Alteration in Genitourinary function Lecture 8 1 Anatomy
- Slides: 44
Alteration in Genitourinary function Lecture 8 1
Anatomy and physiology • The genitourinary is made up of the urinary and reproductive organs. • The urinary system of the kidneys, ureters, bladder and urethra. • Normal function requires the following: – Unimpaired renal blood flow. – Adequate glomerular filtration. – Normal Tubular function. – Un obstructed urine flow. • The functional unit of the kidney is nephron. 2
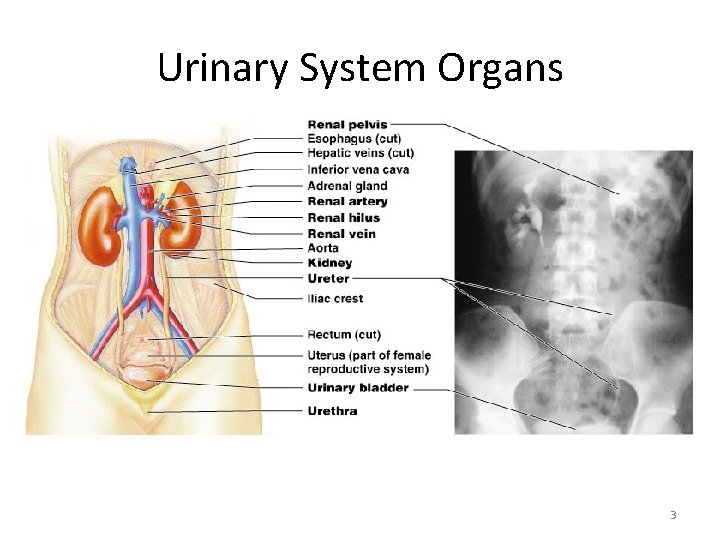
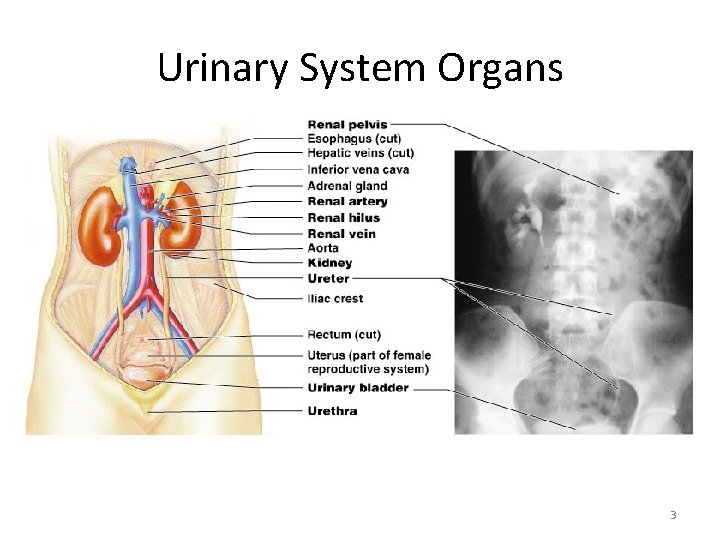
Urinary System Organs 3
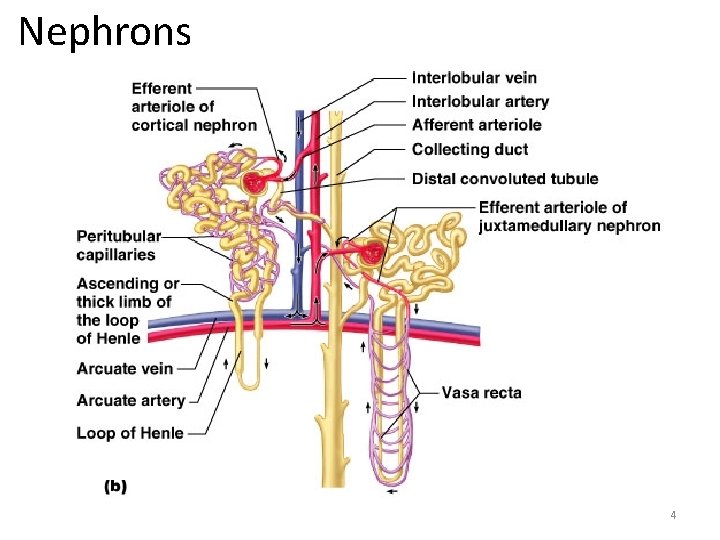
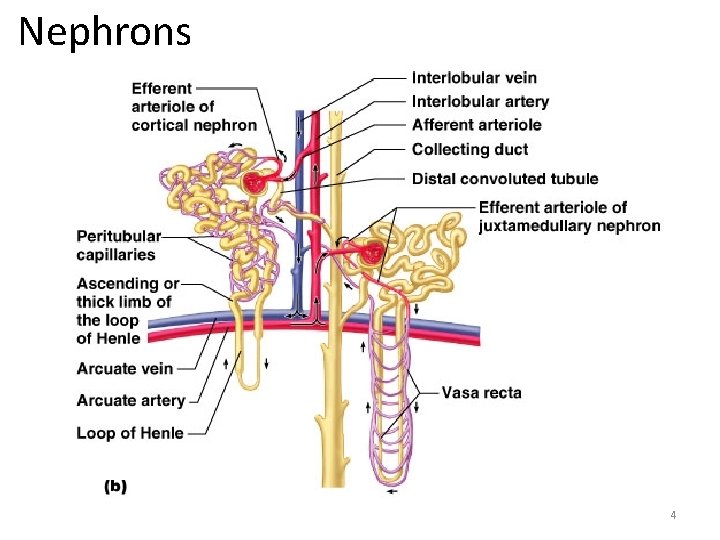
Nephrons 4
Biological Variances • All nephrons are present at birth • Kidneys and tubular system mature throughout childhood reaching full maturity during adolescence. • During first two years of life kidney function is less efficient. 5
Pediatric Differences • Kidney begins to reach adult functioning about 1 year of age • Infants cannot concentrate urine as efficiently as older children and adults. • Urine output: – Infant 2 ml/kg/hr – Children 0. 5 ml/kg/hr. – Adolescent 40 -80 ml/hr 6
