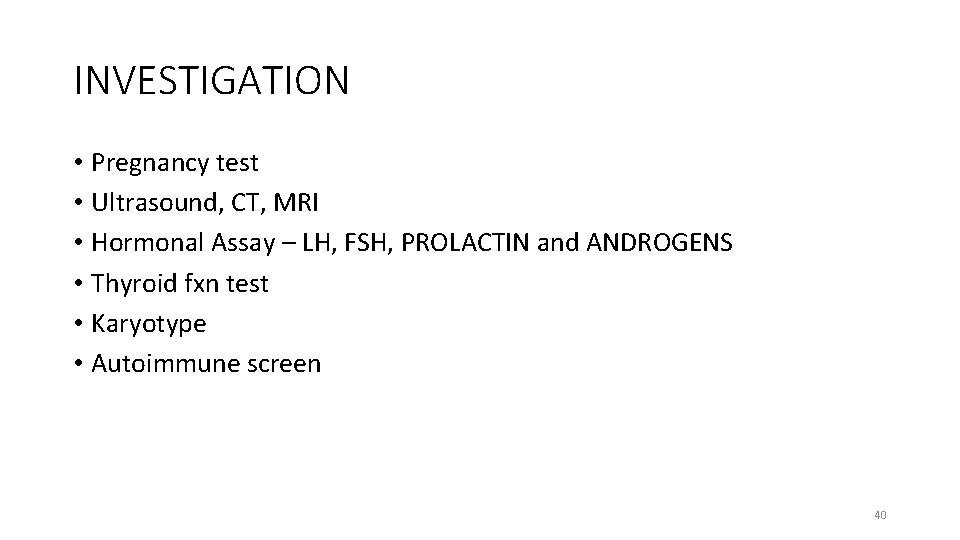
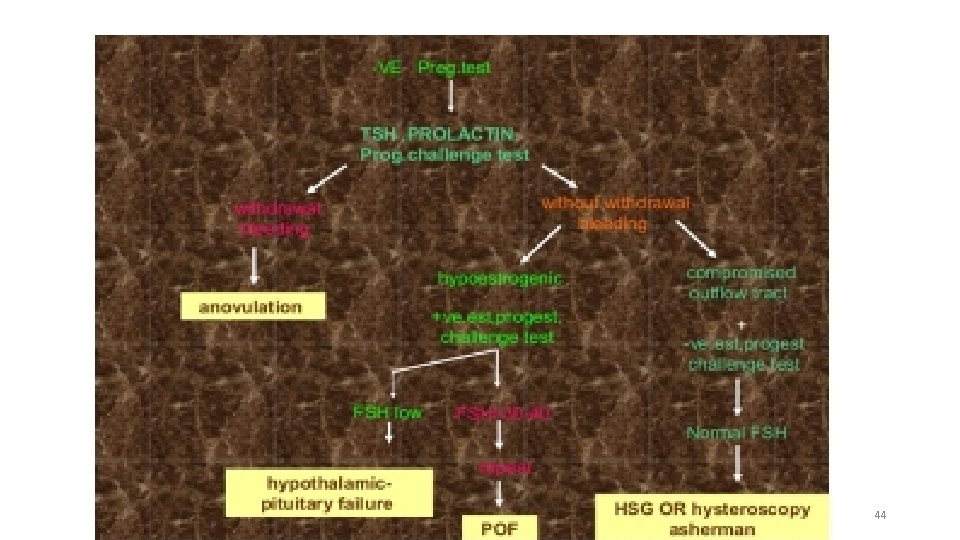
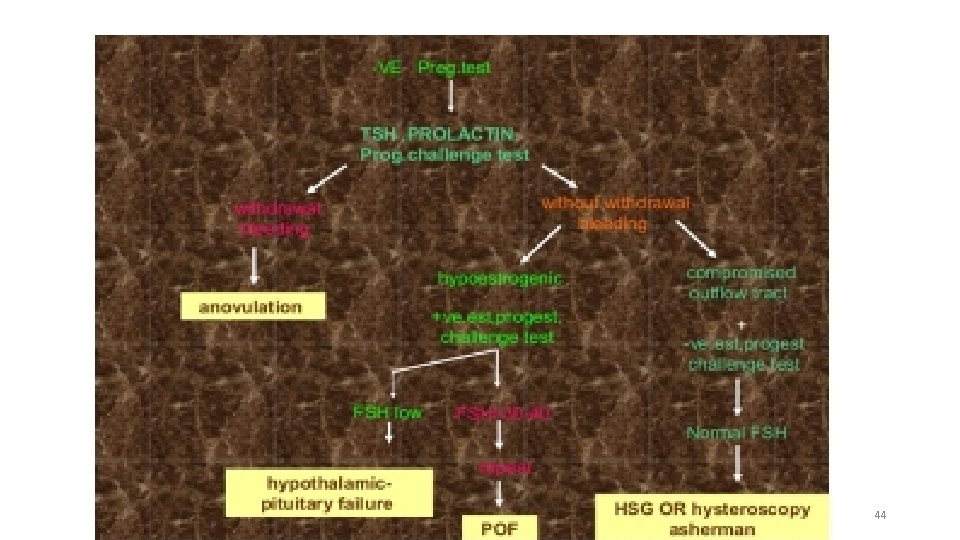
INVESTIGATION • Pregnancy test • Ultrasound, CT, MRI • Hormonal Assay – LH, FSH, PROLACTIN and ANDROGENS • Thyroid fxn test • Karyotype • Autoimmune screen 40
TREATMENT • Depending on the cause of amenorrhoea • The most common cause of primary amenorrhoea is constitutional • MEDICAL • SURGICAL 41
MEDICAL TREATMENT • Dopamine agonist e. g. Bromocriptine • Hormone replacement therapy • Ovulation induction • Treatment of hyperandrogenism 42
SURGICAL THERAPIES • Gonadectomy: XY dysgenesis • Tumour excision –large adenomas • Reconstructive surgeries – Vaginoplasty • Adhesiolysis • Ovarian diathermy • IVF 43
