Allergic Diseases Nima Rezaei MD Ph D Dean







- Slides: 75
Allergic Diseases Nima Rezaei, MD, Ph. D Dean of International Affairs, School of Medicine Director of Global Academic Program Deputy President of Research Center for Immunodeficien Part Five Pediatrics Center of Excellence, Children’s Medical Cente Tehran University of Medical Sciences Tehran, Iran

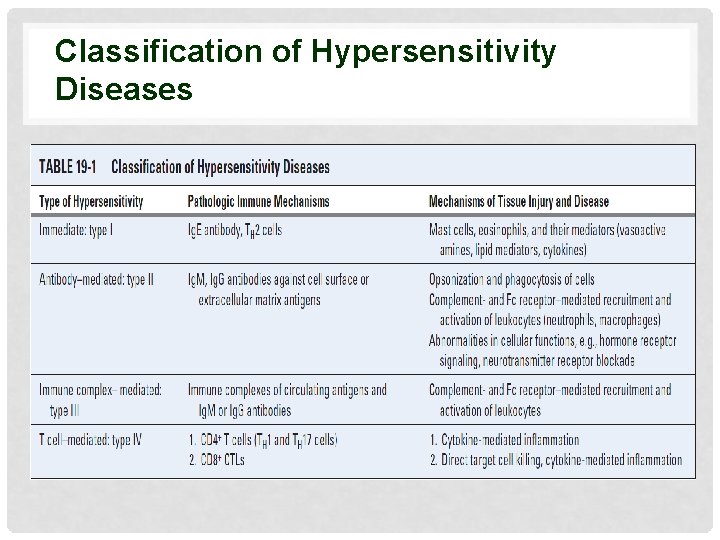
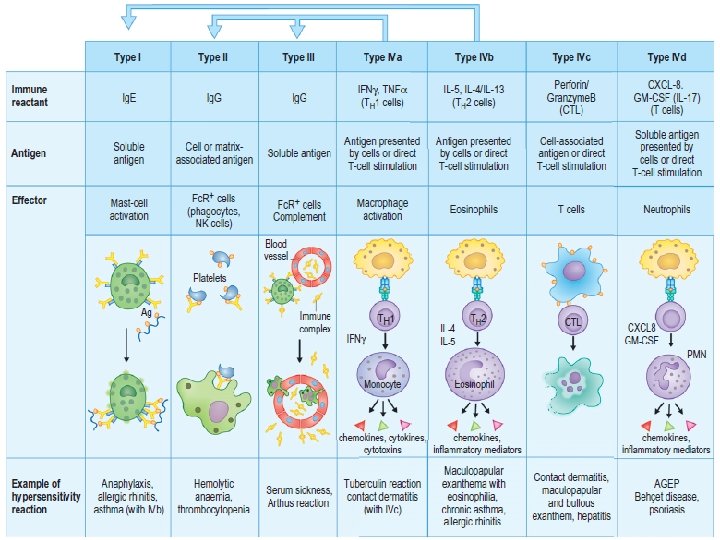
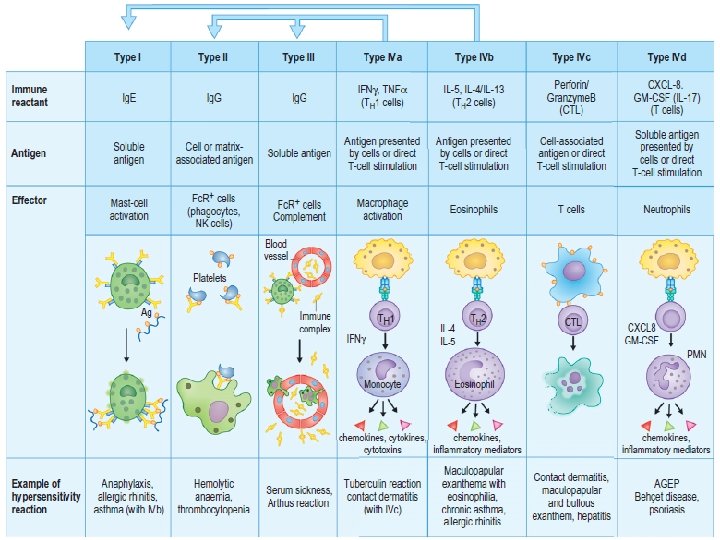
Mechanism of Immunologic Injury (Hypersensitivity) • Type I (Immediate reactions) • Mediated by Ig. E bound to the surface of basophils and mast cells • Type II (Cytotoxic reactions) • Lysis of the Ab-coated cell • Type III (Immune complex reactions) • Results from immune complex formation • Type IV (Cell-mediated reactions) • Cell-mediated or delayed hypersensitivity
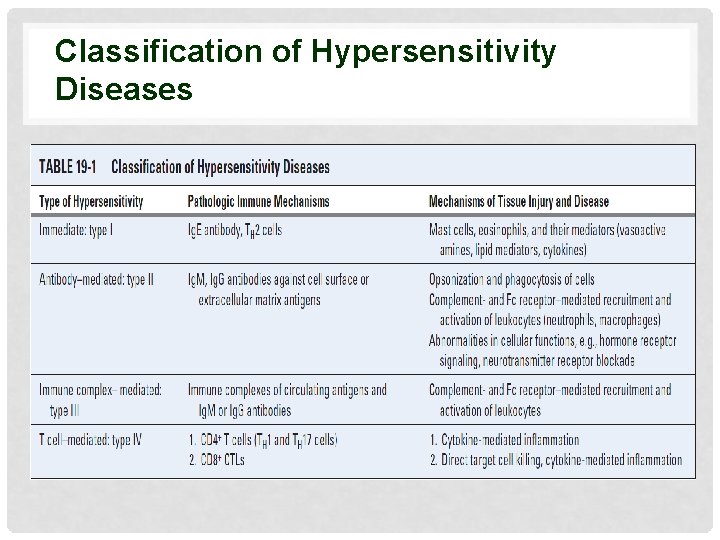
Classification of Hypersensitivity Diseases
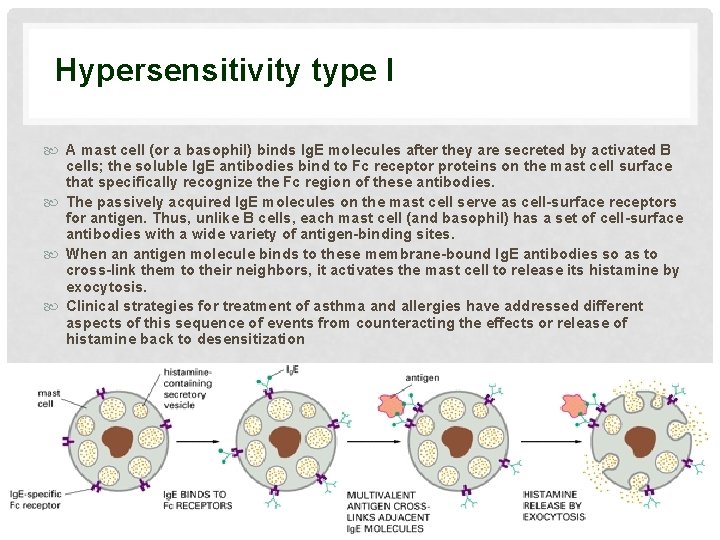
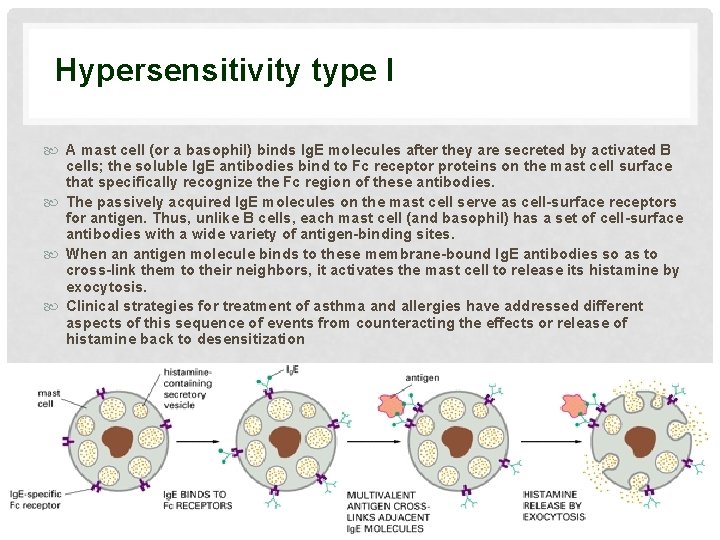
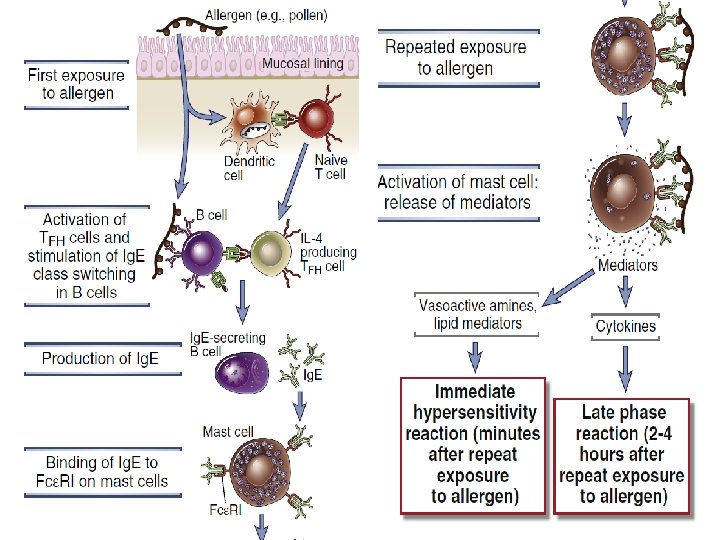
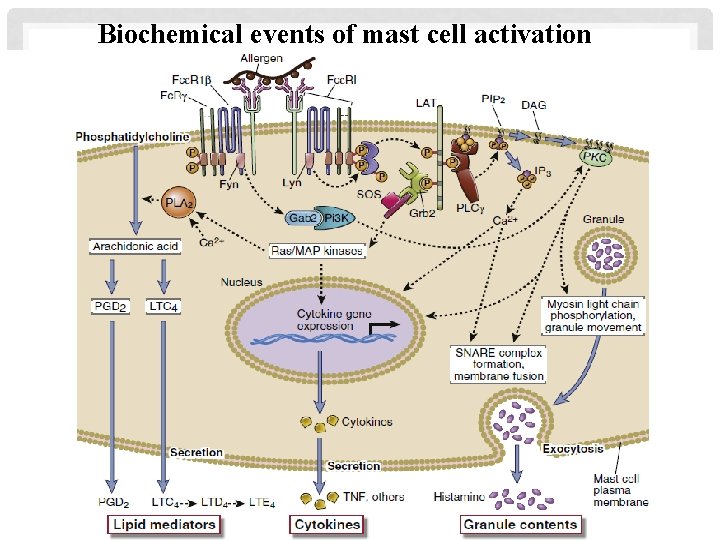
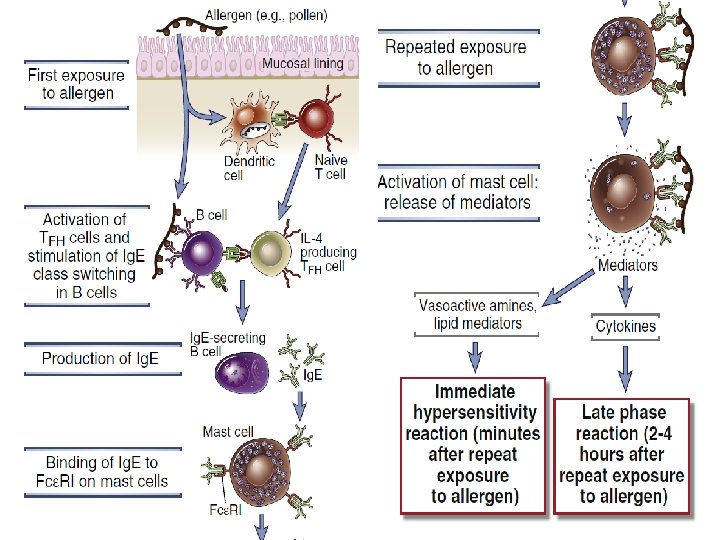
Hypersensitivity type I A mast cell (or a basophil) binds Ig. E molecules after they are secreted by activated B cells; the soluble Ig. E antibodies bind to Fc receptor proteins on the mast cell surface that specifically recognize the Fc region of these antibodies. The passively acquired Ig. E molecules on the mast cell serve as cell-surface receptors for antigen. Thus, unlike B cells, each mast cell (and basophil) has a set of cell-surface antibodies with a wide variety of antigen-binding sites. When an antigen molecule binds to these membrane-bound Ig. E antibodies so as to cross-link them to their neighbors, it activates the mast cell to release its histamine by exocytosis. Clinical strategies for treatment of asthma and allergies have addressed different aspects of this sequence of events from counteracting the effects or release of histamine back to desensitization
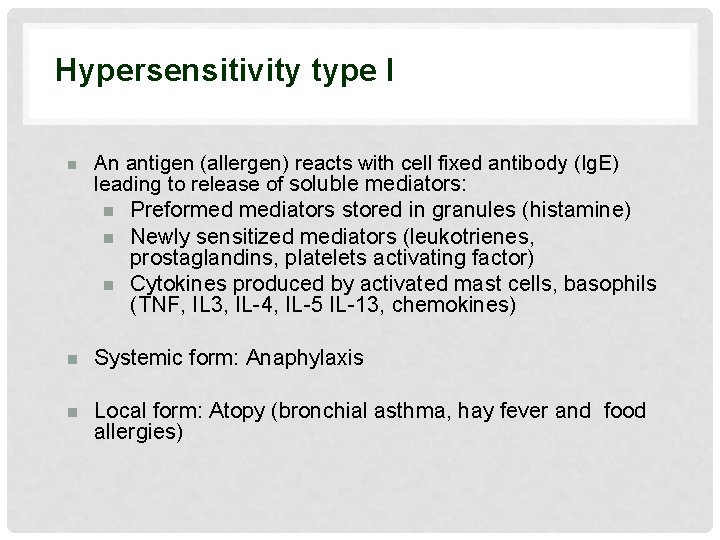
Hypersensitivity type I n An antigen (allergen) reacts with cell fixed antibody (Ig. E) leading to release of soluble mediators: n Preformed mediators stored in granules (histamine) n Newly sensitized mediators (leukotrienes, prostaglandins, platelets activating factor) n Cytokines produced by activated mast cells, basophils (TNF, IL 3, IL-4, IL-5 IL-13, chemokines) n Systemic form: Anaphylaxis n Local form: Atopy (bronchial asthma, hay fever and food allergies)
ALLERGEN Outdoor Air-born allergens Allergens Food allergens Other allergens Indoor
TREES Birch oak cedar olive mapple elm
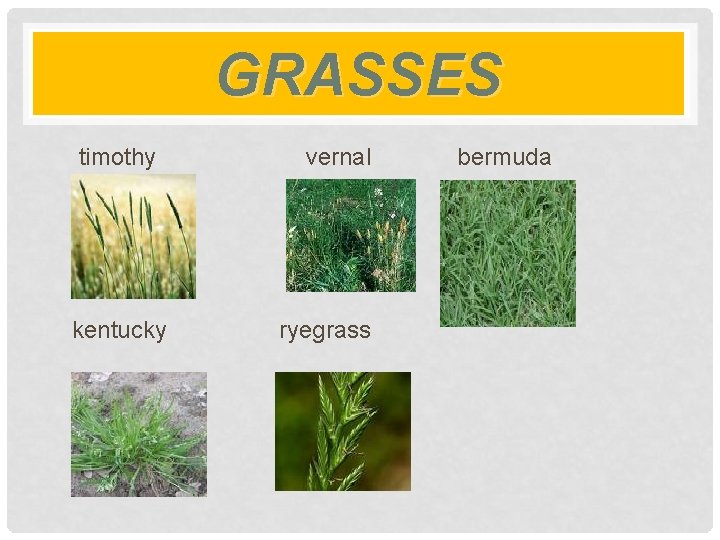
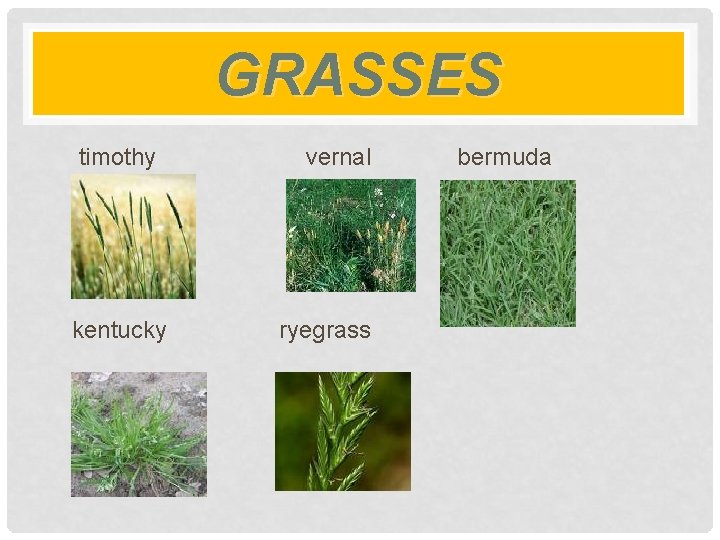
GRASSES timothy kentucky vernal ryegrass bermuda

WEEDS ragweed lambs quarter pigweed sleep sorrel russian thistle mugwort
