Aging and Health Care Disparities in the Older













- Slides: 64
Aging and Health Care Disparities in the Older Adult with Intellectual / Developmental Disabilities (I/DD) Presented By: Ronald Lucchino, Ph. D rvluc@comcast. net
Myths of Aging in the Older Adult with I/DD
• All individuals with I/DD experience pre-mature aging. – Only adult with Down syndrome and Cerebral Palsy experience early aging changes • All adults with Down Syndrome will have Alzheimer’s Disease. – Only 60% by age 60 • Majority of adults with I/DD live in residential care facilities. – Most live with parents
Aging in the Older Adult with I/DD Compared to the General Population
• Age-related (normal) biological changes in individuals with mild to moderate I/DD – Have the same aging changes,
• Age-related (normal) biological changes in individuals with mild to moderate I/DD – Have the same aging changes, – The same rate of aging change, and
• Age-related (normal) biological changes in individuals with mild to moderate I/DD – Have the same aging changes, – The same rate of aging change, and – Similar longevity as the general population. *

• Age-related (normal) biological changes in individuals with mild to moderate I/DD – Have the same aging changes, – The same rate of aging change, and – Similar longevity as the general population * * Exceptions are adults with Down Syndrome and Cerebral Palsy who experience early changes.
What Influences the Aging Process in the Older Adult with I/DD
• The aging process of the older adult with I/DD is the interaction of many factors making this population vulnerable to ambulatory care sensitive conditions (ACSC) which increases the risk for hospitalization. This includes: – Age-related changes, overlaid
• The aging process of the older adult with I/DD is the interaction of many factors making this population vulnerable to ambulatory care sensitive conditions (ACSC) which increases the risk for hospitalization. This includes: – Age-related changes, overlaid – By pre-existing disabilities, associated with the disorder, influencing
• The aging process of the older adult with I/DD is the interaction of many factors making this population vulnerable to ambulatory care sensitive conditions (ACSC) which increases the risk for hospitalization. This includes: – Age-related changes, overlaid – By pre-existing disabilities, associated with the disorder, influencing – Age-associated changes (lifestyle) and co-morbidity of diseases, and
