Almost Everything You Wanted To Know About ECGs
Almost Everything You Wanted To Know About ECGs (But Were Afraid To Ask) Amy Gutman MD ~ EMS Medical Director prehospitalmd@gmail. com / www. TEAEMS. com
Overview Part I: Cardiac Anatomy Review Part II: The Cardiac Cycle Part III: From One Beat to Many Part IV: Rhythm Analysis

Part One: Cardiac Anatomy What is an EKG really looking at?
Electrocardiogram (ECG or EKG) German “Elektrokardiogramm” Record of the heart’s electrical depolarizations & repolarizations over time Arrhythmias, ischemia, & conduction abnormalities Electrolyte disturbances Non-cardiac diseases (i. e. hypothermia, PE)

3 Lead vs 12 Lead 3 lead “overview” image of heart I (lateral) II (inferior) III (inferior) Useful for checking arrhythmias Not great for looking for ischemic changes

What is a 12 Lead EKG?

EKG = Electrical Record of Cardiac Activity
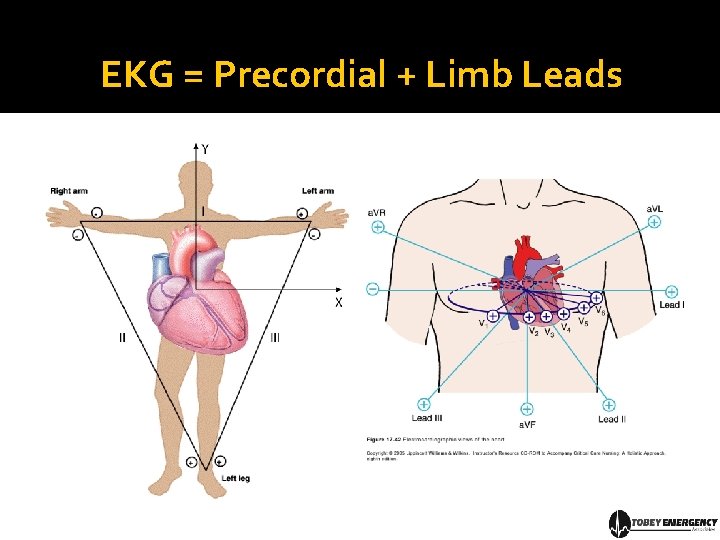
EKG = Precordial + Limb Leads

Limb Leads I, II & III are “limb leads” Leads a. VR, a. VL, & a. VF are “augmented” limb leads
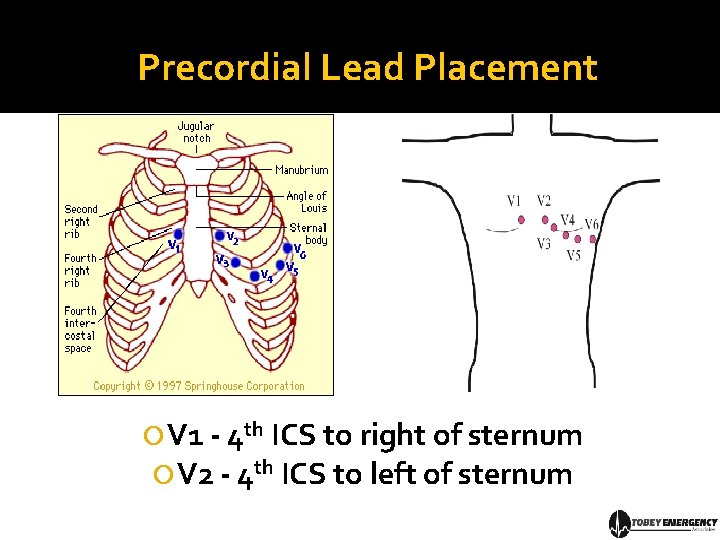
Precordial Lead Placement V 1 - 4 th ICS to right of sternum V 2 - 4 th ICS to left of sternum
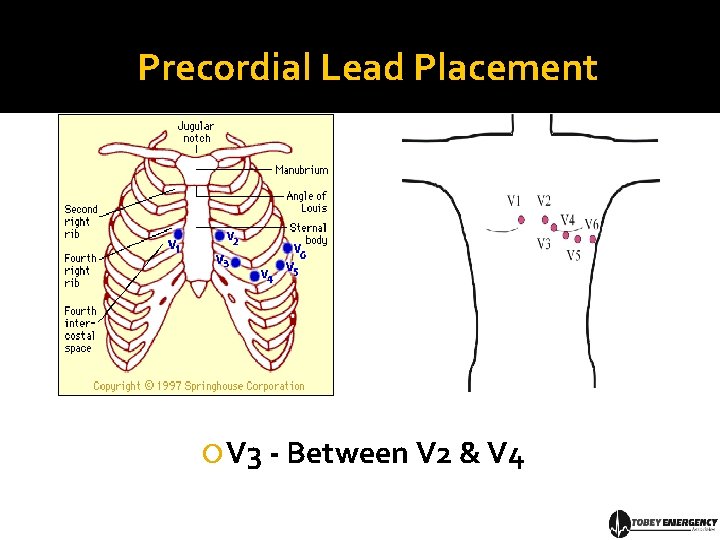
Precordial Lead Placement V 3 - Between V 2 & V 4

Precordial Lead Placement V 4 - 5 th ICS at MCL V 5 - Horizontally with V 4 at AAL
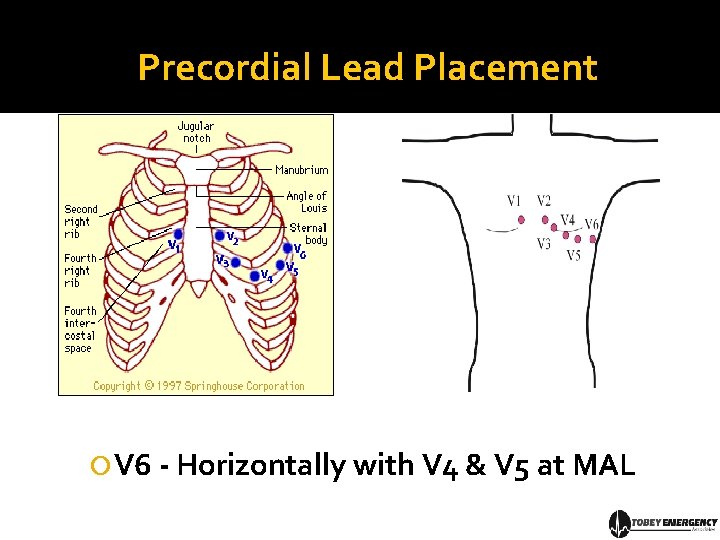
Precordial Lead Placement V 6 - Horizontally with V 4 & V 5 at MAL
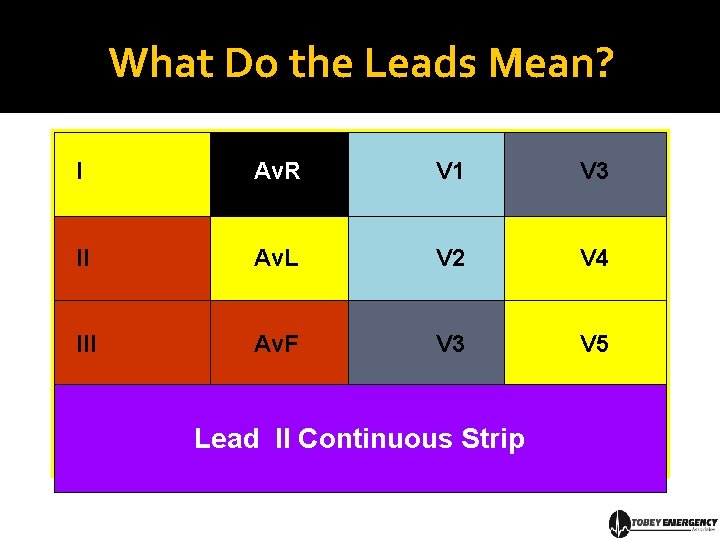
What Do the Leads Mean? I Av. R V 1 V 3 II Av. L V 2 V 4 III Av. F V 3 V 5 Lead II Continuous Strip
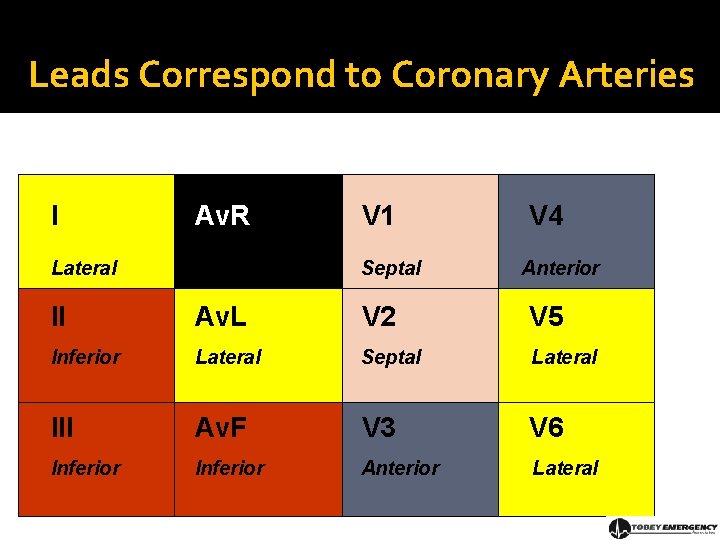
Leads Correspond to Coronary Arteries I Av. R Lateral V 1 Septal V 4 Anterior II Av. L V 2 V 5 Inferior Lateral Septal Lateral III Av. F V 3 V 6 Inferior Anterior Lateral

Coronary Arteries Right Coronary Artery (RCA) perfuses right ventricle / inferior heart Inferior heart Left Main Artery (LMA) divides into: Left Anterior Descending Artery (LAD) perfuses anterior left ventricle Left Circumflex Artery (LCX) perfuses lateral left ventricle
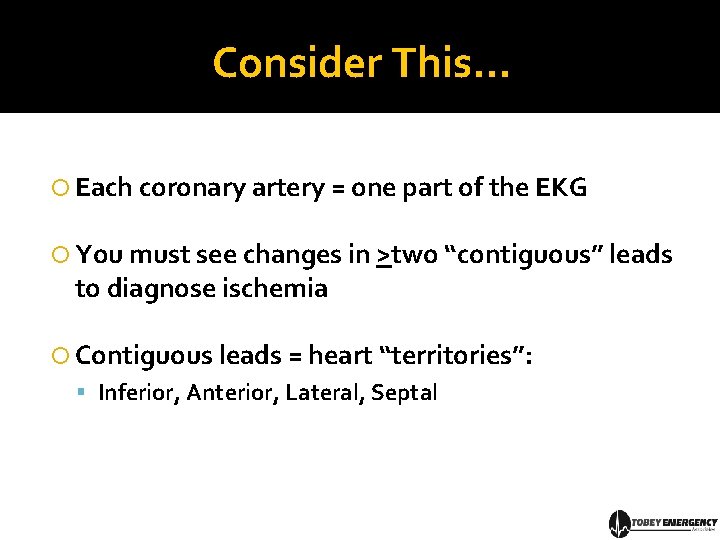