Bladder • Bladder capacity increases with age • 20 to 50 ml at birth • 700 ml in adulthood 7
Review Genitourinary System • Maintain fluid & electrolyte balance through glomerular filtration, tubular reabsorption, and secretion • Hormonal functions – Produces renin in glomerulus—regulates BP – Produces Erythropoietin—stimulates RBC production in bone marrow – Metabolized Vitamin D—to active form which is important in calcium metabolism 8
Diagnostic Tests • • Urinalysis Ultrasound VCUG – Voiding cysto urethrogram IVP – Intravenous pyelogram Cystoscopy CT Scan Renal Biopsy 9
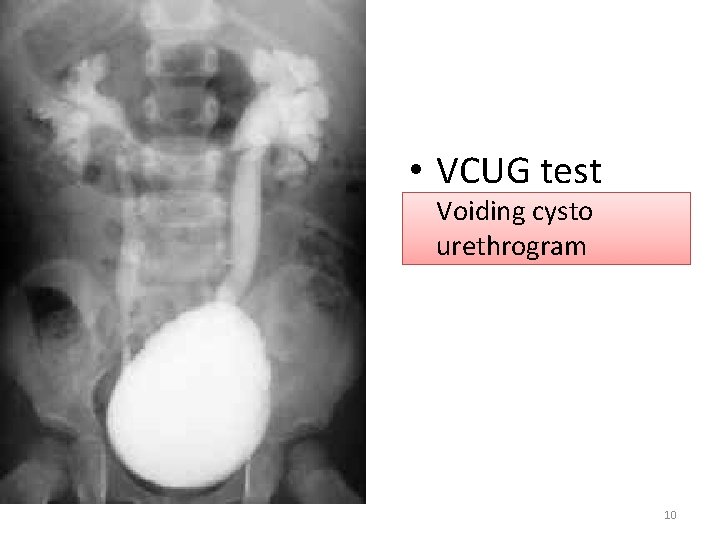
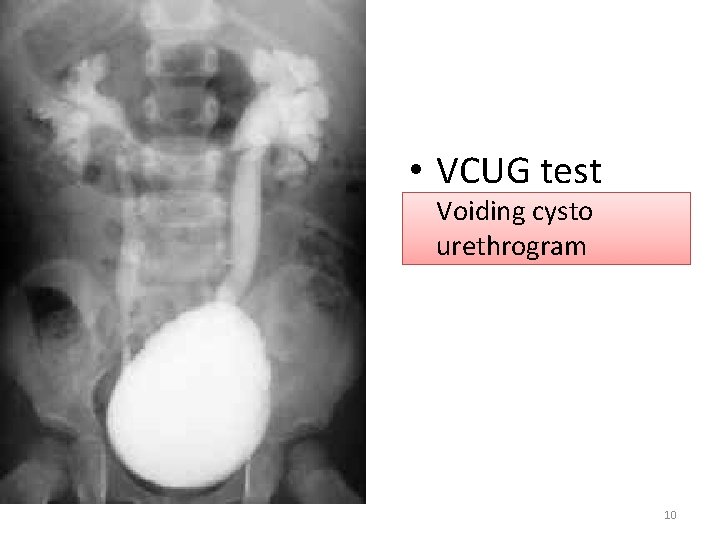
• VCUG test Voiding cysto urethrogram 10
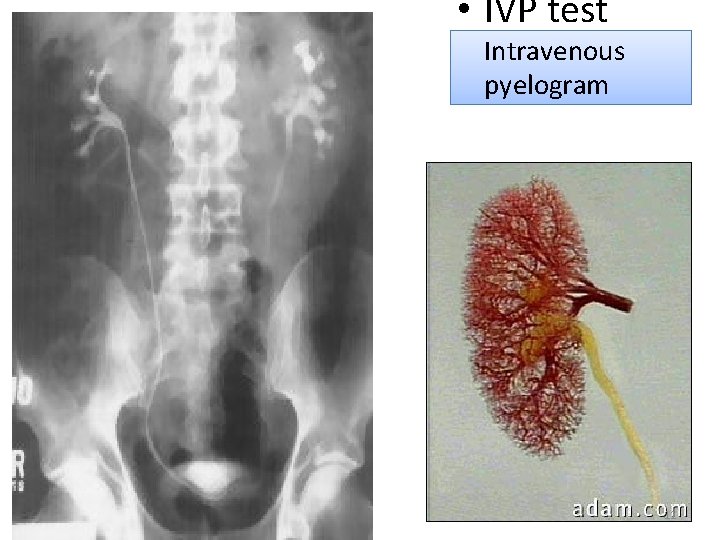
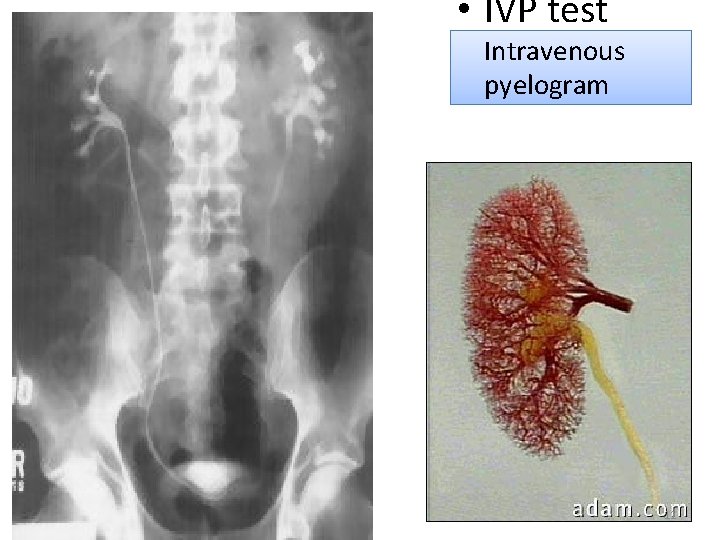
• IVP test Intravenous pyelogram 11
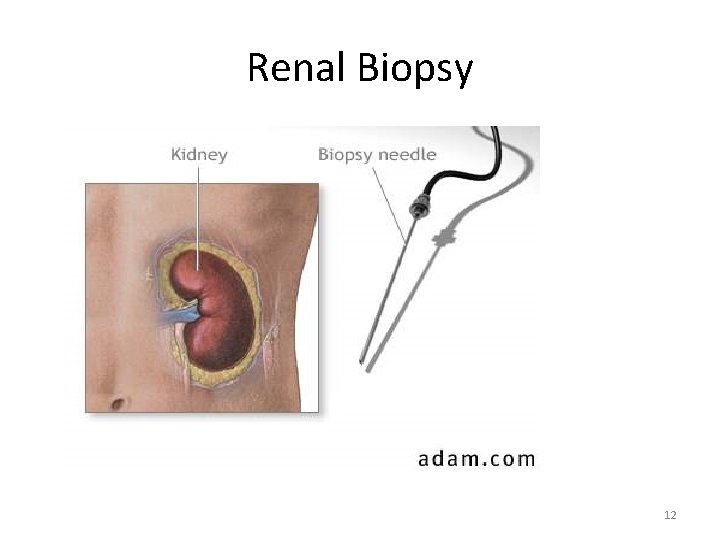
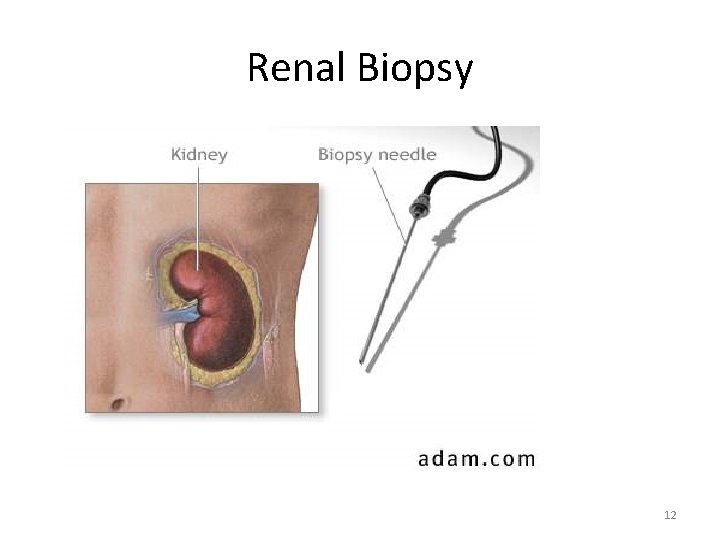
Renal Biopsy 12
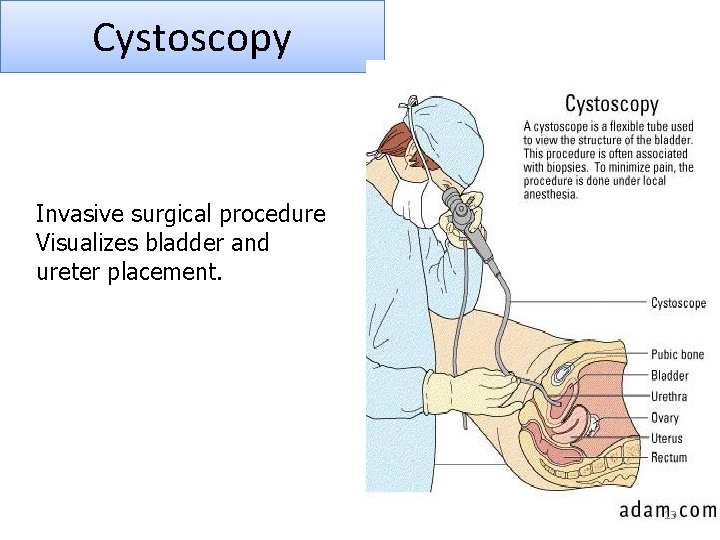
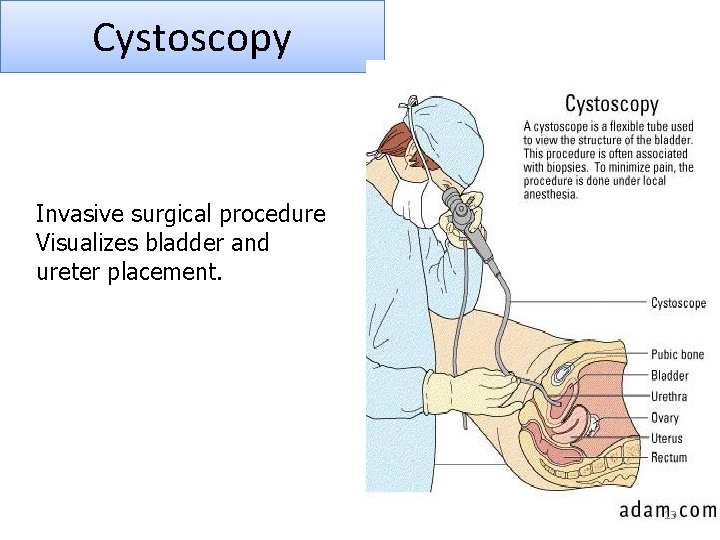
Cystoscopy Invasive surgical procedure Visualizes bladder and ureter placement. 13
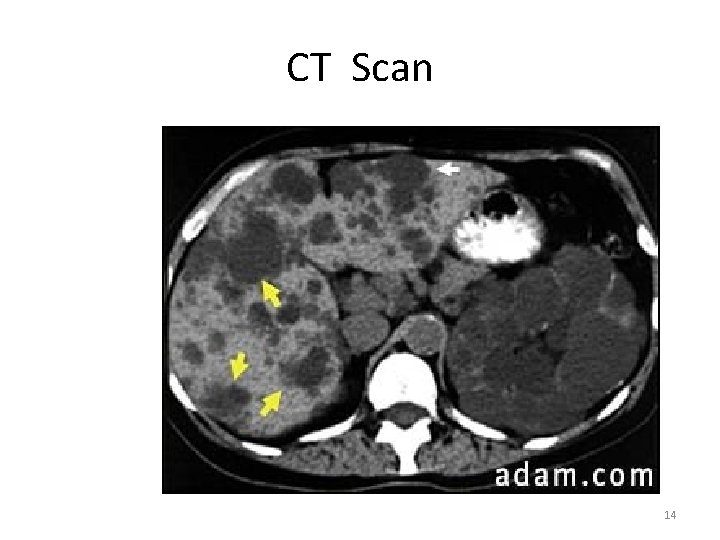
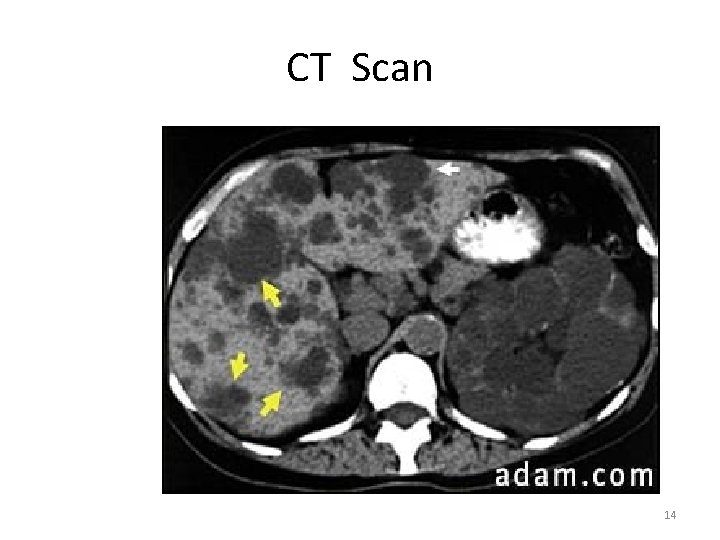
CT Scan 14
Urinalysis • • • Protein Leukocytes Red blood cells Casts Specific Gravity Urine Culture for bacteria 15
