Air Particulate Matter Inhalation Causes Alterations to Brain
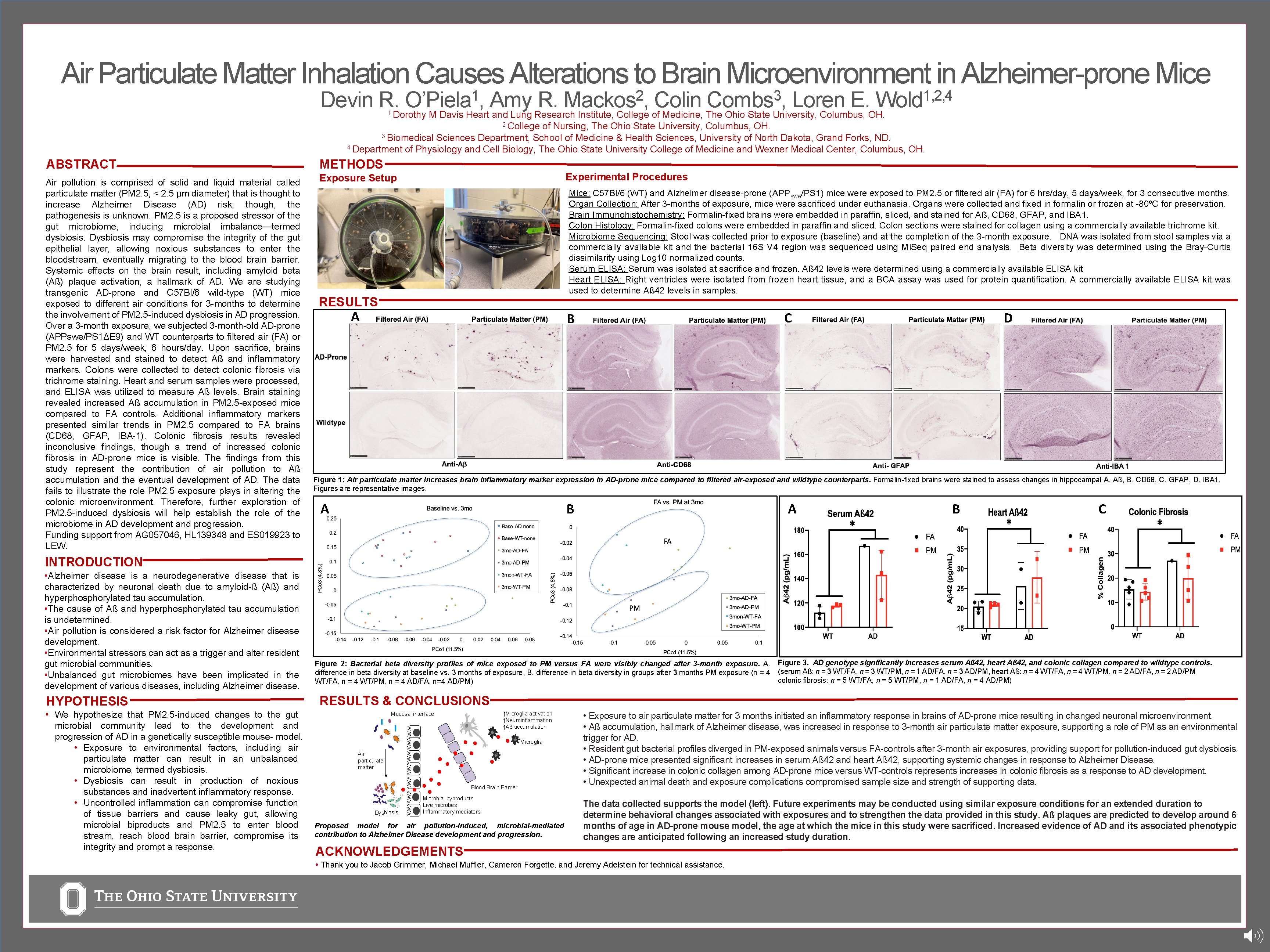
Air Particulate Matter Inhalation Causes Alterations to Brain Microenvironment in Alzheimer-prone Mice 1 O’Piela , Devin R. Dorothy M Davis Heart. Amy R. Colin Loren E. and Lung Research Institute, College of Medicine, The Ohio State University, Columbus, OH. 1 2 Mackos , 3 Combs , 1, 2, 4 Wold 2 College of Nursing, The Ohio State University, Columbus, OH. 3 Biomedical Sciences Department, School of Medicine & Health Sciences, University of North Dakota, Grand Forks, ND. 4 Department of Physiology and Cell Biology, The Ohio State University College of Medicine and Wexner Medical Center, Columbus, OH. ABSTRACT METHODS Air pollution is comprised of solid and liquid material called particulate matter (PM 2. 5, < 2. 5 μm diameter) that is thought to increase Alzheimer Disease (AD) risk; though, the pathogenesis is unknown. PM 2. 5 is a proposed stressor of the gut microbiome, inducing microbial imbalance—termed dysbiosis. Dysbiosis may compromise the integrity of the gut epithelial layer, allowing noxious substances to enter the bloodstream, eventually migrating to the blood brain barrier. Systemic effects on the brain result, including amyloid beta (Aß) plaque activation, a hallmark of AD. We are studying transgenic AD-prone and C 57 Bl/6 wild-type (WT) mice exposed to different air conditions for 3 -months to determine the involvement of PM 2. 5 -induced dysbiosis in AD progression. Over a 3 -month exposure, we subjected 3 -month-old AD-prone (APPswe/PS 1ΔE 9) and WT counterparts to filtered air (FA) or PM 2. 5 for 5 days/week, 6 hours/day. Upon sacrifice, brains were harvested and stained to detect Aß and inflammatory markers. Colons were collected to detect colonic fibrosis via trichrome staining. Heart and serum samples were processed, and ELISA was utilized to measure Aß levels. Brain staining revealed increased Aß accumulation in PM 2. 5 -exposed mice compared to FA controls. Additional inflammatory markers presented similar trends in PM 2. 5 compared to FA brains (CD 68, GFAP, IBA-1). Colonic fibrosis results revealed inconclusive findings, though a trend of increased colonic fibrosis in AD-prone mice is visible. The findings from this study represent the contribution of air pollution to Aß accumulation and the eventual development of AD. The data fails to illustrate the role PM 2. 5 exposure plays in altering the colonic microenvironment. Therefore, further exploration of PM 2. 5 -induced dysbiosis will help establish the role of the microbiome in AD development and progression. Funding support from AG 057046, HL 139348 and ES 019923 to LEW. Exposure Setup Experimental Procedures Mice: C 57 Bl/6 (WT) and Alzheimer disease-prone (APPswe/PS 1) mice were exposed to PM 2. 