Consider This… Each coronary artery = one part of the EKG You must see changes in >two “contiguous” leads to diagnose ischemia Contiguous leads = heart “territories”: Inferior, Anterior, Lateral, Septal
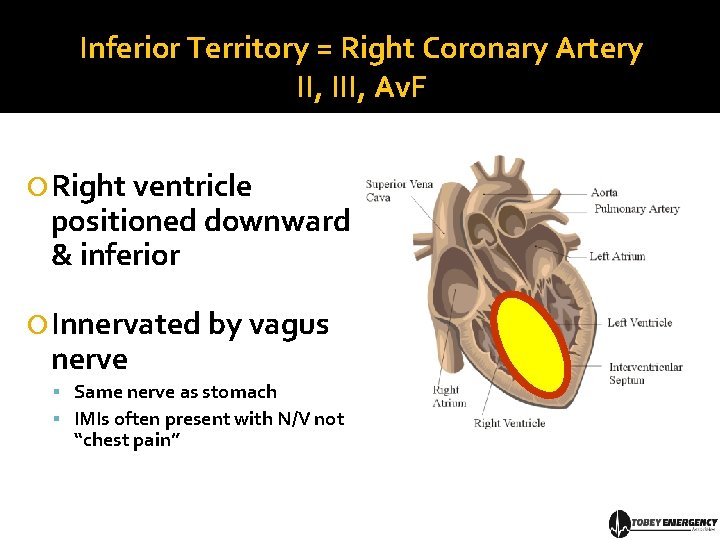
Inferior Territory = Right Coronary Artery II, III, Av. F Right ventricle positioned downward & inferior Innervated by vagus nerve Same nerve as stomach IMIs often present with N/V not “chest pain”
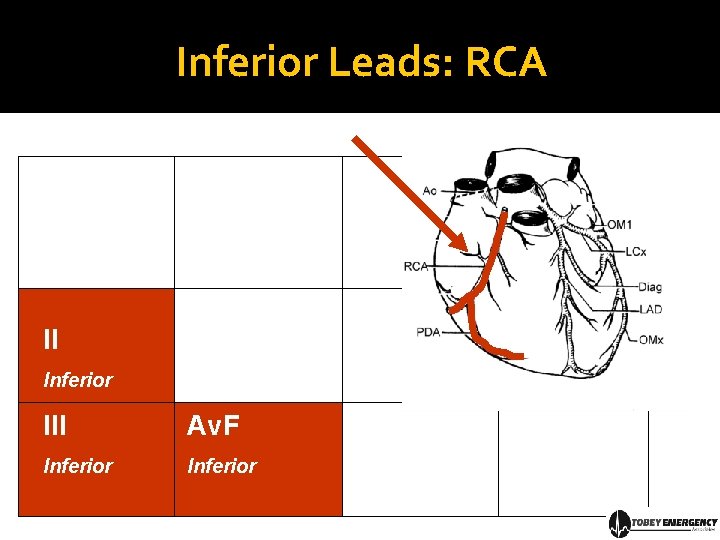
Inferior Leads: RCA II Inferior III Av. F Inferior
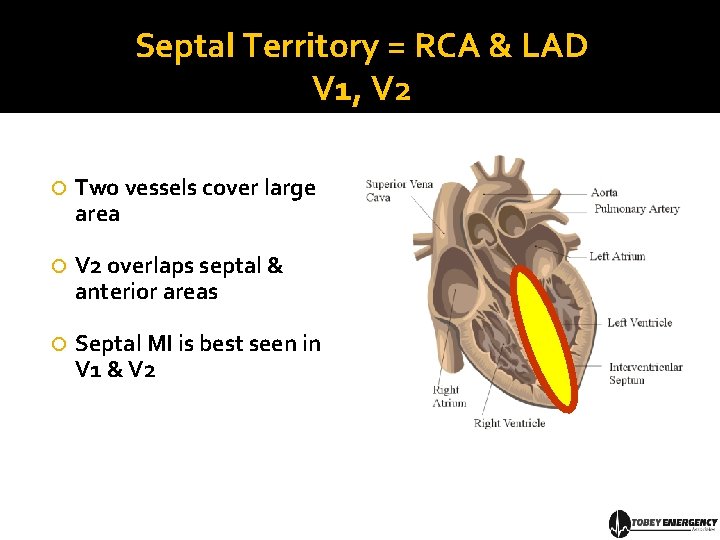
Septal Territory = RCA & LAD V 1, V 2 Two vessels cover large area V 2 overlaps septal & anterior areas Septal MI is best seen in V 1 & V 2
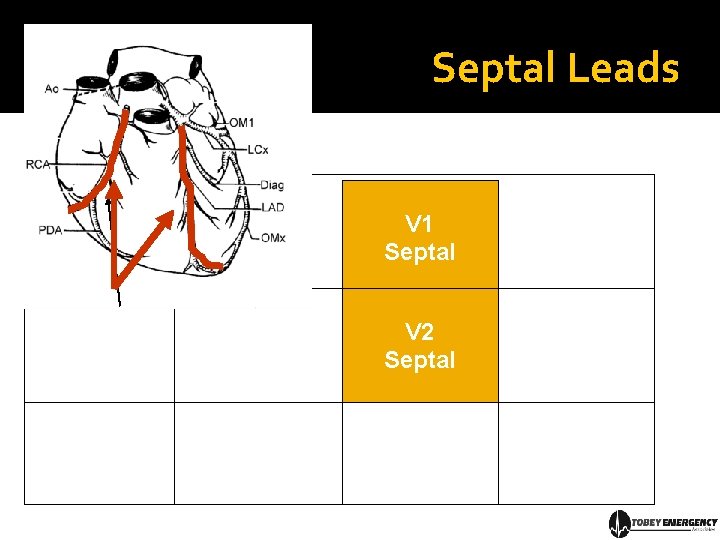
Septal Leads V 1 Septal V 2 Septal
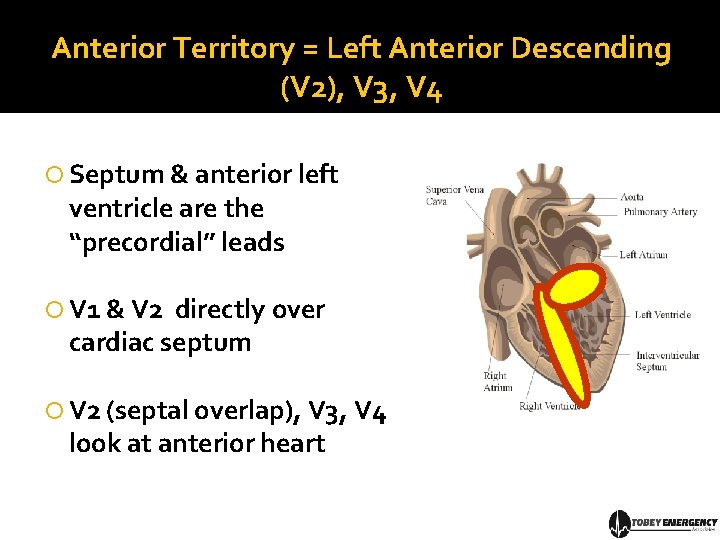
Anterior Territory = Left Anterior Descending (V 2), V 3, V 4 Septum & anterior left ventricle are the “precordial” leads V 1 & V 2 directly over cardiac septum V 2 (septal overlap), V 3, V 4 look at anterior heart
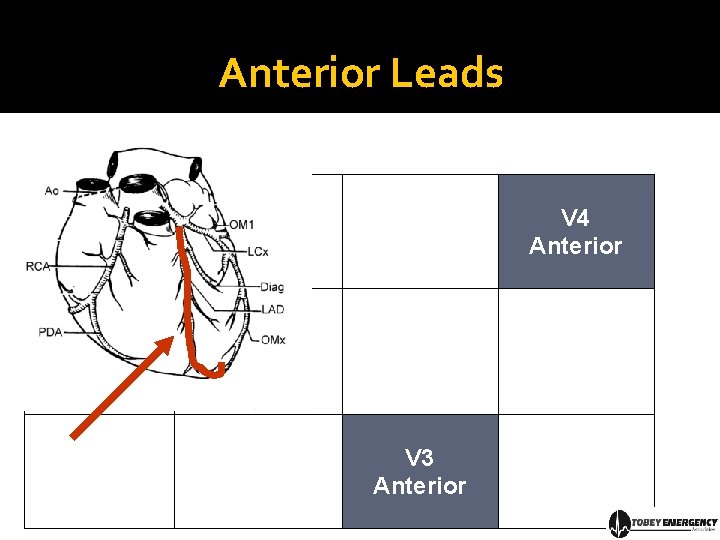
Anterior Leads V 4 Anterior V 3 Anterior
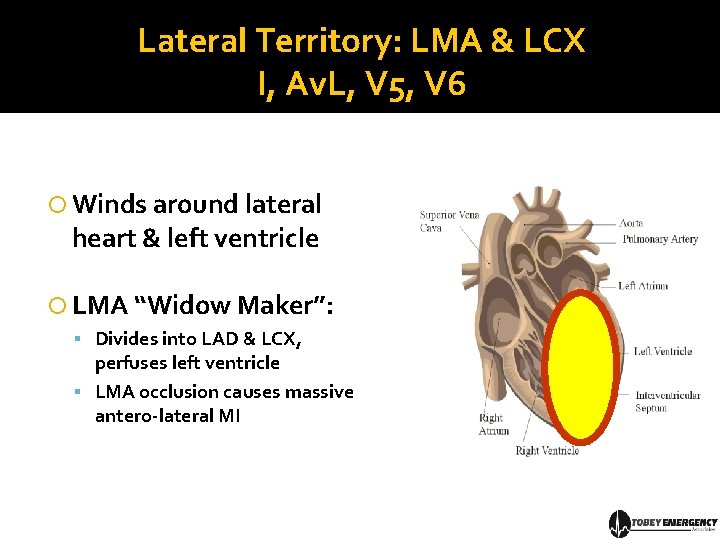
Lateral Territory: LMA & LCX I, Av. L, V 5, V 6 Winds around lateral heart & left ventricle LMA “Widow Maker”: Divides into LAD & LCX, perfuses left ventricle LMA occlusion causes massive antero-lateral MI
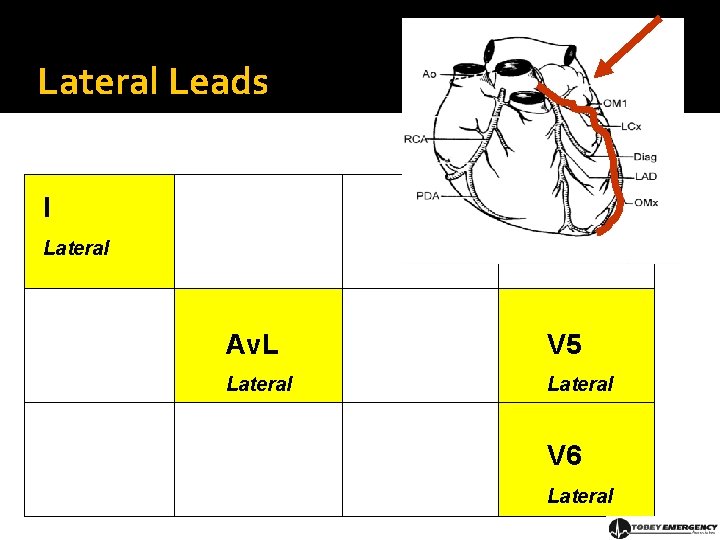
Lateral Leads I Lateral Av. L V 5 Lateral V 6 Lateral
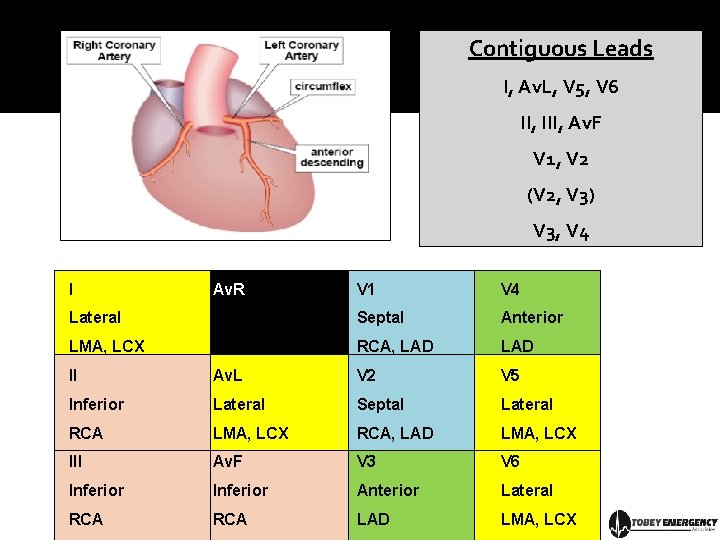
Contiguous Leads I, Av. L, V 5, V 6 II, III, Av. F V 1, V 2 (V 2, V 3) V 3, V 4 I Av. R V 1 V 4 Lateral Septal Anterior LMA, LCX RCA, LAD II Av. L V 2 V 5 Inferior Lateral Septal Lateral RCA LMA, LCX RCA, LAD LMA, LCX III Av. F V 3 V 6 Inferior Anterior Lateral RCA LAD LMA, LCX
Part II: The Cardiac Cycle The heart is nothing more than a mechanical pump running on electricity
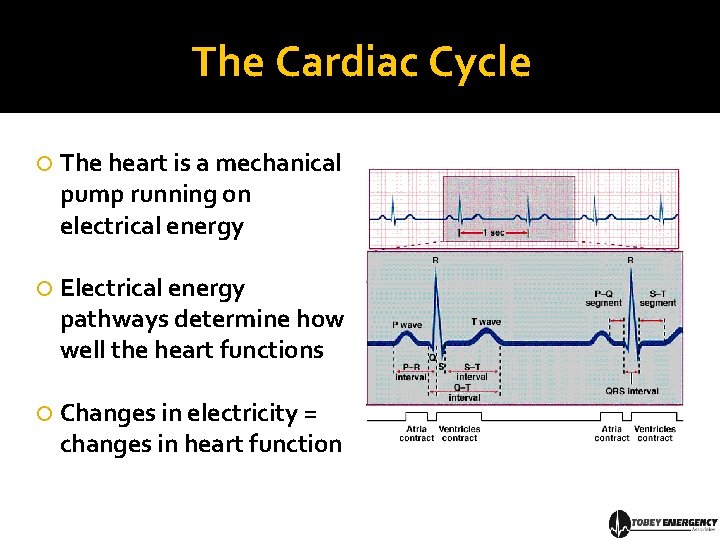
The Cardiac Cycle The heart is a mechanical pump running on electrical energy Electrical energy pathways determine how well the heart functions Changes in electricity = changes in heart function
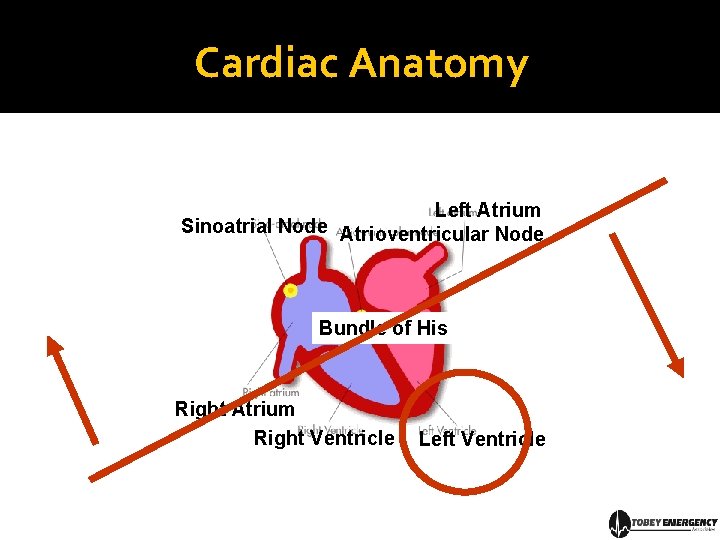
Cardiac Anatomy Left Atrium Sinoatrial Node Atrioventricular Node Bundle of His Right Atrium Right Ventricle Left Ventricle