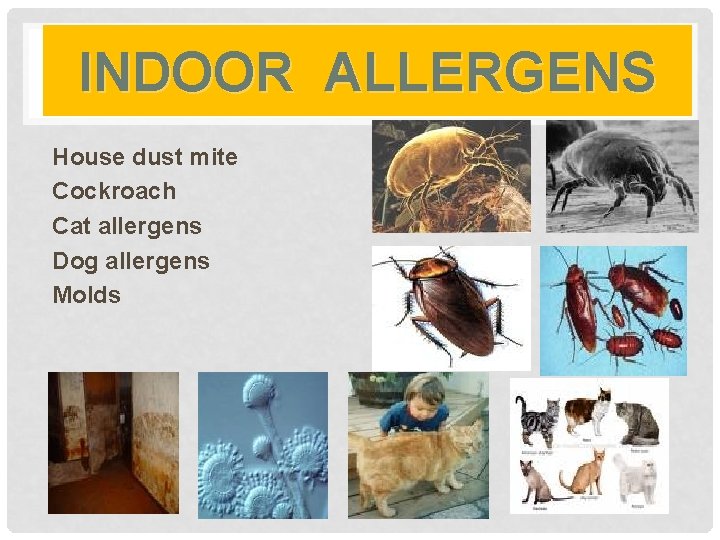
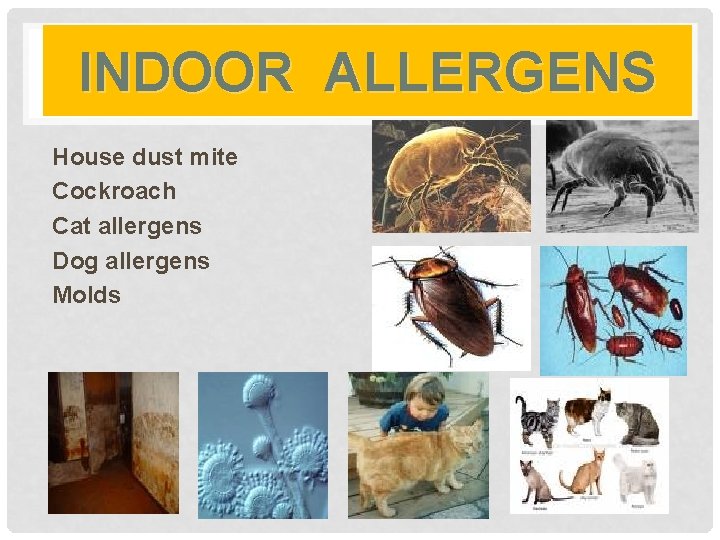
INDOOR ALLERGENS House dust mite Cockroach Cat allergens Dog allergens Molds
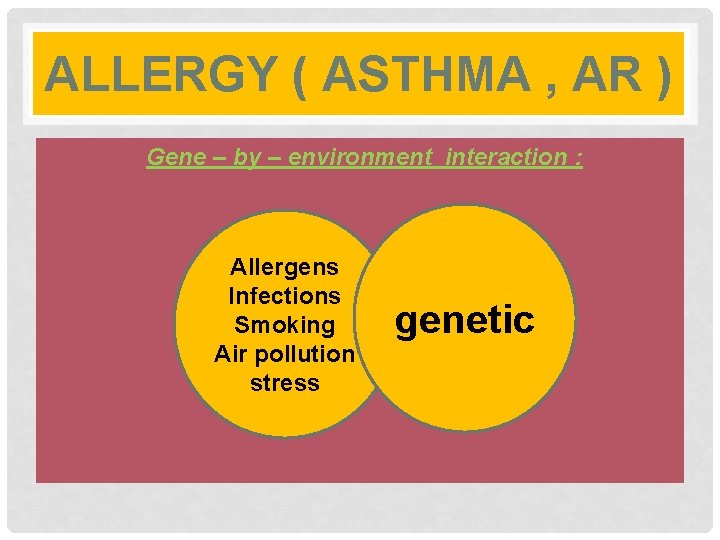
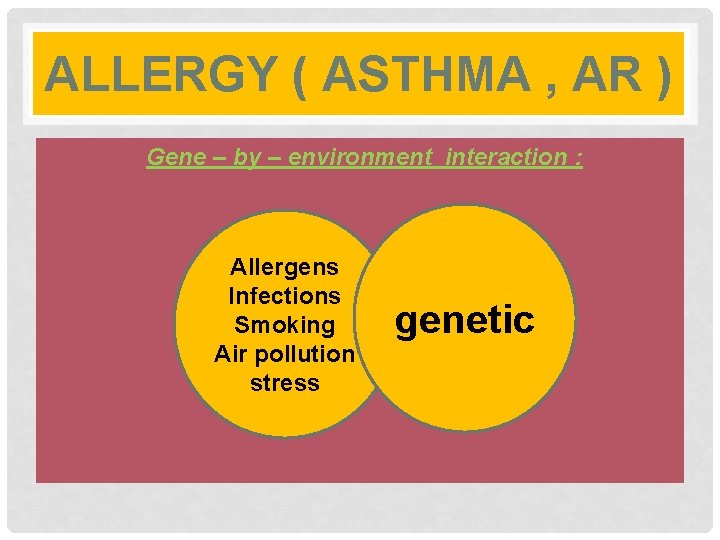
ALLERGY ( ASTHMA , AR ) Gene – by – environment interaction : Allergens Infections Smoking Air pollution stress genetic
Allergies
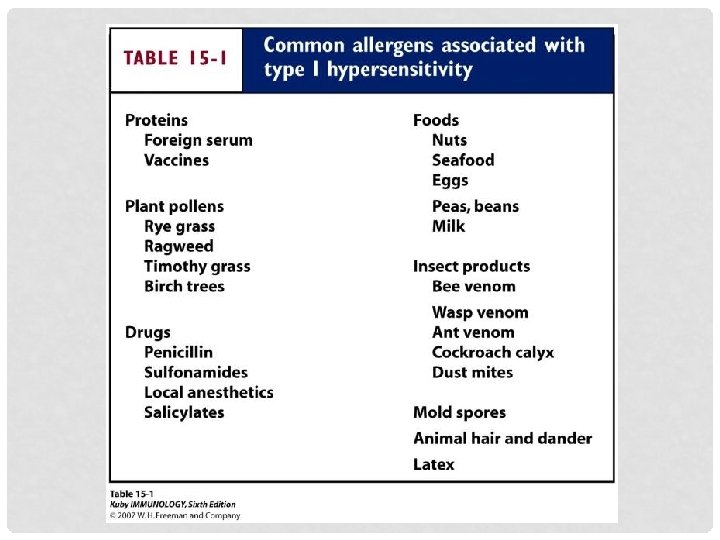
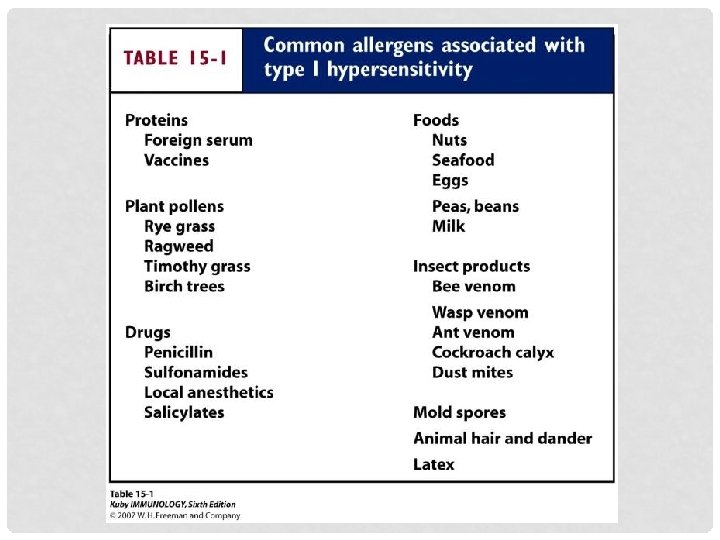
Allergy § Type of hypersensitivity reactions of the immune system. Allergy may involve more the one type of reaction. § Seen in ~30 -35% of the population § An allergy is a q q q q immune reaction to something that does not affect most other people. Substances that often cause reactions are: Pollen Dust mites Mold spores Pet dander Food Insect stings Medicines
ALLERGIC DISEASES § Either Ig E mediated (Type I hypersensitivity) or non-Ig. E mediated § Both mast cells and basophils are involved in immunopathogenesis of Ig. E mediated diseases. Mast cells and basophils have a high affinity Ig. E cell membrane receptors for Ig. E. § Immediate hypersensitivity reactions are mediated by Ig. E, but T and B cells play important roles in the development of these antibodies
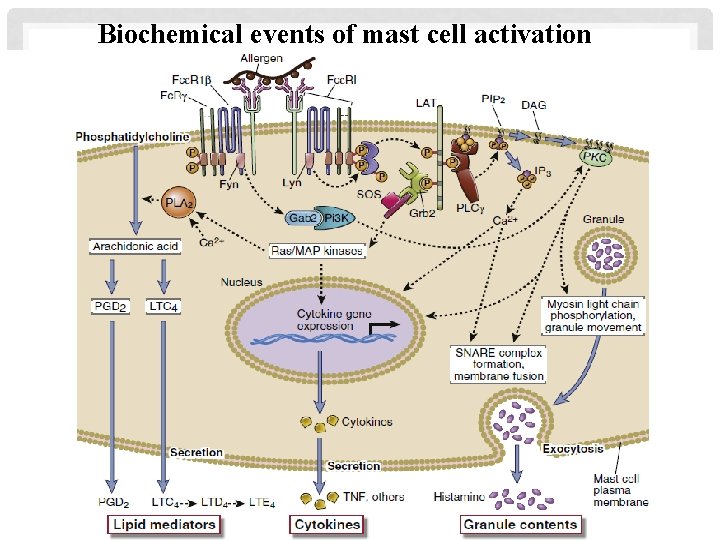
Biochemical events of mast cell activation
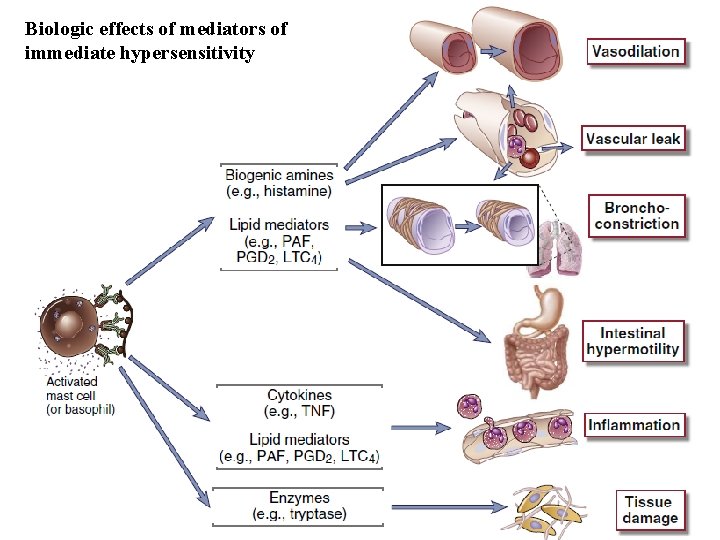
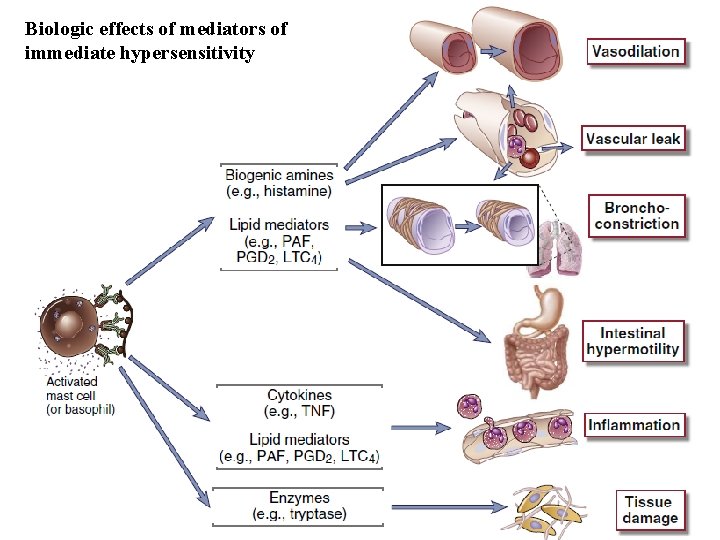
Biologic effects of mediators of immediate hypersensitivity
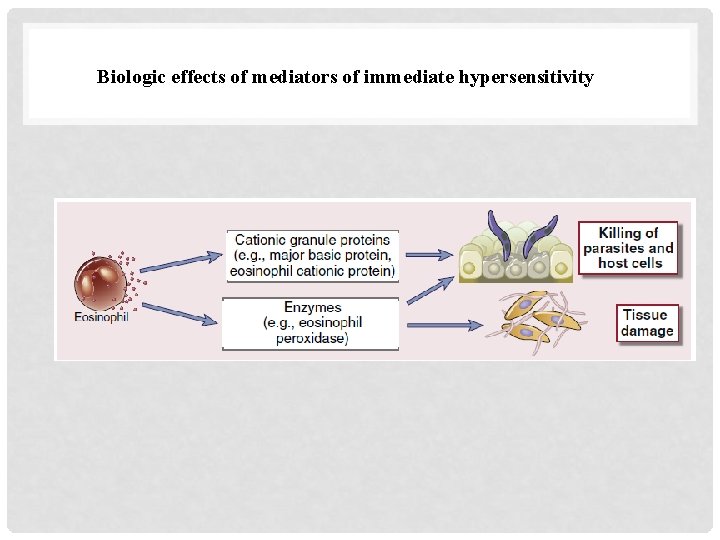
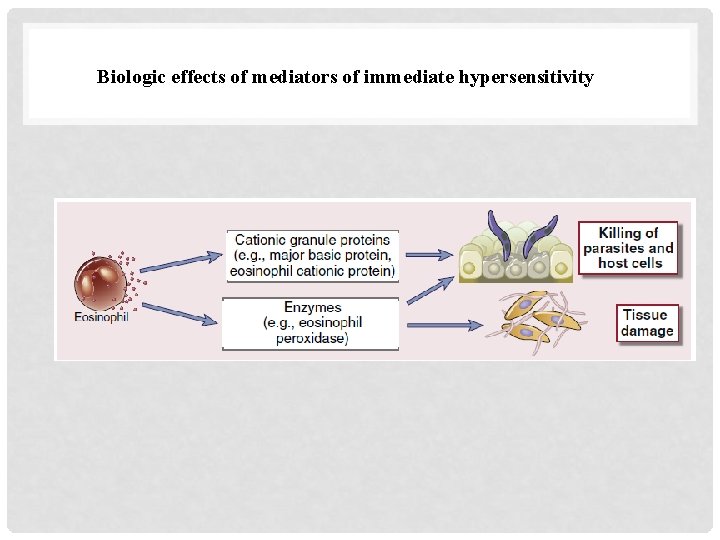
Biologic effects of mediators of immediate hypersensitivity
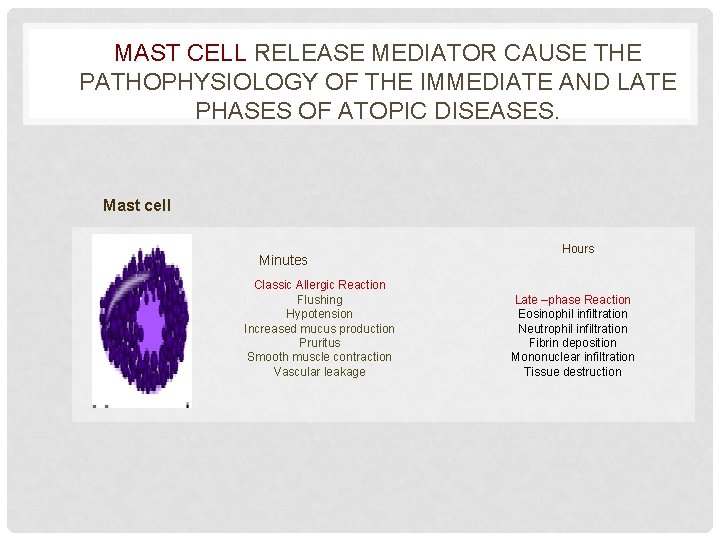
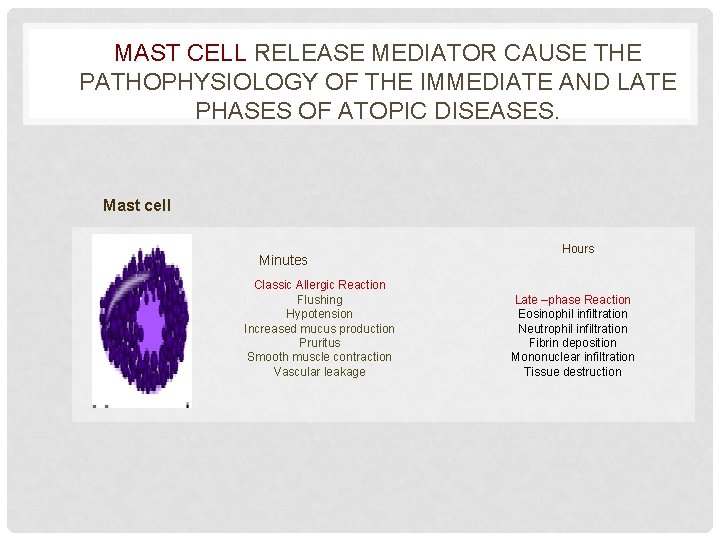
MAST CELL RELEASE MEDIATOR CAUSE THE PATHOPHYSIOLOGY OF THE IMMEDIATE AND LATE PHASES OF ATOPIC DISEASES. Mast cell Minutes Classic Allergic Reaction Flushing Hypotension Increased mucus production Pruritus Smooth muscle contraction Vascular leakage Hours Late –phase Reaction Eosinophil infiltration Neutrophil infiltration Fibrin deposition Mononuclear infiltration Tissue destruction
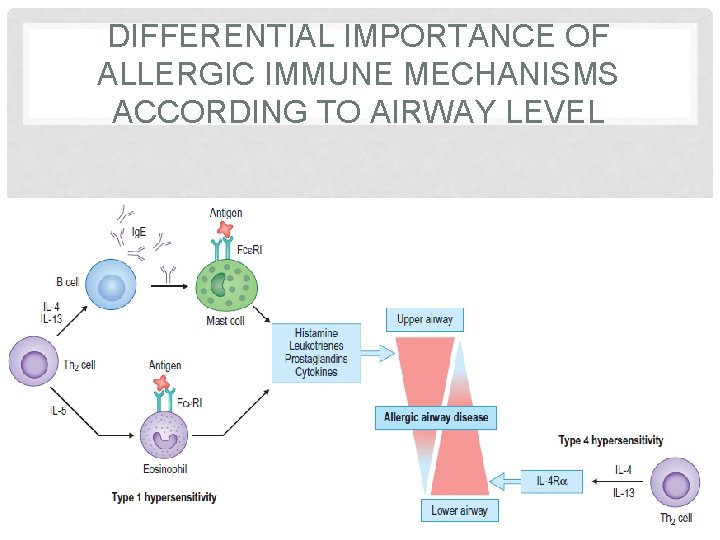
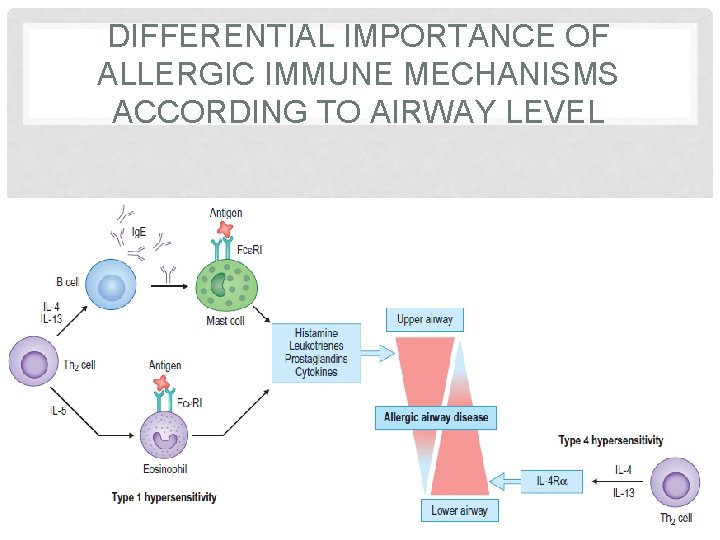
DIFFERENTIAL IMPORTANCE OF ALLERGIC IMMUNE MECHANISMS ACCORDING TO AIRWAY LEVEL
ALLERGIC DISEASES Atopy is the genetic predisposition to make Ig. E antibodies in response to allergen exposure. Allergic rhinitis, allergic asthma, atopic dermatitis are the most common manifestation of atopy. Perennial & seasonal allergic rhinitis Allergic (extrinsic) asthma Atopic and contact dermatitis Urticaria Food intolerance
Allergy Risk factor § Host factors; heredity, gender, race, and age. § Environmental factor; infectious diseases during early childhood, environmental pollution, allergen levels and dietary changes.