44
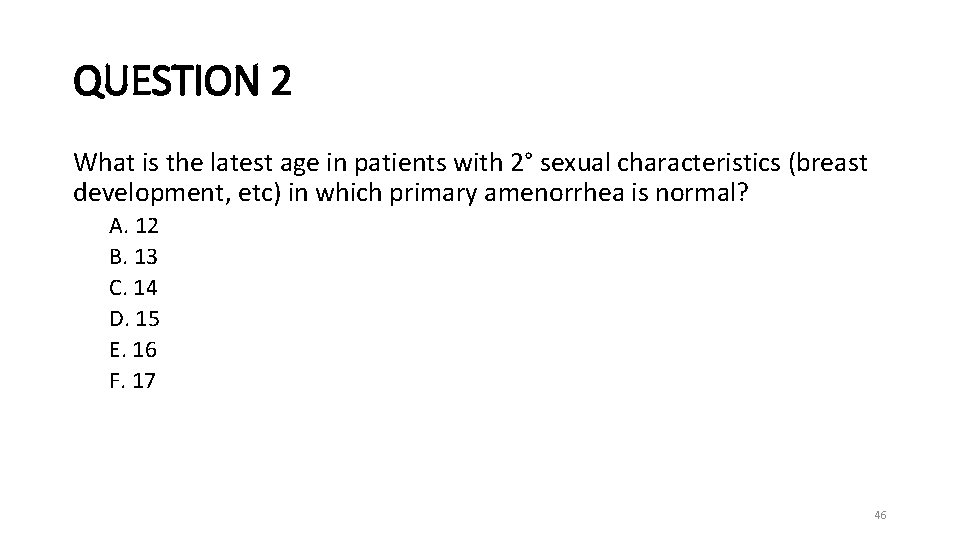
AMENORRHOEA REVISION QUESTIONS • QUESTION 1 In cases of primary amenorrhea, what is the age in patients without 2° sexual characteristics (breast development, etc) at which a “wait and see” approach is no longer appropriate? A. 12 B. 13 C. 14 D. 15 E. 16 F. 17 45
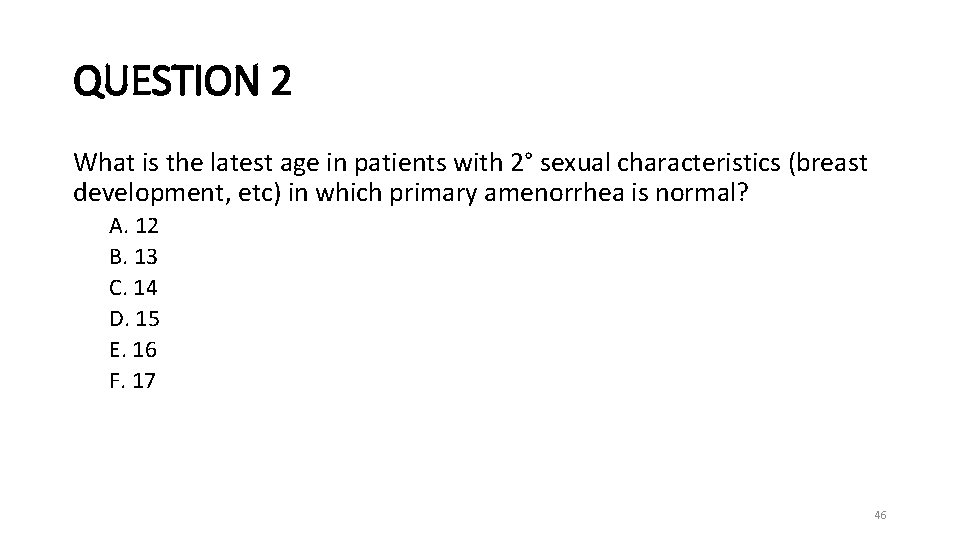
QUESTION 2 What is the latest age in patients with 2° sexual characteristics (breast development, etc) in which primary amenorrhea is normal? A. 12 B. 13 C. 14 D. 15 E. 16 F. 17 46
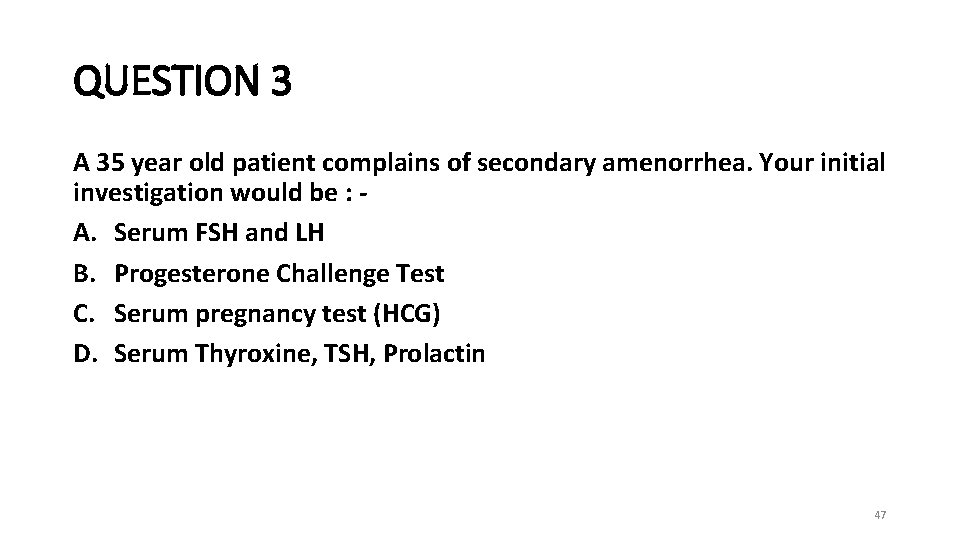
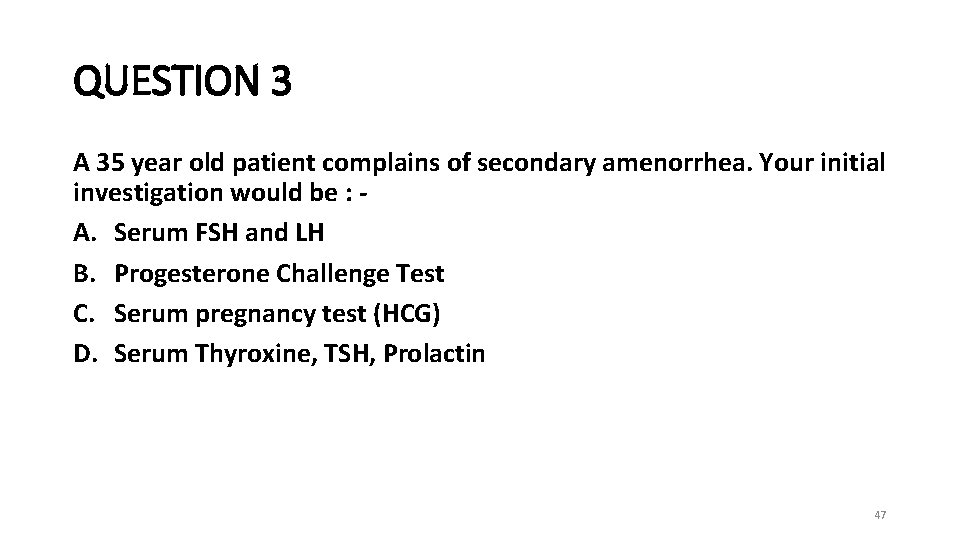