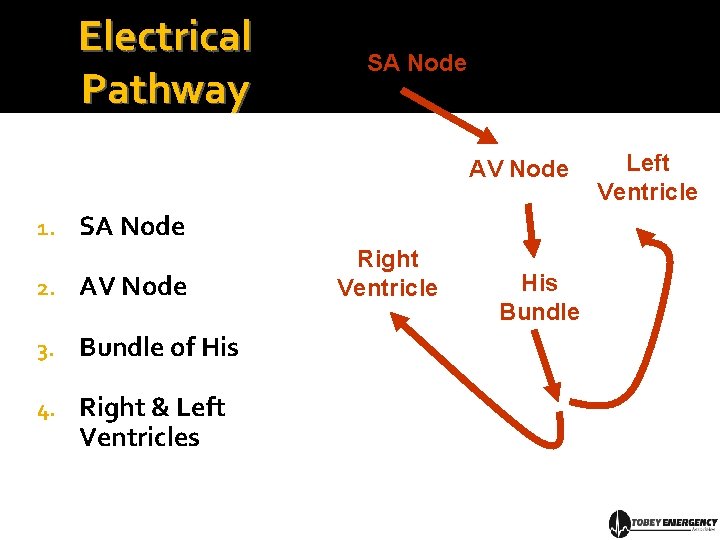
Electrical Pathway SA Node AV Node 1. SA Node 2. AV Node 3. Bundle of His 4. Right & Left Ventricles Right Ventricle His Bundle Left Ventricle
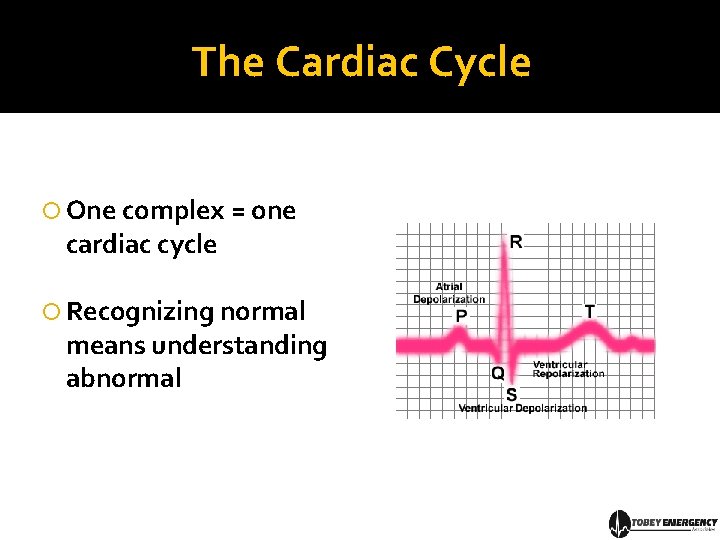
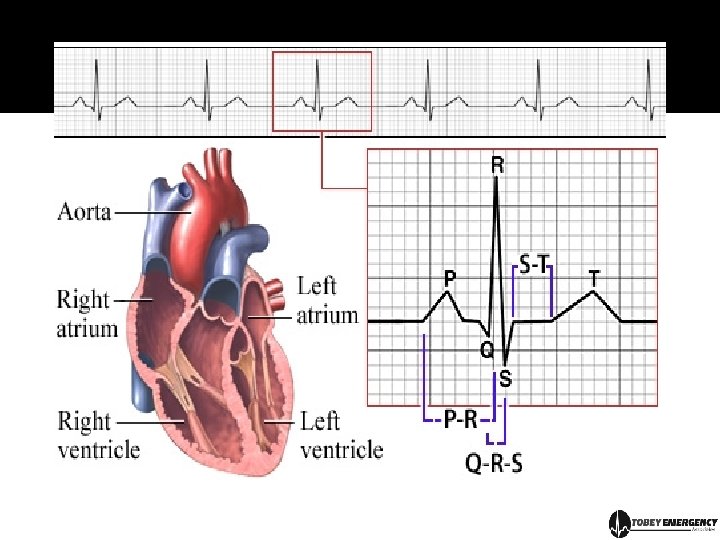
The Cardiac Cycle One complex = one cardiac cycle Recognizing normal means understanding abnormal
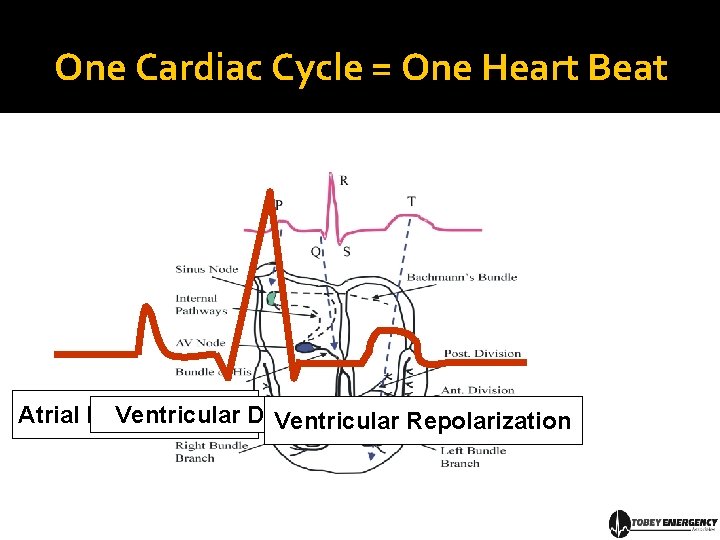
One Cardiac Cycle = One Heart Beat Atrial Depolarization Ventricular Repolarization
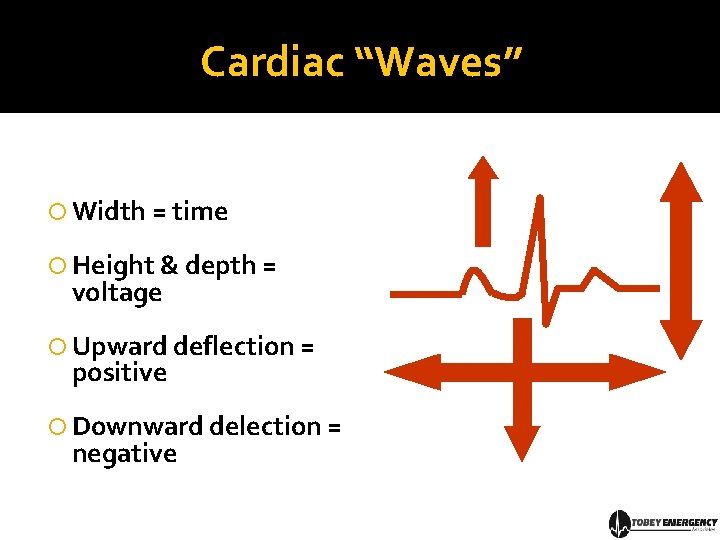
Cardiac “Waves” Width = time Height & depth = voltage Upward deflection = positive Downward delection = negative
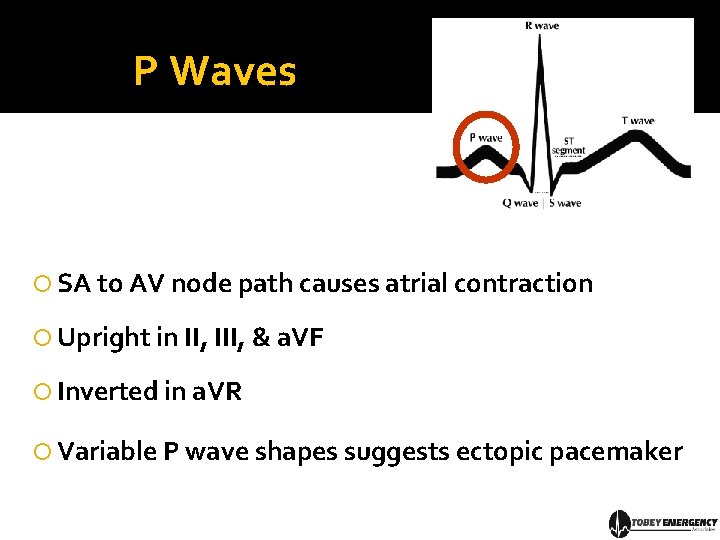
P Waves SA to AV node path causes atrial contraction Upright in II, III, & a. VF Inverted in a. VR Variable P wave shapes suggests ectopic pacemaker
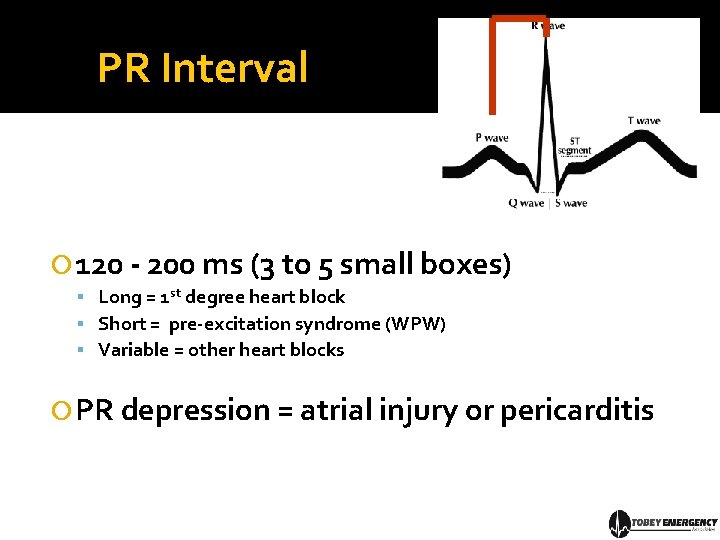
PR Interval 120 - 200 ms (3 to 5 small boxes) Long = 1 st degree heart block Short = pre-excitation syndrome (WPW) Variable = other heart blocks PR depression = atrial injury or pericarditis
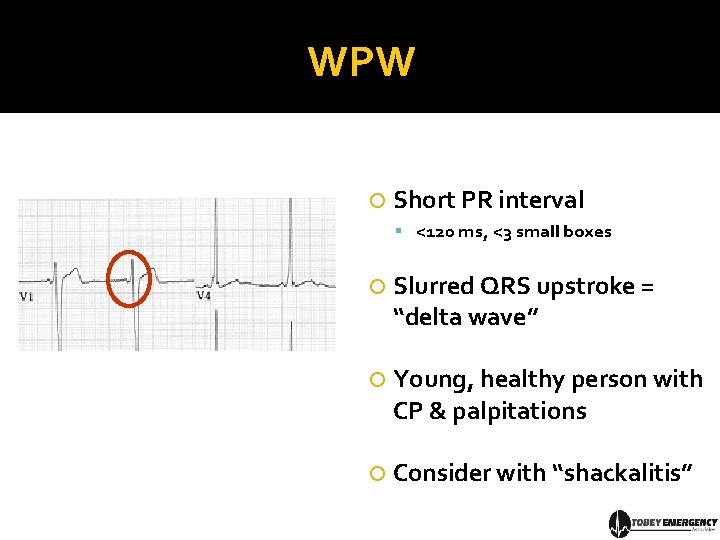
WPW Short PR interval <120 ms, <3 small boxes Slurred QRS upstroke = “delta wave” Young, healthy person with CP & palpitations Consider with “shackalitis”
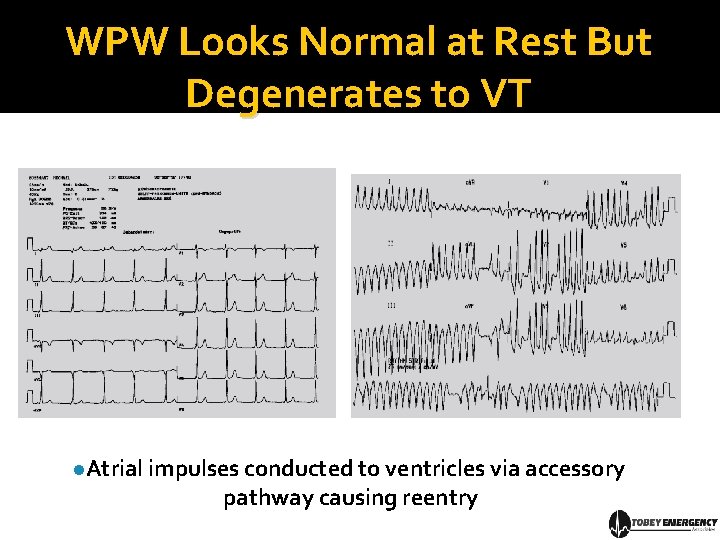
WPW Looks Normal at Rest But Degenerates to VT l. Atrial impulses conducted to ventricles via accessory pathway causing reentry
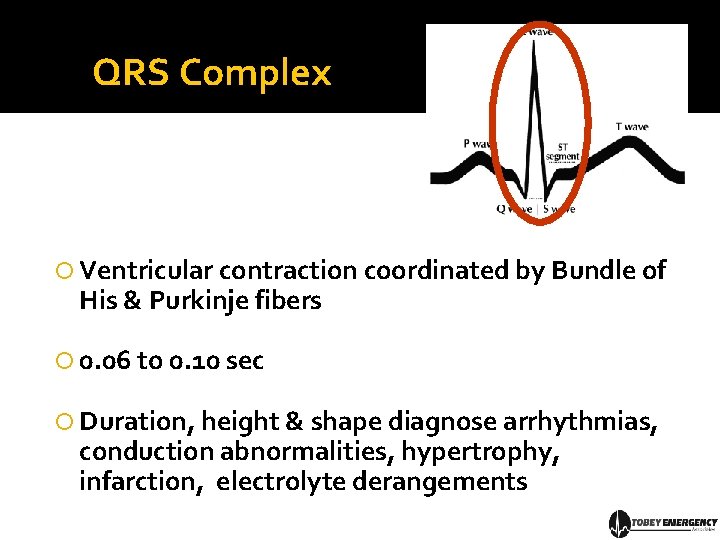
QRS Complex Ventricular contraction coordinated by Bundle of His & Purkinje fibers 0. 06 to 0. 10 sec Duration, height & shape diagnose arrhythmias, conduction abnormalities, hypertrophy, infarction, electrolyte derangements
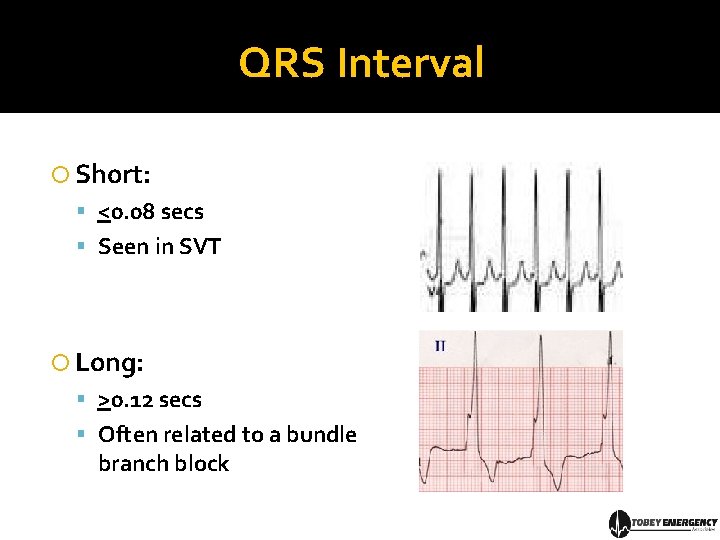
QRS Interval Short: <0. 08 secs Seen in SVT Long: >0. 12 secs Often related to a bundle branch block
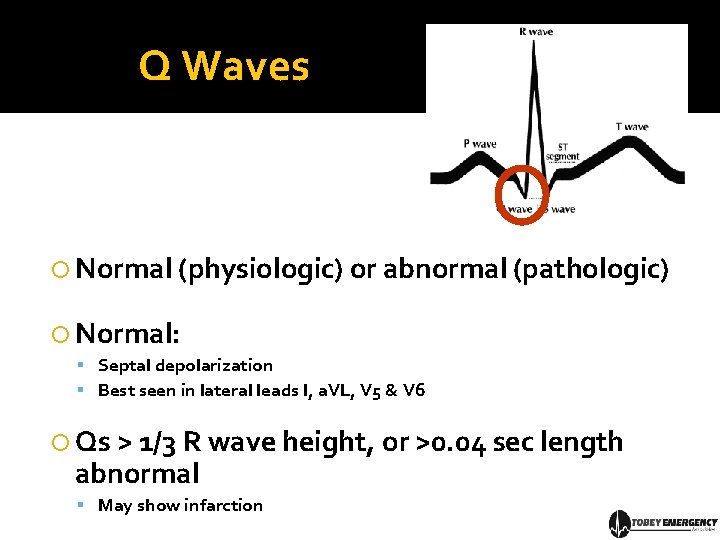
Q Waves Normal (physiologic) or abnormal (pathologic) Normal: Septal depolarization Best seen in lateral leads I, a. VL, V 5 & V 6 Qs > 1/3 R wave height, or >0. 04 sec length abnormal May show infarction
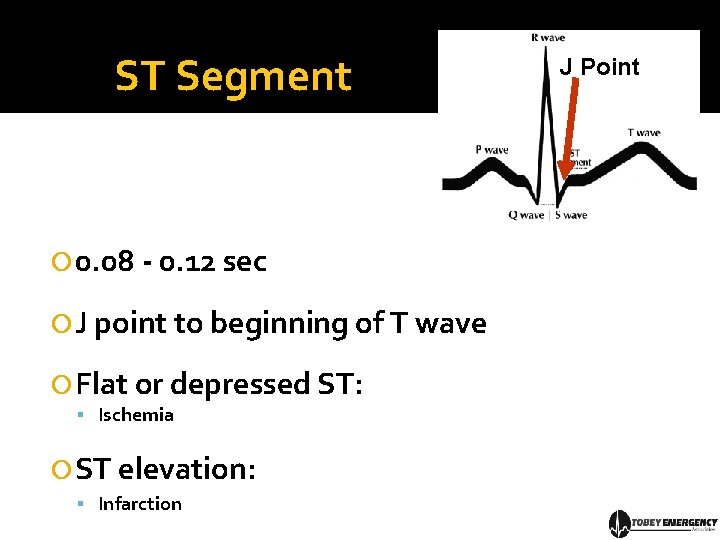