• The aging process of the older adult with I/DD is the interaction of many factors making this population vulnerable to ambulatory care sensitive conditions (ACSC) which increases the risk for hospitalization. This includes: – Age-related changes, overlaid – By pre-existing disabilities, associated with the disorder, influencing – Age-associated changes (lifestyle) and co-morbidity of diseases, and – Disparities to accessing health care, compounded by
• The aging process of the older adult with I/DD is the interaction of many factors making this population vulnerable to ambulatory care sensitive conditions (ACSC) which increases the risk for hospitalization. This includes: – Age-related changes, overlaid – By pre-existing disabilities, associated with the disorder, influencing – Age-associated changes (lifestyle) and co-morbidity of diseases, and – Disparities to accessing health care, compounded by – “Diagnostic Over-Shadowing. ”
What is Aging?
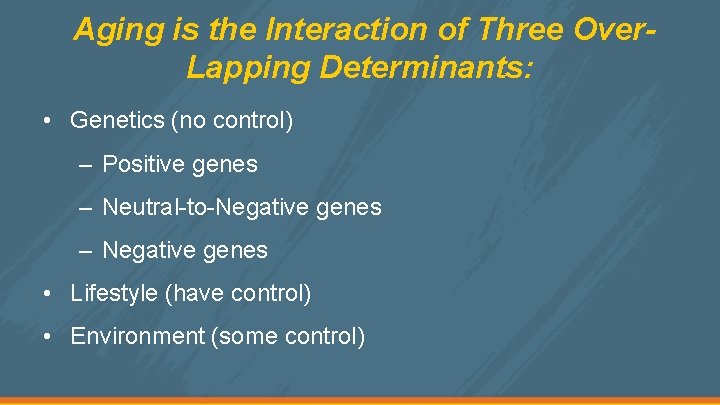
Aging is the Interaction of Three Over. Lapping Determinants: • Genetics (no control) – Positive genes – Neutral-to-Negative genes – Negative genes • Lifestyle (have control) • Environment (some control)
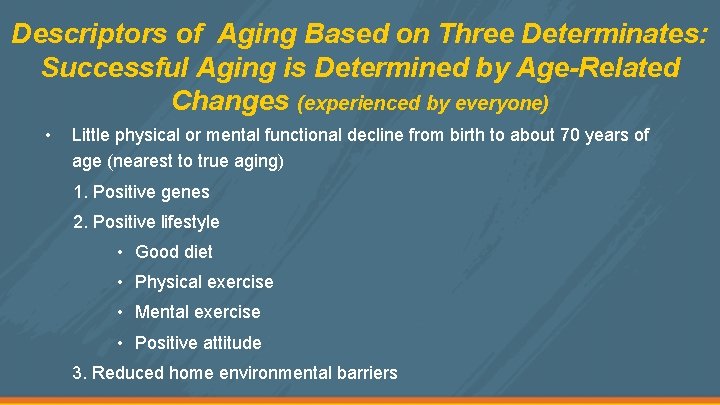
Descriptors of Aging Based on Three Determinates: Successful Aging is Determined by Age-Related Changes (experienced by everyone) • Little physical or mental functional decline from birth to about 70 years of age (nearest to true aging) 1. Positive genes 2. Positive lifestyle • Good diet • Physical exercise • Mental exercise • Positive attitude 3. Reduced home environmental barriers
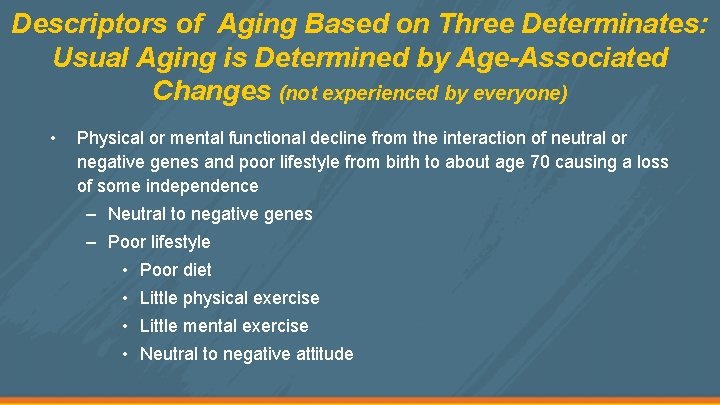
Descriptors of Aging Based on Three Determinates: Usual Aging is Determined by Age-Associated Changes (not experienced by everyone) • Physical or mental functional decline from the interaction of neutral or negative genes and poor lifestyle from birth to about age 70 causing a loss of some independence – Neutral to negative genes – Poor lifestyle • Poor diet • Little physical exercise • Little mental exercise • Neutral to negative attitude
