Alcohol Withdrawal Syndromes AMU Nurse Study Day Tom

- Slides: 26
Alcohol Withdrawal Syndromes AMU Nurse Study Day Tom Heaps Consultant Acute Physician
Lesson Plan Alcohol Withdrawal Syndromes § Introduction and Pathophysiology § Clinical Cases § Complications § Management § HEFT Clinical Guidelines for Alcohol Withdrawal § Summary
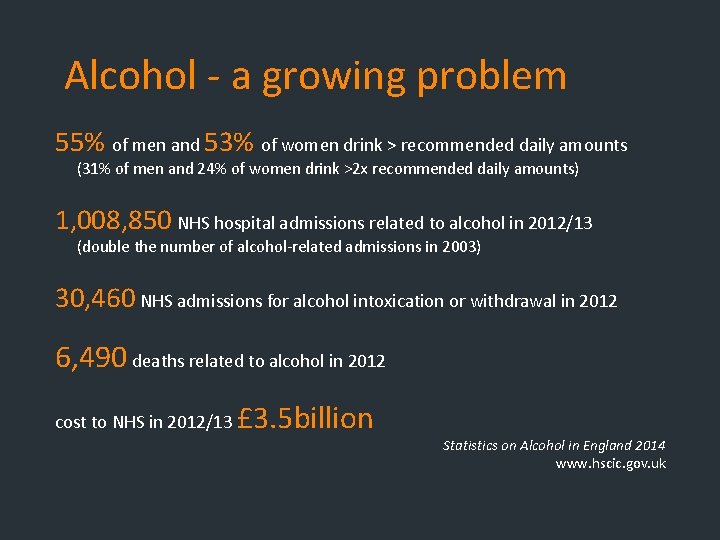
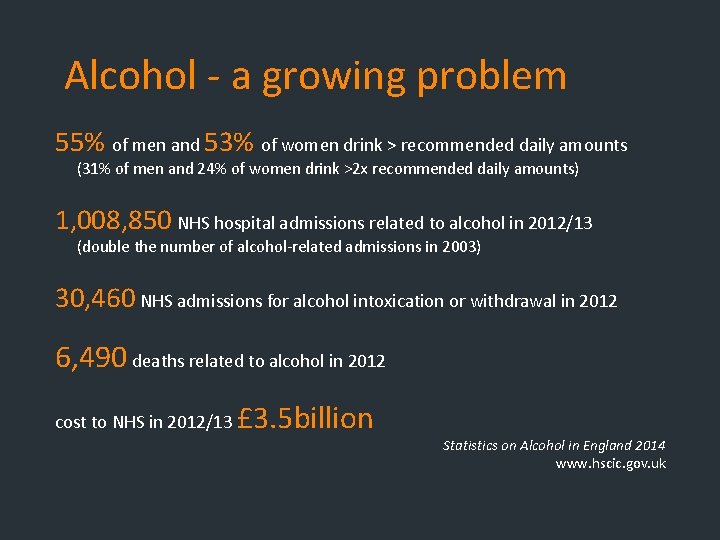
Alcohol - a growing problem 55% of men and 53% of women drink > recommended daily amounts (31% of men and 24% of women drink >2 x recommended daily amounts) 1, 008, 850 NHS hospital admissions related to alcohol in 2012/13 (double the number of alcohol-related admissions in 2003) 30, 460 NHS admissions for alcohol intoxication or withdrawal in 2012 6, 490 deaths related to alcohol in 2012 cost to NHS in 2012/13 £ 3. 5 billion Statistics on Alcohol in England 2014 www. hscic. gov. uk
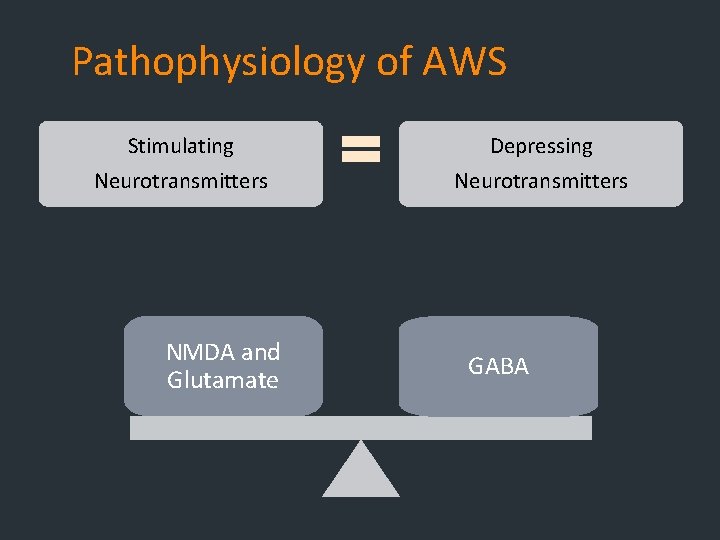
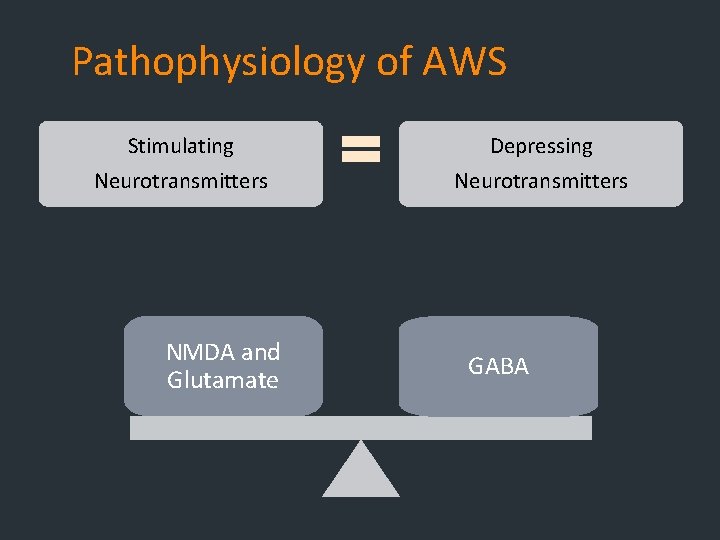
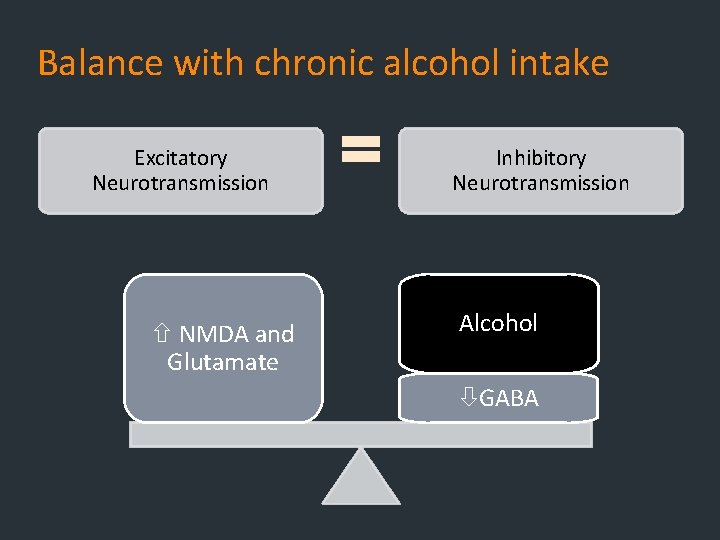
Pathophysiology of AWS Stimulating Depressing Neurotransmitters NMDA and Glutamate GABA
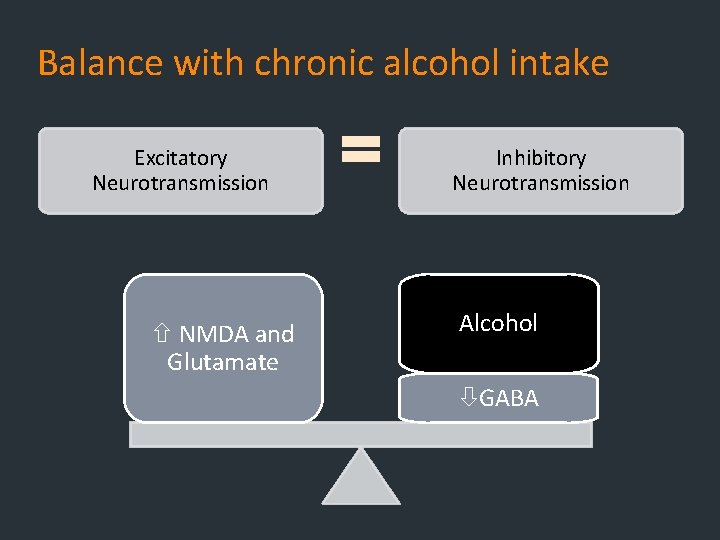
