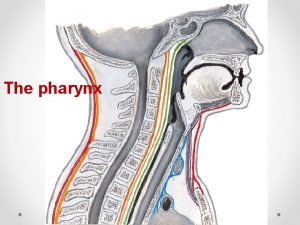
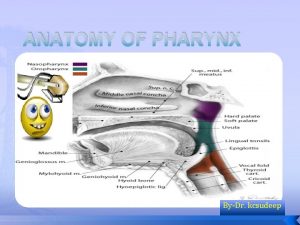
Airway management Airway Anatomy Upper Airway Pharynx Epiglottis









- Slides: 69
Airway management
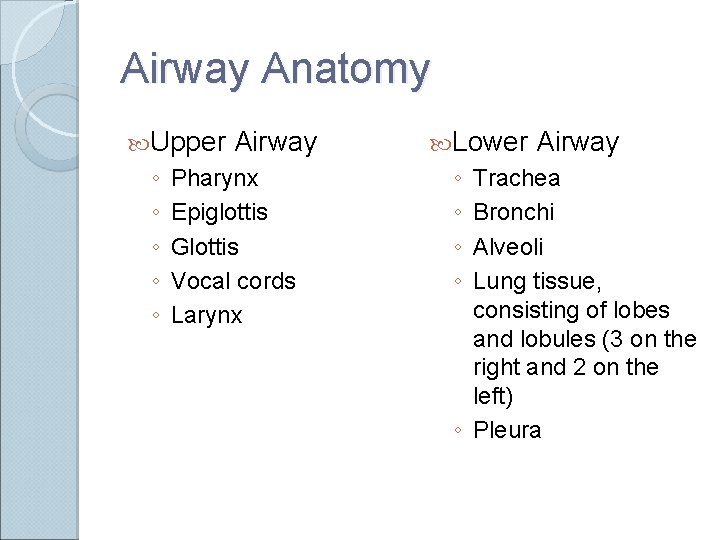
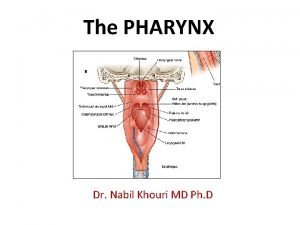
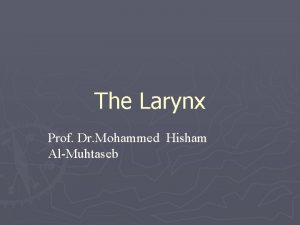
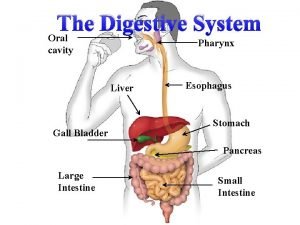
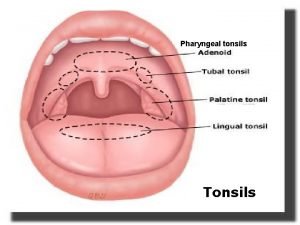
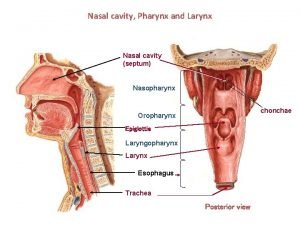
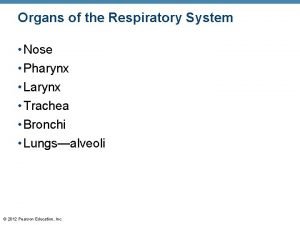
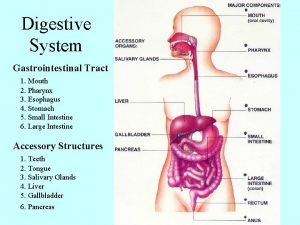
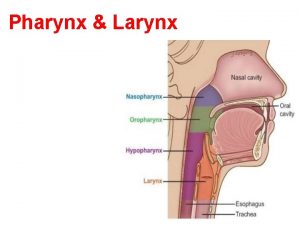
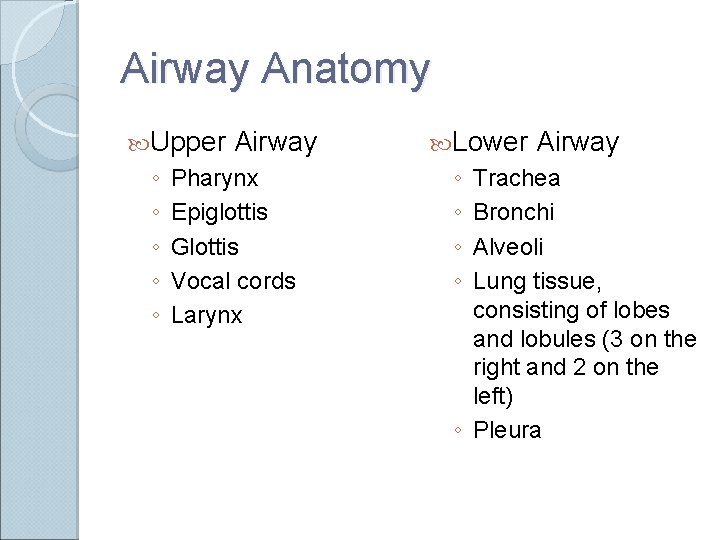
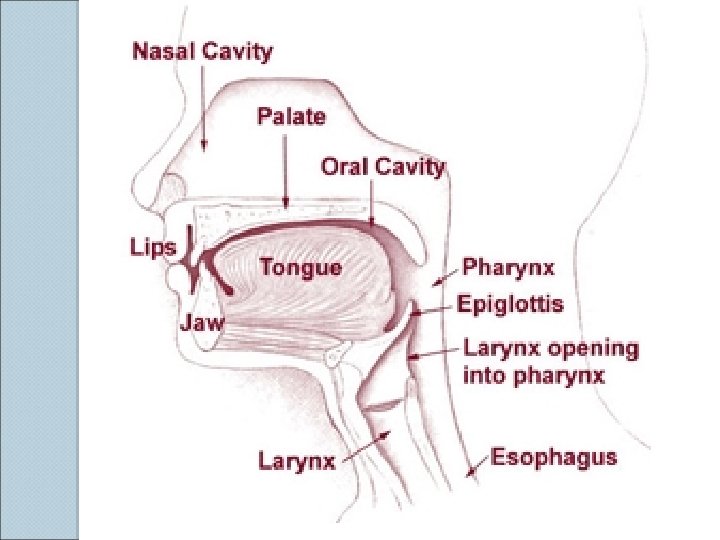
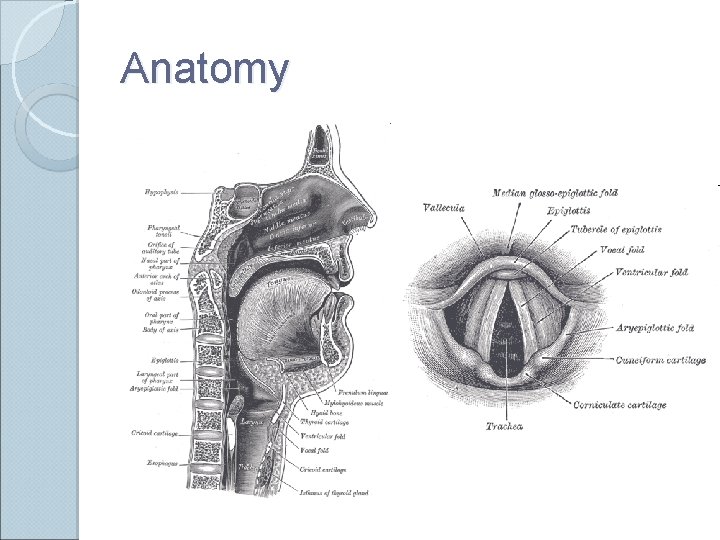
Airway Anatomy Upper ◦ ◦ ◦ Airway Pharynx Epiglottis Glottis Vocal cords Larynx Lower ◦ ◦ Airway Trachea Bronchi Alveoli Lung tissue, consisting of lobes and lobules (3 on the right and 2 on the left) ◦ Pleura


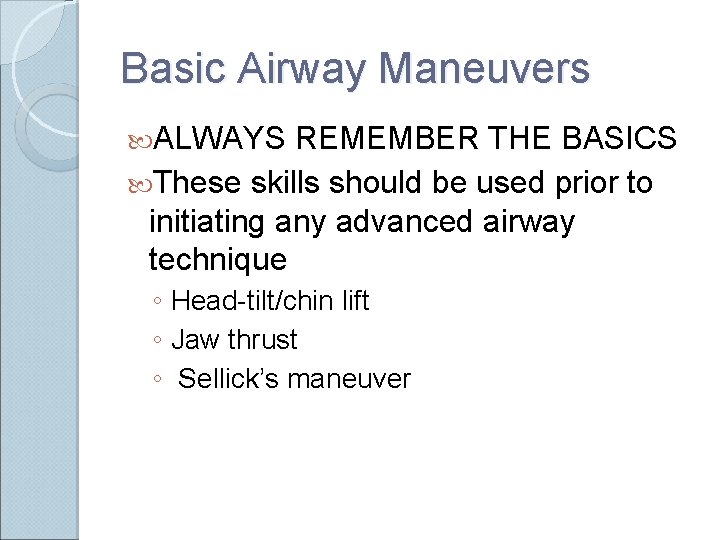
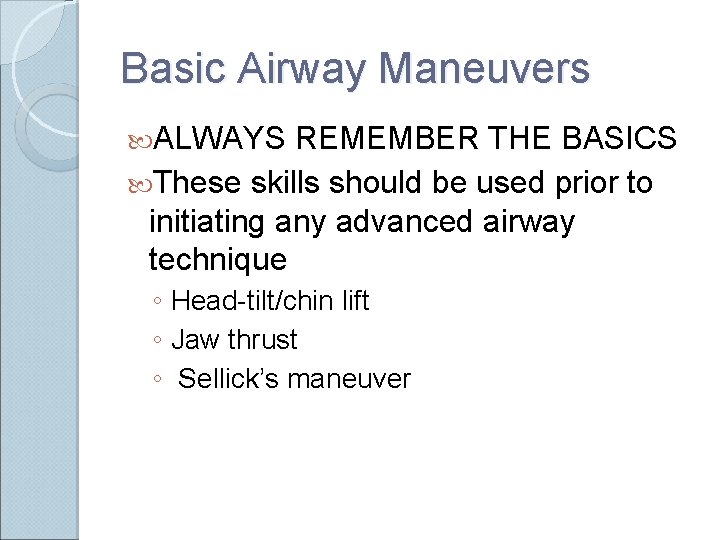
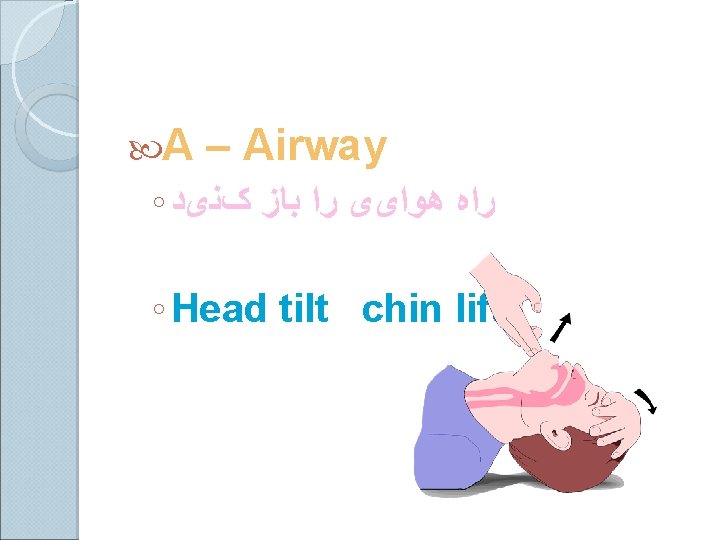
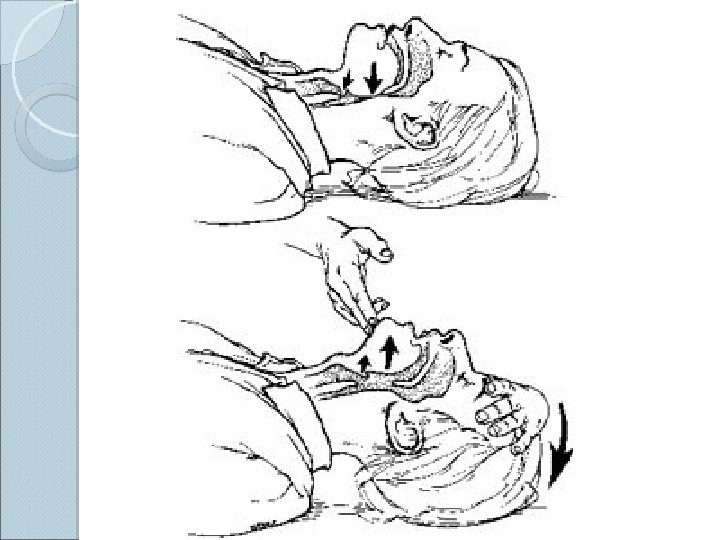
