Aging and Mental Health Whats Normal and When
- Slides: 11
Aging and Mental Health: What’s Normal and When to Seek Professional Assessment Maria Margarita Reyes, MD
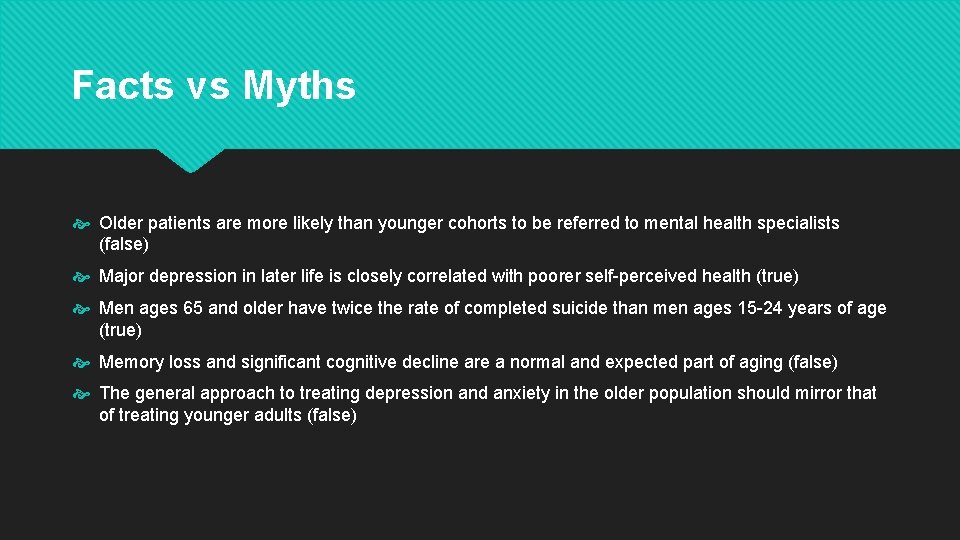
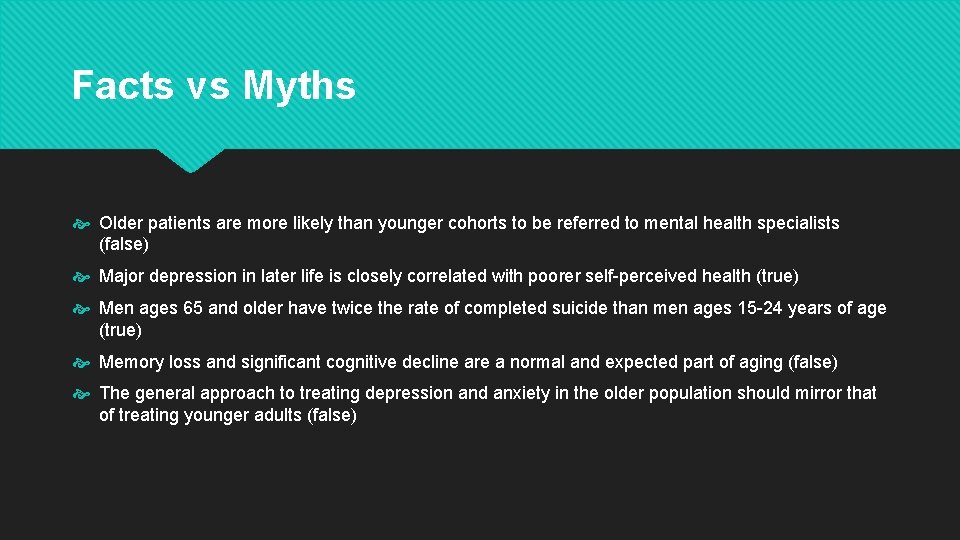
Facts vs Myths Older patients are more likely than younger cohorts to be referred to mental health specialists (false) Major depression in later life is closely correlated with poorer self-perceived health (true) Men ages 65 and older have twice the rate of completed suicide than men ages 15 -24 years of age (true) Memory loss and significant cognitive decline are a normal and expected part of aging (false) The general