Agents used in cardiac arrhythmias Normal heart rate














- Slides: 65

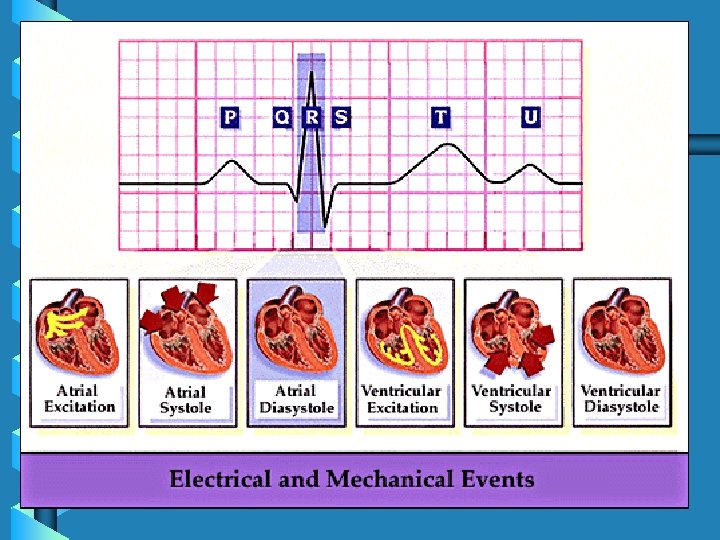
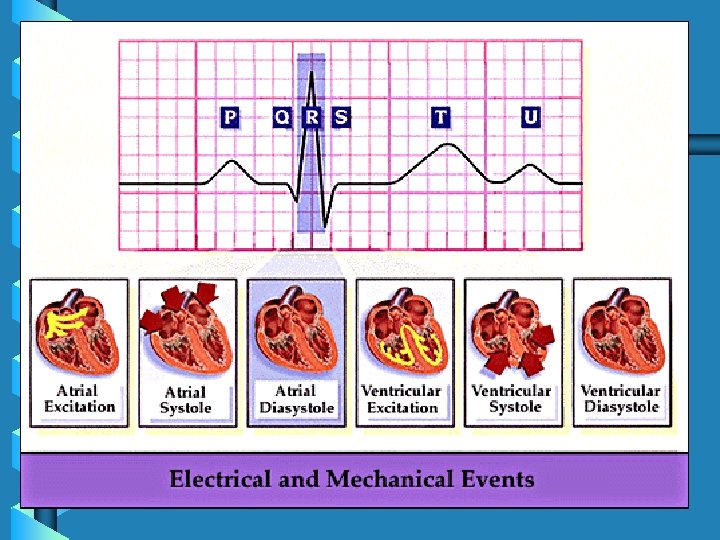
Agents used in cardiac arrhythmias • Normal heart rate • Action potential • ECG

Disturbance of cardiac rhythm • Are classified according to : • 1 - Site of origin of the abnormality ( atrial , nodal , ventricular ). • 2 - Rate ( increased or decreased
Factors precipitate arrhythmias • May includes : • Ischemia, hypoxia, electrolytes disturbance, excessive catecholamines exposure , drug toxicity.
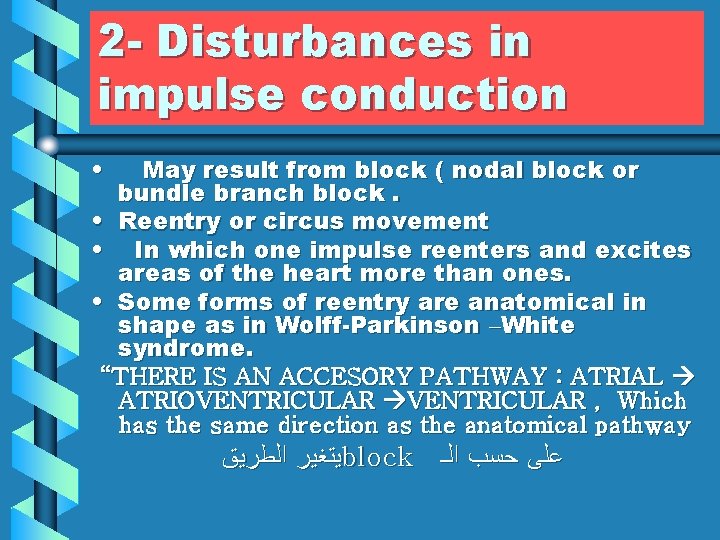
Mechanisms of arrhythmias • 1 - Disturbances in impulse formation. • Vagal stimulation or β- receptor blocking drugs slow normal pacemaker ( reduce the phase 4 slope ). • Acceleration of pacemaker ( increase of phase 4 slope ) by hypokalemia or βadrenoceptor stimulants. • Development of ectopic pacemakers. -
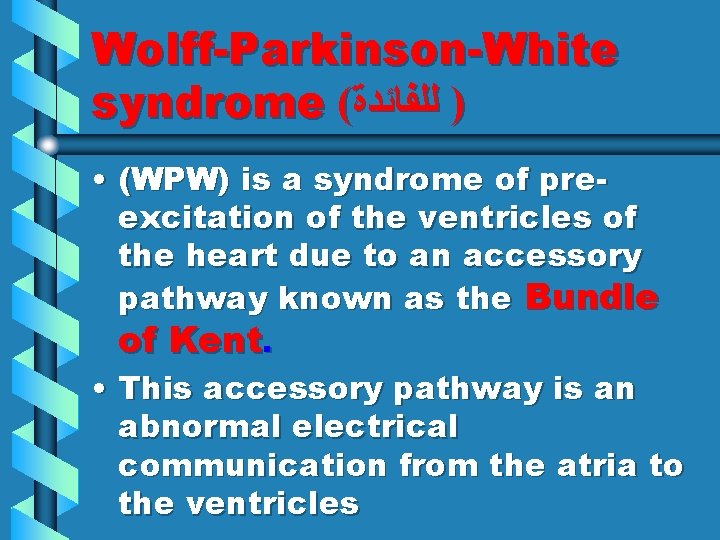
2 - Disturbances in impulse conduction • May result from block ( nodal block or bundle branch block. • Reentry or circus movement • In which one impulse reenters and excites areas of the heart more than ones. • Some forms of reentry are anatomical in shape as in Wolff-Parkinson –White syndrome. “THERE IS AN ACCESORY PATHWAY : ATRIAL ATRIOVENTRICULAR , Which has the same direction as the anatomical pathway ﻳﺘﻐﻴﺮ ﺍﻟﻄﺮﻳﻖ block ﻋﻠﻰ ﺣﺴﺐ ﺍﻟـ



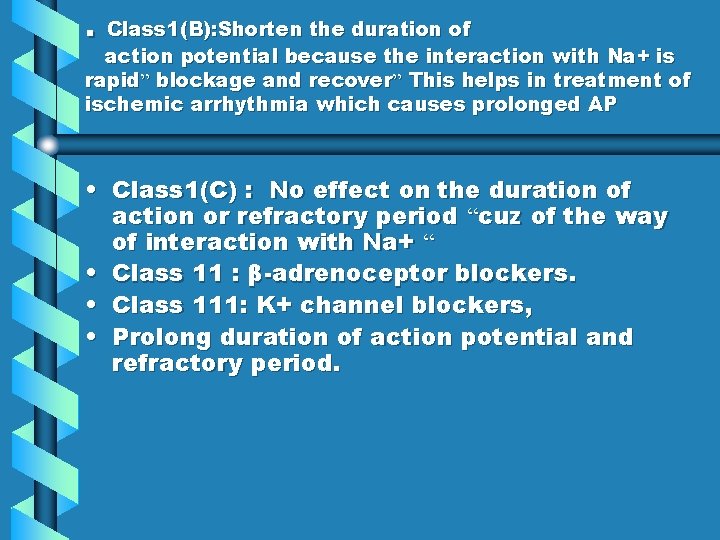
Antiarrhythmic Drugs • IN ARRYTHMIA , WE DON’T TREAT ALL THE PTS WITH DRUGS , CUZ ANTIARRYTHMIC DRUGS MAY CAUSE FATAL ARRYTHMIA AND OTHER SIDE EFFECTS - - WE HAVE ALTERNATIVE TREATMENT , eg. SURGERY • Class 1 : Na+ channel blockers “main mechanism” • Local anaesthetic effect • -ve inotropic action - -may precipitate heart failure • Class 1( A ): prolongs duration of action potential & refractory period” this happens in atrium and ventricle” • Have K+ channel blocking effect • Antimuscarinic & hypotensive effects “accounts as side effect”
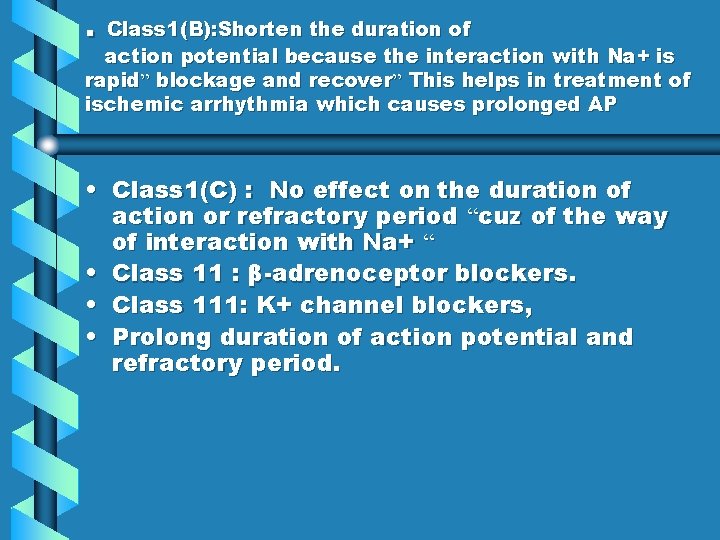
. Class 1(B): Shorten the duration of action potential because the interaction with Na+ is rapid” blockage and recover” This helps in treatment of ischemic arrhythmia which causes prolonged AP • Class 1(C) : No effect on the duration of action or refractory period “cuz of the way of interaction with Na+ “ • Class 11 : β-adrenoceptor blockers. • Class 111: K+ channel blockers, • Prolong duration of action potential and refractory period.

• • • Class 1 V : Ca++ channel blockers. Verapamil, deltizem, pepridil Pepridil – acts by other mechanisms : Na+ channel blocking , K+ channel blocking • Only those 3 drugs from all the Ca+ channel blockers can be use as antiarrhythmics. • Ca+ channel blockers has an effect on tissue that depend mainly on Ca+ to produce AP. • Class V: Miscellaneous group.
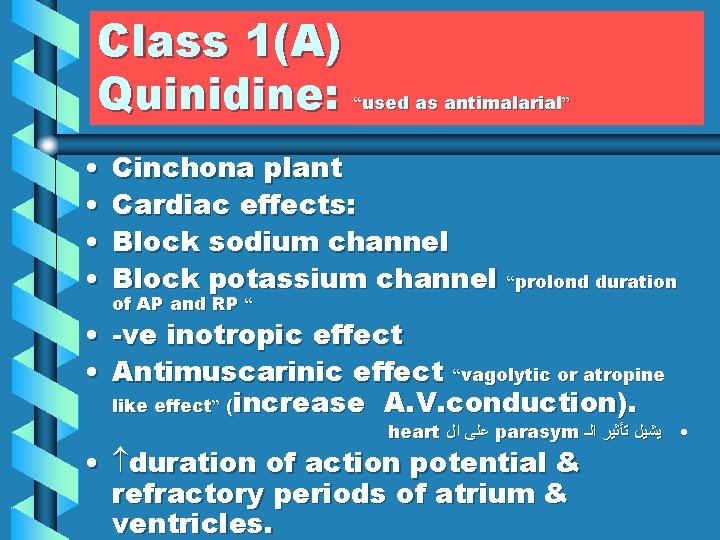
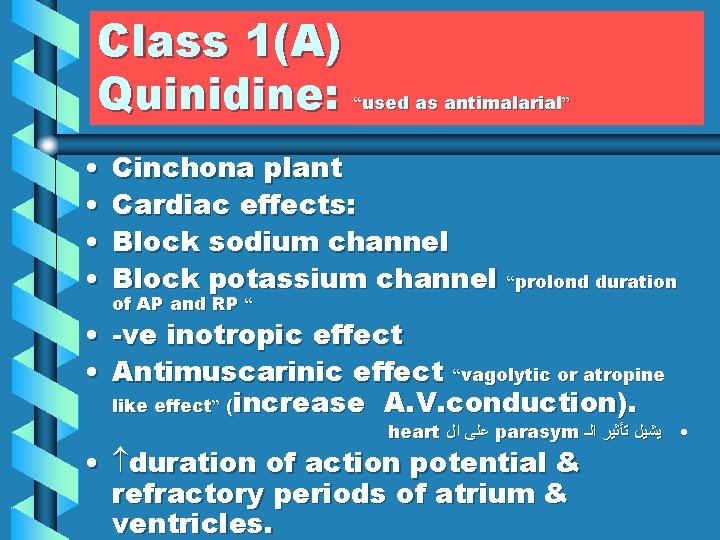
Class 1(A) Quinidine: “used as antimalarial” • • Cinchona plant Cardiac effects: Block sodium channel Block potassium channel of AP and RP “ “prolond duration • -ve inotropic effect • Antimuscarinic effect “vagolytic or atropine like effect” (increase A. V. conduction). heart ﻋﻠﻰ ﺍﻝ parasym • ﻳﺸﻴﻞ ﺗﺄﺜﻴﺮ ﺍﻟـ • duration of action potential & refractory periods of atrium & ventricles.