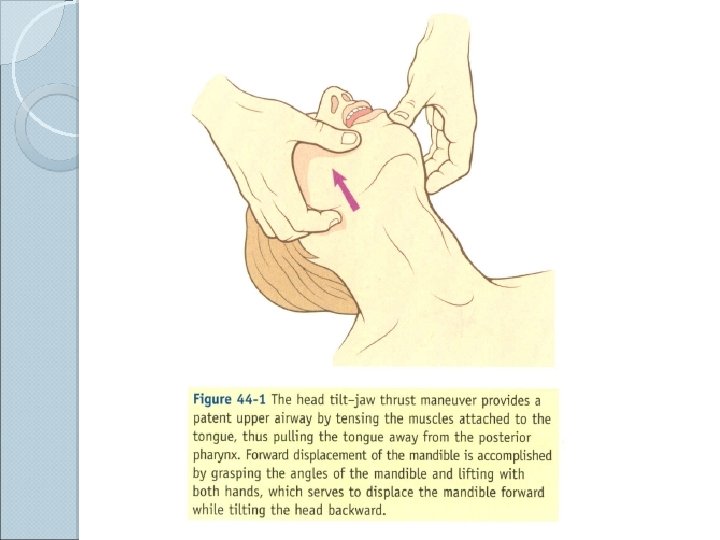
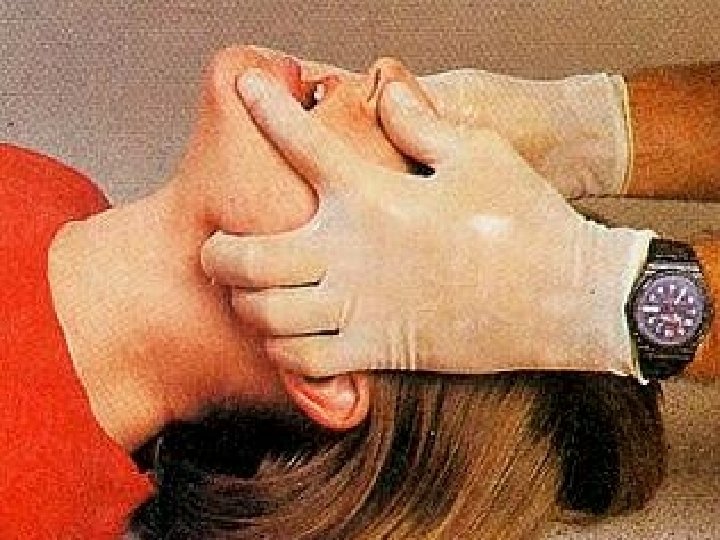
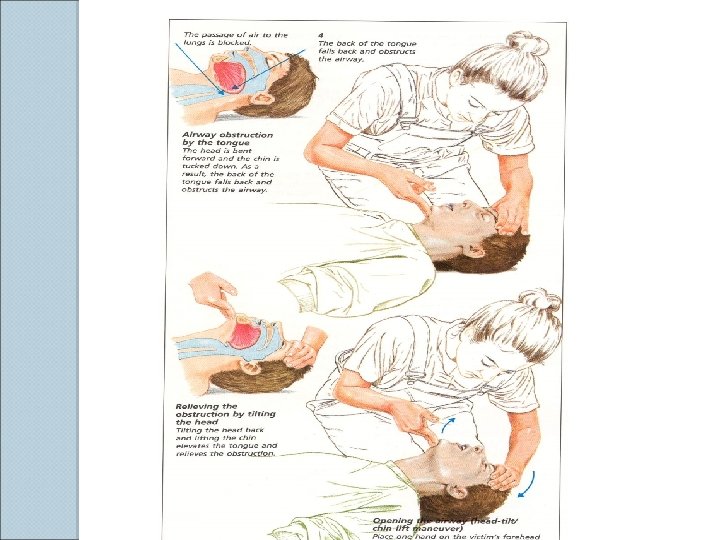
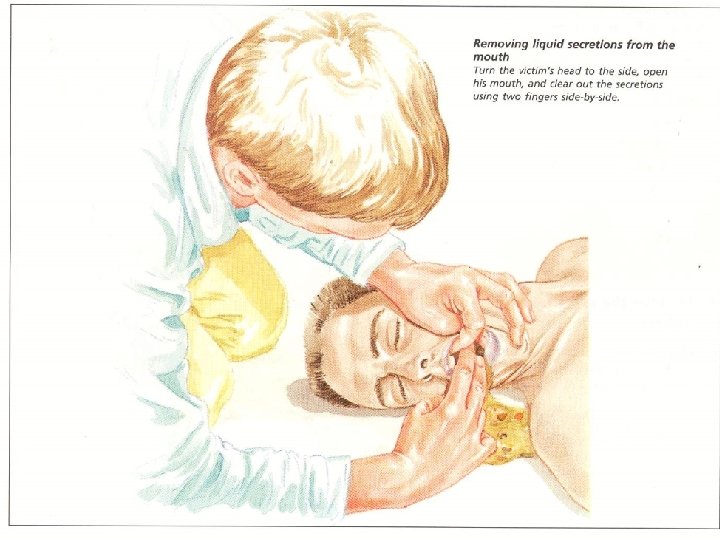
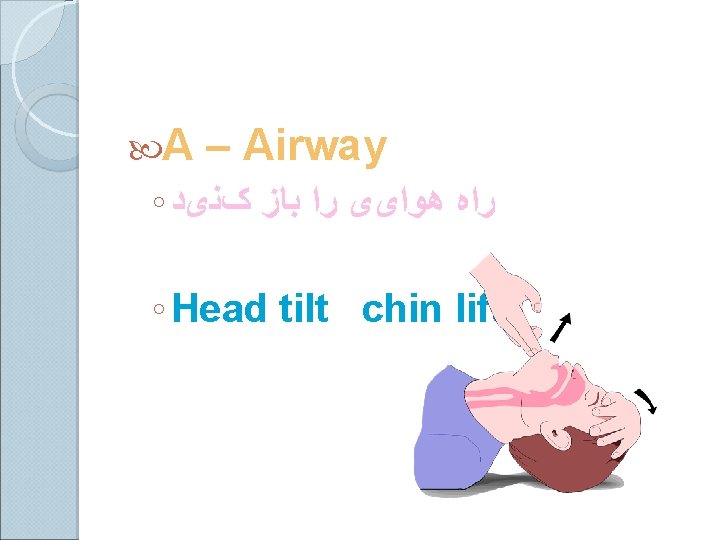
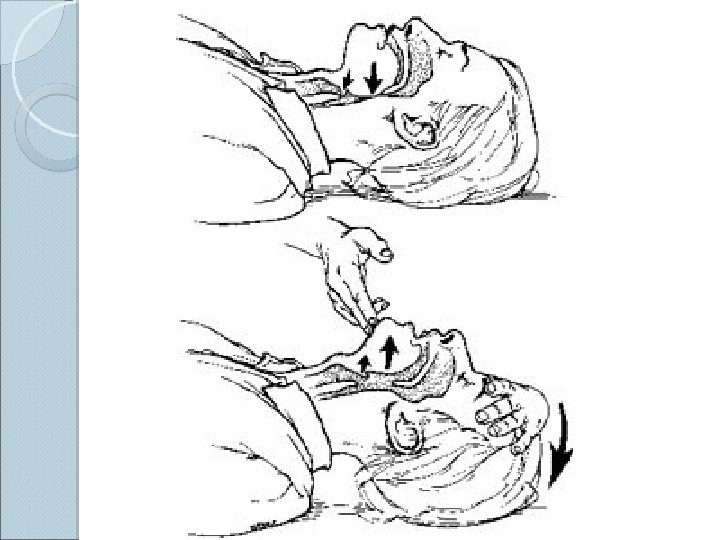
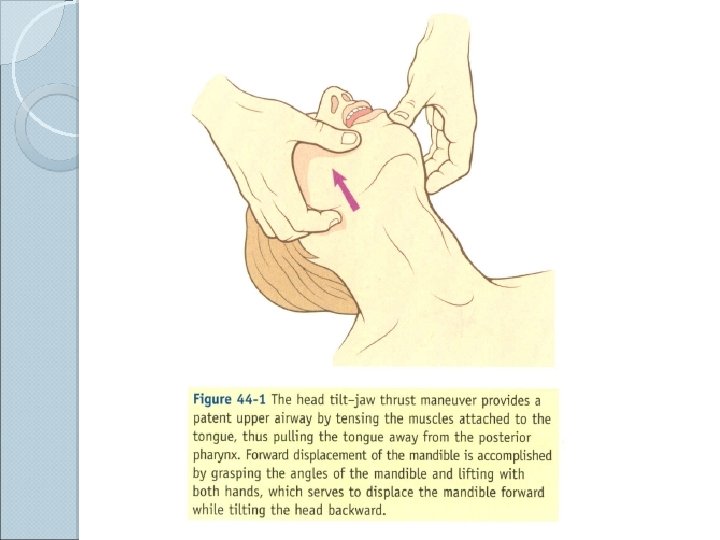
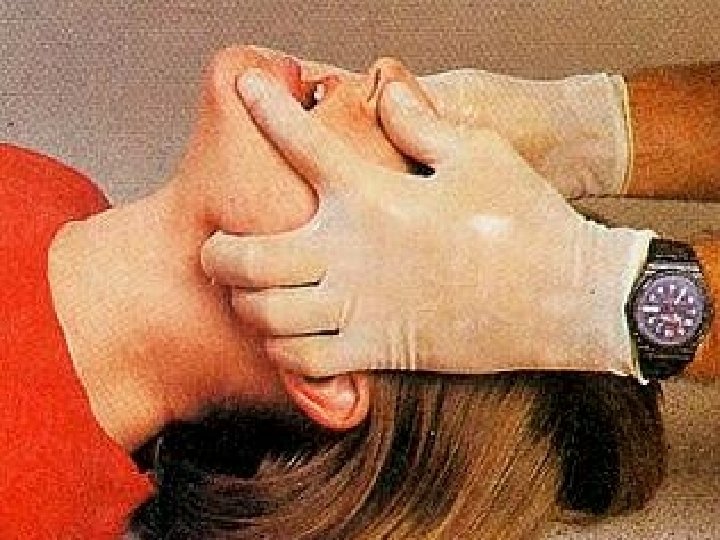
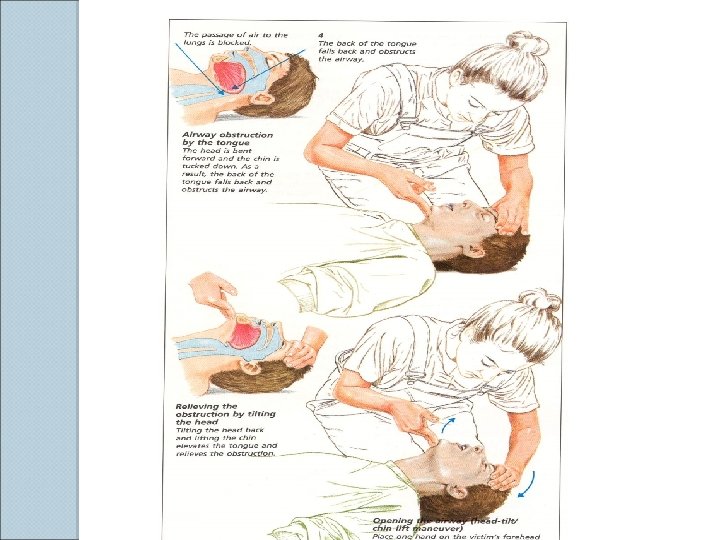
Basic Airway Maneuvers ALWAYS REMEMBER THE BASICS These skills should be used prior to initiating any advanced airway technique ◦ Head-tilt/chin lift ◦ Jaw thrust ◦ Sellick’s maneuver
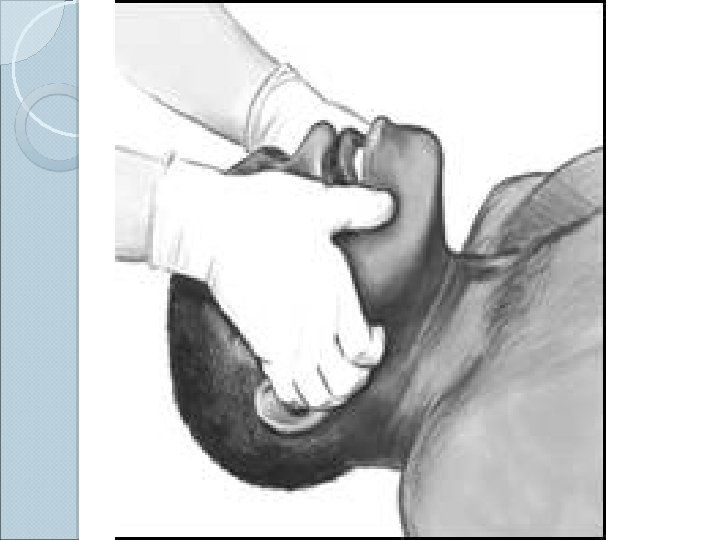

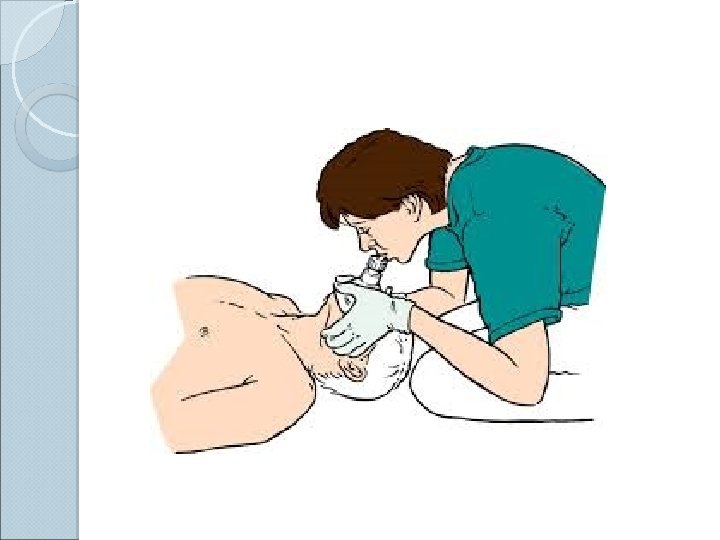
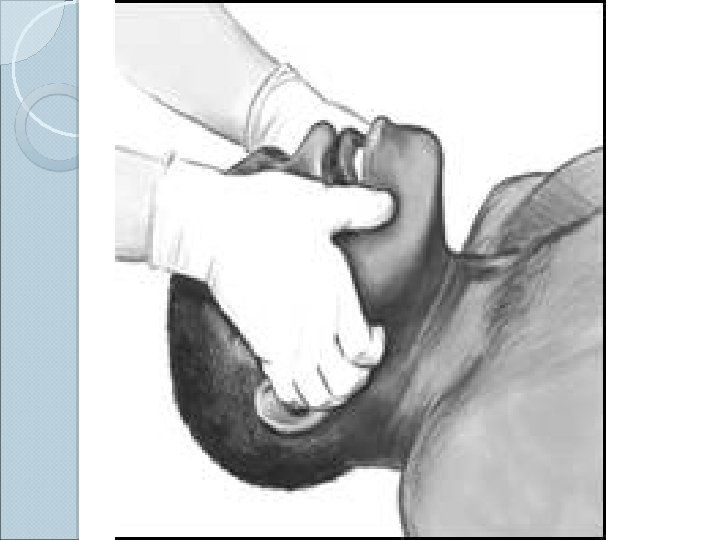
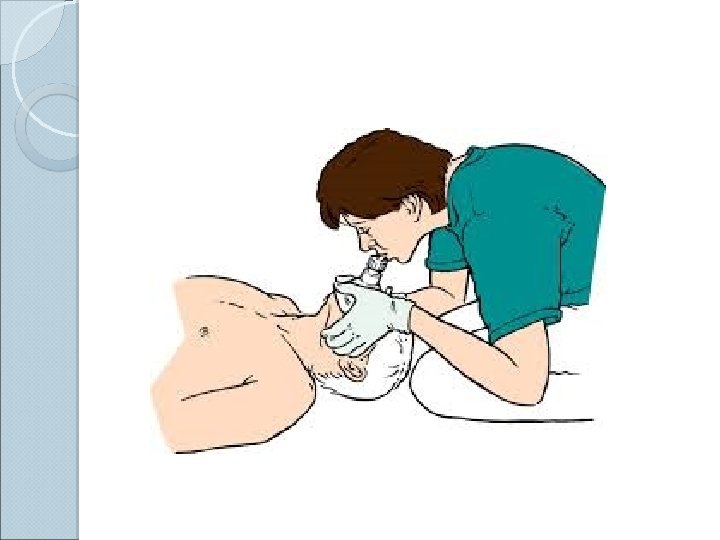
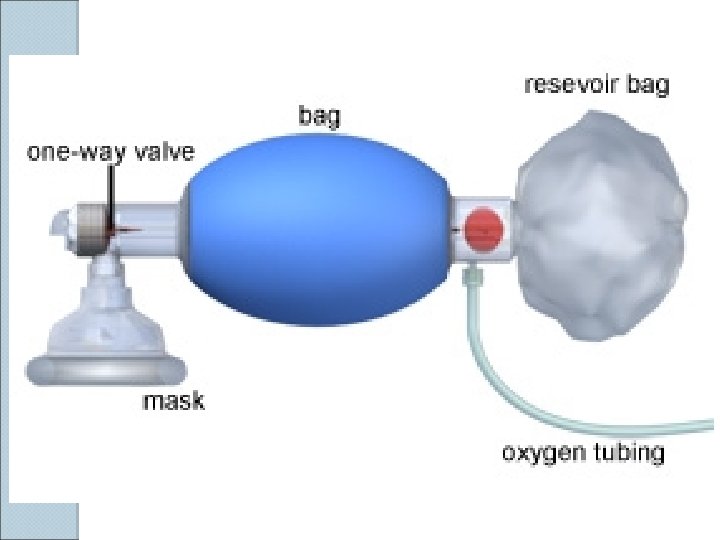
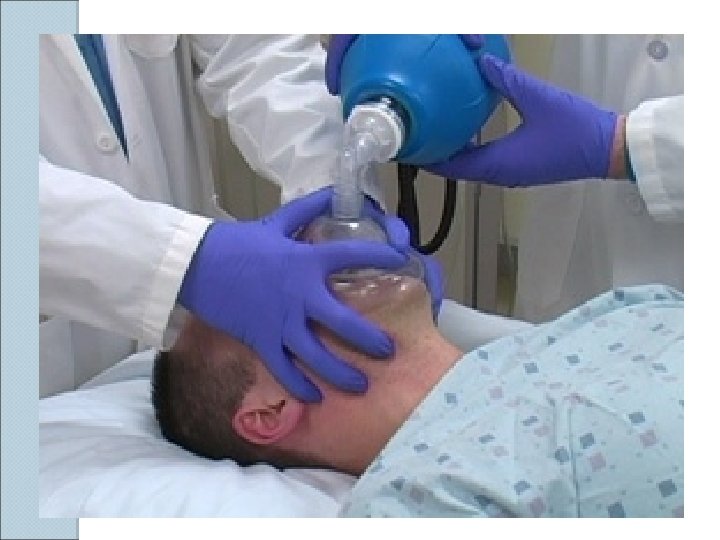
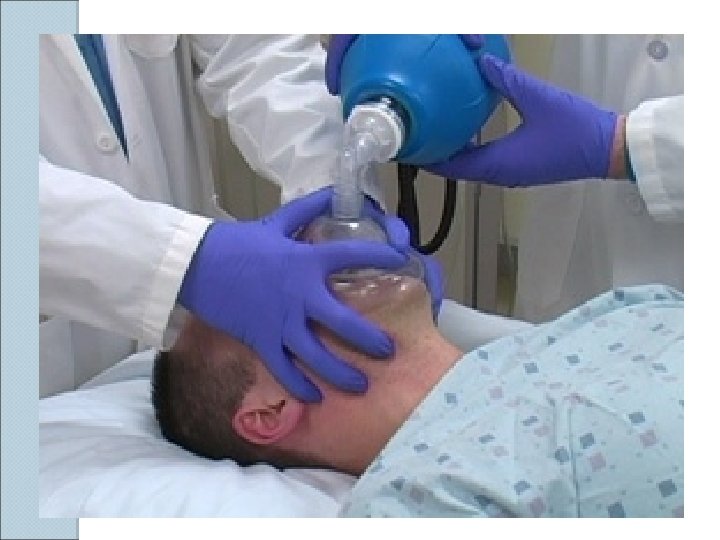
BVM Ventilation The most important airway skill Always the first response to inadequate oxygenation and ventilation The first “bail-out” maneuver to a failed intubation attempt Attenuates the urgency to intubate