GENETICS Family history of allergic disease is a strong risk factor for developing asthma Danger of developing asthma particularly if one or both parents are atopic Children with atopic dermatitis at risk of asthma -– “the allergic march” No single "allergy or asthma chromosome". Several markers demonstrated in small selected populations much further work is required The genetics of allergy and asthma are polygenic influence many factors such as Ig. E secretion, cytokines and inflammatory cell profiles
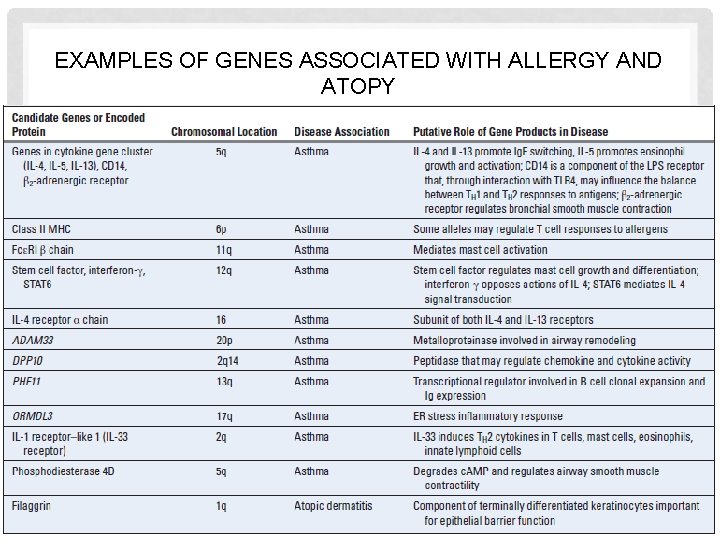
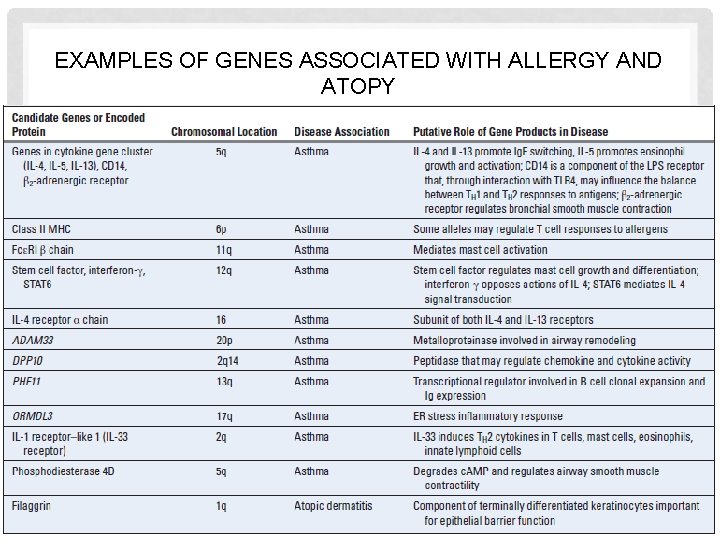
EXAMPLES OF GENES ASSOCIATED WITH ALLERGY AND ATOPY
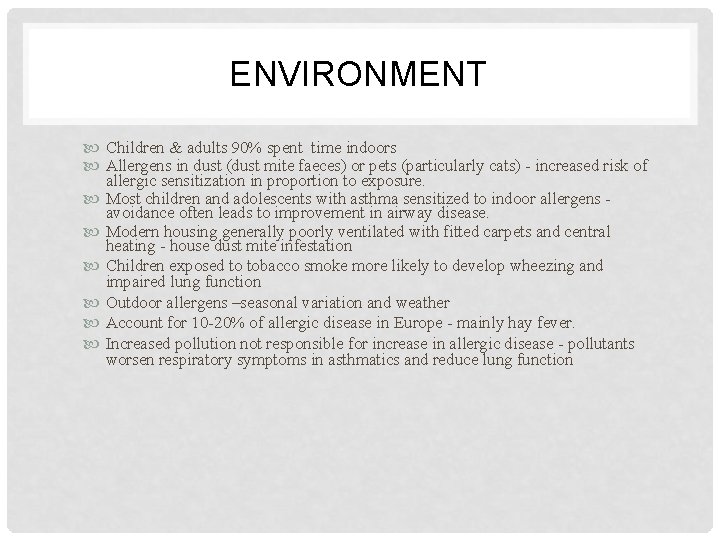
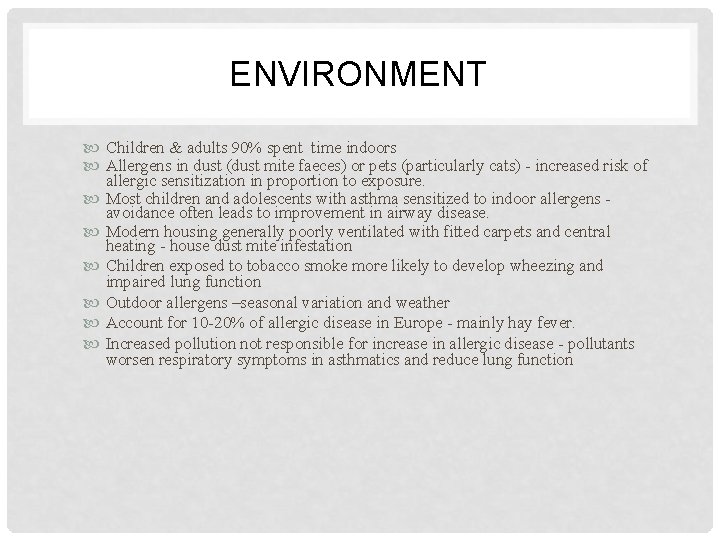
ENVIRONMENT Children & adults 90% spent time indoors Allergens in dust (dust mite faeces) or pets (particularly cats) - increased risk of allergic sensitization in proportion to exposure. Most children and adolescents with asthma sensitized to indoor allergens avoidance often leads to improvement in airway disease. Modern housing generally poorly ventilated with fitted carpets and central heating - house dust mite infestation Children exposed to tobacco smoke more likely to develop wheezing and impaired lung function Outdoor allergens –seasonal variation and weather Account for 10 -20% of allergic disease in Europe - mainly hay fever. Increased pollution not responsible for increase in allergic disease - pollutants worsen respiratory symptoms in asthmatics and reduce lung function
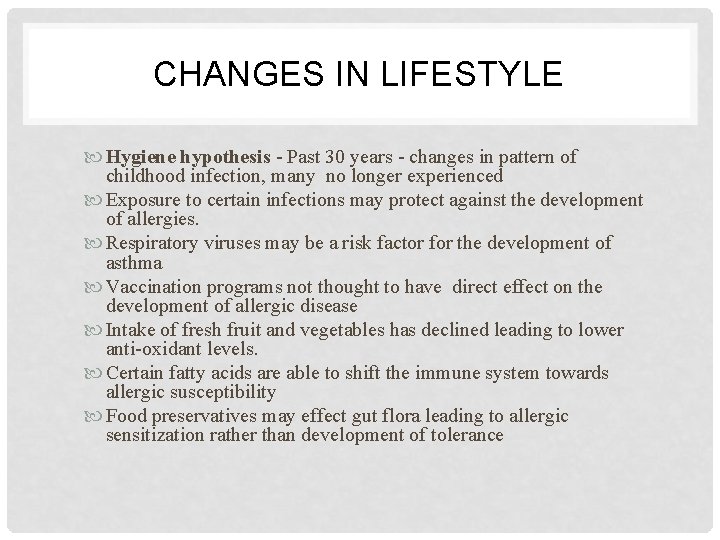
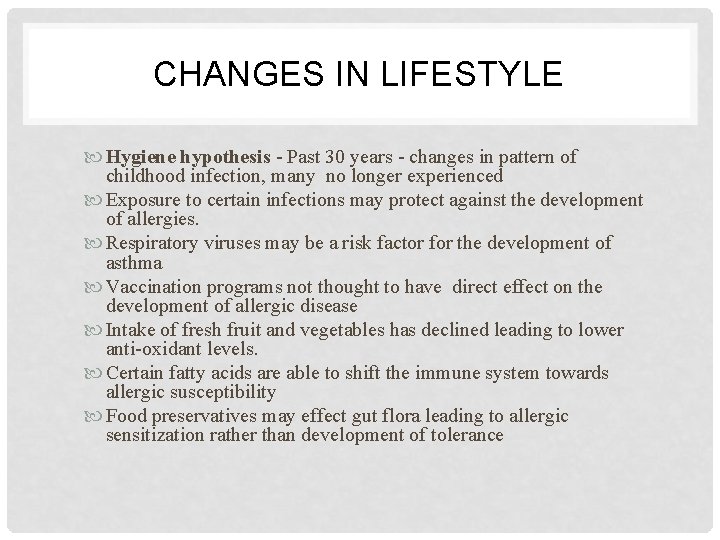
CHANGES IN LIFESTYLE Hygiene hypothesis - Past 30 years - changes in pattern of childhood infection, many no longer experienced Exposure to certain infections may protect against the development of allergies. Respiratory viruses may be a risk factor for the development of asthma Vaccination programs not thought to have direct effect on the development of allergic disease Intake of fresh fruit and vegetables has declined leading to lower anti-oxidant levels. Certain fatty acids are able to shift the immune system towards allergic susceptibility Food preservatives may effect gut flora leading to allergic sensitization rather than development of tolerance
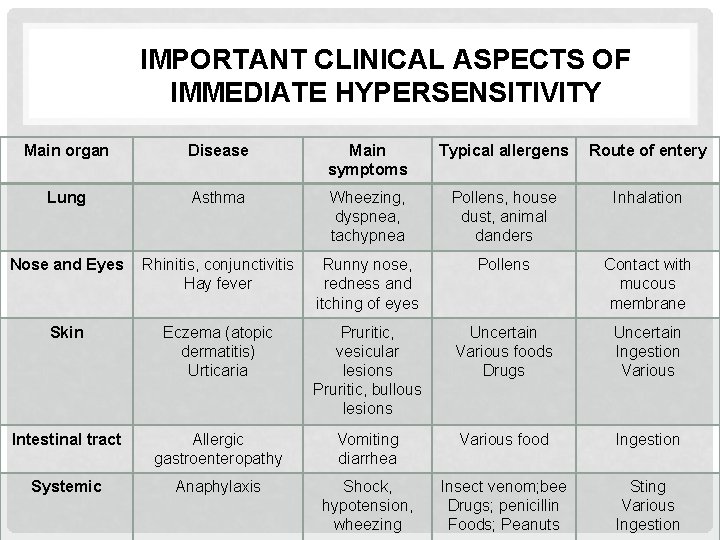
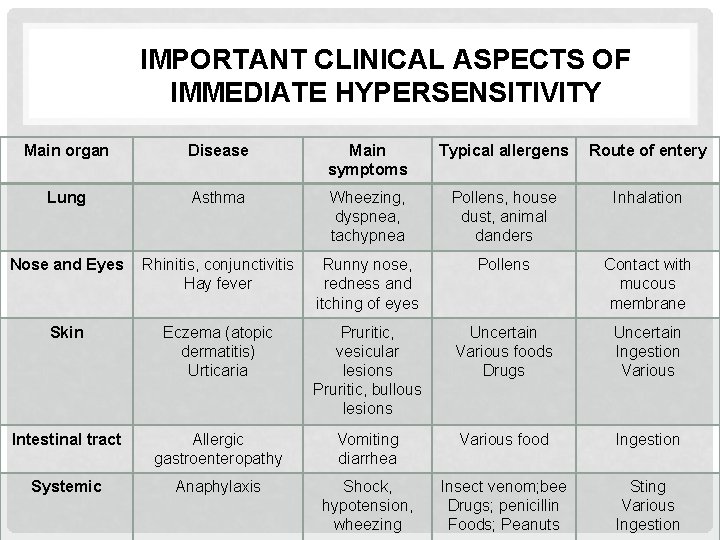
IMPORTANT CLINICAL ASPECTS OF IMMEDIATE HYPERSENSITIVITY Main organ Disease Main symptoms Typical allergens Route of entery Lung Asthma Wheezing, dyspnea, tachypnea Pollens, house dust, animal danders Inhalation Nose and Eyes Rhinitis, conjunctivitis Hay fever Runny nose, redness and itching of eyes Pollens Contact with mucous membrane Skin Eczema (atopic dermatitis) Urticaria Pruritic, vesicular lesions Pruritic, bullous lesions Uncertain Various foods Drugs Uncertain Ingestion Various Intestinal tract Allergic gastroenteropathy Vomiting diarrhea Various food Ingestion Systemic Anaphylaxis Shock, hypotension, wheezing Insect venom; bee Drugs; penicillin Foods; Peanuts Sting Various Ingestion