Balance with chronic alcohol intake Excitatory Neurotransmission NMDA and Glutamate Inhibitory Neurotransmission Alcohol GABA
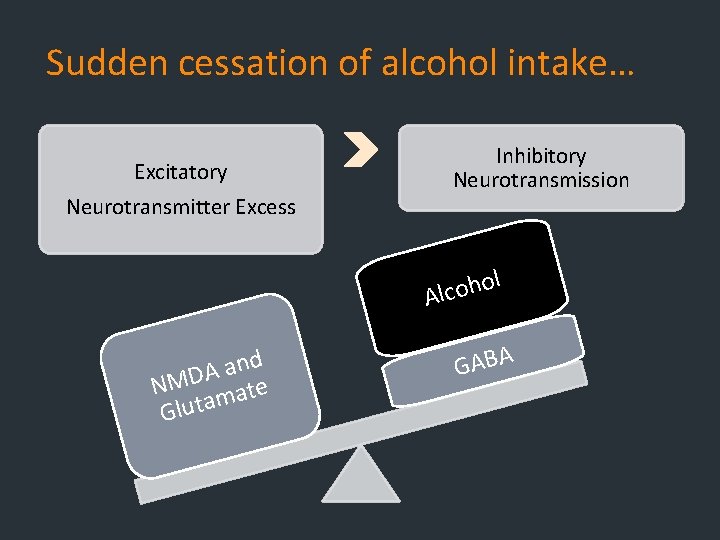
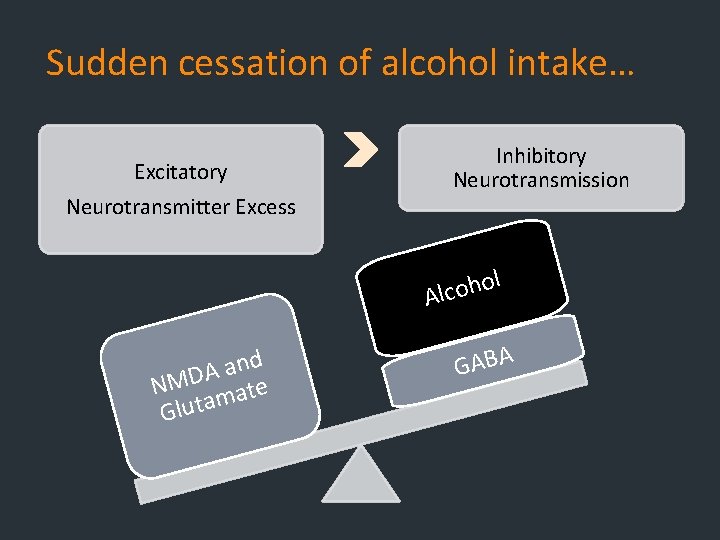
Sudden cessation of alcohol intake… Excitatory Neurotransmitter Excess Inhibitory Neurotransmission l o h o Alc d n a A NMD mate Gluta GABA
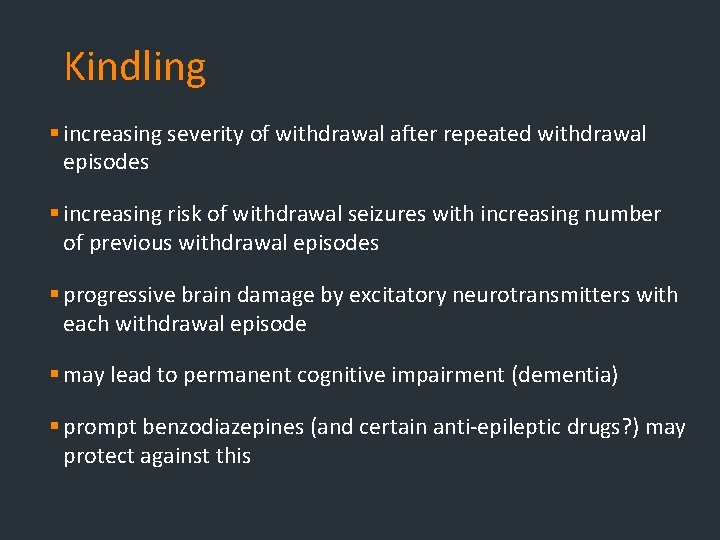
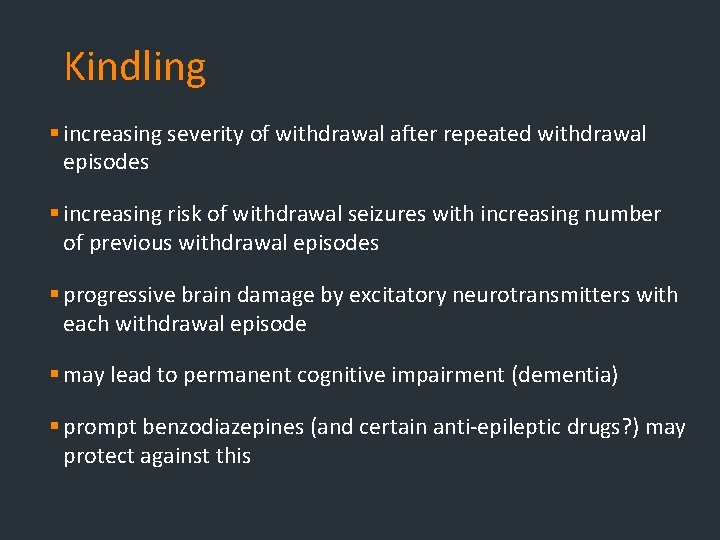
Kindling § increasing severity of withdrawal after repeated withdrawal episodes § increasing risk of withdrawal seizures with increasing number of previous withdrawal episodes § progressive brain damage by excitatory neurotransmitters with each withdrawal episode § may lead to permanent cognitive impairment (dementia) § prompt benzodiazepines (and certain anti-epileptic drugs? ) may protect against this
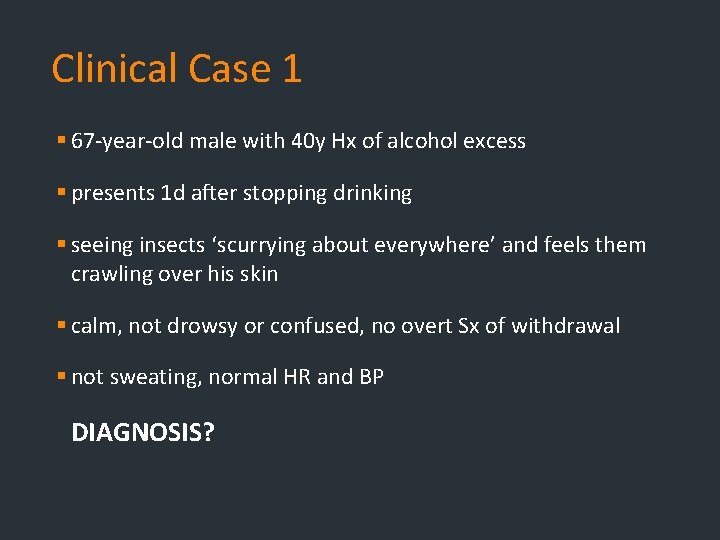
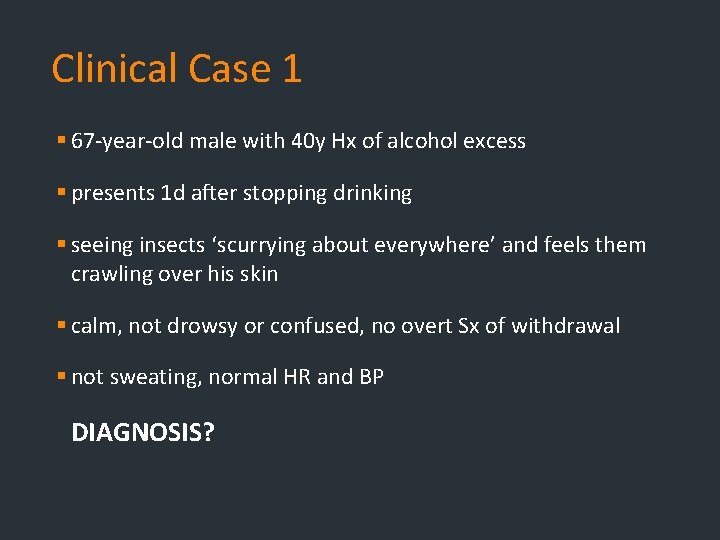
Clinical Case 1 § 67 -year-old male with 40 y Hx of alcohol excess § presents 1 d after stopping drinking § seeing insects ‘scurrying about everywhere’ and feels them crawling over his skin § calm, not drowsy or confused, no overt Sx of withdrawal § not sweating, normal HR and BP DIAGNOSIS?
