All Ceramic Crowns DR MUHAMMAD RIZWAN MEMON F

































- Slides: 89
All Ceramic Crowns DR MUHAMMAD RIZWAN MEMON F. C. P. S Assistant Professor
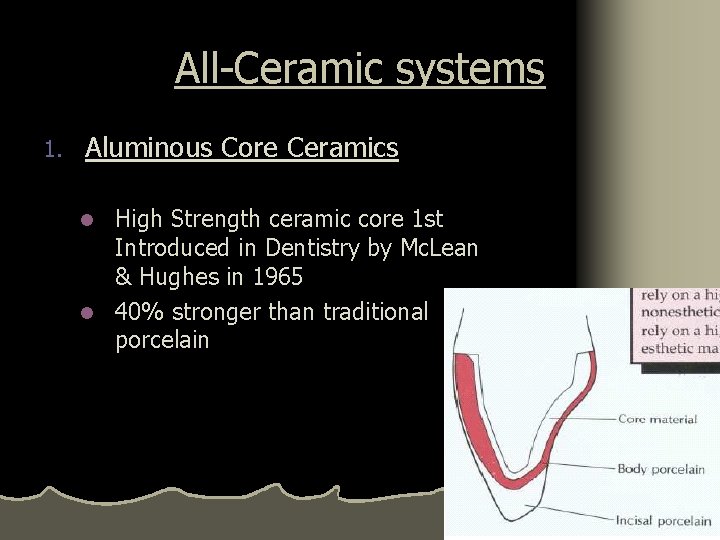
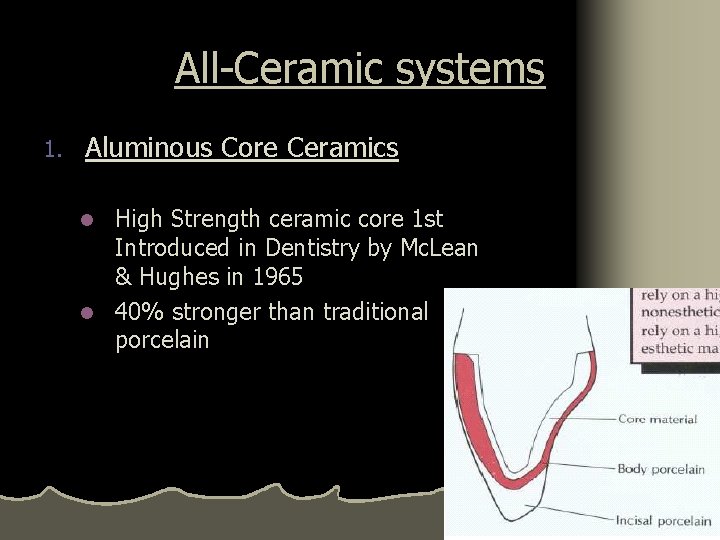
All-Ceramic systems 1. Aluminous Core Ceramics High Strength ceramic core 1 st Introduced in Dentistry by Mc. Lean & Hughes in 1965 l 40% stronger than traditional porcelain l
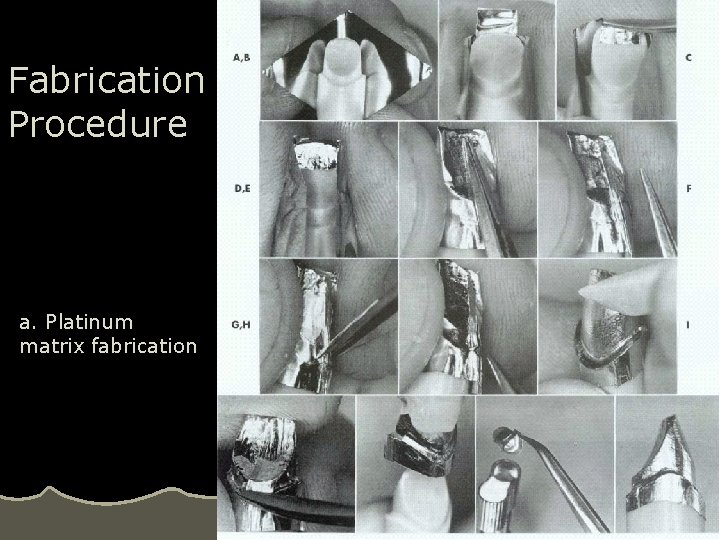
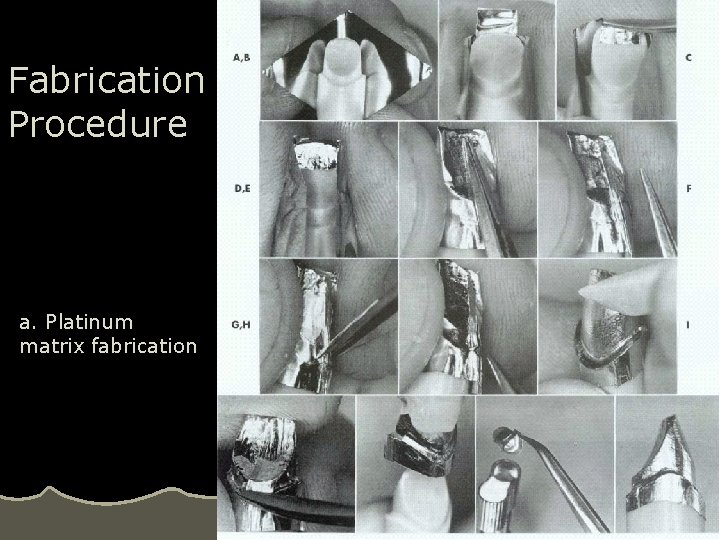
Fabrication Procedure a. Platinum matrix fabrication
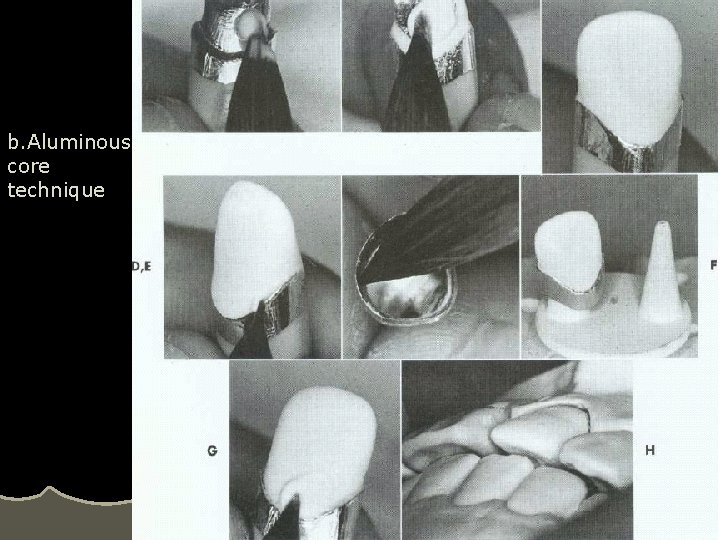
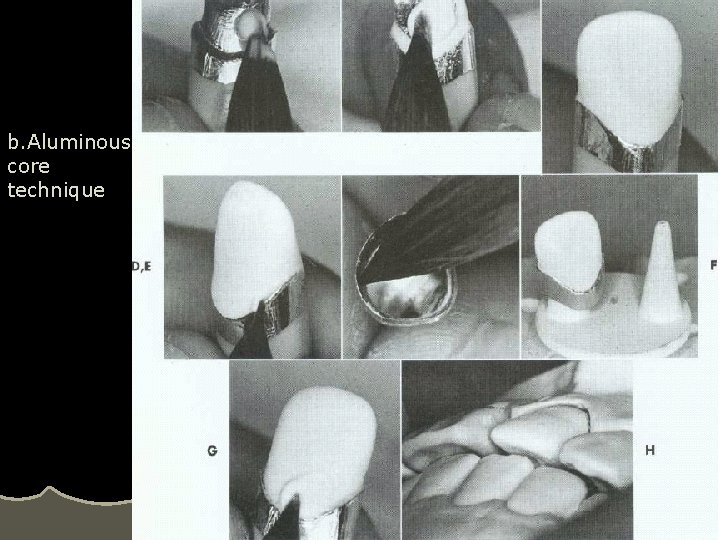
b. Aluminous core technique
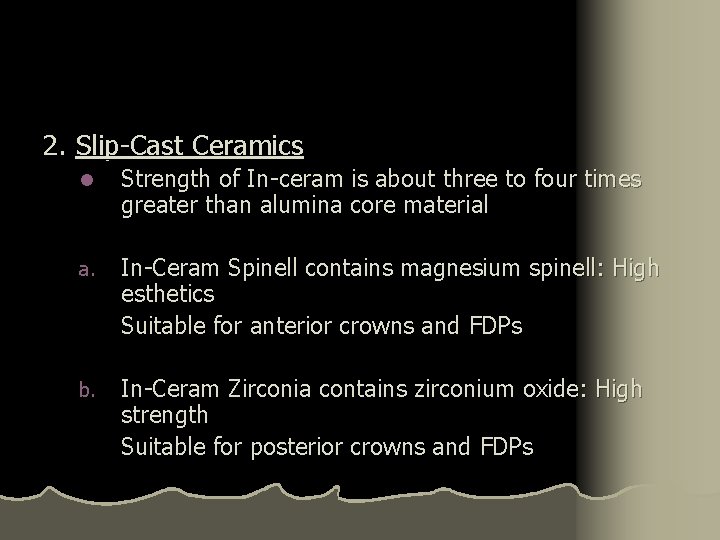
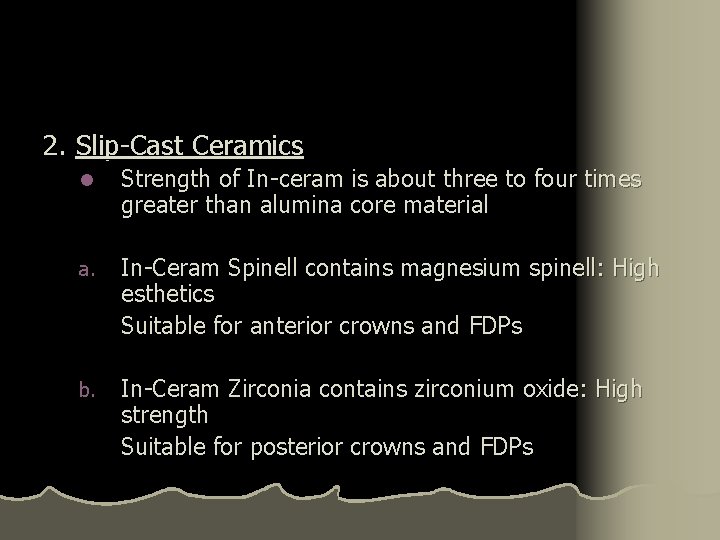
2. Slip-Cast Ceramics l Strength of In-ceram is about three to four times greater than alumina core material a. In-Ceram Spinell contains magnesium spinell: High esthetics Suitable for anterior crowns and FDPs b. In-Ceram Zirconia contains zirconium oxide: High strength Suitable for posterior crowns and FDPs
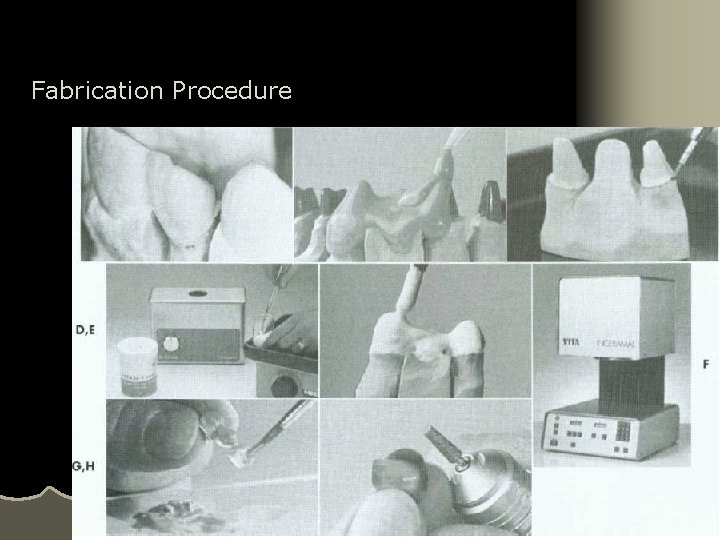
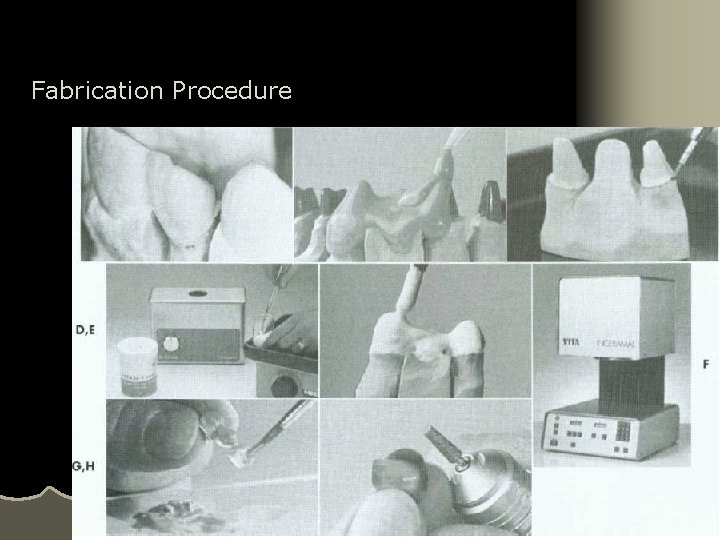
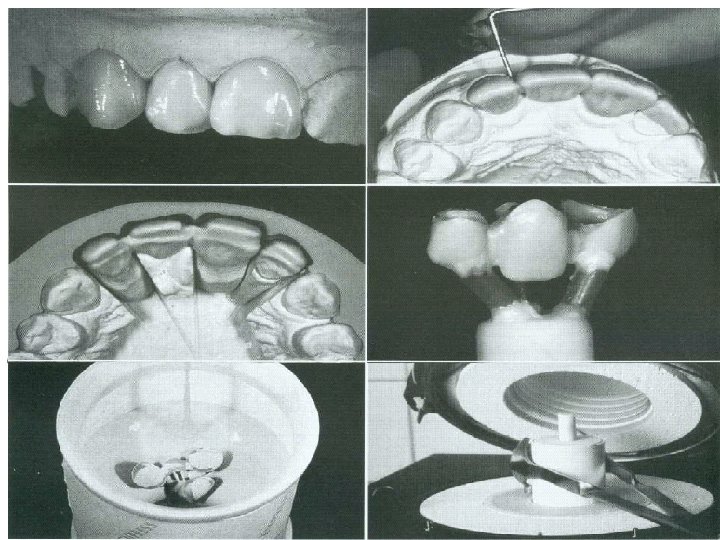
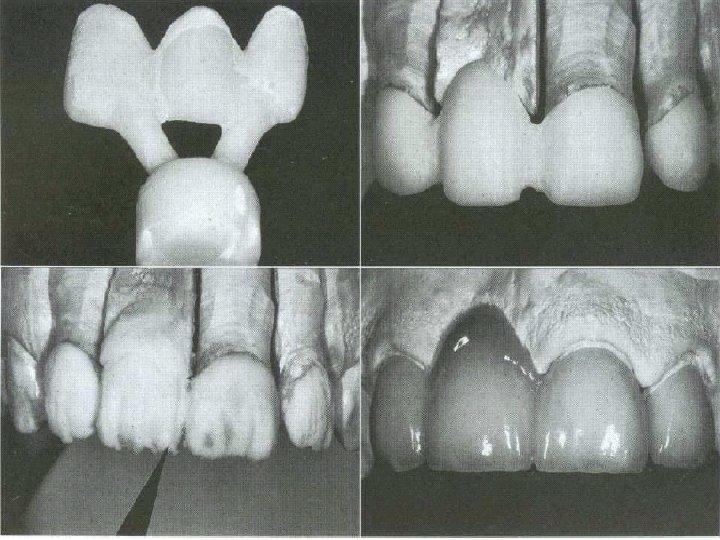