ECG changes • Prolong Q-T interval ”cuz it prolongs the RP “ • Widening QRS complex “ cuz it increases the AP of the ventricle”
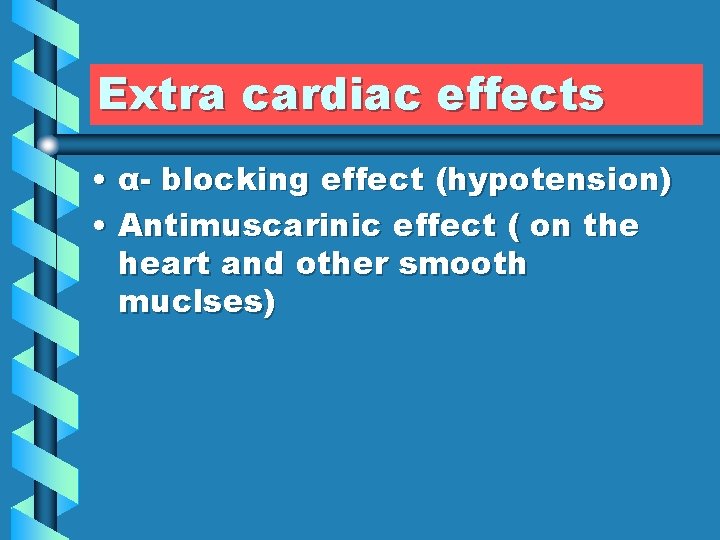
Extra cardiac effects • α- blocking effect (hypotension) • Antimuscarinic effect ( on the heart and other smooth muclses)
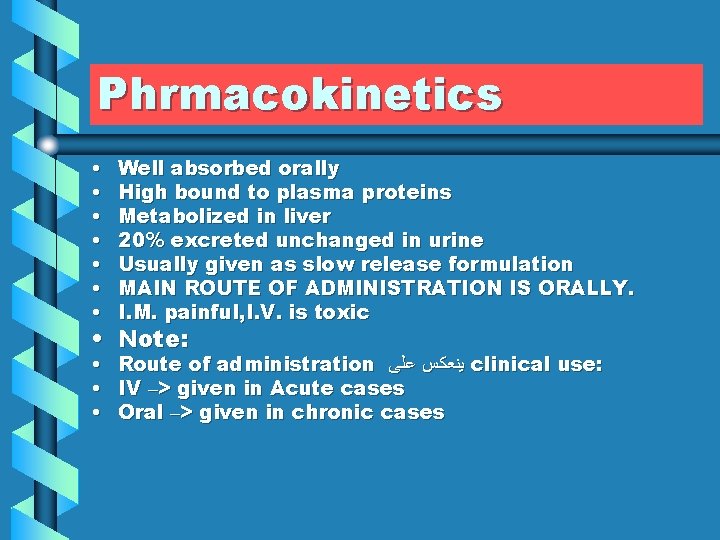
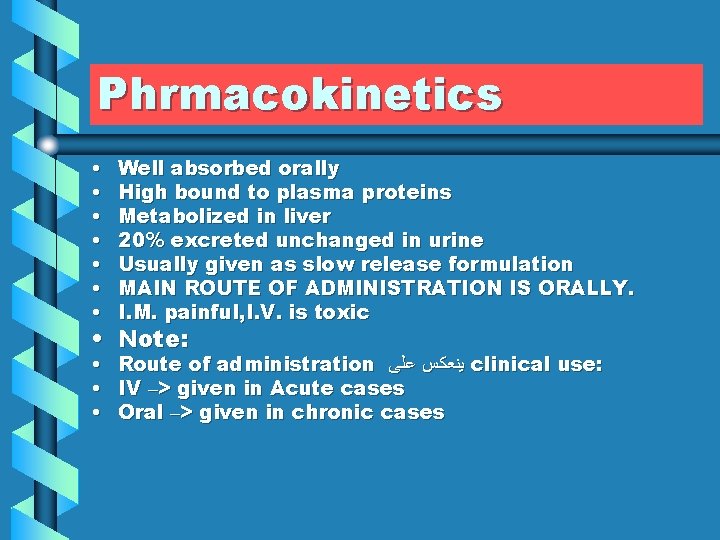
Phrmacokinetics • • Well absorbed orally High bound to plasma proteins Metabolized in liver 20% excreted unchanged in urine Usually given as slow release formulation MAIN ROUTE OF ADMINISTRATION IS ORALLY. I. M. painful, I. V. is toxic • • • Route of administration ﻳﻨﻌﻜﺲ ﻋﻠﻰ clinical use: IV –> given in Acute cases Oral –> given in chronic cases • Note:
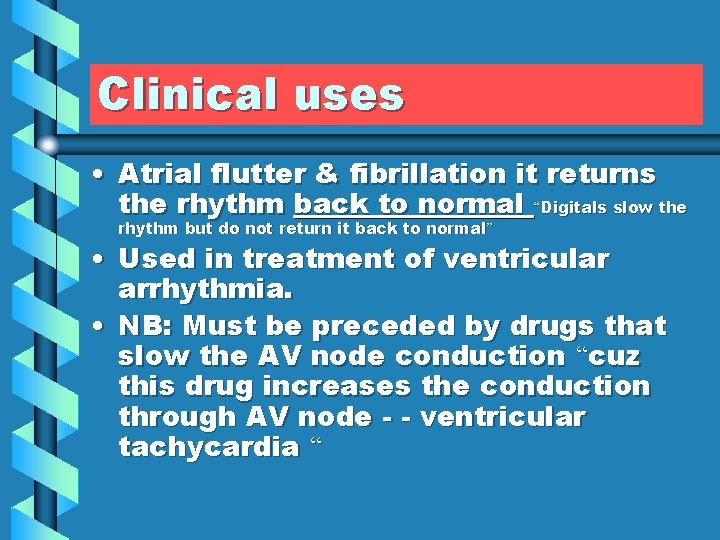
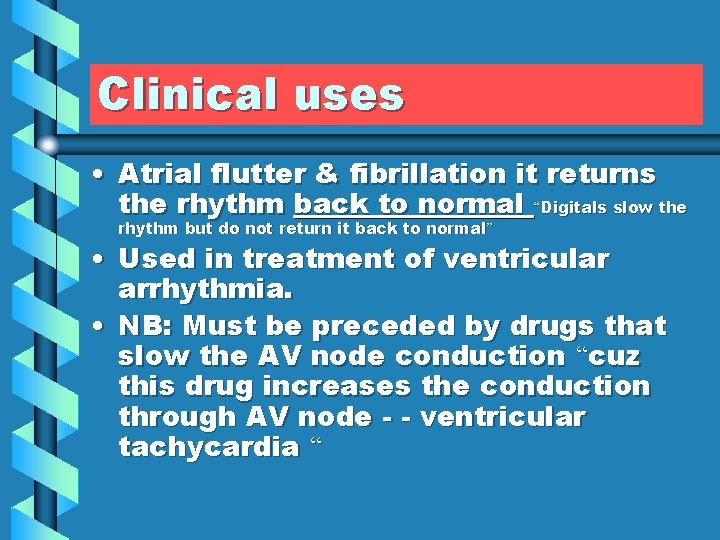
Clinical uses • Atrial flutter & fibrillation it returns the rhythm back to normal “Digitals slow the rhythm but do not return it back to normal ” • Used in treatment of ventricular arrhythmia. • NB: Must be preceded by drugs that slow the AV node conduction “cuz this drug increases the conduction through AV node - - ventricular tachycardia “
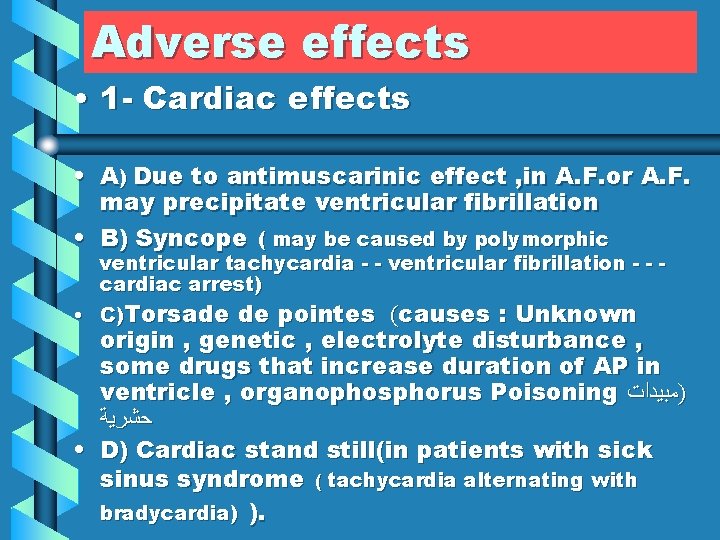
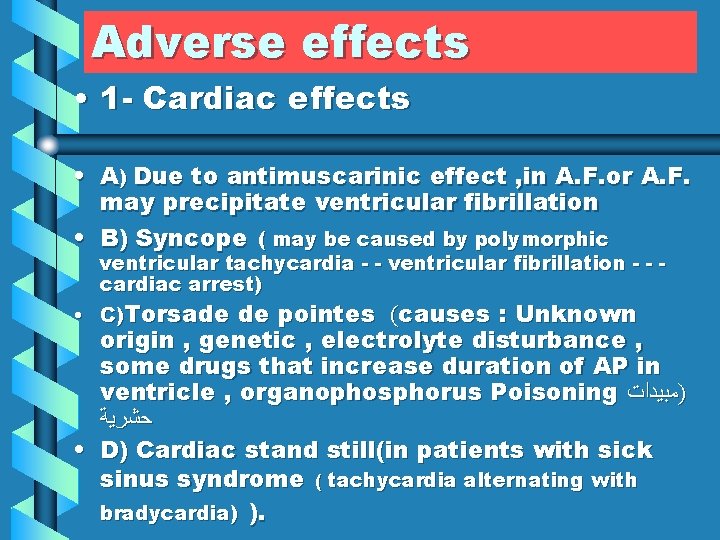
Adverse effects • 1 - Cardiac effects • A) Due to antimuscarinic effect , in A. F. or A. F. may precipitate ventricular fibrillation • B) Syncope ( may be caused by polymorphic ventricular tachycardia - - ventricular fibrillation - - cardiac arrest) • C)Torsade de pointes (causes : Unknown origin , genetic , electrolyte disturbance , some drugs that increase duration of AP in ventricle , organophosphorus Poisoning )ﻣﺒﻴﺪﺍﺕ ﺣﺸﺮﻳﺔ • D) Cardiac stand still(in patients with sick sinus syndrome ( tachycardia alternating with bradycardia) ).