Descriptors of Aging Based on Three Determinates: Pathological Aging is Determined by Age-Associated Co-Morbidity Diseases (decline of age-associated changes without intervention) • Serious functional limitations from the interaction of either genetically inherited or developmental traits with poor lifestyle causing a substantial reduction in daily activities – Negative genes – Negative lifestyle • Poor diet • No physical exercise
Determinants of Aging Adults with I/DD • Remember, we can not change the genetics causing the disabilities associated with an I/DD disorder, but we can enhance lifestyle and environment by: – Better diet, exercising the brain and body, and reducing physical barriers in the home. • We think in terms of better lifestyle for the general population but not for the population with I/DD. • Many of the age-associated changes that will be discussed could be reduced if we develop better lifestyle programs and reduce environmental barriers.
How the Interaction and Overlaying of Three Determinants of Aging (genetics, lifestyle, environment) Influence How the Older Individual with I/DD Ages

Developmental Disabilities (genetics)
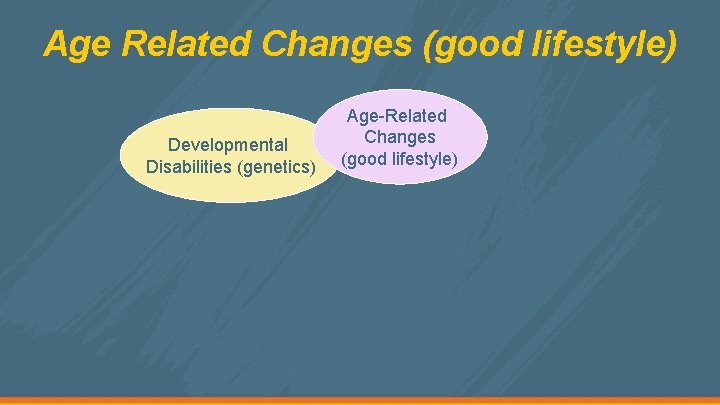
Age Related Changes (good lifestyle) Developmental Disabilities (genetics) Age-Related Changes (good lifestyle)
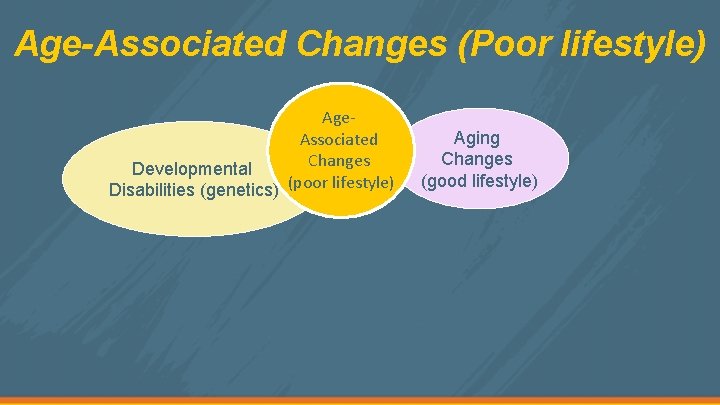
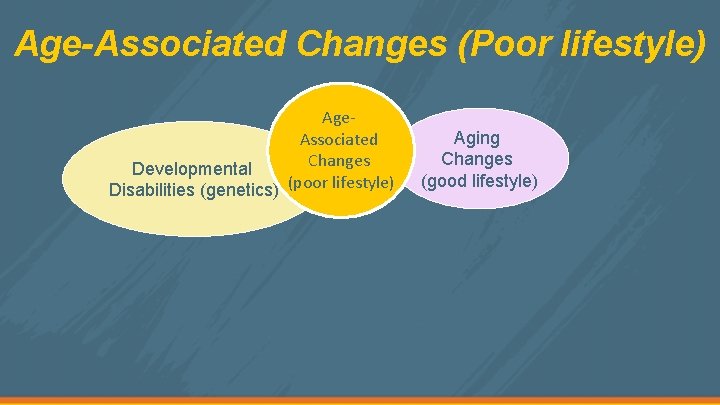
Age-Associated Changes (Poor lifestyle) Age. Associated Changes Developmental Disabilities (genetics) (poor lifestyle) Aging Changes (good lifestyle)
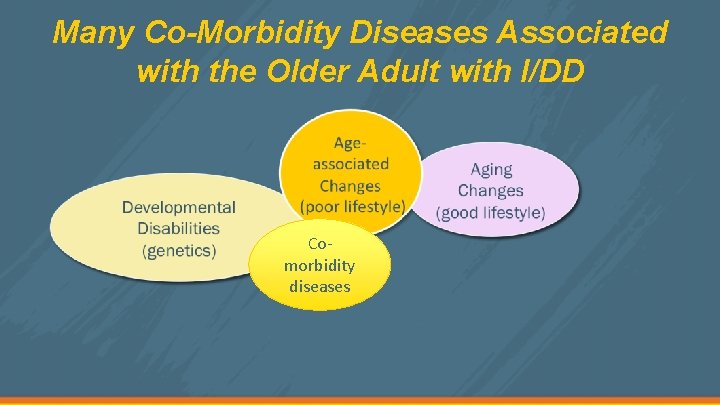
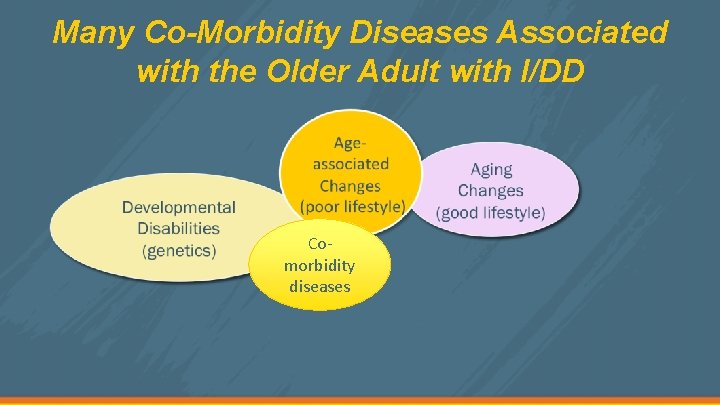
Many Co-Morbidity Diseases Associated with the Older Adult with I/DD Comorbidity diseases

Medications to Treat Co-Morbidity Diseases Comorbidity diseases
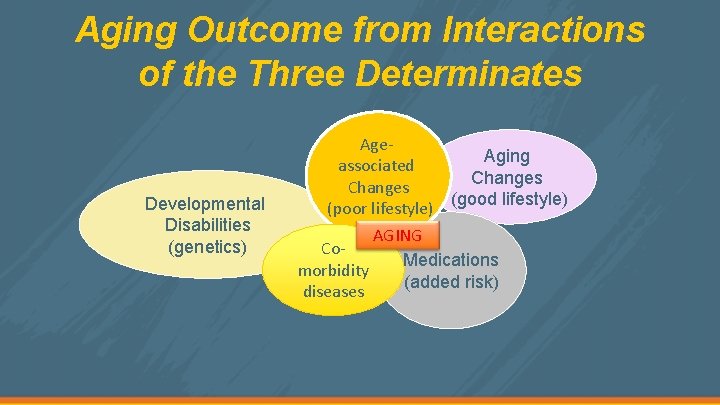
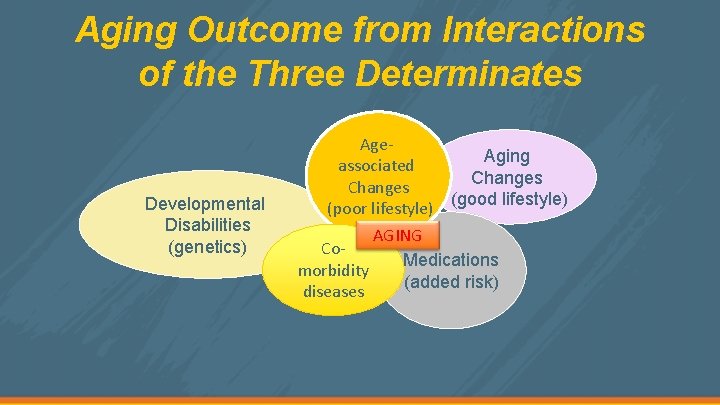
Aging Outcome from Interactions of the Three Determinates Developmental Disabilities (genetics) Age. Aging associated Changes (good lifestyle) (poor lifestyle) Comorbidity diseases AGING Medications (added risk)
• The population with I/DD is at greater risk for health concerns than the general population due, in part, to: – Overlapping of I/DD-associated disabilities with ageassociated and age-related changes – High co-morbidity of age-associated diseases – Health care disparity – Over-use of medications (Adverse Drug Reactions, ADR’s) • The increased health risk results in individuals with I/DD being over-represented by five to six times the general population in hospital admissions due to ACSC.