Golden Rules of Bagging “ Anybody ( almost ) can be oxygenated and ventilated with a bag and a mask “ The art of bagging should be mastered before the art of intubation Manual ventilation skill with proper equipment is a fundamental premise of advanced airway


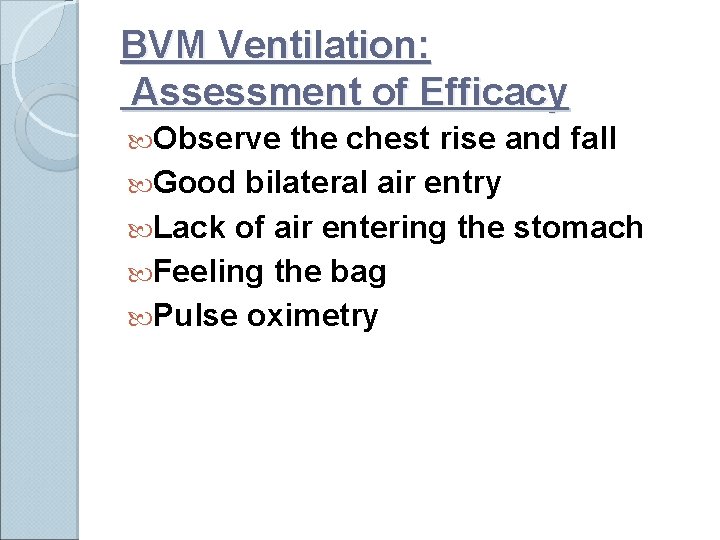
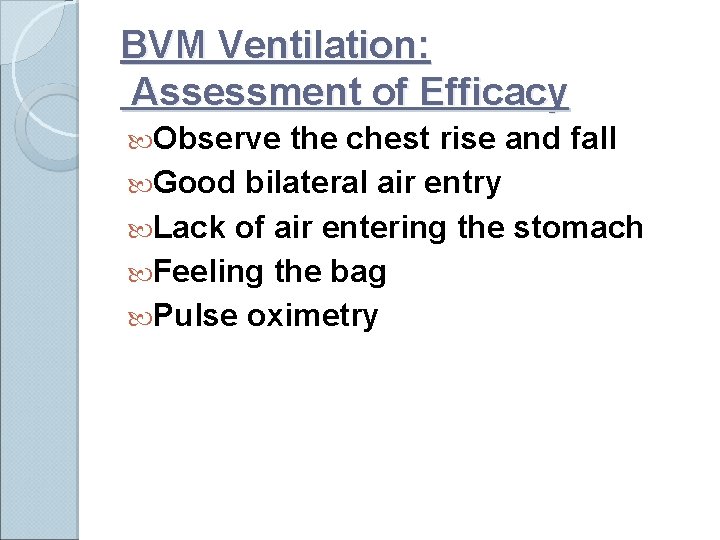
BVM Ventilation: Assessment of Efficacy Observe the chest rise and fall Good bilateral air entry Lack of air entering the stomach Feeling the bag Pulse oximetry
Predictors of difficult face mask ventilation 1 - age>55 years 2 -body mass index>26 Kg/m 2 3 -a beard 4 -lack of teeth 4 -a history of snoring

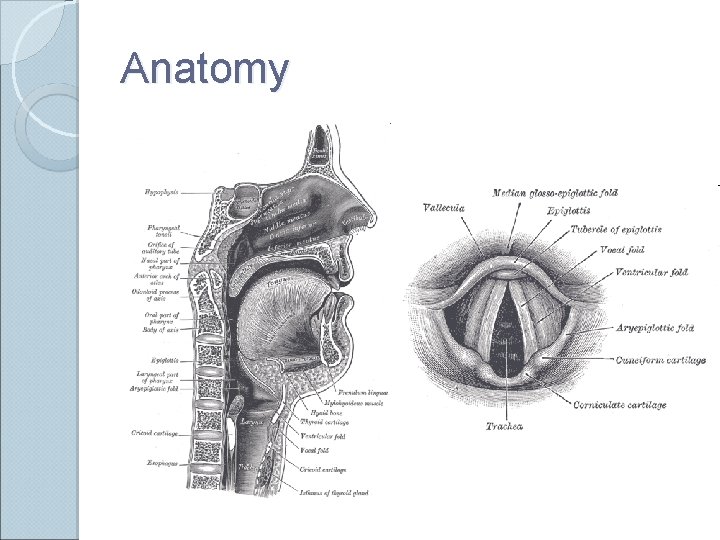
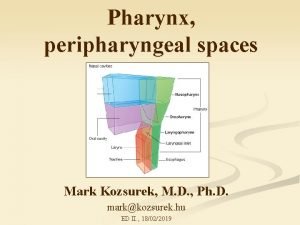
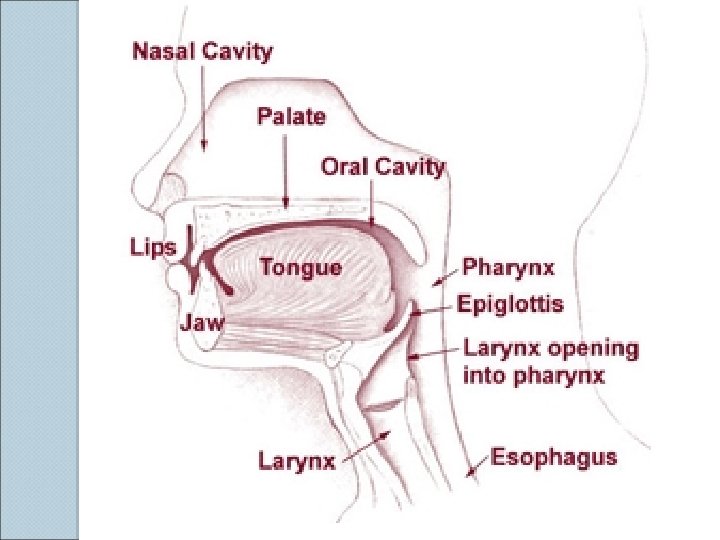
Anatomy
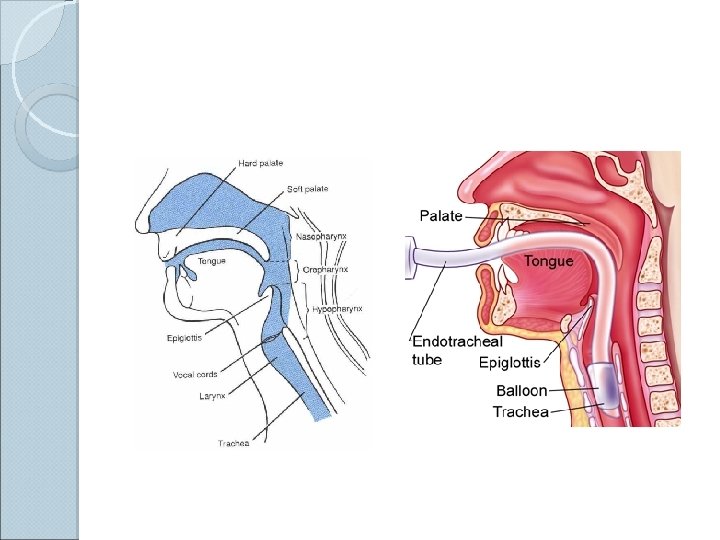
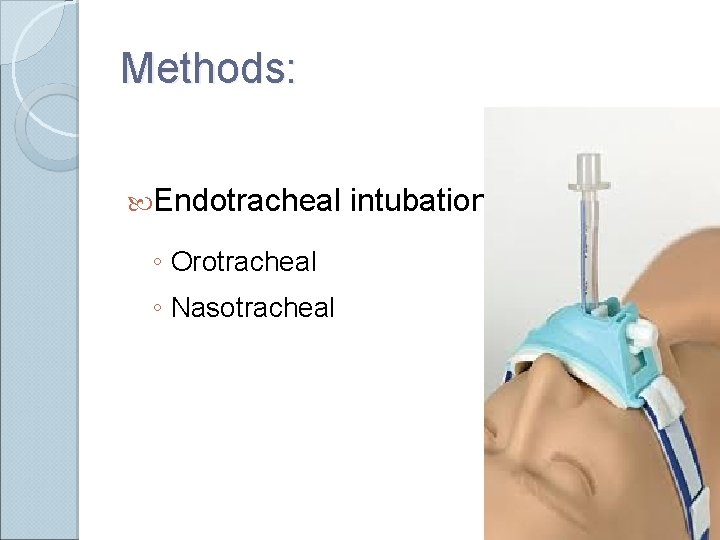
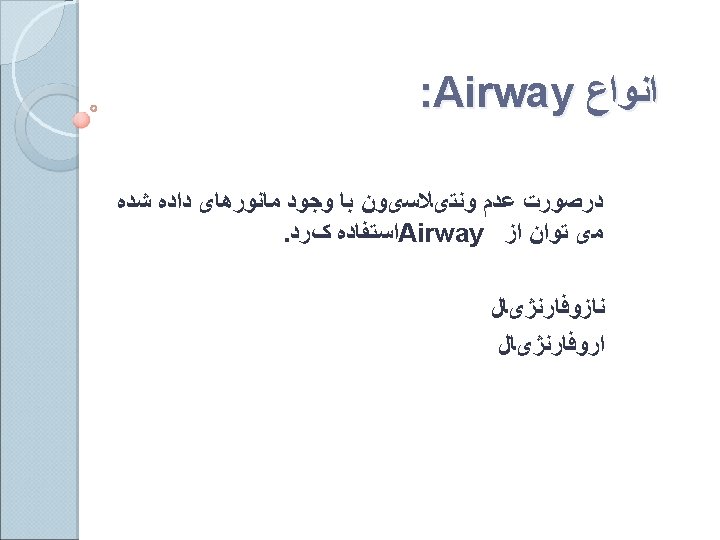
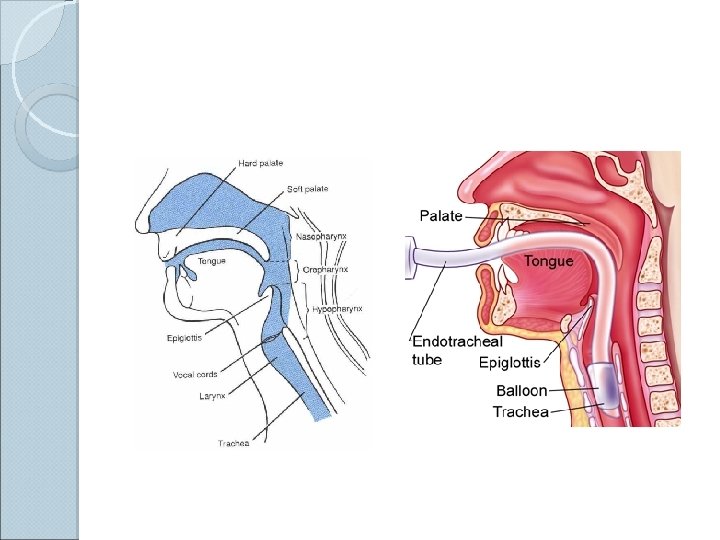
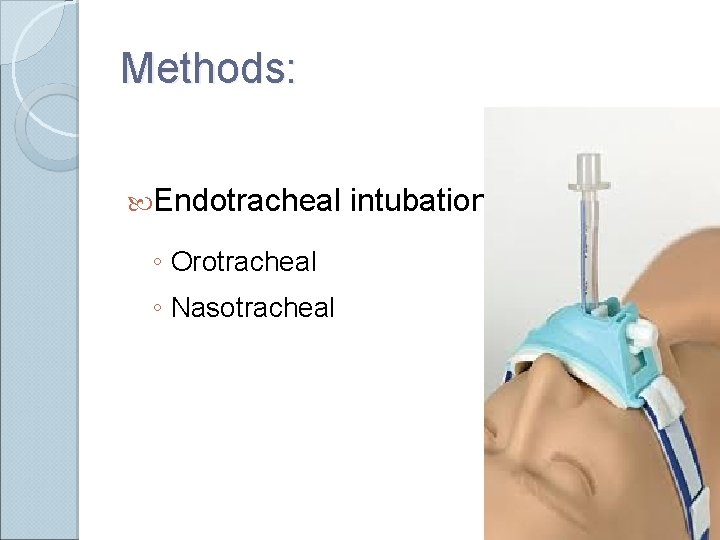
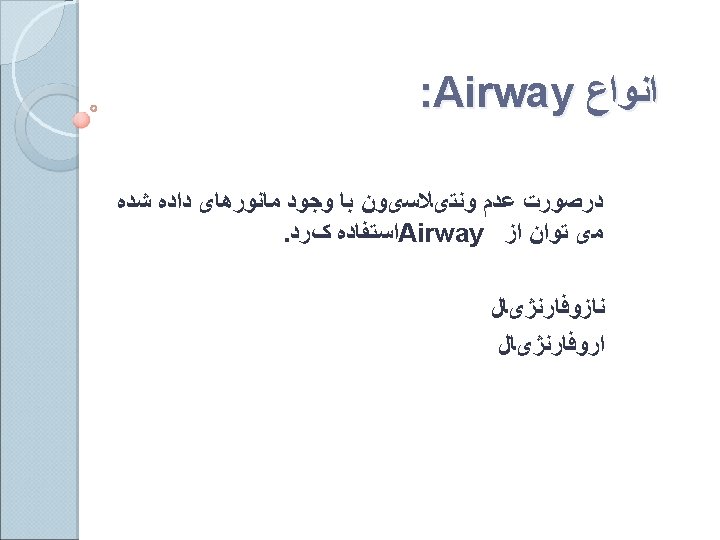
Methods: Endotracheal ◦ Orotracheal ◦ Nasotracheal intubation