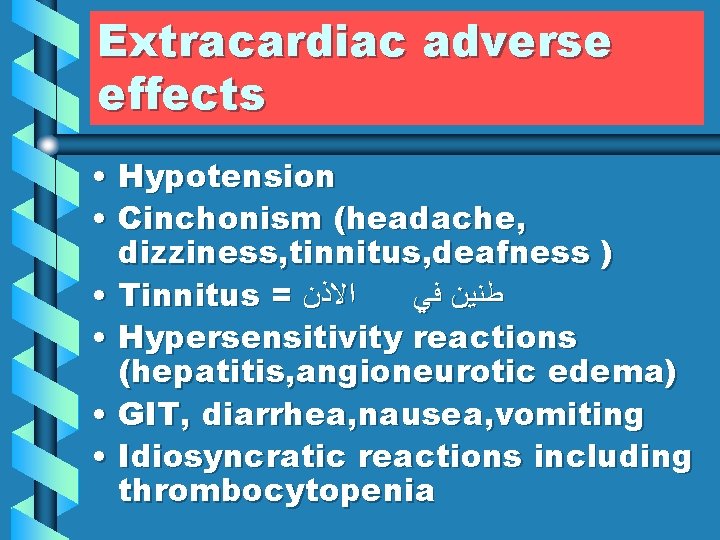
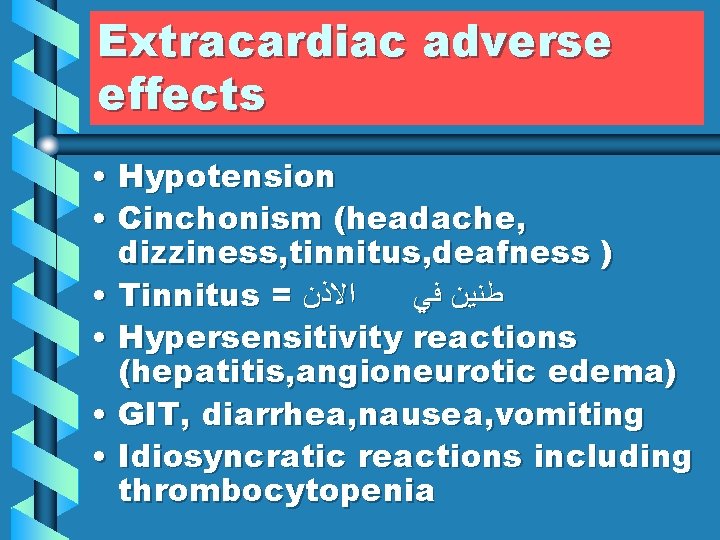
Extracardiac adverse effects • Hypotension • Cinchonism (headache, dizziness, tinnitus, deafness ) • Tinnitus = ﺍﻻﺫﻥ ﻃﻨﻴﻦ ﻓﻲ • Hypersensitivity reactions (hepatitis, angioneurotic edema) • GIT, diarrhea, nausea, vomiting • Idiosyncratic reactions including thrombocytopenia
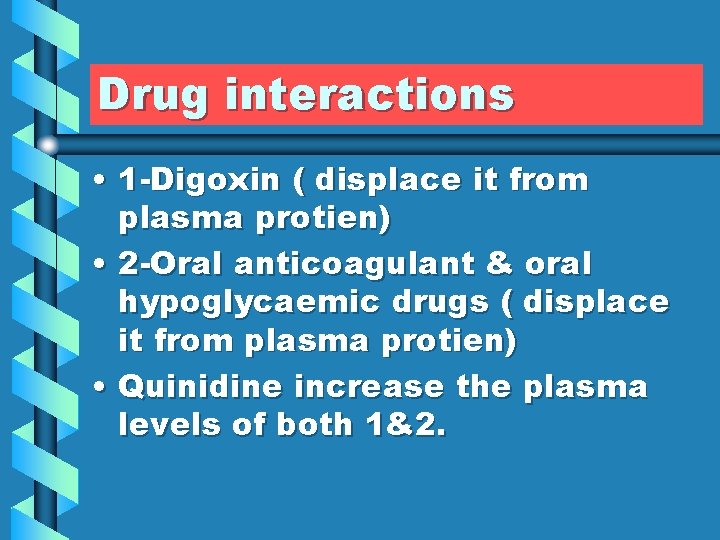
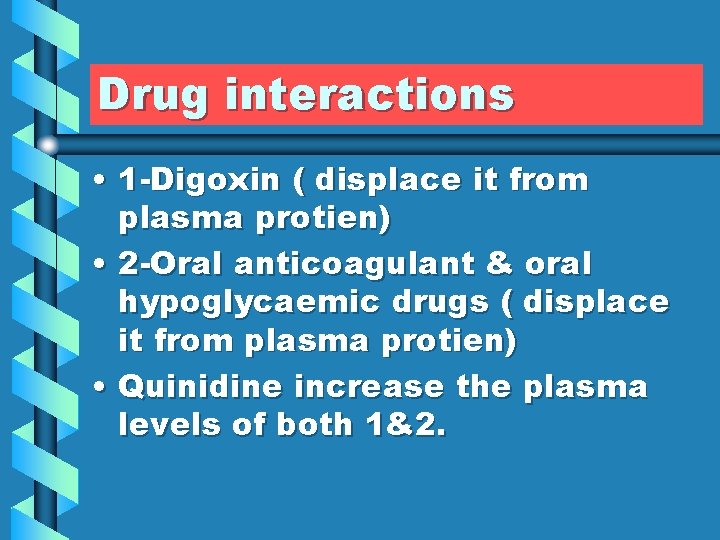
Drug interactions • 1 -Digoxin ( displace it from plasma protien) • 2 -Oral anticoagulant & oral hypoglycaemic drugs ( displace it from plasma protien) • Quinidine increase the plasma levels of both 1&2.
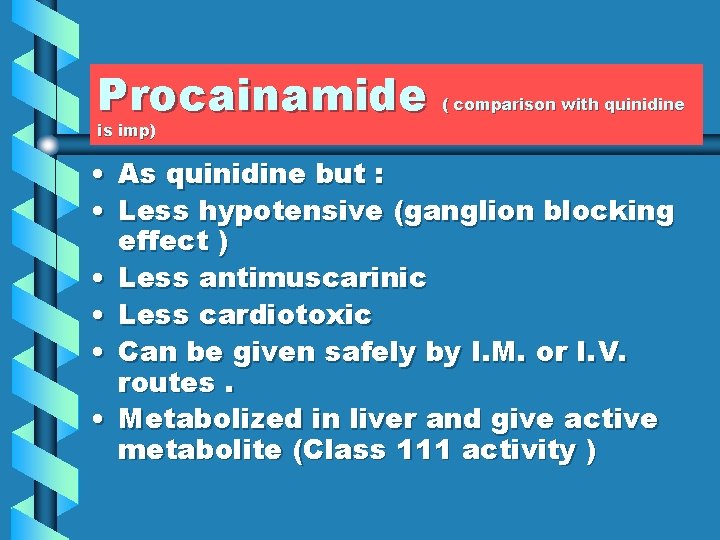
Procainamide ( comparison with quinidine is imp) • As quinidine but : • Less hypotensive (ganglion blocking effect ) • Less antimuscarinic • Less cardiotoxic • Can be given safely by I. M. or I. V. routes. • Metabolized in liver and give active metabolite (Class 111 activity )
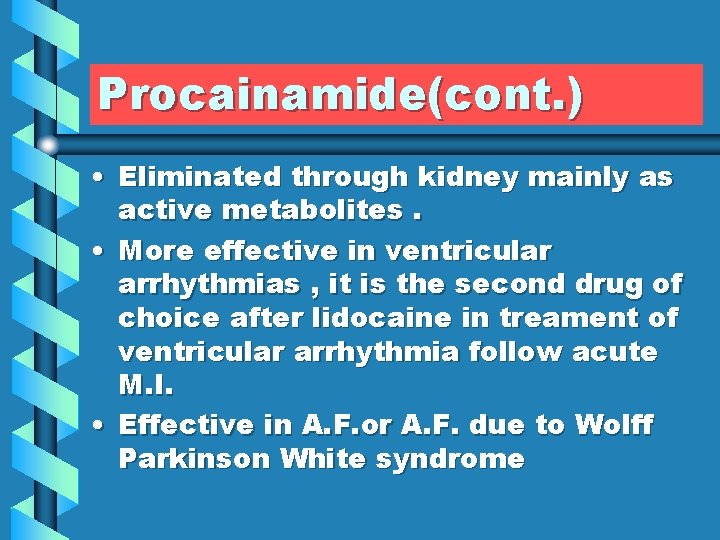
Procainamide(cont. ) • Eliminated through kidney mainly as active metabolites. • More effective in ventricular arrhythmias , it is the second drug of choice after lidocaine in treament of ventricular arrhythmia follow acute M. I. • Effective in A. F. or A. F. due to Wolff Parkinson White syndrome
Wolff-Parkinson-White syndrome ( ) ﻟﻠﻔﺎﺋﺪﺓ • (WPW) is a syndrome of preexcitation of the ventricles of the heart due to an accessory pathway known as the Bundle of Kent. • This accessory pathway is an abnormal electrical communication from the atria to the ventricles

Adverse effects • Systemic lupus erythematosus like syndrome. (occur mainly in some people who have problems in acetylating drug) • GIT : Nausea diarrhea • Torsade de pointes
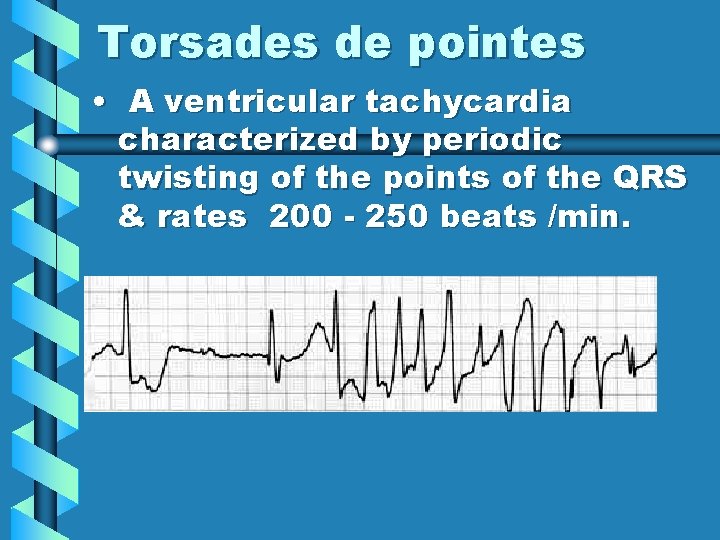
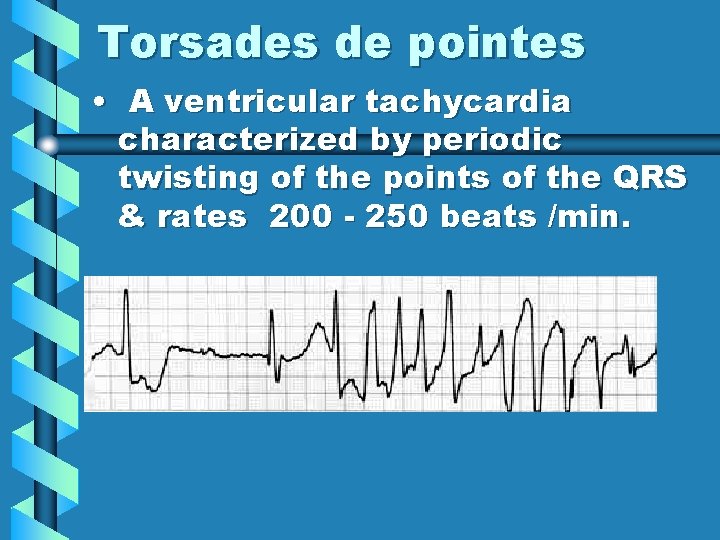
Torsades de pointes • A ventricular tachycardia characterized by periodic twisting of the points of the QRS & rates 200 - 250 beats /min.
Disopyramide • As quinidine but : • Has marked antimuscarinic effect. • Is only available for oral use • In renal impairment dosage must be adjusted
Adverse effects • Can precipitate all of the electrophysiologic disturbance as quinidine. • Potent –Ve inotropic effect on heart may cause heart failure. • Antimuscarinic effects
Contraindications • Heart failure • Glaucoma • Prostatic hypertrophy • Constipation • Sick sinus syndrome
Clinical uses • Used only (main use)for the treatment of ventricular arrhythmias.
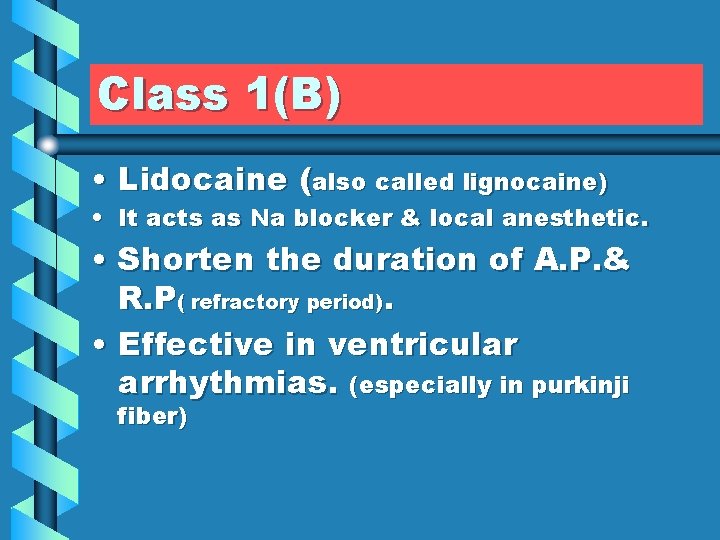
Class 1(B) • Lidocaine (also called lignocaine) • It acts as Na blocker & local anesthetic. • Shorten the duration of A. P. & R. P( refractory period). • Effective in ventricular arrhythmias. (especially in purkinji fiber)
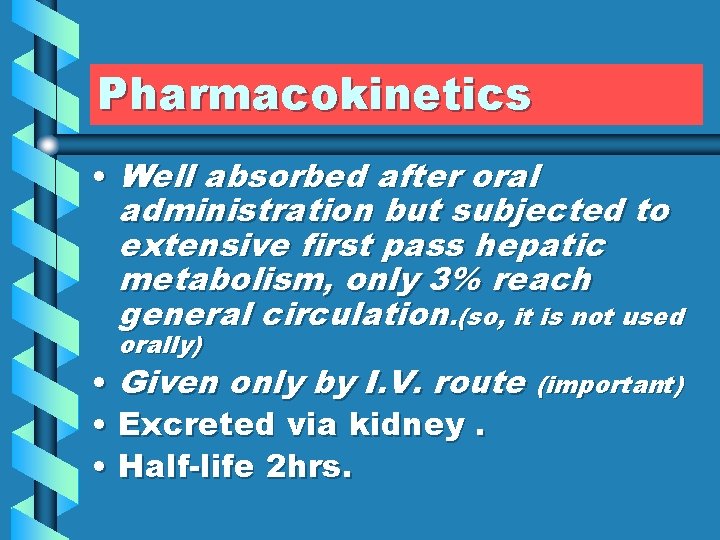
Pharmacokinetics • Well absorbed after oral administration but subjected to extensive first pass hepatic metabolism, only 3% reach general circulation. (so, it is not used orally) • Given only by I. V. route (important) • Excreted via kidney. • Half-life 2 hrs.