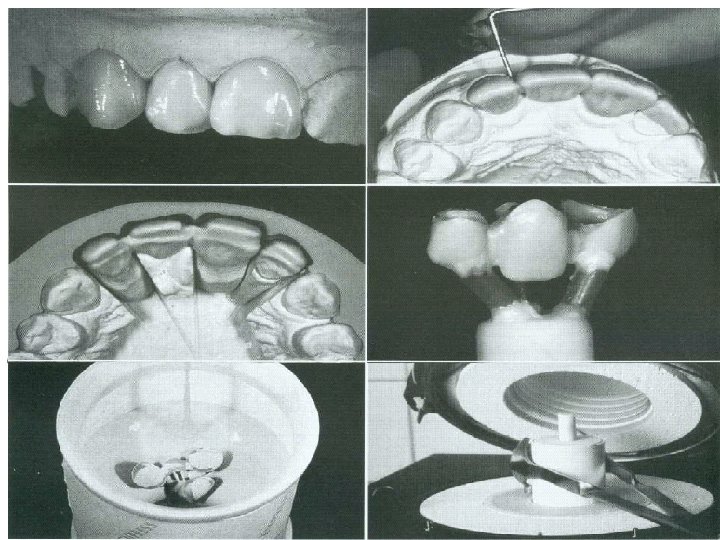
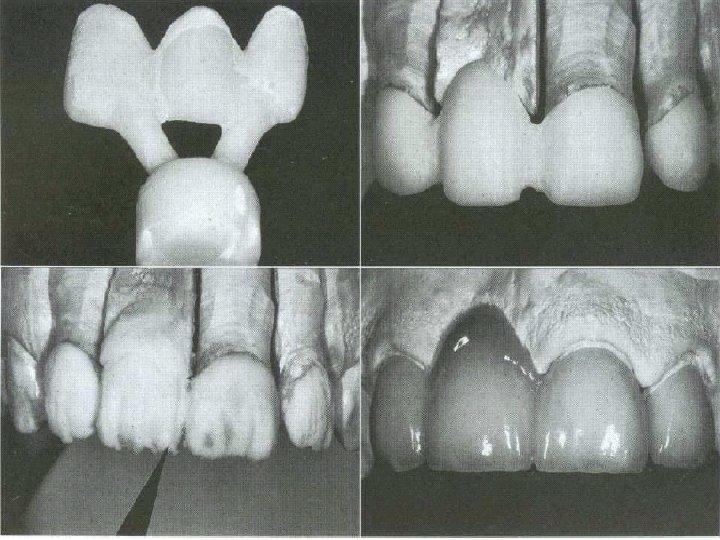
Fabrication Procedure
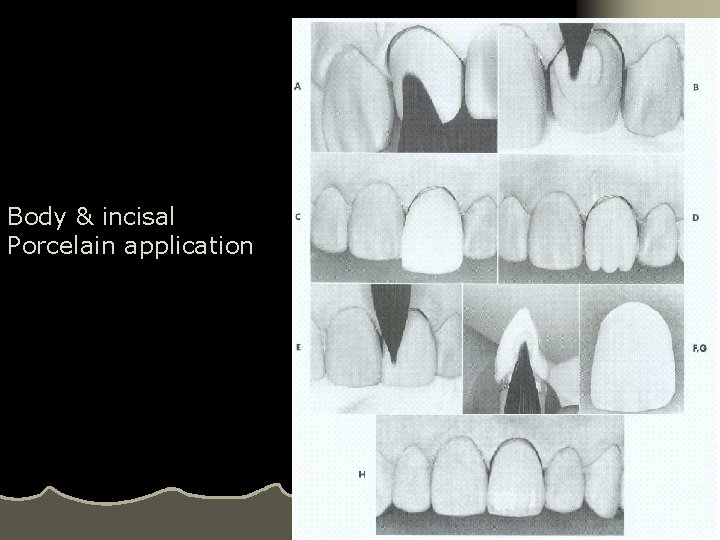
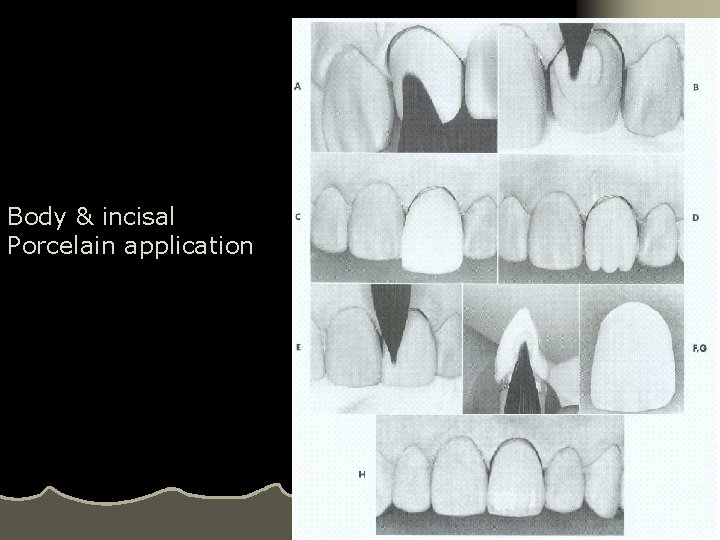
Body & incisal Porcelain application
3. Hot-Pressed Ceramics: a. Leucite based: IPS Impress Used for crowns but not possessed adequate strength for FDPs b. Lithium Silicate based: IPS Impress 2 Used for crowns but also suitable for anterior FDPs
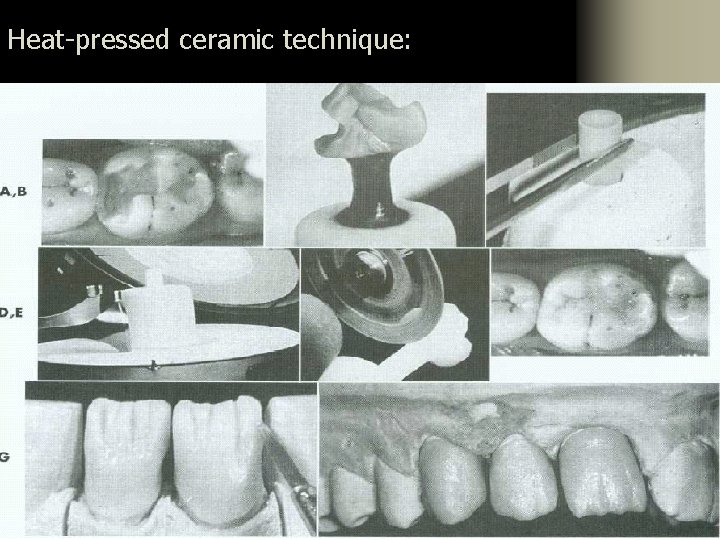
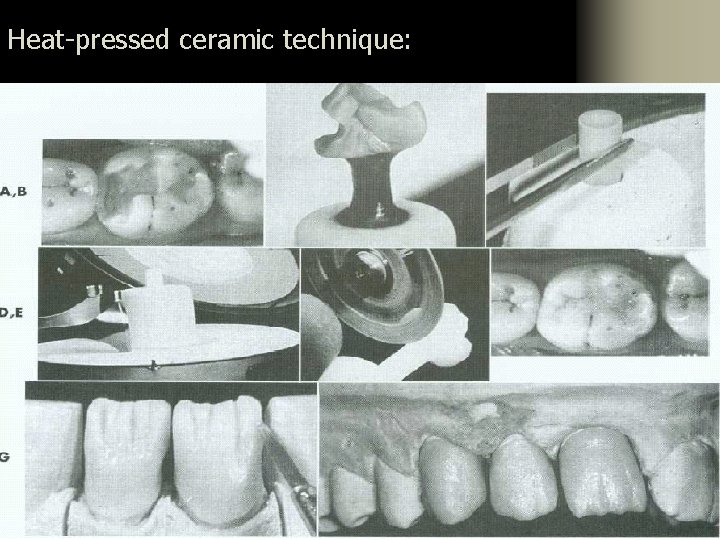
Heat-pressed ceramic technique:
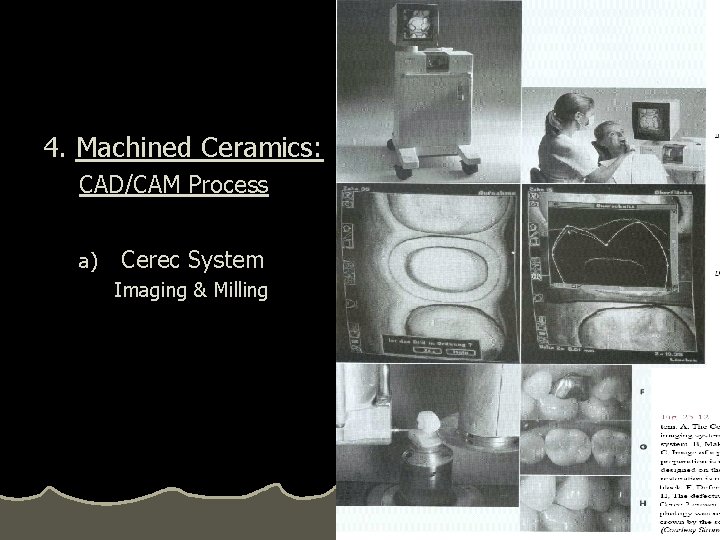
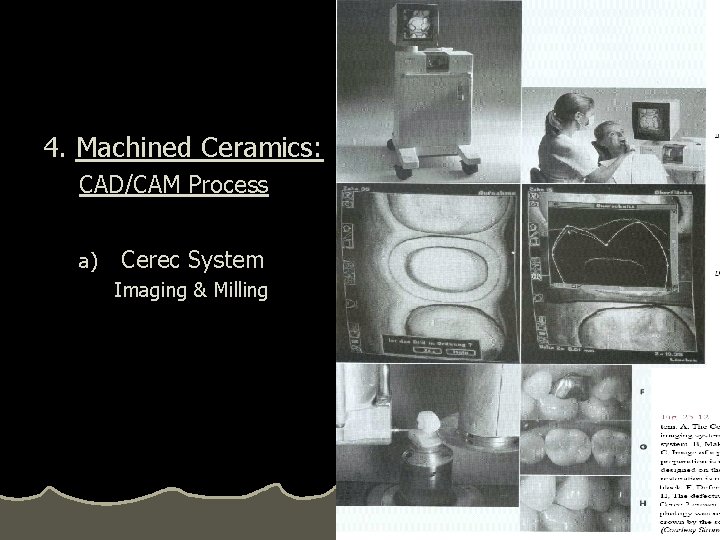
4. Machined Ceramics: CAD/CAM Process a) Cerec System Imaging & Milling
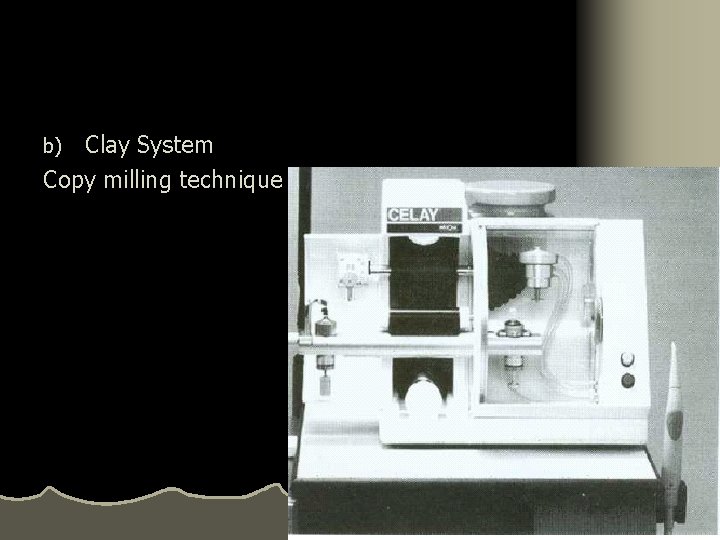
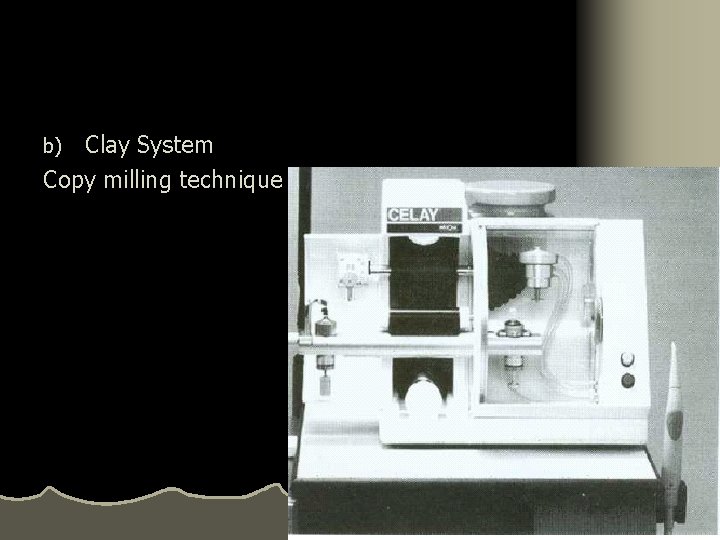
Clay System Copy milling technique b)
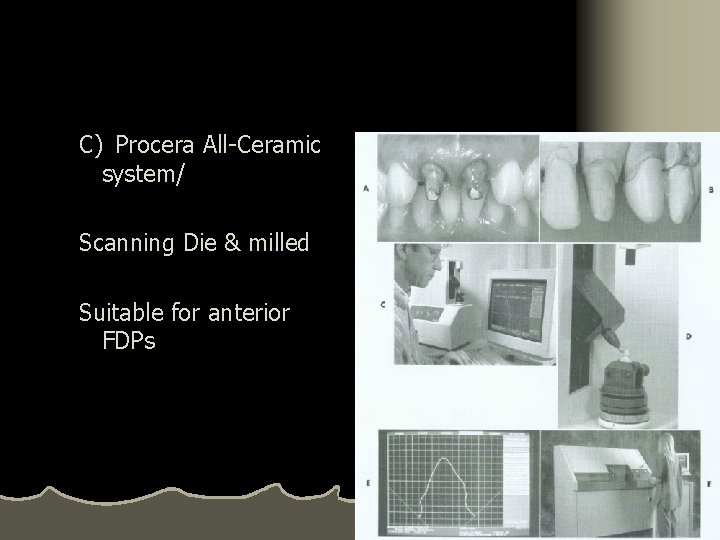
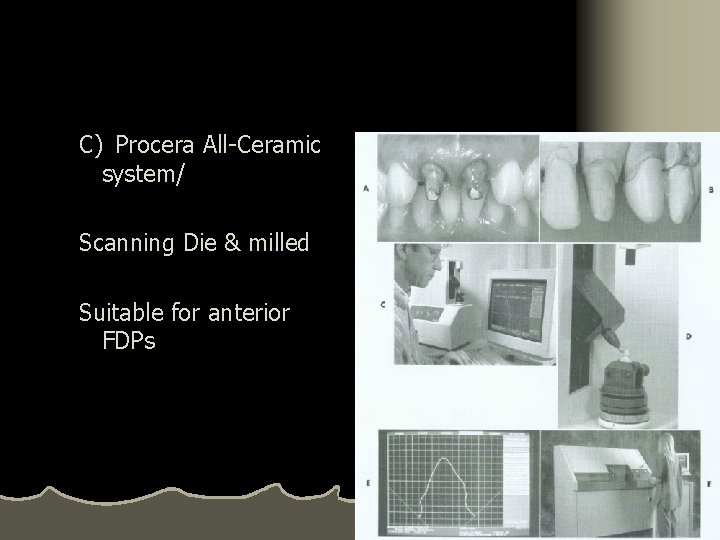
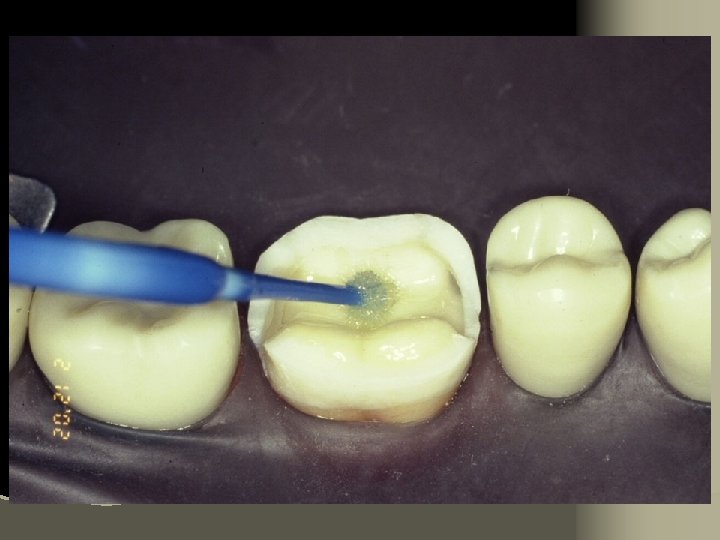
C) Procera All-Ceramic system/ Scanning Die & milled Suitable for anterior FDPs
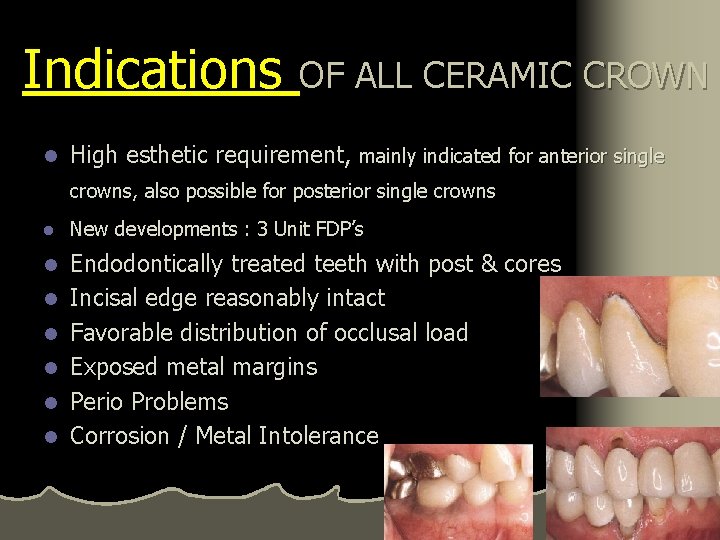
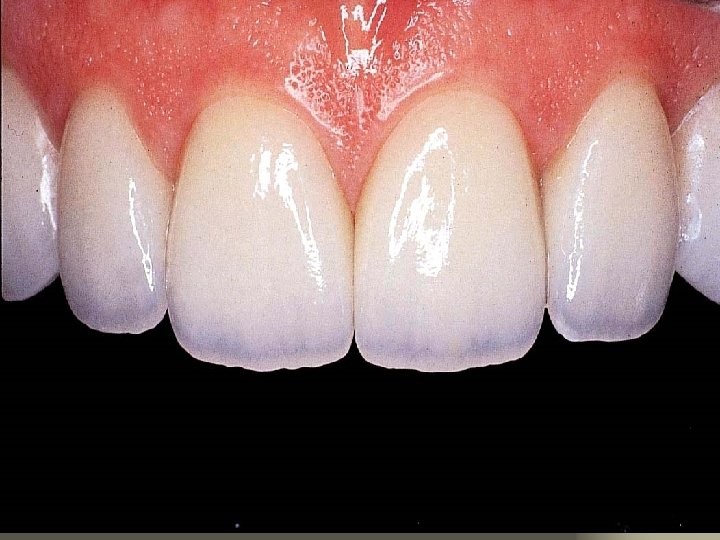
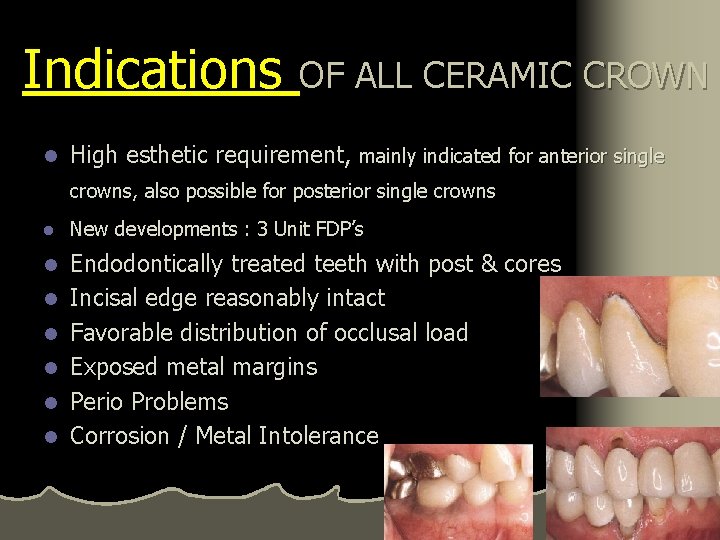
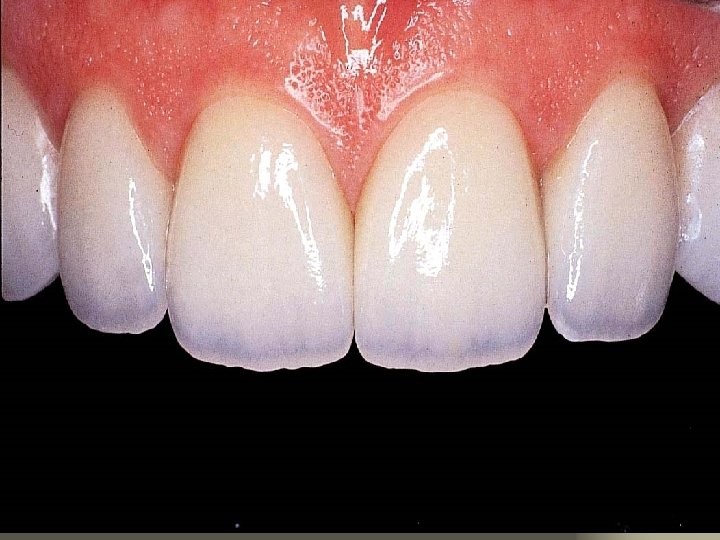