AGING CURVES – HOW INTERACTIONS AFFECT THE AGING CURVE IN OLDER ADULTS WITH I/DD
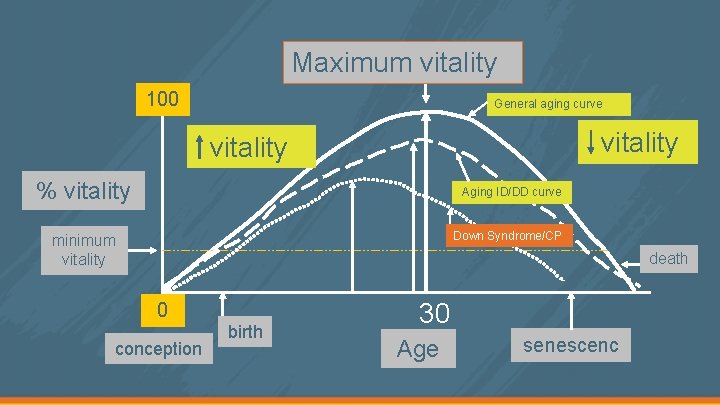
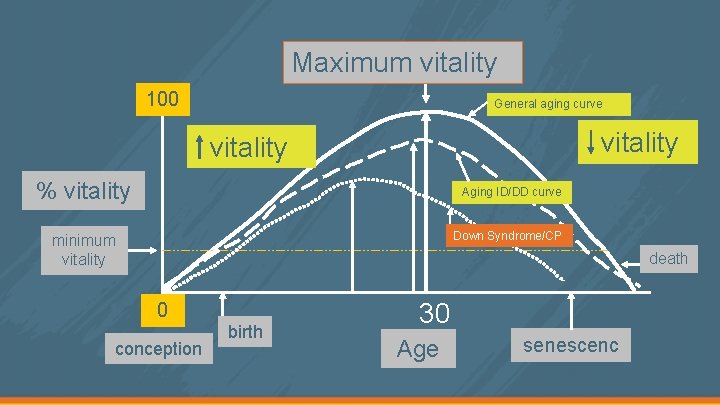
Maximum vitality 100 General aging curve vitality % vitality Aging ID/DD curve Down Syndrome/CP minimum vitality death 0 conception birth 30 Age senescenc e

How the Reduced Vitality Increases Health Care Disparities in the Population with I/DD Persons with I/DD experience poorer health because of health care disparities, as a consequence of overlapping aging changes with the disabilities and the problem of diagnostic over-shadowing and ACSCs. Citation: Gloria L. Krahn, Laura Hammond, and Anne Turner 2006. A CASCADE OF DISPARITIES: HEALTH AND HEALTH CARE ACCESS FOR PEOPLE WITH INTELLECTUAL DISABILITIES. Mental Retardation and Developmental Disabilities Research Reviews. 12: 70– 82

Effects of Reduced Vitality: Increasing Risk for Disparities in Accessing Health Care • Increased risk factors with earlier onset of symptoms • Increased risk for wrong diagnosis and inappropriate medical treatment • Increased vulnerability to a more restrictive environment • Increased challenging behaviors due to communication difficulties • Increased cost for treatment and interventions • Increased staff/family frustration due to lack of communication and knowledge
What are the Disparities to Accessing Health Care in the Population with I/DD?
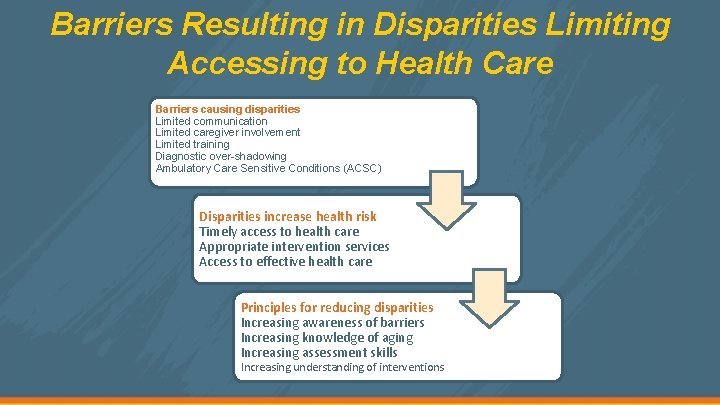
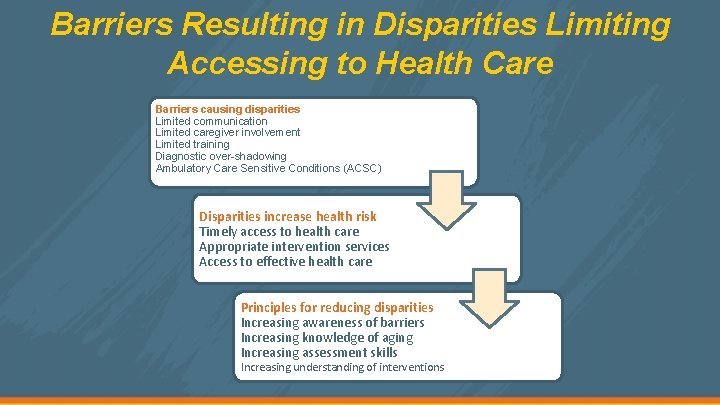
Barriers Resulting in Disparities Limiting Accessing to Health Care Barriers causing disparities Limited communication Limited caregiver involvement Limited training Diagnostic over-shadowing Ambulatory Care Sensitive Conditions (ACSC) Disparities increase health risk Timely access to health care Appropriate intervention services Access to effective health care Principles for reducing disparities Increasing awareness of barriers Increasing knowledge of aging Increasing assessment skills Increasing understanding of interventions
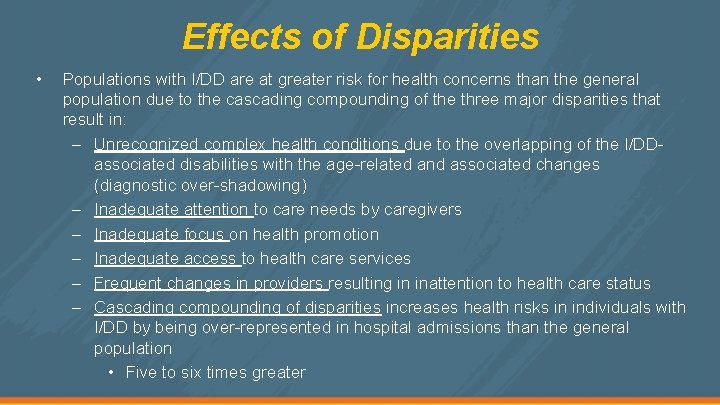
Effects of Disparities • Populations with I/DD are at greater risk for health concerns than the general population due to the cascading compounding of the three major disparities that result in: – Unrecognized complex health conditions due to the overlapping of the I/DDassociated disabilities with the age-related and associated changes (diagnostic over-shadowing) – Inadequate attention to care needs by caregivers – Inadequate focus on health promotion – Inadequate access to health care services – Frequent changes in providers resulting in inattention to health care status – Cascading compounding of disparities increases health risks in individuals with I/DD by being over-represented in hospital admissions than the general population • Five to six times greater
How Diagnostic Over-Shadowing and ACSC Increase the Risk for Hospitalization in the Older Adult with I/DD
Ambulatory Care Sensitive Conditions (ACSC): Increased Risk for Hospitalization