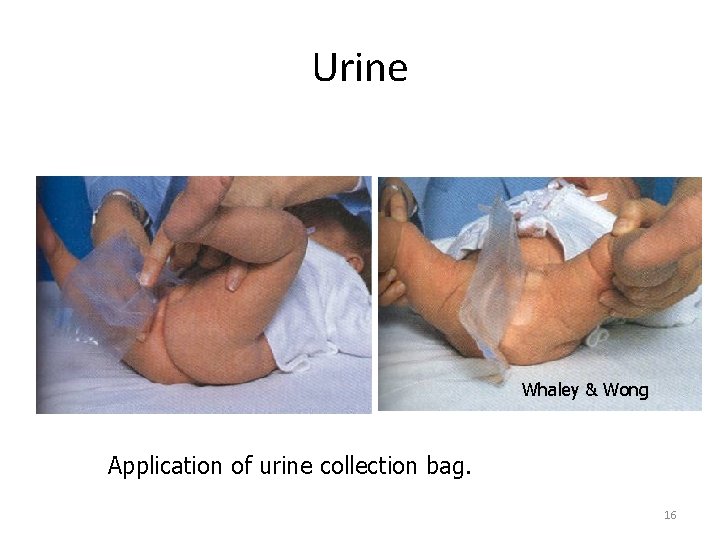
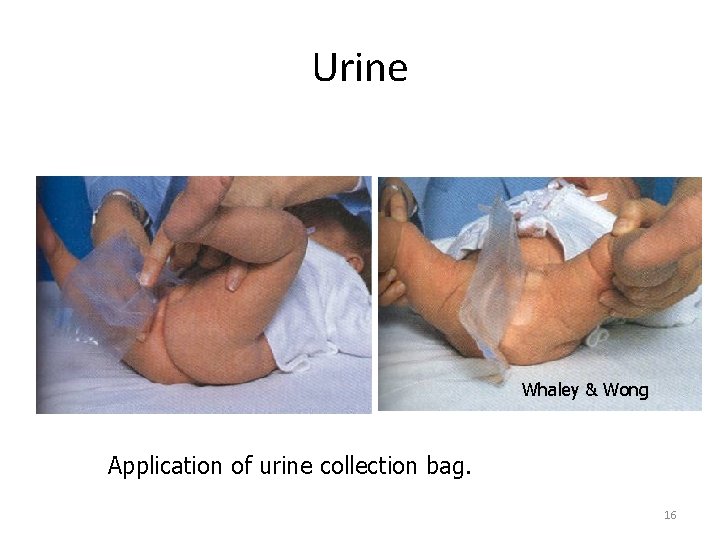
Urine Whaley & Wong Application of urine collection bag. 16
Urinary Tract Infections 17
Urinary tract infection (UTI)? • A urinary tract infection is an infection of the bladder (cystitis) or kidney(s) (pyelonephritis). • Cystitis is considerably more common than the more severe and more serious pyelonephritis. Classification of UTI: • Urethritis: inflammation of the urethra • Cystitis: inflammation of the bladder • Ureteritis: inflammation of the ureters • Pyelonephritis: inflammation of the upper urinary tract and kidneys 18
Causes urinary tract infections in children Escherichia coli accounts for 80% of all cases. 2 Anatomical factors – stasis of urine due to incomplete bladder emptying. – Vesicoureteric reflux (the backward flow of urine from the bladder into the ureters during voiding) Physical factors – The presence of urinary catheters allows ascending infection of the urinary tract. – Tight clothing or pants, . – Bubble baths and shampoos can irritate the ureters in both boys and girls and increase the risk of developing infection. 