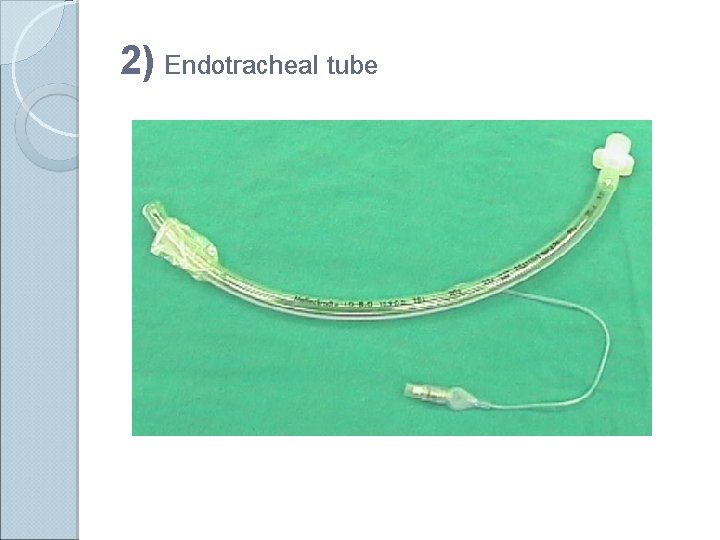
Endotracheal Intubation Placement of a flexible plastic tube into the trachea to: ◦ maintain an open airway, ◦ serve as a conduit through which to administer certain drugs. Is performed in critically injured, ill or anesthetized patients: ◦ to facilitate ventilation of the lungs, including mechanical ventilation, ◦ to prevent the possibility of asphyxiation or airway obstruction.
Indications: For supporting ventilation in patient with pathologic disease: ◦ Upper airway obstruction, ◦ Respiratory failure, ◦ Loss of consciousness For supporting ventilation during general anaesthesia: ◦ Type of surgery: Operative site near the airway, Thoracic or abdominal surgery, Prone or lateral surgery, Long period of surgery Patient has risk of pulmonary aspiration Difficult mask ventilation
BASIC AIRWAY EVALUATION Previous anaesthetic problems and general appearance of the patient. 2. Neck, face, maxilla and mandible with jaw movements. 3. Head extension and movements, teeth, oropharanx and soft tissue of the neck. 1.
