Airway Management Anatomical and Physiological Differences Presented By
Airway Management: Anatomical and Physiological Differences Presented By: Danyel Dorn MSN, RN, CPN, Clinical Nurse Educator-Pediatric Service Line
Purpose The pediatric patient’s airway is significantly different than that of an adult. The pediatric airway is dependent on the physical development of the child and/or specific anatomical issues associated with particular congenital anomalies.
Competency Statement The perianesthesia registered nurse will be able to identify various anatomical differences of the pediatric airway as well as maneuvers and equipment to support the airway.
Developmental Airway Issues Newborns/Infants – large occiput, small nares, enlarged tongue, short neck, large upper airway lymphoid tissue Obligate nose breathers – resulting in airway obstruction Epiglottis is U-shaped, narrow and hard rather than flat as an adult Shape of the larynx is that of an inverted cone rather than cylindrical Cricoid cartilage is the narrowest part of the trachea
Developmental Airway Issues Effects of edema on the pediatric airway, specifically the already cylindrically shaped cricoid, can significantly reduce and endanger the ability of the child to ventilate Sedation and general anesthesia further may complicate these small airways Age and normal growth and development will alter the anatomy of the patient
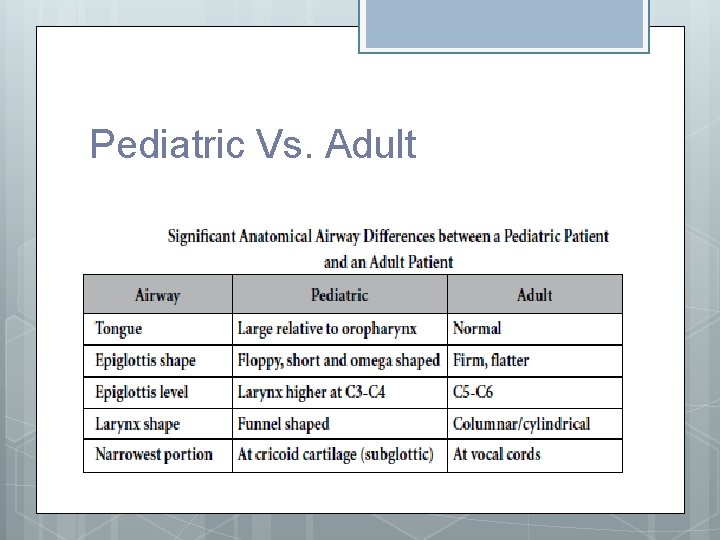
Pediatric Vs. Adult
Airway Management Maneuvers Jaw thrust – open airway by using thumbs to physically push the posterior aspects of the mandible upwards. When the mandible is displaced forward, it pulls the tongue forward and prevents the tongue from occluding the entrance to the trachea.
Airway Management Maneuvers Chin lift – tilt patient’s head back with the palm of one hand while lifting the chin up with the other hand; this maneuver pulls the tongue out of the way
Continuous Positive Airway Pressure (CPAP) CPAP gives positive pressure via either an ETT or by bag/mask The positive pressure prevents the bronchioles and alveoli from collapsing at the end of the expiratory phase Also useful for instances of laryngospasm where the positive pressure prevents the vocal cords from closing, thereby relieving the airway obstruction

Blow by Oxygen This is a simple way to deliver oxygen to the patient by letting either the bag/mask blow close to patient’s face/nose/mouth Downside is the inability to determine the exact amount of oxygen being delivered
Oxygen Delivery Nasal Cannula – delivers small amounts of oxygen, 0. 25 -4 liters, may result in discomfort, drying of nasal passages and epistaxis. Face shield, simple face mask – generally used for the patient not requiring assistance to maintain an open airway, but needs a higher oxygen concentration, 8 -10 liters. Non-rebreather – keep reservoir bag filled, 15 liters, use if patient is experiencing respiratory distress
Oral Airway Used only on the obtunded patient Prevents the tongue from partially or completely obstructing the epiglottis Size is measured by lining up the airway from the patient’s earlobe to the corner of the mouth. Insert the airway upside down; once at the back of the throat, rotate 180 degrees to secure the tongue down Flared end of the oral airway should sit securely at the oral opening
Nasopharyngeal Airway Tube designed to be inserted in the nasal passage to relieve airway obstruction Measured by lining the tube from patient’s nares to the angle of the jaw Usually helpful in the obtunded patient and is tolerated by a drowsy patient Using a NP is very helpful with children that have hypotonia associated with other anomalies such as cerebral palsy or spasticity as these children will frequently present with “floppy” airways as part of generalized hypotonia.
