AKI in the critically ill patient James Beck
AKI in the critically ill patient James Beck

& Consequence
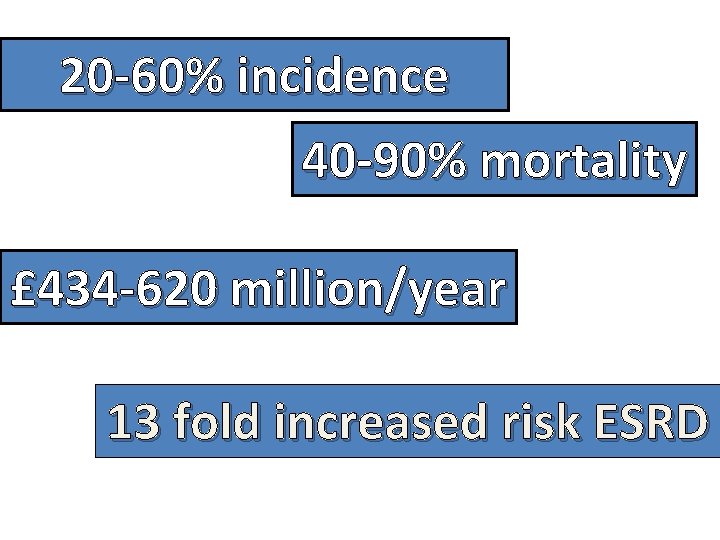
20 -60% incidence 40 -90% mortality £ 434 -620 million/year 13 fold increased risk ESRD
Pathophysiology
Pre renal Intra renal Post renal
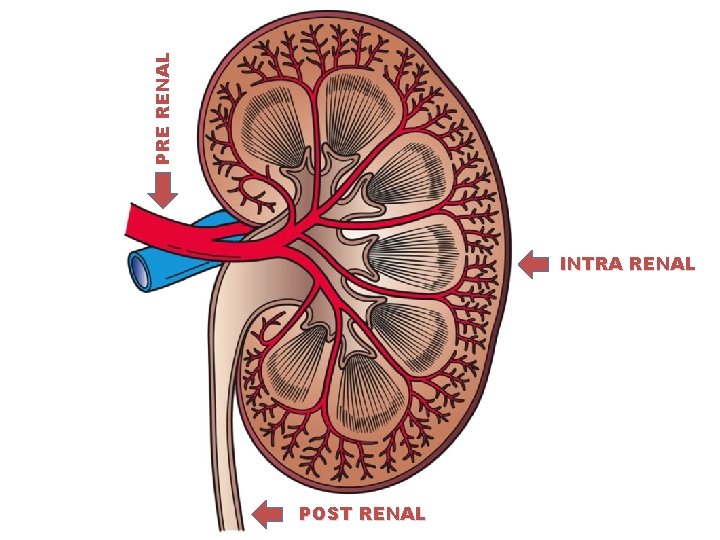
PRE RENAL INTRA RENAL POST RENAL
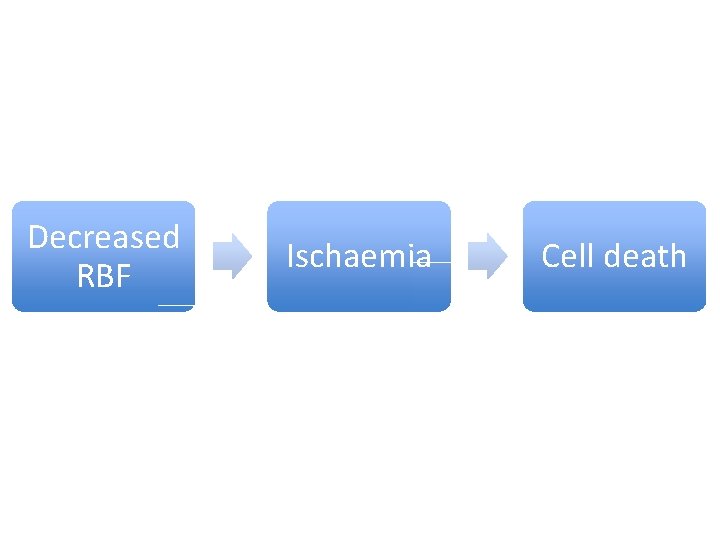
Decreased RBF Ischaemia Cell death
Pre renal Vomiting Iatrogenic Haemorrhage Sepsis Diarrhoea
Intra renal Drugs Toxins Autoimmune
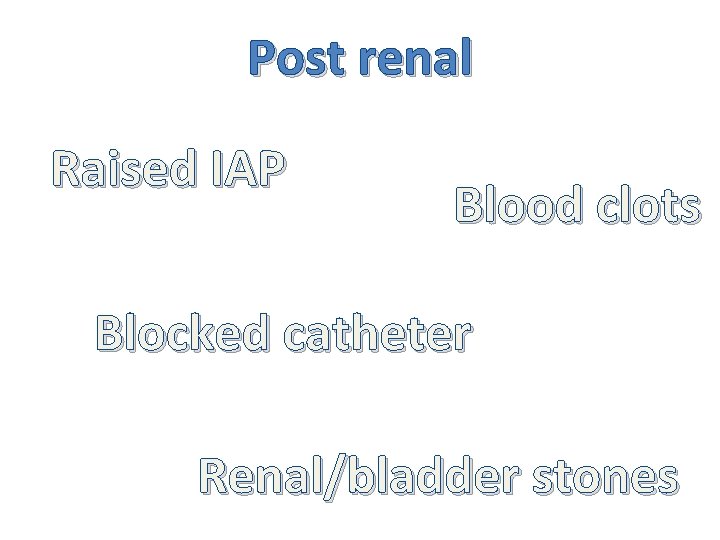
Post renal Raised IAP Blood clots Blocked catheter Renal/bladder stones
Staging