ST Segment 0. 08 - 0. 12 sec J point to beginning of T wave Flat or depressed ST: Ischemia ST elevation: Infarction J Point
T Wave Ventricular repolarization T wave usually upright Inverted: ischemia, hypertrophy, CVA Tall: hyperkalemia Flat: ischemia, hypokalemia
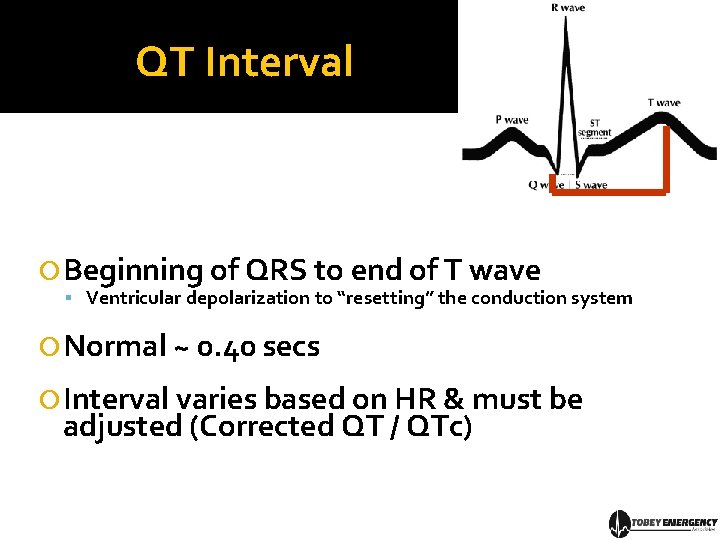
QT Interval Beginning of QRS to end of T wave Ventricular depolarization to “resetting” the conduction system Normal ~ 0. 40 secs Interval varies based on HR & must be adjusted (Corrected QT / QTc)
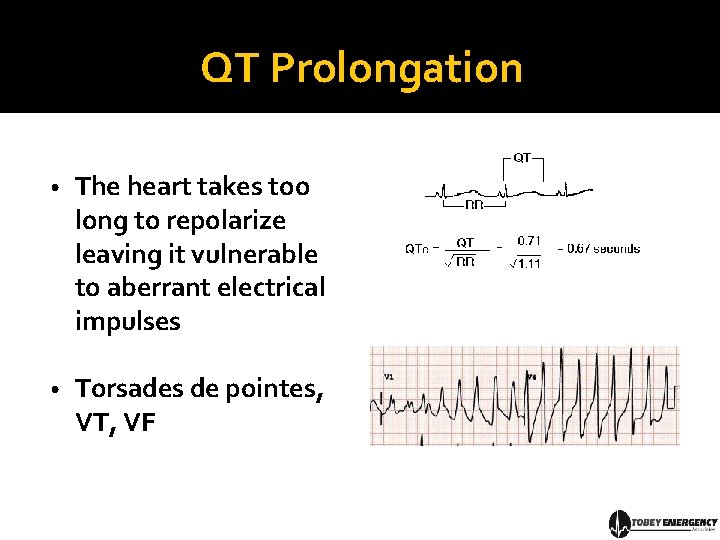
QT Prolongation • The heart takes too long to repolarize leaving it vulnerable to aberrant electrical impulses • Torsades de pointes, VT, VF
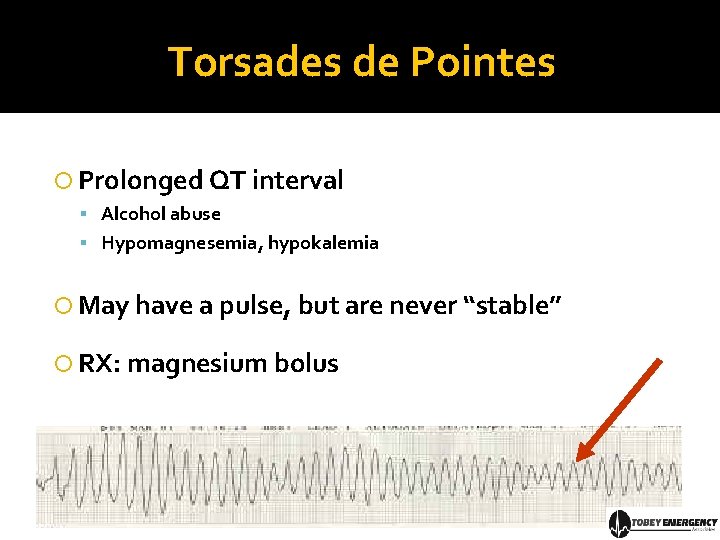
Torsades de Pointes Prolonged QT interval Alcohol abuse Hypomagnesemia, hypokalemia May have a pulse, but are never “stable” RX: magnesium bolus
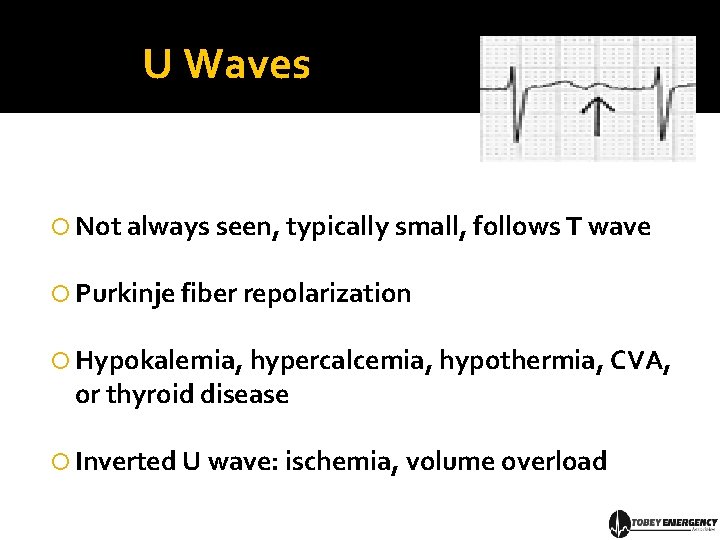
U Waves Not always seen, typically small, follows T wave Purkinje fiber repolarization Hypokalemia, hypercalcemia, hypothermia, CVA, or thyroid disease Inverted U wave: ischemia, volume overload
Part III: From One Beat to Many Putting it together…
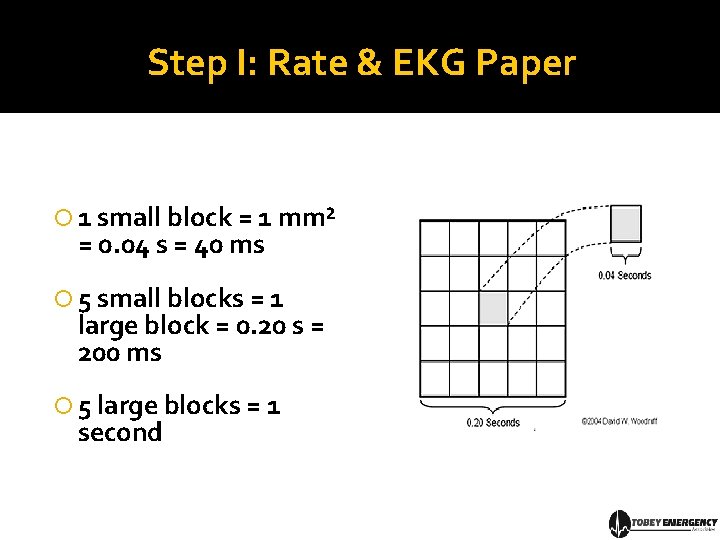
Step I: Rate & EKG Paper 1 small block = 1 mm² = 0. 04 s = 40 ms 5 small blocks = 1 large block = 0. 20 s = 200 ms 5 large blocks = 1 second
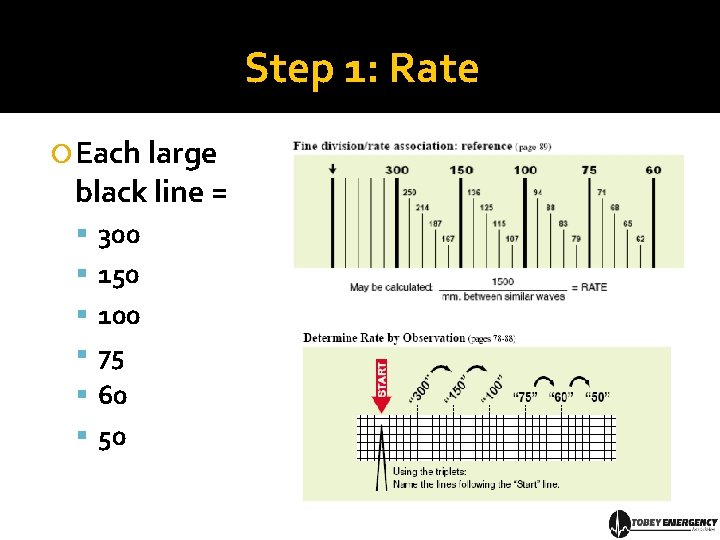
Step 1: Rate Each large black line = 300 150 100 75 60 50
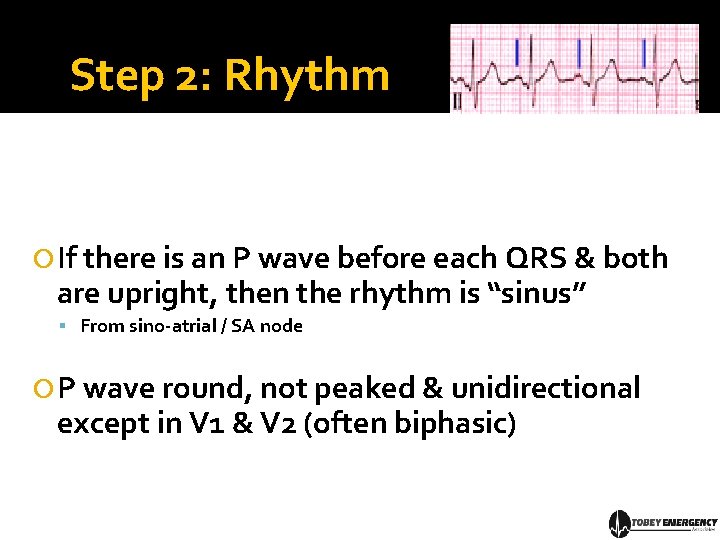
Step 2: Rhythm If there is an P wave before each QRS & both are upright, then the rhythm is “sinus” From sino-atrial / SA node P wave round, not peaked & unidirectional except in V 1 & V 2 (often biphasic)
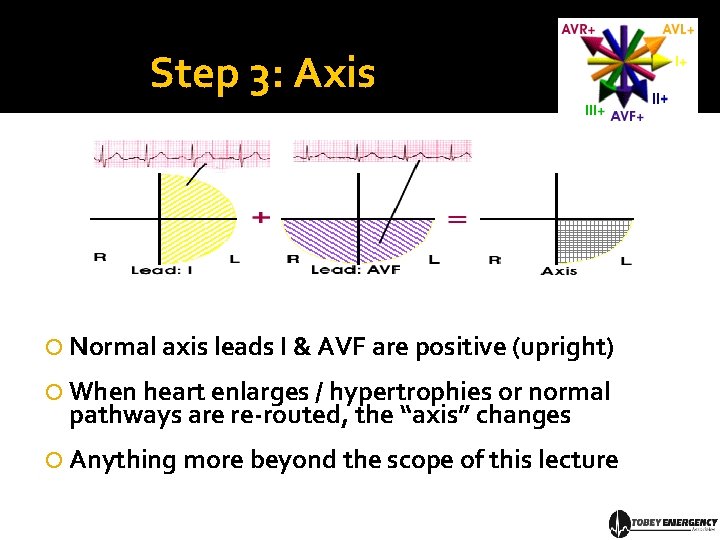
Step 3: Axis Normal axis leads I & AVF are positive (upright) When heart enlarges / hypertrophies or normal pathways are re-routed, the “axis” changes Anything more beyond the scope of this lecture
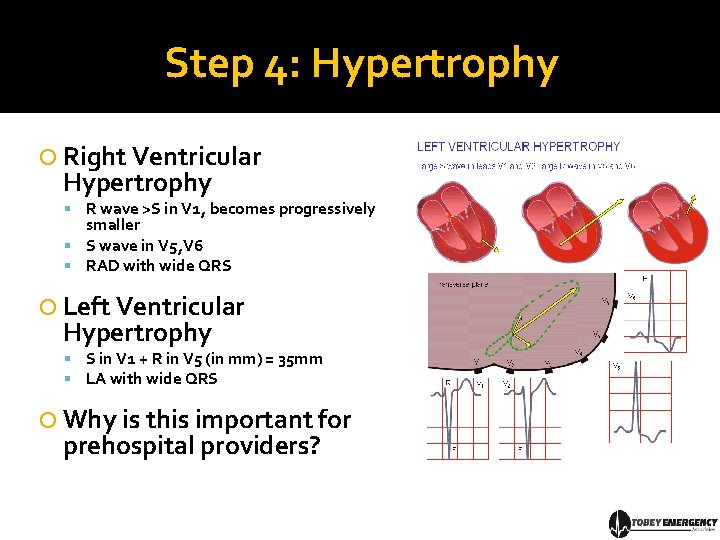
Step 4: Hypertrophy Right Ventricular Hypertrophy R wave >S in V 1, becomes progressively smaller S wave in V 5, V 6 RAD with wide QRS Left Ventricular Hypertrophy S in V 1 + R in V 5 (in mm) = 35 mm LA with wide QRS Why is this important for prehospital providers?