Indications OF ALL CERAMIC CROWN l High esthetic requirement, mainly indicated for anterior single crowns, also possible for posterior single crowns l New developments : 3 Unit FDP’s l Endodontically treated teeth with post & cores Incisal edge reasonably intact Favorable distribution of occlusal load Exposed metal margins Perio Problems Corrosion / Metal Intolerance l l l
Contraindications l When superior strength is warranted High caries index Insufficient coronal tooth structure for support Thin teeth faciolingually Parafunctional habits (Bruxism) Unfavorable distribution of occlusal load Inadequate Training/Understanding l Improper Connector/Pontic Space (FDP) l Bonding contraindicated if isolation cannot be achieved l l l
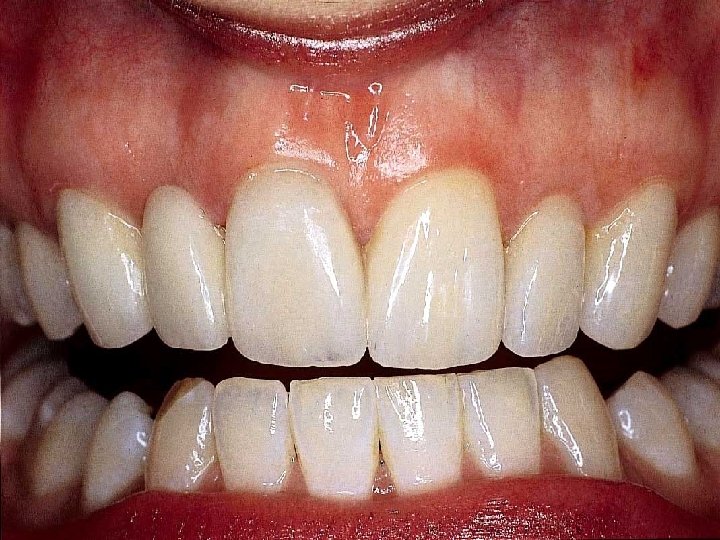
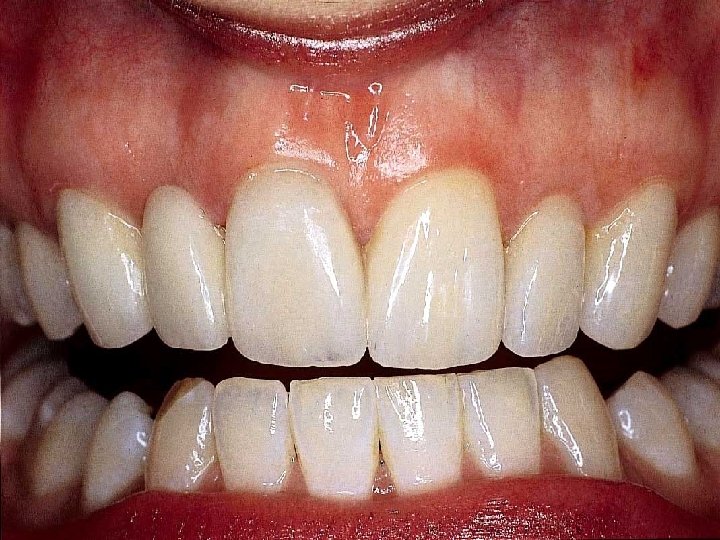
Advantages l Esthetically unsurpassed l Good tissue response even for subgingival margins (Biocompatable) l Slightly more conservative of facial wall than metal ceramic

Disadvantages l Reduced strength compared to metal ceramic crowns l Proper preparation extremely critical l Among least conservative preparations l Brittle nature of material l Poor marginal adaptation
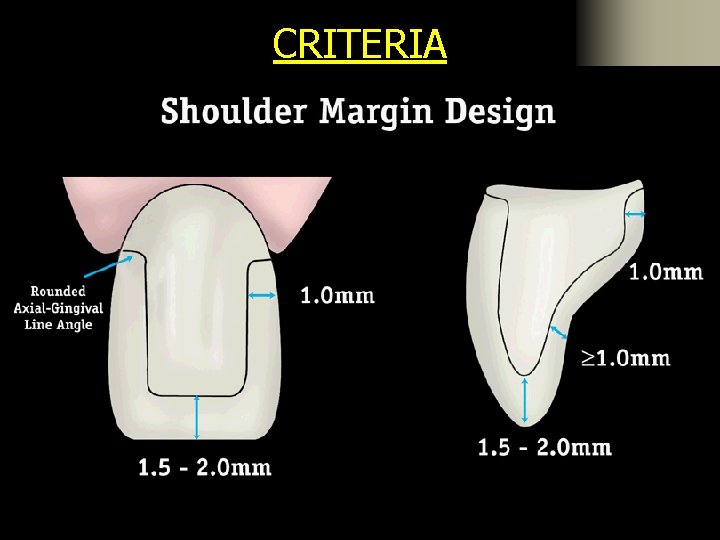
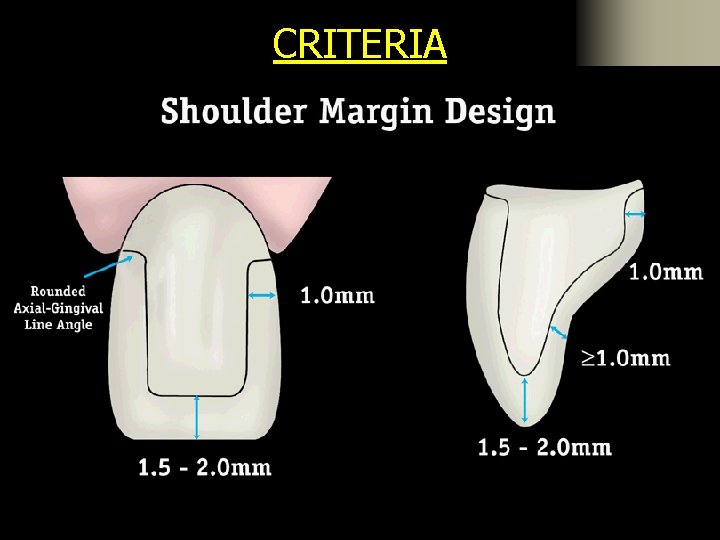