3 Chemical factors – An adequate fluid intake promotes flushing of the bladder, thereby reducing the number of organisms in the urine. – Urine is slightly acidic and most pathogens favour an alkaline medium. Certain beverages such as cranberry juice are thought to lower urinary p. H. 19
Sign and Symptom Specific • • • Frequency Urgency Dysuria Small volumes of urine passed Lower abdominal or flank pain Enuresis in a previously continent child Fever Haematuria Vomiting Smell from urine non-specific • Failure to thrive • Vomiting and diarrhoea • Jaundice • Pyrexia • Irritability • Strong smell from urine • Persistent nappy rash • Frequent/infrequent voiding • Screaming on voiding 20
Management 1. Elimination of the current infection 2. Identification of contributing factors in order to reduce recurrence 3. Prevention of systematic spread of the infection and the preservation of renal function. 21
Can UTIs in children be prevented 1. Hygiene: Wipe females from front to back during diaper changes or after using the toilet in older girls. With uncircumcised males, mild and gentle traction of the foreskin helps to expose the urethral opening. Most boys are able to fully retract the foreskin by 4 years of age. 2. Complete bladder emptying: 3. Avoid the carbonated drinks, high amounts of citrus, caffeine (sodas), and chocolate. 4. Avoid bubble baths 5. Prophylactic antibiotics: Daily low-dose antibiotics under a doctor's supervision may be used in children with recurrent UTIs. 22
Interventions • Antibiotic therapy for 7 to 10 days – E-coli most common organism 85% – Amoxicillin or Cefazol or Bactrim or Septra • • • Increase fluid intake Cranberry juice Sitz bath / tub bath Acetaminophen for pain Teach proper cleansing 23
Enuresis • Unable to control bladder function although reached an age at which control of voiding is expected • “Nocturnal Enuresis”—Bed wetting 24
Pathophys and etiology of Enuresis • Control of urination is r/t maturation of CNS • By 5 years, most are aware of bladder fullness and can control voiding • Daytime first with nighttime dryness later • Girls seems to master before boys • Children with primary enuresis may have delayed maturations of this part of CNS. They are not able to “sense” bladder fullness and do not awaken to void 25
Nsg Dx: Enuresis • low self-esteem r/t bedwetting or urinary incontinence • Impaired social interaction r/t bedwetting or urinary incontinence • Ineffective family coping r/t negative social response 26