QUESTION 3 A 35 year old patient complains of secondary amenorrhea. Your initial investigation would be : A. Serum FSH and LH B. Progesterone Challenge Test C. Serum pregnancy test (HCG) D. Serum Thyroxine, TSH, Prolactin 47
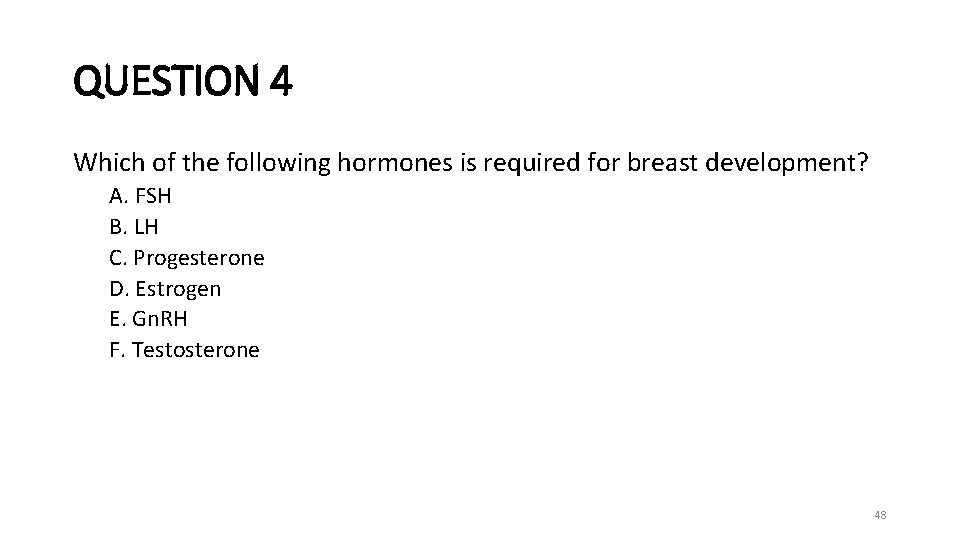
QUESTION 4 Which of the following hormones is required for breast development? A. FSH B. LH C. Progesterone D. Estrogen E. Gn. RH F. Testosterone 48
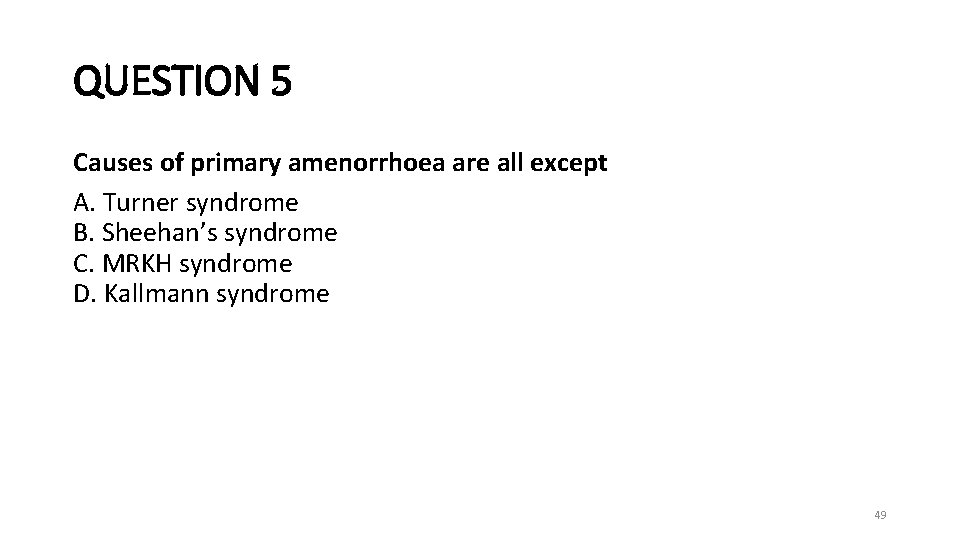
QUESTION 5 Causes of primary amenorrhoea are all except A. Turner syndrome B. Sheehan’s syndrome C. MRKH syndrome D. Kallmann syndrome 49
QUESTION 6 What is the first imaging modality used to further evaluate primary amenorrhea? A. X-ray B. Ultrasound C. FSH level D. Karyotype E. Cranial MRI F. Serum testosterone level 50
QUESTION 7 In a patient with primary amenorrhea, who has had an ultrasound demonstrating the presence of a uterus and has a decreased FSH level, which of the following tests would be most appropriate? A. Ultrasound B. FSH level C. Karyotype D. Cranial MRI E. Serum testosterone level 51
QUESTION 8 Patient with primary amenorrhea and absent secondary sex characteristics shows low FSH/LH and estradiol, with normal T 4, prolactin and testosterone. Most likely diagnosis is : A. Gonadal dysgenesis B. Congenital absence of uterus C. Androgen insensitivity D. Hypogonadotrophic hypogonadism 52
THANK YOU 53