Ambulatory Care Sensitive Conditions (ACSC) • Clustering of serious health-related changes or conditions that increase the older adult’s vulnerability to being admitted to a hospital or residential care facility. Many of the ACSC can be prevented with recognition and intervention of specific conditions. • Clustering of health-related conditions that define the ACSC depends on many factors, including: gender, race/ethnicity, types of disabilities associated with a disorder, location, pre-existing conditions, etc.
ACSC (cont. ’d) • • ACSC in older adults with I/DD accounts for a high rate of hospitalization five to six times greater than the general population. ACSC in individuals with Down syndrome are (not an inclusive list): – psychiatric disorders – seizure disorders – gastrointestinal disorders – tuberculosis – cancer – hepatitis – dental health – Medications
ACSC (cont. ’d) • The major reason for the high rate of hospitalization from ACSC are the barriers (reduced verbal communication, lack of caregiver inclusion, lack of education) that increase disparities (recognition of problem, determining cause of problem, appropriate needed services) in accessing health care for individuals with I/DD.

Diagnostic Over-Shadowing: Increased Risk for Hospitalization
What is Diagnostic Over-Shadowing: Problem with adults with I/DD Definition : Clinicians attribute symptoms or behavior of a person with I/DD to the underlying disorder, therefore, underdiagnosing possible co-morbidities. • Changes related to the disability result in inappropriate or no intervention • Pre-existing cognitive challenges assumed to be symptoms of dementia • Pre-existing disability may be misdiagnosed as disease • Increased risk factors with earlier onset of symptoms
Diagnostic Over-Shadowing (cont. ’d) • Increased risk of inappropriate medical treatment • Increased vulnerability to a more restrictive environment

Outcome Interventions: How to Decrease the Risk of Disparities by Increasing the Health and Social Care Practitioners Awareness of Potential Health Care Risks
• OBSERVATION: To increase awareness of the importance to observe changes in the older adult with I/DD (behavior, coordination, mental and biological).
• OBSERVATION: To increase awareness of the importance to observe changes in the older adult with I/DD (behavior, coordination, mental and biological). • DOCUMENTATION: To increase awareness of documenting the changes.

• OBSERVATION: To increase awareness of the importance to observe changes in the older adult with I/DD (behavior, coordination, mental and biological). • DOCUMENTATION: To increase awareness of documenting the changes. • REPORTING: To increase awareness of the importance to present the documentation, on change, to the health care practitioners.

• OBSERVATION: To increase awareness of the importance to observe changes in the older adult with I/DD (behavior, coordination, mental and biological). • DOCUMENTATION: To increase awareness of documenting the changes. • REPORTING: To increase awareness of the importance to present the documentation, on change, to the health care practitioners. • INTERVENTION: To develop interventions that reduce the disparities to health care, and increase lifestyle.

AGE-ASSOCIATED CHANGES AND DISEASES HOW ASSOCIATED CHANGES AND DISEASES IN THE OLDER ADULT WITH MILD TO MODERATE I/DD MAY INCREASE THE RISK FOR HOSPITALIZATION.
