AHAASA Scientific Statement RaceEthnic Disparities in Stroke Care




- Slides: 27

AHA/ASA Scientific Statement Race-Ethnic Disparities in Stroke Care: The American Experience 0
A Statement for Healthcare Professionals from the AHA/ASA Writing Committee Salvador Cruz-Flores, MD, MPH, FAHA, Chair Jose Biller, MD, FAHA Patrick Griffith, MD George Howard, Ph. D, FAHA Lewis B. Morgenstern, MD, FAHA Eric Peterson, MD, MPH, FAHA Brian Trimble, MD © 2011 American Heart Association, Inc. All rights reserved Alejandro Rabinstein, MD, Vice-Chair Mitchell S. V. Elkind, MD, MS Philip B. Gorelick, MD, MPH, FAHA Enrique C. Leira, MD, MS, FAHA Bruce Ovbiagele, MD, MS, FAHA Wayne Rosamond, Ph. D, MS, FAHA Amy L. Valderrama, Ph. D, RN Cruz-Flores Published online May 26, 2011 1
Slide Set developed by: Aaron Anderson MD Member Stroke Council Professional Education Science Sub-Committee © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011
Purpose • Describe the effect of race and ethnicity on stroke epidemiology, personal beliefs, access to care, response to treatment, and participation in clinical research • Determine the state of knowledge on factors that may explain disparities in stroke care • Identify gaps in knowledge to guide future research © 2011 American Heart Association, Inc. All rights reserved. Cruz-Flores et al. Published online in Stroke May 26, 2011 3
Methods • Members appointed by the AHA Stroke Council Scientific Statement Oversight Committee (SOC) • Reviewed relevant literature with emphasis on reports published since 1972 • Peer reviewed and final approval by the AHA Science Advisory and Coordinating Committee (SACC) © 2011 American Heart Association, Inc. All rights reserved. Cruz-Flores et al. Published online in Stroke May 26, 2011 4
I. Introduction: Background • Racial and ethnic minorities 28% of the US population; expected 40% by 2030 • Striking lifespan disparities between different racial-ethnic groups in the US – 86. 7 Asian women to 61. 7 African American men • Cardiovascular disease, including stroke, was largest contributor to these disparities © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores et al. Published online in Stroke May 26, 2011 5
II. Definitions: Race and Ethnicity • Race encompasses related factors – Biological and geographic origins, ancestry, culture, economics, politics, and racism • Ethnicity has been proposed as a replacement category for race – Share ancestry, history or culture, highlight cultural and social characteristics rather than biological ones © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 6
II. Definitions: Race and Ethnicity • Federal government defined – Race • White • Black or African American • American Indian or Alaskan Native • Asian • Native Hawaiian or Other Pacific Islander – Ethnicity • Hispanic/Latino origin • Not of Hispanic/Latino origin • Despite the limitations, these categories provide the framework to begin our discussion © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 7