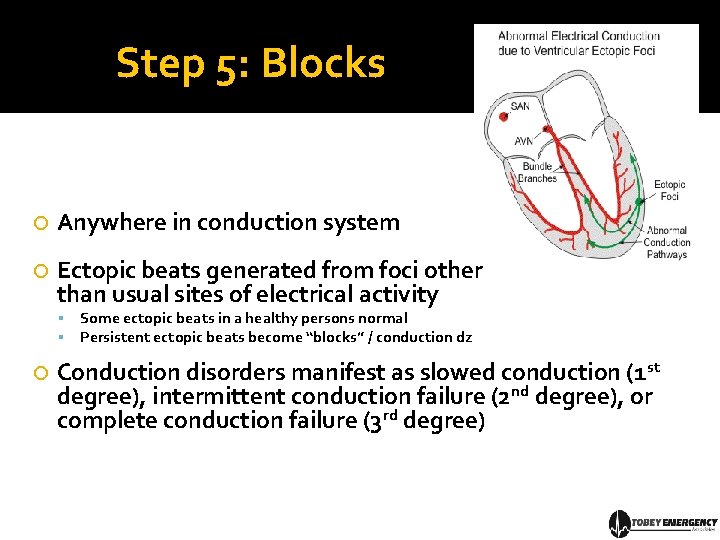
Step 5: Blocks Anywhere in conduction system Ectopic beats generated from foci other than usual sites of electrical activity Some ectopic beats in a healthy persons normal Persistent ectopic beats become “blocks” / conduction dz Conduction disorders manifest as slowed conduction (1 st degree), intermittent conduction failure (2 nd degree), or complete conduction failure (3 rd degree)
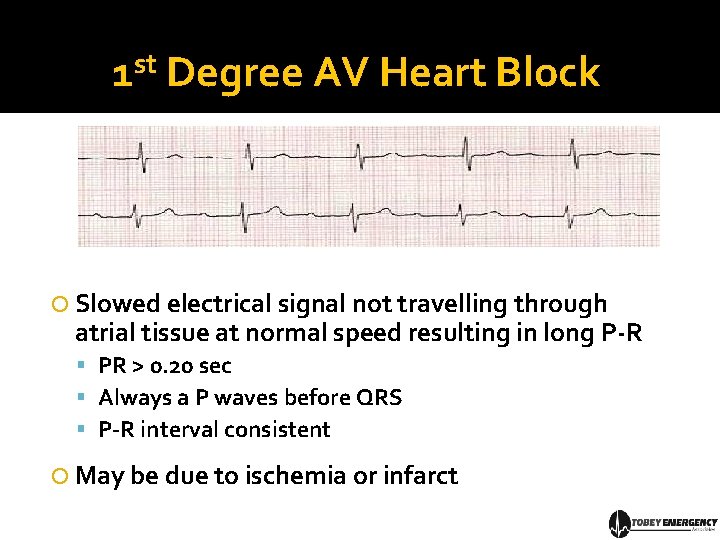
1 st Degree AV Heart Block Slowed electrical signal not travelling through atrial tissue at normal speed resulting in long P-R PR > 0. 20 sec Always a P waves before QRS P-R interval consistent May be due to ischemia or infarct
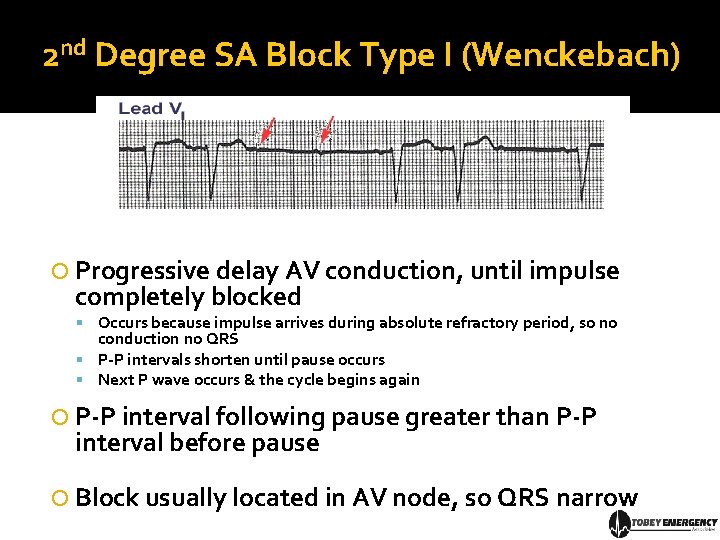
2 nd Degree SA Block Type I (Wenckebach) Progressive delay AV conduction, until impulse completely blocked Occurs because impulse arrives during absolute refractory period, so no conduction no QRS P-P intervals shorten until pause occurs Next P wave occurs & the cycle begins again P-P interval following pause greater than P-P interval before pause Block usually located in AV node, so QRS narrow
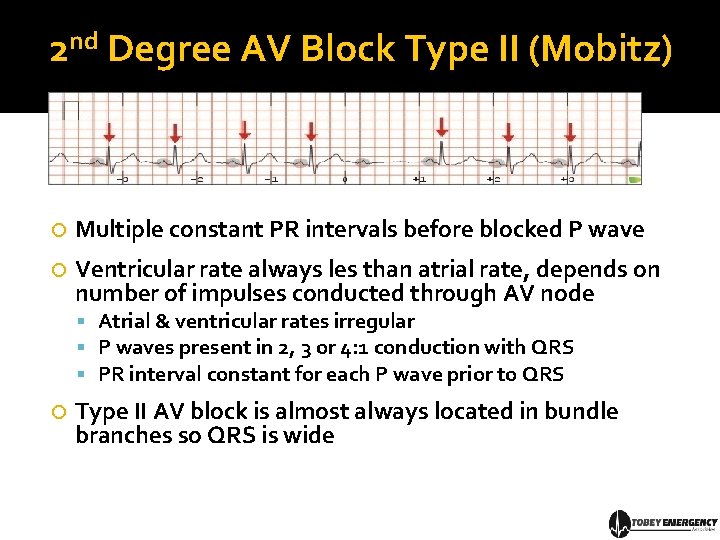
2 nd Degree AV Block Type II (Mobitz) Multiple constant PR intervals before blocked P wave Ventricular rate always les than atrial rate, depends on number of impulses conducted through AV node Atrial & ventricular rates irregular P waves present in 2, 3 or 4: 1 conduction with QRS PR interval constant for each P wave prior to QRS Type II AV block is almost always located in bundle branches so QRS is wide
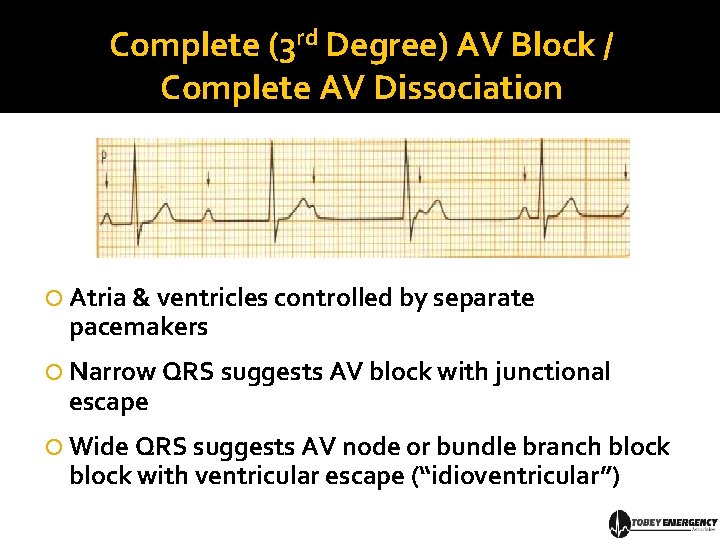
Complete (3 rd Degree) AV Block / Complete AV Dissociation Atria & ventricles controlled by separate pacemakers Narrow QRS suggests AV block with junctional escape Wide QRS suggests AV node or bundle branch block with ventricular escape (“idioventricular”)
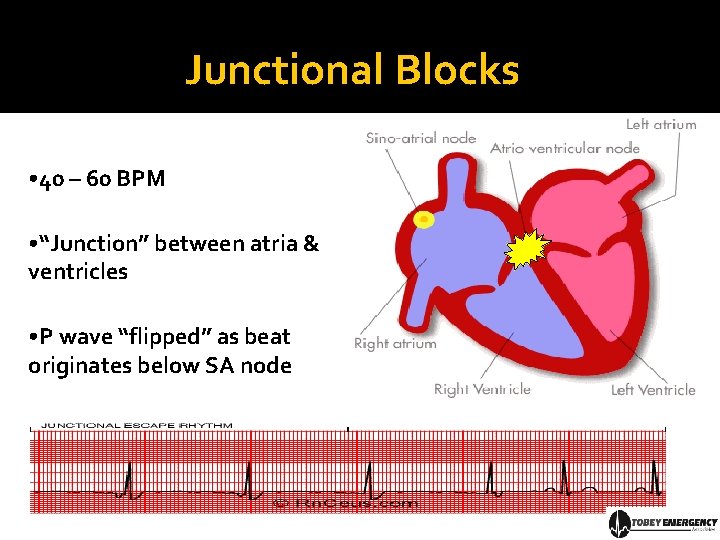
Junctional Blocks • 40 – 60 BPM • “Junction” between atria & ventricles • P wave “flipped” as beat originates below SA node
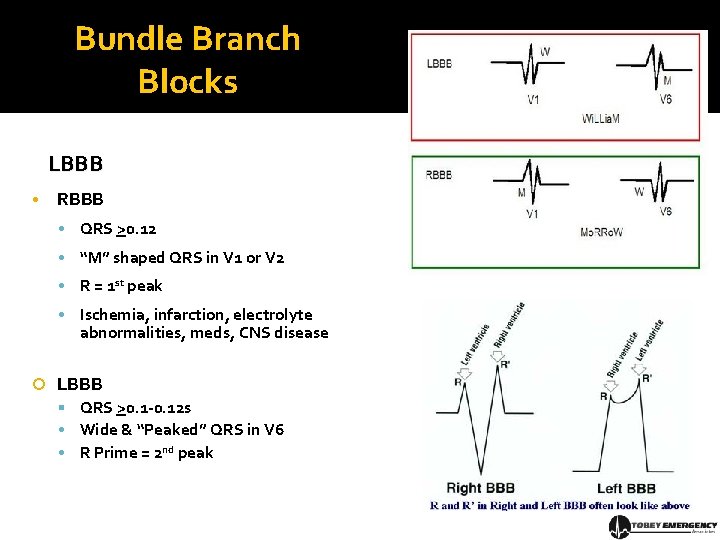
Bundle Branch Blocks LBBB • RBBB • QRS >0. 12 • “M” shaped QRS in V 1 or V 2 • R = 1 st peak • Ischemia, infarction, electrolyte abnormalities, meds, CNS disease LBBB QRS >0. 1 -0. 12 s • Wide & “Peaked” QRS in V 6 • R Prime = 2 nd peak