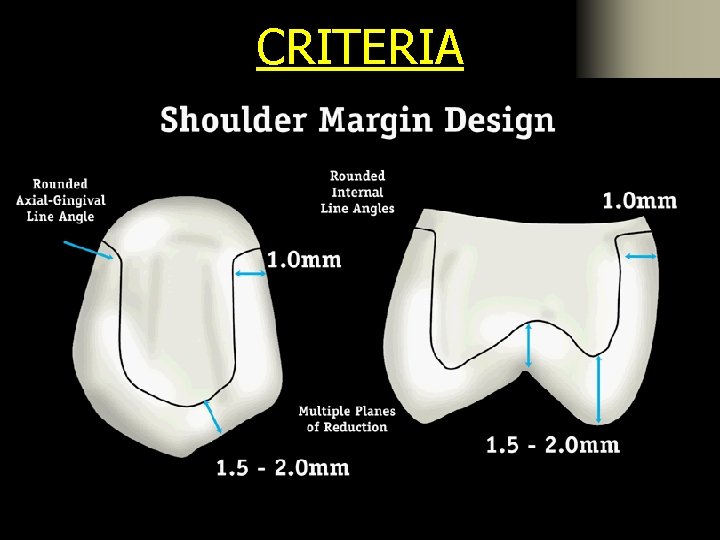
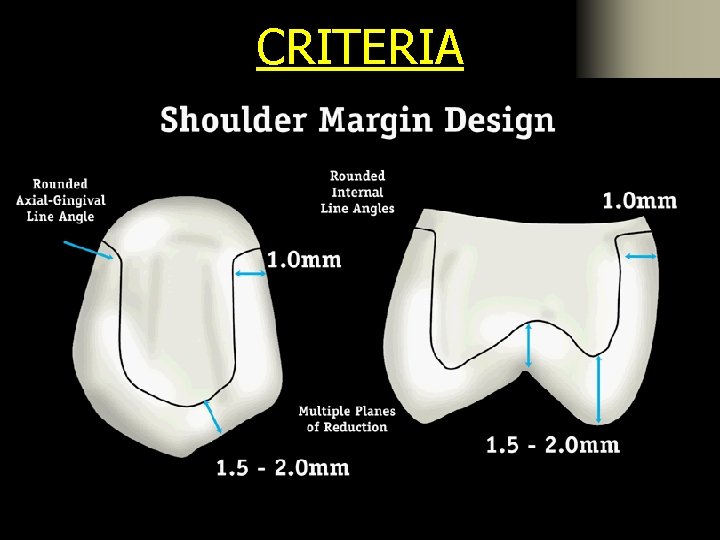
CRITERIA
CRITERIA
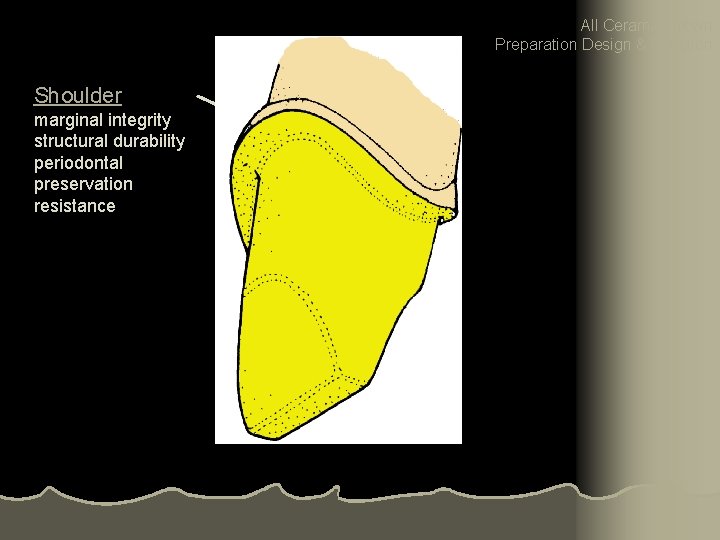
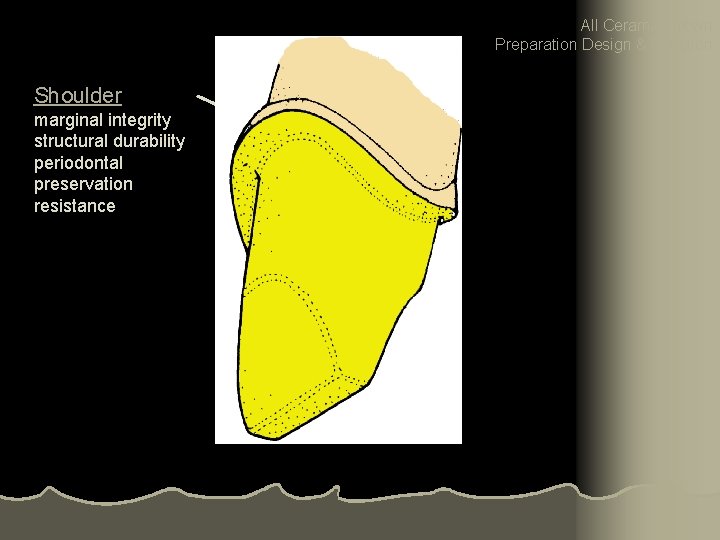
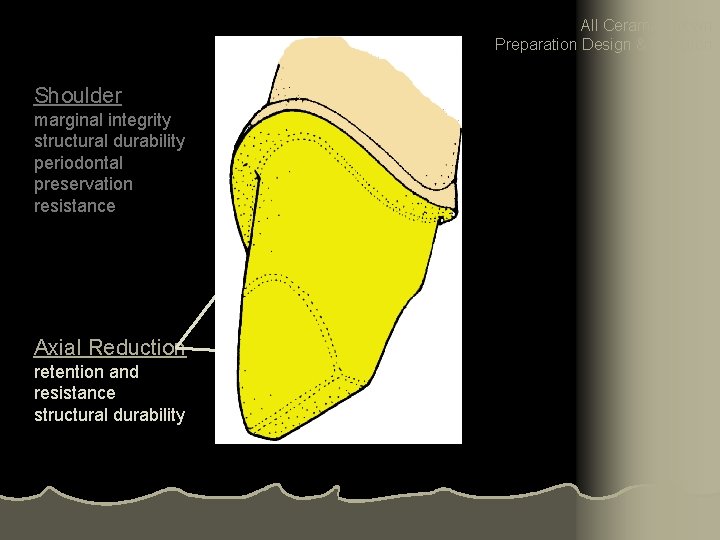
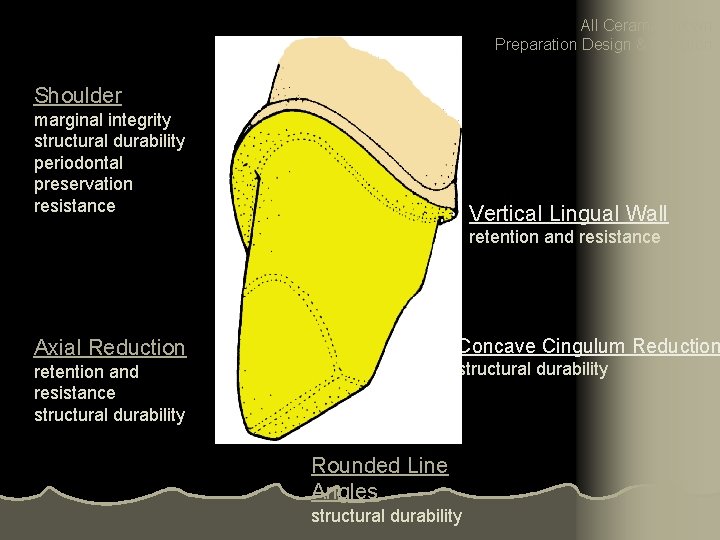
All Ceramic Crown Preparation Design & Function Shoulder marginal integrity structural durability periodontal preservation resistance
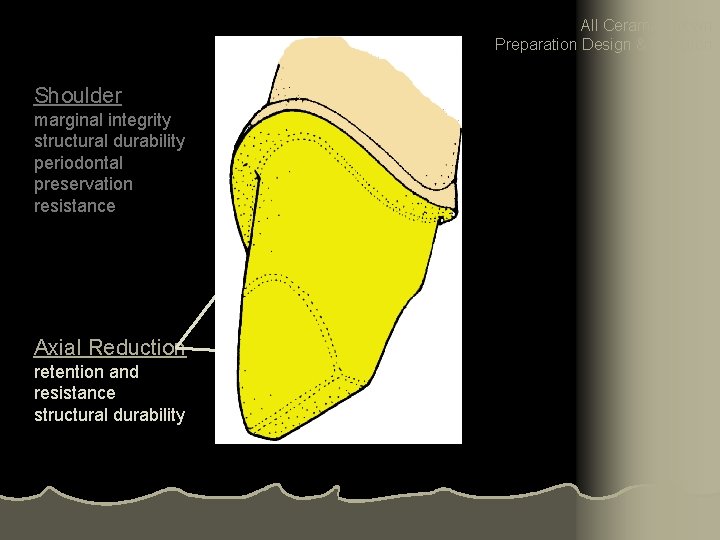
All Ceramic Crown Preparation Design & Function Shoulder marginal integrity structural durability periodontal preservation resistance Axial Reduction retention and resistance structural durability
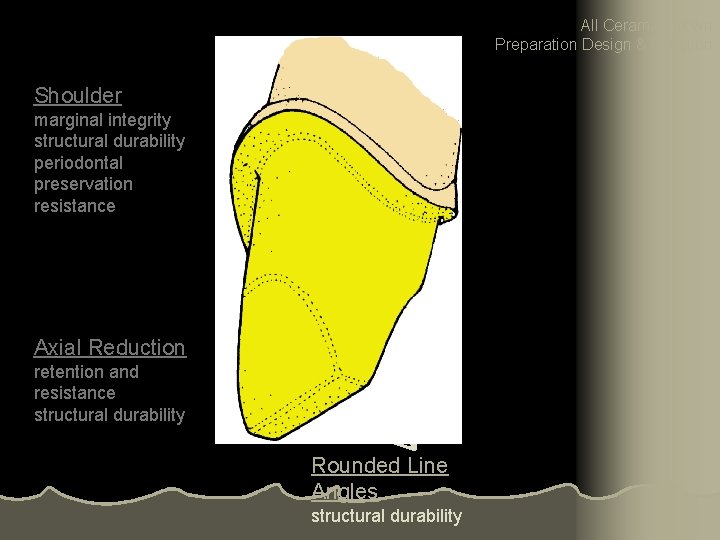
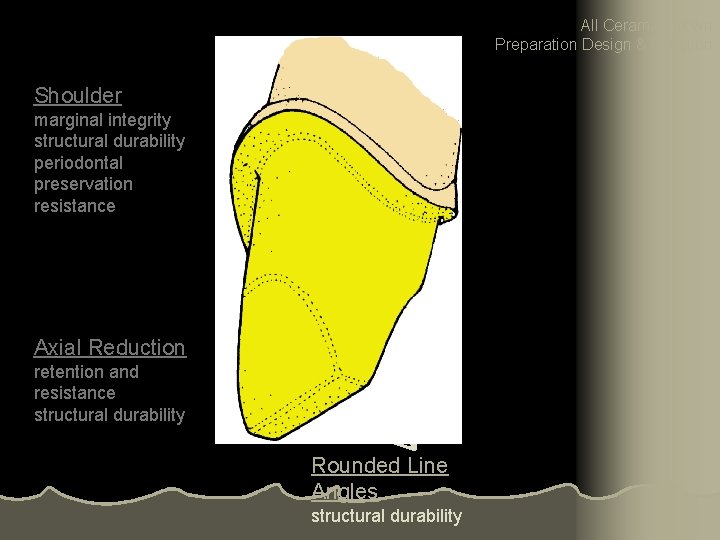
All Ceramic Crown Preparation Design & Function Shoulder marginal integrity structural durability periodontal preservation resistance Axial Reduction retention and resistance structural durability Rounded Line Angles structural durability
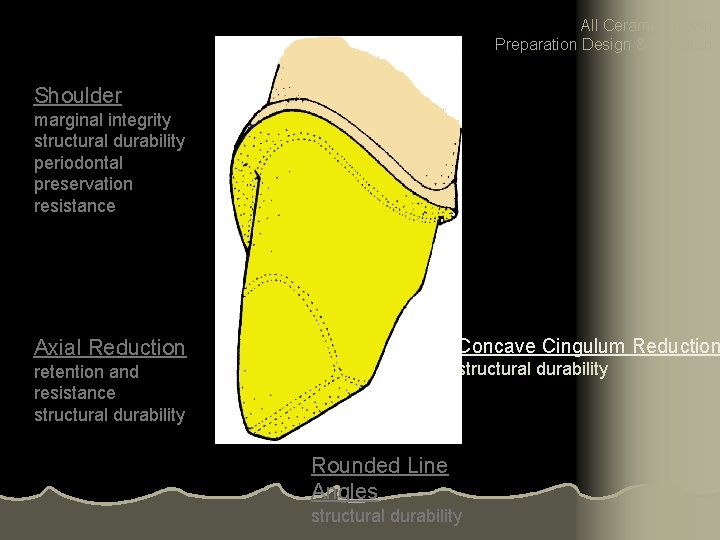
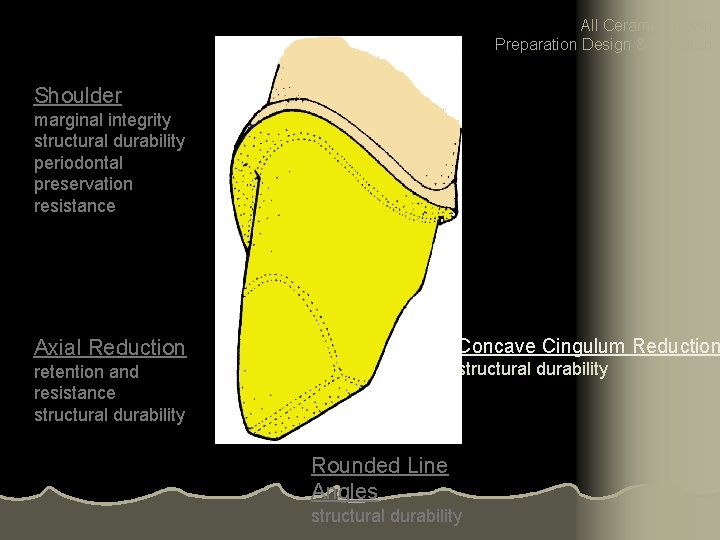
All Ceramic Crown Preparation Design & Function Shoulder marginal integrity structural durability periodontal preservation resistance Concave Cingulum Reduction Axial Reduction structural durability retention and resistance structural durability Rounded Line Angles structural durability