5 or filtered air (FA) for 6 hrs/day, 5 days/week, for 3 consecutive months. Organ Collection: After 3 -months of exposure, mice were sacrificed under euthanasia. Organs were collected and fixed in formalin or frozen at -80ºC for preservation. Brain Immunohistochemistry: Formalin-fixed brains were embedded in paraffin, sliced, and stained for Aß, CD 68, GFAP, and IBA 1. Colon Histology: Formalin-fixed colons were embedded in paraffin and sliced. Colon sections were stained for collagen using a commercially available trichrome kit. Microbiome Sequencing: Stool was collected prior to exposure (baseline) and at the completion of the 3 -month exposure. DNA was isolated from stool samples via a commercially available kit and the bacterial 16 S V 4 region was sequenced using Mi. Seq paired end analysis. Beta diversity was determined using the Bray-Curtis dissimilarity using Log 10 normalized counts. Serum ELISA: Serum was isolated at sacrifice and frozen. Aß 42 levels were determined using a commercially available ELISA kit Heart ELISA: Right ventricles were isolated from frozen heart tissue, and a BCA assay was used for protein quantification. A commercially available ELISA kit was used to determine Aß 42 levels in samples. RESULTS A C B D – Figure 1: Air particulate matter increases brain inflammatory marker expression in AD-prone mice compared to filtered air-exposed and wildtype counterparts. Formalin-fixed brains were stained to assess changes in hippocampal A. Aß, B. CD 68, C. GFAP, D. IBA 1. Figures are representative images. B A A B C INTRODUCTION • Alzheimer disease is a neurodegenerative disease that is characterized by neuronal death due to amyloid-ß (Aß) and hyperphosphorylated tau accumulation. • The cause of Aß and hyperphosphorylated tau accumulation is undetermined. • Air pollution is considered a risk factor for Alzheimer disease development. • Environmental stressors can act as a trigger and alter resident gut microbial communities. • Unbalanced gut microbiomes have been implicated in the development of various diseases, including Alzheimer disease. HYPOTHESIS • We hypothesize that PM 2. 5 -induced changes to the gut microbial community lead to the development and progression of AD in a genetically susceptible mouse- model. • Exposure to environmental factors, including air particulate matter can result in an unbalanced microbiome, termed dysbiosis. • Dysbiosis can result in production of noxious substances and inadvertent inflammatory response. • Uncontrolled inflammation can compromise function of tissue barriers and cause leaky gut, allowing microbial biproducts and PM 2. 