III. Epidemiology: Risk Factor Burden • African Americans – Higher prevalence of hypertension, diabetes, and left ventricular hypertrophy compared to whites • Hispanics – Higher prevalence of metabolic syndrome and diabetes compared to whites and African Americans • American Indians/Alaskan Natives – Higher prevalence of at least two risk factors compared to Whites © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 8
III. Epidemiology: Prevalence, Incidence and Recurrence • African Americans – Prevalence of stroke is about 4. 0% – More likely to report stroke symptoms, experience transient ischemic attacks, be hospitalized for stroke, and have about twice the number of incident strokes as whites – Disparity in stroke incidence is prominent among younger adults • Risk ratio of first ever stroke in African Americans compared to Whites 4. 18 (95% CI 3. 96 -4. 41) in those 35 -44 years and 2. 02 (1. 90 -2. 15) in those 45 -54 years © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 9
III. Epidemiology: Prevalence, Incidence and Recurrence • Hispanics – Prevalence of stroke is about 2. 6% – High risk ratio of stroke among Mexican Americans compared to whites • RR 2. 04 (95% CI 1. 55 -2. 69) in those 45 -59 years – Higher incidence of transient ischemic attacks, intracerebral hemorrhage, and subarachnoid hemorrhage than non-Hispanic whites • American Indians/Alaskan Natives – Prevalence of stroke is about 6. 0% © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 10
III. Epidemiology: Stroke Mortality • African Americans – Bear the highest burden of stroke mortality – Age-specific stroke mortality is approximately three times that of non-Hispanic whites for ages between 45 and 64 – High mortality risks remains after adjustment for socioeconomic status – No differences of in-hospital mortality and case fatality rates among different racial groups © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 11
III. Epidemiology: Stroke Mortality, Prevalence, Incidence and Recurrence – Racial and Ethnic minorities have excess deaths from stroke – Experience greater years of potential life lost compared to non-Hispanic whites – Risk ratio for stroke mortality in all racial and ethnic minorities is higher in the 35 -64 age group – Poor understanding of socioeconomic factors and social networks hinders the development of effective interventions to reduce these disparities © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 12
IV. Differences in Disease Awareness • Minorities have decreased awareness of – Nature of stroke – Signs and symptoms of stroke – The need for urgent treatment – Risk factors for stroke • Education improves knowledge and awareness • Long-term effects of educational campaigns remain unknown and need further research © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 13
V. Differences in Attitudes, Beliefs and Compliance • Medication compliance is reduced in minority groups – Patient-specific barriers • Forgetfulness, medications not needed when one feels well or associated with impotence, denial of disease, belief medications cause kidney disease or diabetes, and no desire to take medications for rest of life – Medication-specific barriers • Side effects of medications: allergies, hives, loss of libido – Disease-specific barriers • absence of symptoms implies lack of need for treatment © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 14
V. Differences in Attitudes, Beliefs and Compliance • Other potential causes of non-compliance – Inability to afford medications – Lower health literacy – Perceived or true presence of racial discrimination during the interaction with the healthcare system • Socio-cultural interventions – Limited evidence of improved communication, education and awareness among minorities © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 15
VI. Disparities in Access to Care • Acute Stroke Treatment – Minorities less likely to utilize emergency medical services – Minorities have delayed arrival times and longer waiting times in Emergency Departments • Contributes to lower likelihood of receiving thrombolysis • Lack of awareness, language barriers, fear of revealing immigration status – Evidence suggests the potential existence of bias in the delivery of care © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 16
VI. Disparities in Access to Care • Stroke Rehabilitation – Minorities have equal access to rehabilitation services – Minorities have longer stays and poorer functional status compared to whites • Stroke Prevention Services – Minorities less likely to receive medications for secondary stroke prevention – Behavioral modification programs may be effective in minority populations © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 17
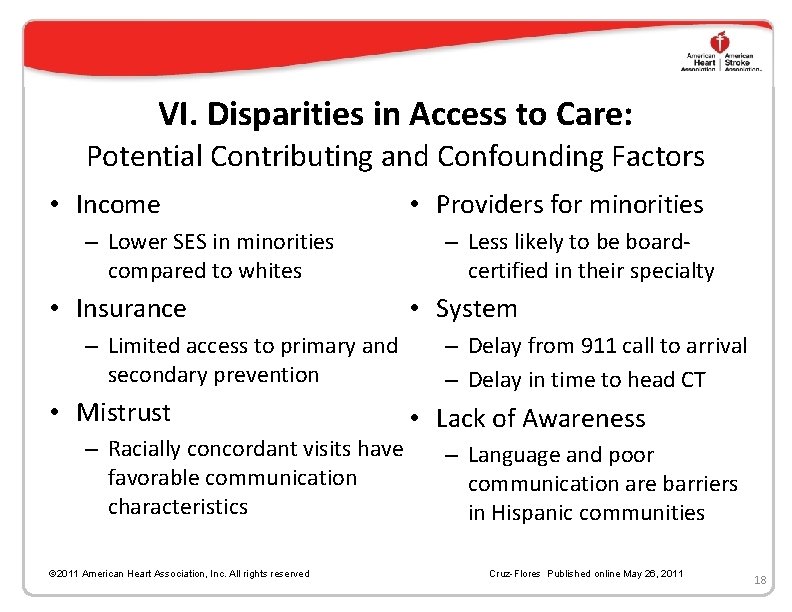
VI. Disparities in Access to Care: Potential Contributing and Confounding Factors • Income – Lower SES in minorities compared to whites • Insurance – Limited access to primary and secondary prevention • Mistrust – Racially concordant visits have favorable communication characteristics © 2011 American Heart Association, Inc. All rights reserved • Providers for minorities – Less likely to be boardcertified in their specialty • System – Delay from 911 call to arrival – Delay in time to head CT • Lack of Awareness – Language and poor communication are barriers in Hispanic communities Cruz-Flores Published online May 26, 2011 18
VII. Disparities in Quality of Stroke Care • Referral to Neurologists – Minority patients are less likely to be evaluated by a neurologist • Treatment with Thrombolytic Therapy – Disparities at several levels in chain of survival in acute stroke care © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 19
VII. Disparities in Quality of Stroke Care • Primary and Secondary Prevention – Minorities inadequately treated with primary and secondary stroke prevention strategies – Community healthcare workers may help provide preventive care and education for minorities • Use and Outcomes of Carotid Endarterectomy – More studies are needed to determine presence and identify causes • Intracerebral or Subarachnoid Hemorrhage – Paucity of data on disparities of surgical care © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 20
VIII. Differences in Access to Research • Participation of Minorities in Clinical Research – Literature contradicts assumptions that minority subjects are reluctant to participate in research • Barriers to Participation in Clinical Research – Social support – Education about the nature of the research – Trust in study personnel © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 21