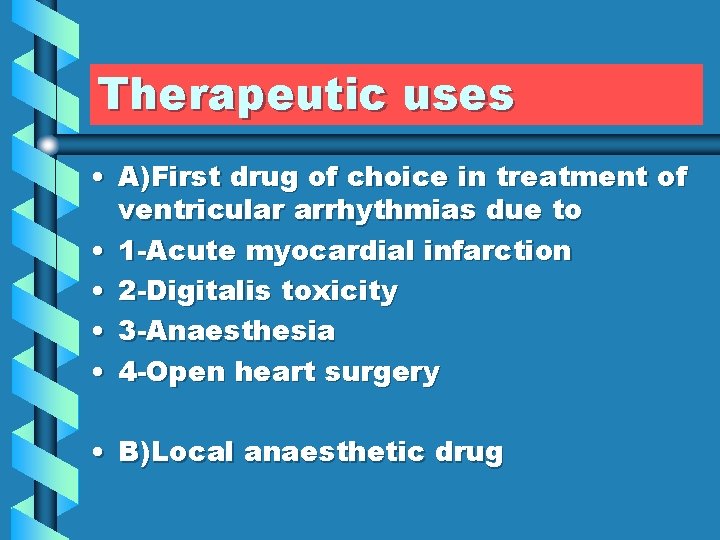
Therapeutic uses • A)First drug of choice in treatment of ventricular arrhythmias due to • 1 -Acute myocardial infarction • 2 -Digitalis toxicity • 3 -Anaesthesia • 4 -Open heart surgery • B)Local anaesthetic drug
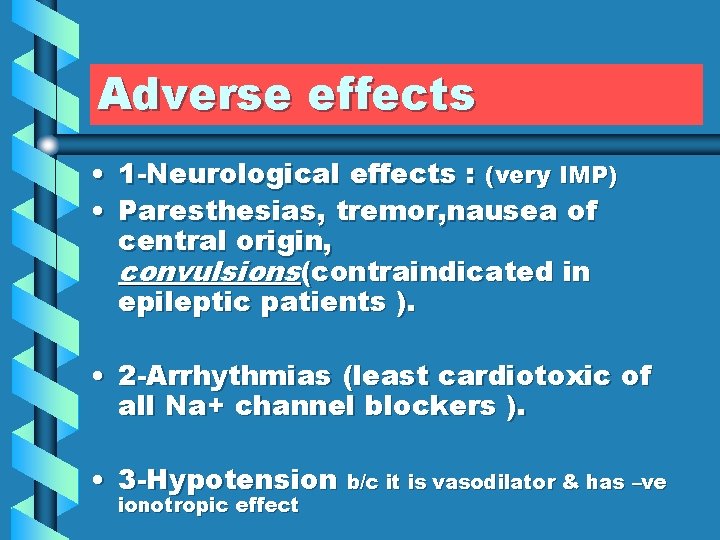
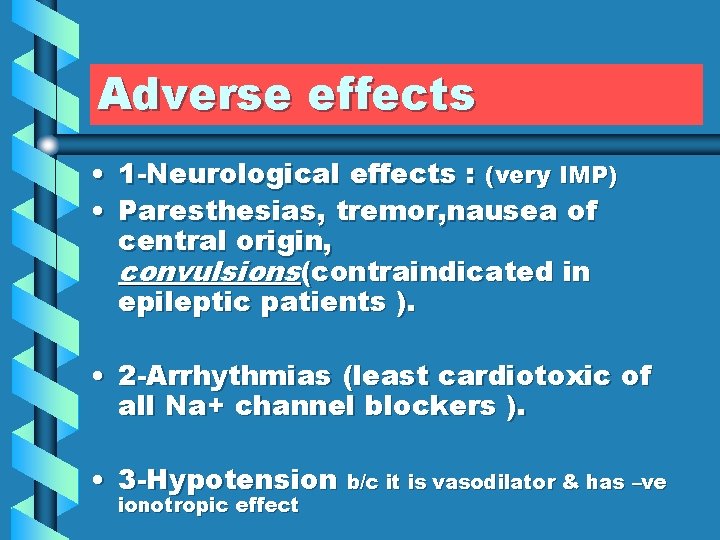
Adverse effects • 1 -Neurological effects : (very IMP) • Paresthesias, tremor, nausea of central origin, convulsions(contraindicated in epileptic patients ). • 2 -Arrhythmias (least cardiotoxic of all Na+ channel blockers ). • 3 -Hypotension b/c it is vasodilator & has –ve ionotropic effect
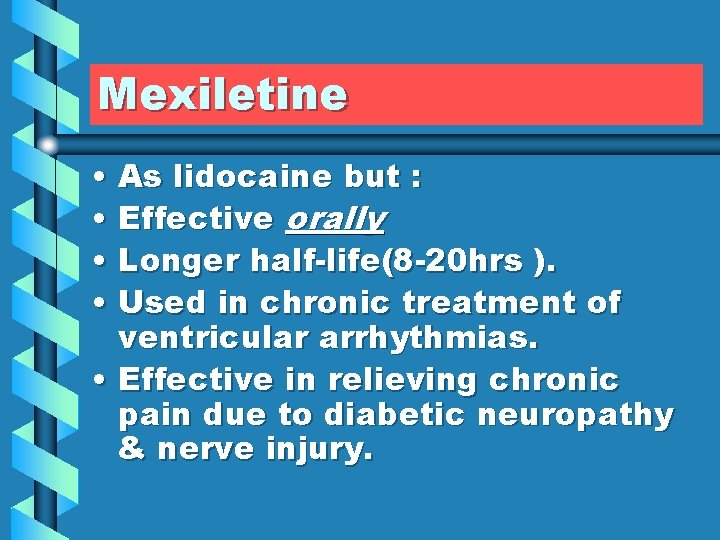
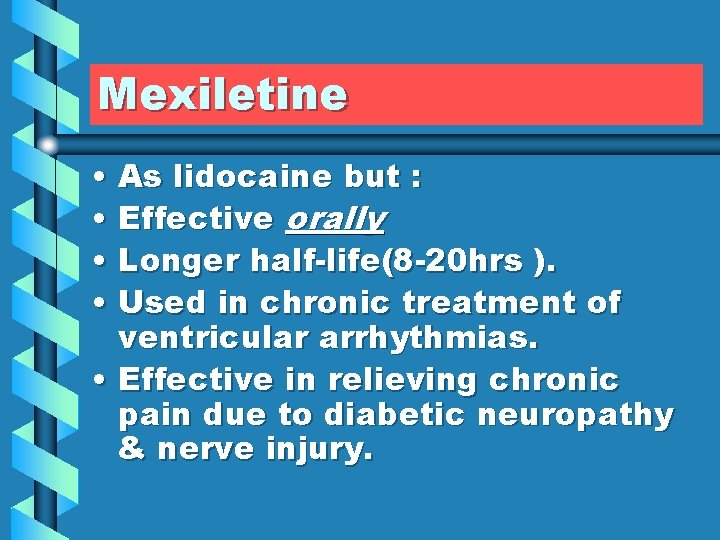
Mexiletine • As lidocaine but : • Effective orally • Longer half-life(8 -20 hrs ). • Used in chronic treatment of ventricular arrhythmias. • Effective in relieving chronic pain due to diabetic neuropathy & nerve injury.
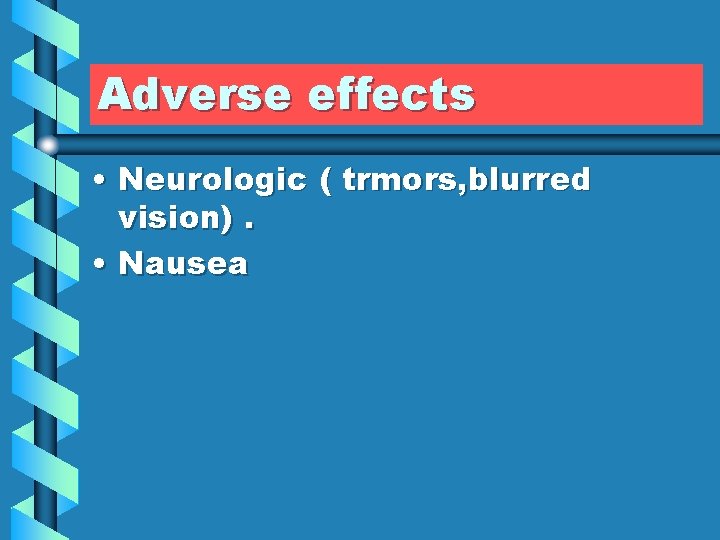
Adverse effects • Neurologic ( trmors, blurred vision). • Nausea
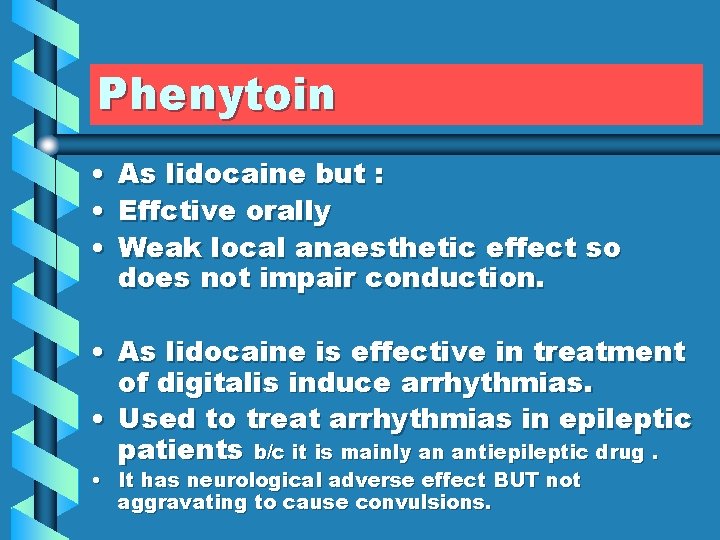
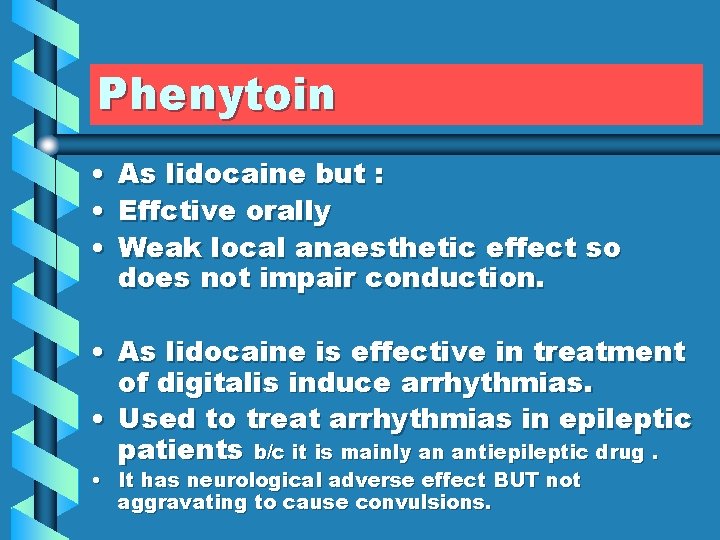
Phenytoin • • • As lidocaine but : Effctive orally Weak local anaesthetic effect so does not impair conduction. • As lidocaine is effective in treatment of digitalis induce arrhythmias. • Used to treat arrhythmias in epileptic patients b/c it is mainly an antiepileptic drug. • It has neurological adverse effect BUT not aggravating to cause convulsions.