approach to treating depression and anxiety in the older population should mirror that of treating younger adults (false)
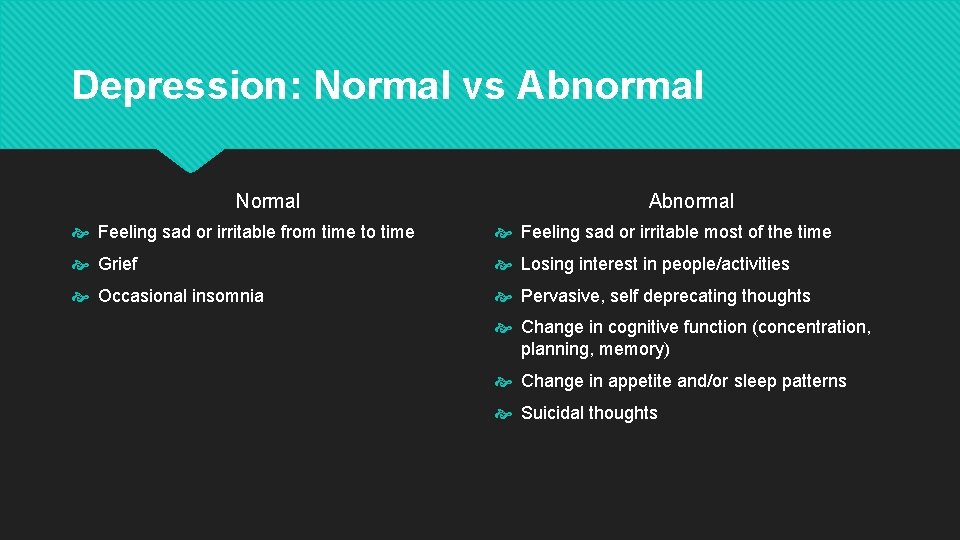
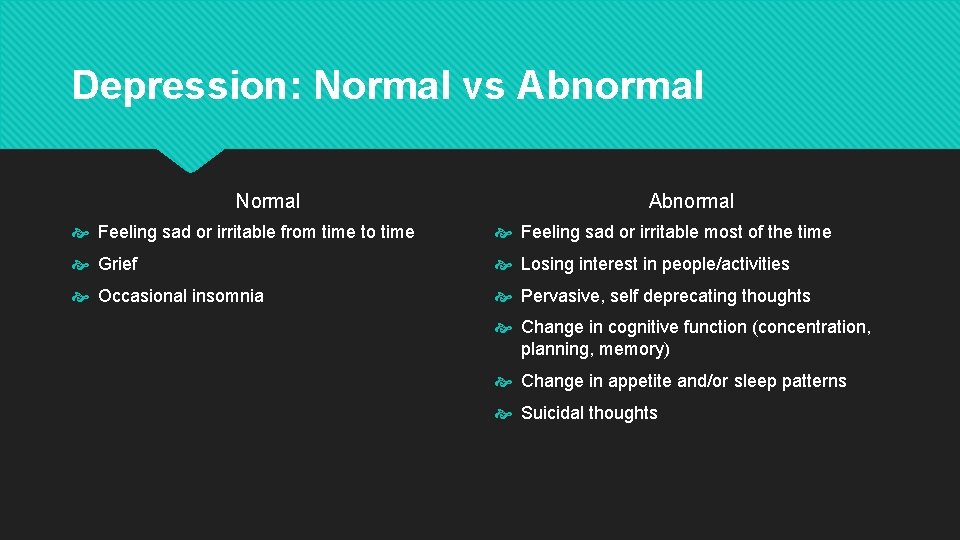
Depression: Normal vs Abnormal Normal Abnormal Feeling sad or irritable from time to time Feeling sad or irritable most of the time Grief Losing interest in people/activities Occasional insomnia Pervasive, self deprecating thoughts Change in cognitive function (concentration, planning, memory) Change in appetite and/or sleep patterns Suicidal thoughts
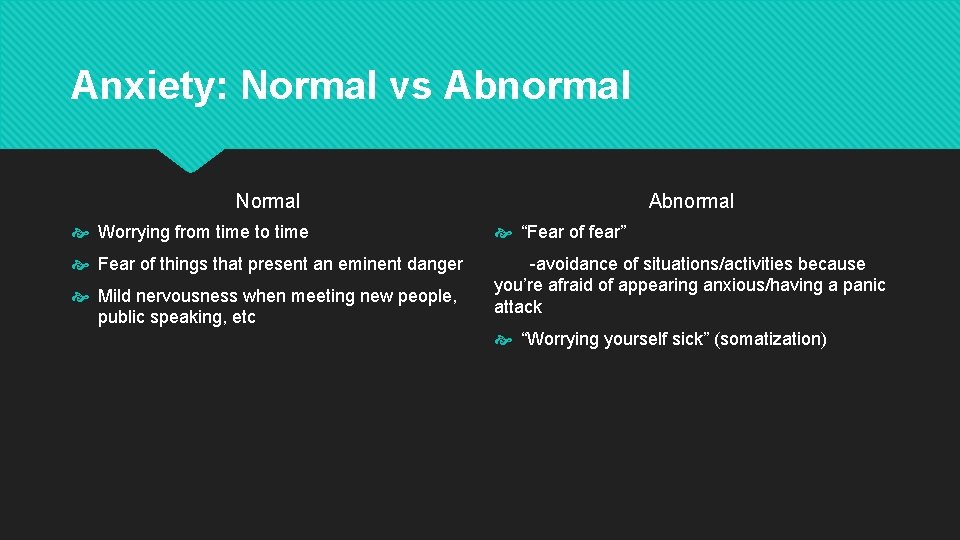
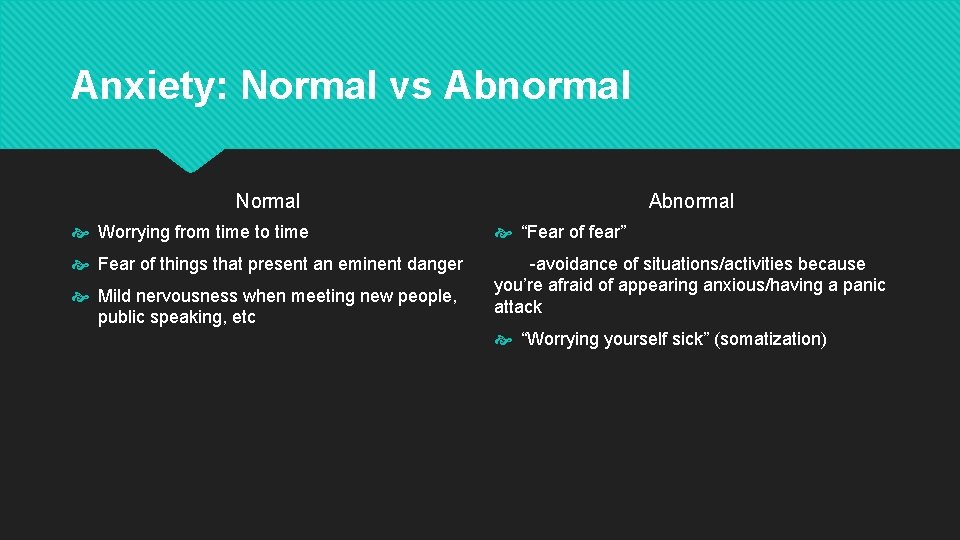