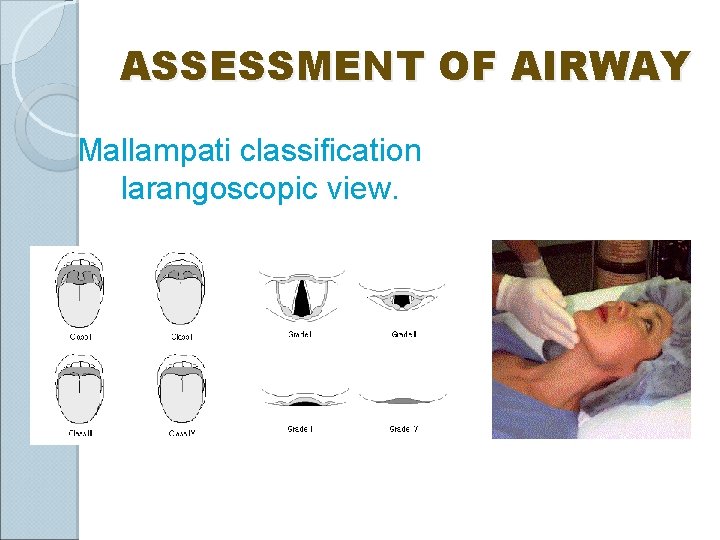
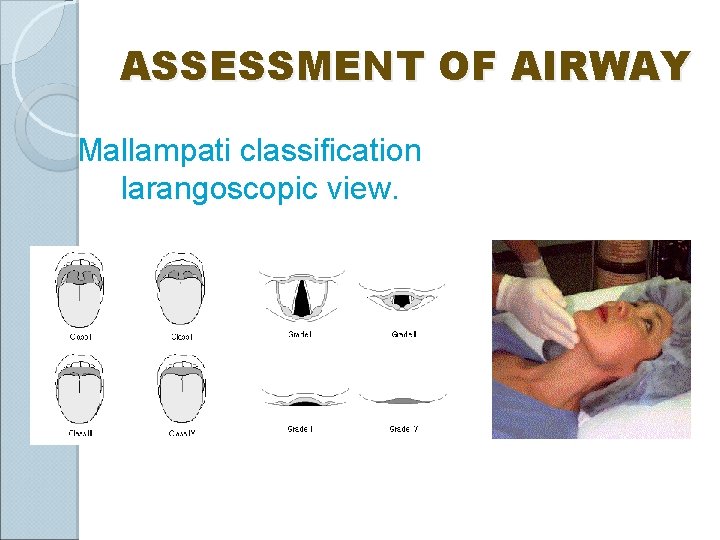
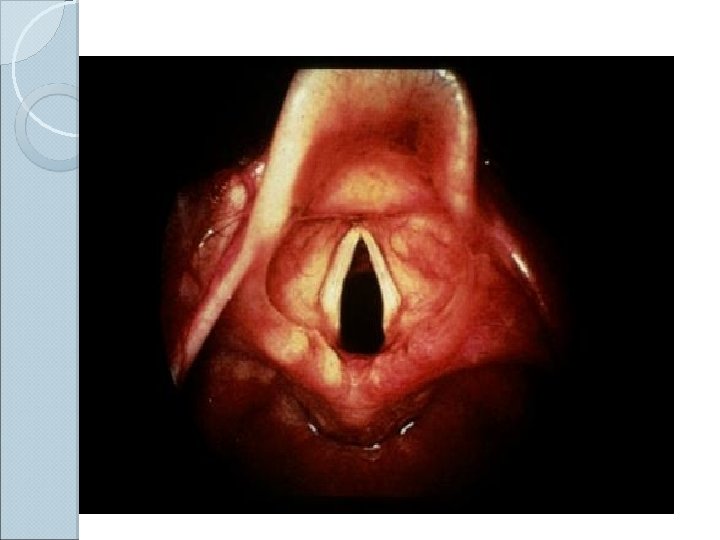
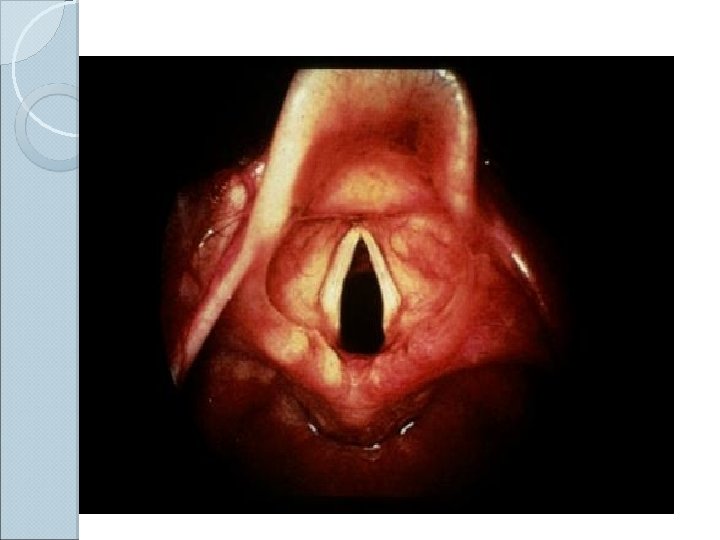
ASSESSMENT OF AIRWAY Mallampati classification larangoscopic view.
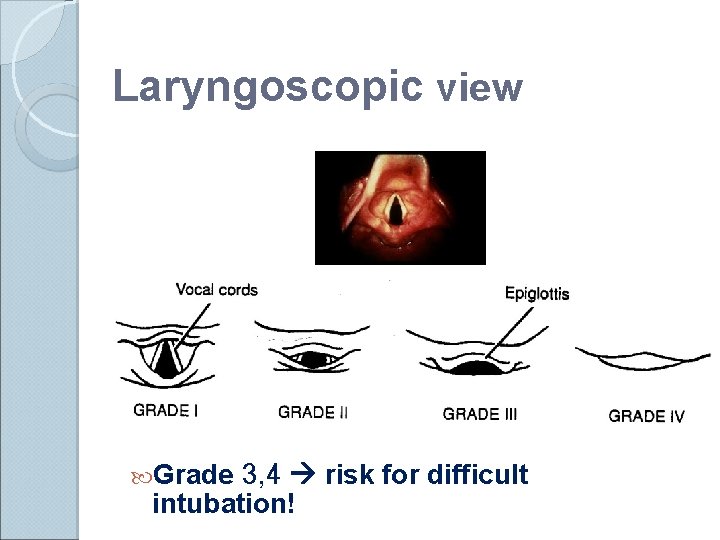
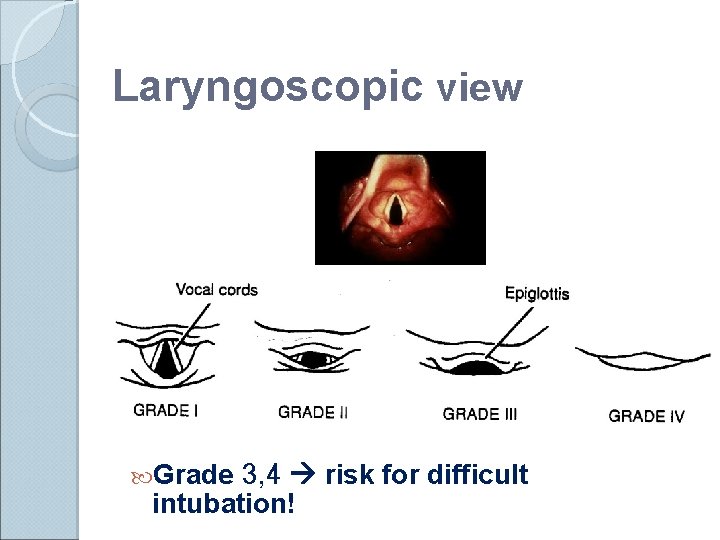
Laryngoscopic view Grade 3, 4 risk for difficult intubation!
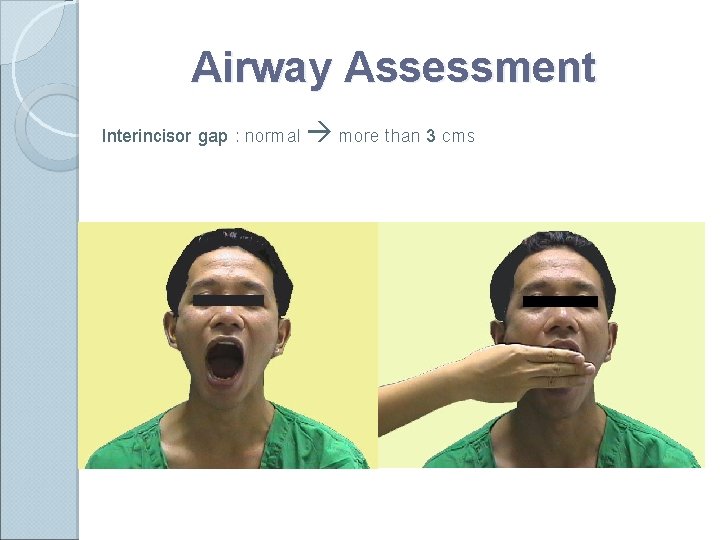
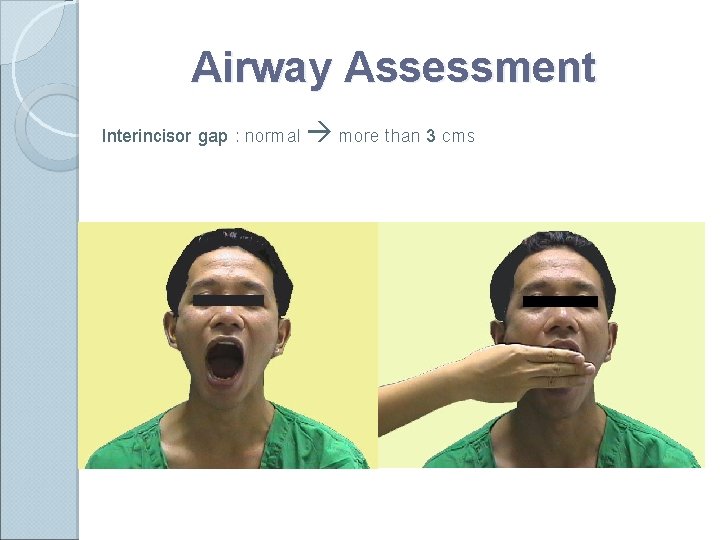
Airway Assessment Interincisor gap : normal more than 3 cms
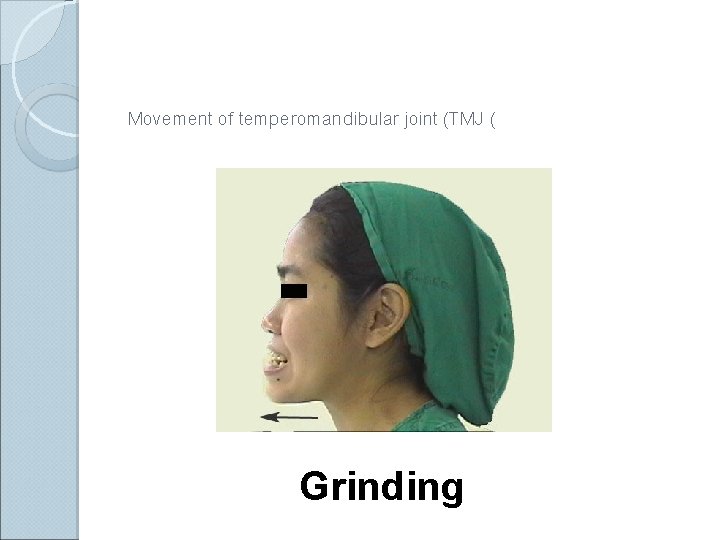
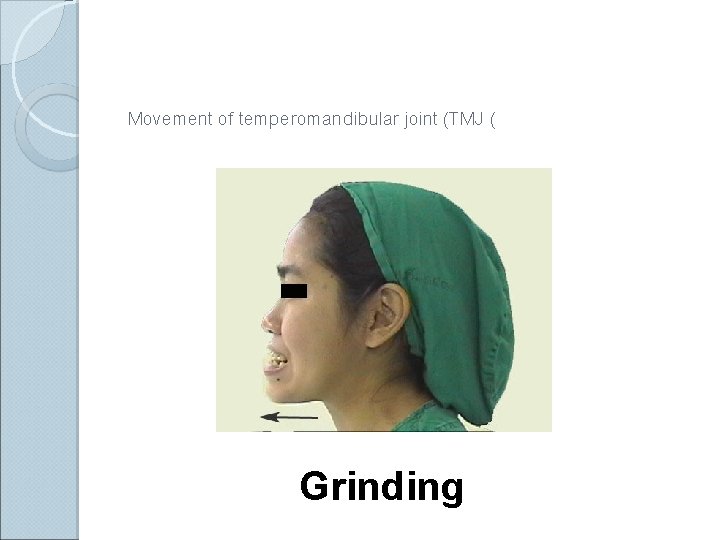
Movement of temperomandibular joint (TMJ ( Grinding
Airway Assessment 1) Condition intubation: that associated with difficult Congenital anomalies Pierre Robin syndrome , Down’s syndrome Infection in airway Retropharyngeal abscess, Epiglottitis Tumor in oral cavity or larynx Enlarge thyroid gland trachea shift to lateral or compressed tracheal lumen
Continuation. . . Maxillofacial , cervical or laryngeal trauma Temperomandibular joint dysfunction Burn scar at face and neck Morbidly obese or pregnancy
Anatomical factors affecting Larangoscopy 1. 2. 3. 4. 5. Short Neck. Protruding incisor teeth. Long high arched palate. Poor mobility of neck. Increase in either anterior depth or Posterior depth of the mandible decrease in Atlanto Occipital distance that's why role of Radiology has increased in our specialty

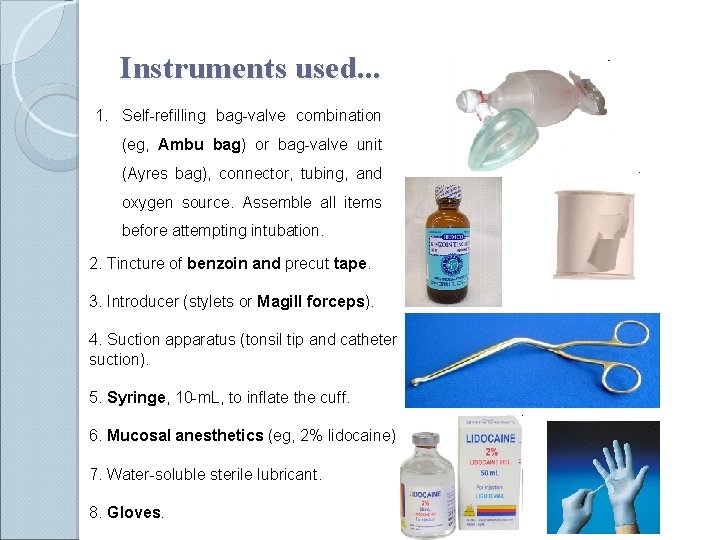
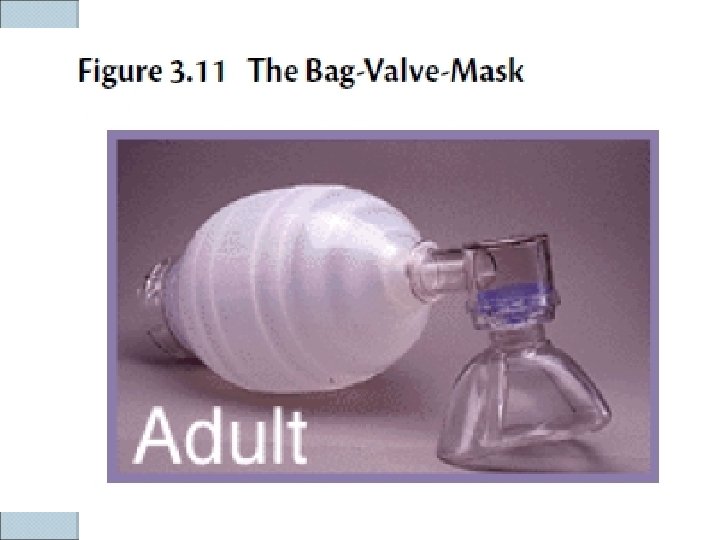