Step 6: Infarction Patterns Stage I: Ischemia Stage 2: Injury Stage 3: Infarction Stage 4: Resolution
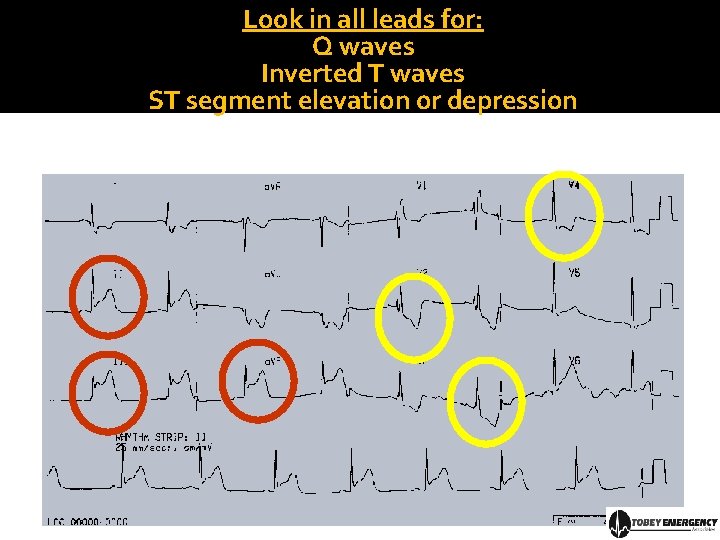
Look in all leads for: Q waves Inverted T waves ST segment elevation or depression
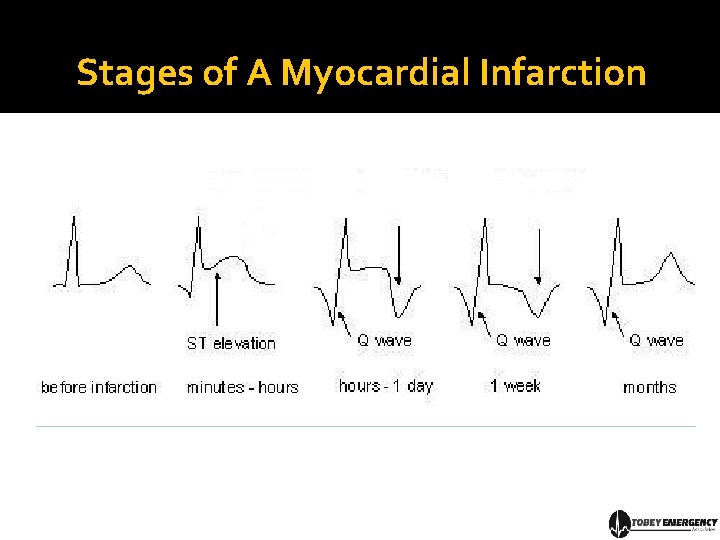
Stages of A Myocardial Infarction
Ischemia = T Wave Inversion • Normal T wave upright when QRS upright • If T wave inverted, then = ischemia • Try and compare with old EKG to determine if inversion is new or old
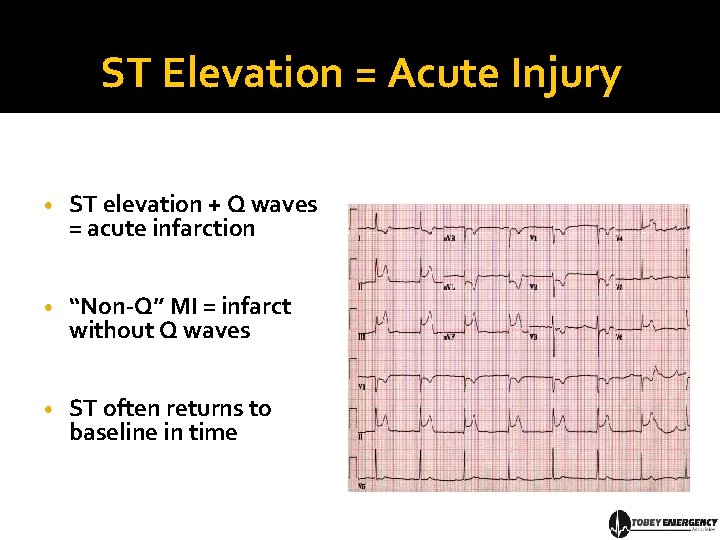
ST Elevation = Acute Injury • ST elevation + Q waves = acute infarction • “Non-Q” MI = infarct without Q waves • ST often returns to baseline in time
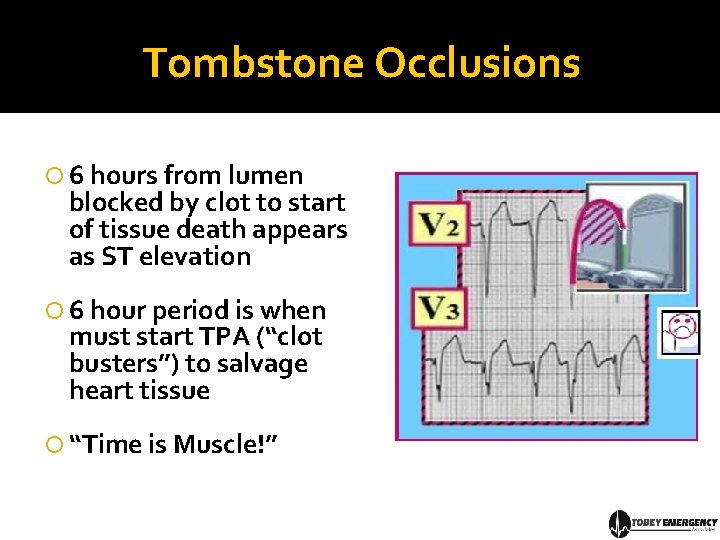
Tombstone Occlusions 6 hours from lumen blocked by clot to start of tissue death appears as ST elevation 6 hour period is when must start TPA (“clot busters”) to salvage heart tissue “Time is Muscle!”
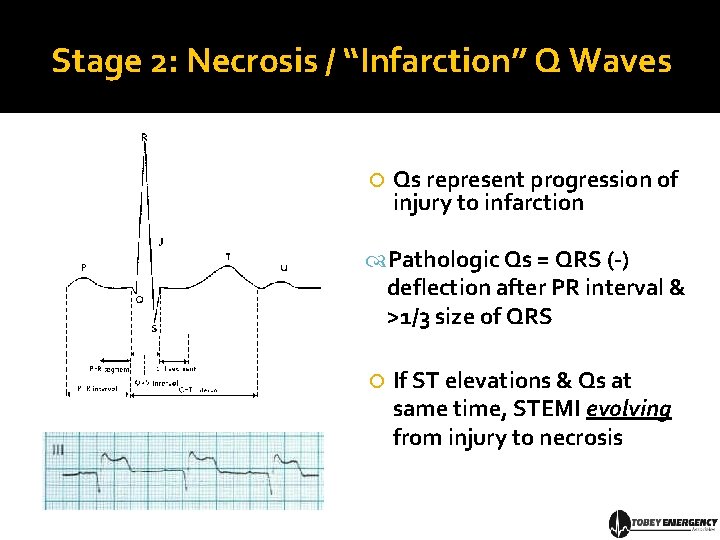
Stage 2: Necrosis / “Infarction” Q Waves Qs represent progression of injury to infarction Pathologic Qs = QRS (-) deflection after PR interval & >1/3 size of QRS If ST elevations & Qs at same time, STEMI evolving from injury to necrosis
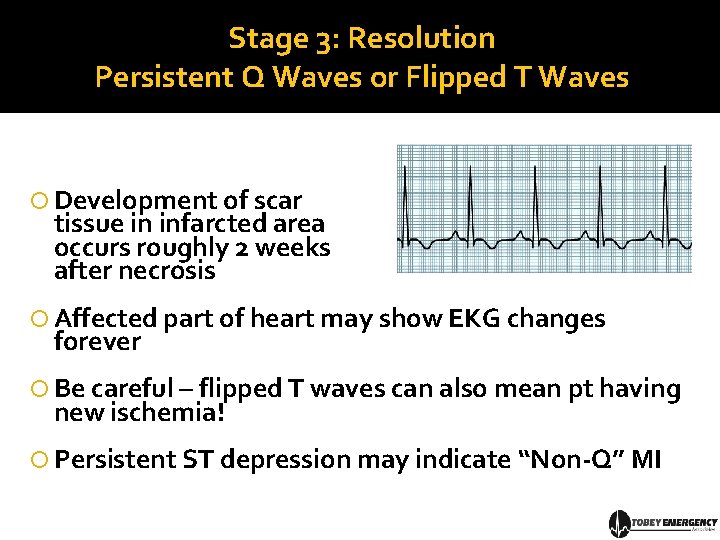
Stage 3: Resolution Persistent Q Waves or Flipped T Waves Development of scar tissue in infarcted area occurs roughly 2 weeks after necrosis Affected part of heart may show EKG changes forever Be careful – flipped T waves can also mean pt having new ischemia! Persistent ST depression may indicate “Non-Q” MI
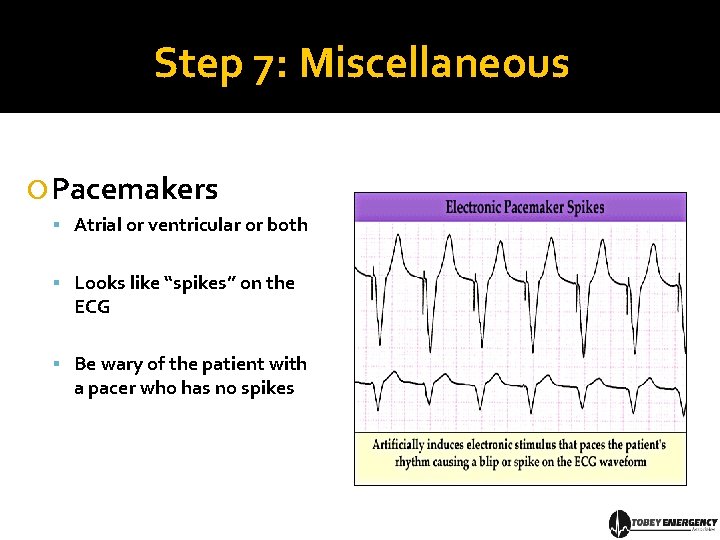
Step 7: Miscellaneous Pacemakers Atrial or ventricular or both Looks like “spikes” on the ECG Be wary of the patient with a pacer who has no spikes
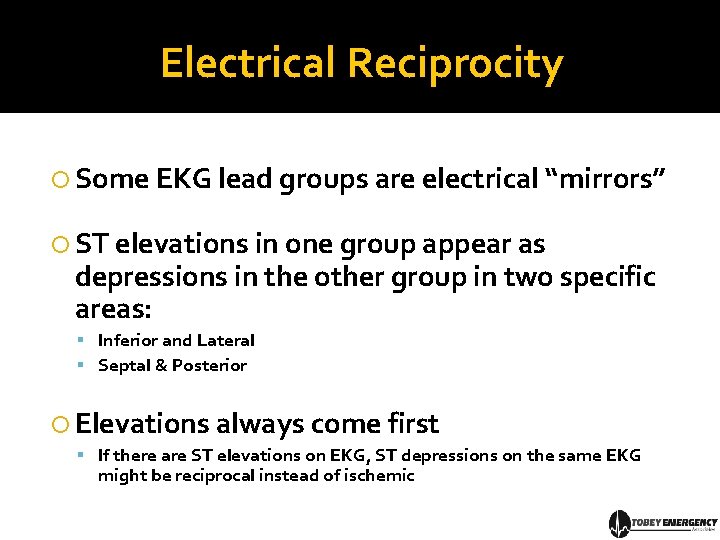
Electrical Reciprocity Some EKG lead groups are electrical “mirrors” ST elevations in one group appear as depressions in the other group in two specific areas: Inferior and Lateral Septal & Posterior Elevations always come first If there are ST elevations on EKG, ST depressions on the same EKG might be reciprocal instead of ischemic
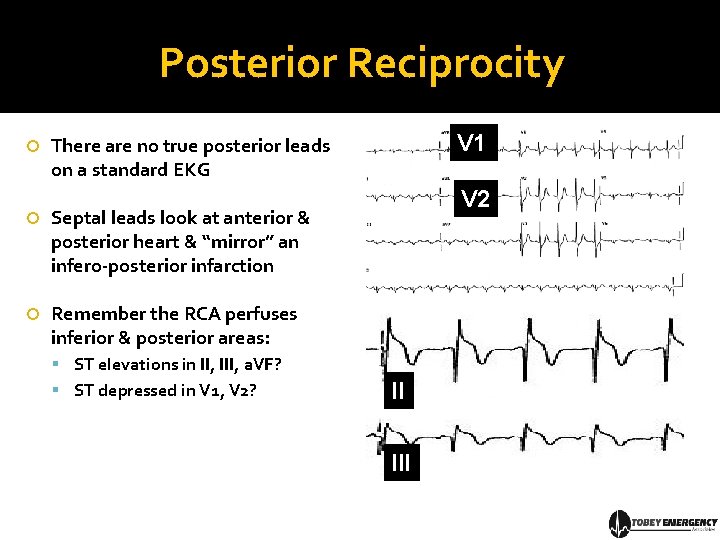
Posterior Reciprocity V 1 There are no true posterior leads on a standard EKG Septal leads look at anterior & posterior heart & “mirror” an infero-posterior infarction Remember the RCA perfuses inferior & posterior areas: V 2 ST elevations in II, III, a. VF? ST depressed in V 1, V 2? II III