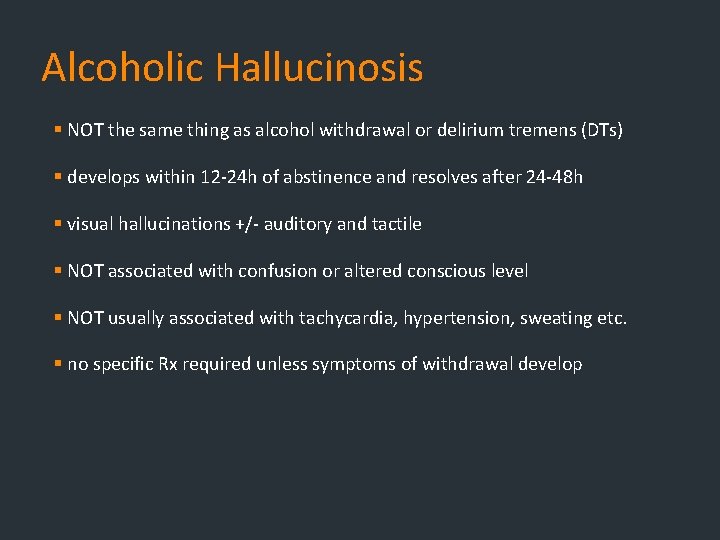
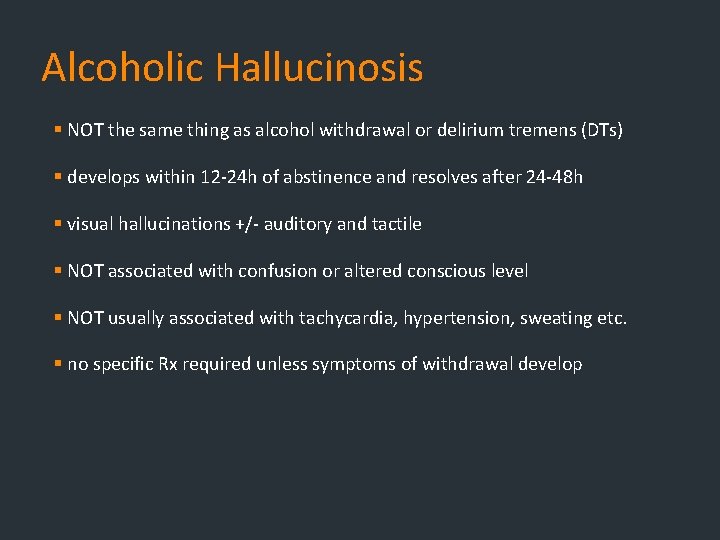
Alcoholic Hallucinosis § NOT the same thing as alcohol withdrawal or delirium tremens (DTs) § develops within 12 -24 h of abstinence and resolves after 24 -48 h § visual hallucinations +/- auditory and tactile § NOT associated with confusion or altered conscious level § NOT usually associated with tachycardia, hypertension, sweating etc. § no specific Rx required unless symptoms of withdrawal develop
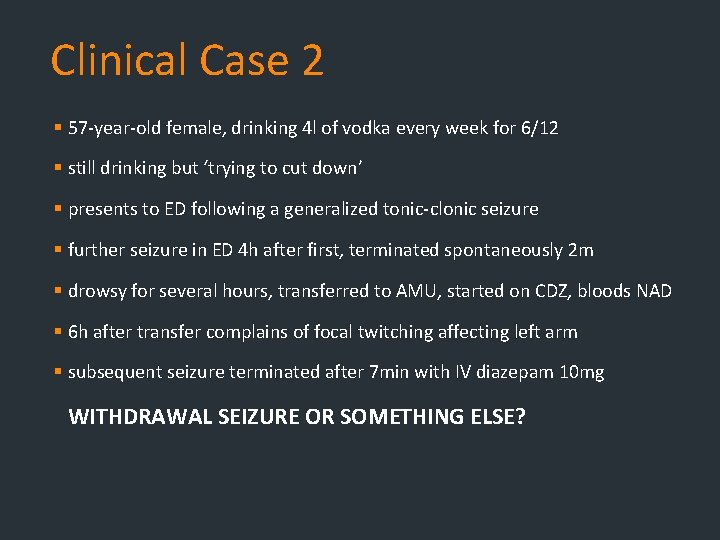
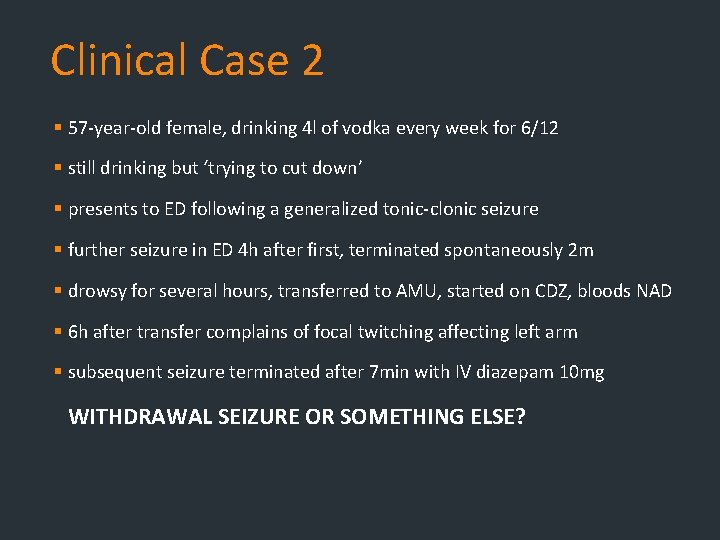
Clinical Case 2 § 57 -year-old female, drinking 4 l of vodka every week for 6/12 § still drinking but ‘trying to cut down’ § presents to ED following a generalized tonic-clonic seizure § further seizure in ED 4 h after first, terminated spontaneously 2 m § drowsy for several hours, transferred to AMU, started on CDZ, bloods NAD § 6 h after transfer complains of focal twitching affecting left arm § subsequent seizure terminated after 7 min with IV diazepam 10 mg WITHDRAWAL SEIZURE OR SOMETHING ELSE?