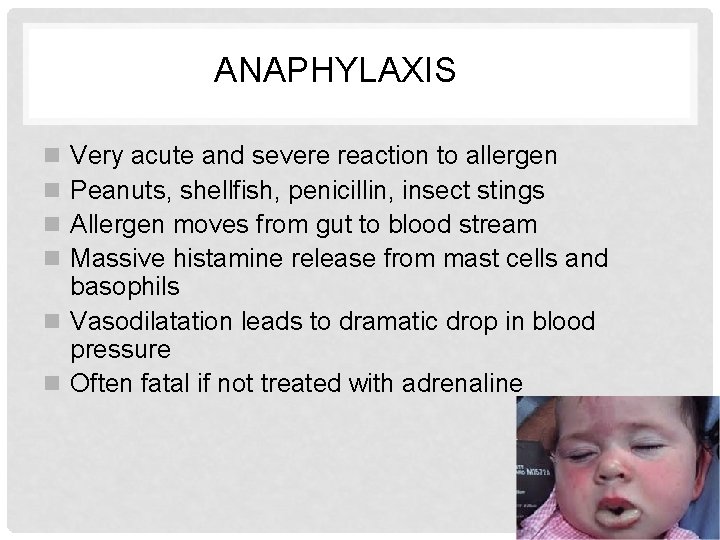
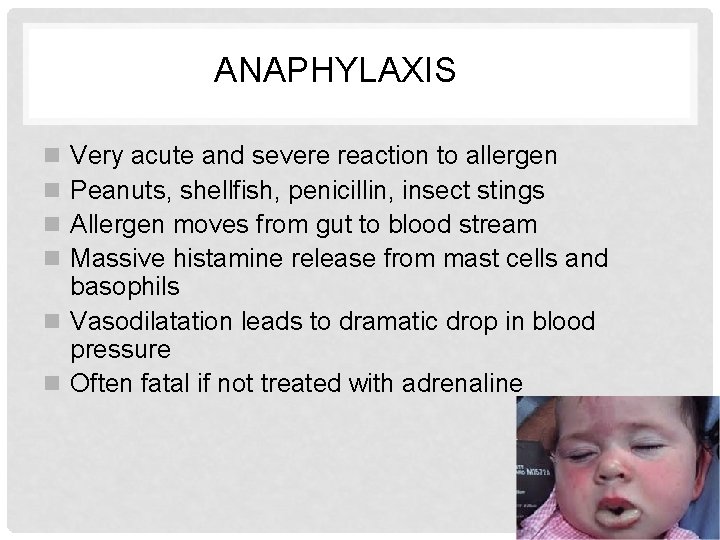
ANAPHYLAXIS Very acute and severe reaction to allergen Peanuts, shellfish, penicillin, insect stings Allergen moves from gut to blood stream Massive histamine release from mast cells and basophils n Vasodilatation leads to dramatic drop in blood pressure n Often fatal if not treated with adrenaline n n
ANAPHYLAXIS • Anaphylaxis is characterized by extreme difficulty with breathing due to airway obstruction from angioedema or bronchoconstriction, circulatory collapse, or both. • It is nearly always accompanied by tachycardia, usually by flushing, urticaria, and panic, and sometimes by vomiting and diarrhea. • Panic attacks do not involve airways obstruction, hypotension, or urticaria but may be accompanied by faintness or tetany of the hands due to rapid overbreathing. • Vasovagal attacks present with fainting, nausea, slow pulse, and pallor without respiratory difficulty, diarrhea, or urticaria.

ALLERGIC RHINITIS n Seasonal (pollen, spores) or perennial (house dust mite) n Mucus production (Runny nose, nasal stuffiness n Itching & sneezing n Treat with antihistamines or nasal steroids
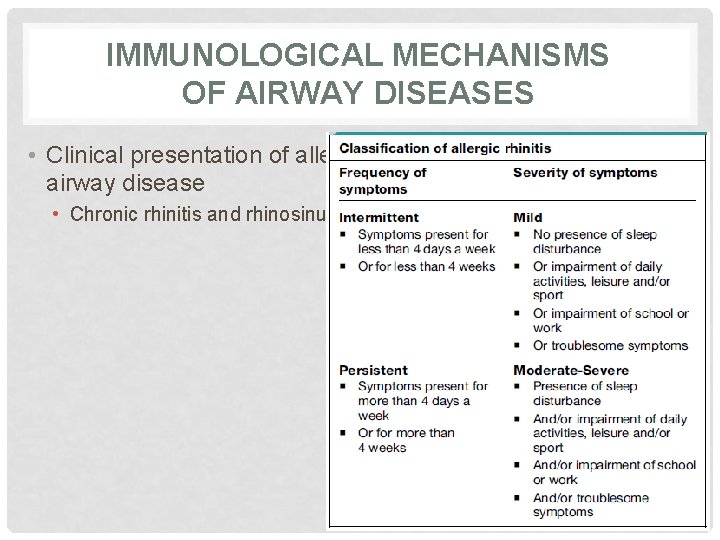
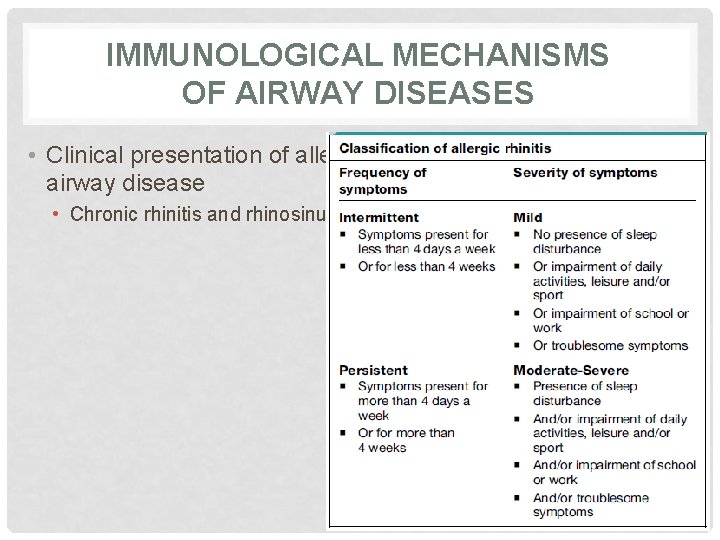
IMMUNOLOGICAL MECHANISMS OF AIRWAY DISEASES • Clinical presentation of allergic airway disease • Chronic rhinitis and rhinosinusitis
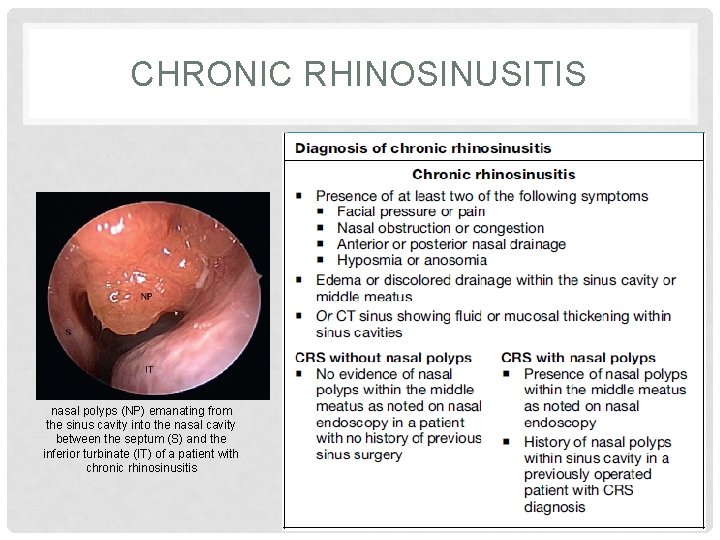
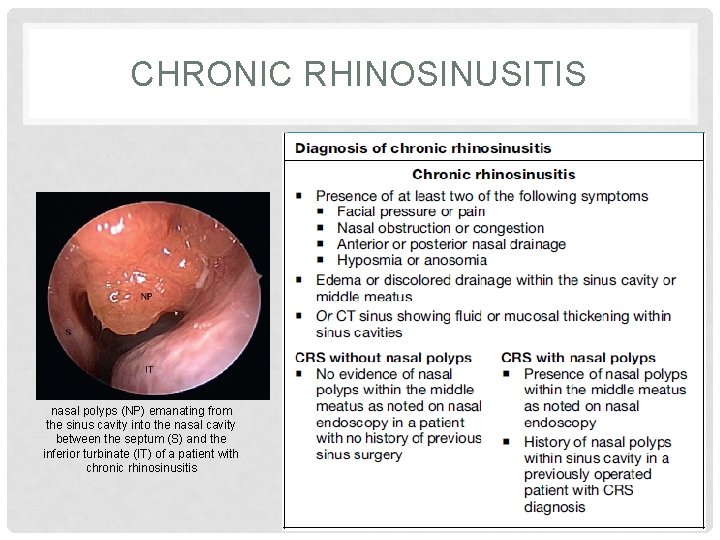
CHRONIC RHINOSINUSITIS nasal polyps (NP) emanating from the sinus cavity into the nasal cavity between the septum (S) and the inferior turbinate (IT) of a patient with chronic rhinosinusitis
ATOPIC DERMATITIS n Allergen –induced particularly milk protein from the gut enters blood stream –deposited in skin – mast cell degranulation n Exfoliating eczema and itching n Treat with antihistamines n May progress to asthma
URTICARIA n Wheal and flare n Itching n Allergen-induced n Idiopathic – pressure, cold etc. n Food – shellfish, strawberries, peanuts n Treat with antihistamines
URTICARIA • Urticaria is characterized by superficial and deep swellings. • Wheals are superficial swellings of the dermis of skin: they are pale and itchy with surrounding redness when they appear and then become pink before fading. • Acute urticaria lasts less than 6 weeks. It is common and often caused by viral infections. Urticaria due to drugs and foods falls in this category, but the diagnosis is usually clear from the history. • Chronic urticaria lasts 6 weeks or more with continuous disease activity. A cause may not be found. Urticaria occurring intermittently over a period of more than 6 weeks can be defined as episodic.