Anxiety: Normal vs Abnormal Normal Abnormal Worrying from time to time “Fear of fear” Fear of things that present an eminent danger -avoidance of situations/activities because you’re afraid of appearing anxious/having a panic attack Mild nervousness when meeting new people, public speaking, etc “Worrying yourself sick” (somatization)
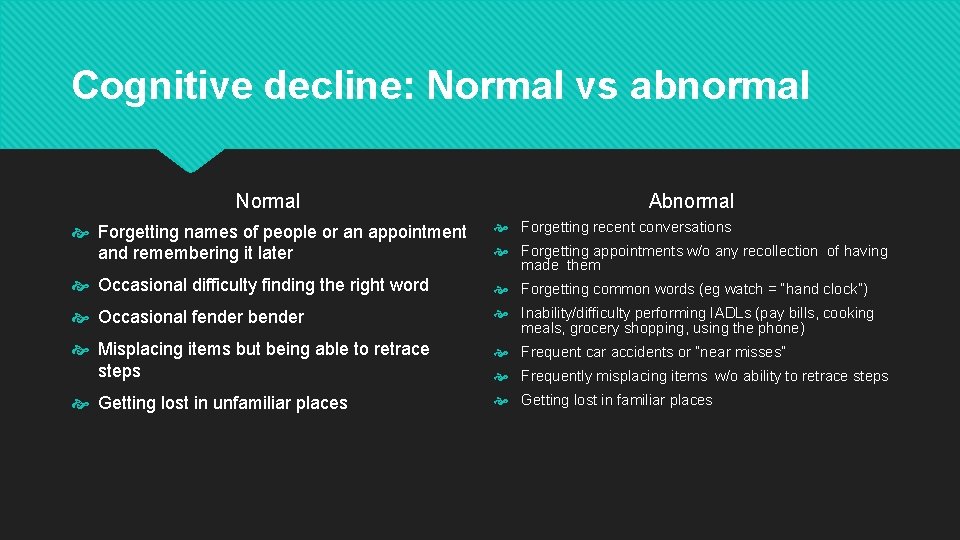
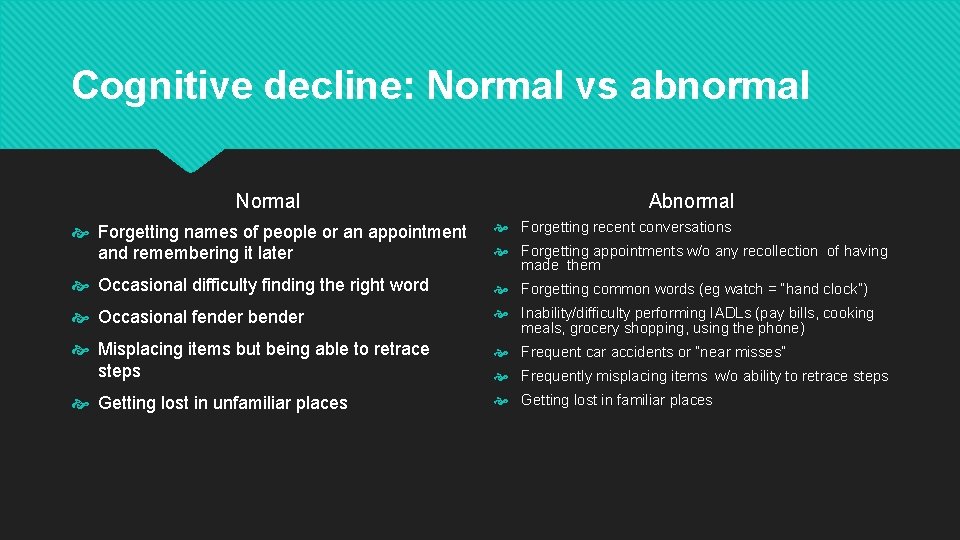
Cognitive decline: Normal vs abnormal Normal Abnormal Forgetting names of people or an appointment and remembering it later Forgetting recent conversations Occasional difficulty finding the right word Forgetting common words (eg watch = “hand clock”) Occasional fender bender