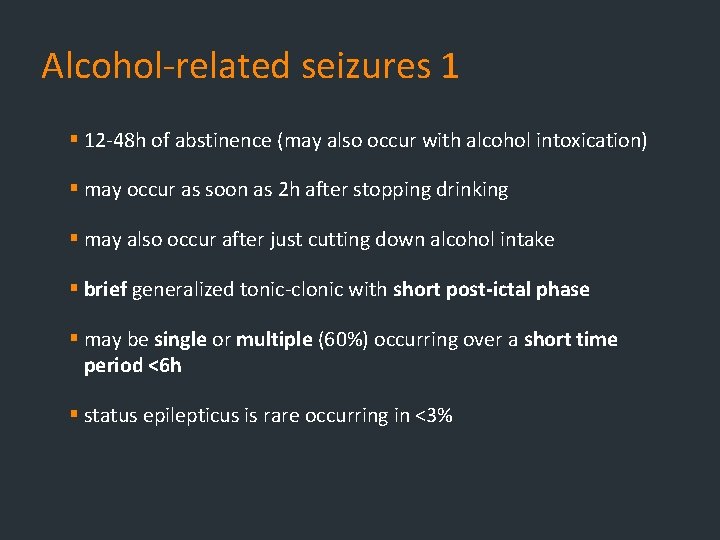
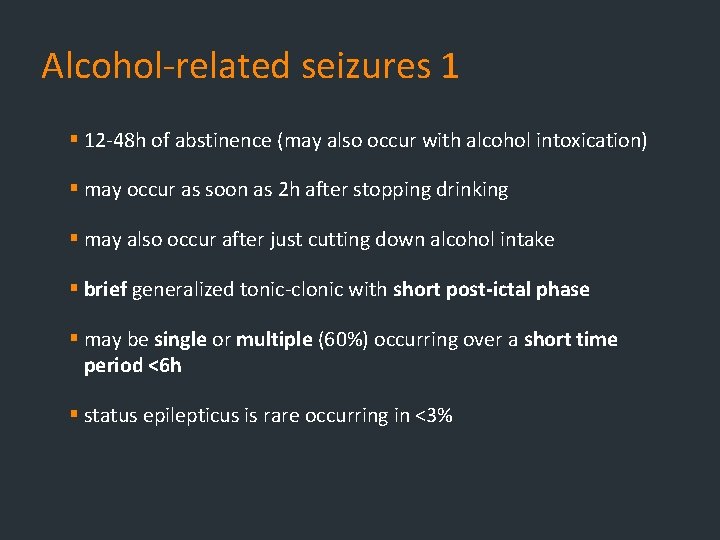
Alcohol-related seizures 1 § 12 -48 h of abstinence (may also occur with alcohol intoxication) § may occur as soon as 2 h after stopping drinking § may also occur after just cutting down alcohol intake § brief generalized tonic-clonic with short post-ictal phase § may be single or multiple (60%) occurring over a short time period <6 h § status epilepticus is rare occurring in <3%
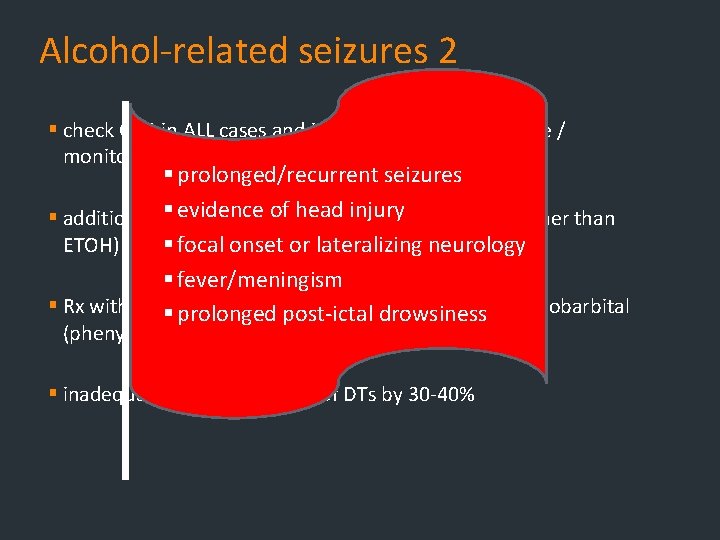
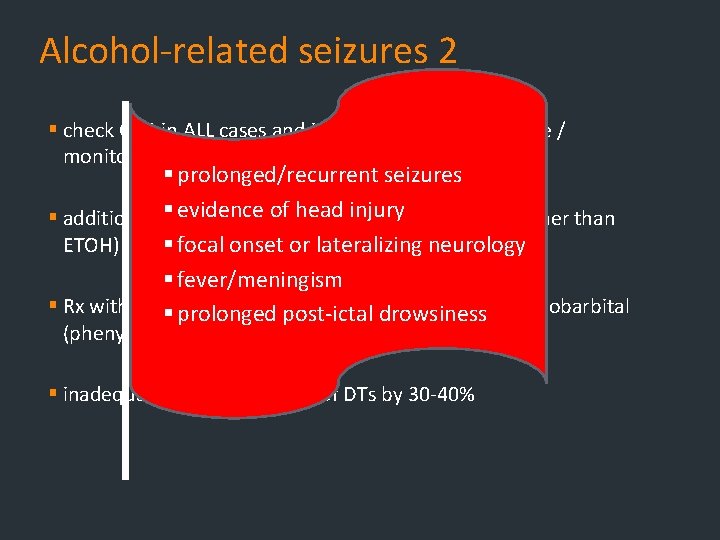
Alcohol-related seizures 2 § check CBG in ALL cases and institute usual nursing care / monitoring § prolonged/recurrent seizures § evidence ofe. g. head § additional investigations CT injury scan, LP (for cause other than ETOH) if any§ focal red flags: onset or lateralizing neurology § fever/meningism § Rx with ADEQUATE dosespost-ictal of benzodiazepines +/- phenobarbital § prolonged drowsiness (phenytoin usually ineffective) § inadequate Rx increases risk of DTs by 30 -40%
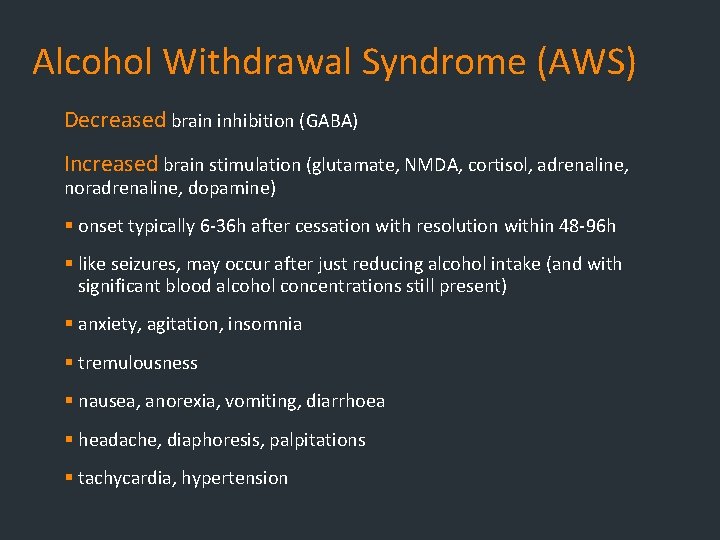
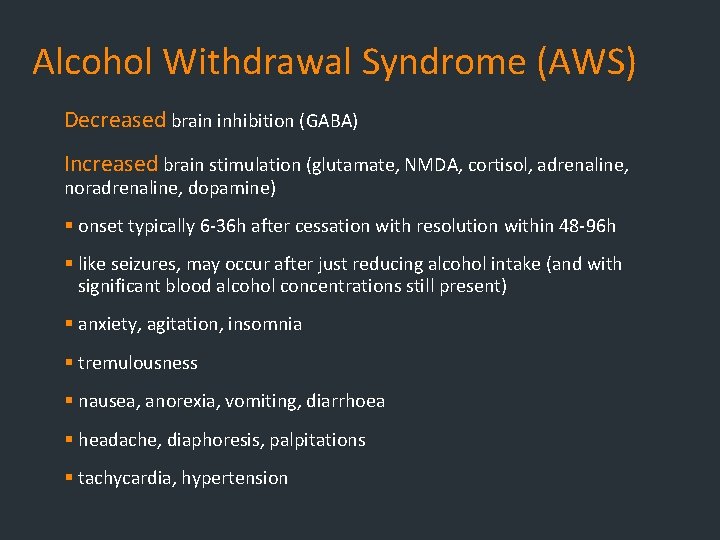
Alcohol Withdrawal Syndrome (AWS) Decreased brain inhibition (GABA) Increased brain stimulation (glutamate, NMDA, cortisol, adrenaline, noradrenaline, dopamine) § onset typically 6 -36 h after cessation with resolution within 48 -96 h § like seizures, may occur after just reducing alcohol intake (and with significant blood alcohol concentrations still present) § anxiety, agitation, insomnia § tremulousness § nausea, anorexia, vomiting, diarrhoea § headache, diaphoresis, palpitations § tachycardia, hypertension