VIII. Differences in Access to Research • Cultural Characteristics (attitudes, beliefs, perceptions) – Mistrust of physicians and medical research • Supported by studies in recent history in which effective treatment was withheld – Fatalistic attitudes about disease and stroke • Structural Factors – Failure to network with local organizations – Physician interest in referring their patients © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 22
IX. Future Directions • Develop strategies aimed at reducing raceethnic disparities in stroke • Support programs designed to identify responsible factors for disparities • Universal nomenclature needed to account for common characteristics of each minority group © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 23
X. Conclusions • Race-ethnic disparities in stroke care exist – Marked among minorities <65 years of age • SES and low education are barriers to delivery of effective health care • Deficiencies exist in the healthcare system – Changes need to ease access and improve modification of vascular risk factors • Call for further research and public health policy development © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 24
Recommendations • Standardize definitions for racial and ethnic groups • Implement programs to increase stroke awareness • Establish programs to increase provider cultural competence • Promote research to better define factors contribute to disparities © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 25

Recommendations • Increase health care access by broadening insurance coverage in minority populations • Expand national strategies for the hospitalbased implementation of quality improvement in acute stroke care • Clinical trials to find interventions to reduce the existent disparities • Expand federal support for trials targeted to minority populations © 2011 American Heart Association, Inc. All rights reserved Cruz-Flores Published online May 26, 2011 26
 Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke 30-30-30 model of health disparities
30-30-30 model of health disparities Health disparity definition
Health disparity definition Health disparities meaning
Health disparities meaning Non malficence
Non malficence Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Jama 2017
Jama 2017 Level of care primary secondary tertiary
Level of care primary secondary tertiary Stroke fast assessment
Stroke fast assessment Scientific inquiry vs scientific method
Scientific inquiry vs scientific method How is a scientific law different from a scientific theory?
How is a scientific law different from a scientific theory? Thermo fisher scientific mission statement
Thermo fisher scientific mission statement Scientific problem statement
Scientific problem statement Duty of care certificate
Duty of care certificate Magnetul atrage corpurile ce contin
Magnetul atrage corpurile ce contin Palliative care vs hospice care
Palliative care vs hospice care Animale care fac oua
Animale care fac oua Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Standard 10 care certificate
Standard 10 care certificate Hip fracture care clinical care standard
Hip fracture care clinical care standard Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Stroke and turn clinic
Stroke and turn clinic Brush strokes writing
Brush strokes writing What is a brush stroke in writing
What is a brush stroke in writing The little decoration at the end of a letter stroke is a
The little decoration at the end of a letter stroke is a Key stroke logger
Key stroke logger Green theorem is the relation between
Green theorem is the relation between National stroke audit rehabilitation services
National stroke audit rehabilitation services