Inability/difficulty performing IADLs (pay bills, cooking meals, grocery shopping, using the phone) Misplacing items but being able to retrace steps Frequent car accidents or “near misses” Getting lost in unfamiliar places Getting lost in familiar places Forgetting appointments w/o any recollection of having made them Frequently misplacing items w/o ability to retrace steps
Types of Major Neurocognitive Impairment Alzheimer’s Vascular Lewy body Parkinson’s plus dementia Frontotemporal lobular dementia Huntington’s, Creuzfield-Jacob, HIV, Alcoholism Mixed
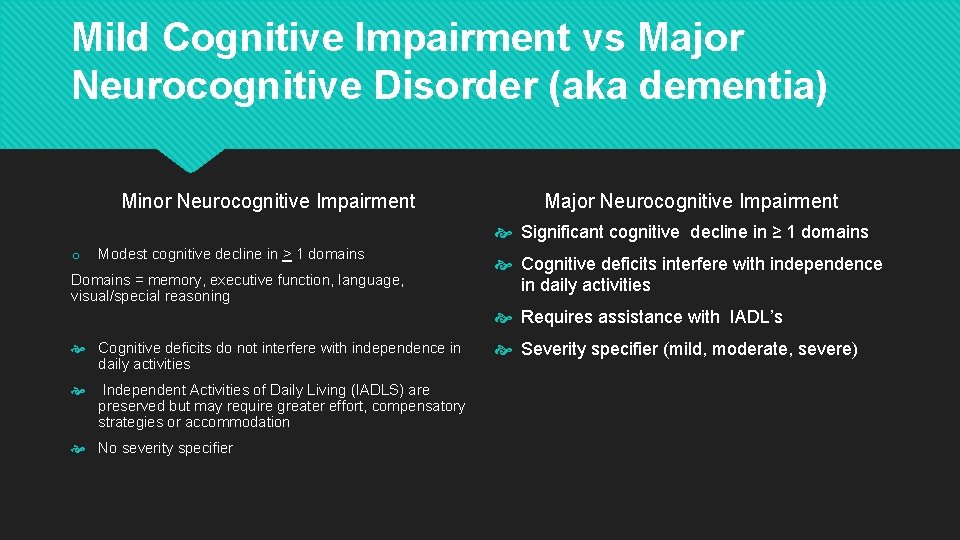