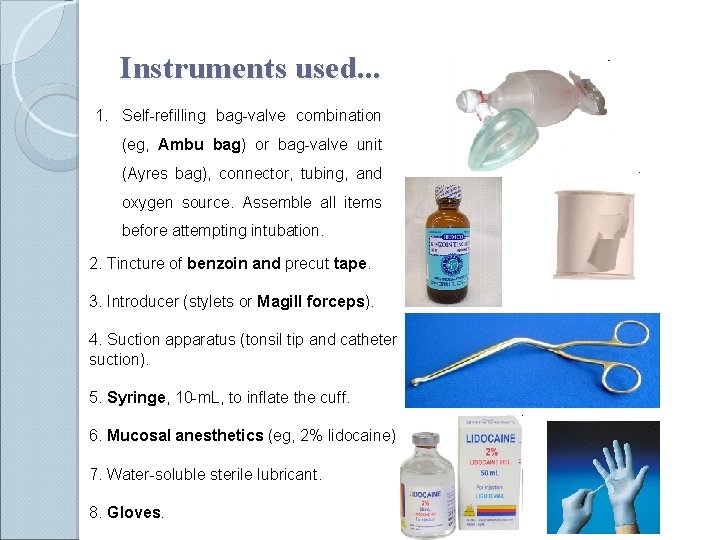
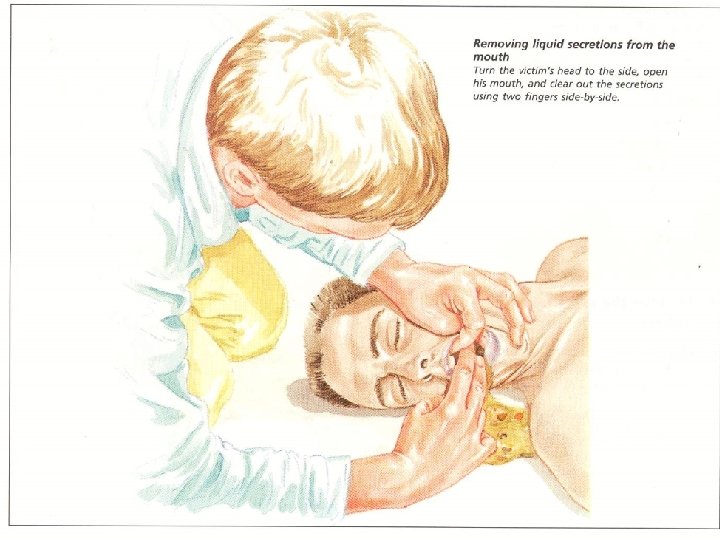
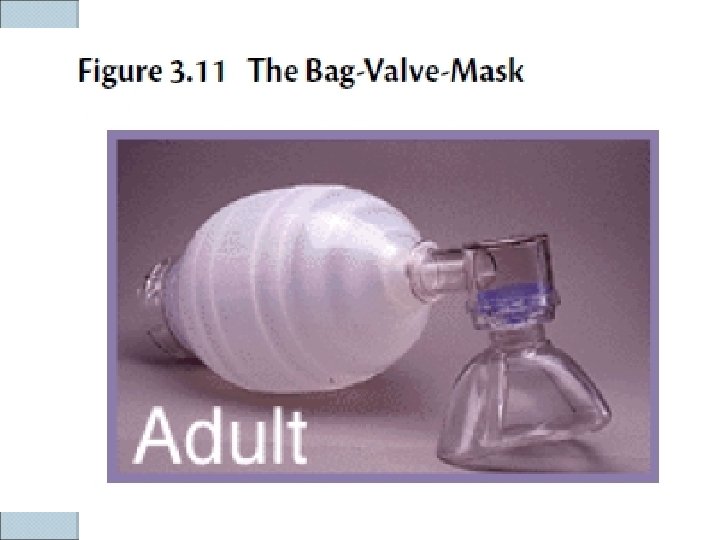
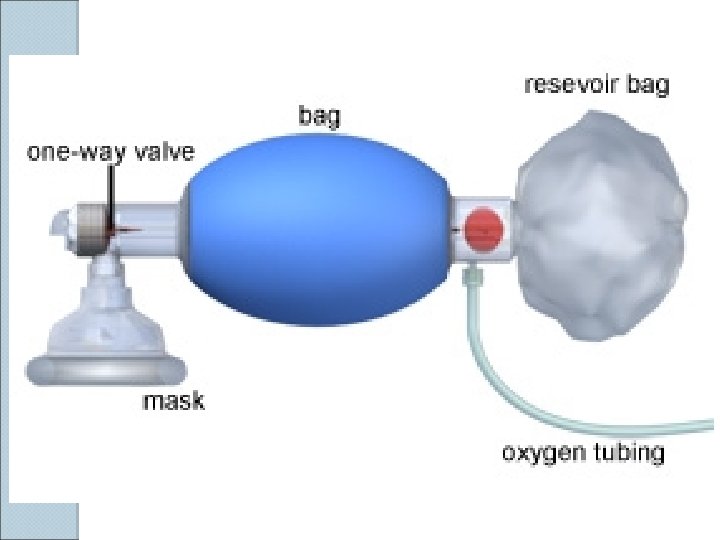
Instruments used. . . 1. Self-refilling bag-valve combination (eg, Ambu bag) or bag-valve unit (Ayres bag), connector, tubing, and oxygen source. Assemble all items before attempting intubation. 2. Tincture of benzoin and precut tape. 3. Introducer (stylets or Magill forceps). 4. Suction apparatus (tonsil tip and catheter suction). 5. Syringe, 10 -m. L, to inflate the cuff. 6. Mucosal anesthetics (eg, 2% lidocaine) 7. Water-soluble sterile lubricant. 8. Gloves.
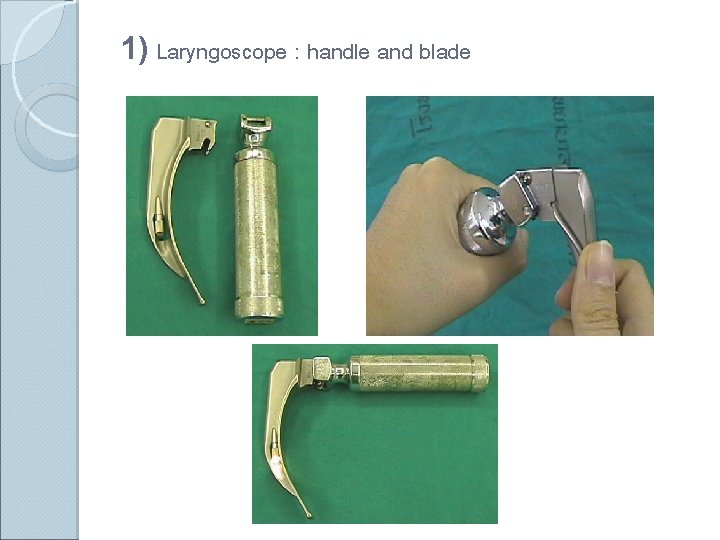
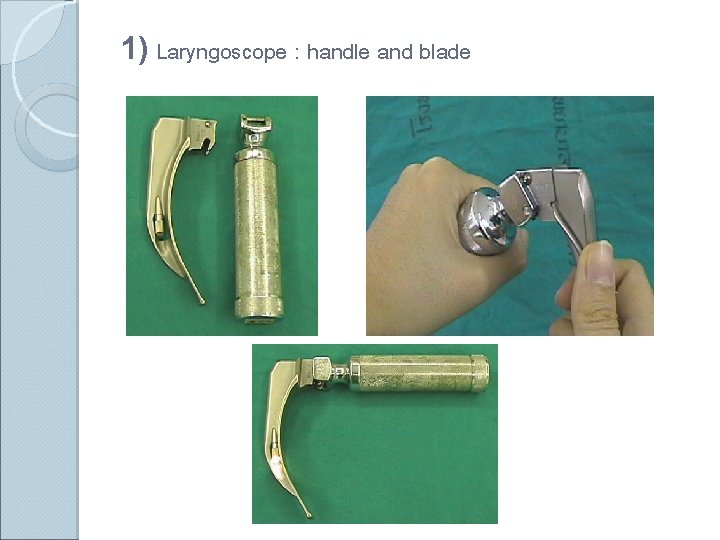
1) Laryngoscope : handle and blade

LARYNGOSCOPIC BLADE F Macintosh (curved) and Miller (straight) blade F Adult : Macintosh blade, small children : Miller blade Macintosh blade
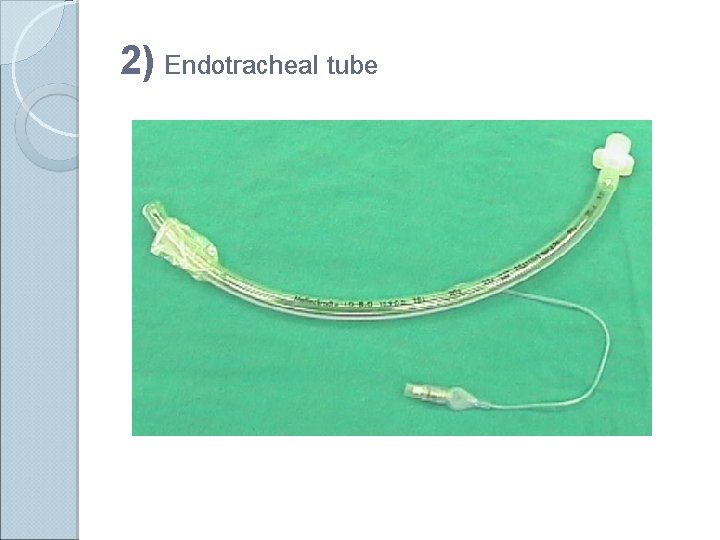
2) Endotracheal tube
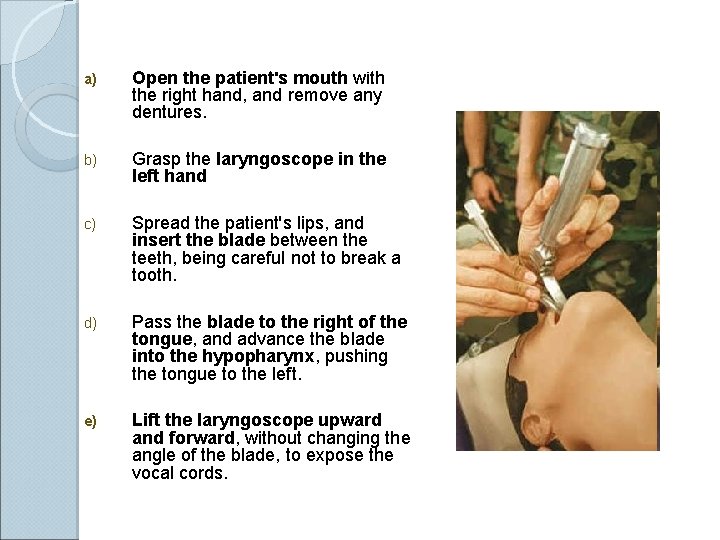
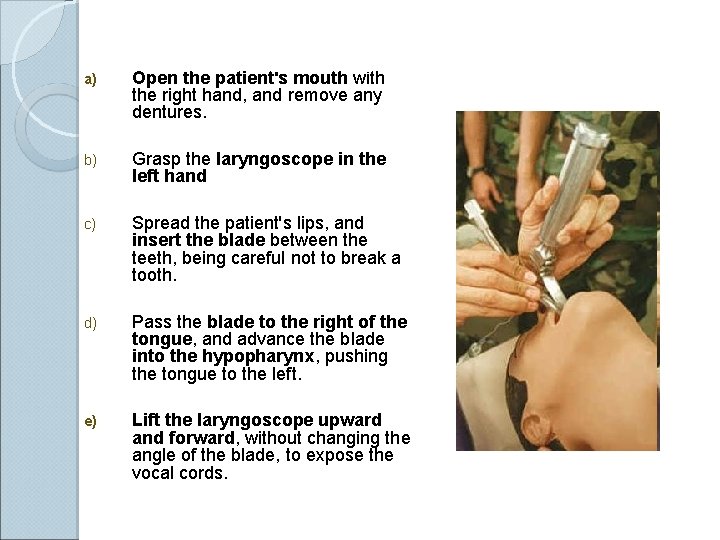
Curved blade technique a) Open the patient's mouth with the right hand, and remove any dentures. b) Grasp the laryngoscope in the left hand c) Spread the patient's lips, and insert the blade between the teeth, being careful not to break a tooth. d) Pass the blade to the right of the tongue, and advance the blade into the hypopharynx, pushing the tongue to the left. e) Lift the laryngoscope upward and forward, without changing the angle of the blade, to expose the vocal cords.