Interventions • Pharmacological intervention: – Desmopressin synthetic vasopressin acts by reducing urine production and increasing water retention and concentration – Tofranil: anticholinrgic effect – FDA approval for treatment of enuresis • Side effect may be dry mouth and constipation • Some CNS: anxiety or confusion • Need to be weaned off 27
Treatment Enuresis • Diet control – Reduce fluids in evening – Control sugar intake • Bladder training – Praise and reward – Behavioral chart to keep track of dry nights – Alarm system 28
Obstructive uropathy • Obstructive uropathy is a condition in which the flow of urine is blocked, causing it to back up and injury one or both kidneys. 29
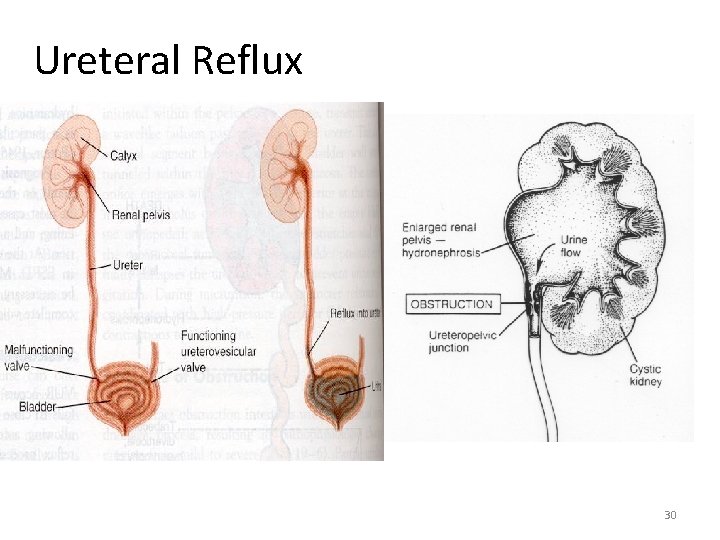
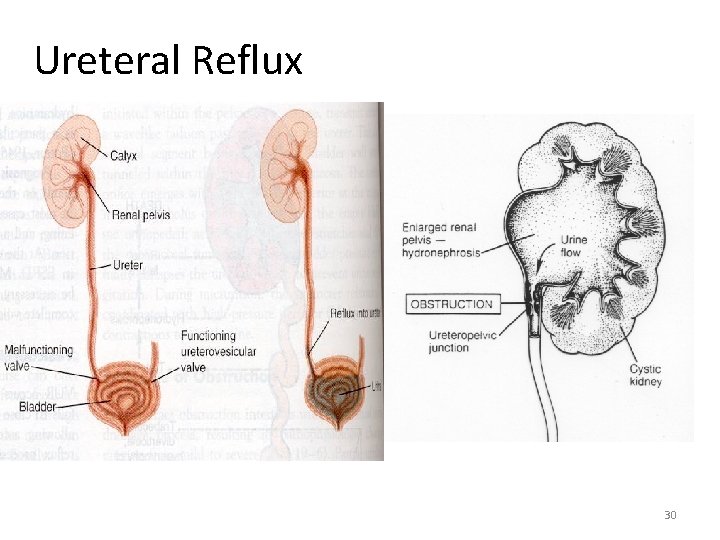
Ureteral Reflux 30
Common causes of obstructive uropathy include: • • • Bladder stones Kidney stones Benign prostatic hyperplasia (enlarged prostate) Bladder or ureteral cancer Colon cancer Cervical cancer Uterine cancer Any cancer that spreads Problems with the nerves that supply the bladder 31