Changes in Central Nervous System • Older Adult with Down syndrome – Higher prevalence of seizures (epilepsy) between the ages of 20 - 30 years, but can occur in older adults – Late-onset seizures after the age of 50 • 85% of adults with Down Syndrome diagnosed with Alzheimer's disease – Usually tonic-clinic seizures most common (Grand mal) but others may occur
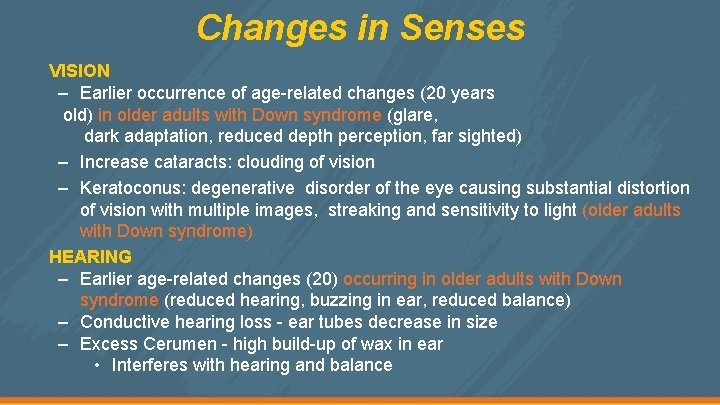
Changes in Senses VISION – Earlier occurrence of age-related changes (20 years old) in older adults with Down syndrome (glare, dark adaptation, reduced depth perception, far sighted) – Increase cataracts: clouding of vision – Keratoconus: degenerative disorder of the eye causing substantial distortion of vision with multiple images, streaking and sensitivity to light (older adults with Down syndrome) HEARING – Earlier age-related changes (20) occurring in older adults with Down syndrome (reduced hearing, buzzing in ear, reduced balance) – Conductive hearing loss - ear tubes decrease in size – Excess Cerumen - high build-up of wax in ear • Interferes with hearing and balance
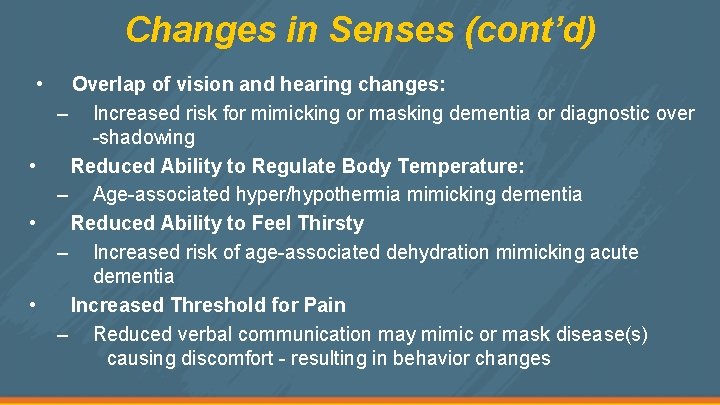
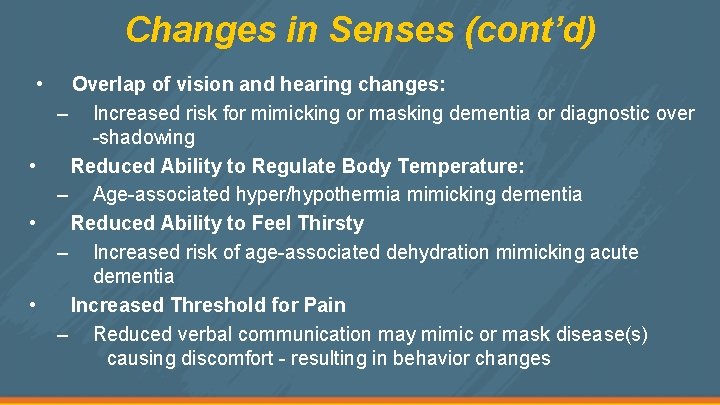
Changes in Senses (cont’d) • • Overlap of vision and hearing changes: – Increased risk for mimicking or masking dementia or diagnostic over -shadowing Reduced Ability to Regulate Body Temperature: – Age-associated hyper/hypothermia mimicking dementia Reduced Ability to Feel Thirsty – Increased risk of age-associated dehydration mimicking acute dementia Increased Threshold for Pain – Reduced verbal communication may mimic or mask disease(s) causing discomfort - resulting in behavior changes
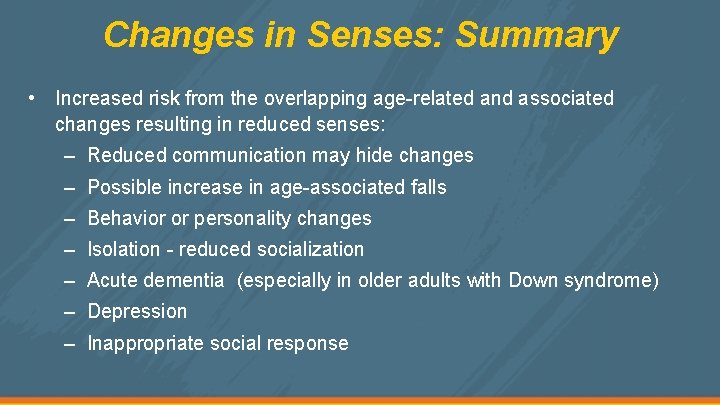
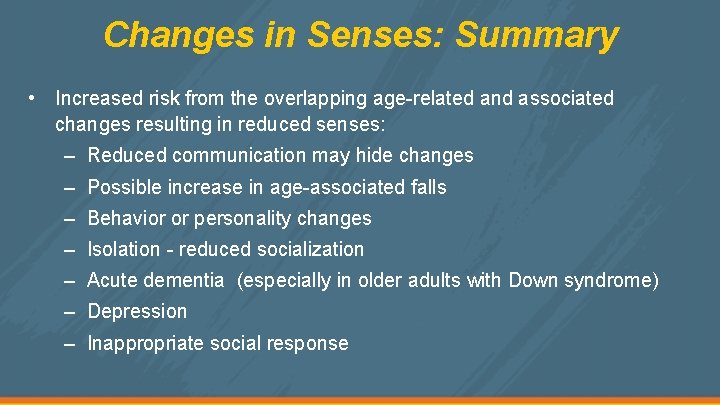
Changes in Senses: Summary • Increased risk from the overlapping age-related and associated changes resulting in reduced senses: – Reduced communication may hide changes – Possible increase in age-associated falls – Behavior or personality changes – Isolation - reduced socialization – Acute dementia (especially in older adults with Down syndrome) – Depression – Inappropriate social response
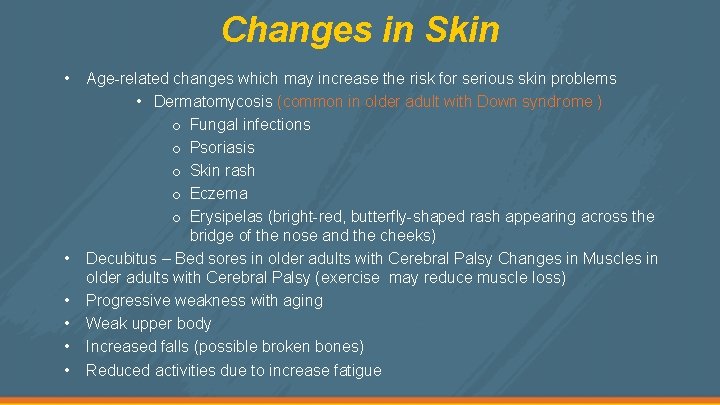
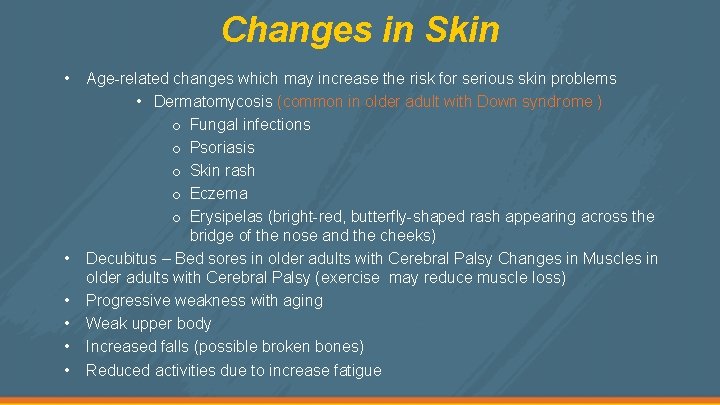