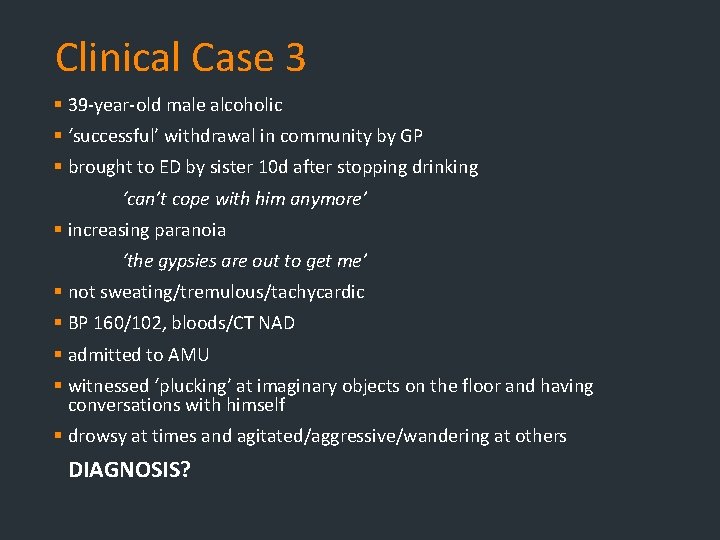
Clinical Case 3 § 39 -year-old male alcoholic § ‘successful’ withdrawal in community by GP § brought to ED by sister 10 d after stopping drinking ‘can’t cope with him anymore’ § increasing paranoia ‘the gypsies are out to get me’ § not sweating/tremulous/tachycardic § BP 160/102, bloods/CT NAD § admitted to AMU § witnessed ‘plucking’ at imaginary objects on the floor and having conversations with himself § drowsy at times and agitated/aggressive/wandering at others DIAGNOSIS?
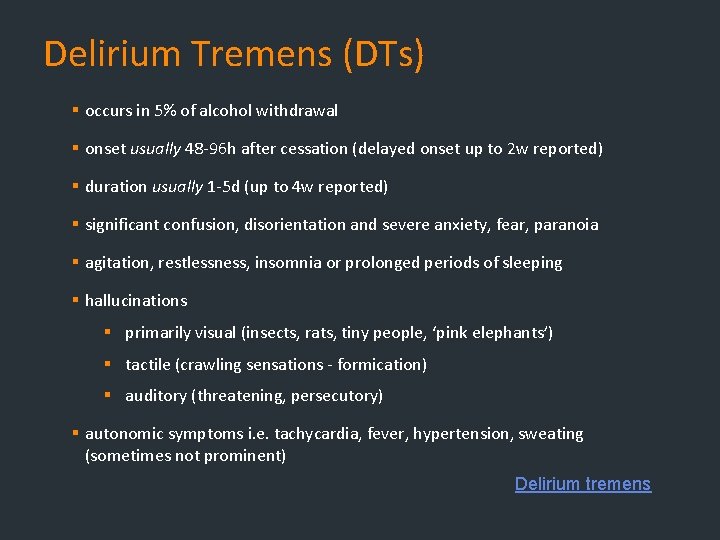
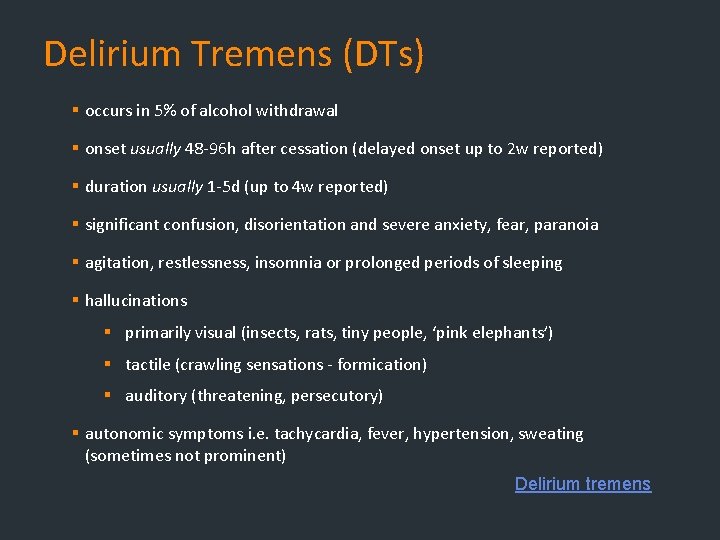
Delirium Tremens (DTs) § occurs in 5% of alcohol withdrawal § onset usually 48 -96 h after cessation (delayed onset up to 2 w reported) § duration usually 1 -5 d (up to 4 w reported) § significant confusion, disorientation and severe anxiety, fear, paranoia § agitation, restlessness, insomnia or prolonged periods of sleeping § hallucinations § primarily visual (insects, rats, tiny people, ‘pink elephants’) § tactile (crawling sensations - formication) § auditory (threatening, persecutory) § autonomic symptoms i. e. tachycardia, fever, hypertension, sweating (sometimes not prominent) Delirium tremens
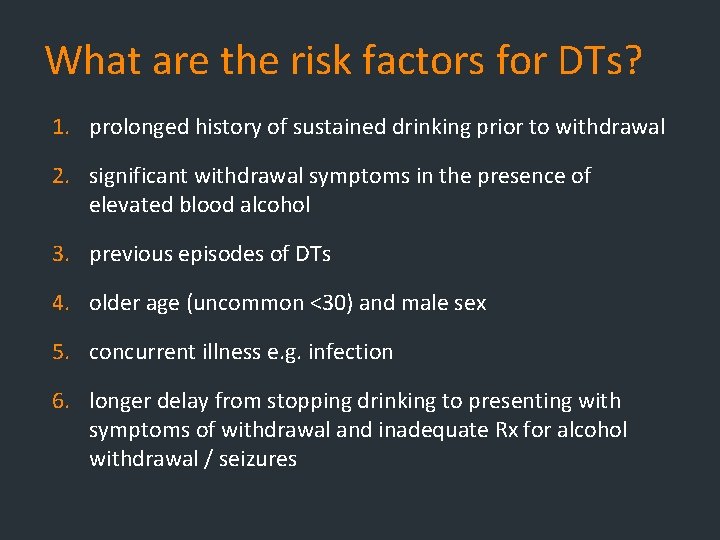
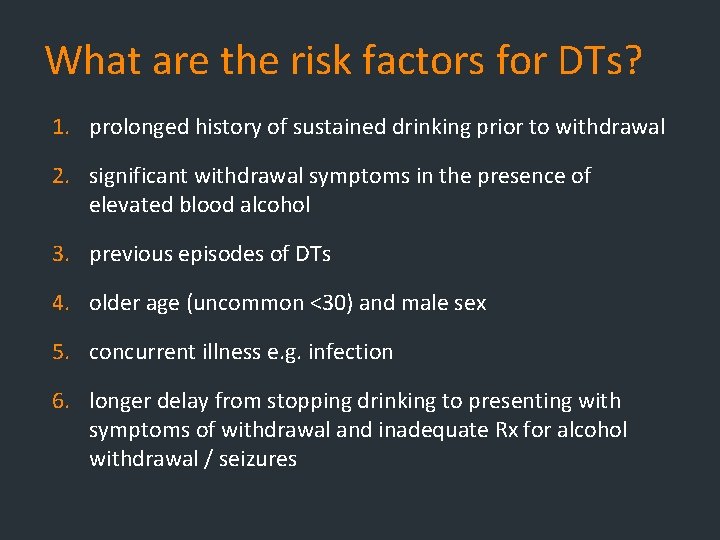