5 to enter blood stream, reach blood brain barrier, compromise its integrity and prompt a response. Figure 2: Bacterial beta diversity profiles of mice exposed to PM versus FA were visibly changed after 3 -month exposure. A. difference in beta diversity at baseline vs. 3 months of exposure, B. difference in beta diversity in groups after 3 months PM exposure (n = 4 WT/FA, n = 4 WT/PM, n = 4 AD/FA, n=4 AD/PM) Figure 3. AD genotype significantly increases serum Aß 42, heart Aß 42, and colonic collagen compared to wildtype controls. (serum Aß: n = 3 WT/FA, n = 3 WT/PM, n = 1 AD/FA, n = 3 AD/PM, heart Aß: n = 4 WT/FA, n = 4 WT/PM, n = 2 AD/FA, n = 2 AD/PM colonic fibrosis: n = 5 WT/FA, n = 5 WT/PM, n = 1 AD/FA, n = 4 AD/PM) RESULTS & CONCLUSIONS ↑Microglia activation ↑Neuroinflammation ↑Aβ accumulation Mucosal interface Microglia Air particulate matter Blood Brain Barrier Dysbiosis Microbial byproducts Live microbes Inflammatory mediators Proposed model for air pollution-induced, microbial-mediated contribution to Alzheimer Disease development and progression. • Exposure to air particulate matter for 3 months initiated an inflammatory response in brains of AD-prone mice resulting in changed neuronal microenvironment. • Aß accumulation, hallmark of Alzheimer disease, was increased in response to 3 -month air particulate matter exposure, supporting a role of PM as an environmental trigger for AD. • Resident gut bacterial profiles diverged in PM-exposed animals versus FA-controls after 3 -month air exposures, providing support for pollution-induced gut dysbiosis. • AD-prone mice presented significant increases in serum Aß 42 and heart Aß 42, supporting systemic changes in response to Alzheimer Disease. • Significant increase in colonic collagen among AD-prone mice versus WT-controls represents increases in colonic fibrosis as a response to AD development. • Unexpected animal death and exposure complications compromised sample size and strength of supporting data. The data collected supports the model (left). Future experiments may be conducted using similar exposure conditions for an extended duration to determine behavioral changes associated with exposures and to strengthen the data provided in this study. Aß plaques are predicted to develop around 6 months of age in AD-prone mouse model, the age at which the mice in this study were sacrificed. Increased evidence of AD and its associated phenotypic changes are anticipated following an increased study duration. ACKNOWLEDGEMENTS • Thank you to Jacob Grimmer, Michael Muffler, Cameron Forgette, and Jeremy Adelstein for technical assistance.
- Slides: 1