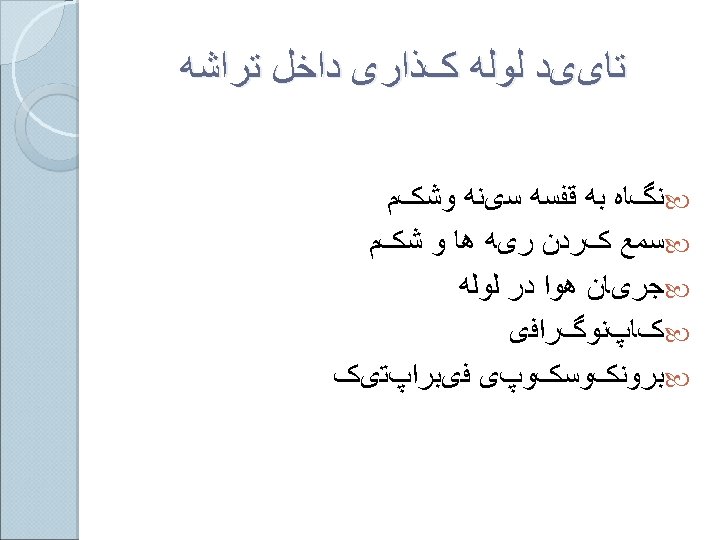
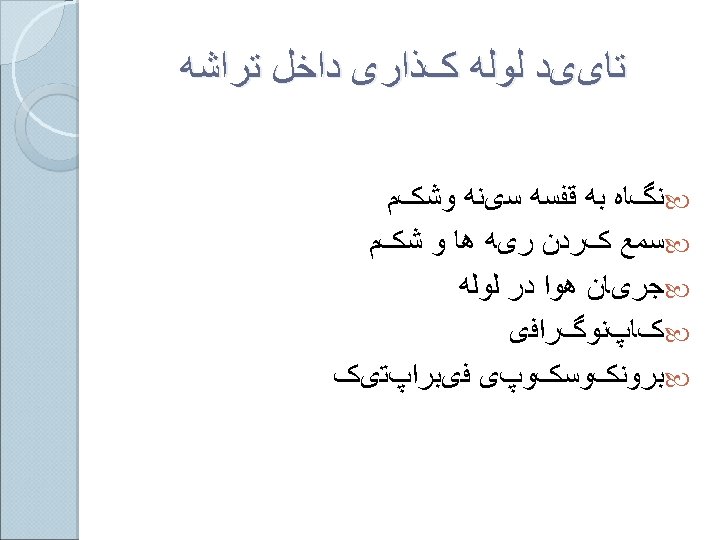
Nasoendotracheal intubation F Advantages: (1 Comfortable for prolong intubation in postoperative period (2 Suitable for oral surgery : tonsillectomy , mandible surgery (3 For blind nasal intubation (4 Can take oral feeding (5 Resist for kinking and difficult to accidental extubation Disadvantages: (1 Trauma to nasal mucosa (2 Risk for sinusitis in prolong intubation (3 Risk for bacteremia (4 Smaller diameter than oral route difficult for suction

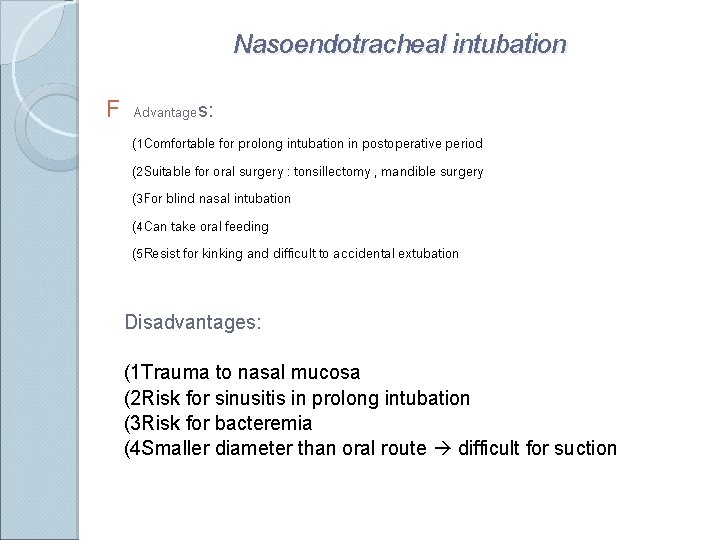
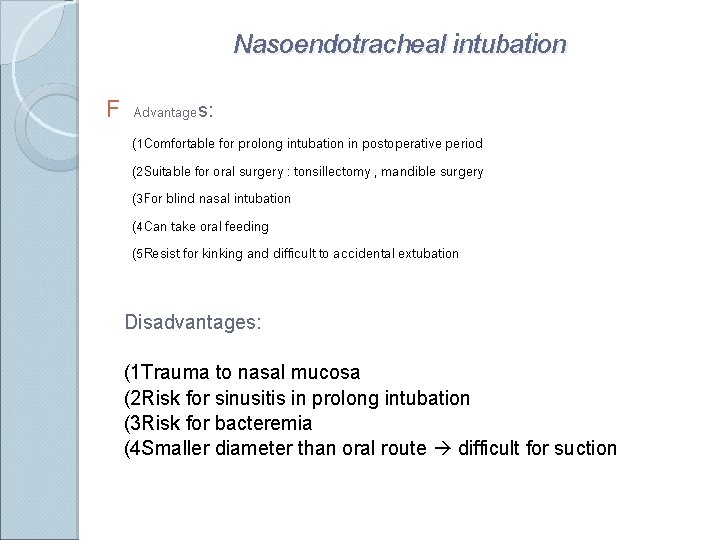
Contraindication for nasoendotracheal intubation (1 Fracture base of skull (2 Coagulopathy (3 Nasal cavity obstruction (4 Retropharyngeal abscess
Complication of endotracheal intubation 1) During intubation 2) During remained intubation 3) During extubation 4) After extubation
(1 During intubation Trauma to lip, tongue or teeth Hypertension and tachycardia or arrhythmia Pulmonary aspiration Laryngospasm Bronchospasm Laryngeal edema Arytenoid dislocation hoarseness Increased intracranial pressure Spinal cord trauma in cervical spine injury Esophageal intubation
2) During remained intubation Obstruction from klinking , secretion or overinflation of cuff Accidental extubation or endobronchial intubation Disconnection from breathing circuit Pulmonary aspiration Lib or nasal ulcer in case with prolong period of intubation Sinusitis or otitis in case with prolong nasoendotracheal intubation 3) During Extubation • Laryngospasm • Pulmonary aspiration • Edema of upper airway
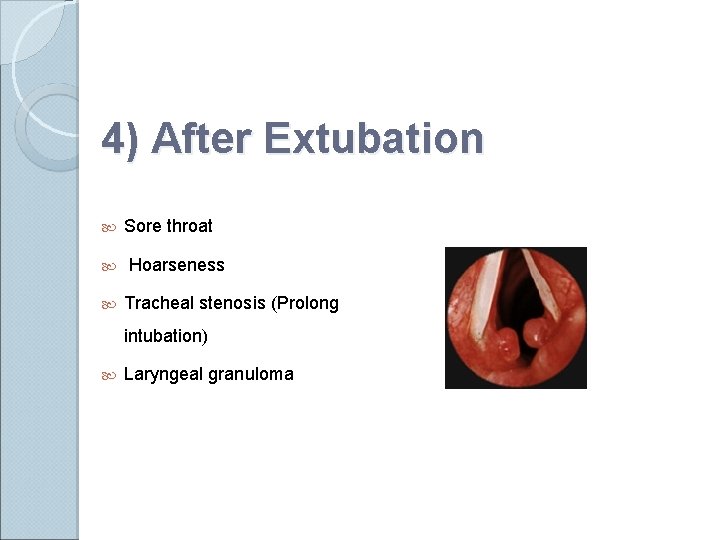
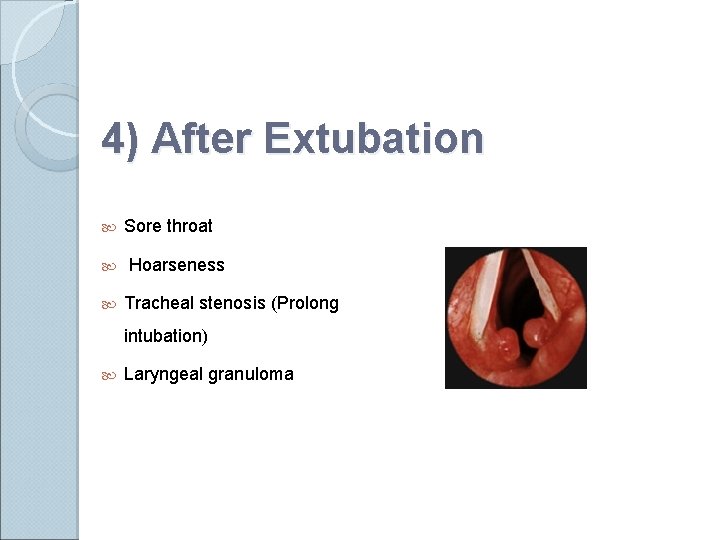
4) After Extubation Sore throat Hoarseness Tracheal stenosis (Prolong intubation) Laryngeal granuloma
Thanks for your attention!