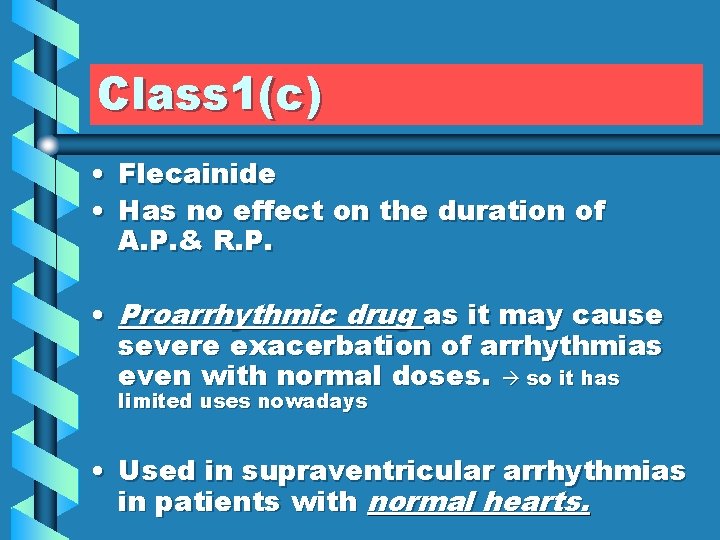
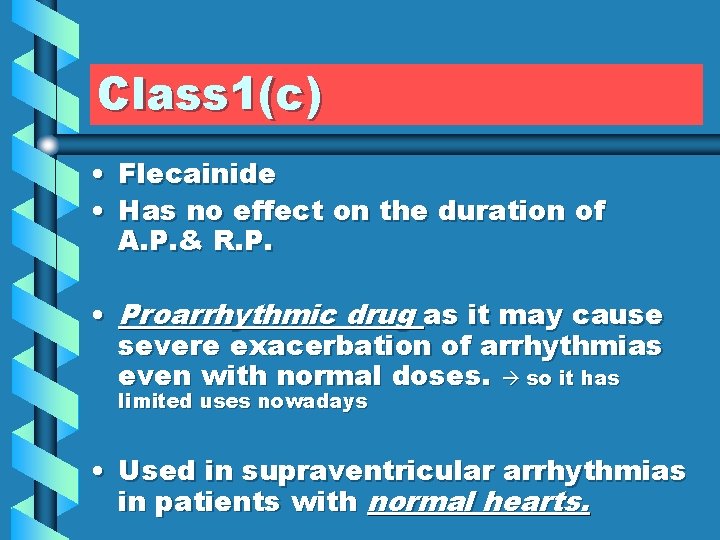
Class 1(c) • Flecainide • Has no effect on the duration of A. P. & R. P. • Proarrhythmic drug as it may cause severe exacerbation of arrhythmias even with normal doses. so it has limited uses nowadays • Used in supraventricular arrhythmias in patients with normal hearts.
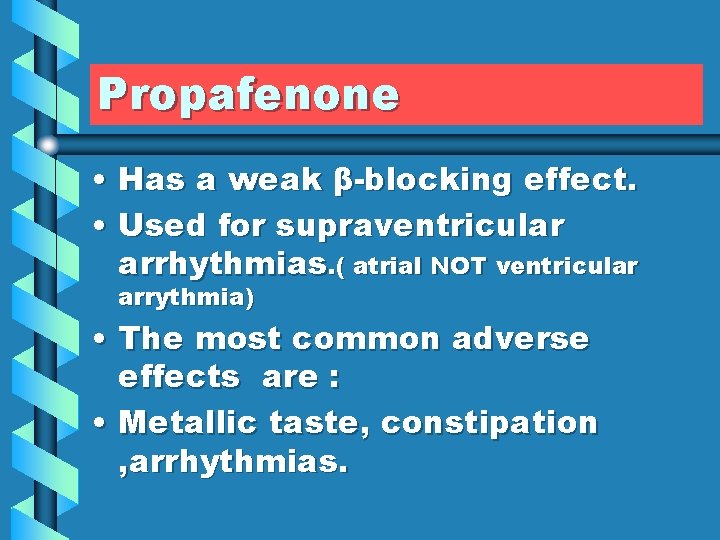
Propafenone • Has a weak β-blocking effect. • Used for supraventricular arrhythmias. ( atrial NOT ventricular arrythmia) • The most common adverse effects are : • Metallic taste, constipation , arrhythmias.
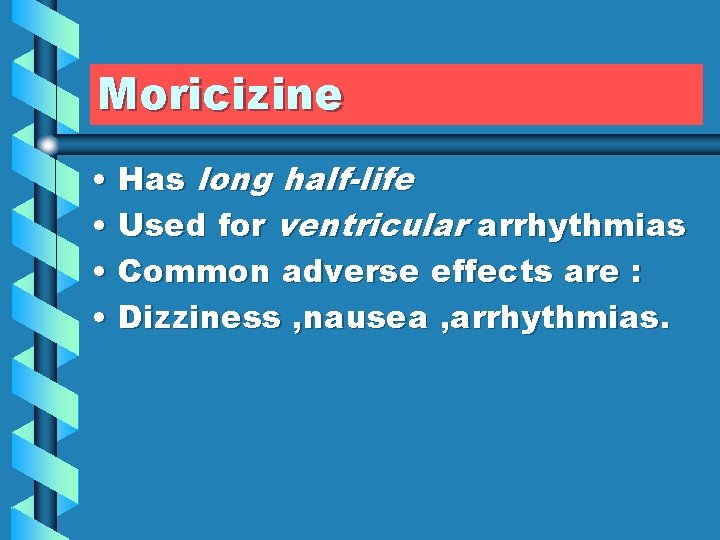
Moricizine • Has long half-life • Used for ventricular arrhythmias • Common adverse effects are : • Dizziness , nausea , arrhythmias.
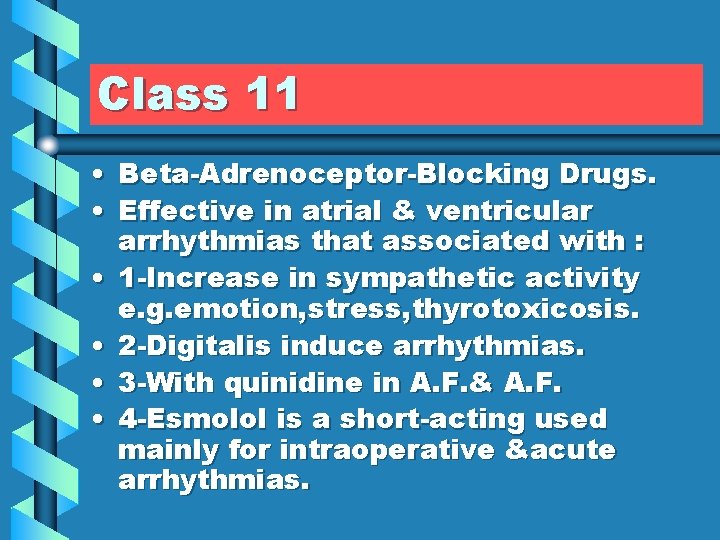
Class 11 • Beta-Adrenoceptor-Blocking Drugs. • Effective in atrial & ventricular arrhythmias that associated with : • 1 -Increase in sympathetic activity e. g. emotion, stress, thyrotoxicosis. • 2 -Digitalis induce arrhythmias. • 3 -With quinidine in A. F. & A. F. • 4 -Esmolol is a short-acting used mainly for intraoperative ´ arrhythmias.


Class 111 • Potassium channel blockers • ( Drugs that Prolong duration of action potential & refractory period ).
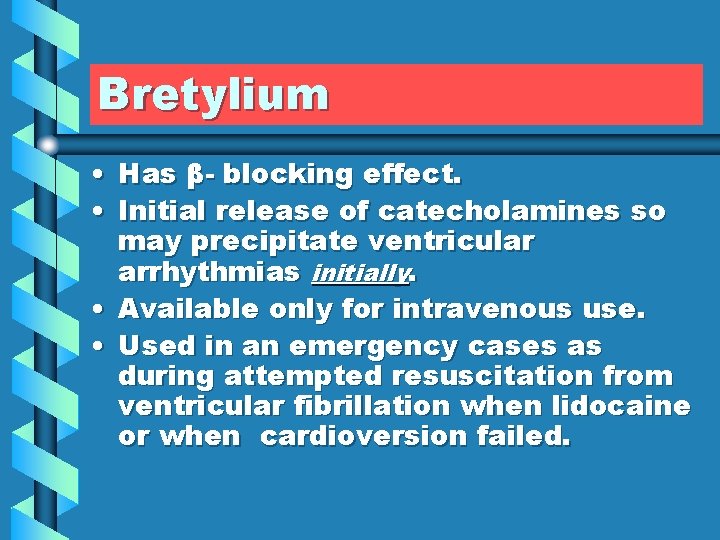
Bretylium • Has β- blocking effect. • Initial release of catecholamines so may precipitate ventricular arrhythmias initially. • Available only for intravenous use. • Used in an emergency cases as during attempted resuscitation from ventricular fibrillation when lidocaine or when cardioversion failed.

Adverse effects • Arrhythmias • Postural hypotension b/c 1 - direct action 2 - release of catecholamine • It has β-blocking effect. • Nausea & vomiting not important side effect b/c it is given IV emergency.
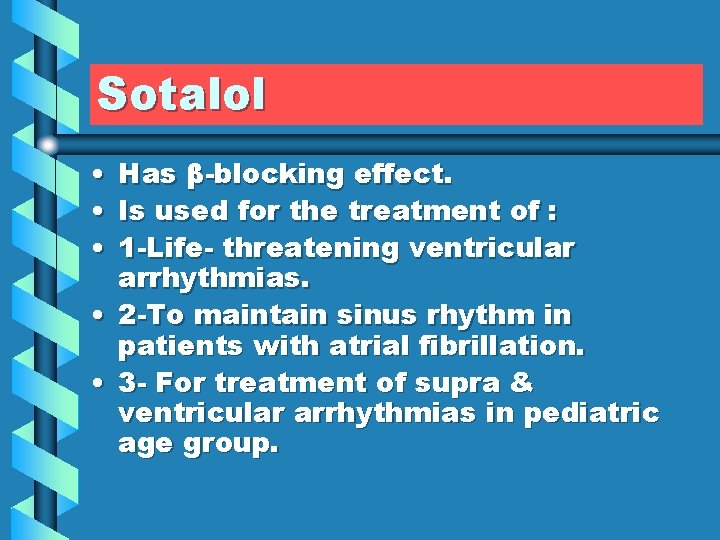
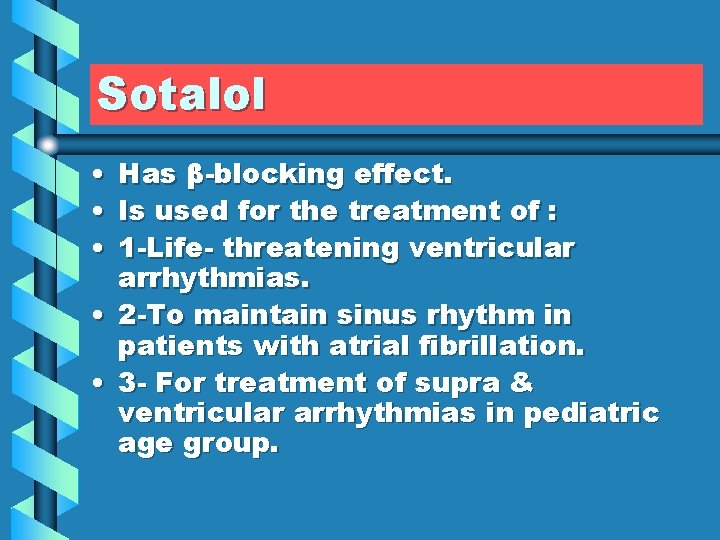
Sotalol • • • Has β-blocking effect. Is used for the treatment of : 1 -Life- threatening ventricular arrhythmias. • 2 -To maintain sinus rhythm in patients with atrial fibrillation. • 3 - For treatment of supra & ventricular arrhythmias in pediatric age group.