Mild Cognitive Impairment vs Major Neurocognitive Disorder (aka dementia) Minor Neurocognitive Impairment Major Neurocognitive Impairment Significant cognitive decline in ≥ 1 domains o Modest cognitive decline in > 1 domains Domains = memory, executive function, language, visual/special reasoning Cognitive deficits interfere with independence in daily activities Requires assistance with IADL’s Cognitive deficits do not interfere with independence in daily activities Independent Activities of Daily Living (IADLS) are preserved but may require greater effort, compensatory strategies or accommodation No severity specifier Severity specifier (mild, moderate, severe)
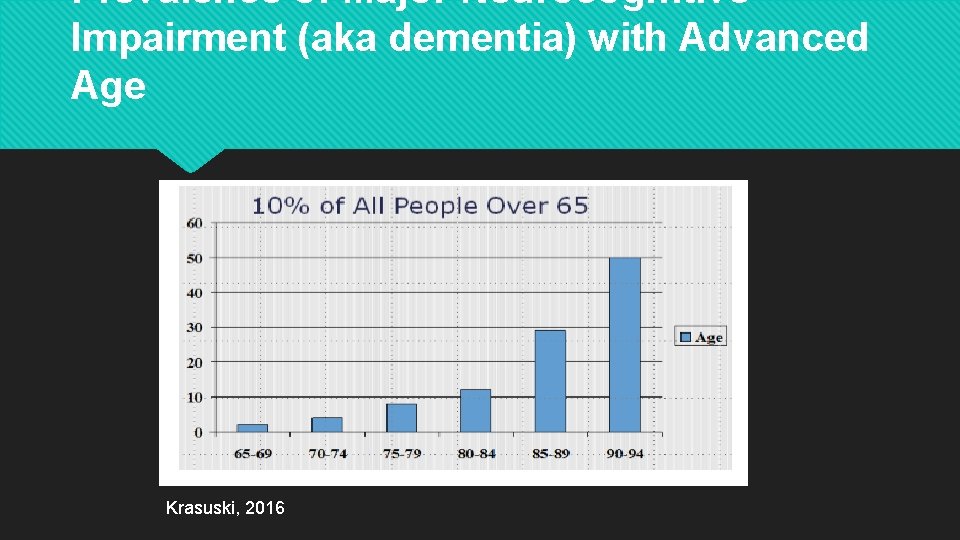
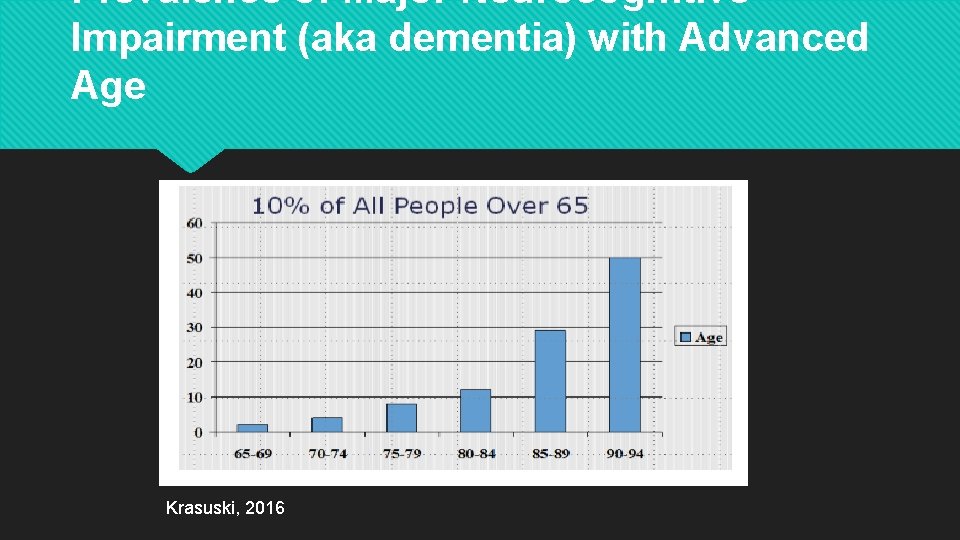