 Upper airway and lower airway
Upper airway and lower airway Upper respiratory tract labeled
Upper respiratory tract labeled Ticls
Ticls Respi
Respi Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Taste buds on cheeks
Taste buds on cheeks Cricoid cartilage
Cricoid cartilage Sinus
Sinus Divisions of larynx
Divisions of larynx Larynx dissection
Larynx dissection Turban epiglottis meaning
Turban epiglottis meaning Floppy larynx baby
Floppy larynx baby Epiglottis
Epiglottis Primary bronchus
Primary bronchus Internal and external nares
Internal and external nares Intubation airway anatomy
Intubation airway anatomy Open the airway
Open the airway Endotracheal intubation
Endotracheal intubation Thin
Thin Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Respiratory zone
Respiratory zone Venous drainage of the upper limb
Venous drainage of the upper limb Airway management acls
Airway management acls Chapter 10 airway management
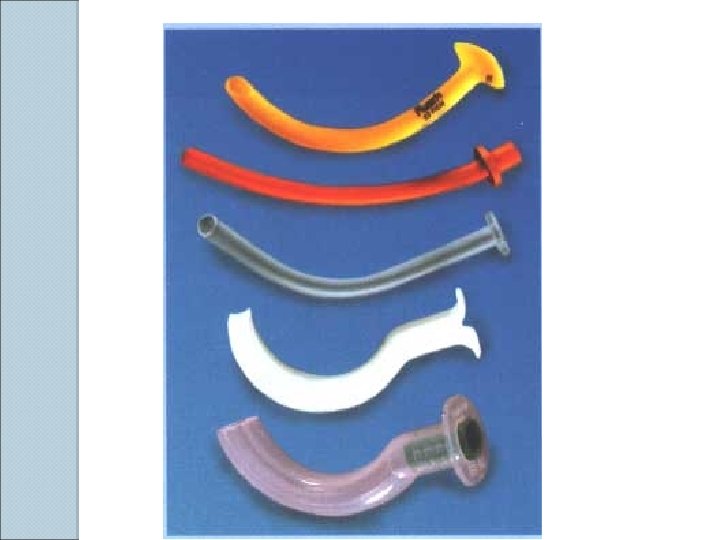
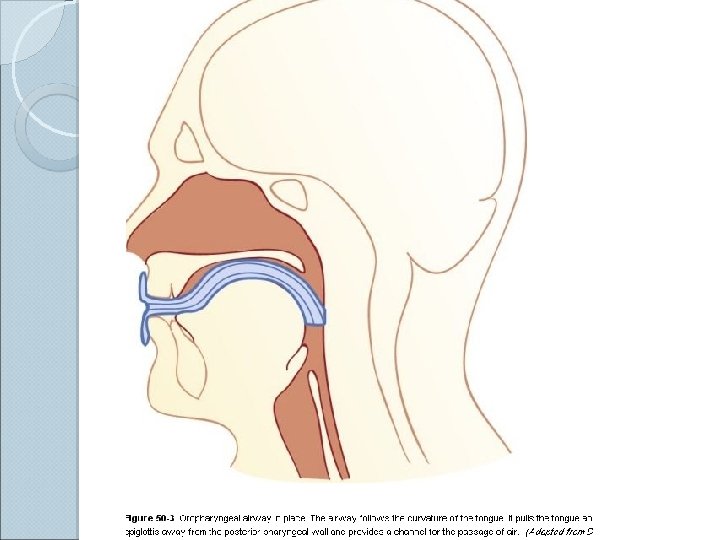
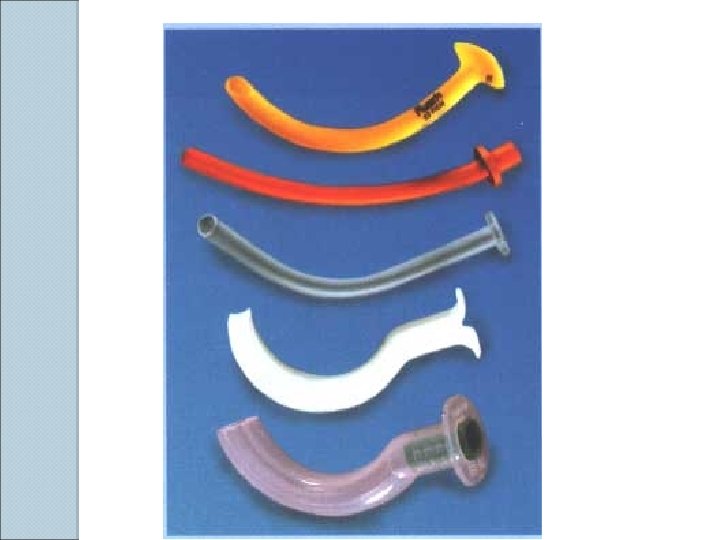
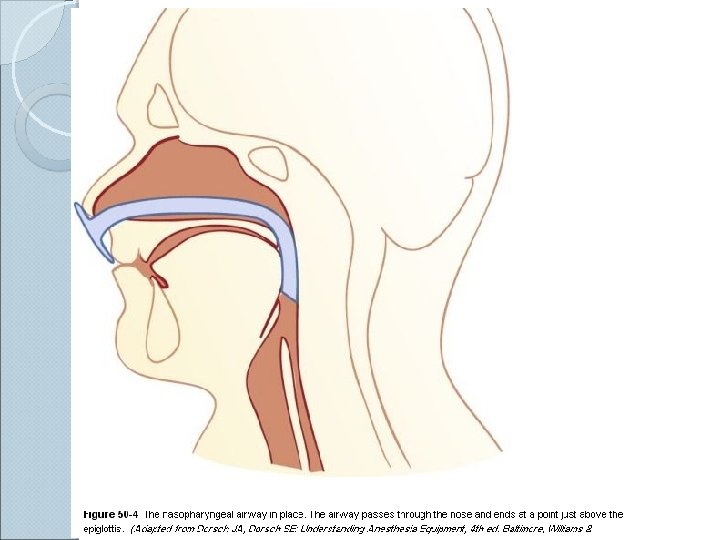
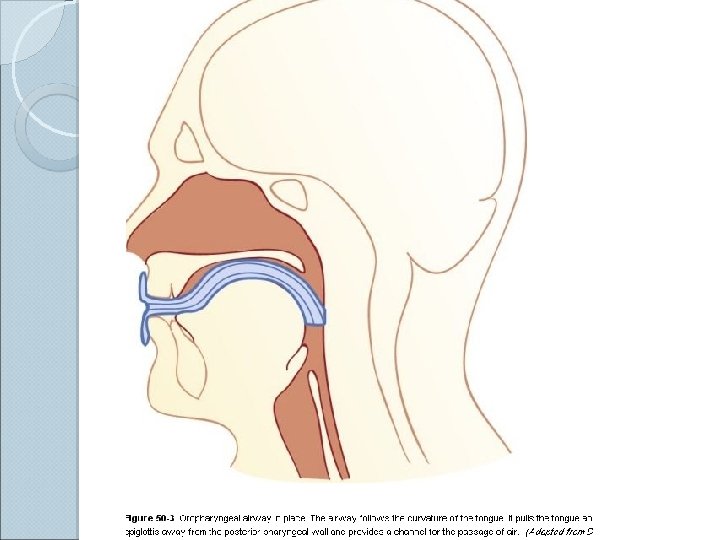
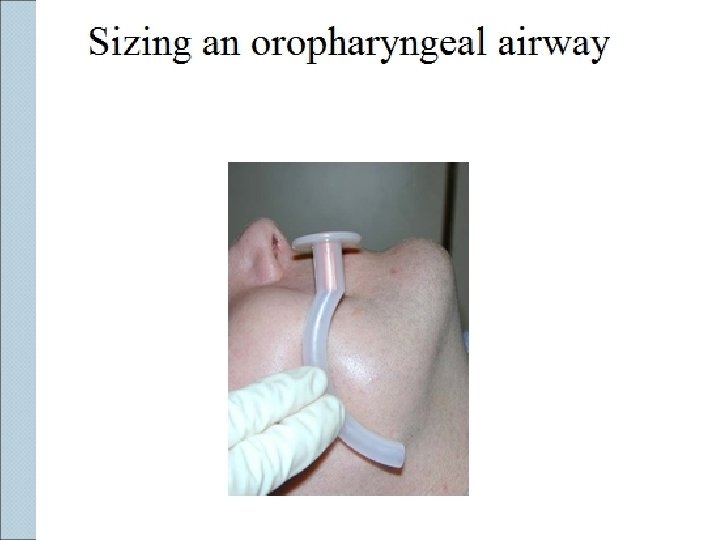
Chapter 10 airway management Opa and npa
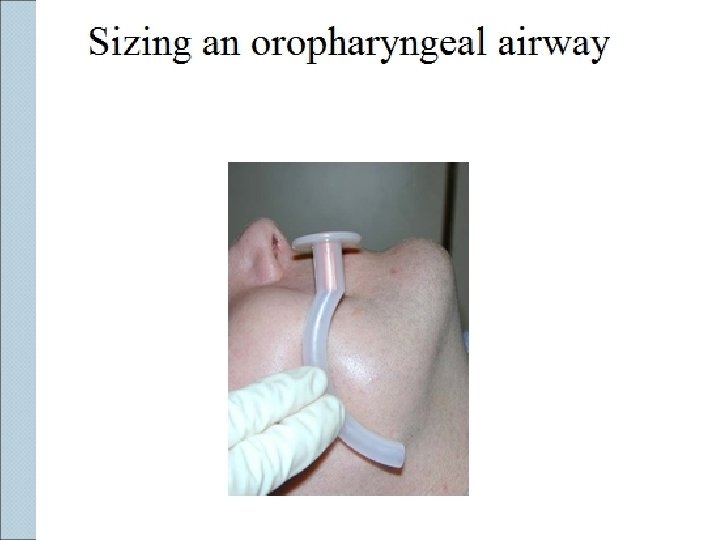
Opa and npa Npa measurement
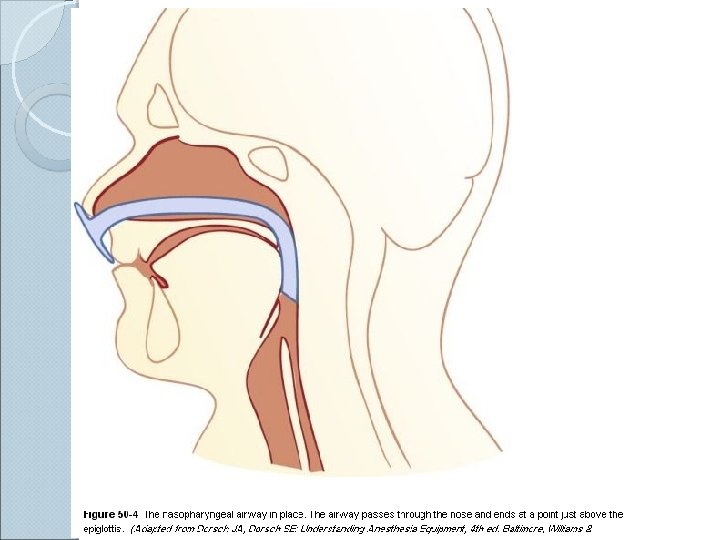
Npa measurement Basic airway management equipment
Basic airway management equipment Sandwich manuver adalah
Sandwich manuver adalah Stepwise approach to airway management
Stepwise approach to airway management Pars chondropharyngea
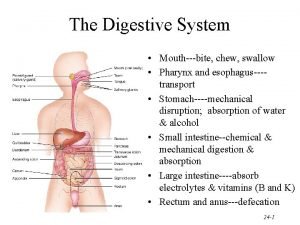
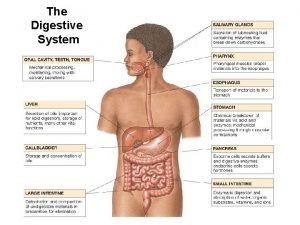
Pars chondropharyngea Digestive system model
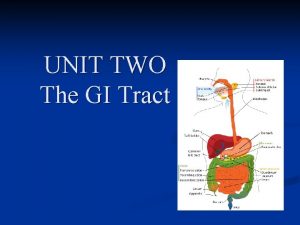
Digestive system model Parts of the pharynx
Parts of the pharynx Pharynx subdivisions
Pharynx subdivisions Microfold
Microfold Post trematic nerve meaning
Post trematic nerve meaning Salpingopharyngeus
Salpingopharyngeus Pyloric orifice function
Pyloric orifice function Horizontal
Horizontal Frog dissection frog scienstructable template colored
Frog dissection frog scienstructable template colored Fornix faringeo
Fornix faringeo Lungs pharynx
Lungs pharynx Physiology of pharynx
Physiology of pharynx Pharynx hiperemija
Pharynx hiperemija Pharyngeal muscles
Pharyngeal muscles Nasal larynx
Nasal larynx Fornix gaster
Fornix gaster Buonator
Buonator Development of respiratory system
Development of respiratory system The parts of the respiratory system
The parts of the respiratory system Choncae
Choncae Food in pharynx
Food in pharynx Muscular pharynx
Muscular pharynx Pharynx
Pharynx Pharynx food pipe
Pharynx food pipe Large intestine histology
Large intestine histology Pharynx food pipe
Pharynx food pipe Pharyngeal vein
Pharyngeal vein Pathway of food from mouth to anus
Pathway of food from mouth to anus Cardiac sphincter
Cardiac sphincter Function of pharynx
Function of pharynx Hemicapsule
Hemicapsule Pharynx
Pharynx Upper gi bleeding management
Upper gi bleeding management Airway assessment in anaesthesia
Airway assessment in anaesthesia Airway pathway
Airway pathway Respiratory airway secretary
Respiratory airway secretary Modified mallampati
Modified mallampati Nasofaringeal
Nasofaringeal Sigh breaths on jet ventilator
Sigh breaths on jet ventilator Mean airway pressure
Mean airway pressure