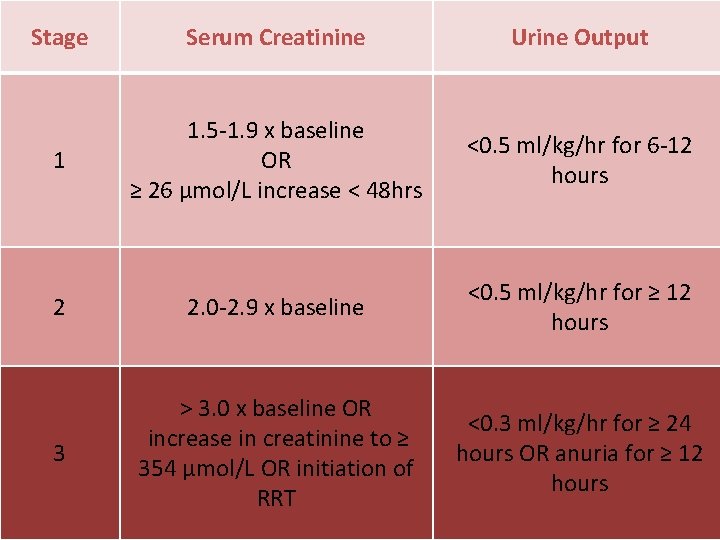
Stage Serum Creatinine Urine Output 1 1. 5 -1. 9 x baseline OR ≥ 26 μmol/L increase < 48 hrs <0. 5 ml/kg/hr for 6 -12 hours 2 2. 0 -2. 9 x baseline <0. 5 ml/kg/hr for ≥ 12 hours 3 > 3. 0 x baseline OR increase in creatinine to ≥ 354 μmol/L OR initiation of RRT <0. 3 ml/kg/hr for ≥ 24 hours OR anuria for ≥ 12 hours

Management

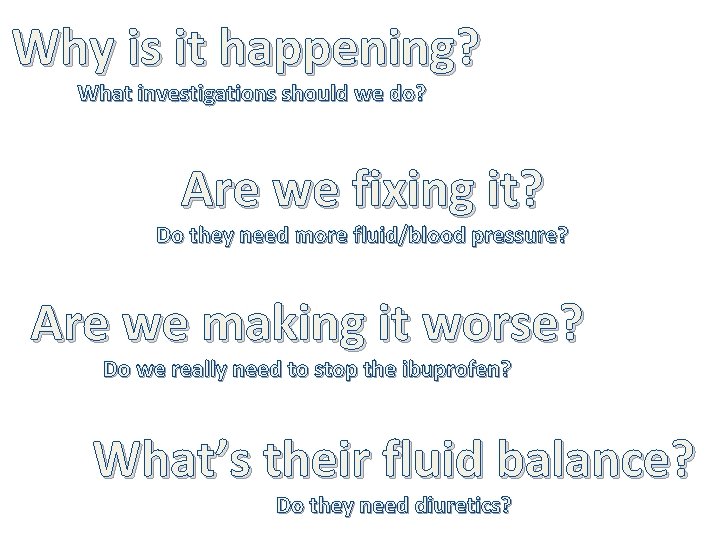
Why is it happening? What investigations should we do? Are we fixing it? Do they need more fluid/blood pressure? Are we making it worse? Do we really need to stop the ibuprofen? What’s their fluid balance? Do they need diuretics?
STOP AKI Sepsis - Think and treat Toxins - Avoid Optimise BP Prevent Harm - Identify cause - Treat complications Review doses Review fluids

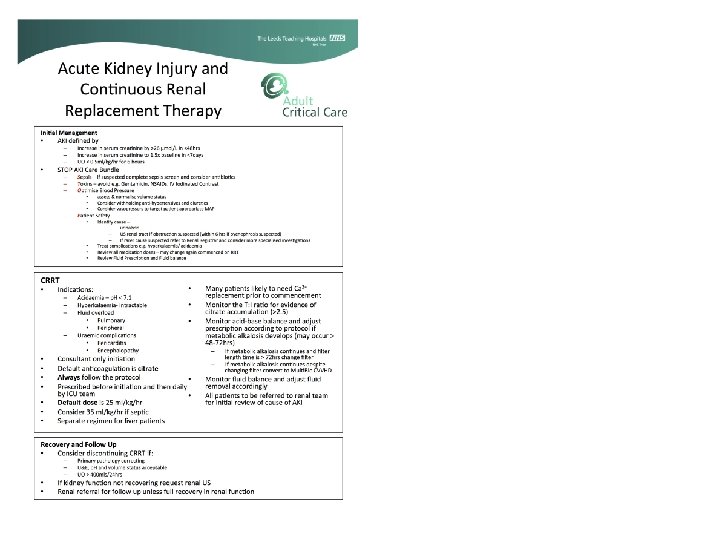
RRT- When to start?
In summary It’s common and serious It costs a lot It’s often either avoidable or fixable It’s a marker for quality of care


www. yorkshireicm. uk @yorkshireicm www. leedsicu. com @leedsicu
- Slides: 23