What are the risk factors for DTs? 1. prolonged history of sustained drinking prior to withdrawal 2. significant withdrawal symptoms in the presence of elevated blood alcohol 3. previous episodes of DTs 4. older age (uncommon <30) and male sex 5. concurrent illness e. g. infection 6. longer delay from stopping drinking to presenting with symptoms of withdrawal and inadequate Rx for alcohol withdrawal / seizures
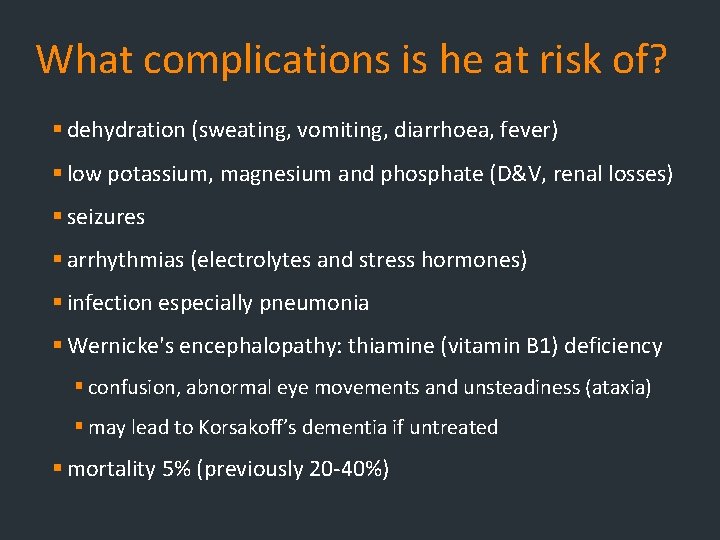
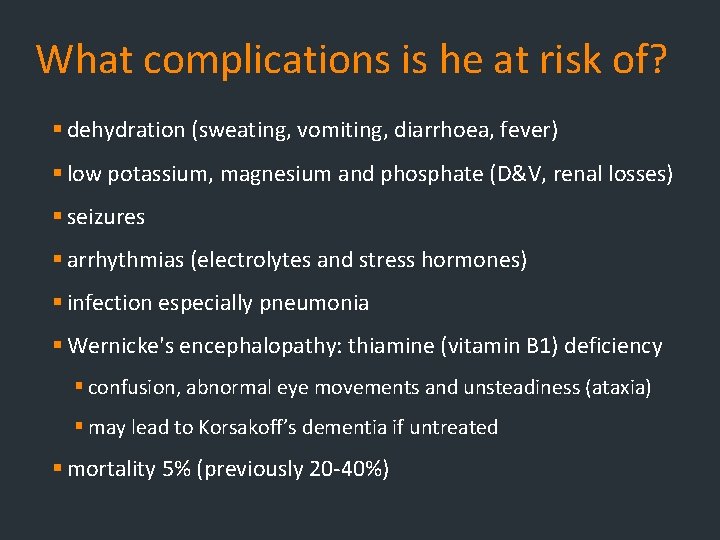
What complications is he at risk of? § dehydration (sweating, vomiting, diarrhoea, fever) § low potassium, magnesium and phosphate (D&V, renal losses) § seizures § arrhythmias (electrolytes and stress hormones) § infection especially pneumonia § Wernicke's encephalopathy: thiamine (vitamin B 1) deficiency § confusion, abnormal eye movements and unsteadiness (ataxia) § may lead to Korsakoff’s dementia if untreated § mortality 5% (previously 20 -40%)
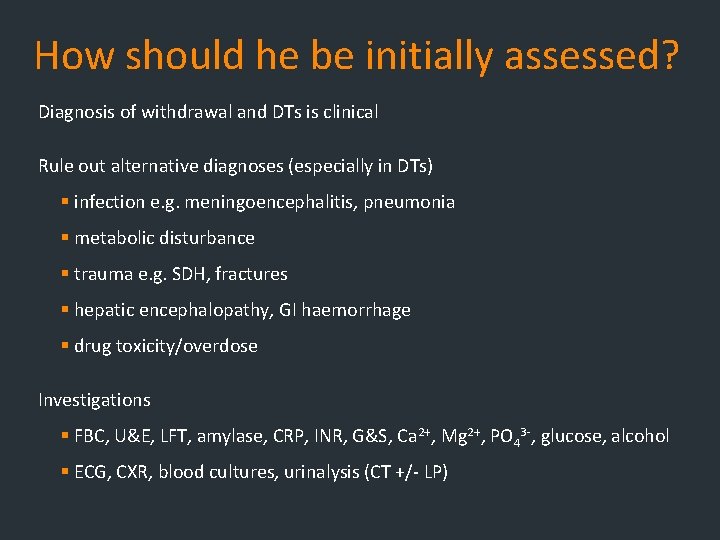
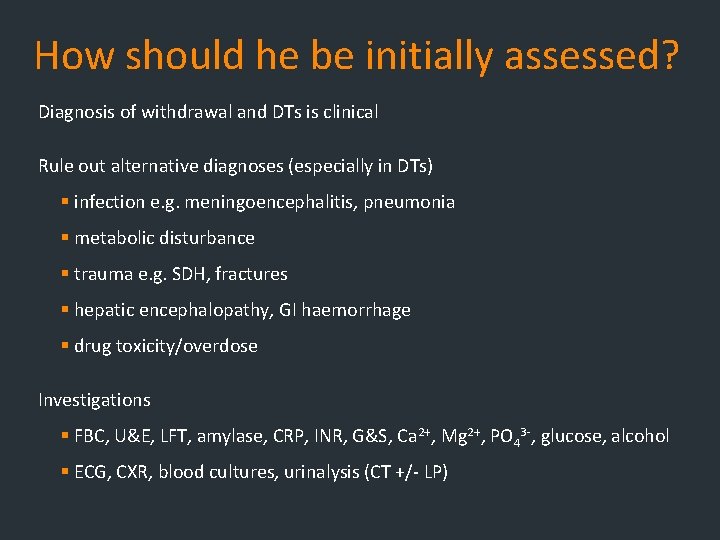
How should he be initially assessed? Diagnosis of withdrawal and DTs is clinical Rule out alternative diagnoses (especially in DTs) § infection e. g. meningoencephalitis, pneumonia § metabolic disturbance § trauma e. g. SDH, fractures § hepatic encephalopathy, GI haemorrhage § drug toxicity/overdose Investigations § FBC, U&E, LFT, amylase, CRP, INR, G&S, Ca 2+, Mg 2+, PO 43 -, glucose, alcohol § ECG, CXR, blood cultures, urinalysis (CT +/- LP)
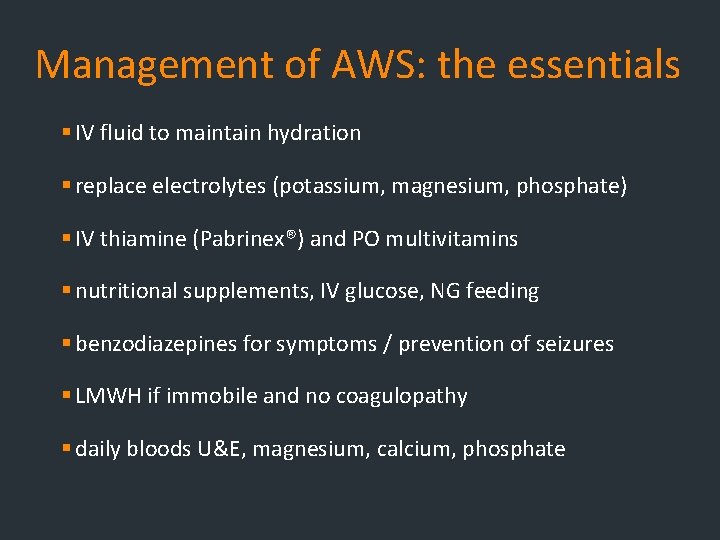
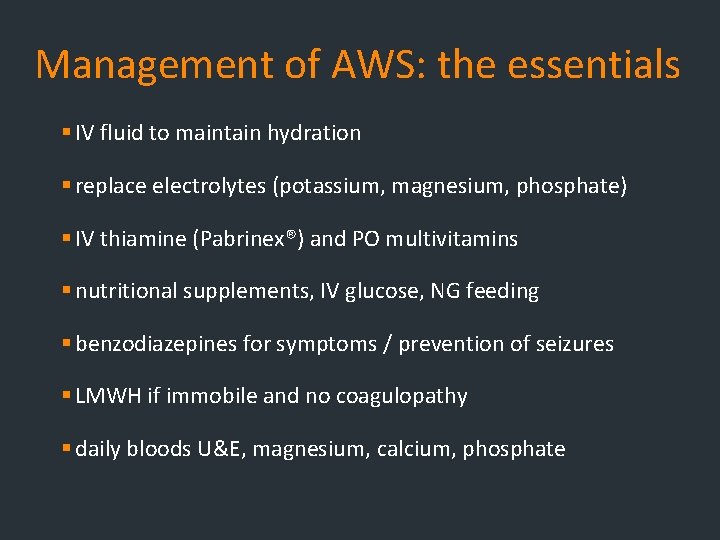