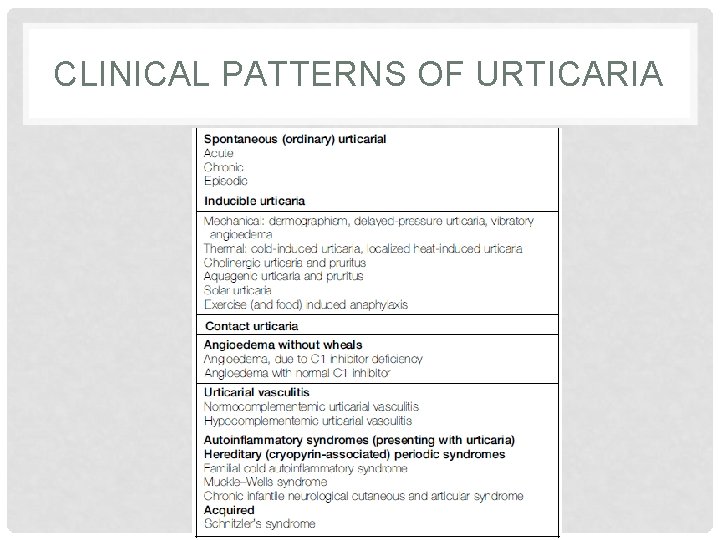
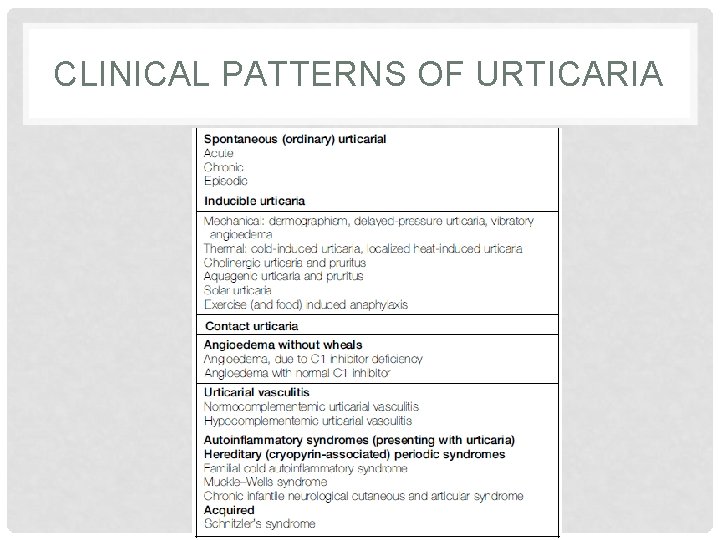
CLINICAL PATTERNS OF URTICARIA
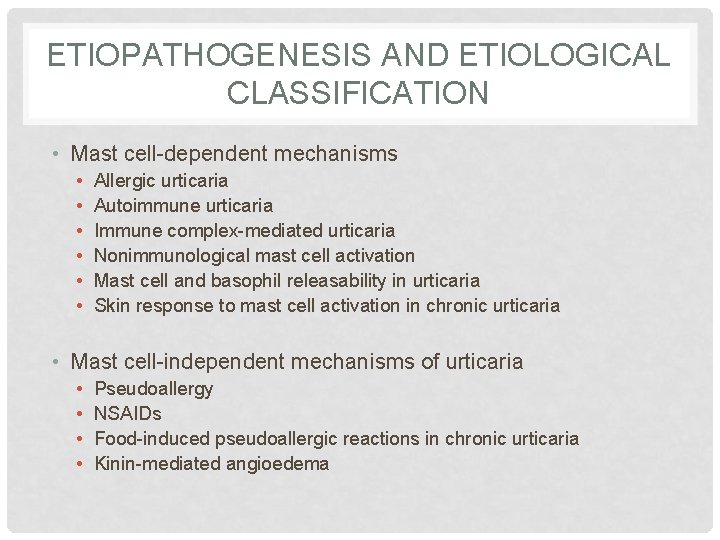
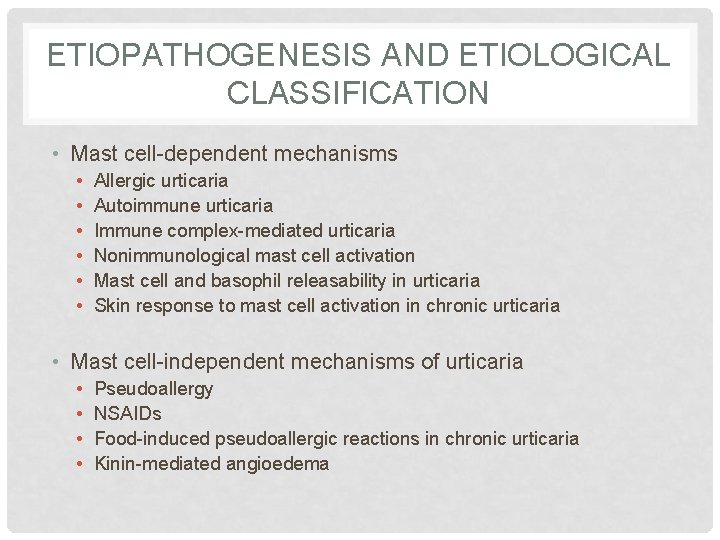
ETIOPATHOGENESIS AND ETIOLOGICAL CLASSIFICATION • Mast cell-dependent mechanisms • • • Allergic urticaria Autoimmune urticaria Immune complex-mediated urticaria Nonimmunological mast cell activation Mast cell and basophil releasability in urticaria Skin response to mast cell activation in chronic urticaria • Mast cell-independent mechanisms of urticaria • • Pseudoallergy NSAIDs Food-induced pseudoallergic reactions in chronic urticaria Kinin-mediated angioedema
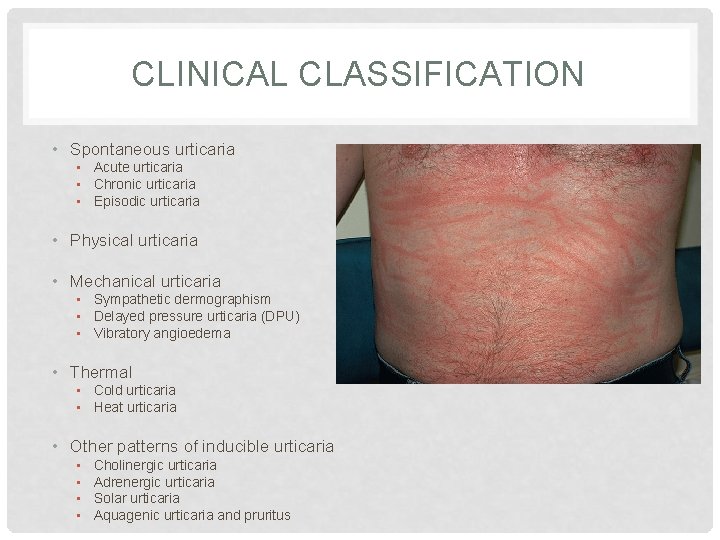
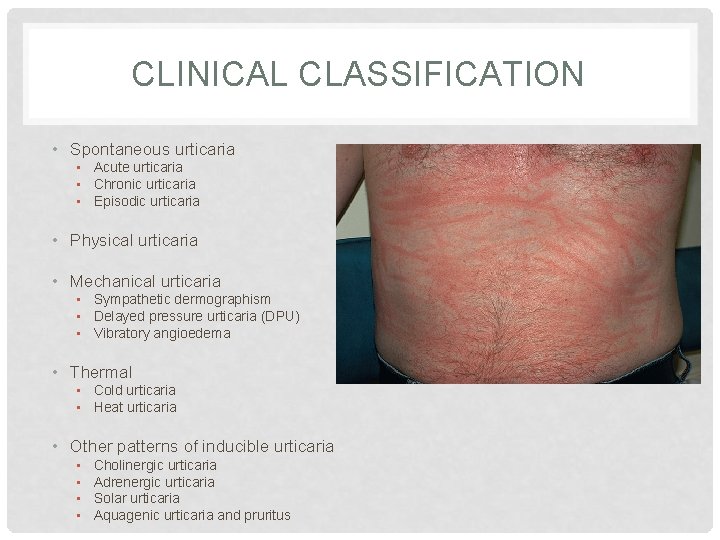
CLINICAL CLASSIFICATION • Spontaneous urticaria • Acute urticaria • Chronic urticaria • Episodic urticaria • Physical urticaria • Mechanical urticaria • Sympathetic dermographism • Delayed pressure urticaria (DPU) • Vibratory angioedema • Thermal • Cold urticaria • Heat urticaria • Other patterns of inducible urticaria • • Cholinergic urticaria Adrenergic urticaria Solar urticaria Aquagenic urticaria and pruritus
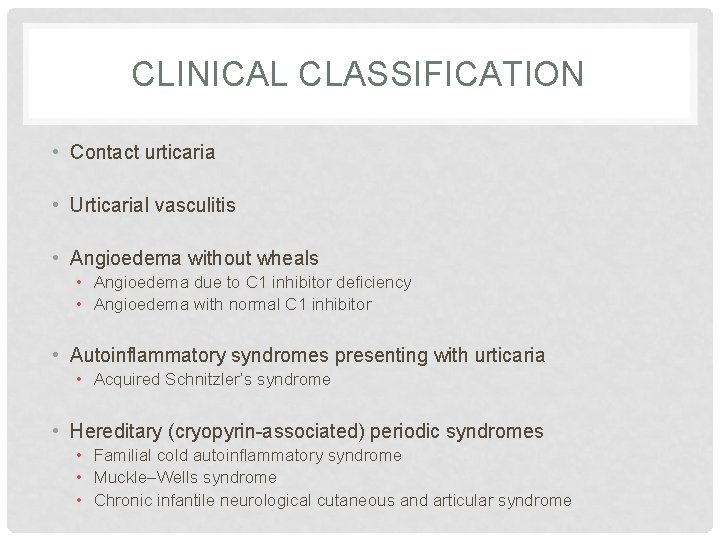
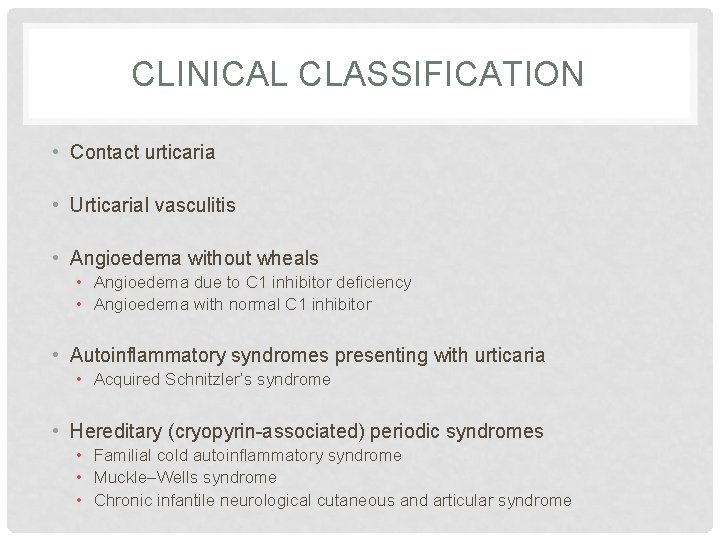
CLINICAL CLASSIFICATION • Contact urticaria • Urticarial vasculitis • Angioedema without wheals • Angioedema due to C 1 inhibitor deficiency • Angioedema with normal C 1 inhibitor • Autoinflammatory syndromes presenting with urticaria • Acquired Schnitzler’s syndrome • Hereditary (cryopyrin-associated) periodic syndromes • Familial cold autoinflammatory syndrome • Muckle–Wells syndrome • Chronic infantile neurological cutaneous and articular syndrome
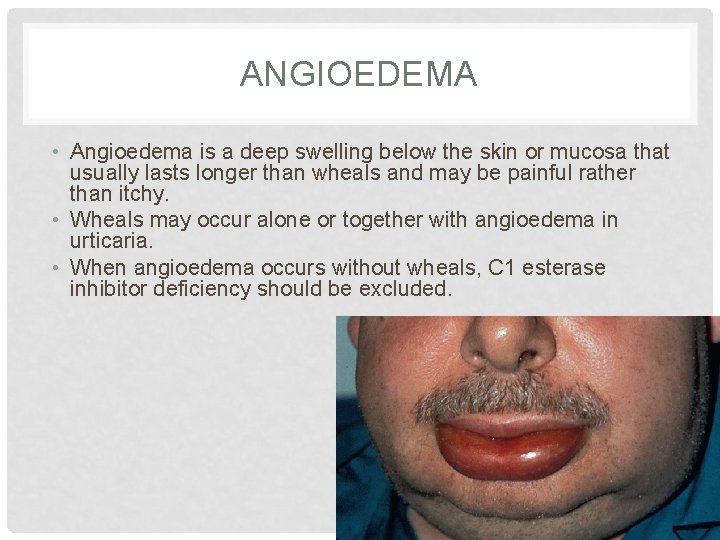
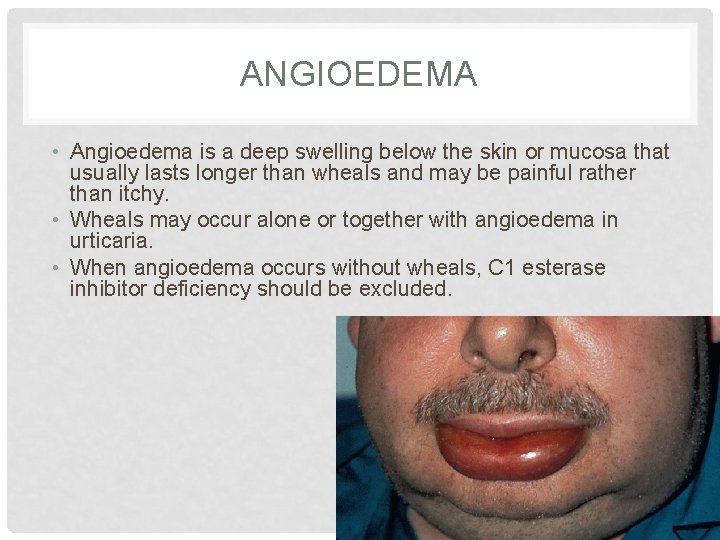
ANGIOEDEMA • Angioedema is a deep swelling below the skin or mucosa that usually lasts longer than wheals and may be painful rather than itchy. • Wheals may occur alone or together with angioedema in urticaria. • When angioedema occurs without wheals, C 1 esterase inhibitor deficiency should be excluded.