Endotracheal Tubes Endotracheal tubes (ETT), whether oral (OTT) or nasal (NTT), are considered the most reliable method of protecting and maintaining a patient’s airway Inserted either through the mouth or nasal passageway into the trachea and ends above the bifurcation of the lungs or just above the carina
ETT Continued Confirmed placement by auscultation of bilateral equal breath sounds, equal chest rise and chest x-ray The most common malpositioning of an ETT is into the right main stem due to the stem’s more vertical orientation ETT sizes range from 2. 5 to 8. 5 cuffed and uncuffed
ETT Continued As a result of the subglottic narrowing, foreign bodies can become lodged below the cords, or the endotracheal tube may be small enough to pass through the cords but not beyond the cricoid ring This narrowing can create an effective anatomic seal without the need for a cuffed ETT With the creation of smaller, newer profile, lower pressure cuffed tubes, the American Heart Assoc. now has approved cuffed ETTs for all pediatric patients outside the newborn period, provided the cuff pressure can be maintained at less than 20 cm H 2 O.
Laryngeal Mask Airway (LMAs) Consists of a tube with an inflatable cuff at the end that is inserted into the pharynx and sits above the vocal cords May cause less pain and coughing compared to the ETT LMA does not protect the patient from aspiration because it does not go through the trachea and vocal cords Use with caution for patients who are at risk for aspiration
High Risk Patients History of difficult intubation Upper/lower respiratory tract infection Previous or current head/neck surgery Andenotonsilar hypertrophy: enlarged tonsils and adenoids are the number one cause of obstructive sleep apnea and hypoventilation in children Micrognathia: abnormal smallness of one or both jaws
High Risk Patients Retrognathia: one or both jaws recede in regards to the frontal plane of the forehead Macroglossia: enlarged tongue Congenital airway lesions: cysts, tumors
High Risk Patients diagnosed with: Down syndrome, shortened mandible/jaw, Goldenhar syndrome, Pierre Robin syndrome, Treacher Collins syndrome, Arthrogryposis Cervical immobility: Klippel-Feil syndrome, Noonan syndrome, Juvenile Rheumatoid Arthritis
High Risk Patients Congenital lesions: Cystic Hygroma (lymphatic lesion classically found in left posterior triangle of the neck and armpits) Gross abnormalities, tongue size, mandible size and symmetry, neck mobility, morbid obesity, trauma
Mallampati Classification Pharyngeal airway opening is typically assessed with a Mallampati Classification Score Allows the practitioner to visualize the oral cavity and rate the level of obstruction to the airway from both the tongue and uvula
Mallampati Scores Class I: Soft palate, uvula, fauces (arched opening), pillars visible Class II: Soft palate, uvula, fauces visible Class III: Soft palate, base of uvula visible Class IV: only hard palate visible
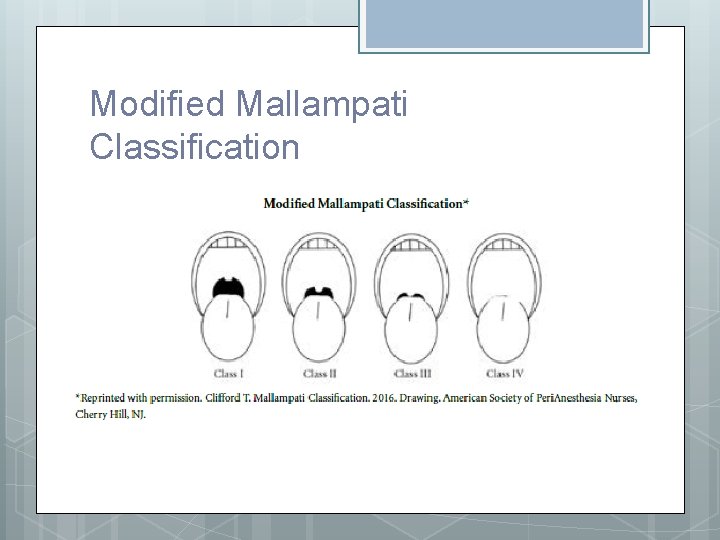
Modified Mallampati Classification
Risks - Postanesthesia Surgical procedures involving the pediatric airway such as the common tonsillectomy and adenoidectomy as well as procedures involving other airway structures (pharynx, larynx, esophagus) should be closely monitored in the Phase I PACU Edema or swelling of the narrow pediatric airway may cause partial or complete airway compromise
Risks - Postanesthesia Bleeding from the surgical site may also cause obstruction • Monitor for signs of bleeding (frequent swallowing, nausea) Patients with limited cervical spine mobility due to injury, previous surgical fusion or congenital issues may need careful maneuvers without overextension to clear obstructed airways until airway adjuncts can be used. Some patients may need to be placed in the “tonsil position” (slight reverse Trendelenburg and on the side) to assist with drainage of airway secretions.
Reference ASPAN (2016). A Competency Based Orientation and Credentialing Program for the Registered Nurse Caring for the Pediatric Patient in the Perianesthesia Setting.
Answers 1. 2. 3. 4. 5. B B B C C
- Slides: 28