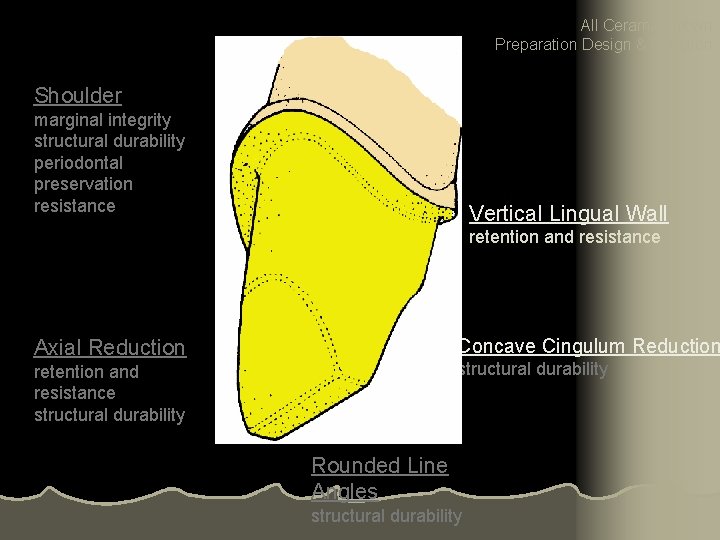
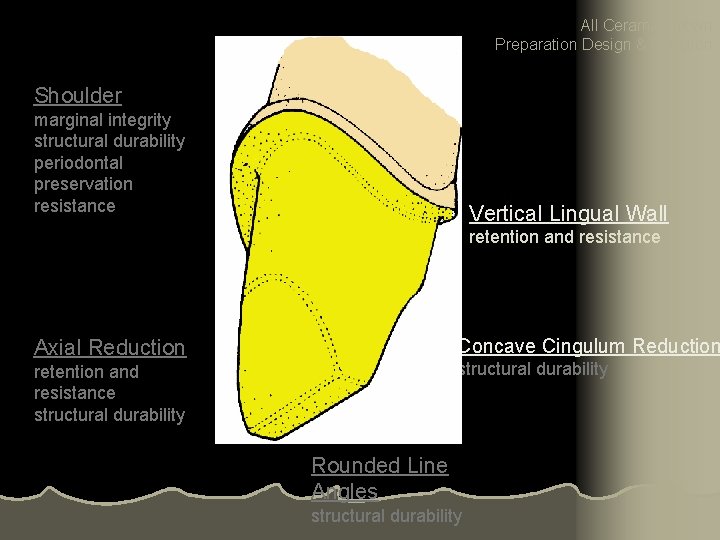
All Ceramic Crown Preparation Design & Function Shoulder marginal integrity structural durability periodontal preservation resistance Vertical Lingual Wall retention and resistance Concave Cingulum Reduction Axial Reduction structural durability retention and resistance structural durability Rounded Line Angles structural durability
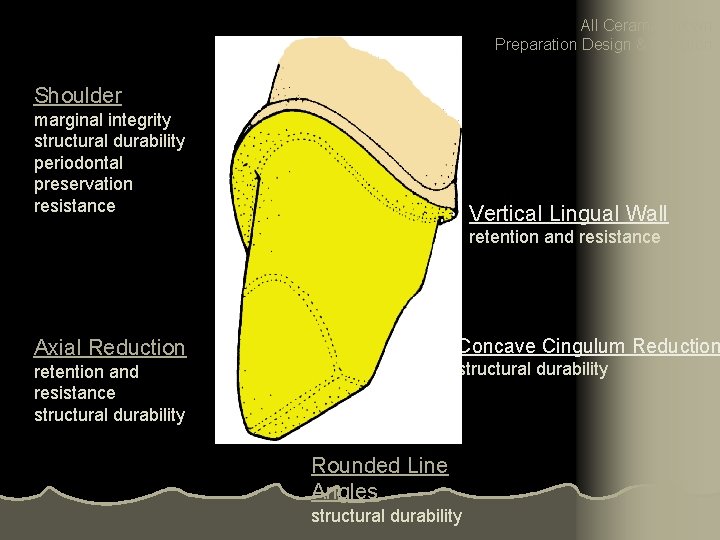
All Ceramic Crown Preparation Design & Function Shoulder marginal integrity structural durability periodontal preservation resistance Vertical Lingual Wall retention and resistance Concave Cingulum Reduction Axial Reduction structural durability retention and resistance structural durability Rounded Line Angles structural durability
PREPARATION STEPS l Incisal (Occlusal) Reduction l Facial Reduction l Lingual Reduction l Finishing

Depth-orientation grooves






Incisal reduction
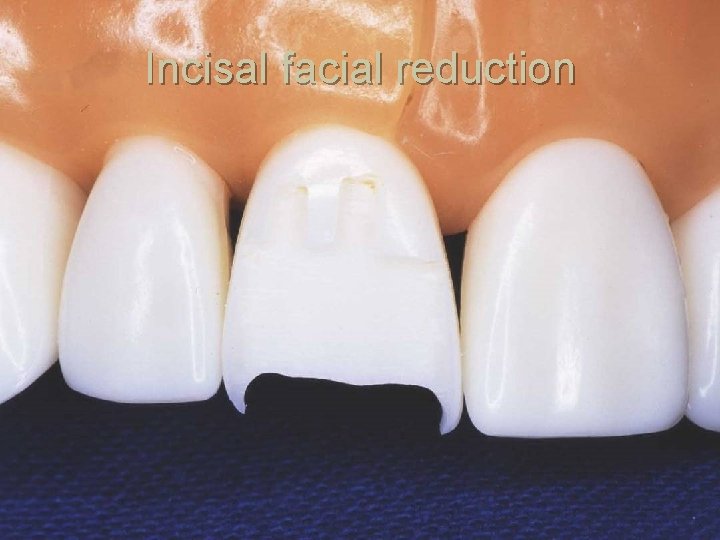
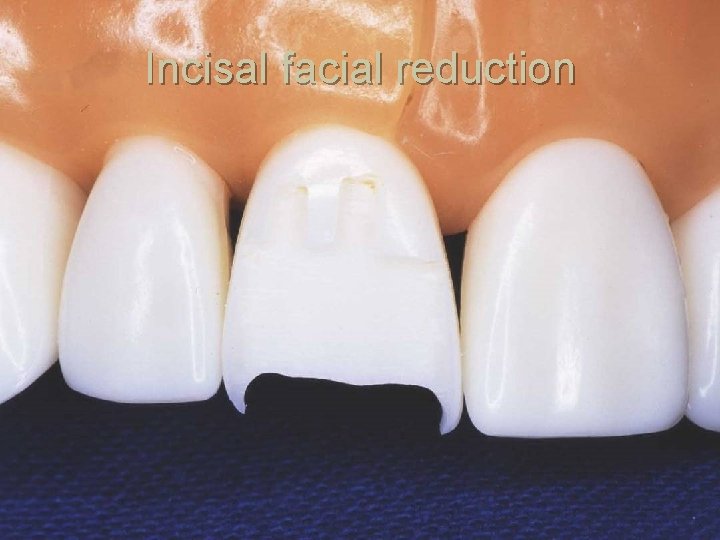
Incisal facial reduction
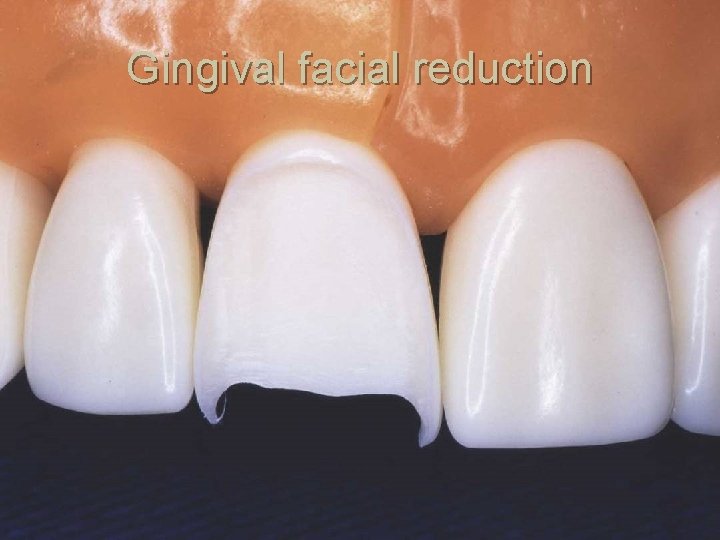
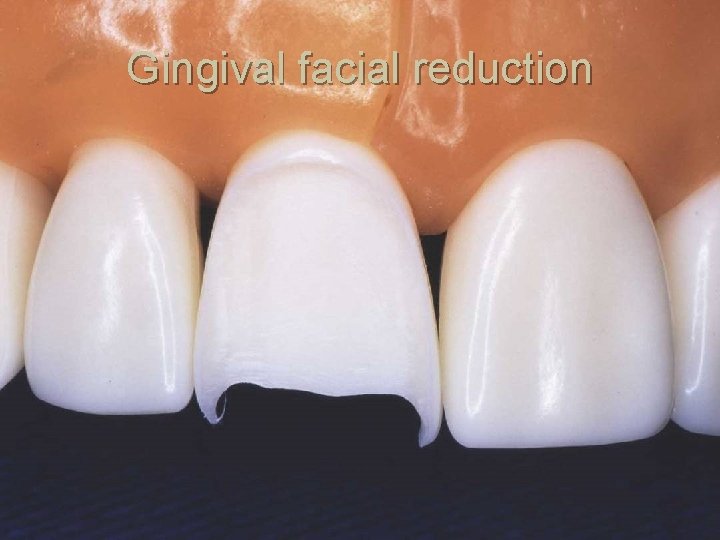
Gingival facial reduction