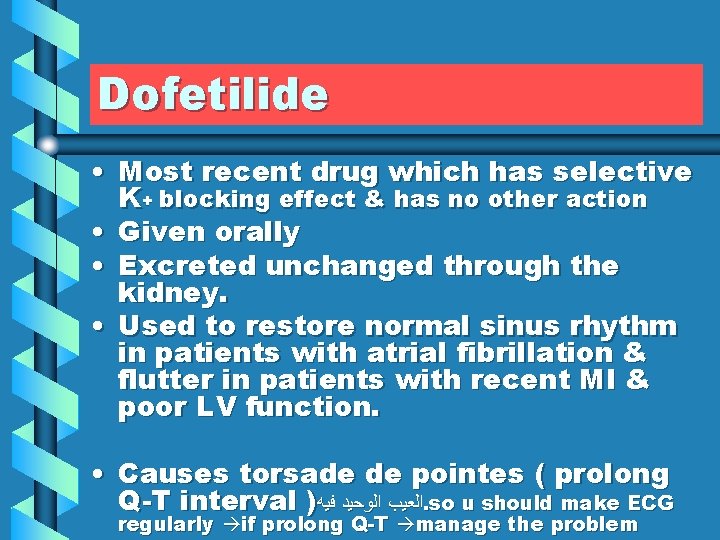
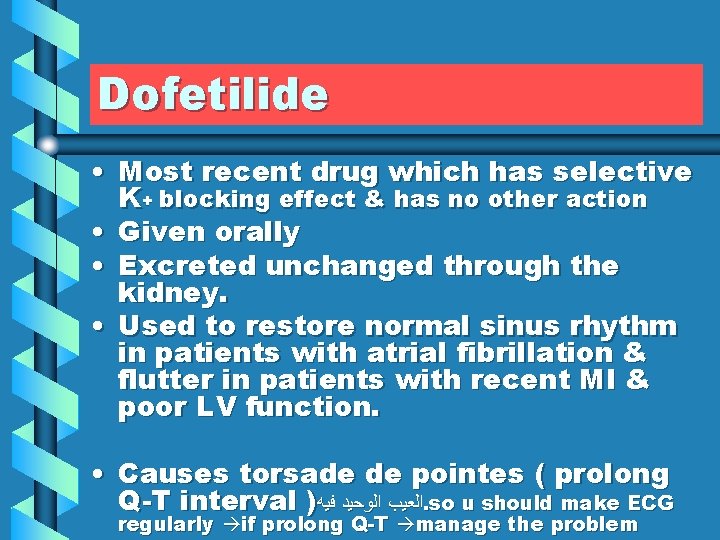
Dofetilide • Most recent drug which has selective K+ blocking effect & has no other action • Given orally • Excreted unchanged through the kidney. • Used to restore normal sinus rhythm in patients with atrial fibrillation & flutter in patients with recent MI & poor LV function. • Causes torsade de pointes ( prolong Q-T interval ) ﺍﻟﻌﻴﺐ ﺍﻟﻮﺣﻴﺪ ﻓﻴﻪ. so u should make ECG regularly if prolong Q-T manage the problem
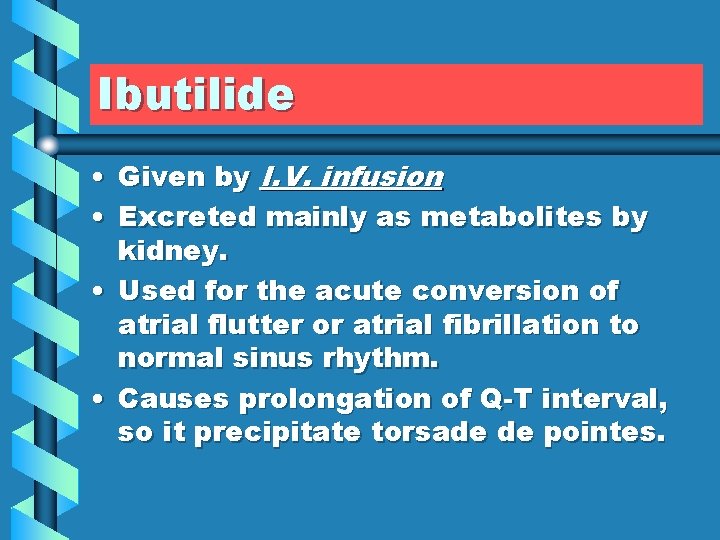
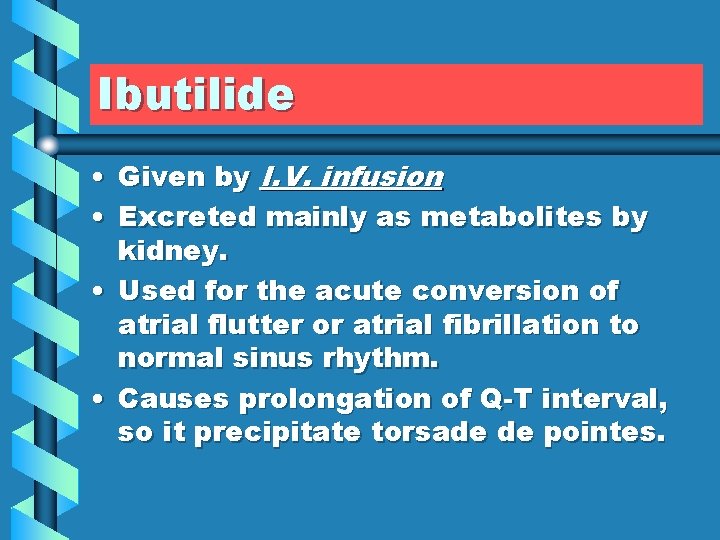
Ibutilide • Given by I. V. infusion • Excreted mainly as metabolites by kidney. • Used for the acute conversion of atrial flutter or atrial fibrillation to normal sinus rhythm. • Causes prolongation of Q-T interval, so it precipitate torsade de pointes.
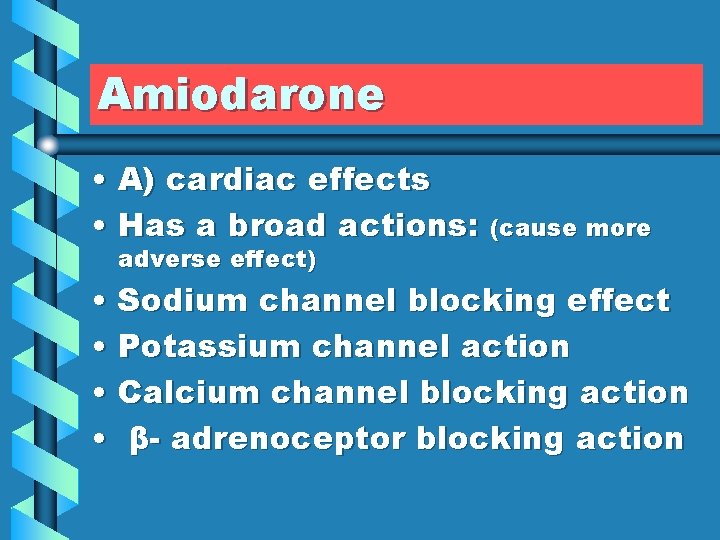
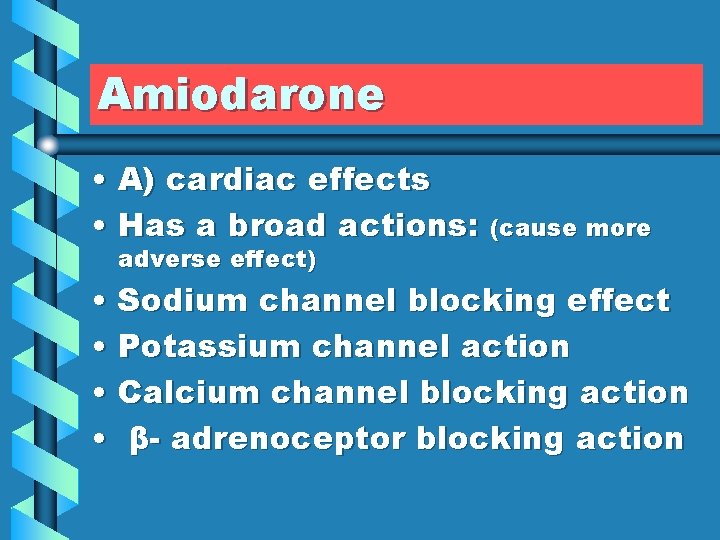
Amiodarone • A) cardiac effects • Has a broad actions: (cause more adverse effect) • Sodium channel blocking effect • Potassium channel action • Calcium channel blocking action • β- adrenoceptor blocking action
Amiodarone(cont. ) • B) Extracardiac effect • Peripheral vasodilation
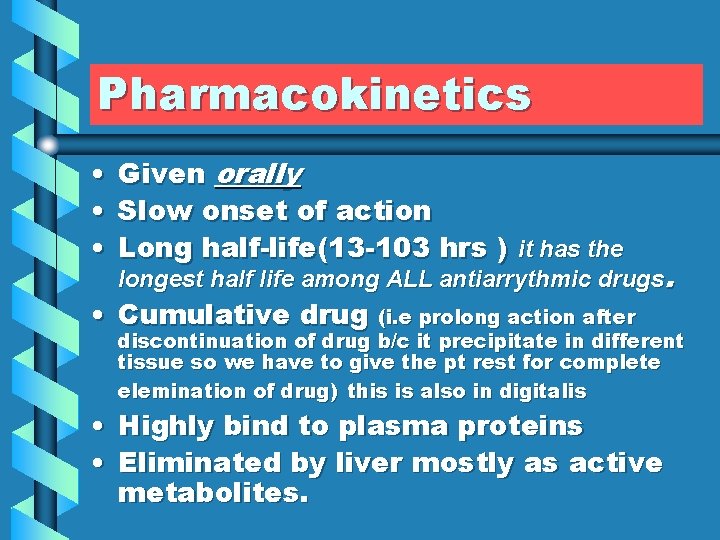
Pharmacokinetics • • • Given orally Slow onset of action Long half-life(13 -103 hrs ) it has the longest half life among ALL antiarrythmic drugs. • Cumulative drug (i. e prolong action after • • discontinuation of drug b/c it precipitate in different tissue so we have to give the pt rest for complete elemination of drug) this is also in digitalis Highly bind to plasma proteins Eliminated by liver mostly as active metabolites.
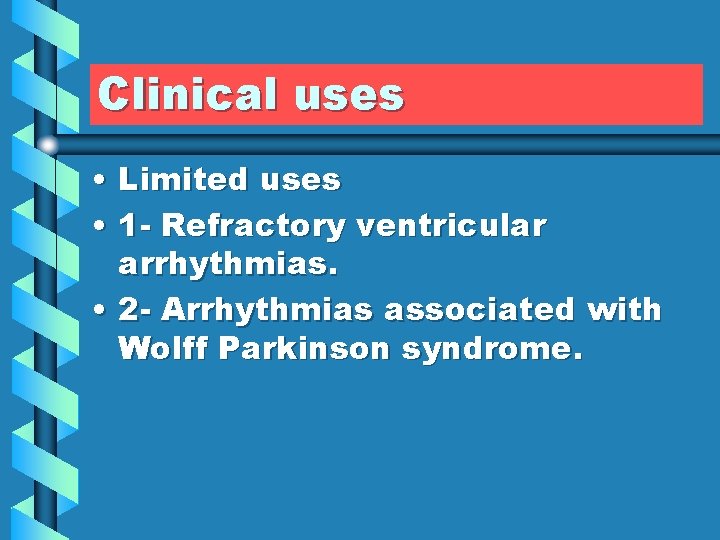
Clinical uses • Limited uses • 1 - Refractory ventricular arrhythmias. • 2 - Arrhythmias associated with Wolff Parkinson syndrome.