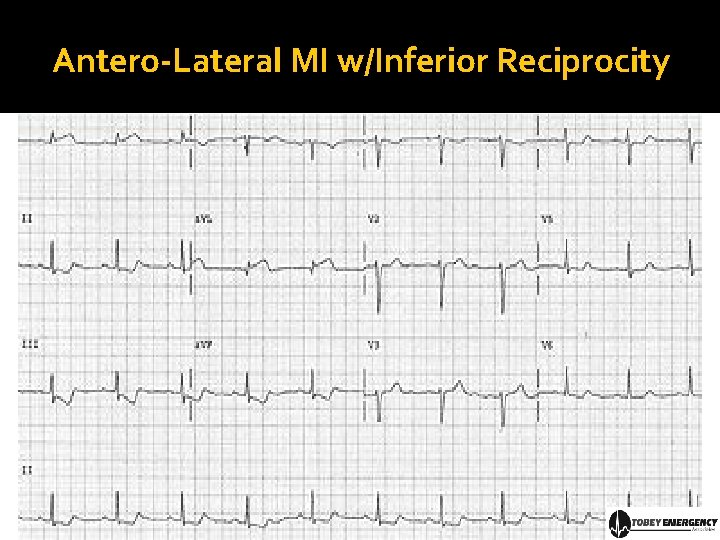
Antero-Lateral MI w/Inferior Reciprocity
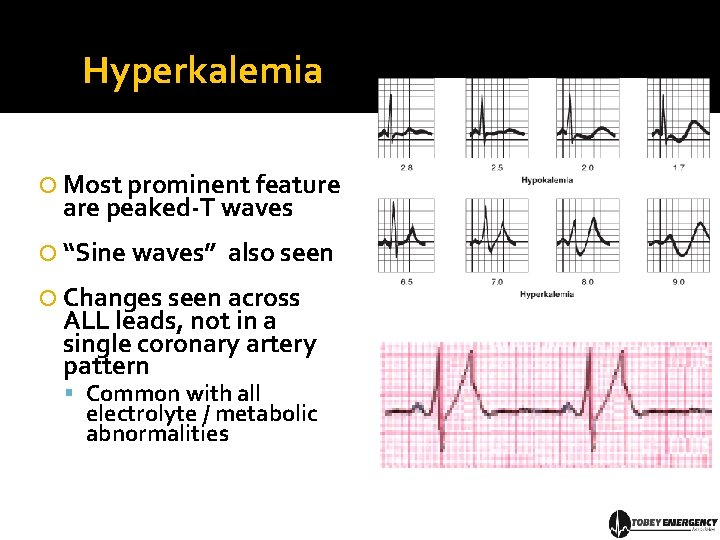
Hyperkalemia Most prominent feature are peaked-T waves “Sine waves” also seen Changes seen across ALL leads, not in a single coronary artery pattern Common with all electrolyte / metabolic abnormalities
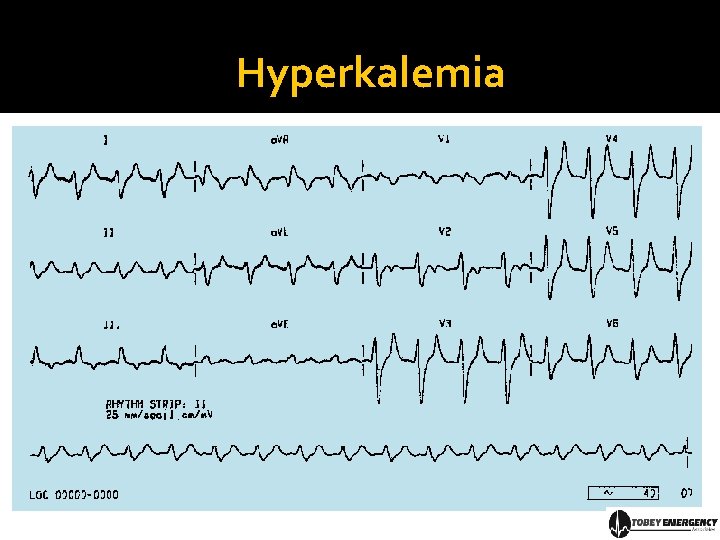
Hyperkalemia
Part IV: Rhythm Analysis Anatomy plus electricity equals rhythm
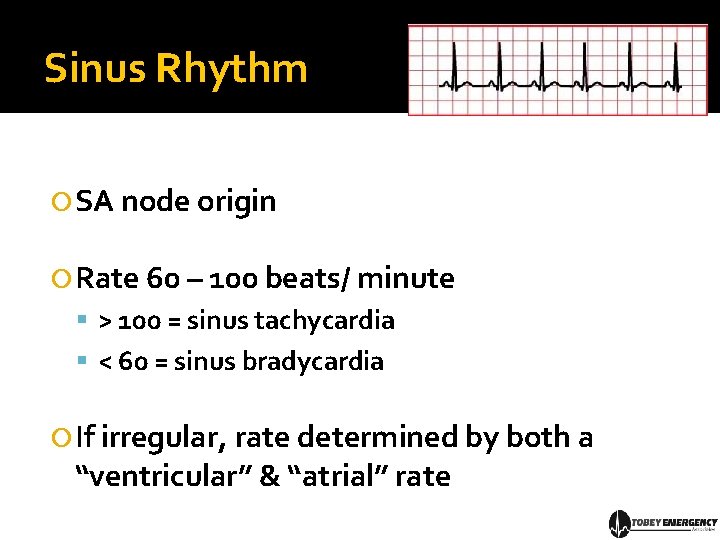
Sinus Rhythm SA node origin Rate 60 – 100 beats/ minute > 100 = sinus tachycardia < 60 = sinus bradycardia If irregular, rate determined by both a “ventricular” & “atrial” rate
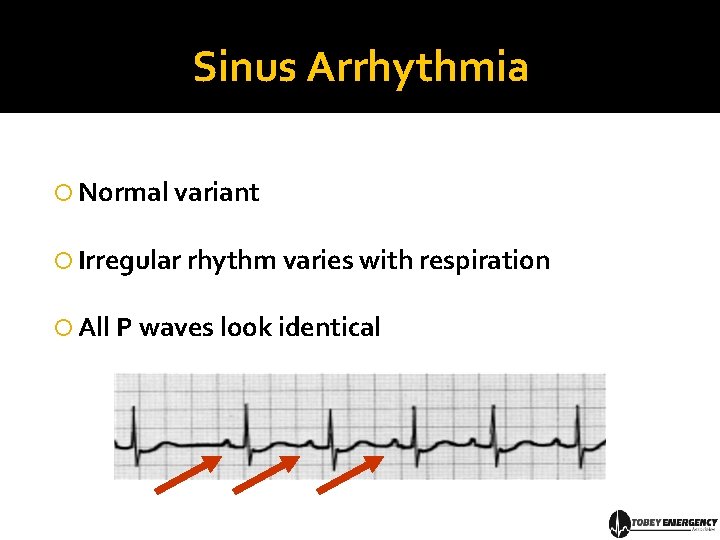
Sinus Arrhythmia Normal variant Irregular rhythm varies with respiration All P waves look identical
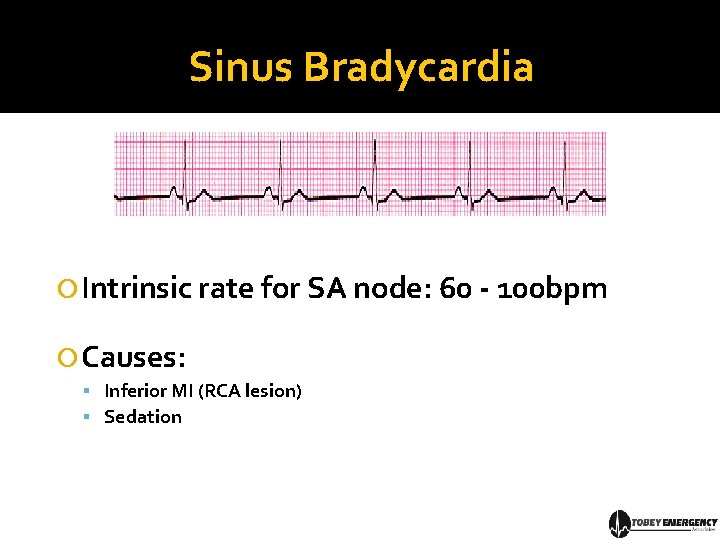
Sinus Bradycardia Intrinsic rate for SA node: 60 - 100 bpm Causes: Inferior MI (RCA lesion) Sedation
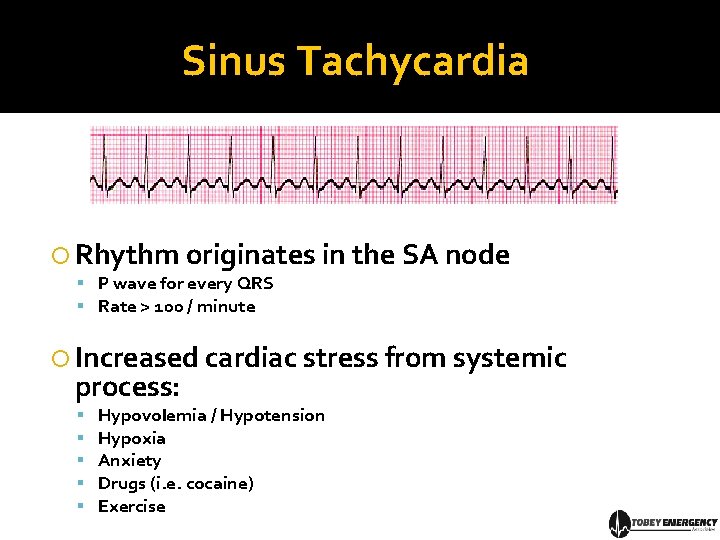
Sinus Tachycardia Rhythm originates in the SA node P wave for every QRS Rate > 100 / minute Increased cardiac stress from systemic process: Hypovolemia / Hypotension Hypoxia Anxiety Drugs (i. e. cocaine) Exercise
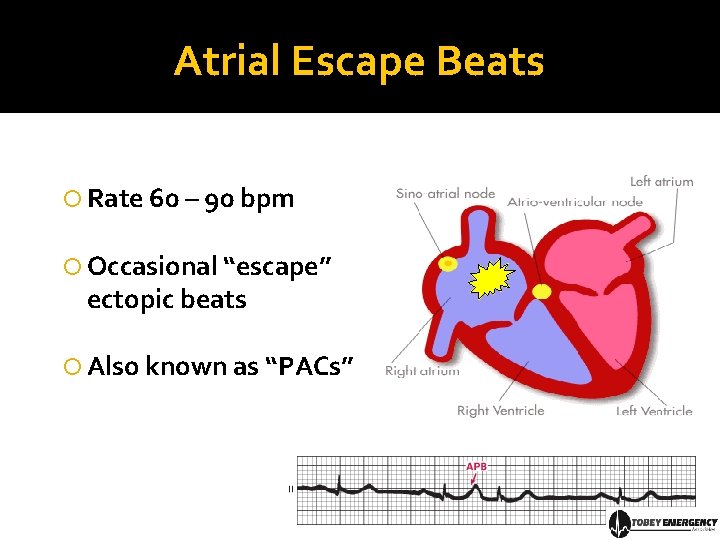
Atrial Escape Beats Rate 60 – 90 bpm Occasional “escape” ectopic beats Also known as “PACs”
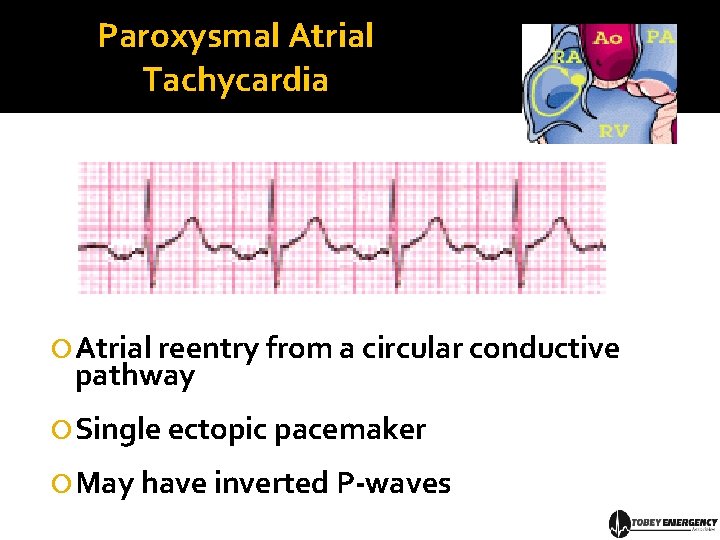
Paroxysmal Atrial Tachycardia Atrial reentry from a circular conductive pathway Single ectopic pacemaker May have inverted P-waves
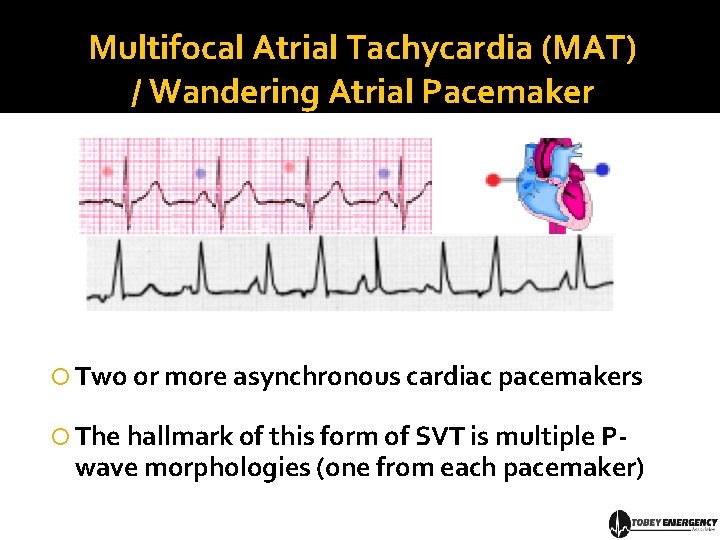
Multifocal Atrial Tachycardia (MAT) / Wandering Atrial Pacemaker Two or more asynchronous cardiac pacemakers The hallmark of this form of SVT is multiple P- wave morphologies (one from each pacemaker)
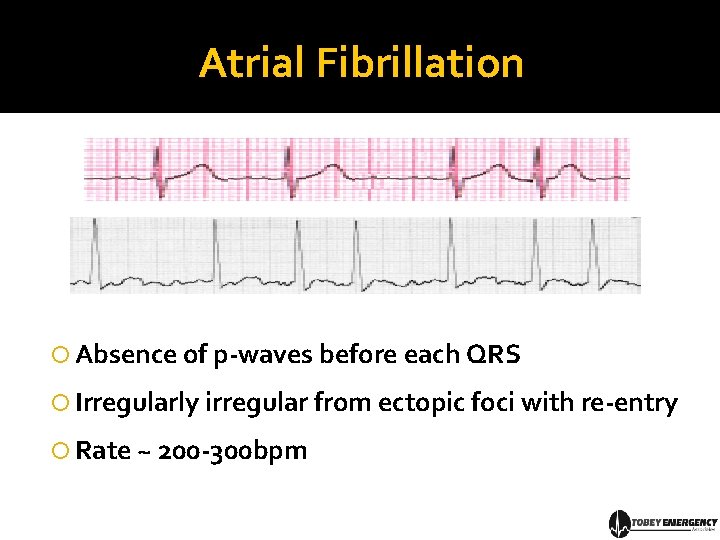
Atrial Fibrillation Absence of p-waves before each QRS Irregularly irregular from ectopic foci with re-entry Rate ~ 200 -300 bpm
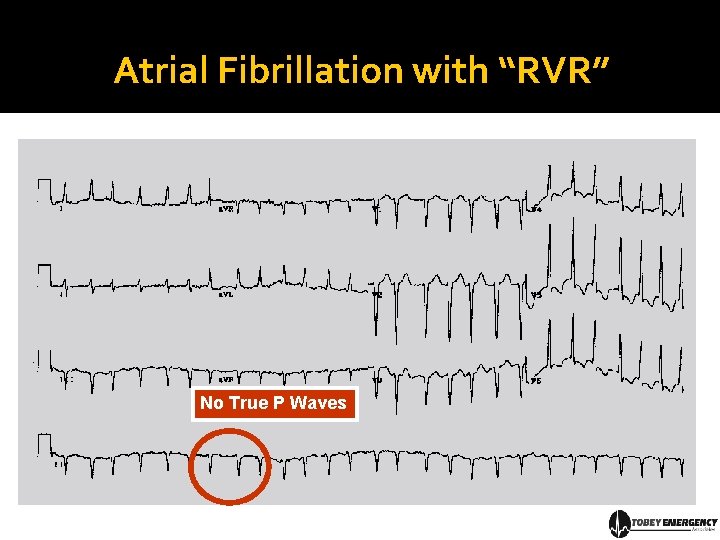
Atrial Fibrillation with “RVR” No True P Waves
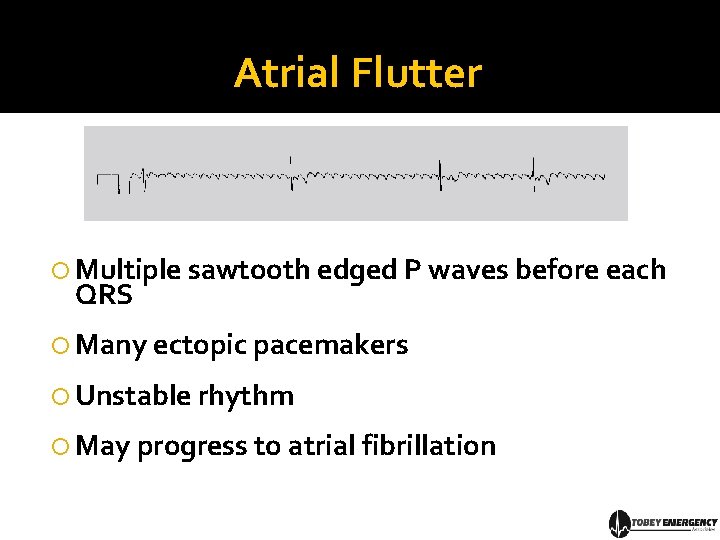
Atrial Flutter Multiple sawtooth edged P waves before each QRS Many ectopic pacemakers Unstable rhythm May progress to atrial fibrillation
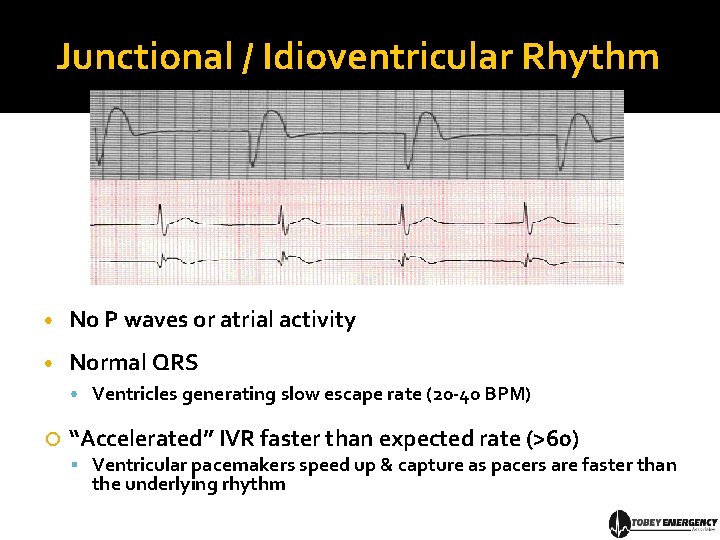