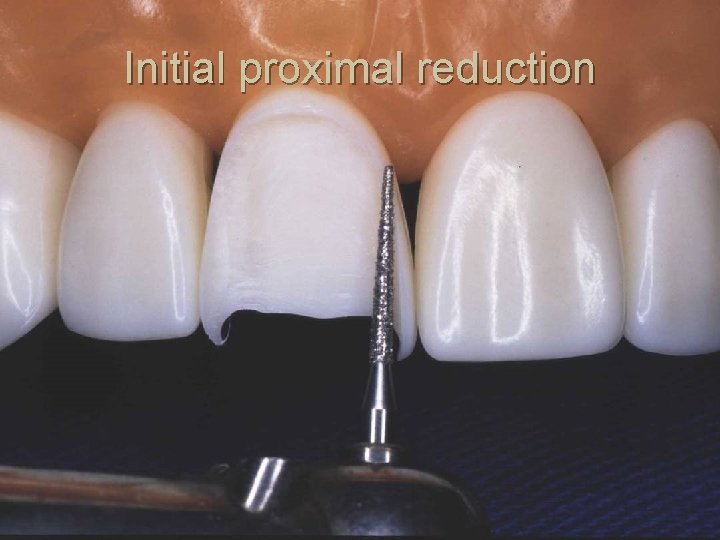
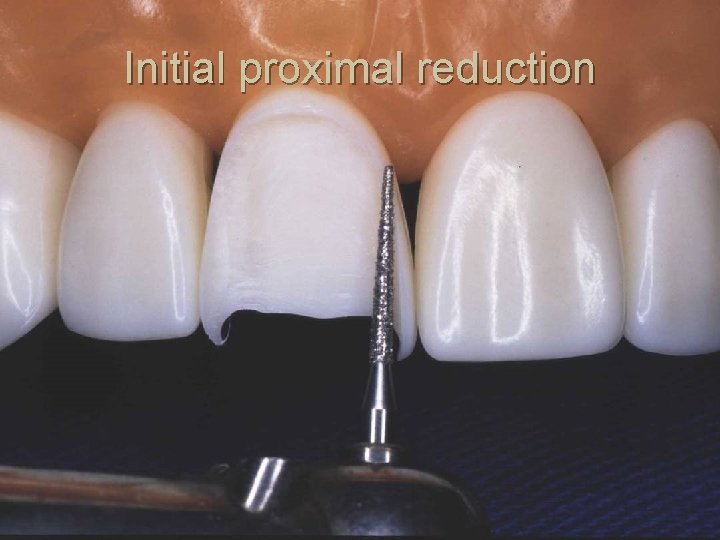
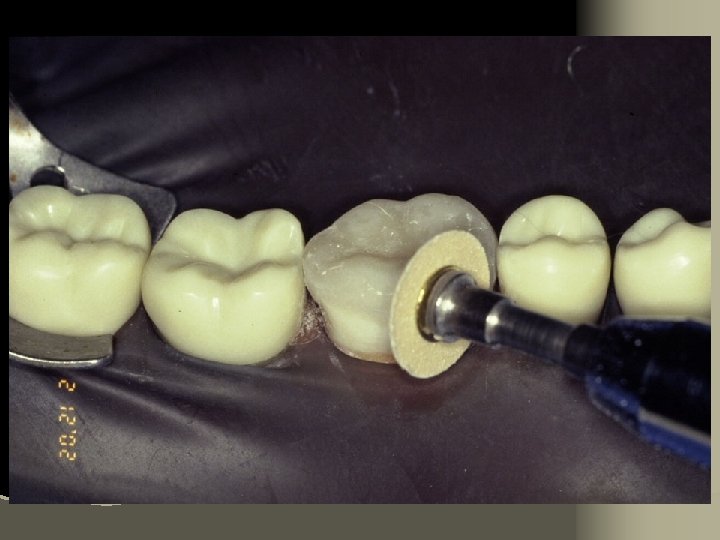
Initial proximal reduction




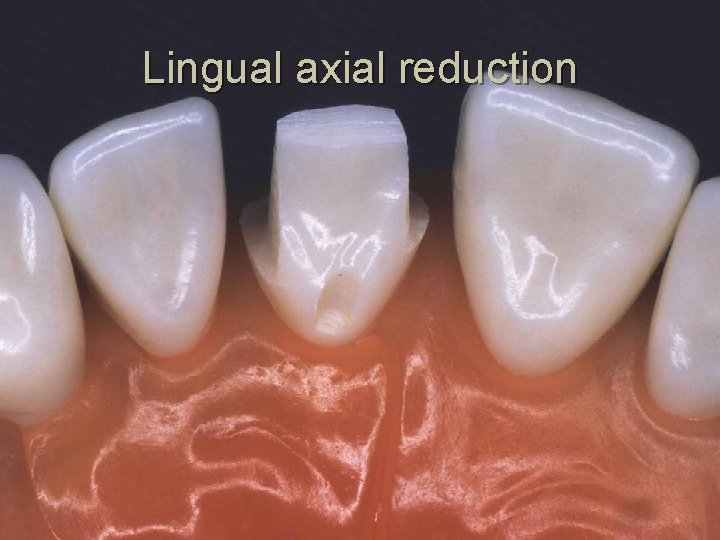
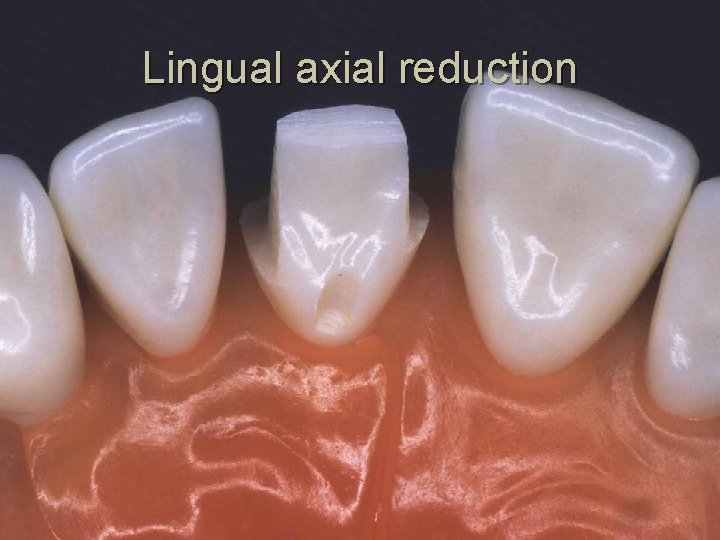
Lingual axial reduction






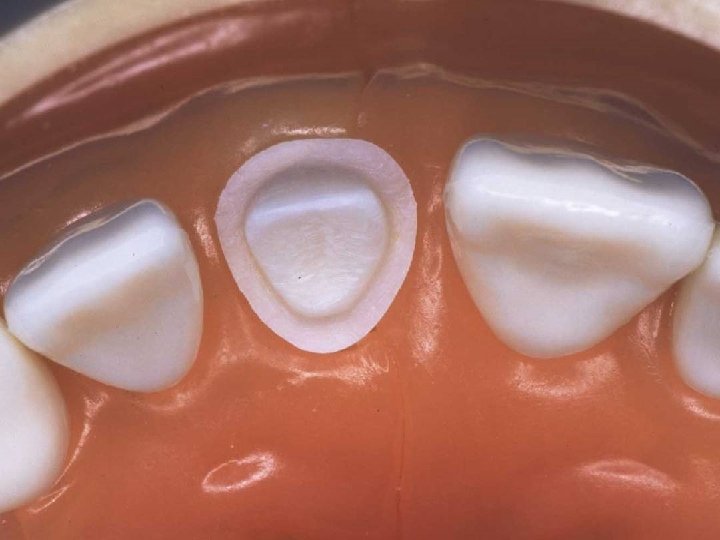
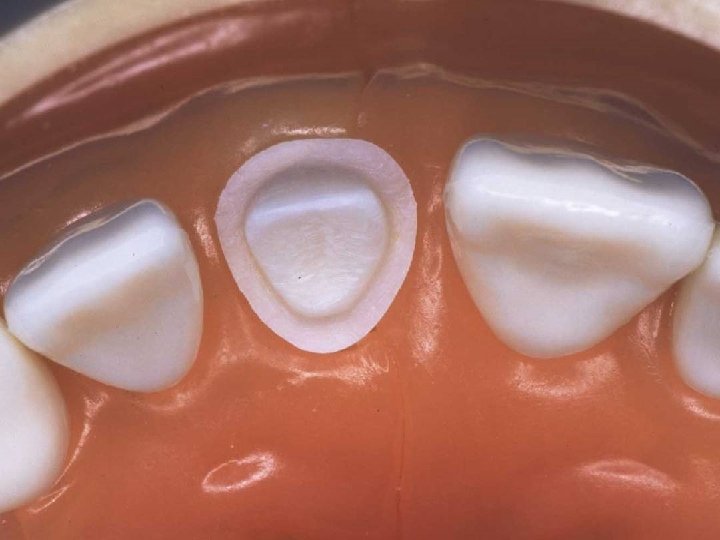
Axial wall and shoulder finishing

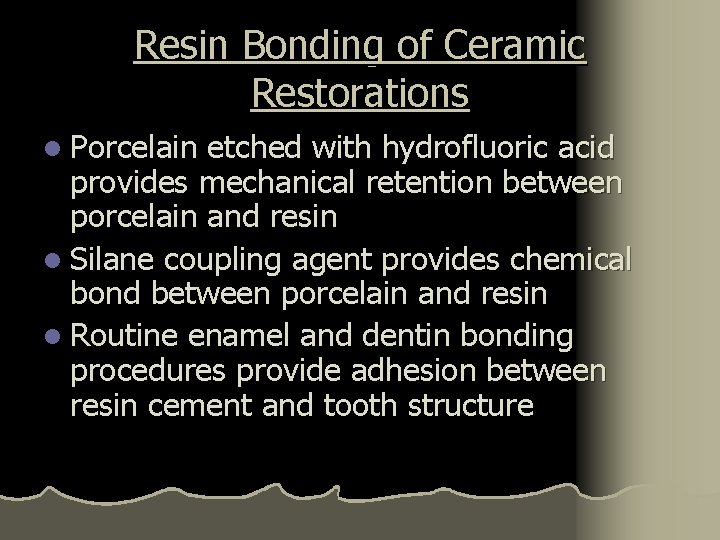
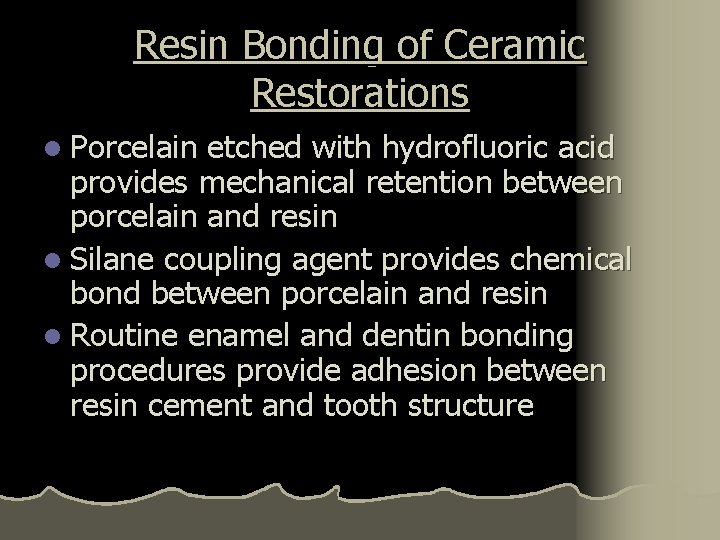
Resin Bonding of Ceramic Restorations l Porcelain etched with hydrofluoric acid provides mechanical retention between porcelain and resin l Silane coupling agent provides chemical bond between porcelain and resin l Routine enamel and dentin bonding procedures provide adhesion between resin cement and tooth structure
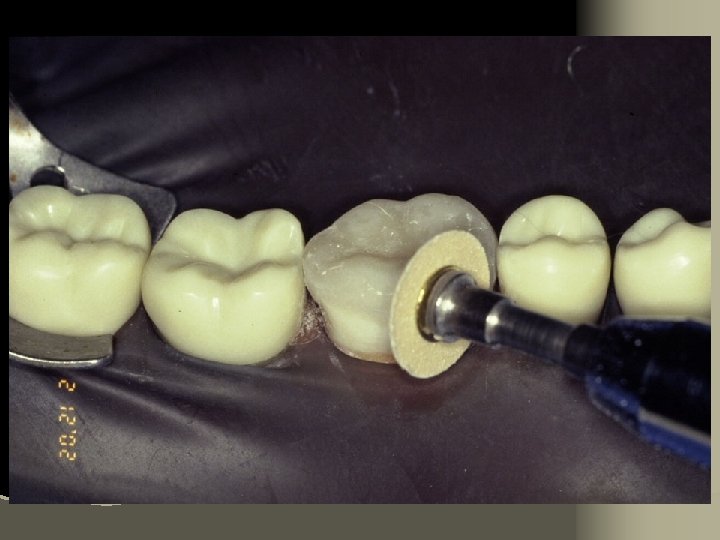
HF etch Intaglio surfaces only
Cementation Procedure 1. Remove temporary and all residue of temporary cement 2. Check occlusion on adjacent teeth (mylar shimstock and articulating paper) 3. Place rubber dam 4. Clean tooth with pumice and rubber cup, rinse and lightly dry 5. Try in restoration for fit.
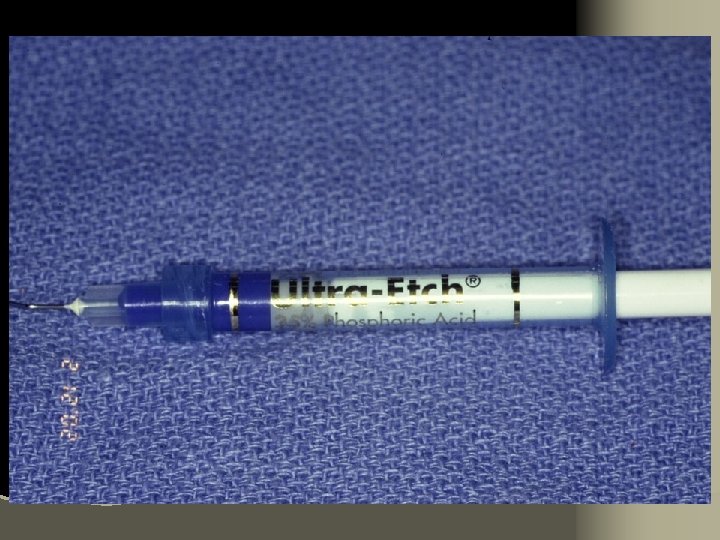
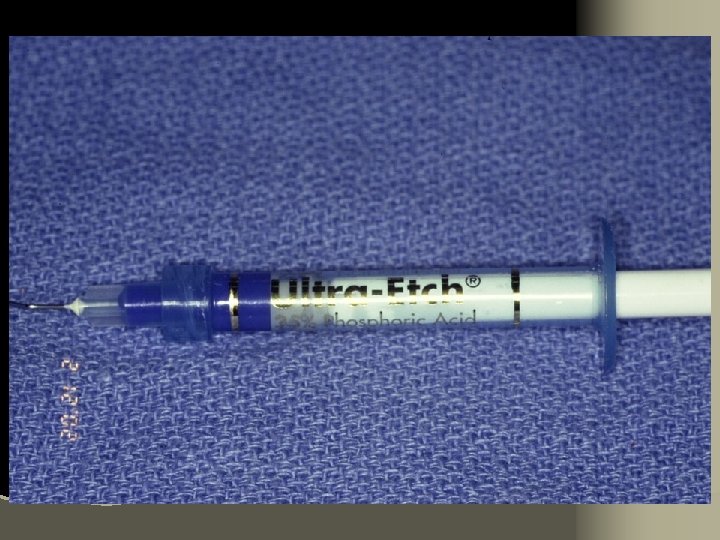