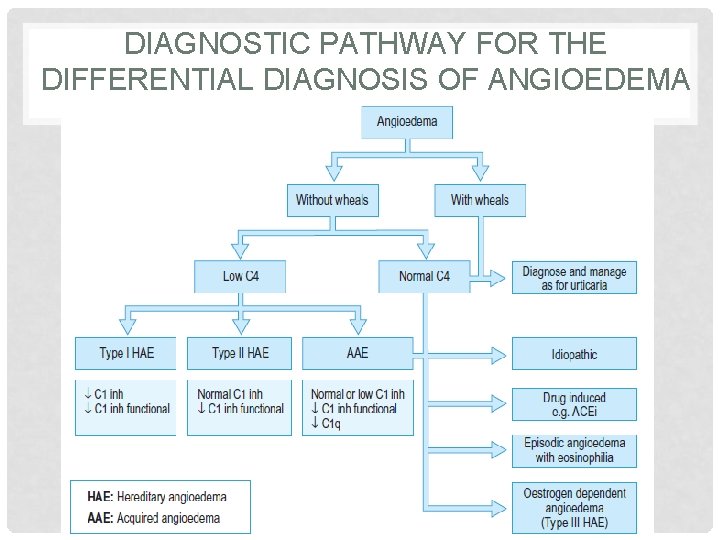
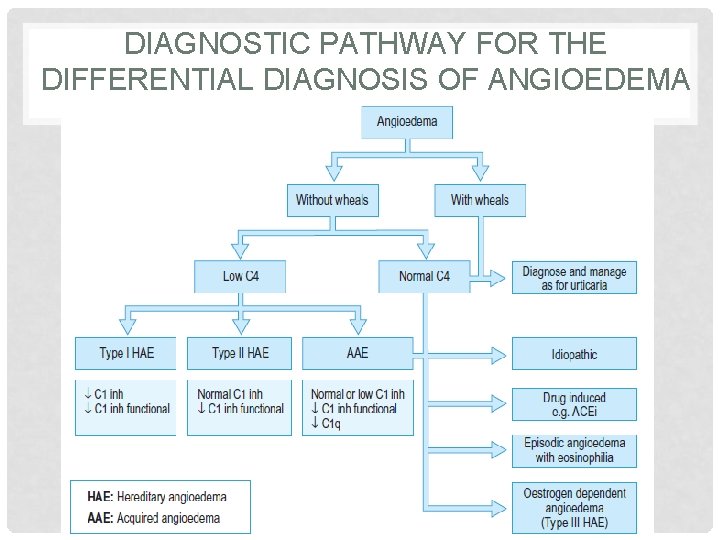
DIAGNOSTIC PATHWAY FOR THE DIFFERENTIAL DIAGNOSIS OF ANGIOEDEMA
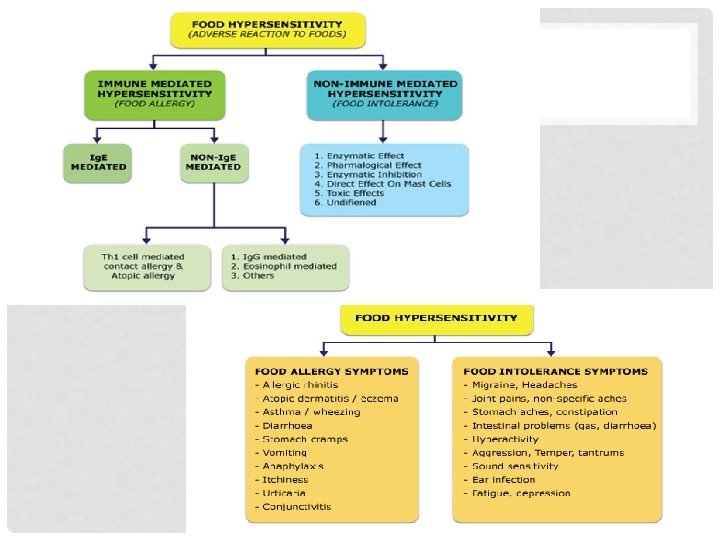
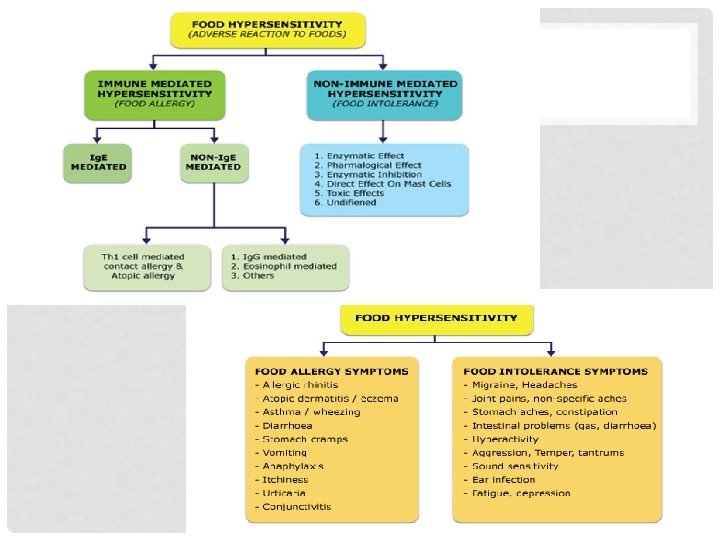
FOOD HYPERSENSITIVITY n Food allergy is an inappropriate immune response to an otherwise harmless food. n True food allergy involves several types of immunological responses. n Food allergens are usually proteins. n Some foods may contain haptens or haptens carrier. (A hepten- a small molecule that has the ability to combine with an Ab or a cell-surface receptor. )
FOOD ALLERGY • The most common allergies to food are Ig. E-mediated reactions. • Class 1 food allergy is considered as a failure to establish or maintain oral tolerance. • Any event causing epithelial barrier defects may cause allergic sensitization to food allergens, not only in the gut, but also in the skin and airways. • Successful tolerance induction depends on the dose and timing of enteric exposure to potential allergens, commensal microbiota, and dietary factors, such as vitamin A and D, or lipids. • Class 2 food allergy is due to immunological cross-reactivity between food and respiratory allergens. • At present no effective specific immunotherapy for Ig. E mediated food allergy exists.
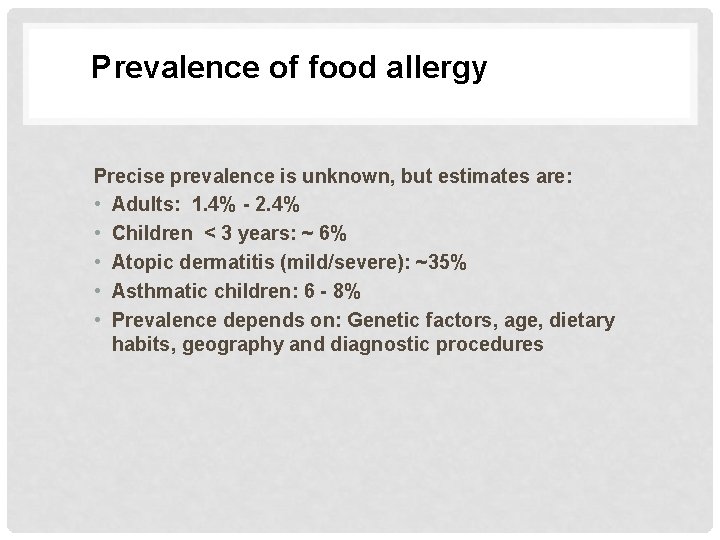
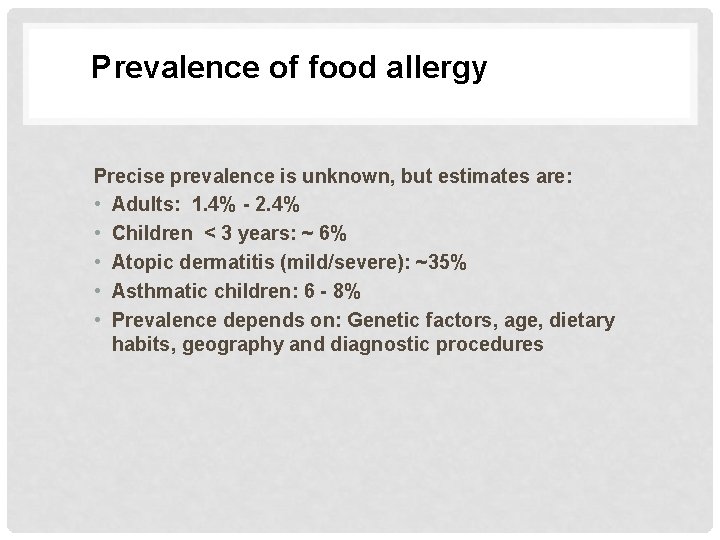
Prevalence of food allergy Precise prevalence is unknown, but estimates are: • Adults: 1. 4% - 2. 4% • Children < 3 years: ~ 6% • Atopic dermatitis (mild/severe): ~35% • Asthmatic children: 6 - 8% • Prevalence depends on: Genetic factors, age, dietary habits, geography and diagnostic procedures

Foods more frequently implicated in food allergy Children Adults ü Cow’s milk ü Egg ü Fish ü Peanut ü Fruits ü Legumes ü Wheat ü Fruits ü Peanuts ü Tree nuts ü Fish ü Shellfish
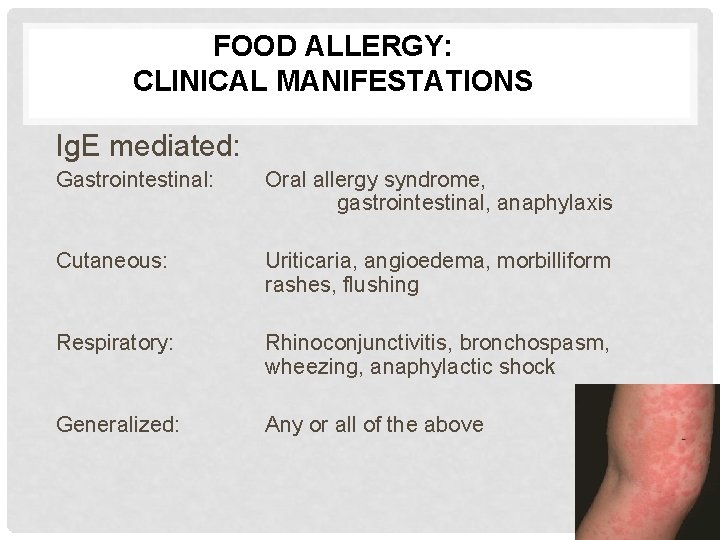
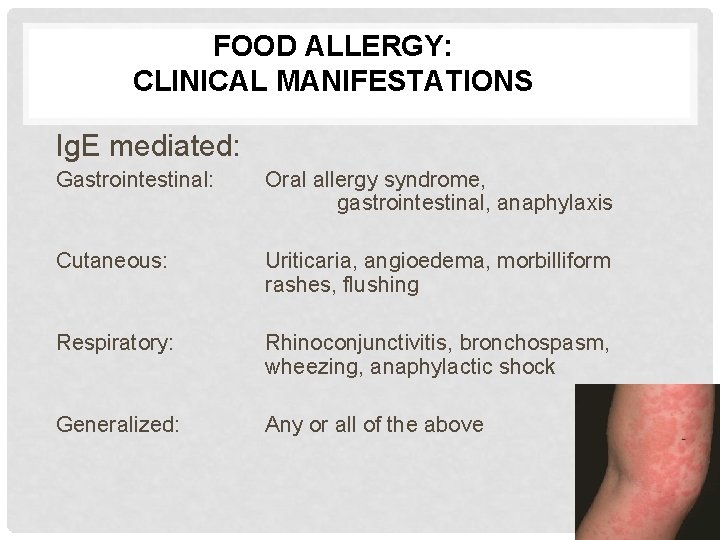
FOOD ALLERGY: CLINICAL MANIFESTATIONS Ig. E mediated: Gastrointestinal: Oral allergy syndrome, gastrointestinal, anaphylaxis Cutaneous: Uriticaria, angioedema, morbilliform rashes, flushing Respiratory: Rhinoconjunctivitis, bronchospasm, wheezing, anaphylactic shock Generalized: Any or all of the above
FOOD ALLERGY: CLINICAL MANIFESTATIONS Cell mediated Gastrointestinal: Food protein-induced: Enterocolitis/proctocolitis/enteropathy syndromes, celiac disease Cutaneous: Contact dermatitis, herpetiformis dermatitis Respiratory: Food-induced pulmonary hemosiderosis (Heiner’s syndrome)
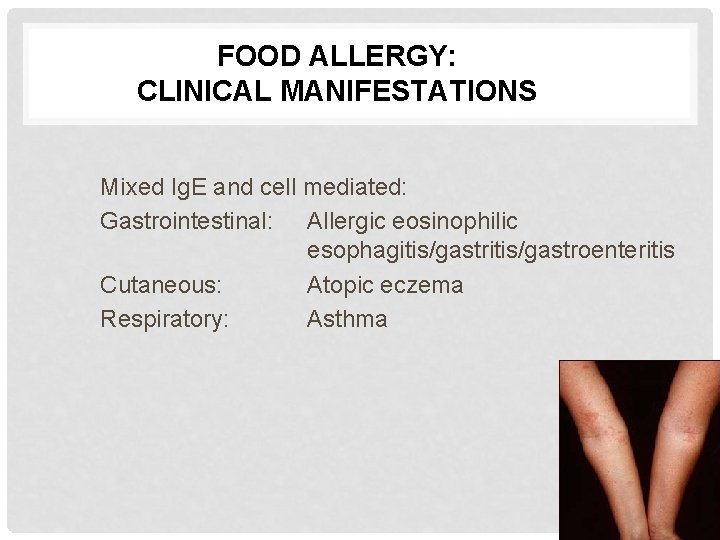
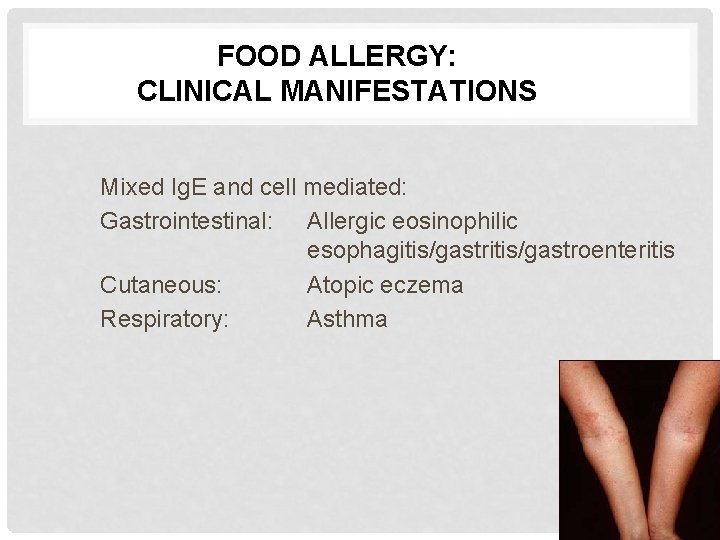
FOOD ALLERGY: CLINICAL MANIFESTATIONS Mixed Ig. E and cell mediated: Gastrointestinal: Allergic eosinophilic esophagitis/gastroenteritis Cutaneous: Atopic eczema Respiratory: Asthma