Symptoms may include: • Mild to severe pain in the middle of the body (flank pain). • Fever • Weight gain or swelling (edema) • Urge to urinate often • Decrease in the force of urine stream • Dribbling of urine • Not feeling as if the bladder is emptied • Decreased amount of urine • Blood in urine 32
Treatment 1. Stents or drains placed in the ureter or in a part of the kidney called the renal pelvis may provide short-term relief of symptoms. 2. Nephrostomy tubes, which drain urine from the kidneys through the back, may be used to bypass the obstruction. 3. A Foley catheter, placed through the urethra into the bladder, may also be helpful. 33
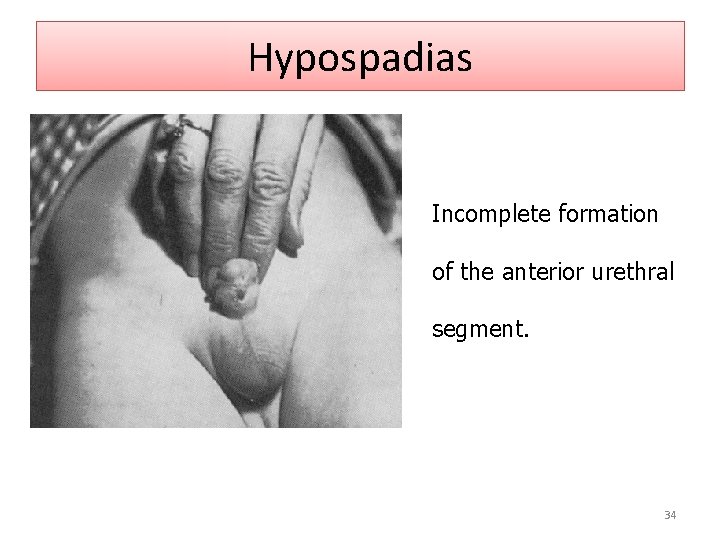
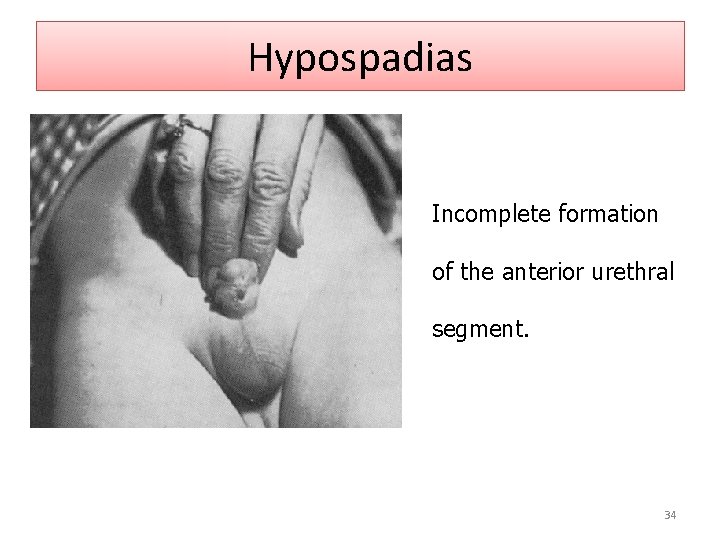
Hypospadias Incomplete formation of the anterior urethral segment. 34
Hypospadias • Incomplete formation of the anterior urethral segment • Cordee – downward curve of penis. • Goal of surgery: to make urinary & sexual function as normal as possible and improve appearance of penis 35
Nsg Dx: Hypospadius • Knowledge deficit (parental) r/t diagnosis, surgical correction, & post-op care • Risk of infection r/t indwelling catheter • Impaired physical mobility r/t surgical procedure of penis 36
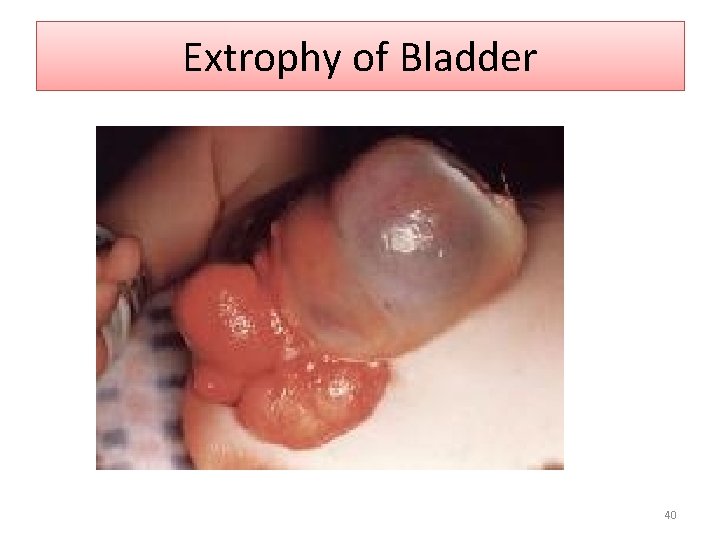