Management of AWS: the essentials § IV fluid to maintain hydration § replace electrolytes (potassium, magnesium, phosphate) § IV thiamine (Pabrinex®) and PO multivitamins § nutritional supplements, IV glucose, NG feeding § benzodiazepines for symptoms / prevention of seizures § LMWH if immobile and no coagulopathy § daily bloods U&E, magnesium, calcium, phosphate
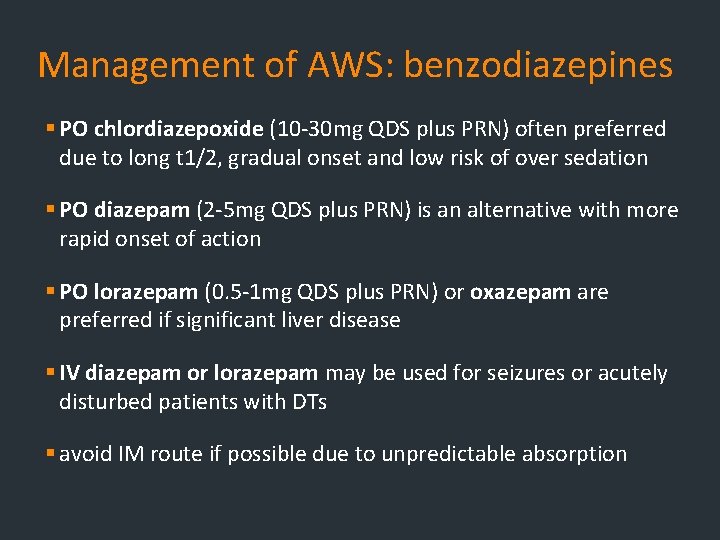
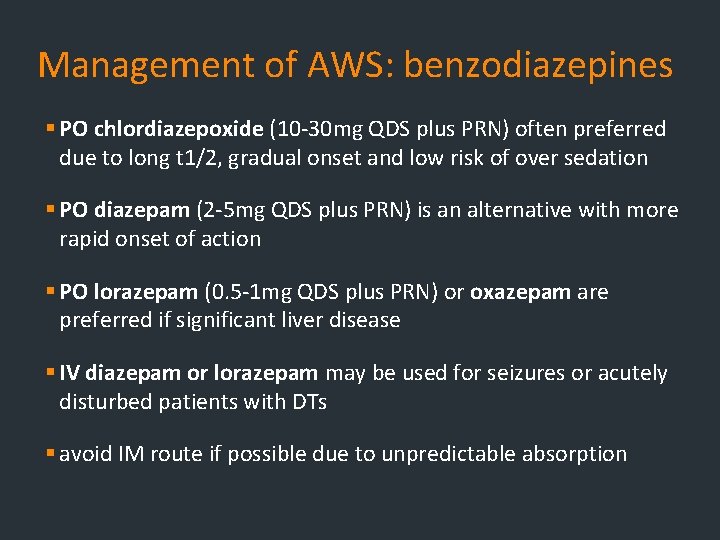
Management of AWS: benzodiazepines § PO chlordiazepoxide (10 -30 mg QDS plus PRN) often preferred due to long t 1/2, gradual onset and low risk of over sedation § PO diazepam (2 -5 mg QDS plus PRN) is an alternative with more rapid onset of action § PO lorazepam (0. 5 -1 mg QDS plus PRN) or oxazepam are preferred if significant liver disease § IV diazepam or lorazepam may be used for seizures or acutely disturbed patients with DTs § avoid IM route if possible due to unpredictable absorption
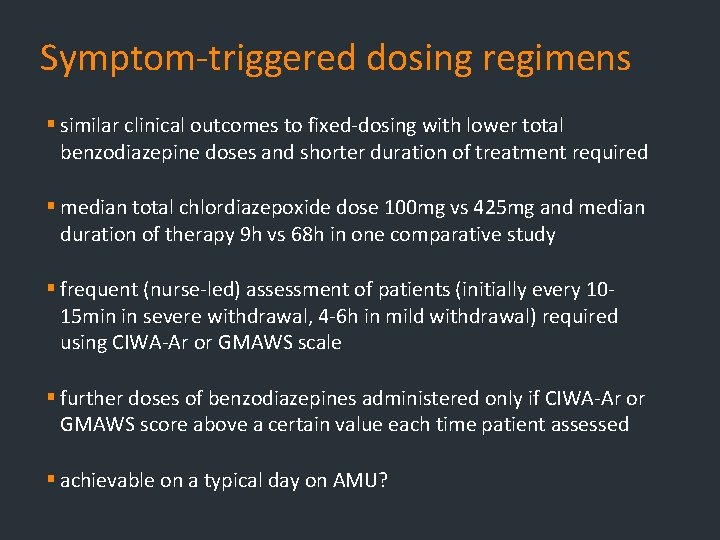
Symptom-triggered dosing regimens § similar clinical outcomes to fixed-dosing with lower total benzodiazepine doses and shorter duration of treatment required § median total chlordiazepoxide dose 100 mg vs 425 mg and median duration of therapy 9 h vs 68 h in one comparative study § frequent (nurse-led) assessment of patients (initially every 1015 min in severe withdrawal, 4 -6 h in mild withdrawal) required using CIWA-Ar or GMAWS scale § further doses of benzodiazepines administered only if CIWA-Ar or GMAWS score above a certain value each time patient assessed § achievable on a typical day on AMU?