Adverse effects • 1 - Gray- blue skin discoloration & photodermatitis. • 2 -Corneal microdeposits corneal opacity , optic neuritis, blindness , yellowish brown haloes. (in digitalis pink to orange haloes) • 3 -pulmonary fibrosis (if precipitate in lung)
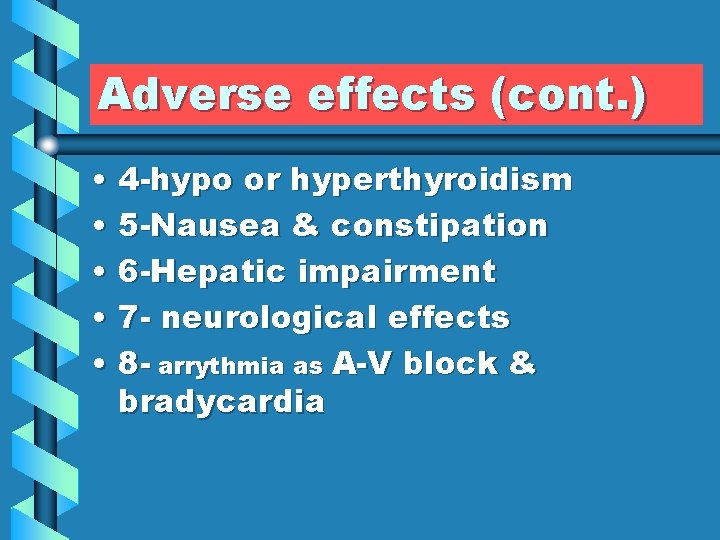
Adverse effects (cont. ) • 4 -hypo or hyperthyroidism • 5 -Nausea & constipation • 6 -Hepatic impairment • 7 - neurological effects • 8 - arrythmia as A-V block & bradycardia
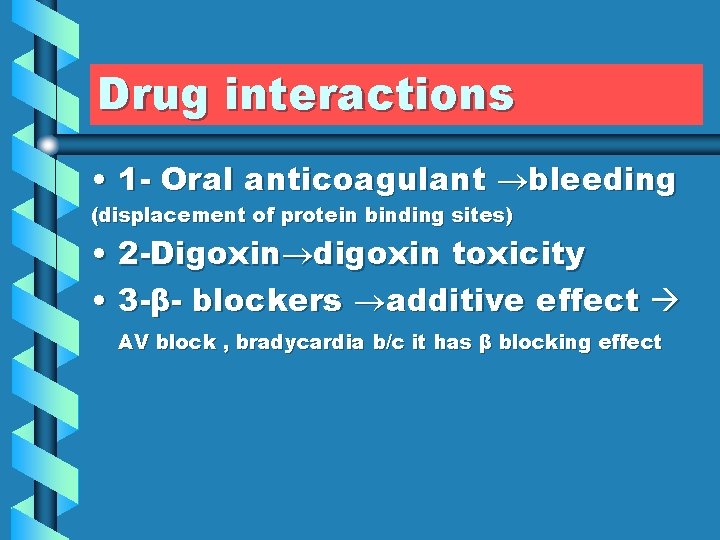
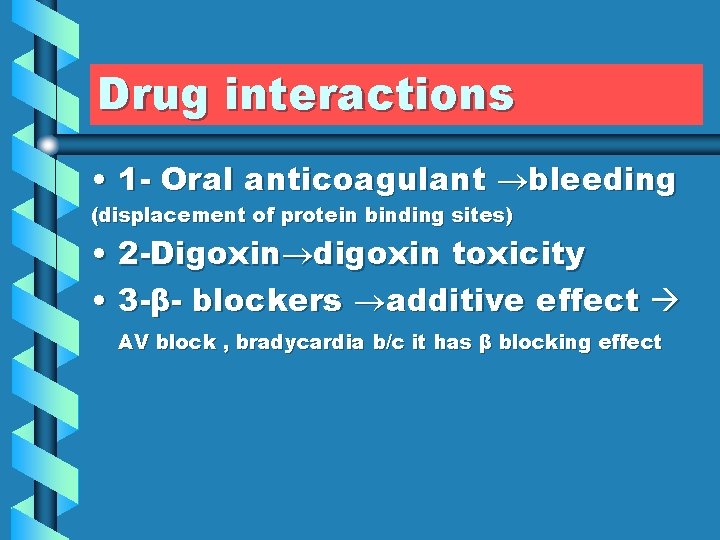
Drug interactions • 1 - Oral anticoagulant bleeding (displacement of protein binding sites) • 2 -Digoxin digoxin toxicity • 3 -β- blockers additive effect AV block , bradycardia b/c it has β blocking effect
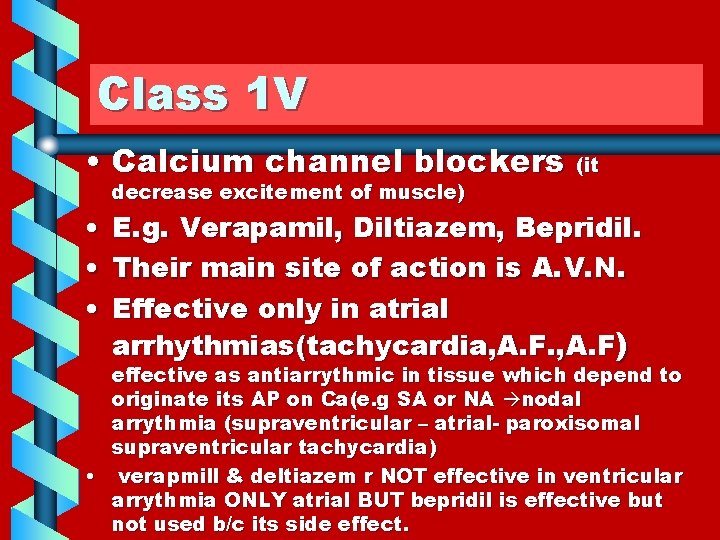
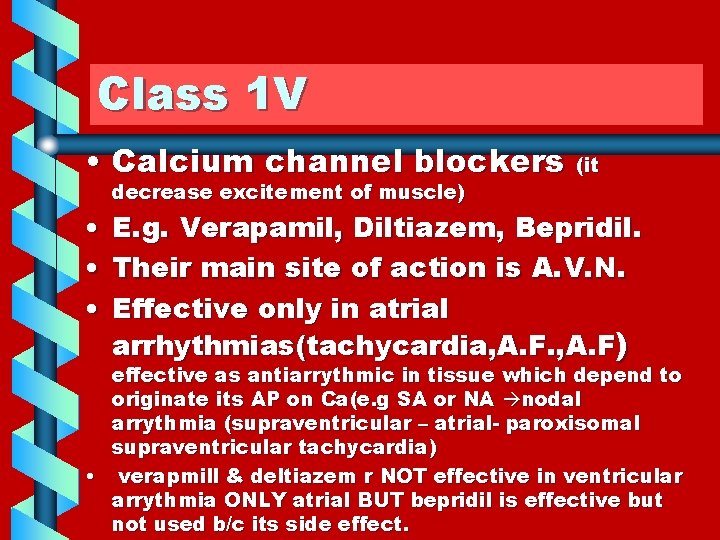
Class 1 V • Calcium channel blockers (it decrease excitement of muscle) • E. g. Verapamil, Diltiazem, Bepridil. • Their main site of action is A. V. N. • Effective only in atrial arrhythmias(tachycardia, A. F) effective as antiarrythmic in tissue which depend to originate its AP on Ca(e. g SA or NA nodal arrythmia (supraventricular – atrial- paroxisomal supraventricular tachycardia) • verapmill & deltiazem r NOT effective in ventricular arrythmia ONLY atrial BUT bepridil is effective but not used b/c its side effect.
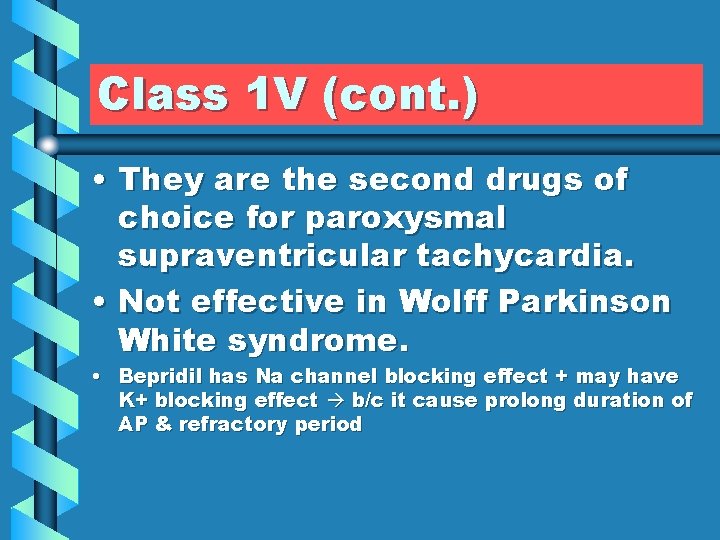
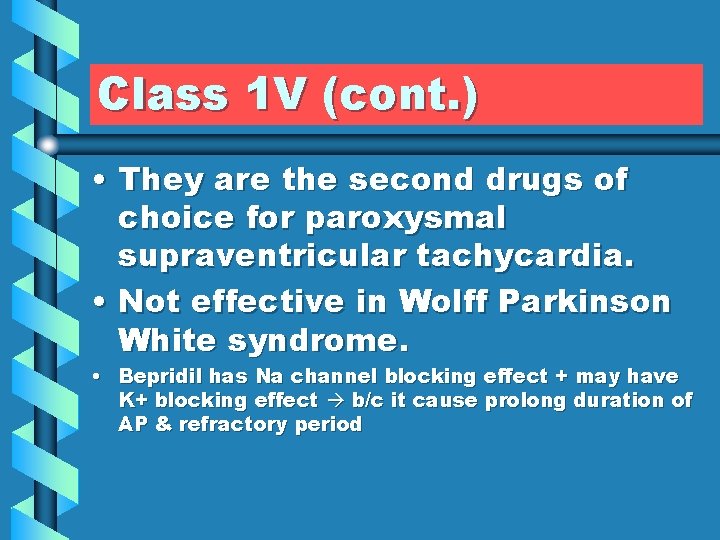
Class 1 V (cont. ) • They are the second drugs of choice for paroxysmal supraventricular tachycardia. • Not effective in Wolff Parkinson White syndrome. • Bepridil has Na channel blocking effect + may have K+ blocking effect b/c it cause prolong duration of AP & refractory period
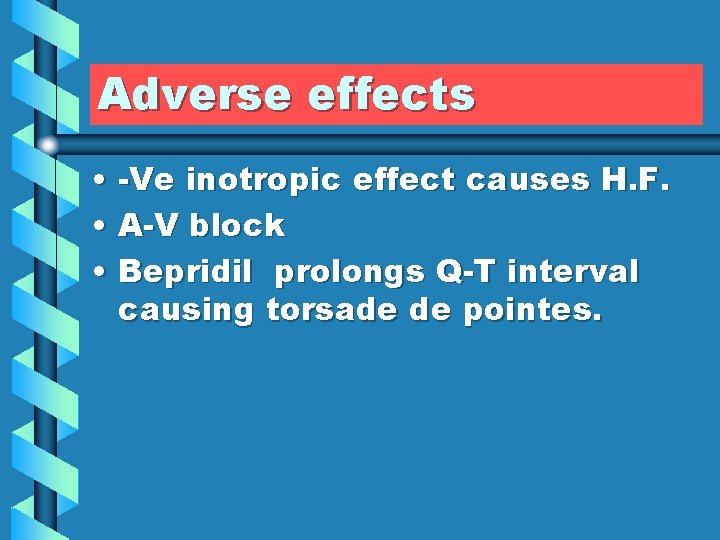
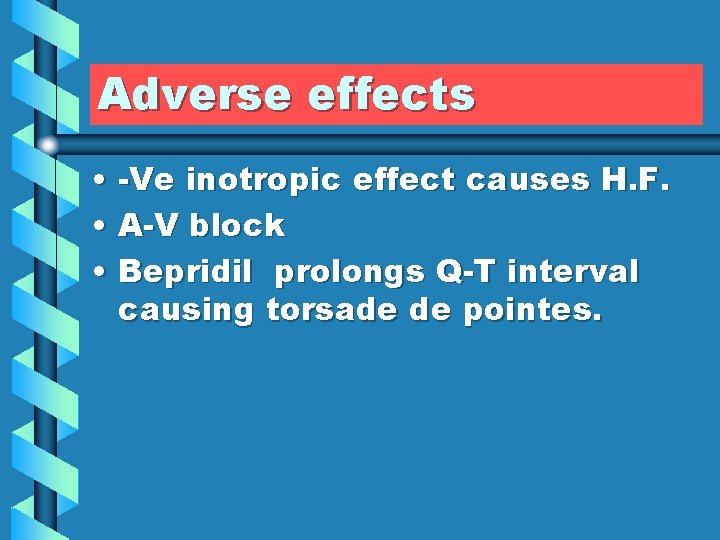
Adverse effects • -Ve inotropic effect causes H. F. • A-V block • Bepridil prolongs Q-T interval causing torsade de pointes.