6. Adjust proximal contacts if necessary 7. Evaluate shade intraorally using water soluble try-in paste (optional) 8. Rinse out try-in paste and air dry 9. Etch inside of restoration (HF porcelain etchant X 2 minutes), rinse with distilled water and air dry 10. Place drop of silane (porcelain primer) on intaglio surface for 1 minute, lightly air thin to evaporate solvent
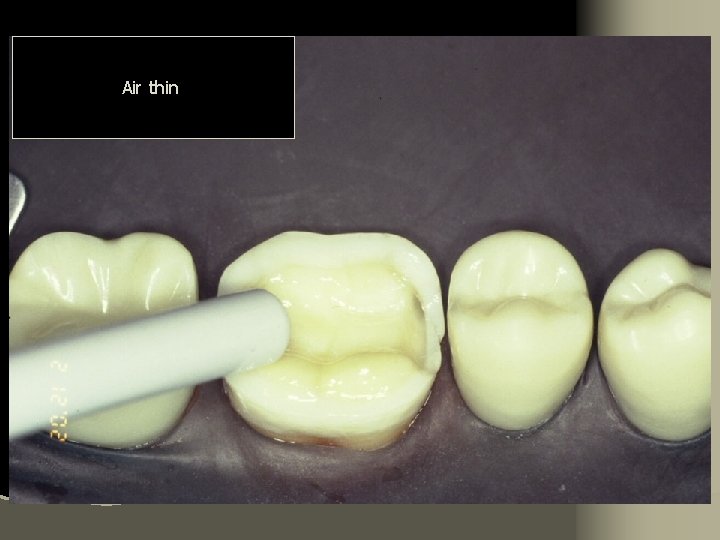
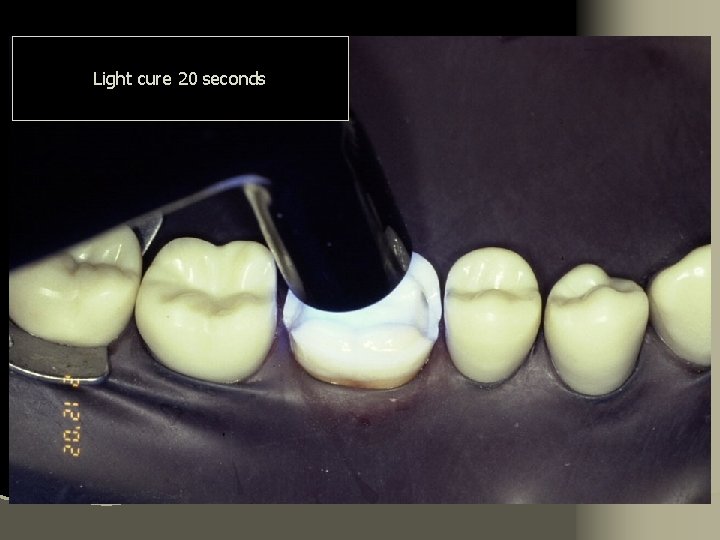
11. Place matrix to protect adjacent teeth from etchant 12. Etch prepared tooth surfaces (phosphoric acid). Rinse and lightly air dry 13. Apply prime/bond for 15 seconds 14. Air thin for 3 seconds – AVOID POOLING 15. Light cure for 20 seconds per surface
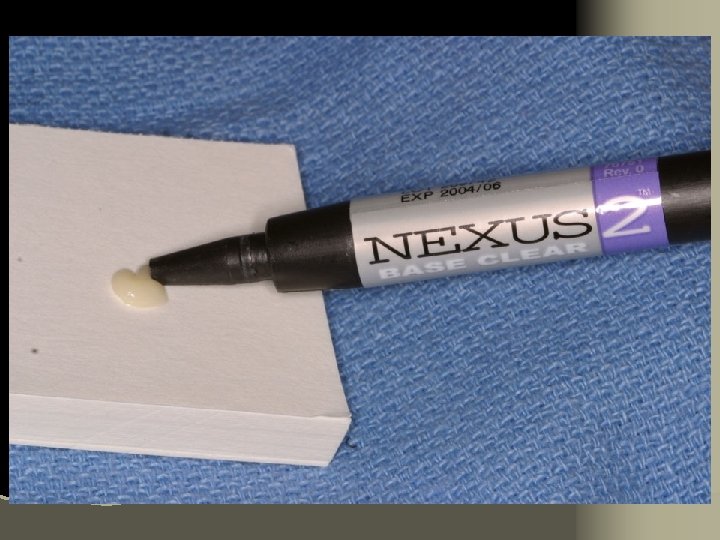
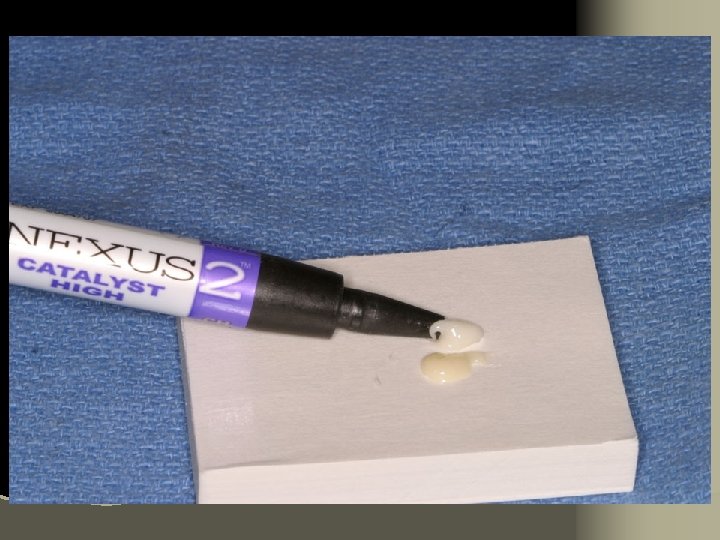
16. Mix dual cure base and catalyst with plastic spatula (for thick restorations). Place resin cement into middle of restoration – avoid air entrapment 17. Gently seat restoration 18. Remove gross excess cement with brush, explorer and/or floss leaving slight excess at margins– AVOID ANY MOVEMENT OF THE RESTORATION 19. Light cure all surfaces for a minimum of 60 seconds per surface
20. Remove remaining cement with scalpel, gold knife or chisels 21. Evaluate contours at margins 22. Polish margins 23. Remove dam, Adjust occlusion and final polish