Junctional / Idioventricular Rhythm • No P waves or atrial activity • Normal QRS • Ventricles generating slow escape rate (20 -40 BPM) “Accelerated” IVR faster than expected rate (>60) Ventricular pacemakers speed up & capture as pacers are faster than the underlying rhythm
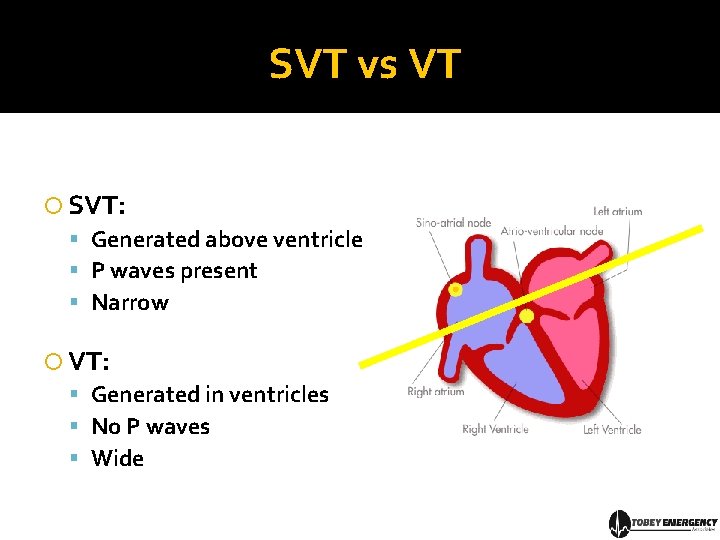
SVT vs VT SVT: Generated above ventricle P waves present Narrow VT: Generated in ventricles No P waves Wide
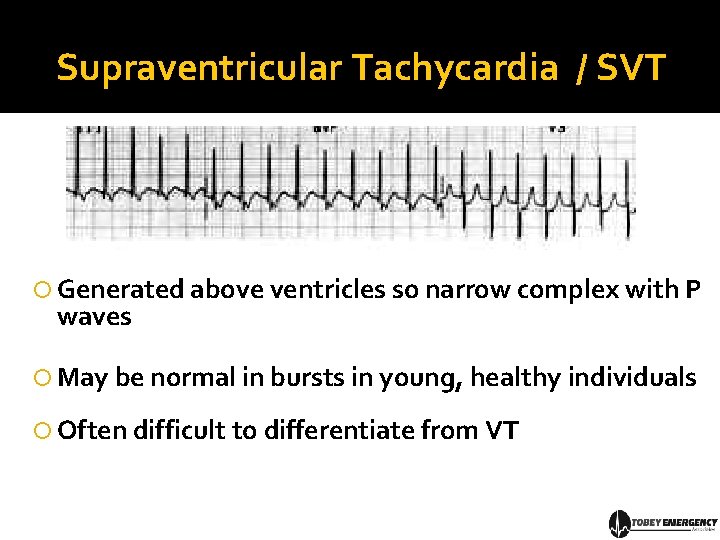
Supraventricular Tachycardia / SVT Generated above ventricles so narrow complex with P waves May be normal in bursts in young, healthy individuals Often difficult to differentiate from VT
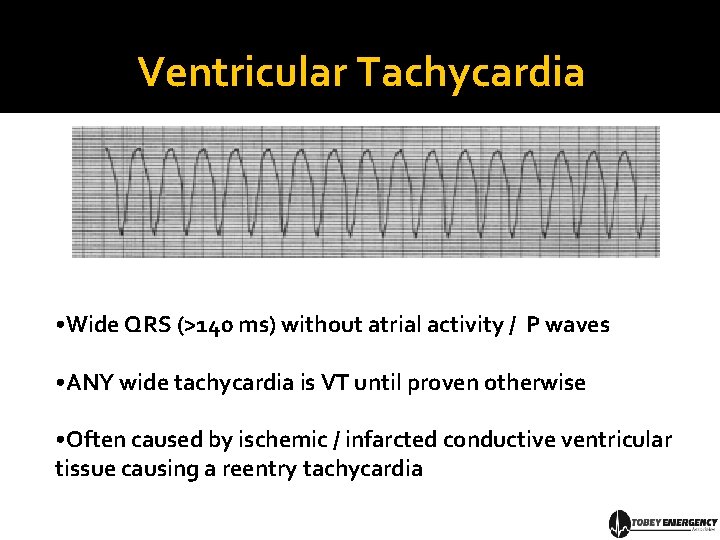
Ventricular Tachycardia • Wide QRS (>140 ms) without atrial activity / P waves • ANY wide tachycardia is VT until proven otherwise • Often caused by ischemic / infarcted conductive ventricular tissue causing a reentry tachycardia
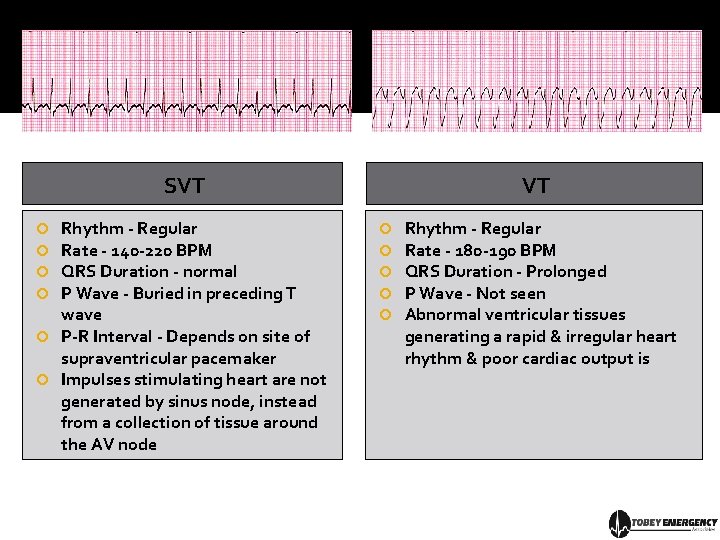
SVT Rhythm - Regular Rate - 140 -220 BPM QRS Duration - normal P Wave - Buried in preceding T wave P-R Interval - Depends on site of supraventricular pacemaker Impulses stimulating heart are not generated by sinus node, instead from a collection of tissue around the AV node VT Rhythm - Regular Rate - 180 -190 BPM QRS Duration - Prolonged P Wave - Not seen Abnormal ventricular tissues generating a rapid & irregular heart rhythm & poor cardiac output is
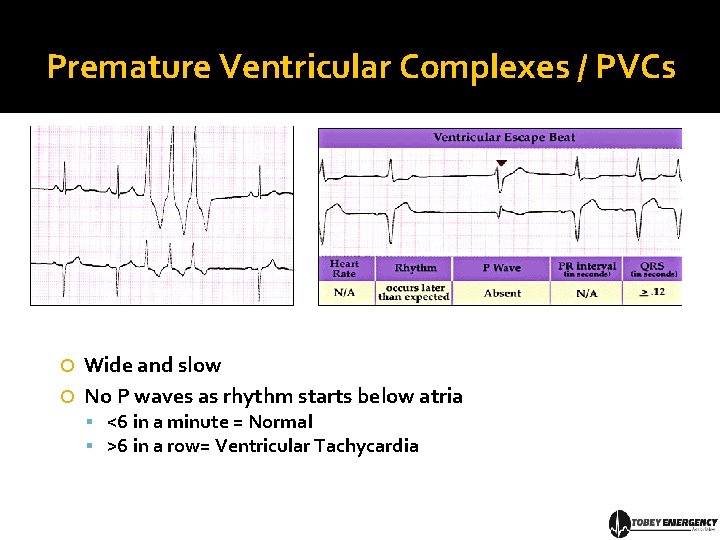
Premature Ventricular Complexes / PVCs Wide and slow No P waves as rhythm starts below atria <6 in a minute = Normal >6 in a row= Ventricular Tachycardia
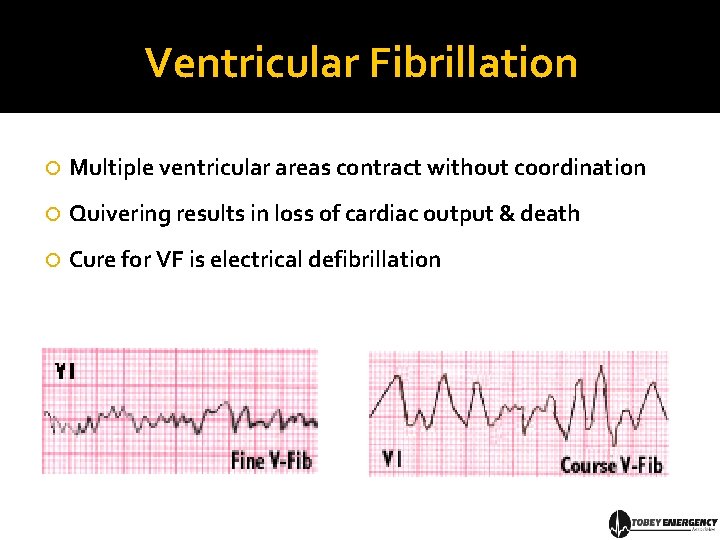
Ventricular Fibrillation Multiple ventricular areas contract without coordination Quivering results in loss of cardiac output & death Cure for VF is electrical defibrillation
References Alan Lindsey ECG Learning Center in Cyberspace Dubin’s Guide to ECGs London Ambulance Sercice Unoffical ECG Guide Brady’s, Mosby’s, Caroline’s Prehospital Provider Textbooks www. The. MDSite. com Wikipedia, Google The ECG Guide (Iphone App)
Summary prehospitalmd@gmail. com / www. TEAEMS. com “Almost” everything you need to know: Part I: Cardiac Anatomy Review Part II: The Cardiac Cycle Part III: From One Beat to Many Part IV: Basic Rhythm Analysis Is this everything you truly need to know? Look at every strip, ECG & rhythm you can…you need to know “normal” before you can know “abnormal”
- Slides: 94