Changes in Skin • • • Age-related changes which may increase the risk for serious skin problems • Dermatomycosis (common in older adult with Down syndrome ) o Fungal infections o Psoriasis o Skin rash o Eczema o Erysipelas (bright-red, butterfly-shaped rash appearing across the bridge of the nose and the cheeks) Decubitus – Bed sores in older adults with Cerebral Palsy Changes in Muscles in older adults with Cerebral Palsy (exercise may reduce muscle loss) Progressive weakness with aging Weak upper body Increased falls (possible broken bones) Reduced activities due to increase fatigue
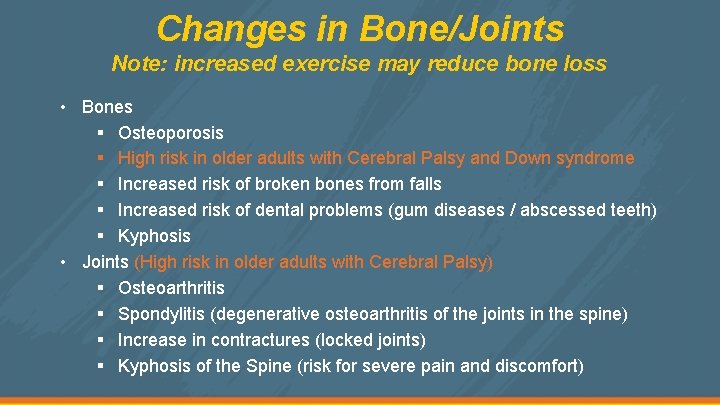
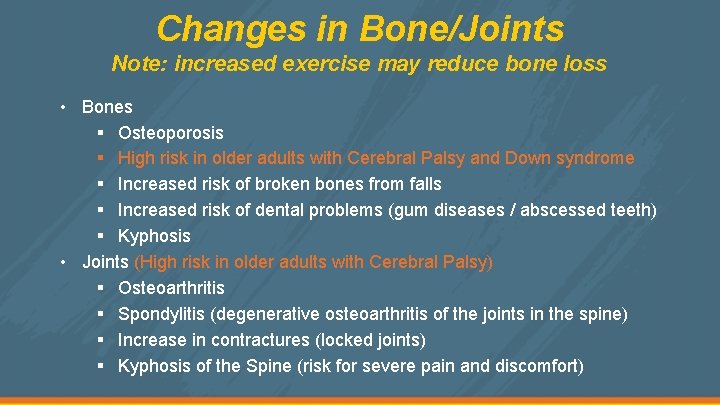
Changes in Bone/Joints Note: increased exercise may reduce bone loss • Bones § Osteoporosis § High risk in older adults with Cerebral Palsy and Down syndrome § Increased risk of broken bones from falls § Increased risk of dental problems (gum diseases / abscessed teeth) § Kyphosis • Joints (High risk in older adults with Cerebral Palsy) § Osteoarthritis § Spondylitis (degenerative osteoarthritis of the joints in the spine) § Increase in contractures (locked joints) § Kyphosis of the Spine (risk for severe pain and discomfort)
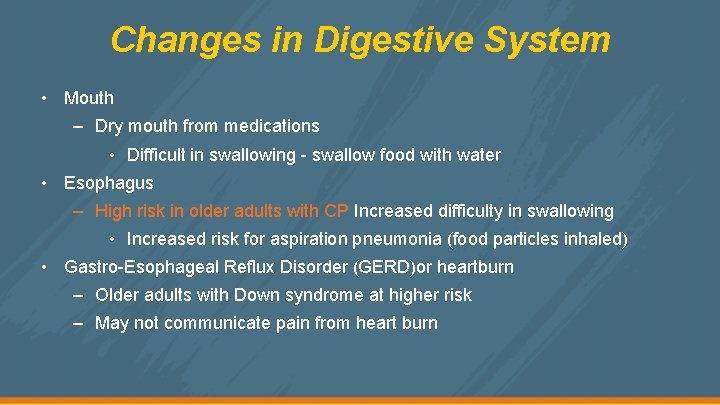
Changes in Digestive System • Mouth – Dry mouth from medications • Difficult in swallowing - swallow food with water • Esophagus – High risk in older adults with CP Increased difficulty in swallowing • Increased risk for aspiration pneumonia (food particles inhaled) • Gastro-Esophageal Reflux Disorder (GERD)or heartburn – Older adults with Down syndrome at higher risk – May not communicate pain from heart burn

Changes in Digestive System (cont’d) • Intestines – Increased risk in older adults with Down syndrome (pain unreported) • Chronic constipation – no bowl movement more than three days • Increase in fecal incontinence • Weakening of anal muscles - possible staining of undergarments • Celiac disease (gluten intolerance): excessive diarrhea, nausea, abdominal distension, or unexplained lethargy
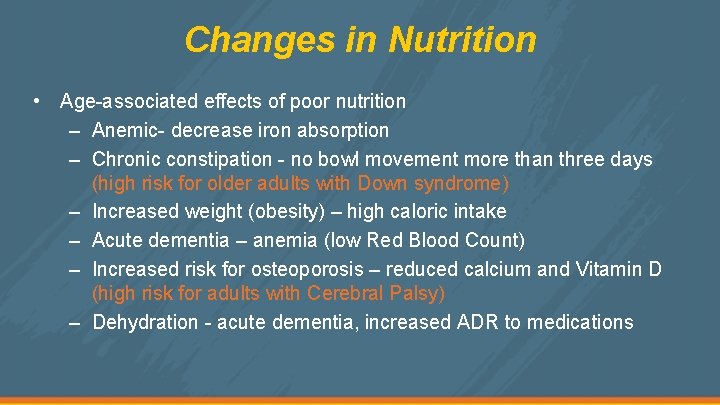