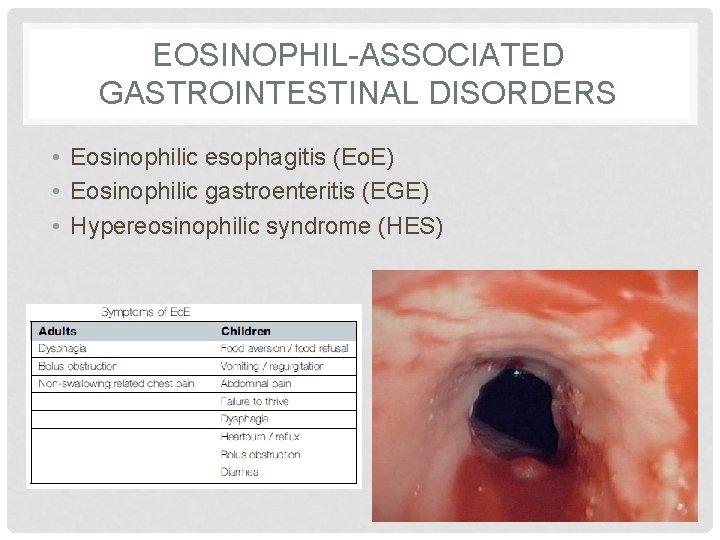
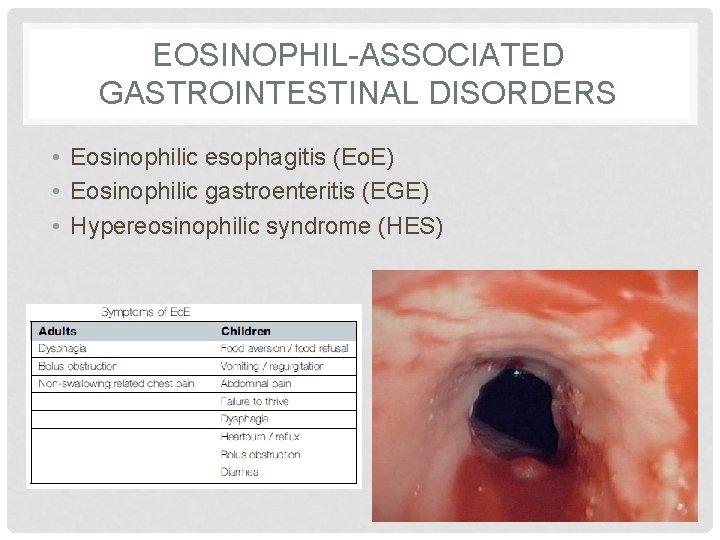
EOSINOPHIL-ASSOCIATED GASTROINTESTINAL DISORDERS • Eosinophilic esophagitis (Eo. E) • Eosinophilic gastroenteritis (EGE) • Hypereosinophilic syndrome (HES)
ASTHMA • Asthma is often recognized on clinical grounds alone, with acute attacks marked by obvious dyspnea, wheezing, cough, and use of accessory muscles of respiration. • Such attacks typically resolve with bronchodilator therapy. • Spirometry can provide more objective evidence of airway obstruction as assessed by decrements in the forced expiratory volume in 1 second (FEV 1) and other measures of air flow
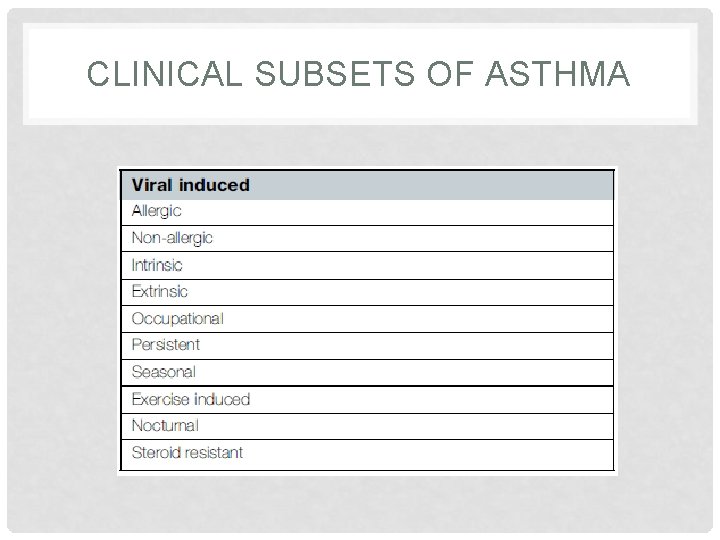
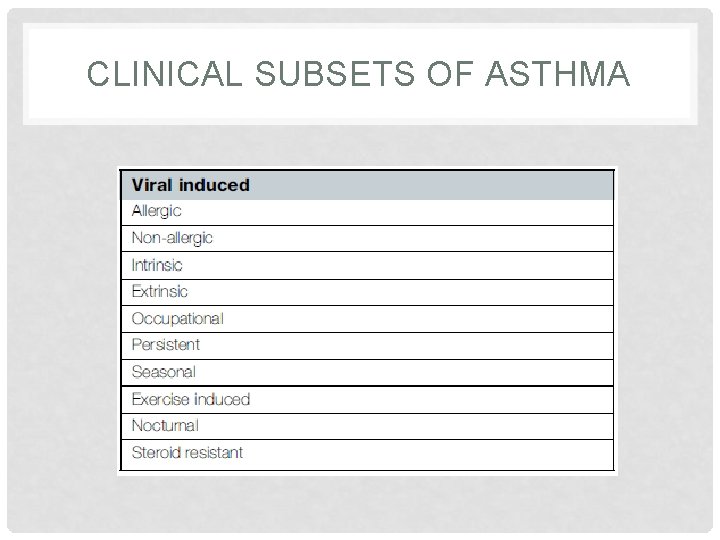
CLINICAL SUBSETS OF ASTHMA
OTHER AIRWAY ALLERGIC DISEASE SYNDROMES • Extrinsic eosinophilic syndromes • Tropical eosinophilic pneumonias • DRESS (drug rash with eosinophilia and systemic symptoms) syndrome • Allergic bronchopulmonary aspergillosis (ABPA) • Acute eosinophilic pneumonia (AEP) • Intrinsic eosinophilic syndromes • Chronic eosinophilic pneumonia (CEP) • Idiopathic hypereosinophilic syndrome (IHES) • Churg-Strauss syndrome (CSS)
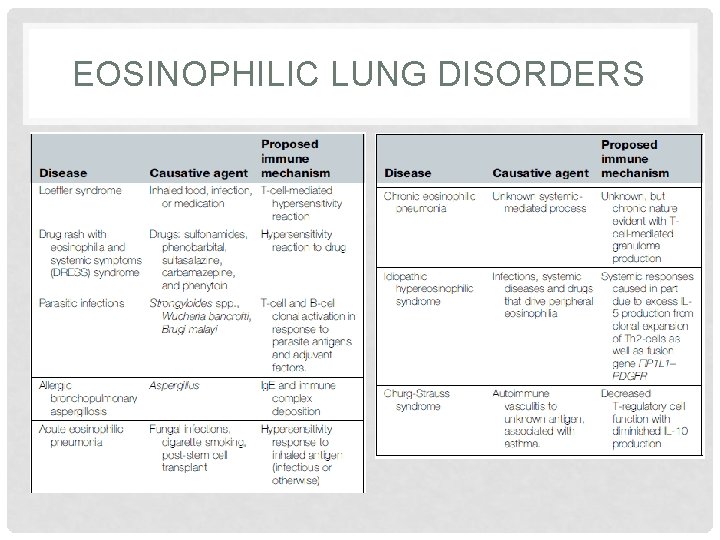
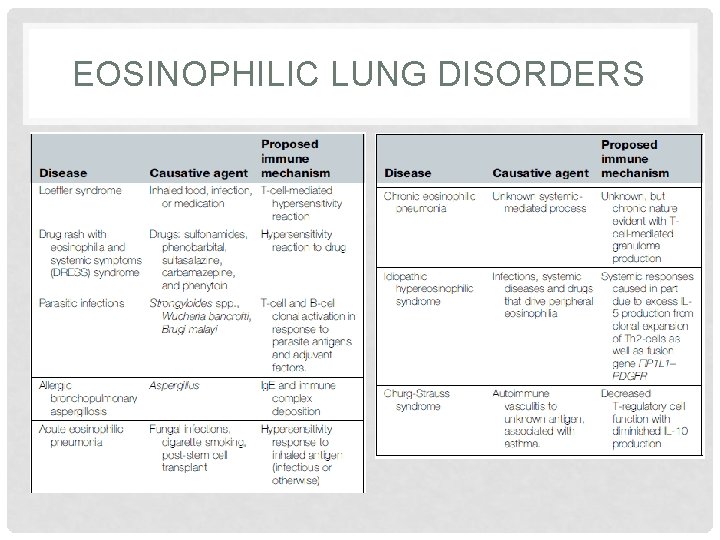
EOSINOPHILIC LUNG DISORDERS
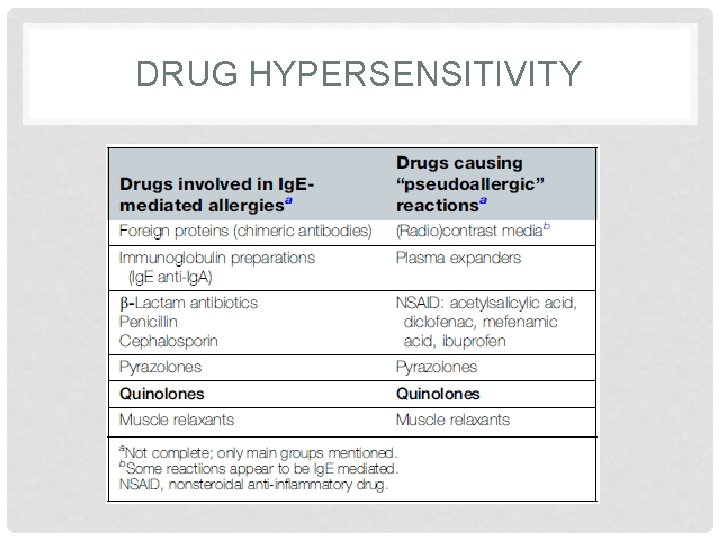
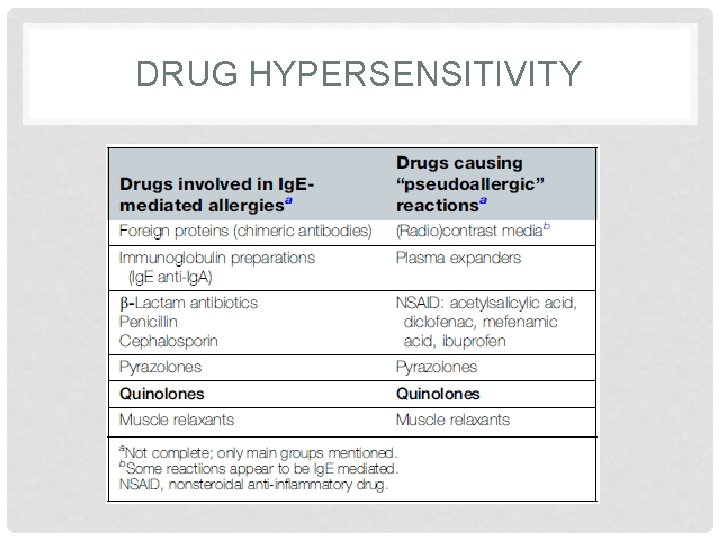
DRUG HYPERSENSITIVITY
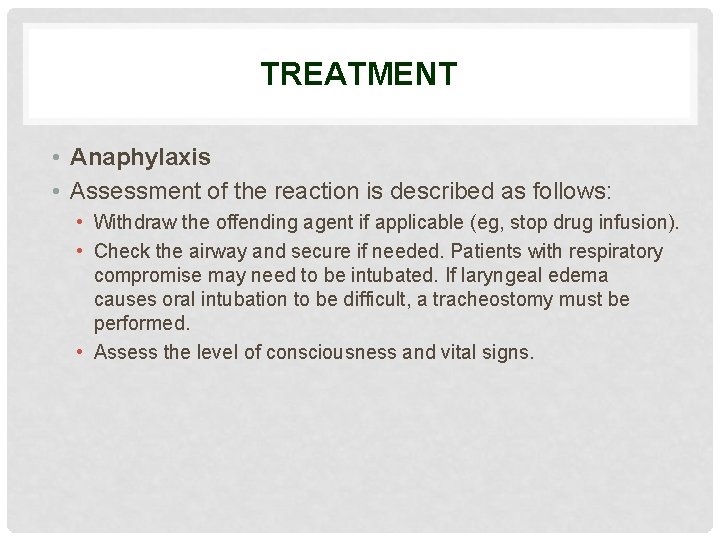
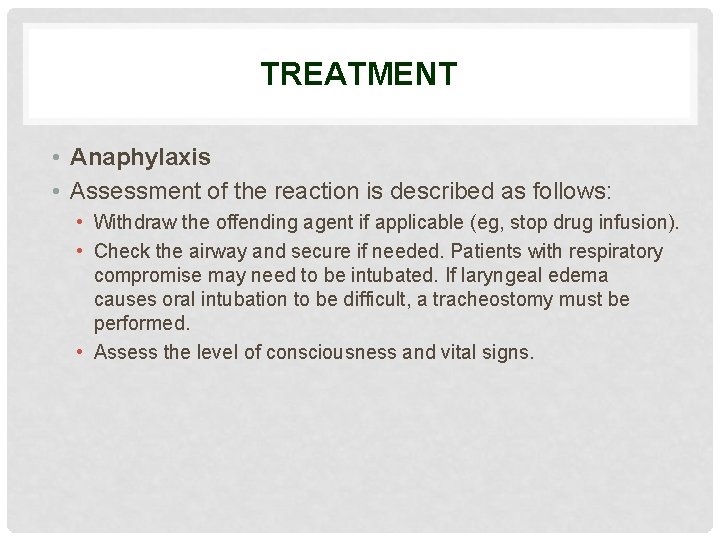
TREATMENT • Anaphylaxis • Assessment of the reaction is described as follows: • Withdraw the offending agent if applicable (eg, stop drug infusion). • Check the airway and secure if needed. Patients with respiratory compromise may need to be intubated. If laryngeal edema causes oral intubation to be difficult, a tracheostomy must be performed. • Assess the level of consciousness and vital signs.
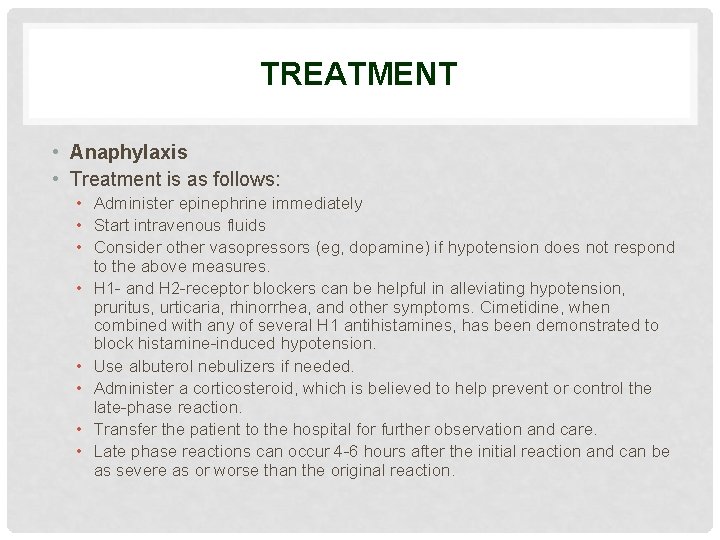
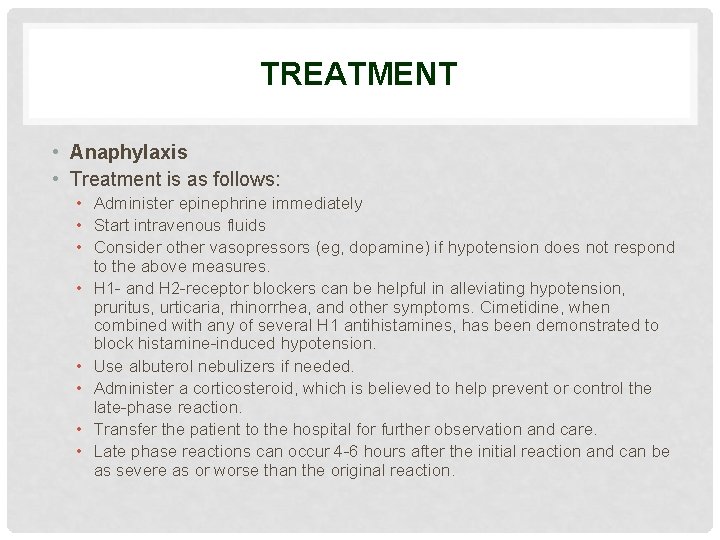
TREATMENT • Anaphylaxis • Treatment is as follows: • Administer epinephrine immediately • Start intravenous fluids • Consider other vasopressors (eg, dopamine) if hypotension does not respond to the above measures. • H 1 - and H 2 -receptor blockers can be helpful in alleviating hypotension, pruritus, urticaria, rhinorrhea, and other symptoms. Cimetidine, when combined with any of several H 1 antihistamines, has been demonstrated to block histamine-induced hypotension. • Use albuterol nebulizers if needed. • Administer a corticosteroid, which is believed to help prevent or control the late-phase reaction. • Transfer the patient to the hospital for further observation and care. • Late phase reactions can occur 4 -6 hours after the initial reaction and can be as severe as or worse than the original reaction.