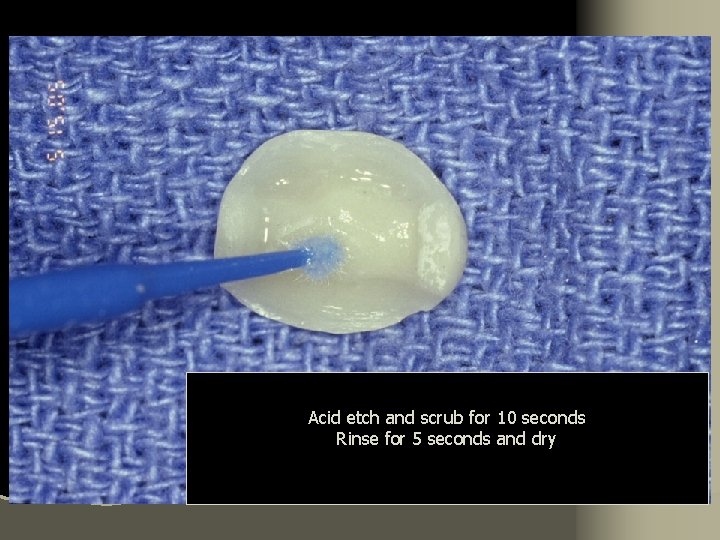
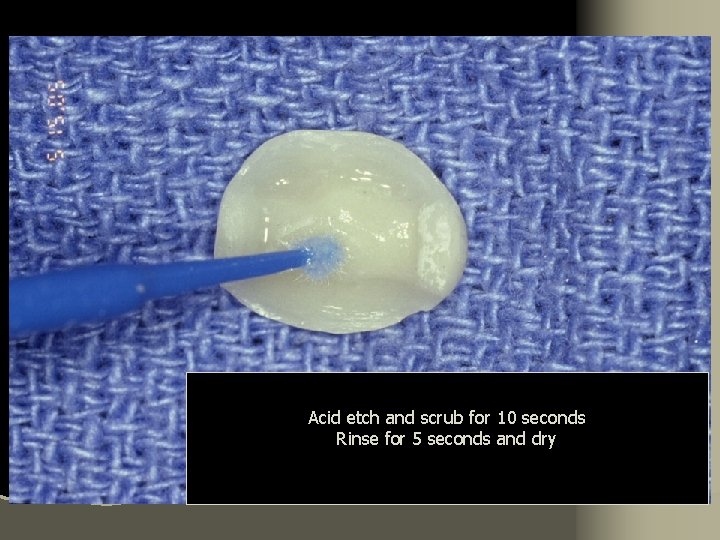
Acid etch and scrub for 10 seconds Rinse for 5 seconds and dry

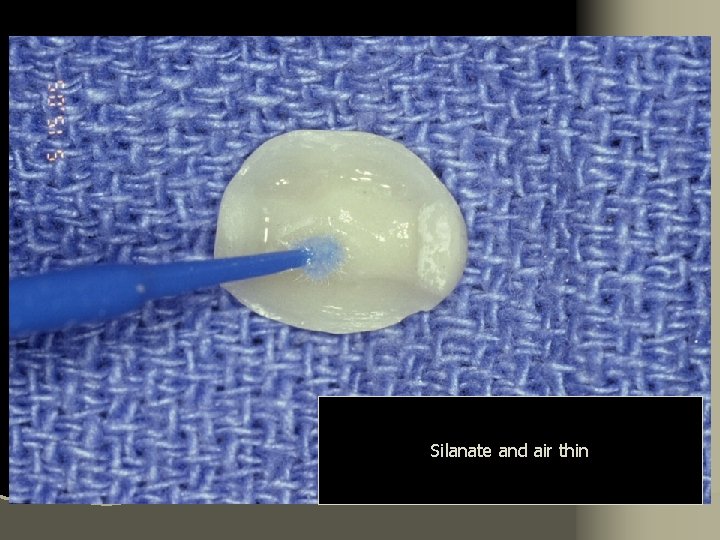
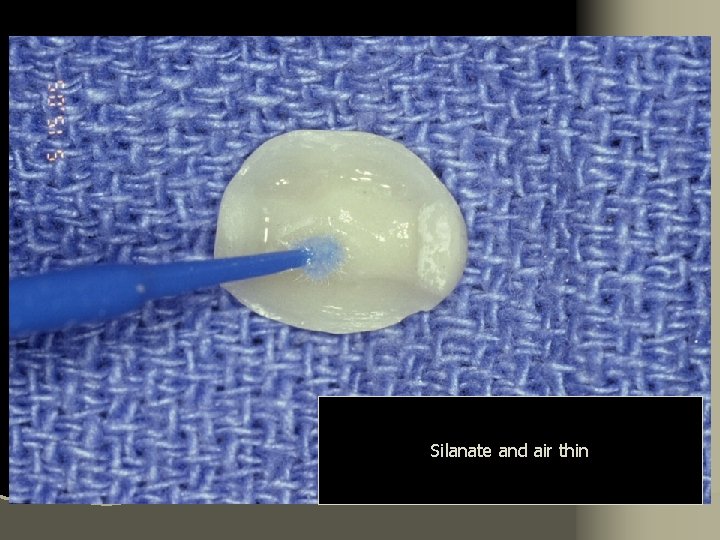
Silanate and air thin
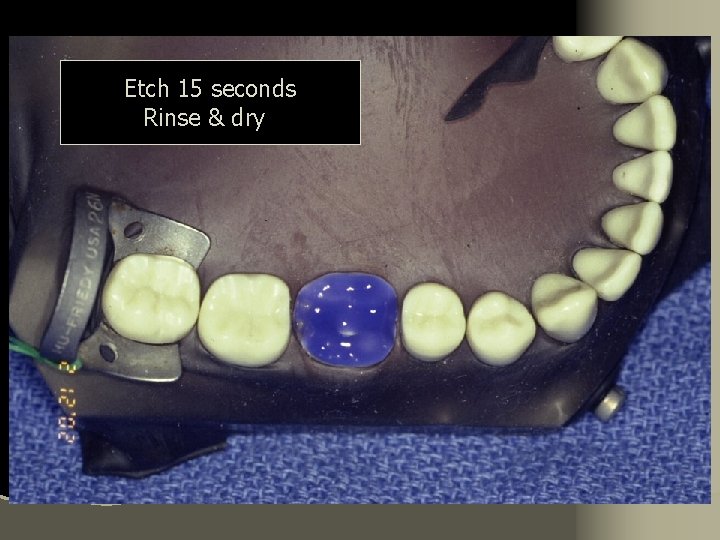
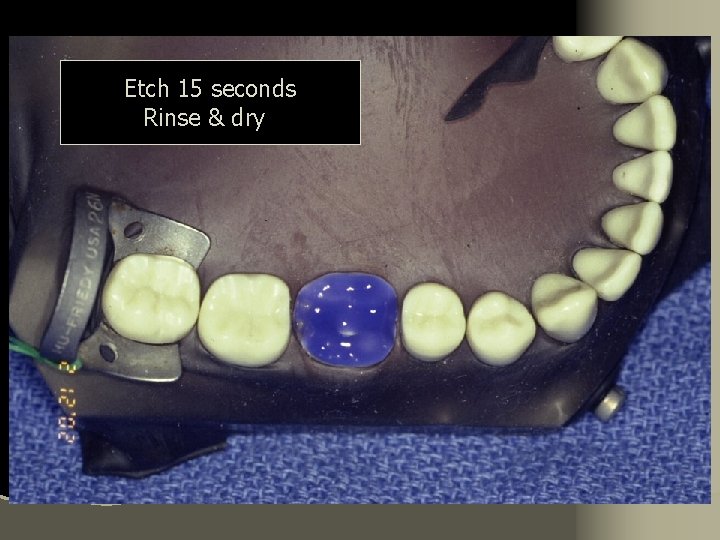
Etch 15 seconds Rinse & dry




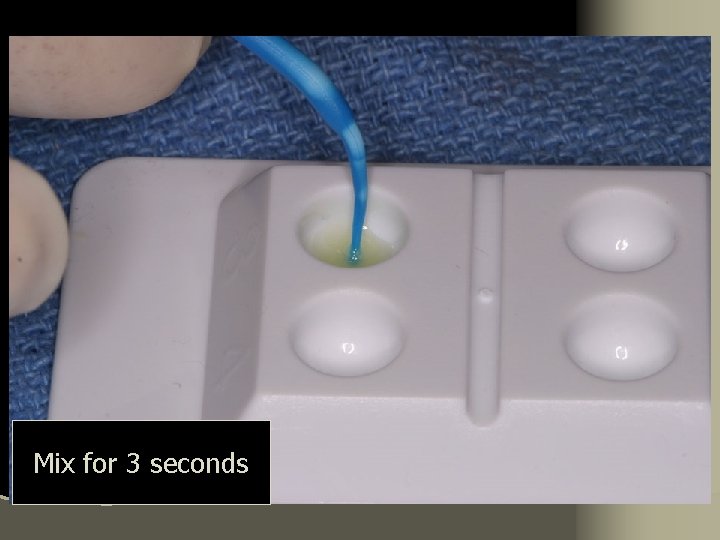
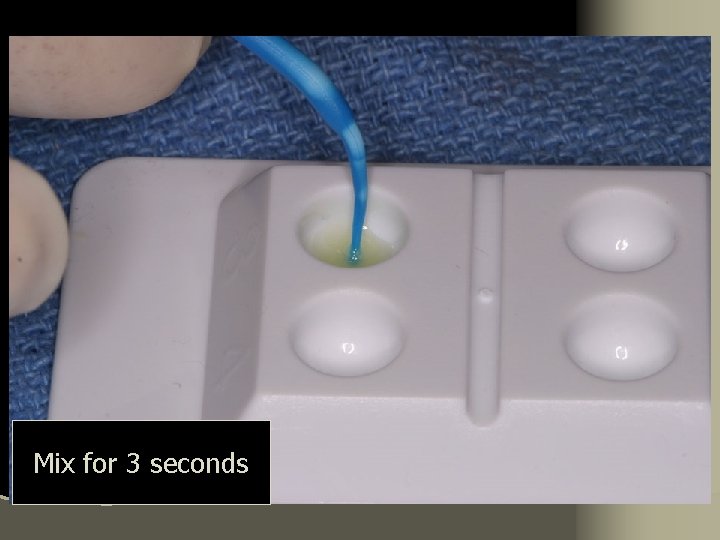
Mix for 3 seconds
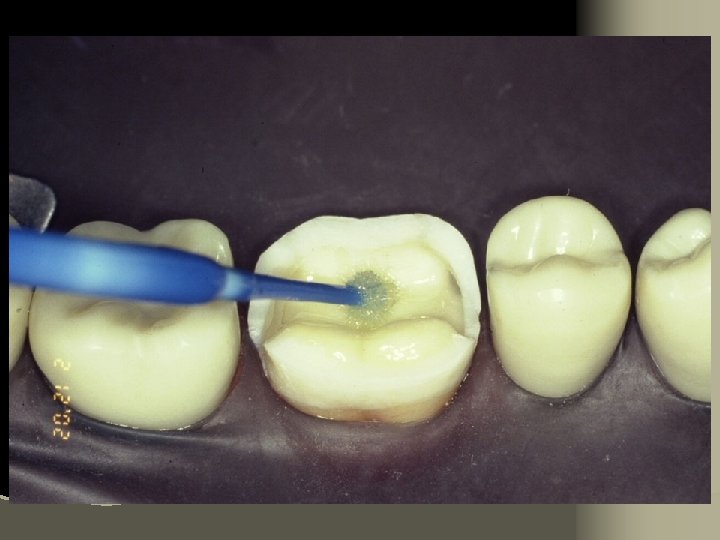
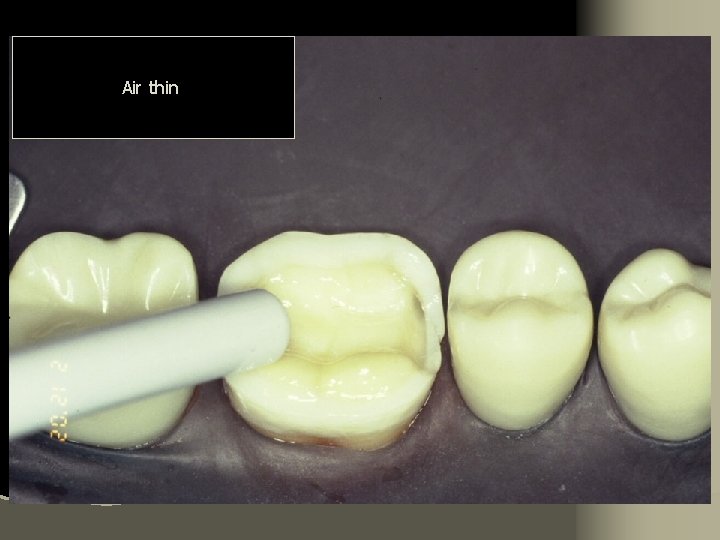
Air thin
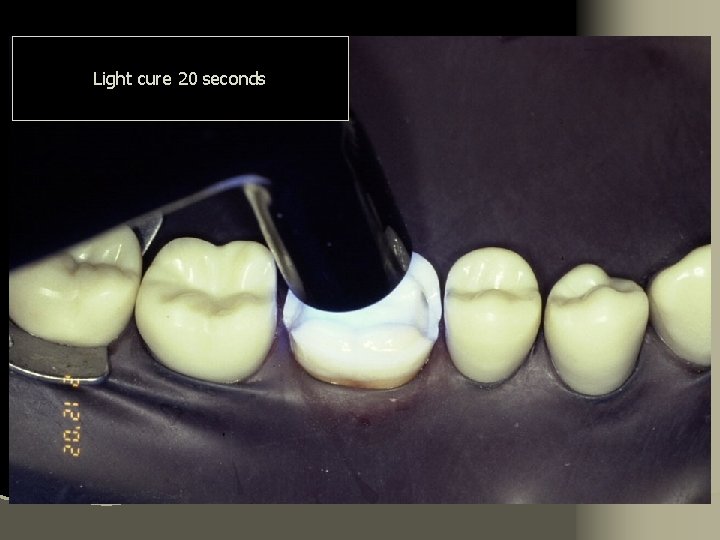
Light cure 20 seconds

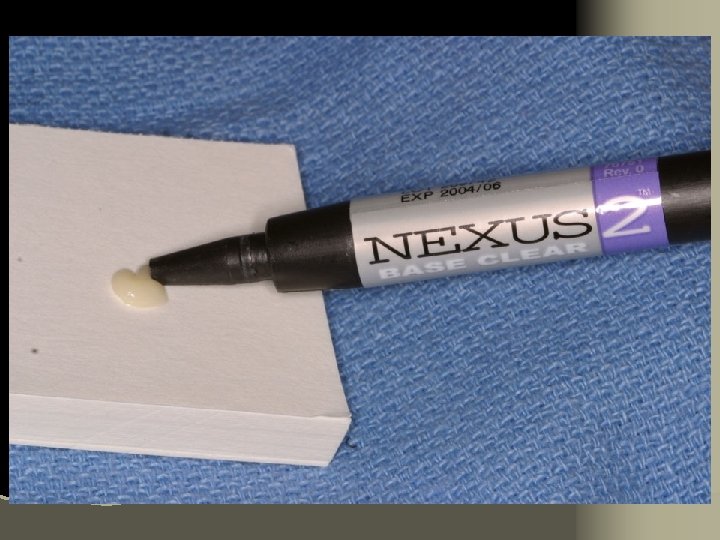
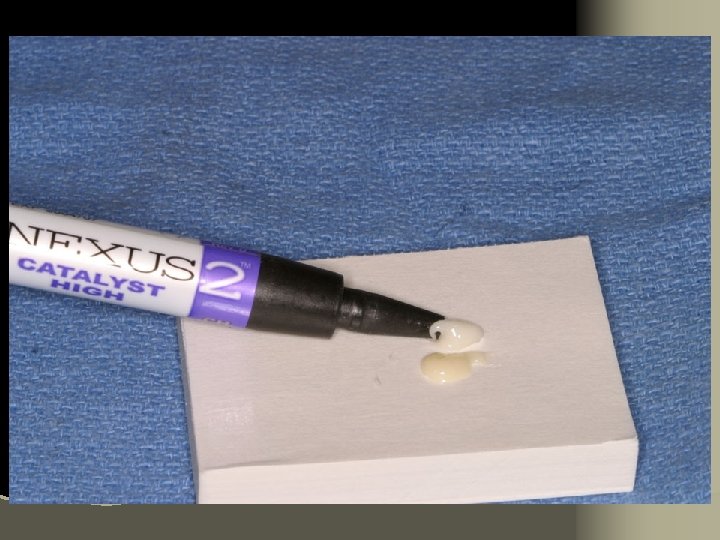
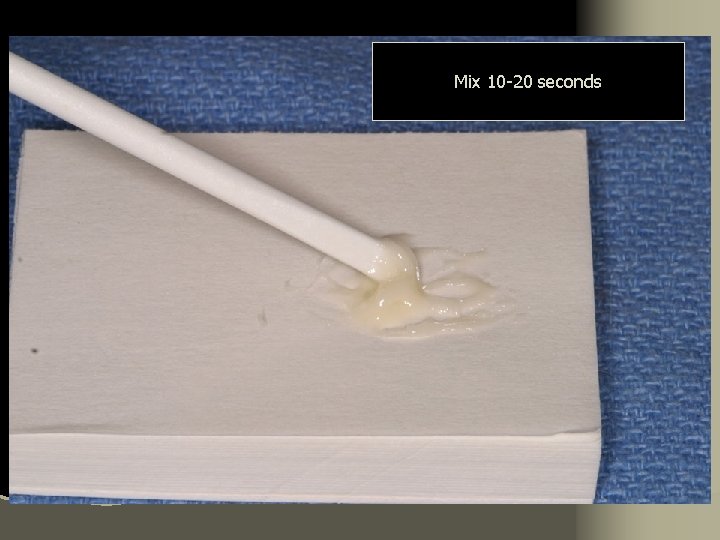
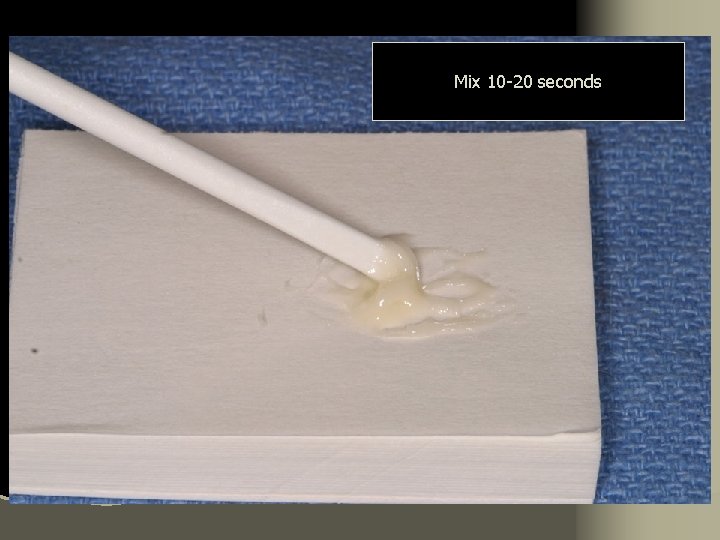
Mix 10 -20 seconds



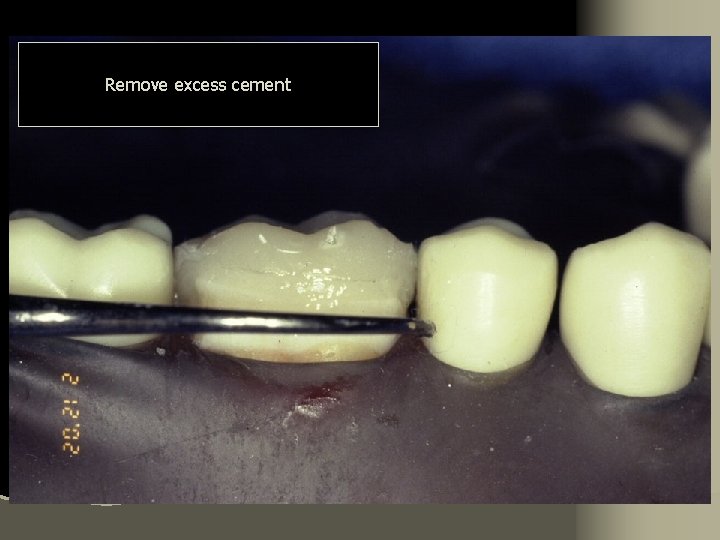
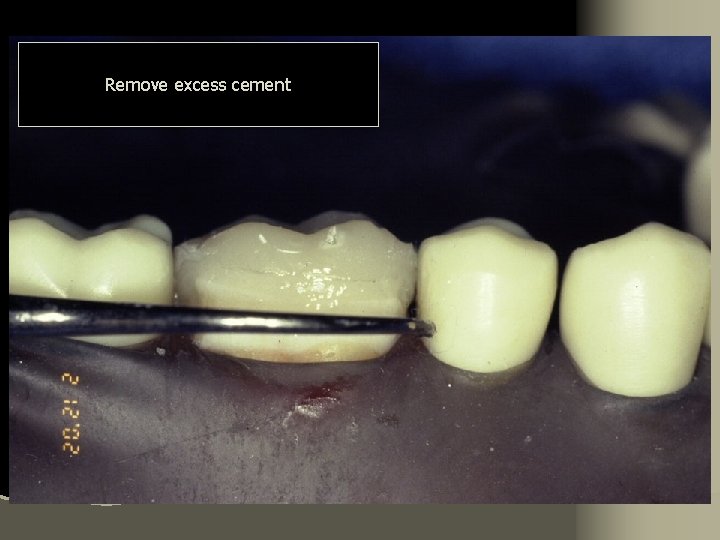
Remove excess cement

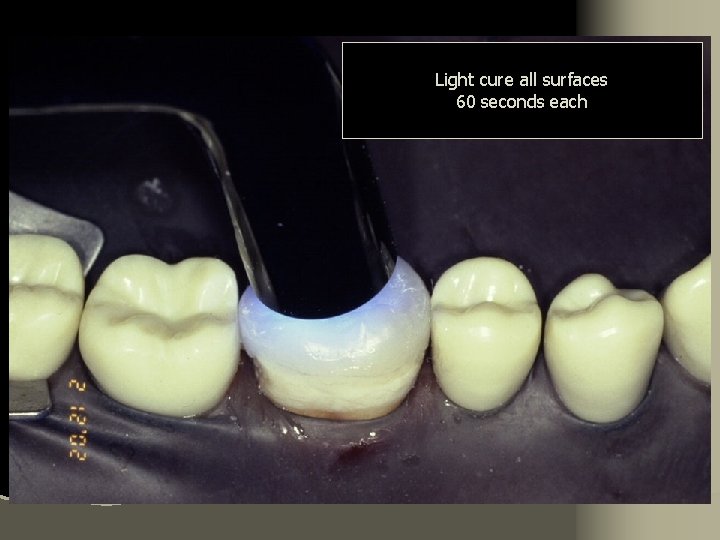
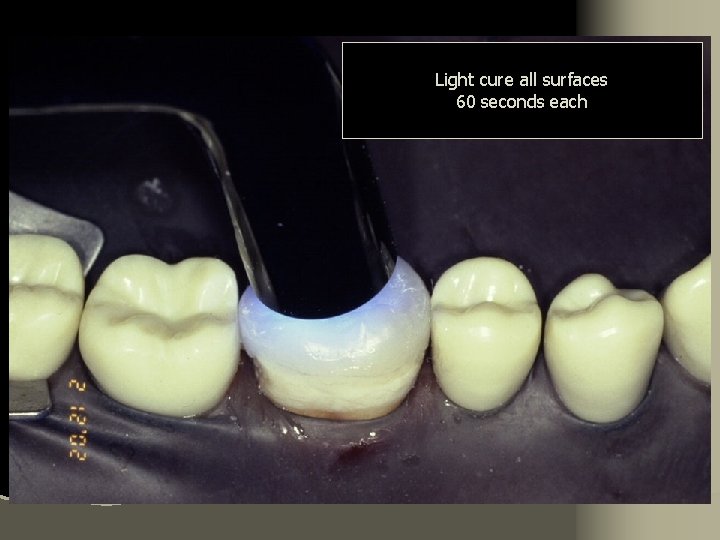
Light cure all surfaces 60 seconds each
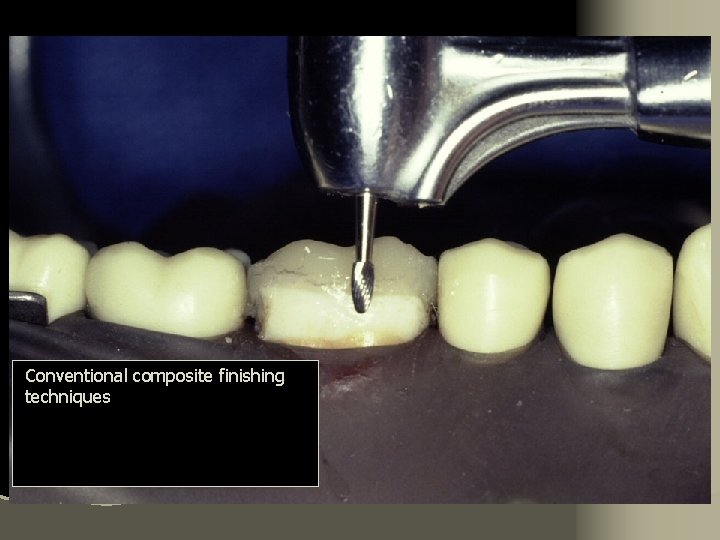
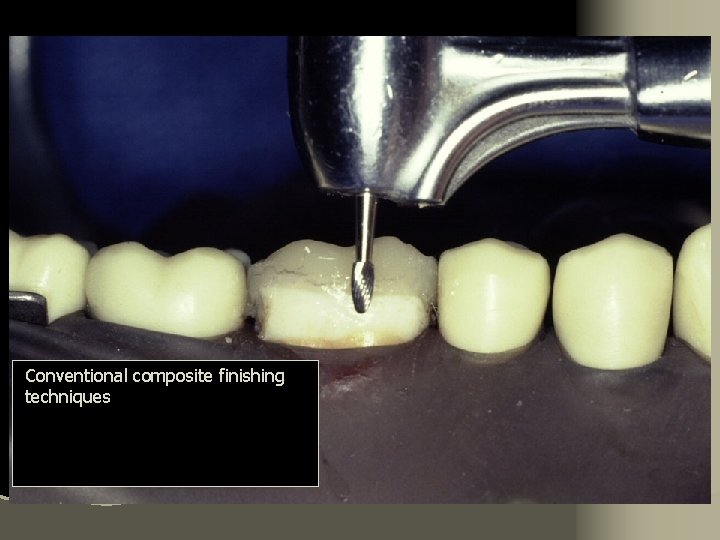
Conventional composite finishing techniques