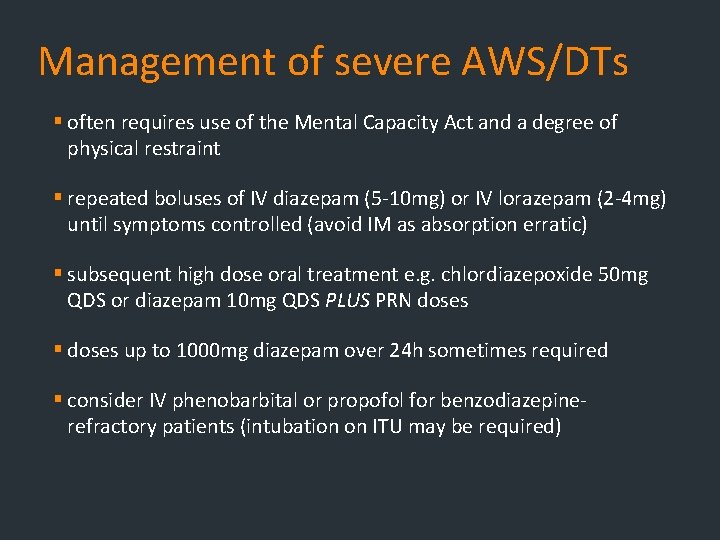
Management of severe AWS/DTs § often requires use of the Mental Capacity Act and a degree of physical restraint § repeated boluses of IV diazepam (5 -10 mg) or IV lorazepam (2 -4 mg) until symptoms controlled (avoid IM as absorption erratic) § subsequent high dose oral treatment e. g. chlordiazepoxide 50 mg QDS or diazepam 10 mg QDS PLUS PRN doses § doses up to 1000 mg diazepam over 24 h sometimes required § consider IV phenobarbital or propofol for benzodiazepinerefractory patients (intubation on ITU may be required)
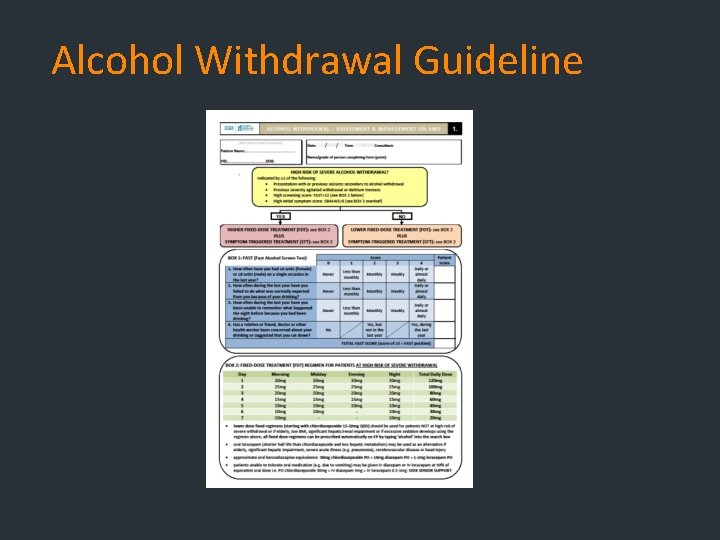
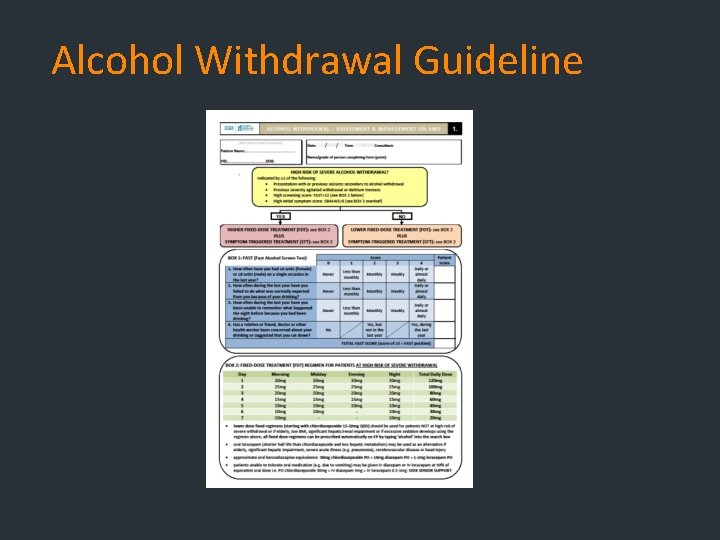
Alcohol Withdrawal Guideline
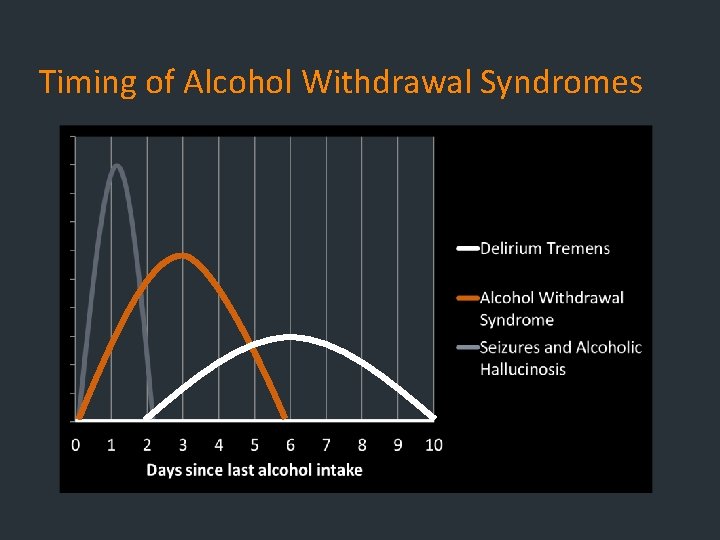
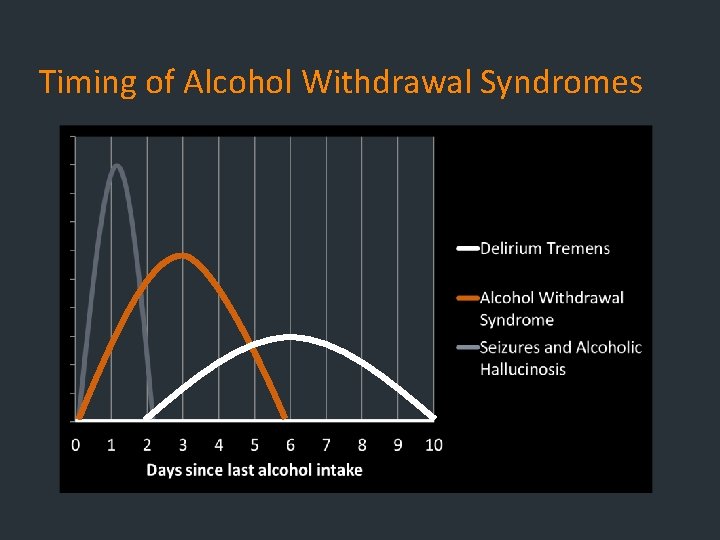
Timing of Alcohol Withdrawal Syndromes
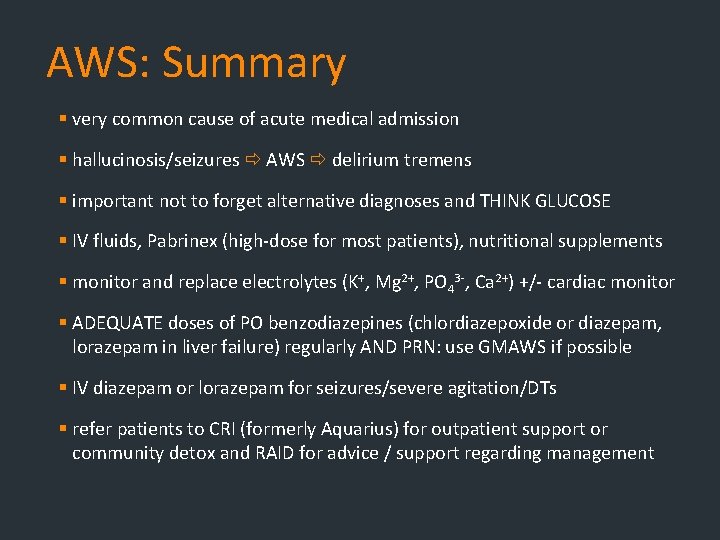
AWS: Summary § very common cause of acute medical admission § hallucinosis/seizures AWS delirium tremens § important not to forget alternative diagnoses and THINK GLUCOSE § IV fluids, Pabrinex (high-dose for most patients), nutritional supplements § monitor and replace electrolytes (K+, Mg 2+, PO 43 -, Ca 2+) +/- cardiac monitor § ADEQUATE doses of PO benzodiazepines (chlordiazepoxide or diazepam, lorazepam in liver failure) regularly AND PRN: use GMAWS if possible § IV diazepam or lorazepam for seizures/severe agitation/DTs § refer patients to CRI (formerly Aquarius) for outpatient support or community detox and RAID for advice / support regarding management

Questions