Changes in Nutrition • Age-associated effects of poor nutrition – Anemic- decrease iron absorption – Chronic constipation - no bowl movement more than three days (high risk for older adults with Down syndrome) – Increased weight (obesity) – high caloric intake – Acute dementia – anemia (low Red Blood Count) – Increased risk for osteoporosis – reduced calcium and Vitamin D (high risk for adults with Cerebral Palsy) – Dehydration - acute dementia, increased ADR to medications

Changes in Nutrition: Obesity • Obesity in older adults with Down syndrome – 70. 58% of males and 95. 83% of females with Down syndrome are obese – 49. 29% males and 62. 96% females from general population with I/DD are obese – Only 40% of males and 32% females from general population are obese • Health problems associated with obesity – Increased blood pressure – Possible increased risk of Diabetes 2 – Increased risk of heart problems – Possible increased risk for Alzheimer’s disease
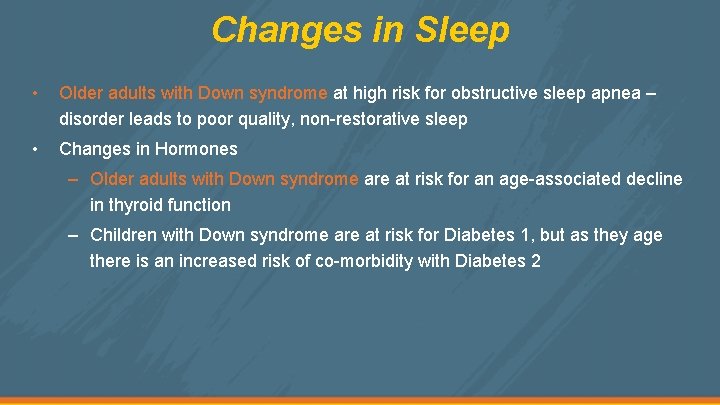
Changes in Sleep • Older adults with Down syndrome at high risk for obstructive sleep apnea – disorder leads to poor quality, non-restorative sleep • Changes in Hormones – Older adults with Down syndrome are at risk for an age-associated decline in thyroid function – Children with Down syndrome are at risk for Diabetes 1, but as they age there is an increased risk of co-morbidity with Diabetes 2
Changes in Sleep (cont’d) • Changes in Respiration (older adults with Cerebral Palsy adults are at risk) – Increased difficulty in breathing (dyspnea) and muscle control making speaking more difficult. – Increased vulnerability to pneumonia – Increased upper respiratory infections – Changes in Prostate Gland • Age-related change with similar symptoms as prostate cancer (Male adults with I/DD may not report reduced ability to urinate due to lack of communication skills)

STRATEGIES FOR REDUCING ACSC AND HOSPITALIZATION
Strategies 1. Better coordinate the continuum of care from community to hospital and back. 2. Reduce ACSC by training caregivers to identify ageassociated changes that increase the risk of ACSC. 3. Empower the care provider or adult with I/DD to better communicate observed changes to the healthcare professional.
Strategies 4. Provide training to the residential care facilities and/or hospital staff on the needs of the older adult with I/DD. 5. Increase advocate’s role to provide documentation of health care concerns to the professional healthcare practitioner