Prevalence of Major Neurocognitive Impairment (aka dementia) with Advanced Age Krasuski, 2016
Medical Contributions to Dementia Infection (HIV/AIDS, even a bladder infection!) Medication toxicity/unintended drug effects/ interactions Over/under active thyroid Vitamin deficiencies Uncontrolled diabetes Cancer Stroke, heart attack, high blood pressure, high cholesterol
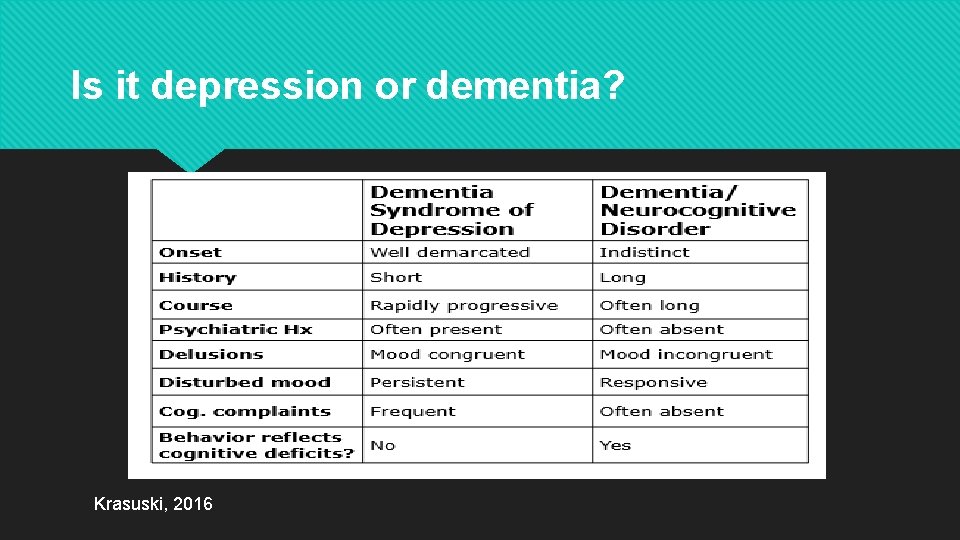
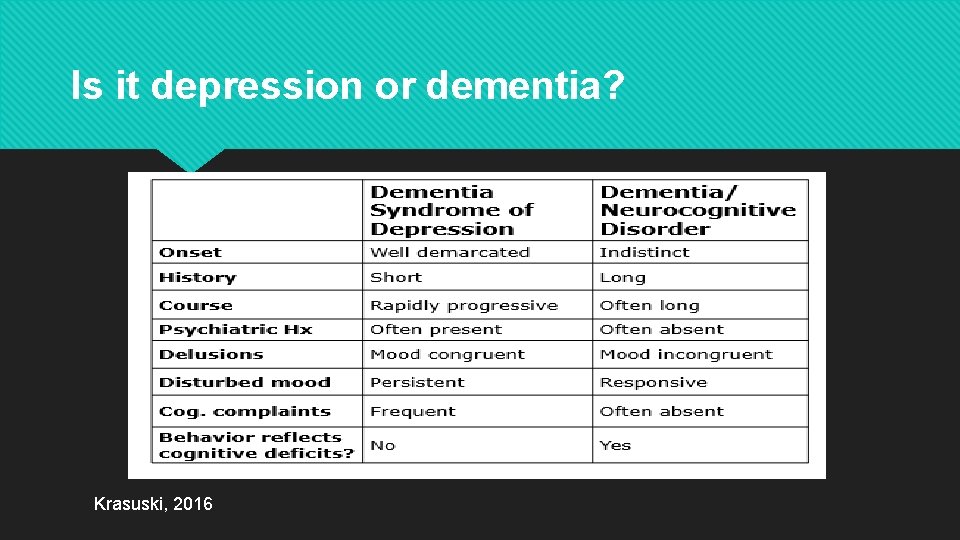
Is it depression or dementia? Krasuski, 2016
Geriatric Psychiatry Evaluation Review of medications Review of health history Basic labs MMSE/Mo. CA (cognitive screening) +/- Brain imaging +/- Psychometric testing