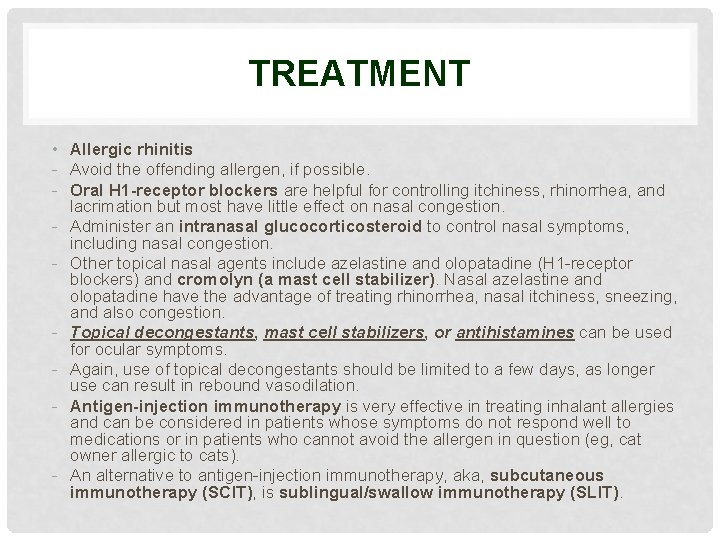
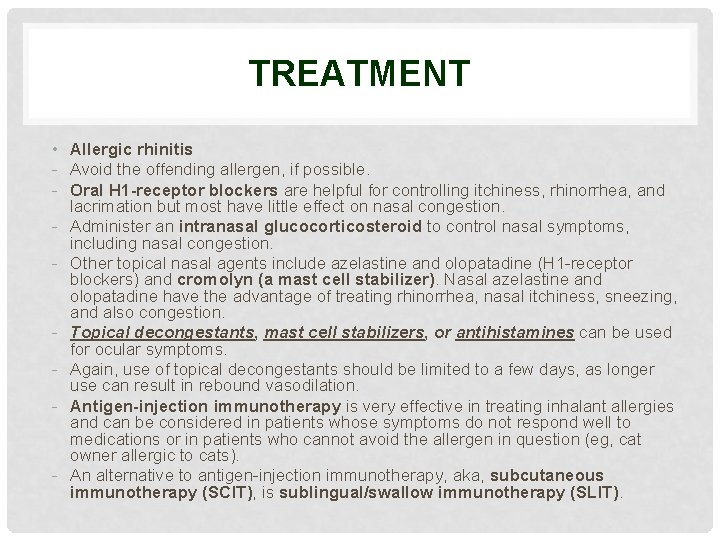
TREATMENT • Allergic rhinitis - Avoid the offending allergen, if possible. - Oral H 1 -receptor blockers are helpful for controlling itchiness, rhinorrhea, and lacrimation but most have little effect on nasal congestion. - Administer an intranasal glucocorticosteroid to control nasal symptoms, including nasal congestion. - Other topical nasal agents include azelastine and olopatadine (H 1 -receptor blockers) and cromolyn (a mast cell stabilizer). Nasal azelastine and olopatadine have the advantage of treating rhinorrhea, nasal itchiness, sneezing, and also congestion. - Topical decongestants, mast cell stabilizers, or antihistamines can be used for ocular symptoms. - Again, use of topical decongestants should be limited to a few days, as longer use can result in rebound vasodilation. - Antigen-injection immunotherapy is very effective in treating inhalant allergies and can be considered in patients whose symptoms do not respond well to medications or in patients who cannot avoid the allergen in question (eg, cat owner allergic to cats). - An alternative to antigen-injection immunotherapy, aka, subcutaneous immunotherapy (SCIT), is sublingual/swallow immunotherapy (SLIT).
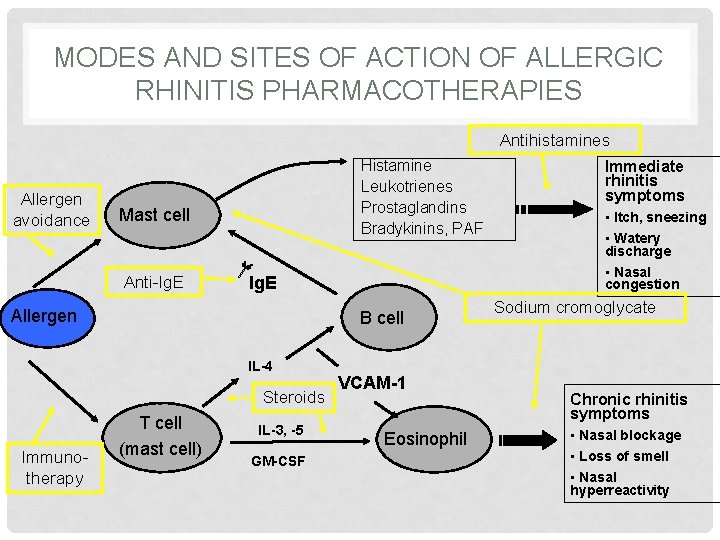
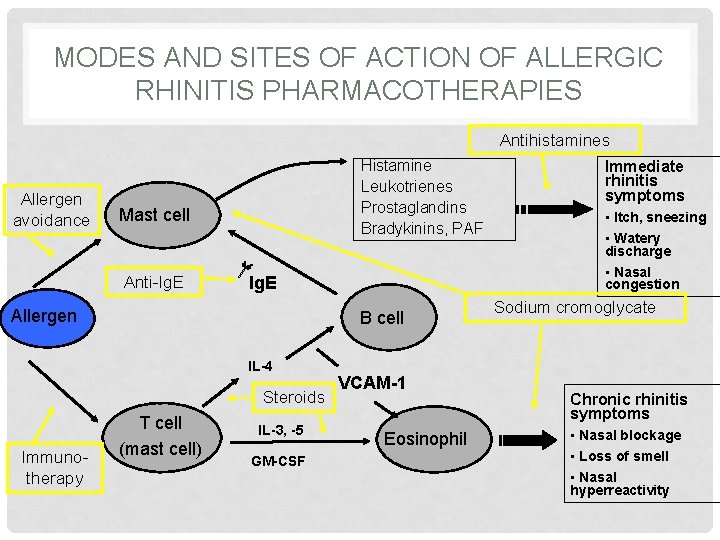
MODES AND SITES OF ACTION OF ALLERGIC RHINITIS PHARMACOTHERAPIES Antihistamines Allergen avoidance Histamine Leukotrienes Prostaglandins Bradykinins, PAF Mast cell Anti-Ig. E Allergen B cell IL-4 Steroids Immunotherapy T cell (mast cell) IL-3, -5 GM-CSF VCAM-1 Eosinophil Immediate rhinitis symptoms • Itch, sneezing • Watery discharge • Nasal congestion Sodium cromoglycate Chronic rhinitis symptoms • Nasal blockage • Loss of smell • Nasal hyperreactivity
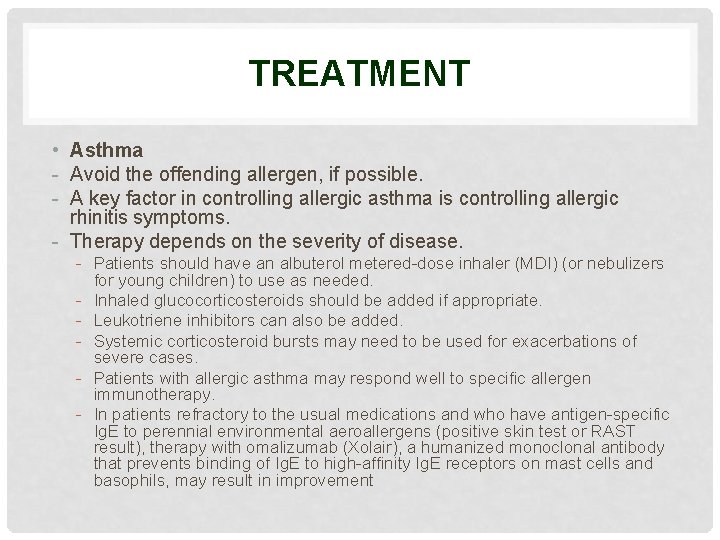
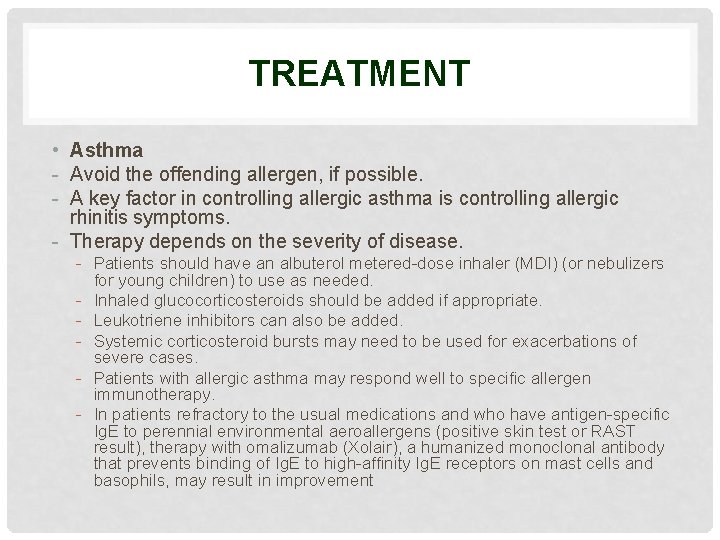
TREATMENT • Asthma - Avoid the offending allergen, if possible. - A key factor in controlling allergic asthma is controlling allergic rhinitis symptoms. - Therapy depends on the severity of disease. - Patients should have an albuterol metered-dose inhaler (MDI) (or nebulizers for young children) to use as needed. - Inhaled glucocorticosteroids should be added if appropriate. - Leukotriene inhibitors can also be added. - Systemic corticosteroid bursts may need to be used for exacerbations of severe cases. - Patients with allergic asthma may respond well to specific allergen immunotherapy. - In patients refractory to the usual medications and who have antigen-specific Ig. E to perennial environmental aeroallergens (positive skin test or RAST result), therapy with omalizumab (Xolair), a humanized monoclonal antibody that prevents binding of Ig. E to high-affinity Ig. E receptors on mast cells and basophils, may result in improvement
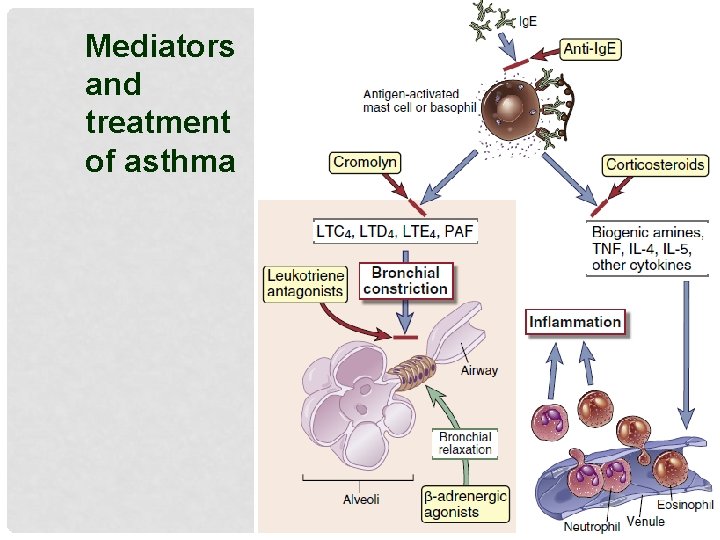
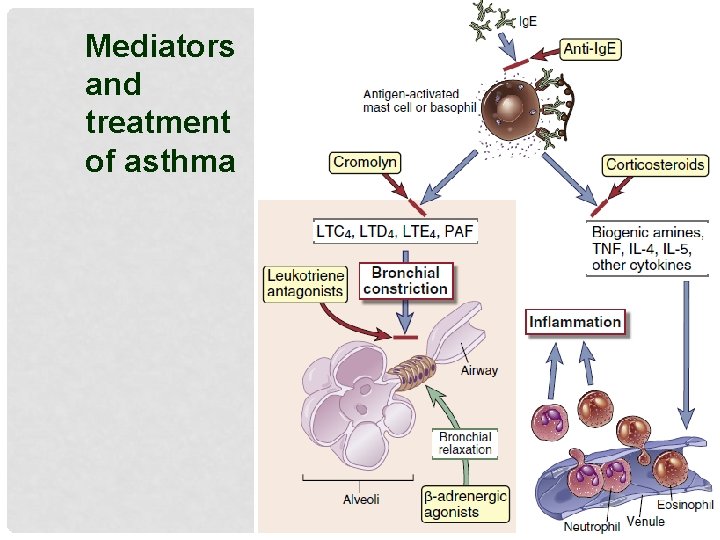
Mediators and treatment of asthma
TREATMENT • • Urticaria/angioedema Eliminate infectious, drug, or food causes. Avoid the offending allergen if known. Minimize nonspecific aggravators, including heat, stress, alcohol, nonsteroidal anti-inflammatory drugs, and pressure. Regular oral antihistamines are the first line of therapy for all spontaneous and inducible urticarias. Second-line treatments, including short courses of oral corticosteroids, may be necessary for specific clinical situations. An H 1 -receptor blocker should be added. If symptoms are not controlled with this alone, an H 2 -receptor blocker, leukotriene inhibitor, or oral glucocorticosteroid can be added. Most patients require higher than the usual doses; employing twice daily H 1 and H 2 antihistamines for successful control is not uncommon. Immunosuppressive therapies should be reserved for patients with severe autoimmune urticaria or steroid dependent urticaria that has not responded to other first and second-line measures.
TREATMENT • Atopic dermatitis • 1. Skin care to restore and preserve the epidermal barrier function • Individually adapted emollients and/or ointments with or without urea • 2. Recognize and eliminate the provocation factors • Allergological diagnostic, food allergens and aeroallergens, encasing • 3. Control of skin inflammation and pruritus • • Topical steroids (first-line), topical calcineurin inhibitors Phototherapy Antihistamines Systemic steroids, immunosuppressive agents (cyclosporine A, azathioprine, mycophenolate mofetil) • Specific immunotherapy • Biologicals • 4. Reduce microbial colonization • Topical antiseptics • Systemic antibiotics only in severely infected cases • 5. Education • Need for early intervention • Atopic dermatitis educational programs, atopic dermatitis schools

MCQ * Hypersensitivity reaction of the immune system to a component in a food is called _____. A. A food allergy B. food intolerance C. food malabsorption D. metabolic syndrome * A cluster of GI symptoms that occur after eating a particular food is called ______. A. food intolerance A B. GI disorders C. food malabsorption D. food allergy
MCQ Which one of the following statements is NOT true for peanut allergy? A. Peanut allergy is an example of immediate hypersensitivity B. Atopy is a risk factor in peanut allergy C. Anaphylaxis can occur on first exposure D D. Ig. G is believed to be centrally involved in anaphylaxis to peanut antigens E. Self administered adrenaline can be life saving
MCQ Systemic anaphylaxis is NOT caused by which one of the following: A. Wasp venom B. ACE inhibitors B C. Penicillin D. Nut ingestion E. Latex
MCQ Which one of the following statements about food allergy is true? A In children, it is often due to cow's milk. B Food allergy can be diagnosed confidently by skin-prick testing. C Migraine is a common presenting feature. D Food allergy is a common cause of irritable bowel syndrome. E Most children will ‘grow out’ of nut allergy by the age of 11 years.
MCQ Which one of the following is a FALSE statement about atopic eczema? A It commonly begins in infancy. B Super-added herpes simplex infection is a serious complication. C The serum Ig. E level is normally raised. D The skin lesions are typically itchy. E Treatment with systemic steroids is often necessary.

Reference

Thank you for your attention