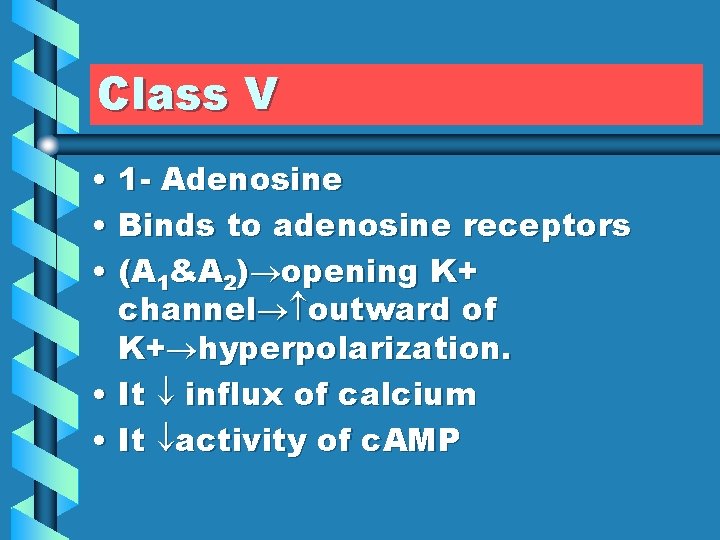
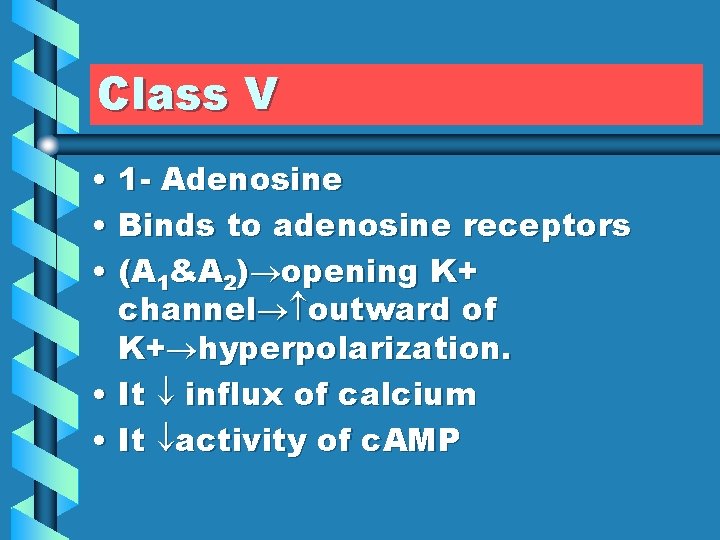
Class V • 1 - Adenosine • Binds to adenosine receptors • (A 1&A 2) opening K+ channel outward of K+ hyperpolarization. • It influx of calcium • It activity of c. AMP
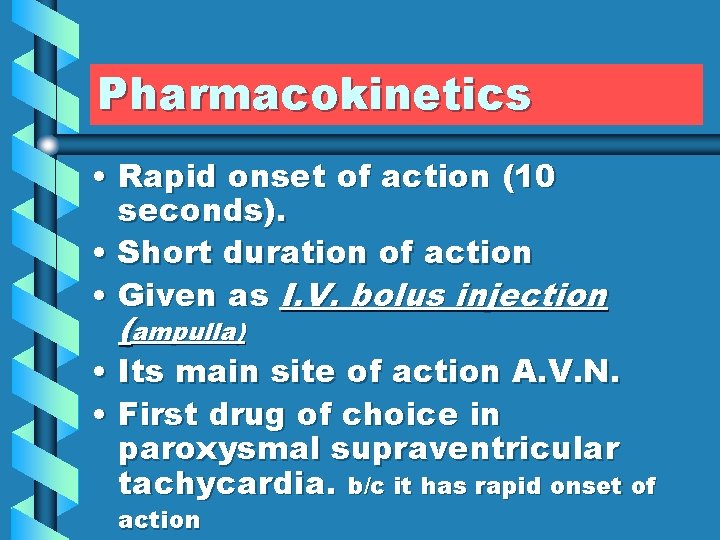
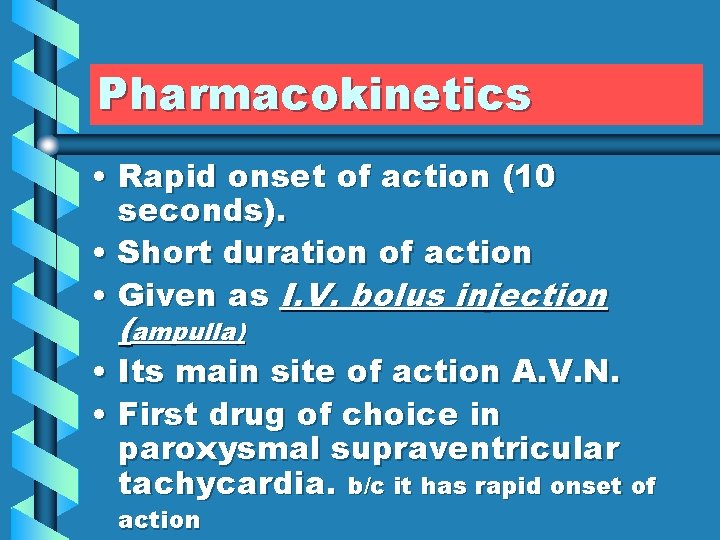
Pharmacokinetics • Rapid onset of action (10 seconds). • Short duration of action • Given as I. V. bolus injection (ampulla) • Its main site of action A. V. N. • First drug of choice in paroxysmal supraventricular tachycardia. b/c it has rapid onset of action
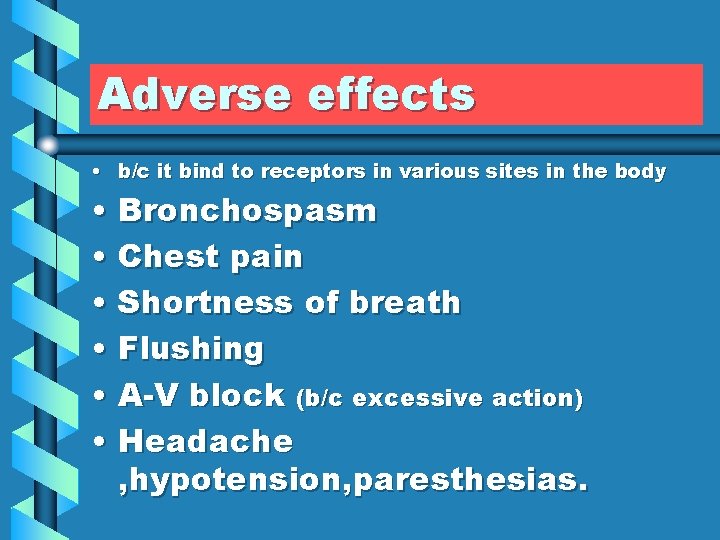
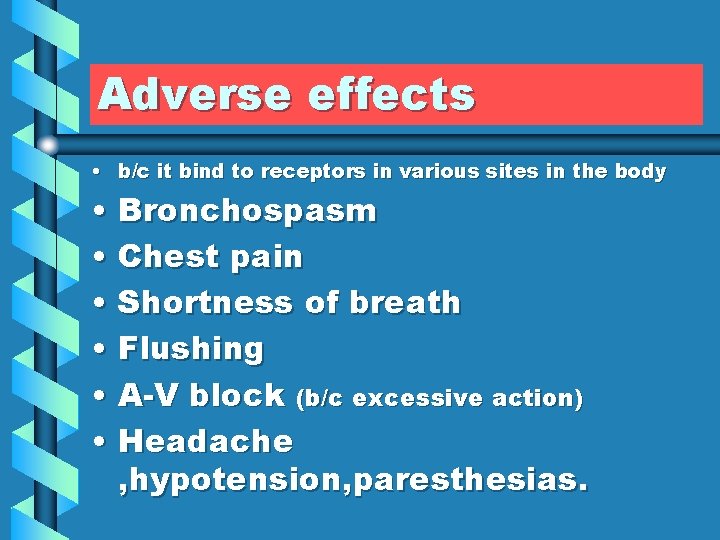
Adverse effects • b/c it bind to receptors in various sites in the body • Bronchospasm • Chest pain • Shortness of breath • Flushing • A-V block (b/c excessive action) • Headache , hypotension, paresthesias.
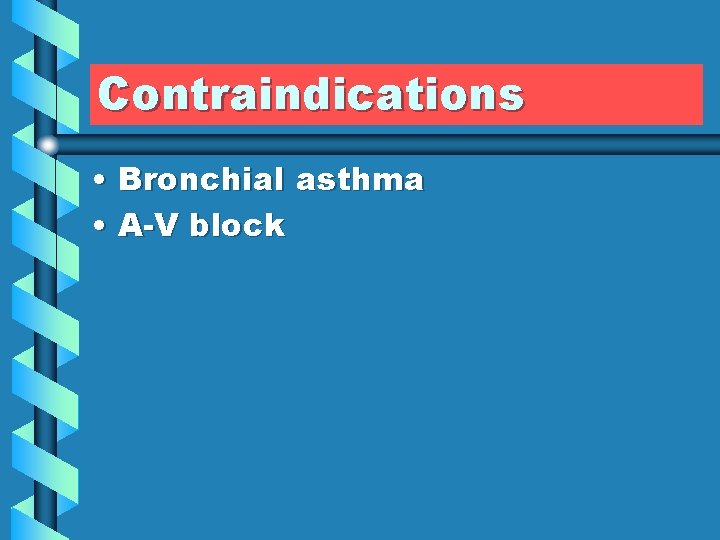
Contraindications • Bronchial asthma • A-V block

Drug interactions • 1 - With Caffeine or theophylline • Adenosine is less effective (They are adenosine receptor blockers ). • 2 - With dipyridamole is more effective (As it inhibits adenosine uptake ).

Magnesium • By unknown mechanism • Used in: • 1 - Digitalis induced arrhythmias • 2 -Torsade de pointes • 3 -Sinus tachycardia
Potassium • By unknown mechanism • Used in: • Digitalis induced arrhythmias
 Refractory period cardiac
Refractory period cardiac Heart sounds and murmurs
Heart sounds and murmurs Chronotropic
Chronotropic Normal beats per minute by age
Normal beats per minute by age Radial pulse range
Radial pulse range Orthopnue
Orthopnue 139
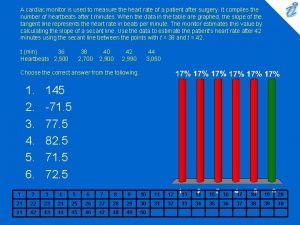
139 A cardiac monitor is used to measure
A cardiac monitor is used to measure Quick breads belong to what group in the food pyramid
Quick breads belong to what group in the food pyramid Drop batters
Drop batters Leavening agents used in quick breads
Leavening agents used in quick breads Preparation of monophasic liquid dosage form
Preparation of monophasic liquid dosage form Diagnostic agents are the compounds used to
Diagnostic agents are the compounds used to Spirit is
Spirit is Heart border percussion of heart
Heart border percussion of heart How to dissect a sheep heart
How to dissect a sheep heart Stars plowhorses puzzles dogs
Stars plowhorses puzzles dogs Normal heart
Normal heart Hymen
Hymen Nichd category
Nichd category Iht spirit heart rate monitors
Iht spirit heart rate monitors Resting heart rate women
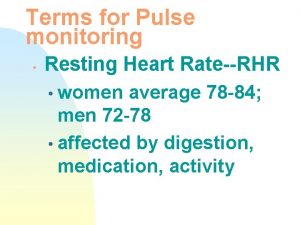
Resting heart rate women Target heart rate zone
Target heart rate zone Heart rate during exercise
Heart rate during exercise Heart rate of 80 bpm
Heart rate of 80 bpm Athletic heart rate
Athletic heart rate Apical pulse location
Apical pulse location Ominous periodic change in the fetal heart rate
Ominous periodic change in the fetal heart rate Spo2 normal range by age chart
Spo2 normal range by age chart Normal bowel sound
Normal bowel sound Sinusoidal ctg
Sinusoidal ctg Anaerobic zone
Anaerobic zone Athlete resting heart rate
Athlete resting heart rate Veal chop fht
Veal chop fht Sinusoidal fetal heart rate
Sinusoidal fetal heart rate Heart rate during exercise
Heart rate during exercise Can music affect heart rate
Can music affect heart rate Purpose of circuit training
Purpose of circuit training Heart rate during exercise
Heart rate during exercise Cardiac output trained vs untrained
Cardiac output trained vs untrained How to calculate heart rate from ecg with irregular rhythm
How to calculate heart rate from ecg with irregular rhythm Pseudoephedrine heart rate
Pseudoephedrine heart rate Target heart rate formula
Target heart rate formula Maximal heart rate
Maximal heart rate American researcher who involved in getting heart rate
American researcher who involved in getting heart rate How to calculate heart rate from ecg
How to calculate heart rate from ecg Examples of physiological indicators
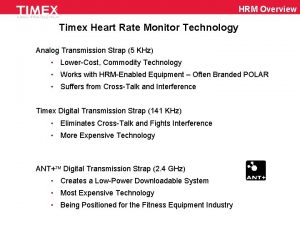
Examples of physiological indicators Timex digital flex tech hrm sensor
Timex digital flex tech hrm sensor Daphnia heart rate lab
Daphnia heart rate lab What is a healthy heart rate?
What is a healthy heart rate? What is a healthy heart rate?
What is a healthy heart rate? Metallica total eclipse of the heart
Metallica total eclipse of the heart Abbreviation for temporal temperature
Abbreviation for temporal temperature What is a healthy heart rate?
What is a healthy heart rate? Rpe means
Rpe means Maximal heart rate
Maximal heart rate Site of pulse
Site of pulse What is maximum heart rate
What is maximum heart rate Polargofit
Polargofit Category 1 tracing
Category 1 tracing Slow heart rate
Slow heart rate Russel jel
Russel jel Heart rate line
Heart rate line Intrapartum meaning
Intrapartum meaning Basal metabolic rate
Basal metabolic rate Vitals normal ranges
Vitals normal ranges