Algorithm For the Management of Increased ICP Maintenance
- Slides: 1
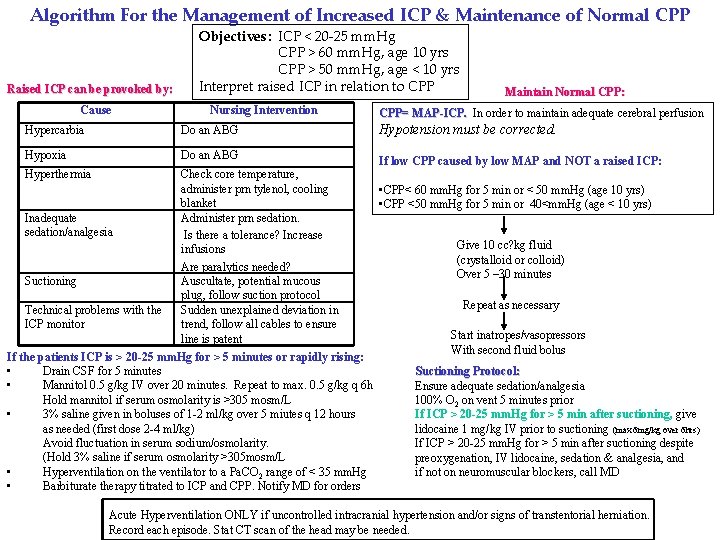
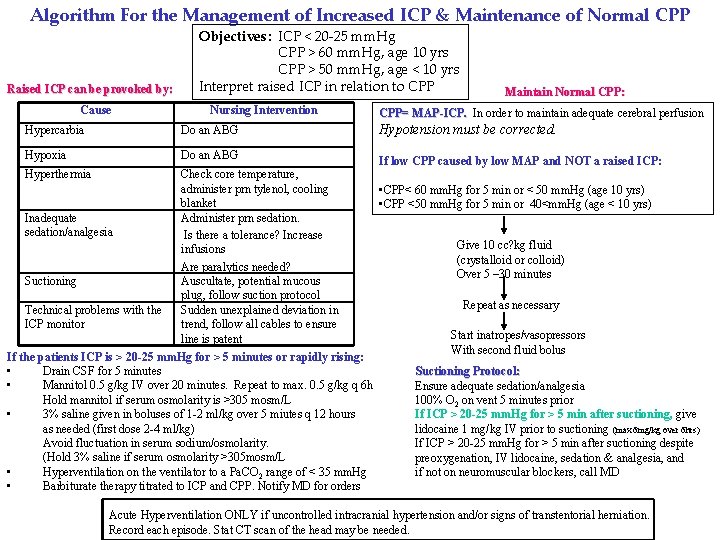
Algorithm For the Management of Increased ICP & Maintenance of Normal CPP Raised ICP can be provoked by: Cause Objectives: ICP < 20 -25 mm. Hg CPP > 60 mm. Hg, age 10 yrs CPP > 50 mm. Hg, age < 10 yrs Interpret raised ICP in relation to CPP Nursing Intervention Hypercarbia Do an ABG Hypoxia Do an ABG Hyperthermia Check core temperature, administer prn tylenol, cooling blanket Administer prn sedation. Is there a tolerance? Increase infusions Are paralytics needed? Auscultate, potential mucous plug, follow suction protocol Sudden unexplained deviation in trend, follow all cables to ensure line is patent Inadequate sedation/analgesia Suctioning Technical problems with the ICP monitor If the patients ICP is > 20 -25 mm. Hg for > 5 minutes or rapidly rising: • Drain CSF for 5 minutes • Mannitol 0. 5 g/kg IV over 20 minutes. Repeat to max. 0. 5 g/kg q 6 h Hold mannitol if serum osmolarity is >305 mosm/L • 3% saline given in boluses of 1 -2 ml/kg over 5 miutes q 12 hours as needed (first dose 2 -4 ml/kg) Avoid fluctuation in serum sodium/osmolarity. (Hold 3% saline if serum osmolarity >305 mosm/L • Hyperventilation on the ventilator to a Pa. CO 2 range of < 35 mm. Hg • Barbiturate therapy titrated to ICP and CPP. Notify MD for orders Maintain Normal CPP: CPP= MAP-ICP. In order to maintain adequate cerebral perfusion Hypotension must be corrected. If low CPP caused by low MAP and NOT a raised ICP: • CPP< 60 mm. Hg for 5 min or < 50 mm. Hg (age 10 yrs) • CPP <50 mm. Hg for 5 min or 40<mm. Hg (age < 10 yrs) Give 10 cc? kg fluid (crystalloid or colloid) Over 5 – 30 minutes Repeat as necessary Start inatropes/vasopressors With second fluid bolus Suctioning Protocol: Ensure adequate sedation/analgesia 100% O 2 on vent 5 minutes prior If ICP > 20 -25 mm. Hg for > 5 min after suctioning, give lidocaine 1 mg/kg IV prior to suctioning (max 6 mg/kg over 6 hrs) If ICP > 20 -25 mm. Hg for > 5 min after suctioning despite preoxygenation, IV lidocaine, sedation & analgesia, and if not on neuromuscular blockers, call MD Acute Hyperventilation ONLY if uncontrolled intracranial hypertension and/or signs of transtentorial herniation. Record each episode. Stat CT scan of the head may be needed.