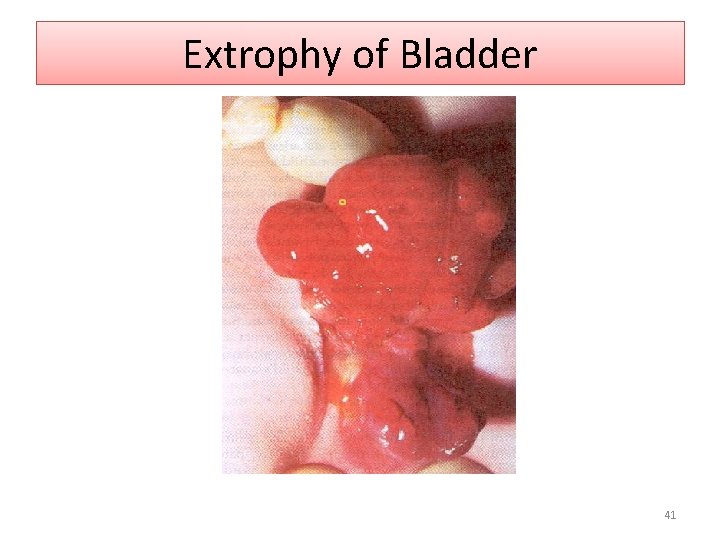
Extrophy of Bladder • Interrupted abdominal development in early fetal life produces an exposed bladder and urethra, pubic bone separation, and associated anal and genital abnormalities. 37
Extrophy of Bladder • Occurs is 1 of 400, 000 births • Congenital malformation in which the lower portion of abdominal wall and anterior bladder wall fail to fuse during fetal development. 38
Clinical Manifestations • Visible defect that reveals bladder mucosa and ureteral orifices through an open abdominal wall with constant drainage of urine. 39
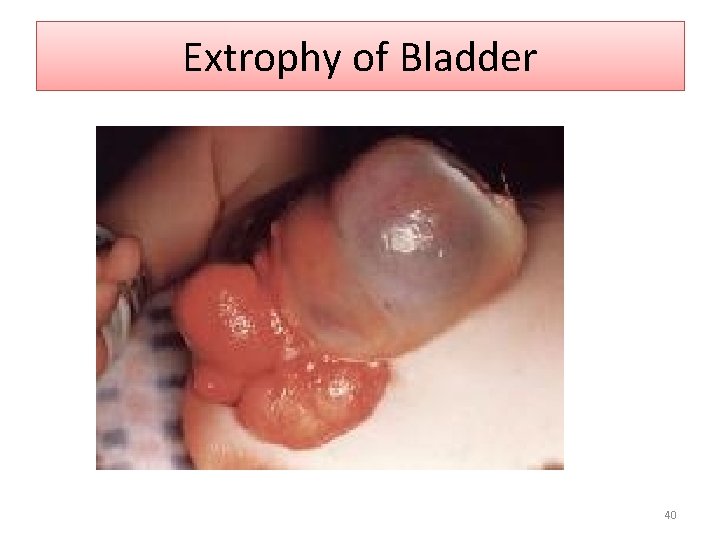
Extrophy of Bladder 40
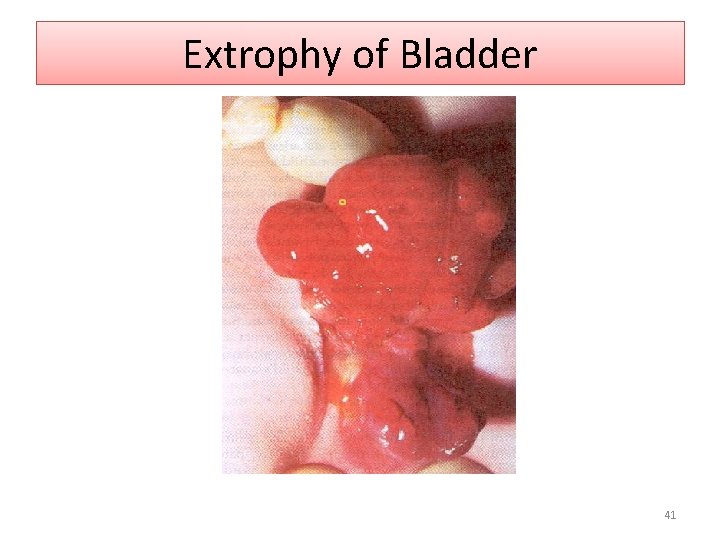
Extrophy of Bladder 41
Treatment • Surgery within first hours of life to close the skin over the bladder and reconstruct the male urethra and penis. • Urethral stents and suprapubic catheter to divert urine • Further reconstructive surgery can be done between 18 months to 3 years of age 42
Goals of Treatment • Preserve renal function: prevent infection • Attain urinary control • Re-constructive repair • Sexual function 43
Long Term Complications • Urinary incontinence • Infection • Body image • Inadequate sexual function 44